Abstract
Cannabidiol (CBD), a specialized metabolite (phytocannabinoid) abundant in Cannabis sativa, is attracting increasing attention for its alleged health-promoting properties. The present study aimed to investigate the pharmacokinetics of CBD and its primary metabolite, 7‐hydroxy‐cannabidiol (7-OH-CBD), following a single oral dose of a CBD-rich Cannabis sativa extract, equivalent to 70 mg CBD, in healthy male (n=5) and female (n=6) participants. Using a randomized crossover design, the study evaluated the impact of a standardized high-fat meal compared to fasting on the oral bioavailability of CBD. Consumption of a high-fat meal significantly increases the bioavailability of CBD. The geometric mean ratio (GMR) of CBD Cmax was 17.4 (90% CI 12.4–24.2 and of the AUC 9.7 (90% CI 7.7–12.3), demonstrating a substantial increase in peak concentration and total CBD exposure under fed conditions. A notable double peak phenomenon was observed after meal consumption, with a less pronounced effect in the fasted state. This contributes to sustained high plasma concentrations and may be (partially) attributed to lymphatic transport, enterohepatic recirculation, and/or a secondary meal effect.
This trial was registered on October 19, 2020, with ClinicalTrials.gov under the identifier NCT04589455. The registration title is: Determination of Pharmacokinetics and Food-effect of CBD from a Hemp Extract in Healthy Human Volunteers.
Similar content being viewed by others
Introduction
The plant Cannabis sativa is extremely rich in specialized (‘secondary’) metabolites, of which more than 130 with a typical terpenophenolic, referred to as (phyto-)cannabinoid, structure have been described1. Of these, the most commonly known are delta-9 tetrahydrocannabinol (THC) and cannabidiol (CBD). THC is responsible for the psychotropic effects of cannabis, producing the “high” associated with its use, whereas CBD is non-psychotropic. CBD is currently gaining considerable attention because of its claimed pharmacological and health-promoting properties, its low abuse potential, and its favorable safety profile2,3,4. For the extraction of CBD from cannabis plants, the flowers or leaves are typically used, yielding a mixture of bioactive compounds, including cannabinoids, terpenes, and flavonoids. From this mixture, CBD can be extracted to a high degree of purity. Additionally, full-spectrum extracts (which may contain trace amounts of THC) or a broad-spectrum (without THC) extract are produced, collectively referred to as ‘plant-identical’ extracts. In addition to plant-derived CBD products, there is increasing use of chemically synthesized CBD, for which several methods have become available5. In current practice, ‘natural’ CBD and synthetic CBD are used side by side in preparations, irrespective of their classification as ‘food supplements’ or medicinal products.
In most European countries, CBD currently reaches patients (or consumers) through two distinct channels. First, CBD is an ingredient in approved medicinal products, primarily used for neurological indications. The oral CBD product Epidyolex® is approved by several authorities, including EMA and FDA, and is used to treat patients from the age of two years with certain forms of refractory epilepsy, Lennox-Gastaut syndrome, and Dravet syndrome6,7. Recommended doses range from 2.5 mg/kg twice daily as a starting dose, to a maximum of 10 mg/kg twice daily during maintenance therapy. The oromucosal spray Sativex®, containing both THC and CBD, has been approved to alleviate symptoms in adult patients with moderate to severe spasticity resulting from Multiple Sclerosis (MS)8. Additionally, CBD preparations can be prescribed by doctors and delivered through pharmacies for the management of conditions involving pain, inflammation, or other immune-related factors9,10. Second, there is a variety of CBD preparations available online, through drugstores or other retail outlets, which in many countries are unofficially classified as food supplements. In general, these products contain a small quantity of CBD, less than 100 mg per dose, and in some cases only a fraction of that. In the European Union, the classification of CBD as a food supplement conflicts with food legislation because CBD has not been granted the required ‘novel food’ status. In 2022, EFSA issued a formal opinion stating “Considering the significant uncertainties and data gaps, the EFSA panel concludes that the safety of CBD as a novel food cannot currently be established11. Consequently, no health claims can be submitted, and these OTC products lack indications for use. Despite this, there is widespread use of low-dose CBD-containing preparations among the general public, which also underlines the need for more insight into the pharmacokinetics of CBD from such preparations, particularly concerning full-spectrum and broad-spectrum extracts. Additionally, there is growing interest in factors that may influence CBD pharmacokinetic parameters, including the impact of food.
Regarding pharmacokinetics, the majority of studies focus on the pharmacokinetics of pure CBD oil. However, a host of other constituents, including flavonoids and a relatively high number of terpenes, are present in Cannabis, which may impact CBD’s bioavailability. As an example, the sesquiterpenes ß-caryophyllene and α-humulene, present in our extract (see Supplemental Table S1), have been described to inhibit the liver metabolizing enzyme CYP3A412,13,14. Despite several theories, the precise significance of these compounds for the bioavailability of CBD is not known15. CBD is known to be highly lipophilic, poorly water-soluble, and may therefore be classified as a class II compound in the Biopharmaceutical Classification System16,17,18. Upon oral administration, CBD may precipitate in the gastrointestinal tract, leading to a low absorption rate19.In addition to its low absorption rate, a significant first-pass metabolism contributes to a poor oral bioavailability of approximately 6%, in the absence of a meal20,21,22. In the liver, CBD undergoes oxidative metabolism by CYP450 enzymes and conjugative metabolism by UDP-glucuronosyltransferase (UGT) enzymes, particularly UGT1A7, UGT1A9, and UGT2B723,24. CYP3A4 and CYP2C19, are considered to be the major enzymes in the oxidative metabolism of CBD, leading to the formation of several metabolites, including the primary active metabolite 7‐hydroxy‐cannabidiol (7‐OH‐CBD)24. The AUC of 7-OH-CBD is approximately 38% of CBD, and the metabolite is considered to have equipotent activity in comparison with CBD25,26. In vitro results from Beers et al. (2021) suggest that not only CYP2C19 but also CYP2C9 plays a role in the CBD 7-hydroxylation26. The formation of the inactive metabolite 7-carboxy-cannabidiol (7‐COOH‐CBD) is proposed to occur through the further metabolism of 7-OH-CBD by CYP3A427.
This study aimed to investigate the pharmacokinetics of CBD and one of its primary metabolites, 7-OH-CBD, in healthy volunteers, after a single oral dosage of a broad-spectrum CBD-rich Cannabis sativa extract equivalent to 70 mg CBD. Furthermore, the effect of a high-fat meal on the bioavailability of CBD and 7-OH-CBD was examined. Since both men and women volunteered to participate, the study also explored the pharmacokinetic outcomes of CBD and its metabolite 7-OH-CBD in men and women separately.
Methods
Regulatory framework and ethical approval
The study protocol (NL74963.041.21) was approved as a food supplement study (which distinguishes it from a Phase I trial) by the METC (Medical Ethics Committee) of Utrecht University on December 24, 2021. This classification was based on the fact that, at that time, EFSA had not yet issued a formal statement regarding the novel food status of CBD and in consideration of the existing situation regarding the widespread, uncontrolled use of CBD supplements. Consequently, no approval from the national competent authority was required for this study.
Participants
Regulatory bodies including the FDA and EMA, recommend a minimal number of twelve participants in pharmacokinetic studies investigating food effects25. In accordance with these recommendations, 12 participants were included. To be eligible, candidate participants had to meet the following inclusion criteria: age 18-60 years, BMI 18.5-25 kg/m2, weight ≥50 kg, good general health (assessed via a general health questionnaire), suitable veins for blood sampling, language proficiency in Dutch. Exclusion criteria included current illness, gastrointestinal diseases within the last three months, hemoglobin level <8.5 mmol/L, the use of medication two months before and/or during the intervention (except for oral contraceptives and occasional use of NSAIDs or paracetamol), weight changes of >2 kg in the month before the intervention, the use of dietary supplements for at least three weeks prior to the test days or in the washout period, allergies to products provided as part of the standardized diet, following a specific diet (e.g. vegetarian, gluten-free), drug abuse (>1 x per month recreational drug use), cannabis use within 14 days before the first test day, smoking, alcohol consumption >10 units per week, recent or planned blood donation (within three months before or during the study day), pregnancy or breastfeeding within the past six months, or pregnancy during the study.
Recruitment and screening
Volunteers were recruited from the area in the vicinity of Wageningen University in The Netherlands, between May 10, 2022, and June 3, 2022. Prior to inclusion, an in-person information meeting was organized at the research facility. Interested participants were contacted for an on-site screening, after signing the informed consent. The screening process comprised a general and medical questionnaire, a single blood sample for hemoglobin estimation, height, and weight measurements, and an assessment of vein suitability for the placement of a catheter. See Supplementary Table S2 for details about the questionnaires.
Study design
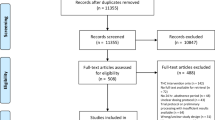
The study was a randomized cross-over single-dose trial. An overview of the study design is summarized in the flowchart (Fig. 1). Participants were randomly assigned to receive capsules containing a CBD-rich extract, equivalent to a dose of 70 mg CBD, either in fasting condition (participants were required to remain fasted until four hours after ingestion of the study product) or preceded by a high-fat meal. The hard gelatin capsules (size 00) were manually filled two hours before consumption at room temperature. The high-fat meal was consumed half an hour before ingesting the CBD extract. The two conditions were separated by a washout period of 13 days. A baseline blood sample was taken at timepoint minus one (t=-1), one hour before the extract was ingested at timepoint zero (t=0). Blood samples were taken by vena puncture at t=0.25, 0.5, 0.75, 1, 1.5, 2, 2.5, 3, 3.5, 4, 5, 6, 8, 10, and 12 hours. At 24 hours and 48 hours after ingestion, the study participants returned to the facility in a fasted state for the last two blood samples. Participants were randomly assigned to start with either the fasted or fed condition. The randomization process was conducted by a staff member from the Division of Human Nutrition at Wageningen University, who was not involved in the study. All samples were labeled with a unique participant number and the date and time of collection. The laboratory analyses were performed in a blinded manner (blinding participants to the intervention was not feasible).
Experimental procedure
The study participants visited the university research facility on two separate test days in a fasted state. The evening before, a standardized meal was consumed at home. On each test day, participants were requested to fill out a well-being questionnaire (See Supplementary Table S2). Subsequently, a venous catheter was placed and a baseline blood sample was taken. In random order, the participants consumed the CBD extract either in fasting condition or preceded by a high-fat meal consumed within 30 minutes. The composition of the high-fat meal (±800kcal) and the standardized meal that was consumed the evening before the test day, was determined in consultation with a dietician and following existing FDA and EFSA guidelines for studying food effects on drug kinetics (See guidelines in Table 1). During the blood sampling period, study participants were provided standardized meals or snacks supplied by the university at t=4, 6, 9, and 12 hours after ingestion of the study product. See Supplementary Tables S3 and S4 for details about the consumed meals and snacks.
Study product and dosing
The study participants received a CBD-rich Cannabis extract equivalent to a total dose of 70 mg CBD once daily, administered as three capsules of 23.3 mg each. This was done to exclude any potential buccal absorption, and the capsules were therefore swallowed whole with a glass of water (240 mL). The manufacturing process of the CBD extract ensured maximum retention of terpenes and cannabinoids, while selectively removing THC. A detailed description of the extraction process can be found in Supplementary Table S1. The extract contained between 70 and 75% CBD. To achieve a final concentration of 5% CBD, extracts were diluted using medium-chain triglyceride oil. The CBD-rich Cannabis extract was supplied by Becanex GmbH (Berlin, Germany).
Chemical analysis
Concentrations of CBD and 7-OH-CBD in human K2-EDTA plasma samples were determined by Ardena Bioanalysis BV (Assen, the Netherlands) using a validated LC-MS/MS method. The validation was performed in accordance with the guidelines set by the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) and conducted under Good Laboratory Practice (GLP) conditions28,29. Briefly, CBD (Lipomed AG; Weil am Rhein, Germany), 7-OH-CBD, and the internal standards cannabidiol-D3 (Lipomed AG, Weil am Rein, Germany, certified concentration 100.3 µg/mL) and 7-hydroxy cannabidiol-D3 (Merck, Darmstadt, Germany, certified concentration 99.8 µg/mL), both added to a final concentration of 10.0 ng/mL were isolated from human K2-EDTA plasma via liquid-liquid extraction using 25% tert-butyl methyl ether (Baker) in n-pentane (Biosolve). Following extraction, the samples were evaporated under a stream of nitrogen and the analytes were reconstituted in 300 µl acetonitrile (ACN)/ ultrapure water (UPW) 1:2. Subsequently, they were derivatized with 2-fluoro-1-methylpyridine (FMP) (TCI, Zwijndrecht, Belgium) by adding 200 µL of a solution (75 mg/mL) of FMP in ACN, 50.0 µL NaHCO3 buffer (pH 10.5) and 10.0 µL triethylamine and incubating the mixtures for 5 min. The derivatized analytes were subsequently extracted by solid-phase extraction (SPE) using Oasis WCX 30 mg 96-well columns (Waters). After elution, the samples were evaporated under nitrogen and reconstituted in 300 µl injection solvent (ACN/UPW 1:2). Chromatographic separation was performed on an XSelect CSH Phenyl-Hexyl column (Waters, Netherlands). The mobile phase consisted of 5% acetonitrile (ACN) in ultrapure water (UPW)(LC-A), 100 mM ammonium formate (NH4FA) in 5% ACN in UPW + 1 % formic acid (FA)(LC-B), and 100% ACN (LC-C). Ternary gradient elution was performed at a flow rate of 0.700 mL/min with gradient slope and times as follows:
Time | Flow | A. Conc | B. Conc | C. Conc |
|---|---|---|---|---|
min | mL/min | % | % | % |
0.00 | 0.70 | 60.0 | 15.0 | 25.0 |
3.50 | 0.70 | 0.0 | 15.0 | 85.0 |
5.20 | 0.70 | 0.0 | 15.0 | 85.0 |
5.30 | 0.70 | 60.0 | 15.0 | 25.0 |
The total run time was 6.8 minutes per sample. CBD, 7-OH-CBD, and THC were fully separated at baseline with elution times of 1.6, 1.4, and 3.5 min., respectively. An API 6500 tandem mass spectrometer equipped with a turbo ion spray probe operating in positive multiple reaction monitoring (MRM) mode was employed for quantification. The following MRM transitions of the respective precursors and product ions were used to quantify the analytes in human K2-EDTA plasma:
MS transitions | |||||
|---|---|---|---|---|---|
Component | Period | Tune mass#1 | Q1 mass | Q3 mass | Dwell (ms) |
1-methyl-pyridinyl-CBD | 1 | 496 | 249 | 215 | 25 |
1-methyl-pyridinyl- CBD-D3 | 1 | 499 | 250.5 | 216.5 | 25 |
7-OH-1-methyl-pyridinyl- CBD | 1 | 512 | 257 | 223 | 25 |
7-OH-1-methyl-pyridinyl- CBD-D3 | 1 | 515 | 258.5 | 224.5 | 25 |
The mass spectrometer was operating using unit Q1 and Q3 resolution, curtain gas pressure was 35 psi, CAD collision gas pressure was 10 psi, GS1 nebulizer gas pressure was 30 psi, GS2 turbo gas pressure was 80 psi, IS (ion spray) was 5000 V and source temperature was 500°℃. The method was validated in the analytical range of 0.100–20.0 ng/mL for CBD and 7-OH-CBD in human plasma according to the FDA and EMA guidelines28,29. Validation parameters included response function, selectivity (including blank matrix evaluation, matrix effect, hemolyzed plasma effect (interference observed), lipemic plasma effect, mutual interference and potential interference from co-administered drugs and other xenobiotics, carryover, precision, accuracy, recovery, stability (including bench-top stability, re-injection stability, processed sample stability, freeze/thaw stability, short term stock/spike stability, long term stock and spike solution stability, long-term frozen sample storage stability), dilution (50 times), and batch size determination. Data acquisition was performed using Analyst software (version 1.7.2) from AB Sciex. Following peak area integration, regression was also performed using Analyst. Concentrations for CBD and 7-OH-CBD were calculated using 9-point curves with weighted linear regression (weighting factor = 1/x2).
The calibration curves of the validation runs showed an accuracy and precision of the calibrators within the predefined criteria for bioanalytical method validation, i.e., bias ±20.0% for the lowest calibrator and ±15.0% for all other calibrators. The overall CV of the CBD and 7-OH-CBD calibration standards were within 20.0% for the lowest calibrator and within 15.0% for all other calibrators). In addition, the mean biases were within ±20.0% of the nominal value for the lowest calibrator and ±15.0% for all other calibrators.
The assay was linear over the concentration range of 0.100 to 20.0 ng/mL in human K2-EDTA plasma with coefficients of determination (r) ≥ 0.99. The within-run accuracy of the quality control samples, evaluated using samples at the level QC-LLOQ (0.100 ng/mL), QC-Low (0.300 ng/mL), QC-Medium (2.00 ng/mL), QC-medium-2 (10.0 ng/mL) and QC-High (16.0 ng/mL), and measured as %bias, ranged from 6.0 to 14.7% for CBD and from 4.0 to 9.8% for 7-OH-CBD and the between run-accuracy of the quality control samples (measured as %bias) ranged from 1.4 to 2.8% for CBD and from 0.6 to 2.5% for 7-OH-CBD. The precision of the method was measured in terms of between run precision (%CV) and ranged from 3.0 to 4.4% for CBD and from 2.8 to 6.0% for 7-OH-CBD. Back-calculated concentrations of calibration standards and calibration curve parameters of CBD and 7-OH-CBD are provided in Supplementary Table S5, S6. Plasma concentrations of CBD and 7-OH-CBD measured at different time points for all participants with both interventions are provided in Supplemental Table S7.
Statistics
Data processing and statistical analyses were conducted using GraphPad Prism 10 and SPSS version 29.0.
GraphPad Prism was used for descriptive statistics and to visualize the plasma curves and spaghetti plots. Mean CBD and 7-OH-CBD concentrations were plotted over time for both the fasted and fed states, with separate plots for the total population, male participants, and female participants. Individual trends were visualized using spaghetti plots, including Cmax values for the fasted and fed conditions. For both CBD and 7-OH-CBD under fasted and fed conditions, the geometric means with 90% confidence intervals (90% CI) for Cmax and AUC were calculated with SPSS, using one-way analysis of variance (ANOVA) on the log-transformed pharmacokinetic parameters, with condition (fed versus fasted), sequence (of conditions), period, and sex as fixed factors. The outcomes of the ANOVA were exponentiated to obtain the geometric means, the geometric mean ratios (GMRs), and corresponding 90% CI’s on the original scale. For Tmax, medians with ranges were determined. Plasma half-life was not determined due to the double-peak phenomenon observed in the kinetic profiles. Subgroup analyses for men and women were performed to explore potential differences in pharmacokinetic parameters. These results should be interpreted with caution due to the small sample size. The SPSS syntax and dataset can be found in Supplementary Data S8.
Sample size
An a priori power analysis was conducted, using G*Power version 3.1.9.4. The sample size calculation was based on 80% power, a significance level of 0.05, and an effect size of 1.37, derived from a study by Birnbaum et al. (2019), which investigated the effect of food on the pharmacokinetics of pure CBD30. The analysis indicated that a sample size of 7 participants would provide an actual power of 85% (see Supplementary Table S9). However, regulatory guidelines, including those from the FDA, recommend a minimum of 12 participants for pharmacokinetic studies assessing food effects25. To comply with these guidelines, 12 participants were included in this study.
Results
Participants
Eleven participants completed the study. One male participant dropped out of the study due to technical problems with repeated blood sampling. A total of 396 primary human K2-EDTA plasma samples were collected and analyzed for CBD and 7-OH-CBD levels. The investigational product was well tolerated, and no adverse events were observed during the study. Participant characteristics are described in Table 2. The mean age for men was 7.4 years higher compared to women.
Pharmacokinetics
Table 3 shows that consuming a high-fat meal significantly increased the Cmax and bioavailability of CBD compared to fasting. The GMR of Cmax was 17.4 (90% CI 12.4–24.2) and of the AUC 9.7 (90% CI 7.7–12.3). Tmax was increased from 5 hours to 10 hours (P = <0.01). Table 4 suggests that the food effect on CBD’s pharmacokinetic parameters was more pronounced in males than in females, as reflected by higher GMRs for both Cmax and AUC.
Figure 2 illustrates the occurrence of two CBD concentration peaks following the consumption of a high-fat meal; the first peak appears approximately five hours post-meal and the second peak around five hours later.
It is relevant to note that the curves in Fig. 2 represent the mean CBD concentration of all study participants (n=11) at the measured time points. The resulting peaks indicate the maximum mean CBD concentration of the study population at a sampled time point. These peaks slightly differ from the Cmax values presented in Table 3 (and Table 4), which reflect the geometric means of the individual Cmax values across all 11 study participants. In these tables, the variable Cmax represents the maximum CBD concentration observed for each individual, which may occur at different time points for other individuals.
Figure 3 shows the plasma profile of the 7-OH metabolite, which generally followed that of CBD but with consistently lower plasma concentrations. A distinct second concentration peak second peak was observed here as well.
The spaghetti plots in Fig. 4 illustrate that CBD exposure (Cmax and AUC) increased in all participants under fed conditions compared to fasting (Fig. 4a–d). Cmax and AUC values were low and clustered in the fasted condition and substantially higher and more variable in the fed condition. The plots highlight the interindividual differences in CBD exposure among the 11 participants.
Figure 5 shows that in women, the second peak after a meal was particularly prominent, exceeding the first peak in magnitude, while men exhibited a less pronounced second peak (please note the difference in the y-axis between the fasted and fed conditions). The plasma curves of individual participants displayed a relatively uniform shape after oral administration in the fasting state. However, after a meal, the curves exhibited less uniformity, with notable variation between the participants.
Discussion
To the best of our knowledge, this is the first study that compared the effect of a high-fat meal on the pharmacokinetics of CBD and its pharmacologically active metabolite 7-OH-CBD after administration of a capsule containing a CBD-rich extract instead of purified CBD. Furthermore, we explored the pharmacokinetic outcomes of male and female participants.
Both the geometric mean ratio (GMR) for Cmax (17.4; 90% CI 12.4–24.2) and AUC (9.7; 90% CI 7.7–12.3) of CBD were significantly higher in the fed condition compared to fasting, indicating a substantial food effect on CBD bioavailability. These results are consistent with previous studies. Crockett et al. (2020) reported 3.8-fold and 5.2-fold increases in AUC and Cmax, respectively, after administering a single dose of 750 mg CBD in oral solution to healthy adult volunteers31. Taylor et al. (2018) reported a 4.2-fold and 4-fold increase in AUC and Cmax, respectively, following a single dose of 1500 mg CBD co-administered with a high-fat breakfast32. Similarly, Birnbaum et al. (2019) found a 4.2-fold increase in AUC and a 14-fold increase in Cmax in healthy adult volunteers after a 300 mg CBD dose provided in capsules30. Compared to these studies, our results demonstrate a larger food effect. The plasma concentration-time course and peak plasma CBD concentration in fasted male participants in our study align with results from a recent study by Johnson et al. (2023), in which healthy male volunteers received a single dose of 69 mg CBD provided as capsules or sublingual drops33. The CBD metabolite 7-OH-CBD exhibited a similar pattern to CBD, with a 3.2-fold increase in AUC and a 2.5-fold increase in Cmax. Given the low oral bioavailability of CBD in the fasted state as reported in literature (around 6%)20,21 this food effect may have clinical relevance for CBD use in practice.
The mean peak concentration (Tmax) in the fasted state was reached 5.0 (0.8-6.0) hours after CBD administration in our study population. Taylor et al. (2018) and Crocket et al. (2020) reported Tmax values of 4.0 hours after doses of 750 mg and 1500 mg CBD27,32; while Birnbaum et al. (2019) observed a Tmax of 3.2 hours following a 300 mg dose30. Upon consumption of a high-fat meal, we observed a delayed Tmax of 10 (1.5-12.0) hours. In contrast to our findings, Taylor et al., Crockett et al., and Birnbaum et al. reported no effect of food on Tmax27,30,32. Regarding 7-OH-CBD, the Tmax followed a similar pattern to CBD.
A notable observation was the second peak in the CBD plasma curve seen in some participants, in particular after food consumption. In six participants, a pronounced second peak was visible, and in five out of the six participants, the second peak was higher than the first peak. The literature offers a few possible explanations for this phenomenon. One explanation is that CBD is partially carried by chylomicrons and taken up by the intestinal lymphatic system upon oral administration with lipids34. In vitro lipolysis experiments by Zgair et al. demonstrated that approximately one-third of the administered CBD dose was taken up in the micellular layer when co-administered orally with lipids. In addition, CBD showed a high affinity for chylomicron-like particles, implying potential uptake of CBD by the lymphatic system34. Characteristics indicative of lymphatic transport include a log P >5 and high solubility in long-chain triglycerides35. CBD meets the first criterion, with reported log P values of approximately 6.336,37. However, a study by Alhadid et al. (2022) demonstrated that CBD is better soluble in medium-chain than in long-chain triglycerides38. Another explanation may be enterohepatic recirculation, i.e. the reabsorption of a compound or its metabolite(s) from the intestine back into the bloodstream after they have been secreted into the bile and released into the digestive tract39. Enterohepatic recirculation is often reflected in two (or more) peaks in the plasma concentration-time profiles, affecting overall pharmacokinetics and prolonging the presence of a compound or its metabolites in the body. Regarding cannabinoids, biliary excretion is an important route of elimination for cannabinoids and their metabolites, as demonstrated by the study of Fabritius et al. (2012) for THC40. Another explanation mentioned in the literature involves the effect of food on gastric emptying, which is known to influence the rate and extent of absorption of some drugs41. This effect mainly applies to hydrophilic drugs, which dissolve rapidly, making gastric emptying an important factor in their absorption42. However, given CBD’s highly lipophilic properties and the late appearance of the second peak (around 10 hours), far beyond the residence time in the stomach, this explanation is very unlikely. During the blood sampling period, participants consumed standardized meals and snacks at t=4, 6, 9, and 12 hours after administration of the study product. At timepoint 9 participants consumed dinner, which may also have played a role in the timing of the second peak. Overall, it is plausible that a combination of the effects discussed above contribute to the double peak phenomenon. Interestingly, a second peak was also observed with the 7-OH metabolite of CBD. A similar observation has been described by Lunn et al. (2019) for the 7-OH metabolite and 7-COOH metabolite of THC43.
We observed substantially higher GMRs for Cmax of CBD in male participants compared to female participants, while the ratios for CBD AUC and food effects on the pharmacokinetic parameters of 7-OH-CBD were comparable. These findings suggest that although the food effect on CBD Cmax may be more pronounced in males, overall CBD bioavailability appears to be similar between sexes. The comparable 7-OH-CBD Cmax and AUC values suggest that the conversion of CBD to 7-OH-CBD by CYP2C19 is not influenced by sex-specific differences in enzyme activity. This is consistent with findings by Soldin et al. (2009), who reported no sex difference in the activity of CYP2C19, the enzyme responsible for the conversion of CBD into its 7-hydroxy metabolite44. In comparison, a study by MacNair et al. (2023) reported no significant sex differences in both CBD Cmax, CBD AUC, and 7-OH-CBD Cmax, but observed higher AUC values of 7-OH-CBD in women compared to men45, as observed in our findings as well. The higher AUC values observed in women may be attributed to the uniform dosing applied to all participants. This approach may have resulted in relatively higher serum concentrations in women due to their lower average body weight (62.2 kg for women versus 75.8 kg for men). Moreover, the age difference between the sexes (22.4 years for women versus 29.8 years for men) was not accounted for in this study. These factors, combined with the small sample sizes (6 males and 5 females), warrant caution in the interpretation of our findings.
The CBD-rich extract used in our study is a broad-spectrum extract, designed to maximize the preservation of terpenes and cannabinoids, while selectively removing THC. This makes our extract different from purified CBD extracts used in most pharmacokinetic studies, including those discussed above. This distinction is important, as the presence of additional constituents in a full-spectrum extract may influence the observed pharmacokinetic profiles. It is hypothesized that sesquiterpenes, including β-caryophyllene and α-humulene present in the extract used in this study, may modulate the activity of cytochrome P450 enzymes. An in vitro study using human and rat hepatic microsomes demonstrated the inhibitory effects of β-caryophyllene and α-humulene on CYP3A4 activity13. CBD is a substrate of this enzyme3 and inhibition of CYP3A4 by terpenes could potentially increase CBD exposure by slowing its breakdown in the gut and liver. However, due to the absence of a purified CBD control group, this remains highly speculative.
The study deliberately used capsules that were swallowed whole, ensuring that the entire dose entered the gastrointestinal tract, although sublingual administration is often advised for CBD. The latter is based on the idea that this route might allow for rapid transport into the bloodstream across the oromucosal membrane 46,47. In theory, this could improve CBD bioavailability by passing poor epithelial transport and hepatic first-pass metabolism48. However, a study by Johnson et al. (2023) indicates that sublingual absorption of CBD is negligible, despite its lipophilicity33. Even for situations of intended sublingual administration (for example by holding drops under the tongue), there is increasing consensus that the majority of the CBD is swallowed and subsequently absorbed through the gastrointestinal tract33,46.
A key strength of our study is the use of a broad-spectrum extract, which contains not only CBD but also terpenes and other cannabinoids. This is particularly relevant as most pharmacokinetic studies to date have focused on purified CBD. Using a broad-spectrum extract, our study more closely reflects the complexity of CBD oils often used in practice and their potential interactions. Another strength of our study is the administration of CBD in capsule form, ensuring that the entire dose was delivered directly to the gastrointestinal tract, thereby excluding variation in absorption due to a potentially prolonged residence time in the mouth and the contribution of oromucosal absorption. Our meals were highly standardized, ensuring consistency in the potential food effect on CBD absorption, which is known to influence the bioavailability of cannabinoids. The assay performance met the predefined quality criteria, demonstrating linearity over the concentration range of 0.100 to 20.0 ng/mL in human K2-EDTA plasma, with coefficients of determination (r) equal to or exceeding 0.99. Values in some samples exceeded the established upper or lower concentration limit. However, through incurred sample reanalysis (ISR), accurate concentrations of CBD or 7-OH-CBD were determined, ensuring proper quantification.
Regarding the limitations of this trial, it should be noted that the included participants were healthy and relatively young, which limits the generalizability of our findings to a broader population. Additionally, our study investigated the pharmacokinetics of one specific CBD-rich Cannabis sativa extract. Therefore, other CBD products may give results that differ from those obtained in the present study. Another limitation is the sample sizes of the subgroups of male and female participants, with 6 and 5 participants respectively, which were too small to allow for statistical analysis of sex differences in pharmacokinetic parameters. Initially, we also aimed to analyze the presence of 7-carboxy-cannabidiol (7-COOH-CBD). However, as the bioanalytical method was not validated for the quantitative analysis of this metabolite, we have decided not to include these data in the paper. Finally, this trial only assessed the effects of a single dose of a CBD-rich Cannabis extract; further research is needed to evaluate the effects of repeated administration and long-term use.
In conclusion, the present study enhances our understanding of the pharmacokinetics of CBD from a cannabis extract. The observed second peak phenomenon in both CBD and its metabolite 7-OH-CBD is an interesting finding, which merits further investigation to confirm its relevance before practical implications can be drawn. On the other hand, the meal effect and the associated increase in bioavailability have clear practical implications. Healthcare professionals and users of CBD should be aware that consuming CBD with a meal significantly increases its bioavailability and standardizing CBD intake to meals is important for achieving consistent and optimal effects.
Data availability
All data supporting the findings of this study are available within the manuscript and its Supplementary Information. The analytical report of cannabidiol (CBD) and 7-hydroxy cannabidiol (7-OH-CBD) measured in human K2-EDTA plasma samples is provided in Supplementary Table S7.
References
Lange, B. M. & Zager, J. J. Comprehensive inventory of cannabinoids in Cannabis sativa L.: Can we connect genotype and chemotype?. Phytochem. Rev. 21, 1273–1313 (2021).
Iffland, K. & Grotenhermen, F. An update on safety and side effects of cannabidiol: A review of clinical data and relevant animal studies. Cannabis Cannabinoid Res. 2, 139–154 (2017).
Millar, S. A. et al. A systematic review of cannabidiol dosing in clinical populations. Br. J. Clin. Pharmacol. 85, 1888–1900 (2019).
Chesney, E. et al. Adverse effects of cannabidiol: a systematic review and meta-analysis of randomized clinical trials. Neuropsychopharmacology 8, 1799–1806 (2020).
Pirrung, M. C. Synthetic access to cannabidiol and analogs as active pharmaceutical ingredients. J. Med. Chem. 63, 12131–12136 (2020).
Epidyolex | European Medicines Agency (EMA). https://www.ema.europa.eu/en/medicines/human/EPAR/epidyolex.
Epidyolex 100 mg/ml, drank | Geneesmiddeleninformatiebank | College ter Beoordeling van Geneesmiddelen. https://www.geneesmiddeleninformatiebank.nl/nl/cp122465.
Sativex, spray voor oromucosaal gebruik | Geneesmiddeleninformatiebank | College ter Beoordeling van Geneesmiddelen. https://www.geneesmiddeleninformatiebank.nl/nl/rvg111277.
Maayah, Z. H., Takahara, S., Ferdaoussi, M. & Dyck, J. R. B. The anti-inflammatory and analgesic effects of formulated full-spectrum cannabis extract in the treatment of neuropathic pain associated with multiple sclerosis. Inflamm. Res. 69, 549–558 (2020).
Häuser, W., Petzke, F. & Pain, M. F. Efficacy, tolerability and safety of cannabis-based medicines for chronic pain management–An overview of systematic reviews. Eur. J. Pain 22, 455–470 (2018).
Turck, D. et al. Statement on safety of cannabidiol as a novel food: data gaps and uncertainties. EFSA J. https://doi.org/10.2903/j.efsa.2022.7322 (2022).
Zehetner, P., Höferl, M. & Buchbauer, G. Essential oil components and cytochrome P450 enzymes: a review. Flavour Fragr. J. 34, 223–240 (2019).
Nguyen, L. T. et al. The inhibitory effects of β-caryophyllene, β-caryophyllene oxide and α-humulene on the activities of the main drug-metabolizing enzymes in rat and human liver in vitro. Chem. Biol. Interact. 278, 123–128 (2017).
Špičáková, A., Bazgier, V., Skálová, L., Otyepka, M. & Anzenbacher, P. β-caryophyllene oxide and trans-nerolidol affect enzyme activity of CYP3A4-in vitro and in silico studies. Physiol. Res. 68, 51–58 (2019).
Nahler, G., Jones, T. M. & Russo, E. B. Cannabidiol and contributions of major hemp phytocompounds to the “entourage effect”; possible mechanisms. J. Altern. Complement. Integr. Med. 5, 1–16 (2019).
Perucca, E. & Bialer, M. Critical aspects affecting cannabidiol oral bioavailability and metabolic elimination, and related clinical implications. CNS Drugs 34, 795–800 (2020).
Benet, L. Z., Broccatelli, F. & Oprea, T. I. BDDCS applied to over 900 drugs. AAPS J. 13, 519–547 (2011).
Cannabidiol: Uses, Interactions, Mechanism of Action | DrugBank Online. Drugbank CA https://go.drugbank.com/drugs/DB09061.
Grifoni, L., Vanti, G., Donato, R., Sacco, C. & Bilia, A. R. Promising nanocarriers to enhance solubility and bioavailability of cannabidiol for a plethora of therapeutic opportunities. Molecules 27, 6070 (2022).
Agurell, S. et al. Interactions of delta 1-tetrahydrocannabinol with cannabinol and cannabidiol following oral administration in man. Assay of cannabinol and cannabidiol by mass fragmentography. Experientia 37, 1090–1092 (1981).
Ohlsson, A. et al. Single-dose kinetics of deuterium-labelled cannabidiol in man after smoking and intravenous administration. Biomed. Environ. Mass Spectrom. 13, 77–83 (1986).
Millar, S. A., Stone, N. L., Yates, A. S. & O’Sullivan, S. E. A systematic review on the pharmacokinetics of cannabidiol in humans. Front. Pharmacol. 9, 425858 (2018).
Mazur, A. et al. Characterization of human hepatic and extrahepatic UDP-glucuronosyltransferase enzymes involved in the metabolism of classic cannabinoids. Drug Metab. Dispos. 37, 1496–1504 (2009).
Jiang, R., Yamaori, S., Takeda, S., Yamamoto, I. & Watanabe, K. Identification of cytochrome P450 enzymes responsible for metabolism of cannabidiol by human liver microsomes. Life Sci. 89, 165–170 (2011).
FDA. Assessing the Effects of Food on Drugs in INDs and NDAs-Clinical Pharmacology Considerations Guidance for Industry. https://www.fda.gov/drugs/guidance-compliance-regulatory-information/guidances-drugs (2022).
Beers, J. L., Fu, D. & Jackson, K. D. Cytochrome P450–catalyzed metabolism of cannabidiol to the active metabolite 7-hydroxy-cannabidiol. Drug Metab. Dispos. 49, 882–891 (2021).
Morrison, G., Crockett, J., Blakey, G. & Sommerville, K. A phase 1, open-label, pharmacokinetic trial to investigate possible drug-drug interactions between clobazam, stiripentol, or valproate and cannabidiol in healthy subjects. Clin. Pharmacol. Drug Dev. 8, 1009–1031 (2019).
U.S. Department of Health and Human Services, F. and D. A. (FDA), C. for D. E. and R. (CDER), C. for V. M. (CVM). Guidance for Industry: Bioanalytical Method Validation. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/bioanalytical-method-validation-guidance-industry (2018).
European Medicines Agency (EMA), C. for M. P. for H. U. (CHMP). Guideline on Bioanalytical Method Validation - Scientific Guideline. https://www.ema.europa.eu/en/bioanalytical-method-validation-scientific-guideline (2009).
Birnbaum, A. K. et al. Food effect on pharmacokinetics of cannabidiol oral capsules in adult patients with refractory epilepsy. Epilepsia 60, 1586–1592 (2019).
Crockett, J., Critchley, D., Tayo, B., Berwaerts, J. & Morrison, G. A phase 1, randomized, pharmacokinetic trial of the effect of different meal compositions, whole milk, and alcohol on cannabidiol exposure and safety in healthy subjects. Epilepsia 61, 267–277 (2020).
Taylor, L., Gidal, B., Blakey, G., Tayo, B. & Morrison, G. A phase I, randomized, double-blind, placebo-controlled, single ascending dose, multiple dose, and food effect trial of the safety, tolerability and pharmacokinetics of highly purified cannabidiol in healthy subjects. CNS Drugs 32, 1053–1067 (2018).
Johnson, D. A. et al. Cannabidiol oil ingested as sublingual drops or within gelatin capsules shows similar pharmacokinetic profiles in healthy males. Cannabis Cannabinoid Res. 9, e1423–e1432 (2023).
Zgair, A. et al. Dietary fats and pharmaceutical lipid excipients increase systemic exposure to orally administered cannabis and cannabis-based medicines. Am. J. Transl. Res. 8, 3448–3459 (2016).
Charman, W. N. A. & Stella, V. J. Estimating the maximal potential for intestinal lymphatic transport of lipophilic drug molecules. Int. J. Pharm. 34, 175–178 (1986).
Cannabidiol | C21H30O2 | CID 644019 - PubChem. https://pubchem.ncbi.nlm.nih.gov/compound/644019.
Cannabidiol: Uses, Interactions, Mechanism of Action | DrugBank Online. https://go.drugbank.com/drugs/DB09061.
Alhadid, A., Luca, S. V., Nasrallah, S. & Minceva, M. Experimental investigation and thermodynamic modeling of cannabidiol solubility in plant oils and hydrophobic eutectic systems. Molecules 27, 121172 (2022).
Roberts, M. S., Magnusson, B. M., Burczynski, F. J. & Weiss, M. Enterohepatic circulation physiological, pharmacokinetic and clinical implications. Clin. Pharmacokinet. 41, 751–790 (2002).
Fabritius, M., Staub, C., Mangin, P. & Giroud, C. Distribution of free and conjugated cannabinoids in human bile samples. Forensic Sci. Int. 223, 114–118 (2012).
Welling, P. G. Effects of food on drug absorption. Annu. Rev. Nutr. 16, 383–415 (1996).
Oberle, R. L. & Amidon, G. L. The influence of variable gastric emptying and intestinal transit rates on the plasma level curve of cimetidine; an explanation for the double peak phenomenon. J. Pharmacokinet. Biopharm. https://doi.org/10.1007/BF01061761 (1987).
Lunn, S. et al. Human pharmacokinetic parameters of orally administered Δ9-tetrahydrocannabinol capsules are altered by fed versus fasted conditions and sex differences. Cannabis Cannabinoid Res. 4, 255–264 (2019).
Soldin, O. P. & Mattison, D. R. Sex differences in pharmacokinetics and pharmacodynamics. Clin. Pharmacokinet. 48, 143–157 (2009).
MacNair, L. et al. Sex differences in the pharmacokinetics of cannabidiol and metabolites following oral administration of a cannabidiol-dominant cannabis oil in healthy adults. Cannabis Cannabinoid Res. 9, e1170–e1178 (2024).
Itin, C., Domb, A. J. & Hoffman, A. A meta-opinion: cannabinoids delivered to oral mucosa by a spray for systemic absorption are rather ingested into gastro-intestinal tract: the influences of fed / fasting states. Expert Opin. Drug Deliv. 16, 1031–1035 (2019).
Itin, C., Barasch, D., Domb, A. J. & Hoffman, A. Prolonged oral transmucosal delivery of highly lipophilic drug cannabidiol. Int. J. Pharm. 581, 119276 (2020).
Millar, S. A., Maguire, R. F., Yates, A. S. & O’sullivan, S. E. Towards better delivery of cannabidiol (CBD). Pharmaceuticals 13, 219 (2020).
Acknowledgments
We acknowledge Becanex GmbH (Berlin, Germany) for providing the CBD-rich Cannabis sativa extract and for their financial support of the study.
Funding
Wageningen University,Becanex GmbH.
Author information
Authors and Affiliations
Contributions
BS wrote the manuscript and analyzed the results with AvO. AvO and TdB wrote the protocol. TdB was primarily responsible for conducting the experimental study. RW, AvO, EO, and TdB reviewed the manuscript as co-authors. RW supervised the project as the Principal Investigator (PI).
Corresponding author
Ethics declarations
Competing interests
The author BS and co-authors AvO, and RW declare no competing interests. TvdL was an employee of Becanex GmbH at the time of the trial; EO is an employee of the company. Becanex GmbH did not influence the design or execution of the study. AWT is an employee of Ardena, the company responsible for the sample analysis. The final approval of the manuscript was solely the responsibility of RW as the overall project leader and PI.
Ethics statement
All study procedures were conducted according to the principles of the Declaration of Helsinki (64th WMA General Assembly, Fortaleza, Brazil, October 2013) and with the Medical Research Involving Human Subjects Act (WMO). All study participants gave their written informed consent. The protocol (NL74963.041.21) was approved on December 24, 2021, by the METC (Medical Ethics Committee) of Utrecht University. There was no competent authority approval needed for this study, as the METC decided to assess the trial as nutritional research.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Saals, B.A.D.F., De Bie, T.H., Osmanoglou, E. et al. A high-fat meal significantly impacts the bioavailability and biphasic absorption of cannabidiol (CBD) from a CBD-rich extract in men and women. Sci Rep 15, 3678 (2025). https://doi.org/10.1038/s41598-025-87621-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-87621-4
This article is cited by
-
An open-label phase I comparator-controlled clinical trial to assess tolerability and pharmacokinetics of IHL-675 A a fixed dose combination of cannabidiol plus hydroxychloroquine in healthy volunteers
Scientific Reports (2025)
-
Double Peaking Phenomena in Pharmacokinetic Disposition Revisited
Clinical Pharmacokinetics (2025)
-
Same-Day Sedative and Night-Time Sleep Effects Following Combined Cannabinoid Formulations: A Randomised-Controlled Trial
Clinical Drug Investigation (2025)