Abstract
Intrauterine fetal programming determines cardiorenal interaction later in life. We hypothesize that early life factors affect adult glomerular filtration rate and mean arterial pressure (MAP) directly or by interacting with postnatal growth trajectories. The population-based LifeGene study (Sweden) randomly recruited individuals aged 18 to 43 years (n = 12 167). They filled in a web-questionnaire and performed health tests (including bioimpedance measurements). Birth weight (BW), gestational age (GA), head circumference (HC), and birth length data were acquired from the Swedish Medical Birth Register. Postnatal growth was determined from BWz-scores and adult fat mass index. Creatinine and cystatin C-based kidney function were calculated (eGFRcr, eGFRcysC). After adjusting for sex, GA, adult age, and eGFRcr, a 1SD increase in BWz-score predicted a 1.15 mmHg increase in MAP. Meanwhile, every 1 cm decrease in HC was associated with an expected 0.29 mL/min/1.73m2 decrease in eGFRcr. Lower birth weight-to-placenta ratio was inversely related to eGFRcysC (p = 0.034). Postnatal down-regulation significantly affected a relatively lower eGFR but within normal range (p < 0.001). The postnatal catch-up did not affect kidney function. This study reveals the complex interrelationship between early life factors and adult kidney function that could be directly and indirectly influenced by adult body fat accumulation.
Similar content being viewed by others
Introduction
The kidney is a structurally complex organ in the human body that ensures blood filtration, excretion of waste products, regulation of blood pressure, fluid, electrolyte, acid-base balance, hormonal production, etc. In the presence of kidney dysfunction, this homeostatic balance is disrupted; however, signs and symptoms of chronic kidney disease (CKD) manifest later in the process. Identifying and preventing harmful factors that trigger chronic kidney damage is central in treating CKD. Thus, perinatal kidney development and postnatal maturation are pivotal components in the progression and onset of CKD1.
Kidney development starts during the first trimester of pregnancy2. The number of nephrons after birth, in combination with environmental and genetic factors, determines kidney function and health later in life3. The perinatal and postnatal exposures (nutrition, prematurity, low birth weight (BW))4,5, and early life exposures to adverse maternal factors (smoking, preeclampsia, hypoxia, etc.)6,7, might interrupt the natural development of kidneys and result in reduced kidney volume in adolescence8. Low kidney volume increases the susceptibility to kidney dysfunction throughout the lifespan9,10.
Overall, intrauterine fetal programming and postnatal growth patterns influence the development of chronic diseases11. Early life factors also seem to represent an important etiology for cardiovascular and kidney interactions12. We know from studies in adults that increased arterial stiffness and blood pressure could lead to deterioration of kidney function13. On the other hand, kidney injury and loss of functioning tissue14 alongside glomerular hyperfiltration15 might, in turn, cause hypertension and arterial stiffening. Thus, early life exposures might explain this complex crosstalk since reduced fetal growth, low birth weight, and postnatal growth trajectories have been attributed to CKD and kidney failure4,16,17, arterial stiffness18, and cardiometabolic health19,20.
Adiposity might be a mediator linking fetal programming with cardiovascular and kidney outcomes. Fetal origin of increased visceral and total fat mass among children and adults has been acknowledged during the last decades21,22,23. The U-shaped association for which both low and high birth weight are attributed to increased risk for adult obesity has been described22,23. It can particularly justify findings contradicting Brenner´s hypothesis24,25. For example, when combining birth weight and body composition at different stages of life, large-for-gestational-age (LGA) born children showed a higher risk for obesity and hypertension if their postnatal development did not slow down (no catch-down weight trajectory)26,27 Hypothetically, in this population, kidney function decline is secondary to obesity and high blood pressure. Previously, we could show that large for gestational female babies with postnatal down-regulation have worse kidney function in adult life compared to small babies who experience gradual postnatal development17. However, no other studies could so far confirm that.
This observational, population-based study focuses on kidney function in younger adults unaffected by advanced ageing and chronic disease burden. Here, we aim to analyze if the same observations apply to individuals aged 18 to 43 years included in the LifeGene study, Sweden. Additionally, we aim to shed light on cardiovascular and kidney interaction by hypothesizing that early life factors either directly affect adult estimated glomerular filtration and mean arterial pressure or via metabolic health (mediators), e.g., body composition (Fig. 1).
Results
Descriptive statistics
A total of 12 167 individuals (42.2% males) who had data on birth-related characteristics (birth weight, head circumference (HC), birth length (BL), gestational age (GA)) and plasma-creatinine levels were analyzed. Of these, 2499 participants also had information on placental weight (PW), maternal height, and maternal body weight before pregnancy and at delivery. However, only 2395 of the total study sample had serum cystatin C measurement. Of these, 561 subjects also had data on placental weight (Fig. 2). Clinical and descriptive characteristics and p-values for differences between men and women are presented in Table 1. Overall, men had significantly higher BW, BL, HC and PW than women (p < 0.001). The prevalence of prematurity, SGA and LGA was the same between sexes. Maternal anthropometrics did not differ, nor did the prevalence of diabetes and kidney disease in adult life. Women had significantly higher eGFR (p < 0.001 for both eGFRcr and eGFRcys) alongside a lower prevalence of CKD (p < 0.001). Moreover, women had lower BMI and FMI (p < 0.001 for both variables).
Flow chart of individuals selected. Figure 2 represents the availability of renal function related data in the LifeGene cohort. Abbreviations: BMI, body mass index; MAP, mean arterial pressure; WC, waist circumference; eGFRcr, estimated creatinine-based glomerular filtration rate; eGFRcys, estimated cystatin-based glomerular filtration rate
Association of adult glomerular filtration rate as an outcome with fetal factors
eGFRcr was weakly correlated to BW (r=-0.08, p < 0.001), BW z-score (-0.09, p < 0.001), BL (-0.12, p < 0.001), and HC (-0.09, p < 0.001), but not GA in the whole cohort. eGFRcys was available in 2 395 individuals but was not correlated to these early life factors.
After performing univariable linear regression analysis with eGFR as an outcome, we found that neither prevalent kidney disease nor diabetes were associated with eGFR levels (p > 0.05). Smoking was associated with a decreased GFRcr within the normal range (ß -0.46, 95%CI (-3.52;2.60)) but not eGFRcys (ß 1.68, 95%CI (1.14;2.23)). Snuff was related to lower both eGFRcr (ß -4.45, 95%CI (-5.06;-3.83)) and eGFRcys (ß -4.07, 95%CI (-6.07;-2.07)).
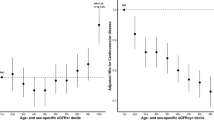
Multivariable linear regression revealed that every 1 cm decrease in HC was associated with an expected 0.29 mL/min/1.73m2decrease in eGFRcr in the whole population (p < 0.001). In women compared to men, this expected decrease in eGFRcr was as follows: 0.37 compared to 0.20 mL/min/1.73m2 (p < 0.001) (Fig. 3). BW, BW z-score, and BL had no significant relationship with eGFRcr in adjusted Models 1 to 4 (p > 0.05).
Placental weight (PW) and eGFRcr were available in 3 637 individuals (1 474 men and 2 163 women). Of these, 561 (195 men and 366 women) had additional data on eGFRcys. We observed that PW could neither predict adult eGFRcr nor eGFRcys. However, when used as birth weight-to-placenta weight ratio (BW/PW), the higher ratio was associated with a lower eGFRcys. It was found that for each 1 unit increase in BW/PW ratio, the expected decrease in eGFRcys adjusted for gestational age, sex, adult age, body mass index, mean arterial pressure and smoking/snuff status was 1.87 mL/min/1.73m2 (p = 0.034) (Fig. 4). These findings were not relevant to eGFRcr.
Associations between head circumference and estimated creatinine-based glomerular filtration rate (eGFRcr) with and without adjustment for confounders. Forest plots for linear regression models where eGFRcr is a dependent variable. Abbreviations: CI, Confidence Interval. For men: Unadjusted model, p = 0.045; Model 1, p = 0.012; Model 2, p = 0.025; Model 3, p = 0,030; Model 4, p = 0.024. For women: p-values for all models < 0.001.
Associations between the birth weight to placenta weight ratio and estimated cystatin C-based glomerular filtration rate (eGFRcys) with and without adjustment for confounders in 561 individuals. Forest plot for linear regression models where eGFRcys is a dependent variable. Abbreviations: CI, Confidence Interval. Unadjusted model, p = 0.039; Model 1, p = 0.037; Model 2, p = 0.041; Model 3, p = 0.036; Model 4, p = 0.034. R2 = 1.8% in Model 4.
Association of adult glomerular filtration rate as an outcome with maternal factors
Data on maternal age was available for all study participants. Meanwhile, the maternal body weight at both early pregnancy and delivery was only available in 2 499 individuals and was not associated with adult kidney function in the offspring (unadjusted p = 0.625 for eGFRcys and p = 0.866 for eGFRcr). After adjustments for covariates, a one-year increase in the maternal age during pregnancy could predict a 0.08 mL/min/1.73m2 decrease in eGFRcr in the adult daughters (p = 0.013) (Fig. 5). In sons, this association was absent.
Associations between maternal age during pregnancy and estimated creatinine-based glomerular filtration rate (eGFRcr) with and without adjustment for confounders in women. Forest plot for linear regression models where eGFRcr is a dependent variable. Abbreviations: CI, Confidence Interval. Unadjusted model, p = 0.159; Model 1, p = 0.008; Model 2, p = 0.007; Model 3, p = 0,013; Model 4, p = 0,013. R2 = 1.8% in Model 4.
Kidney function and postnatal growth mismatch
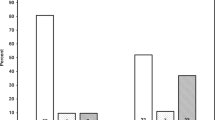
In all, 728 individuals (30.5% of them men) were born extremely small (BW z-score more than − 2SD deviation from the mean), and 888 individuals (57.9% of them men) were extremely large (BW z-score deviation than + 2SD away from the mean). Interestingly, small babies had 4.57 mL/min/1.73m2lower eGFRcr in adult life than the large ones (p < 0.001). Cystatin C-based eGFR could not provide this evidence.
A comparison of postnatal growth groups is presented in Table 2. Significantly lower percentage of men was observed in the low BW z-score and lower-than-average adult FMI group (Group 1) (p < 0.001). As depicted in Supplemental Figure S1, subjects with high BW z-score but lower-than-average FMI (Group 3) or high BW z-score and higher-than-average FMI (Group 6) had significantly lower eGFRcr as compared to those with low BW z-score and lower-than-average adult FMI (Group 1) (both p values < 0.001), as well as individuals with low BW z-score and higher-than-average adult FMI (Group 4) (p < 0.001 and p = 0.038, respectively).
Except for kidney and body composition parameters, the blood pressure variables were heterogeneous among subgroups Table 2). The individuals with low BW z-score and lower-than-average FMI (Group 1) had significantly lower systolic blood pressure compared to other subgroups and significantly lower diastolic blood pressure in combination with mean arterial pressure as compared to Groups 4 to 6 (all p values < 0.001).
Mean arterial pressure as an outcome in relation to early life factors and kidney function
In unadjusted linear models, MAP (outcome) was associated with BW, BL, and HC (all p values < 0.001). Interestingly, the BW z-scor2e became significant for predicting MAP after adjusting for sex, gestational age, adult age, and eGFRcr (p = 0.022 and 0.021, respectively) (Table 3, Models 2 and 3), but not in further models. Moreover, shorter GA (Table 3, Models 1 to 5, all p values < 0.001) and lower eGFRcr (Models 3 to 5) were related to higher MAP (all p values < 0.001).
Postnatal mismatch subgroup analysis revealed that in postnatal down-regulation, i.e., high BW z-score and lower-than-average FMI (Group 3), a 1 SD increase in BW z-score predicted a 1.15 mmHg increase in MAP after adjusting for sex, GA, adult age, and eGFRcr (p = 0.025).
As for the relationship between DBP and BW z-score, for each 1 SD increase in BW z-score the expected increase in DBP is 1.72 mmHg (p = 0.002), adjusted for sex, GA, adult age, and eGFRcr. SBP was not affected by BW z-score (p = 0.758).
The difference in MAP between premature babies and term babies was significant but minor: 84 (±9) vs. 85 (±9) mmHg (p = 0.019), respectively.
Discussion
This population-based study summarizes data on early life factors and its cardiovascular–kidney interactions in over 12,0000 young adults born in Sweden between 1973 and 1998. A smaller head circumference could predict lower creatinine-based kidney function in adult life. In women, the higher birth weight-to-placenta weight ratio was associated with lower cystatin C-based kidney function. In men, no such relationship was observed. We found that a postnatal down-regulation weight trajectory was detrimental to adult kidney function. Meanwhile, the postnatal catch-up pattern was associated with normal kidney function traits. Regarding the bidirectional cardiovascular-renal relationship, the findings indicated that a lower birth weight score was significantly associated with lower MAP – after adjusting for sex, adult age, and creatinine-based kidney function. However, the association was clinically irrelevant.
Cardiovascular-renal interactions are viewed as the cornerstone in the cardiometabolic health and pathogenesis of the so-called cardiorenal syndrome. A plausible mutual origin of disrupted kidney function and cardiovascular development is early life exposures28, as previously depicted in Fig. 1. For example, kidneys might specifically be damaged, either directly due to nephron and podocyte endowment3 or secondary to accelerated vascular ageing and hypertension29. Worsened cardiometabolic health30,31,32,33, a mediator affecting the cardiovascular-renal continuum, is very likely to be a consequence of deviations in BW and GA or postnatal growth trajectories30,34. Establishing this complex cause-effect relationship in adults requires a deeper understanding of how different environmental and socioeconomic factors interact from early life towards adulthood.
Undoubtedly, postnatal growth trajectories influence cardiometabolic health19,35,36. Amongst babies born small-for-gestational-age or large-for-gestational-age, if exposed to too fast or too slow postnatal weight gain, the prevalence of chronic diseases in adulthood is increased30,34. Postnatal catch-up defines individuals with low BW exposed to postnatal overfeeding, while postnatal down-regulation weight development characterizes high BW but sub-optimal postnatal weight gain35. Postnatal growth trajectories influence kidney development since postnatal weight gain from 6 to 24 months shapes the kidney volume37. Hence, a postnatal down-regulation is associated with smaller kidneys, and in contrast, postnatal catch-up with larger kidney volume. However, it’s unclear if kidney volume governs earlier manifestation of CKD. Our previous work showed that in a small sample of middle-aged Swedish women (n = 94), a higher sex-specific BW z-score in combination with lower than median body mass index (BMI) at 20 years of age was associated with lower cystatin C-based eGFR17. Here, we reveal that sex-specific BW z-score above 2 SD in combination with lower-than-average FMI is associated with a decrease in creatinine-based eGFR in young adults. In other words, we confirm that a postnatal down-regulation body weight trajectory is a risk marker for reduced adult kidney function, although within the normal range. Regarding the individuals with sex-specific BW z-score below − 2 SD in combination with higher-than-average FMI (postnatal catch-up), the significantly higher creatinine-based kidney function as compared to postnatal down-regulation group (p < 0.001) could reflect glomerular hyperfiltration, which is per se a marker of future cardiometabolic risk15,38,39. Hence, these individuals should not be misclassified and would benefit from a more precise measurement of the glomerular filtration rate with iohexol plasma clearance40.
The significant positive relationship between birth weight and MAP observed in this study is a subject of debate. We show that the higher BW z-score could predict the rise in adult MAP and DBP independently of kidney function. These findings contradict the proposed Brenner´s hypothesis. We know from previous reports4,41,42,43 that adults with a history of low birth weight or born preterm have higher blood pressure. Nevertheless, the opposite association has also been recognized. For example, according to a recent meta-analysis44, higher BW determines predisposition to higher DBP in an age-dependent manner. Obesity mediates this cross-talk, especially if large for gestational age born babies develop obesity during childhood26,27. Although the findings show that the association between BW z-score and MAP in the postnatal down-regulation is significant, the effect (1.15 mmHg increase in MAP) is very small and thus clinically irrelevant.
The observed smaller HC in association with reduced adult kidney function in subjects studied, supposedly reflects an unfavorable intrauterine environment. Adverse maternal factors mediate chronic intrauterine hypoxia and cardiac overload, thus causing blood redistribution to essential organs37. It was demonstrated by Montaldo et al.45 that neonates with intrauterine growth restriction (IUGR) compared to normal neonates were exposed to decreased postnatal regional cerebral and renal oxygenation. Moreover, IUGR was related to higher prevalence of microalbuminuria alongside elevated neutrophil gelatinase-associated lipocalin (NGAL) – a marker of acute kidney injury. Kooijman et al.46 could associate preferential fetal blood flow redistribution to the brain with kidney volume at 5.9 years of age; however, not linked to kidney dysfunction or albuminuria46. A report from the Netherlands37 showed that lower third-trimester HC, in concordance with abdominal circumference, was associated with reduced combined and relative kidney volume at two years of age. Since head circumference (HC) is also a proxy of maternal nutrition and lifestyle habits47,48,49 our findings should be analyzed considering Swedish maternal care quality and environmental factors between 1973 and 1998. Firstly, Nordic Nutritional Recommendations were launched in 1980 and updated several times50 resulting in diverse dietary recommendations in pregnancy. Previous reports show that maternal undernutrition is associated with worse kidney outcomes51 and altered neurodevelopment52 secondary to intrauterine micronutrient, energy, and protein deficits. Similarly, maternal obesity is also responsible for altered fetal brain and kidney development52,53. Secondly, a decreasing prevalence of maternal smoking was documented from 1983 to 199254. Smoking has been attributed to smaller HC in Swedes49 and smaller infant kidneys in the Netherlands55. Finally, climate change and variability and increasing air pollution trends due to urbanization might also influence our findings56,57,58.
Placental failure to ensure sufficient nutrition results in a discrepancy between BW and PW59. Typically, the BW-to-PW ratio reaches 5 to 7 at delivery60. A hypothesis that is currently debated proposes that smaller babies with relatively larger placentas might represent placenta insufficiency and increase the risk for fetal death59. However, a Norwegian report61 could confirm the opposite, i.e., that much larger babies relative to PW are exposed to a higher relative risk for fetal death. We could previously show that a lower BW-to-PW ratio predicts higher creatinine-based eGFR in middle-aged men17. We could also observe that this finding might even be related to lower cystatin C-based eGFR in younger adults. Unfortunately, this variable was only available in a small subset of the LifeGene cohort. These results should be carefully considered since the average eGFRcys was 103 (59 to 189) mL/min/1.732 and the average eGFRcr 89 (57 to 146) mL/min/1.732, i.e., within the normal range.
The study limitations should be highlighted. Firstly, this study enrolled mostly Swedish-born subjects from the Stockholm Region; therefore, it is hard to generalize for the global population. The maternal country/region of origin was diverse (Supplemental Table S2), but it mainly consisted of mothers born in Sweden. Secondly, the analysis of serum cystatin C was performed between 2009 and 2010, before the worldwide introduction of a calibrated method62, and therefore a slight deviation in cystatin C-based eGFR might exist. As expected, eGFRcr and eGFRcys demonstrate different associations to several parameters. These two GFR markers show different results which most often is dependent of body composition, e.g. muscle mass. This fact makes the conclusions less sharp. Thirdly, not all birth variables and eGFRcys data were available in the participants studied plausibly affecting predictive effects. Fourthly, temporal aspects of body composition could not be addressed properly due to the lack of data representing BMI or FMI variation through the lifetime. Fifthly, manual measurement of office blood pressure was utilized. Either 24-hour ambulatory blood pressure measurement or standardized home blood pressure measurement would provide more accurate information on hemodynamic regulation. Lastly, the absence of data on albuminuria limits the identification of kidney damage that manifests without a significant decline in eGFR. Other urinary markers, as well as urinary proteomics, could be of value in better defining early life influences on renal function.
The strength of this work is analysis of younger individuals in a sample size of over 12,000 individuals allows the identification of early stages of organ damage. Preventive medicine is very important due to population aging and aims to moderate the chronic disease burden trends worldwide. The high quality of birth data was also ensured by using the Swedish Medical Birth Register for LifeGene subjects born in 1973 or thereafter63. Inconsistent findings of studies clarifying the link between early life anthropometry and non-communicable diseases are widely discussed in the meta-analysis by Brander et al.64. The use of body composition over BMI and adjustment for current body size in regression analysis are critical in exploring the link between perinatal and postnatal factors and risk of adult chronic diseases64.
In conclusion, smaller head circumference is associated with lower estimated creatinine-based GFR in adult life. A lower birth weight-to-placenta ratio is also related to lower estimated cystatin C-based GFR. The postnatal weight down-regulation trajectory significantly affects a relatively lower eGFR but within the normal range. However, the postnatal catch-up pattern is associated with unaffected kidney function in young adults. The relationship between lower birth weight z-score and lower adult mean arterial and diastolic blood pressure was statistically but not clinically significant. This study reveals the complex interrelationship between early life factors and adult kidney function that could be directly and indirectly influenced by body fat accumulation.
Methods
Study sample
The LifeGene study randomly invited individuals 18 years or older from the general population in Stockholm, Sweden, between 2009 and 201665. The participants completed a comprehensive web-based questionnaire consisting of nine main parts: sociodemographic variables, lifestyle, women’s health, self-care, living conditions, health history, mental health, asthma or allergies, and injuries. A total of 12 167 individuals from the LifeGene Study between the ages of 18 and 43 were included in this study. Exclusion criteria: absence of data on birth weight, length and head circumference, gestational age, maternal age, body composition, blood pressure, and plasma creatinine.
All participants signed informed consent forms either at the site for blood sample collection or electronically. The ethical principles applied in this study was in line with The World Medical Association Declaration of Helsinki. Non-fasting blood samples were collected.
The study data were linked with the Swedish Medical Birth Register63, launched in 1973, which collects data on early life factors. In contrast, the registration of maternal data (weight, body mass index and smoking habits) started in 1983.
Study variables
Variables and data sources utilized for this study are listed in Supplemental Table S1.
Postnatal growth mismatch
The postnatal growth pattern was defined from BW z-score and bioimpedance acquired fat mass index (FMI). We have especially focused on two main features – postnatal down-regulation and postnatal catch-up. Postnatal down-regulation represents babies that are born larger in size than expected for gestational age but, during the postnatal period, develop at a slower pace than their counterparts. Postnatal catch-up defines a combination of poor fetal growth with rapid postnatal growth dramatically altering cardiometabolic health36,66.
FMI was used to explore the postnatal growth curve because it performed better in defining body composition and metabolic health than body mass index (BMI)67 in non-obese LifeGene Study participants.
The birth weight (BW) z-scores were calculated according to intrauterine growth curves for boys and girls68, as described in more detail in statistical part. Low BWz corresponded to more than − 2SD deviation from the mean, normal BWz - +/-2SD from the mean, and high BWz is a deviation more than + 2SD from the mean. Adult FMI was categorized as lower-than-average FMI – below sex-specific average, 6.1 kg/m2 for women, and 3.9 kg/m2 for men; higher-than-average FMI – equal or above sex-specific average.
The study sample was then divided into six groups:
1: Low BWz and lower-than-average FMI;
2: Normal BWz and lower-than-average FMI;
3: High BWz and lower-than-average FMI (postnatal down-regulation);
4: Low BWz and higher-than-average FMI (postnatal catch-up);
5: Normal BWz and higher-than-average FMI;
6: High BWz and higher-than-average FMI.
Definition of kidney function
Estimated glomerular filtration rate (eGFR) formulas were employed: i.e., cystatin C eGFR equation based on Caucasian, Asian, pediatric, and adult cohorts (CAPA, eGFRcys)69 and the Lund-Malmö revised creatinine-based eGFR equation (LMrev, eGFRcr)70. Both equations are validated and recognized by KDIGO 202471. The latter eGFR equation is widely used in Sweden since it is validated72 and is superior to other creatinine-based equations in defining kidney function.
Statistical analysis
Continuous normally distributed variables are presented as means with standard deviation (SD), skewed data – as median with interquartile range (IQR), and categorical variables – as frequencies with percentages. The birth weight (BW) z-scores were calculated as described below68.
The equation for expected BW:
For boys:
For girls:
The equation BW z-score:
Where BW(measured) is a raw value, BW(expected) is the calculated value, and SD(expected) is the population standard deviation.
For researching cardiovascular and renal interaction we utilized linear regression analysis with two different outcomes: (1) eGFR (creatinine or cystatin C-based ), and (2) mean arterial pressure (MAP). First, the univariate regression analysis with variables listed in Supplemental Table S1 was employed. Then, maternal and fetal factors (as explanatory variables) were adjusted for covariates such as adult age, sex, body mass index, and smoking/snuff status.
The linear regression models for eGFR as an outcome:
-
Model 1: eGFR (outcome) ~ early life factor adjusted for sex and gestational age.
-
Model 2: + adjustment for adult age and body mass index.
-
Model 3: + adjustment for mean arterial pressure.
-
Model 4: + adjustment for smoking/snuff status.
The linear regression models for MAP as an outcome:
-
Model 1: MAP (outcome) ~ birth weight z-score adjusted for sex and gestational age.
-
Model 2: + adjustment for adult age.
-
Model 3: + adjustment for eGFR.
-
Model 4: + adjustment for body mass index.
-
Model 5: + adjustment for smoking/snuff status.
To measure the amount of multicollinearity in linear models, the Variation Inflation Factors (VIF) were calculated. Variables with VIF levels above 2.0 were excluded from the models. Statistical analysis was performed with IBM SPSS Statistics software (Version 29.0, Chicago, IL, USA) and Microsoft® Excel for Mac (Version 16.88, Microsoft Corporation, 2021). P values below 0.05 were considered significant.
Data availability
Due to Swedish laws on personal integrity and health data, as well as the Ethics Review Board, we are not allowed to make any data, including health variables, open to the public, even if made anonymous. The data could be shared with other researchers after a request to the contact persons for The LifeGene study – Prof. Nancy Pedersen, nancy.pedersen@ki.se, or Dr. Sara Hagg, sara.hagg@ki.se. For details about the LifeGene cohort and instructions on how to apply for data, see link: www.lifegene.se.
References
Liu, C., He, Y., Venn, A. J., Jose, M. D. & Tian, J. Childhood modifiable risk factors and later life chronic kidney disease: A systematic review. BMC Nephrol. 24, 184 (2023).
Short, K. M. & Smyth, I. M. The contribution of branching morphogenesis to kidney development and disease. Nat. Rev. Nephrol. 12, 754–767 (2016).
Luyckx, V. et al. A developmental approach to the prevention of hypertension and kidney disease: A report from the Low Birth Weight and Nephron Number Working Group. The Lancet 390, 424–428 (2017). https://doi.org/10.1016/S0140-6736(17)30576-7
Grillo, M. A., Mariani, G. & Ferraris, J. R. Prematurity and low birth weight in neonates as a risk factor for obesity, hypertension, and chronic kidney disease in pediatric and adult age. Front. Med. (Lausanne) 8, 769734 (2022).
Terstappen, F. & Titia Lely, A. Long-term renal disease after prematurity or fetal growth restriction: Who is at risk? Nephrol. Dial. Transplant. 35, 1087–1090 (2020). https://doi.org/10.1093/ndt/gfaa167
van Lopes, V. A., Spaan, J. J., Cornelis, T. & Spaanderman, M. E. A. Prevalence of chronic kidney disease after preeclampsia. J. Nephrol. 30, 403–409 (2017).
Gonçalves, G. D. et al. Maternal hypoxia developmentally programs low podocyte endowment in male, but not female offspring. Anat. Rec. 303, 2668–2678 (2020).
Liefke, J. et al. Fetal growth restriction followed by very preterm birth is associated with smaller kidneys but preserved kidney function in adolescence. Pediatr. Nephrol. 38, 1855 (2023).
Ziauddeen, N. et al. Role of foetal kidney size on kidney function in childhood: The born in bradford cohort renal study. BMC Nephrol. 24, 41 (2023).
Wu, J. et al. Kidney volume and risk of incident kidney outcomes. J. Am. Soc. Nephrol. https://doi.org/10.1681/ASN.0000000000000419 (2024).
Barker, D. J. P. Developmental origins of chronic disease (2012). https://doi.org/10.1016/j.puhe.2011.11.014
Ronco, C., Bellasi, A. & Di Lullo, L. Cardiorenal syndrome: An overview. Adv. Chronic Kidney Dis. 25, 382–390 (2018).
Inserra, F., Forcada, P., Castellaro, A. & Castellaro, C. Chronic kidney disease and arterial stiffness: A two-way path. Front. Med. (Lausanne) 8, 765924 (2021).
Chade, A. R. Renal vascular structure and rarefaction (2013). https://doi.org/10.1002/cphy.c120012
Palatini, P. Glomerular hyperfiltration: A marker of early renal damage in pre-diabetes and pre-hypertension. Nephrology, dialysis, transplantation: Official publication of the European Dialysis and Transplant Association - European Renal Association 27, 1708–1714 (2012). https://doi.org/10.1093/ndt/gfs037
Gjerde, A., Lillas, B. S., Marti, H. P., Reisaeter, A. V. & Vikse, B. E. Intrauterine growth restriction, preterm birth and risk of end-stage renal disease during the first 50 years of life. Nephrol. Dial. Transplant. 35, 1157 (2020).
Laucyte-Cibulskiene, A., Sharma, S., Christensson, A. & Nilsson, P. M. Early life factors in relation to albuminuria and estimated glomerular filtration rate based on cystatin C and creatinine in adults from a Swedish population-based cohort study. J. Nephrol. 2021 1, 1–12 (2021).
Oren, A. et al. Gestational age and birth weight in relation to aortic stiffness in healthy young adults: Two separate mechanisms? Am. J. Hypertens. 16, 76–79 (2003).
Fagerberg, B., Bondjers, L. & Nilsson, P. Low birth weight in combination with catch-up growth predicts the occurrence of the metabolic syndrome in men at late middle age: The atherosclerosis and insulin resistance study. J. Intern. Med. 256, 254–259 (2004).
Ni, Y., Beckmann, J., Hurst, J. R., Morris, J. K. & Marlow, N. Size at birth, growth trajectory in early life and cardiovascular and metabolic risk in early adulthood: The EPICure study. Arch. Dis. Child. Fetal Neonatal Ed. 106, 149 (2021).
Rallis, D., Balomenou, F., Tzoufi, M. & Giapros, V. A systematic review indicates an association between birth weight and body fat in childhood. Acta Paediatr. 110, 2023–2039 (2021).
Stansfield, B. K. et al. Nonlinear relationship between birth weight and visceral fat in adolescents. J. Pediatr. 174, 185–192 (2016).
Resende, C. B. et al. Birth weight and body fat mass in adults assessed by bioimpedance in the ELSA-Brasil study. Cad Saude Publ. 37, (2021).
Mackenzie, H. S. & Brenner, B. M. Fewer nephrons at birth: A missing link in the etiology of essential hypertension? Am. J. Kidney Dis. 26, 91–98 (1995).
Luyckx, V. A. & Brenner, B. M. Birth weight, malnutrition and kidney-associated outcomes—A global concern. Nat. Rev. Nephrol. 11, 135–149 (2015).
Lei, X. et al. Childhood health outcomes in term, large-for-gestational-age babies with different postnatal growth patterns. Am. J. Epidemiol. 187, 507–514 (2018).
Himuro, H. et al. The association of birth weight and current BMI on the risk of hypertension: The Tohoku medical megabank community-based cohort study. Hypertens. Res. 47, 3025–3034 (2024).
Amine, I. et al. Environmental exposures in early-life and general health in childhood. Environ. Health 22, (2023).
Lopez-Sublet, M. et al. Birth weight and subclinical cardiovascular and renal damage in a population-based study (the STANISLAS cohort study). J. Hypertens. 41, (2023).
Pimenta, I. T. et al. Body shape trajectories are associated with birth weight, body mass index and sociodemographic conditions in participants of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil): A multiple correspondence analysis. BMC Public. Health 23, (2023).
Waage, C. W. et al. Cohort profile update: The Norwegian STORK Groruddalen (STORK G) pregnancy and birth cohort—the role of ethnicity and causal pathways for obesity, type 2 diabetes, cardiovascular disease and other health issues. BMJ Open. 13, (2023).
Jańczewska, I., Wierzba, J., Jańczewska, A., Szczurek-Gierczak, M. & Domżalska-Popadiuk, I. Prematurity and low birth weight and their impact on childhood growth patterns and the risk of long-term cardiovascular sequelae. Children 10 (2023). https://doi.org/10.3390/children10101599
Raisi-Estabragh, Z. et al. Lower birth weight is linked to poorer cardiovascular health in middle-aged population-based adults. Heart 109, (2023).
Prinz, N. et al. The association between perinatal factors and cardiometabolic risk factors in children and adolescents with overweight or obesity: A retrospective two-cohort study. PLoS Med. 20 (2023).
Nordman, H., Jääskeläinen, J. & Voutilainen, R. Birth size as a determinant of cardiometabolic risk factors in children. Horm. Res. Paediatr. 93, 144–153 (2020).
Kim, Y. J. et al. Impact of size at birth and postnatal growth on metabolic and neurocognitive outcomes in prematurely born school-age children. Sci. Rep. 11, 1–8 (2021).
Geelhoed, J. J. M. et al. Tracking and determinants of kidney size from fetal life until the age of 2 years: The Generation R study. Am. J. Kidney Dis. 53, 248–258 (2009).
Tomaszewski, M. et al. Glomerular hyperfiltration: A new marker of metabolic risk. Kidney Int. 71, 816–821 (2007).
Sasson, A. N. Renal hyperfiltration related to diabetes mellitus and obesity in human disease. World J. Diabetes 3, 1 (2012).
Delanaye, P. et al. Iohexol plasma clearance for measuring glomerular filtration rate in clinical practice and research: A review. Part 2: Why to measure glomerular filtration rate with iohexol? Clin. Kidney J. 9, 700–704 (2016). https://doi.org/10.1093/ckj/sfw071
Edwards, M. O. et al. Higher systolic blood pressure with normal vascular function measurements in preterm-born children. Acta Paediatr. 103, 904–912 (2014).
Kistner, A., Celsi, G., Vanpee, M. & Jacobson, S. H. Increased blood pressure but normal renal function in adult women born preterm. Pediatr. Nephrol. 15, 215–220 (2000).
Branda, J. I. F., de Almeida-Pititto, B., Bensenor, I., Lotufo, P. A. & Ferreira, S. R. G. Associations of prematurity and low birth weight with blood pressure and kidney function in middle-aged participants of the Brazilian longitudinal study of Adult Health: ELSA-Brasil. J. Nephrol. 36 (2023).
Zhang, Y. et al. The associations of high birth weight with blood pressure and hypertension in later life: A systematic review and meta-analysis. Hypertens. Res. 36:8 (36), 725–735 (2013).
Montaldo, P. et al. Impact of intrauterine growth restriction on cerebral and renal oxygenation and perfusion during the first 3 days after birth. (123AD) https://doi.org/10.1038/s41598-022-09199-5
Kooijman, M. N. et al. Childhood kidney outcomes in relation to fetal blood flow and kidney size. J. Am. Soc. Nephrol. 25, 2616–2624 (2014).
Miele, M. J. et al. Head circumference as an epigenetic risk factor for maternal nutrition. Front. Nutr. 9, (2022).
Tiwari, K. et al. Impact of malnutrition on head size and development quotient. Int. J. Res. Med. Sci. 5, (2017).
Källén, K. Maternal smoking during pregnancy and infant head circumference at birth. Early Hum. Dev. 58, (2000).
Saunders, C. M. et al. Food and nutrient intake and adherence to dietary recommendations during pregnancy: A nordic mother–child population-based cohort. Food Nutr. Res. 63 (2019).
Lee, Y. Q., Collins, C. E., Gordon, A., Rae, K. M. & Pringle, K. G. The relationship between maternal nutrition during pregnancy and offspring kidney structure and function in humans: A systematic review. Nutrients 10 (2018). https://doi.org/10.3390/nu10020241
Cortés-Albornoz, M. C., García-Guáqueta, D. P., Velez-Van-meerbeke, A. & Talero-Gutiérrez, C. Maternal nutrition and neurodevelopment: A scoping review. Nutrients 13 (2021). https://doi.org/10.3390/nu13103530
Wong, M. G., The, N. L. & Glastras, S. Maternal obesity and offspring risk of chronic kidney disease. Nephrology 23 (2018). https://doi.org/10.1111/nep.13462
Cnattingius, S. & Haglund, B. Decreasing smoking prevalence during pregnancy in Sweden: The effect on small-for-gestational-age births. Am. J. Public. Health 87 (1997).
Taal, H. R. et al. Maternal smoking during pregnancy and kidney volume in the offspring: The generation R study. Pediatr. Nephrol. 26 (2011).
Alvarez-Elias, A. C., Brenner, B. M. & Luyckx, V. A. Climate change and its influence in nephron mass. Curr. Opin. Nephrol. Hypertens. 33 (2024). https://doi.org/10.1097/MNH.0000000000000932
Henning, M., Westlund, H. & Enflo, K. Urban–rural population changes and spatial inequalities in Sweden. Reg. Sci. Policy Pract. 15 (2023).
Esper, J., Büntgen, U., Timonen, M. & Frank, D. C. Variability and extremes of northern scandinavian summer temperatures over the past two millennia. Glob Planet. Change 88–89, 1–9 (2012).
Sferruzzi-Perri, A. et al. Placental adaptation: What can we learn from Birthweight: Placental weight ratio? Front. Physiol. 7, 28 (2016).
Wallace, J. M., Bhattacharya, S. & Horgan, G. W. Gestational age, gender and parity specific centile charts for placental weight for singleton deliveries in Aberdeen, UK. https://doi.org/10.1016/j.placenta.2012.12.007
Haavaldsen, C., Samuelsen, S. O. & Eskild, A. Fetal death and placental weight/birthweight ratio: A population study. Acta Obstet. Gynecol. Scand. 92, 583–590 (2013).
Grubb, A. et al. Generation of a new cystatin C-based estimating equation for glomerular filtration rate by use of 7 assays standardized to the international calibrator. Clin. Chem. 60, 974–986 (2014).
Cnattingius, S. et al. The Swedish medical birth register during five decades: Documentation of the content and quality of the register. Eur. J. Epidemiol. 38, 109–120 (2023).
Bander, A. et al. Childhood BMI and other measures of body composition as a predictor of cardiometabolic non-communicable diseases in adulthood: A systematic review. Public Health Nutr. 26 (2023). https://doi.org/10.1017/S136898002200235X
Almqvist, C. et al. LifeGene—A large prospective population-based study of global relevance. Eur. J. Epidemiol. 26, 67 (2011).
Ong, Y. Y. et al. Erratum to: Mismatch between poor fetal growth and rapid postnatal weight gain in the first 2 years of life is associated with higher blood pressure and insulin resistance without increased adiposity in childhood: The GUSTO cohort study. Int. J. Epidemiol. 50, 702–702 (2021).
Liu, P., Ma, F., Lou, H. & Liu, Y. The utility of fat mass index vs. body mass index and percentage of body fat in the screening of metabolic syndrome (2013). https://doi.org/10.1186/1471-2458-13-629
Maršál, K. et al. Intrauterine growth curves based on ultrasonically estimated foetal weights. Acta Paediatr. 85, 843–848 (1996).
Inker, L. A. et al. Estimating glomerular filtration rate from serum creatinine and Cystatin C. N. Engl. J. Med. 367, 20–29 (2012).
Björk, J., Grubb, A., Sterner, G. & Nyman, U. Revised equations for estimating glomerular filtration rate based on the Lund-Malmö Study cohort. Scand. J. Clin. Lab. Invest. 71, 232–239 (2011).
Stevens, P. E. et al. KDIGO 2024 Clinical Practice Guideline for the evaluation and management of chronic kidney disease. Kidney Int. 105, S117–S314 (2024).
Nyman, U. et al. The revised Lund-Malmö GFR estimating equation outperforms MDRD and CKD-EPI across GFR, age and BMI intervals in a large Swedish population. Clin. Chem. Lab. Med. 52, 815–824 (2014).
Acknowledgements
The LifeGene Study has been funded by the Torsten and Ragnar Söderbergs Foundation, AFA Insurance, Karolinska Institute, the Stockholm County Council, and the Swedish Research Council. The funders had no role in study design, data collection and analysis, decision to publish, or manuscript preparation.
Funding
Open access funding provided by Lund University.
Author information
Authors and Affiliations
Contributions
AL-C designed the study, conducted the statistical analyses, and wrote the first draft. All authors (AL-C, SH, AC, PMN) contributed with intellectual content, revised and approved the final version of the manuscript before submission. SH is the current PI for the LifeGene cohort. PMN is the academic guarantor of the study, its data, and statistical analyses.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Ethics Review Authority (Etikprövningsmyndigheten), Sweden (Dnr: 2019–02408), based on an earlier approval of the LifeGene study from the Ethics Review Board at Karolinska Institute (Dnr: 2009/615 − 31/1), and in addition the LifeGene legal permission by Swedish law (Lag 2013:794).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Laucyte-Cibulskiene, A., Hägg, S., Christensson, A. et al. Early life factors and variation in adult kidney function in the Swedish LifeGene cohort. Sci Rep 15, 5046 (2025). https://doi.org/10.1038/s41598-025-88928-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-88928-y