Abstract
Spinal Muscular Atrophy (SMA) is a genetic neuromuscular disorder caused by homozygous mutation or deletion of the survival motor neuron 1 (SMN1) gene, leading to a low quantity of SMN protein in cells. This depletion of SMN protein preferentially leads to death of motor neurons and, consequently, muscle atrophy, in addition to defects in many other peripheral tissues. SMN protein is naturally loaded into extracellular vesicles (EVs), which are sub-micron-sized, membrane-bound particles released from all cell types. The innate ability of EVs to deliver cargo to recipient cells has caused these vesicles to gain interest as therapeutic delivery vehicles. In this study, we show that adenovirus-mediated overexpression of SMN protein in HepG2 cells leads to the release of EVs loaded with high levels of SMN protein into conditioned medium. Application of this medium to recipient cells in tissue culture led to uptake of the SMN protein, which subsequently transited to the nucleus and co-localized with Gemin2 protein, forming nuclear gem-like structures similar to the native SMN protein. Overall, this work demonstrates that SMN protein can be delivered to cells through EVs, which holds promise as a potential therapy for patients with SMA.
Similar content being viewed by others
Introduction
Spinal muscular atrophy (SMA) is a neuromuscular disorder caused by homozygous mutation or deletion of the survival motor neuron 1 (SMN1) gene1, resulting in inadequate levels of survival motor neuron (SMN) protein within cells2. Depletion of SMN protein causes degeneration of alpha motor neurons in the spinal cord, leading to progressive muscle weakness and atrophy3. For the most common and severe form of SMA, Type I, patients typically succumb to respiratory failure around 8 months of age if untreated4,5,6. Although SMA is primarily considered a neuromuscular disease, low levels of SMN protein also has detrimental effects on many other tissues and organs, including the heart7,8, liver9,10, thymus11, pancreas12,13, gastrointestinal and enteric nervous system14, and spleen11,15. Several therapies are available for treatment of SMA, each focusing on increasing SMN protein levels16,17,18. Although the use of these therapeutics can improve both the length and quality of life, patients can show varying response to treatment16,17,19,20. Furthermore, each treatment comes with advantages and risks21,22,23,24, suggesting that there is still a need to investigate alternative approaches to treatment.
SMN protein is present in both the nucleus and cytoplasm of cells25,26. In the nucleus, SMN protein localizes to structures called Gemini of coiled bodies (gems). SMN protein associates with Gemin proteins 2–8 and Unrip to form the SMN complex, a multiprotein complex crucial for assembly of small nuclear ribonucleoproteins (snRNPs) which are essential for pre-messenger ribonucleic acid (mRNA) splicing27,28,29,30,31,32,33. The SMN complex is also believed to play a role in the assembly of small nucleolar ribonucleoproteins (snoRNPs), which are involved in post-transcriptional processing and modification of ribosomal RNA in the nucleolus34,35. There is also some evidence that the SMN complex is associated with telomerase, a complex that adds repeat sequences at chromosomal ends, thus elongating telomeres36,37,38. SMN protein has been implicated in numerous other cellular functions, including translational regulation39,40,41, active transport of mRNA42,43, actin dynamics44,45, and resolution of R-loops in genetic terminal regions46. Although many functions of SMN protein have been described, the precise cellular role of SMN protein that results in pathogenesis of SMA remains unclear.
Interestingly, SMN protein is naturally loaded into extracellular vesicles (EVs)47,48,49,50,51,52. EVs are sub-micron-sized, membrane-bound particles released from all cell types into bodily fluids, or culture media in tissue culture53. There are several types of EVs that are classified based on mechanism of biogenesis and diameter, the most extensively characterized being exosomes and microparticles53. EVs are packed with proteins, nucleic acids, and lipids, and can deliver these biomolecules to recipient cells that take up the EVs, which can be located near or distant from where the vesicles originate53,54,55. EVs possess many desirable attributes that can be exploited to deliver therapeutic cargo, such as a lipid bilayer that protects contents from degradation in the bloodstream56, the ability to transit the blood–brain barrier (BBB)57,58,59, and the capacity to be bioengineered to increase loading of desirable therapeutic cargo60. EVs have been used successfully to deliver a variety of therapeutic proteins in many different studies. For example, delivery of catalase-loaded EVs led to rapid uptake of the protein by neuronal cells in culture, and neuroprotection in a mouse model of Parkinson’s disease61. Similarly, neprilysin-loaded EVs provided neuroprotection and improved behavioural function in a mouse model of Alzheimer’s disease62.
In this study, we show that overexpression of SMN protein in tissue culture leads to the release of EVs containing high quantities of the SMN protein. Importantly, these EVs were able to transfer the protein to recipient cells, where the exogenous SMN protein localized to nuclear gem-like structures and interacted with normal cellular protein partners. Our work suggests that EVs loaded with SMN protein may represent a new therapeutic class to treat patients with SMA.
Results
Development and characterization of a donor cell line for production of EVs loaded with SMN protein
For our studies of EV-mediated delivery of SMN protein to recipient cells, we needed to distinguish between endogenous and exogenous SMN protein. We, and many others, have shown that the presence of an N-terminal FLAG tag does not appear to affect protein localization and ability to interact with natural protein partners63,64,65. We also previously showed that two common methods can be used to generate cell lines expressing a FLAG-tagged version of SMN protein that is subsequently efficiently loaded into EVs: plasmid-based expression and selection of a stable cell line or adenovirus (Ad)-mediated overexpression of the protein47. We initially explored the first option, generation of a stable cell line, as this represents a simpler “one component” production system (i.e. only the EV-producer cell line), compared to the “two-component” Ad system that requires a vector and an EV-producer cell line. Furthermore, Ad-mediated overexpression of a protein typically results in supraphysiological levels of the protein47,63,66, which would impede our ability to determine whether the protein was acting as normal in the producer cell line.
We generated a stable cell line expressing a triple FLAG-tagged version of the SMN (3F-SMN) protein using the HepG2 cell line, originally derived from a human male hepatocellular carcinoma67. We chose HepG2 cells, since we previously showed that this cell line naturally releases EVs with high SMN protein content47. In the stable cell line, SMN expression is controlled by the human cytomegalovirus (CMV) immediate early enhancer/promoter, with the SMN1 cDNA located upstream of an internal ribosome entry site (IRES) derived from the encephalomyocarditis virus (EMCV)68, hygromycin resistance gene, and simian virus 40 (SV40) polyadenylation sequence. The pooled population of hygromycin resistant cells, designated HepG2:3F-SMN, were first analyzed by immunoblot. Both the parental HepG2 and HepG2:3F-SMN cell lines showed a protein of ~ 38 kDa, representing the endogenous SMN protein (Fig. 1A). The signal for this SMN protein in the HepG2:3F-SMN cell line was ~ 75% of that observed in the parental HepG2 cells. HepG2:3F-SMN also contained an SMN-positive band of ~ 41 kDa, representing the 3F-SMN protein. Densitometry analysis showed that the total level of SMN protein (i.e. the ~ 38 kDa SMN and ~ 41 kDa 3F-SMN) in HepG2:3F-SMN cells was approximately 1.5-fold higher than the level of endogenous SMN protein in the parental HepG2 cells. As anticipated, there was no FLAG signal present in parental HepG2 cells, but a positive signal of ~ 41 kDa in the HepG2:3F-SMN cell line. We also observed a minor band of ~ 35 kDa in both the SMN and FLAG immunoblots, which may represent a proteolytically cleaved form of SMN protein. A co-immunoprecipitation (co-IP) experiment was performed to confirm that the N-terminal triple FLAG tag did not interfere with the ability of the protein to self-associate or interact with normal cellular partners, such as Gemin2. As shown in Fig. 1B, pulldown of the tagged SMN protein with antibody to FLAG resulted in co-IP of both endogenous SMN and Gemin2 proteins. Finally, we examined localization of the tagged SMN protein within the cells by immunofluorescence. In parental HepG2 cells, SMN protein was located in both the cytoplasm and nucleus, with nuclear-localized SMN protein localized in gem-like foci (Fig. 1C). For HepG2:3F-SMN, the 3F-SMN protein was also located in both the cytoplasm and nucleus and, again, within gem-like structures in the nucleus. The average integrated SMN signal intensity in HepG2:3F-SMN cells was ~ 1.2-fold above that of HepG2 cells, supporting the increase in total SMN protein level shown in Fig. 1A. Interestingly, the average number of gems per 100 cells ± SD was 146 ± 11.5 and 257 ± 28.2 in the HepG2 and HepG2:3F-SMN cell lines, respectively (Fig. 1D), consistent with the observation that gem number roughly correlated with level of SMN expression within the cell26. Overall, these data demonstrate that HepG2:3F-SMN cells were effectively engineered to overexpress SMN protein that localizes normally and interacts with normal cellular partners in the producer cell line.
The presence of a 3xFLAG-tag on SMN protein does not affect protein localization within the cell or ability to interact with normal cellular protein partners. Panel A: A HepG2 cell line stably expressing a 3xFLAG-tagged SMN protein was assessed for protein expression by immunoblot. Grey arrows indicate the 3F-SMN protein and the black arrow indicates endogenous SMN protein. Panel B: Co-immunoprecipitation (Co-IP) was performed using anti-FLAG or isotype control (IgG). Input, bound, and unbound fractions were assessed by immunoblot. Grey arrows indicate the 3F-SMN protein and the black arrow indicates endogenous SMN protein. Panel C: Epifluorescence microscopy images of HepG2:3F-SMN cells stained with antibodies to tubulin and SMN, or tubulin and FLAG. Arrows indicate representative nuclear gems. Scale bars represent 10 µm. Panel D: Quantified nuclear gems per 100 cells in epifluorescence microscopy images of HepG2 and HepG2:3F-SMN stained with anti-tubulin and anti-SMN. Data was tested for significance using an unpaired t-test, where two asterisk (**) indicates p < 0.01. Data represents 3 independent experiments.
We next characterized EVs released from the HepG2:3F-SMN cell line, and specifically the incorporation of the 3F-SMN protein into EVs. HepG2 and HepG2:3F-SMN cells were plated at equal density, and equal volumes of conditioned medium (CM) were collected from these cells after 72 h. EVs were isolated by ultracentrifugation from the CM and resuspended in equal volumes of PBS. We first characterized the size and number of EVs isolated from the HepG2 and HepG2:3F-SMN cell lines by nanoparticle tracking analysis (NTA) (Fig. 2A). The majority of particles isolated from both cell lines were ≤ 200 nm in diameter, and there appeared to be no significant difference between the concentration or distribution of particle sizes isolated from HepG2 and HepG2:3F-SMN cells. The peak particle diameter for EVs isolated by ultracentrifugation from HepG2 and HepG2:3F-SMN were 87 nm and 91 nm, respectively. We next analyzed the protein content of the EVs by immunoblot, and we included lysates from the cells as control (Fig. 2B). EVs isolated from both cell types had similar Flotillin-2, ALIX (ALG-2-interacting protein X), and CD29 (integrin beta-1) protein signals, common markers of EVs53. As anticipated, EVs released by parental HepG2 cells had a single SMN protein species of ~ 38 kDa representing the native protein. For EVs isolated from HepG2:3F-SMN cells, we observed a signal corresponding to the native SMN protein, but also SMN-positive signals at approximately 41 and 35 kDa. The 41 kDa species represents the 3xFLAG-tagged version of SMN protein, as a band of similar size was detected on immunoblots probed with antibody to FLAG, and the 35 kDa species may represent a proteolytically cleaved product. The overall SMN protein signal within EVs isolated from HepG2:3F-SMN cells was approximately 2.5-fold higher than that observed in EVs isolated from parental HepG2 cells, consistent with the level of expression of SMN protein within the two cell lines. Taken together, these data show that the presence of the 3xFLAG tag on the SMN protein does not appear to adversely affect localization within the cell, interaction with normal protein partners, or the ability of the protein to be incorporated into EVs.
EVs released by HepG2:3F-SMN cells contain 3F-SMN protein. Panel A: Conditioned medium (CM) was collected from HepG2 and HepG2:3F-SMN cells 72 h post-plating. Cellular debris and apoptotic bodies were removed by low-speed centrifugation, and EVs were isolated by ultracentrifugation. Particle diameter was assessed by nanoparticle tracking analysis. Panel B: Protein content of isolated EVs was examined by immunoblot with the indicated antibodies, with total cellular lysates from the two cell lines included as controls.
Generation of a recipient cell line containing HA-tagged Gemin2
SMN protein naturally co-localizes and interacts with Gemin2 protein within the nucleus of cells29, an observation that we ultimately hoped to use as a read-out for successful delivery of SMN protein from our EVs. However, Gemin2 protein is also naturally contained in EVs48, precluding our ability to distinguish between association of the delivered 3F-SMN protein with Gemin2 protein that was co-delivered in the EVs and native protein within the recipient cell. We therefore generated a recipient cell line stably expressing a human influenza hemagglutinin (HA)-tagged Gemin2 protein. We used A549 cells to establish the cell line, as they are a flat, robust cell line ideal for immunofluorescence studies. For this cell line, expression is once again controlled by the human CMV immediate early enhancer/promoter, with the N-terminal tagged HA-Gemin2 cDNA located upstream of an EMCV-derived IRES, hygromycin resistance gene, and SV40 polyadenylation sequence. The pooled population of hygromycin resistant cells, designated A549:HA-Gemin2, were subsequently analyzed by immunoblot (Fig. 3). In this cell line, the HA-tagged Gemin2 protein was expressed at approximately the same level as endogenous protein (Fig. 3A), and was capable of interacting with SMN protein as assessed by co-IP (Fig. 3B). Immunofluorescence microscopy showed that the HA-tagged Gemin2 protein was present in both the cytoplasm and nucleus, similar to endogenous protein, and localized in the nucleus to gem-like structures (Fig. 3C). Thus, the presence of the HA tag on Gemin2 protein does not appear to affect protein localization or normal protein interactions. Interestingly, immunofluorescence microscopy revealed that A549:HA-Gemin2 cells possessed less SMN-containing nuclear gems than parental A549 cells (Fig. 3D, 3E). Indeed, the A549 cell line possessed 134 ± 22.5 SMN-positive nuclear gems per 100 cells, whereas A549:HA-Gemin2 cell line possessed 38 ± 9.8 SMN-positive gems per 100 cells ± SD. Nuclear gems are comprised of SMN protein along with several members of the Gemin protein family, amongst other proteins69,70. Previous work has shown that knockdown of SMN protein or any of the Gemin proteins reduces the number of gems observed within the nucleus of the cell69. Conversely, overexpression of Gemin4, which is naturally found predominantly in the nucleus of cells, causes a relocalization of the endogenous SMN protein to almost exclusive nuclear localization, and a concomitant increase in the number of nuclear gems71. In A549:HA-Gemin2 cells, HA-Gemin2 was found in both the cytoplasm and the nucleus, which correlated with a reduction in the number of SMN protein-positive gems in the nucleus of these cells, suggesting that the endogenous SMN protein was partly relocalized by the overexpressed Gemin2 to the cytoplasm in these cells. Nevertheless, these data suggest that A549:HA-Gemin2 is a suitable cell line to evaluate EV-mediated delivery of 3F-SMN protein.
Generation and characterization of an A549 cell line expressing an HA-tagged Gemin2 protein. Panel A: An A549 cell line stably expressing HA-tagged Gemin2 protein was assessed by immunoblot with the indicated antibodies. Panel B: Co-immunoprecipitation (Co-IP) was performed using anti-HA or isotype control (IgG). Input, bound, and unbound fractions were assessed by immunoblot. Panel C: Epifluorescence microscopy images of A549:HA-Gemin2 cells stained with anti-HA and anti-Gemin2. Arrows indicate nuclear gems. Panel D: Epifluorescence microscopy images of A549:HA-Gemin2 cells stained with anti-HA and anti-SMN, with arrows indicating nuclear gem-like structures. Scale bars represent 10 µm. Panel E: Quantified SMN-positive nuclear gems per 100 cells in epifluorescence microscopy images as processed in panel D. Data was tested for significance using an unpaired t-test, where two asterisk (**) indicates p < 0.01. Data represents 3 independent experiments.
Enhancing the quantity of 3F-SMN protein in EVs through Ad-vector mediated overexpression in the donor cell line
We initially examined whether application of CM (i.e. clarified medium from cells, without concentration of the EVs) from HepG2:3F-SMN could result in detectable uptake of the protein on A549:HA-Gemin2 cells, but were unable to detect FLAG-positive signal by immunofluorescence microscopy (data not shown). Subsequent work showed that if we concentrated the EVs from CM approximately 200-fold through ultracentrifugation, we could detect significant FLAG-positive signal on the recipient cells. However, this FLAG-positive signal appeared to be primarily large aggregates that were likely on the cell surface, which precluded us from confidently detecting internalization and correct localization of the protein (data not shown).
We previously showed that we could significantly increase the quantity of SMN protein within EVs through the use of Ad-mediated overexpression47. This approach would allow us to increase the quantity of 3F-SMN protein in each EV, and avoid the complications associated with EV concentration noted above. HepG2 cells were transduced with a non-replicating Ad vector containing a gene for expression of 3F-SMN protein (Ad3F-SMN) at varying multiplicities of infection (MOI). Seventy-two hours post-infection (hpi), cell lysates and CM were collected. As shown in Fig. 4A, infection of HepG2 cells with Ad3F-SMN resulted in a dose-dependent increase in quantity of 3F-SMN protein within the cells, which amounted to a 15- to 25-fold increase in total SMN protein within the cells (Fig. 4B). A similar relationship was noted for SMN protein content in EVs isolated from CM from the infected cells, with a > 20-fold increase in SMN protein content at the highest MOI examined (Fig. 4C). Thus, HepG2 cells expressing 3F-SMN protein through Ad vector transduction release EVs loaded with ~ tenfold more SMN protein than EVs isolated from the HepG2:3F-SMN cell line. We also characterized the size and concentration of EVs isolated from HepG2 cells transduced with Ad3F-SMN by NTA (Fig. 4D). The populations of EVs released from HepG2 cells transduced at different MOIs appear to have similar concentrations and size distributions, primarily ≤ 200 nm, and are not significantly different from EVs released from mock-infected cells. All samples had a similar median particle diameter of ~ 100 nm, regardless of MOI. The NTA data demonstrates that Ad transduction has no overt effect on release of EVs from HepG2 cells at the MOIs used, and the population of particles are consistent with small EVs. Collectively, this data shows that Ad-mediated overexpression of SMN protein can be utilized as a technique to significantly increase the concentration of SMN protein contained in EVs. For the remainder of this study, “3F-SMN CM” indicates CM collected from HepG2 cells transduced with Ad3F-SMN at an MOI = 200.
Adenoviral-mediated overexpression of 3F-SMN protein in HepG2 cells leads to the release of EVs containing high levels of the 3F-SMN protein. Panel A: HepG2 cells were infected with Ad3F-SMN at an MOI = 50, 100, 200, or mock infected (PBS). Seventy-two hpi, cell lysates were collected and EVs were isolated using polyethylene glycol (PEG). Protein content of the EVs was examined by immunoblot. Endogenous SMN protein is indicated by a grey arrow and 3F-SMN protein is indicated by a black arrow. The red square indicates the region used for quantification of SMN protein signal for Panel B and C. Panel B: SMN protein signal in cell lysates were quantified, and the fold change in SMN protein signal relative to endogenous SMN protein signal is shown. Panel C: SMN protein signal in EVs was quantified and presented as the fold change in SMN protein signal relative to endogenous SMN protein signal. Panel D: Particle size and diameter of isolated EVs was assessed by nanoparticle tracking analysis. In panels B and C, significance was calculated after transforming data by log transformation, then tested for significance using one-way ANOVA followed by Tukey’s multiple comparisons test. An asterisk (*) indicates p < 0.05, two asterisk (**) indicates p < 0.01, and three asterisk (***) indicates p < 0.001. Data represents 3 independent experiments.
EVs can deliver SMN protein to recipient cells
We next examined whether CM from Ad3F-SMN-transduced cells could be used to transfer 3F-SMN protein to recipient cells. HepG2 cells were transduced with Ad3F-SMN at an MOI = 200 or mock infected with PBS and, 72 h later, CM was collected for transfer onto A549:HA-Gemin2 cells. Of note, for all media transfer experiments, the CM was subjected to low-speed centrifugation to remove cell debris and large EV (e.g. apoptotic bodies) prior to application to the recipient cells, but was not concentrated or further processed. Although the residual Ad3F-SMN inoculum was washed from the HepG2 cells prior to the 72 h incubation, small amounts of Ad vector could be present in the medium, which may lead to de novo synthesis of 3F-SMN protein in the A549:HA-Gemin2 cell line, confounding our analysis. We used two strategies to alleviate this concern. First, transcription from an infecting Ad genome typically does not initiate before ~ 2 h after application of the virus72,73, so we limited our CM incubation to 2 h. Second, we performed our incubation of CM with the A549:HA-Gemin2 cells in the presence or absence of 5,6-dichloro-1-β-D-ribofuranosylbenzimidazole (DRB), an inhibitor of RNA polymerase transcription elongation74. We previously showed that DRB effectively prevents transcription from the Ad genome75,76, and thus would prevent gene expression from any vector inadvertently transferred in the CM. Control CM (from mock-infected HepG2) or 3F-SMN CM was applied to A549:HA-Gemin2 cells for 2 h, in the presence or absence of DRB, and then analyzed for the presence of 3F-SMN protein by epifluorescence microscopy. As expected, no FLAG signal was detected in the mock treatment groups (Fig. 5A). In cells treated with 3F-SMN CM, a similar FLAG signal was visible in both DRB- and vehicle-treated groups. Indeed, in DRB- and vehicle-treated groups, ~ 730 and ~ 820 FLAG-positive nuclear foci per 100 cells, respectively, were detected, which may represent a combination of 3F-SMN protein in nuclear gems and also other smaller foci. Thus, at least a portion of the delivered 3F-SMN protein was localizing to the nucleus. We also observed concentrated FLAG signal within the cytoplasm of treated cells. Overall, this data suggests that EVs can be used to deliver SMN protein to recipient A549:HA-Gemin2 cells in tissue culture.
Application of conditioned medium containing EVs loaded with 3F-SMN protein onto A549:HA-Gemin2 cells results in FLAG-positive nuclear foci. Panel A: Conditioned medium (CM) from HepG2 cells infected with Ad3F-SMN or mock-infected was applied to A549:HA-Gemin2 cells in the presence or absence of 100 μM 5,6-dichloro-1-β-D-ribofuranosylbenzimidazole (DRB). Two h post-treatment, the cells were washed and processed for immunofluorescent staining with anti-FLAG and anti-HA, and images were captured by epifluorescence microscopy. Arrows indicate representative nuclear gem-like foci. Scale bars represent 10 µm. Panel B: FLAG-positive nuclear foci were quantified and expressed per 100 cells. Significance was calculated after transforming data by log transformation using two-way ANOVA followed by Tukey’s multiple comparisons test. Four asterisk (****) indicates p < 0.0001. Data represents 3 independent experiments.
To more precisely evaluate the localization of the EV-delivered 3F-SMN protein in the A549:HA-Gemin2 cells, we performed confocal microscopy and examined orthogonal projections generated from three-dimensional (3D) reconstructions. As in our previous experiment, CM was applied for 2 h in the presence or absence of DRB to inhibit de novo gene expression from any residual Ad vector that may have been present. Once again, no FLAG signal was observed in cells treated with mock CM (Fig. 6A). For both vehicle- and DRB-treated cells, application of 3F-SMN CM resulted in the presence of FLAG signal in both the cytoplasm and nucleus. An analysis of orthogonal projections of the images presented in Fig. 6A clearly showed that treatment with 3F-SMN CM resulted in the presence of 3F-SMN protein in specific foci in the nucleus that resemble nuclear gems (Fig. 6B). Indeed, the nuclear structures observed in 3F-SMN treated cells appear similar in size and morphology to native SMN-containing gems in untreated cells (Fig. 6C). Interestingly, in both treated and untreated cells, the SMN-positive nuclear gems appear more like cylindrical structures rather than spheres, that are oriented perpendicular to the plane of the coverslip on which the cells were grown.
EV-delivered 3F-SMN protein is internalized by recipient A549:HA-Gemin2 cells and localizes in gem-like structures. Panel A: Confocal immunofluorescence images of A549:HA-Gemin2 cells that were treated for 2 h with mock or 3F-SMN CM, and processed with antibodies to HA and FLAG. Panel B: Images in panel A were examined through orthogonal projections generated from z-stacks. Panel C: Orthogonal projections generated of z-stacks of parental A549 cells stained with antibodies to tubulin and SMN. Scale bars represent 10 µm.
We also examined whether the 3F-SMN protein present in nuclear gem-like structures co-localized with HA-Gemin2 protein (Fig. 7A). As expected, no FLAG signal was present in A549:HA-Gemin2 cells treated with CM from mock-infected HepG2 cells. In cells treated with 3F-SMN CM, there was a clear overlap between FLAG and HA signals indicating these proteins co-localized in the nucleus. Indeed, in orthogonal projections of 3F-SMN treated cells, there were distinct merged regions of yellow signals in the nucleus, clearly illustrating co-localization of the HA-Gemin2 and 3F-SMN proteins (Fig. 7B, 7C). We also examined whether EVs could be used to deliver SMN protein tagged with mCherry. CM was prepared as in our previous experiments: HepG2 cells were transduced with AdmCherry-SMN at an MOI = 200 for 1 h, CM was collected 72 h post-infection, and centrifuged to remove large debris. Once again, the EV were not concentrated from the CM before application to the recipient cells. The mCherry-SMN CM was applied to recipient parental A549 cells (i.e. not overexpressing the HA-tagged Gemin2 protein) for 2 h, and delivery of mCherry-SMN protein was analyzed by confocal microscopy. As in our previous experiments, mCherry-SMN protein was present in the cytoplasm and nucleus of treated A549 cells (Fig. 8A). In the nucleus, mCherry-SMN protein localized in nuclear gem-like structures that appeared similar in size and morphology to those observed in Figs. 6 and 7. Taken together these data suggest that EV can efficiently deliver SMN protein to A549 cancer cells in culture.
3F-SMN protein co-localizes with HA-Gemin2 in nuclear gem-like structures in A549:HA-Gemin2 cells. Panel A: Confocal immunofluorescence images of A549:HA-Gemin2 cells that were treated for 2 h with mock or 3F-SMN CM, and processed with antibodies to HA and FLAG. Panel B: The image in panel A (lower panel) was further examined through orthogonal projections generated from z-stacks. Panel C: Additional images and orthogonal projections from A549:HA-Gemin2 cells treated with 3F-SMN CM showing colocalization of 3F-SMN and HA-Gemin2 proteins. Scale bars represent 10 µm.
EV-mediated delivery of mCherry-SMN and 3F-SMN protein to A549 cells and fibroblasts derived from an SMA patient. Panel A: CM from HepG2 cells infected with AdmCherry-SMN was applied to A549 cells. Two h post-treatment, the cells were washed, fixed, and stained with Hoechst to visualize nuclei. Images were captured by confocal microscopy. Panel B: CM from HepG2 cells infected with Ad3F-SMN or mock-infected was applied to fibroblasts derived from a patient with SMA. Two h post-treatment, the cells were washed and processed for immunofluorescence staining with anti-FLAG and anti-tubulin, and images were captured by confocal microscopy. Scale bars represent 10 µm.
Finally, we examined whether EVs could efficiently deliver SMN protein to fibroblasts derived from an SMA patient. Fibroblasts were treated for 2 h with mock or 3F-SMN CM, and delivery of 3F-SMN protein was assessed by confocal microscopy. As expected, no FLAG signal was present in the cells treated with mock CM (Fig. 8B). In cells treated with 3F-SMN CM, there was a strong FLAG signal present in both the cytoplasm and nucleus of these cells. Within the nucleus, FLAG-positive foci resembling nuclear gems were present. Thus, EV can be used to deliver SMN protein to SMN-deficient cells.
Overall, these data show that EVs can effectively deliver SMN protein to recipient cells in tissue culture, including cells with low levels of SMN protein, resulting in accumulation of the protein in both the cytoplasm and gem-like structures within the nucleus of the treated cells.
Discussion
SMA is a devastating disease characterized by degeneration of the alpha motor neurons of the spinal cord leading to atrophy of skeletal muscle, although primary defects also occur in many other tissues and organs3,77,78. Severe forms of the disease are lethal at a very early age if left untreated. SMA is caused by inadequate levels of SMN protein within cells1,2. All three of the currently approved therapeutics for treatment of SMA focus on increasing cellular levels of SMN protein. Nusinersen is an anti-sense oligonucleotide (ASO) that acts on SMN2 pre-mRNA to promote inclusion of exon 7, ultimately leading to greater production of full-length protein16,79,80. However, patients can show a variable response to treatment, with up to 50% of treated patients failing to respond in clinical trial, for reasons that are unknown19. Furthermore, ASOs, including nusinersen, come with risks, such as coagulation abnormalities, renal toxicity, and thrombocytopenia21, and intrathecal administration also comes with risks, including meningitis81 and post-lumbar puncture syndrome82. Risdiplam is another drug available for treatment of SMA that increases production of full-length SMN protein also by modulating splicing of SMN2 pre-mRNA22. Daily oral administration of risdiplam led to modest improvements in motor function in clinical trial, but lower than that observed with nusinersen79,83. In animal models, risdiplam has been associated with retinal toxicity and off-target splicing of other genes22. Onasemnogene abeparvovec is an adeno-associated virus (AAV) gene therapy drug that increases cellular levels of SMN protein through delivery of a functional copy of the SMN1 cDNA84,85. Many of the children treated in clinical trial gained new motor milestones and survived without the need for permanent ventilation, which rarely occurs in untreated patients84,85,86,87,88. However, many safety concerns have been raised due to the high absolute dose of vector delivered to patients, up to 2.3 × 1015 vector genomes89, and the severe adverse events that have occurred in some treated patients or preclinical models, including thrombotic microangiopathy24, necrotizing enterocolitis90, and acute liver failure23,91,92. As there are several issues with the available therapies for treatment of SMA, there is still a need for development of alternative therapeutics.
A number of different approaches have been investigated to deliver SMN protein to cells. A recombinant SMN protein fused to the catalytic and transmembrane domains of diphtheria toxin (Dtx) and tetanus toxin fragment C (TTC) was investigated as a method to target the SMN protein specifically to neurons93. Unfortunately, in tissue culture, the SMN-Dtx-TTC fusion protein remained at the surface of primary neurons, and was unable to transit to the nucleus. A fusion protein of SMN and the cell-penetrating peptide transactivator of transcription (TAT) of human immunodeficiency virus was also unable to be internalized by rat cortical neurons or SH-SY5Y cells, a neuroblastoma cell line94. We have now shown that an Ad-based vector can be used to greatly enhance the quantity of SMN protein within EVs released from cells, and that such EVs can very effectively deliver the protein to recipient cells. Previous studies have shown that many EV-delivered proteins aggregate in the cytoplasm, or fail to escape the endosome and consequently these EVs and their contents are degraded in the lysosome95. Importantly, in our study, the delivered 3F-SMN protein localized to gem-like structures in the nucleus and co-localized with cellular Gemin2 protein. Thus, we have developed a new and effective method to deliver SMN protein to cells in tissue culture.
EV-mediated delivery of SMN protein could be a useful therapeutic approach to supply SMN protein to patients with SMA. EVs can naturally cross the BBB to efficiently deliver cargo to recipient cells in the CNS57,58,96. In vivo, systemically administered EVs can deliver cargo to cells of various tissues including the brain, heart, kidney, lung, and skeletal muscle58,97. Thus, SMN protein-loaded EVs would likely be able to replenish SMN protein levels in a wide variety of cell types in patients with SMA. However, due to the ~ 6-h half-life of SMN protein98,99, daily injection of SMN-loaded EVs would likely be required to ensure the treatment remained effective. There are a number of methods that could be used to prepare the large batches of EVs that would be required for such a therapy, such as tangential flow filtration (TFF) that can effectively purify EVs from large volumes of biofluid53,100,101. EVs have been shown to be safe in clinical trials for treatment of COVID-19-induced pneumonia and respiratory failure102,103,104, cancer105,106, and wound healing107. EVs have several other advantages as therapeutic platforms, such as their relatively stable shelf life108,109 and low immunogenicity when delivered to allogenic recipients110.
EVs loaded with SMN protein could also be useful as a transient or top-up therapy. Typically, there is a delay between initial diagnosis and initiation of treatment for patients with SMA, which is usually ~ 1–2 months for administration of onasemnogene abeparvovec, during which the individual may continue to decline due to disease progression2,111,112. SMN-loaded EVs could be used to supply SMN protein during this lag-time. EVs can cross the placental barrier113, suggesting administration of SMN-loaded EVs could be a potential therapeutic strategy to deliver supplemental SMN protein to a fetus identified as at-risk of severe SMA, to slow SMA pathology until alternative therapy can be administered post-birth. Supplemental SMN protein delivered in EVs could also benefit patients receiving nusinersen and/or risdiplam. Patients receiving these drugs can show varying responses, with some patients not gaining or maintaining motor milestones19,79,83,114,115. Supplemental SMN protein therapy could augment the therapeutic benefit of these drugs in these patients. In short, SMN-loaded EVs could provide an additional supply of SMN protein, potentially providing therapeutic benefit to a spectrum of patients with SMA.
All current therapeutics for SMA increase SMN protein levels in peripheral tissues, including liver and muscle116,117,118. For example, systemic administration of onasemnogene abeparvovec in human patients with SMA led to ~ 300 vector genomes per hepatocyte117, and high levels of SMN mRNA transcripts relative to GADPH in liver tissue, which would almost certainly be accompanied by significant increases in SMN protein expression in the liver. The liver readily releases EVs97 that can be found in blood119,120. It is intriguing to speculate that at least some of the therapeutic efficacy of these three approved treatments may be due to the production of SMN protein at sites other than the CNS, such as the liver, resulting in release of EVs containing the SMN protein, which can then be taken up by virtually all tissues in the body. Full-length SMN mRNA transcripts have also been detected within EVs isolated from the serum of patients with SMA treated with nusinersen, but not within EVs isolated from cerebral spinal fluid (CSF)121. These EVs could deliver the SMN mRNA to cells throughout the body, resulting in an increase in synthesis of full-length SMN protein in these cells in the nusinersen-treated patients. Since EVs readily cross the BBB58, our work suggests a new approach in which therapeutics do not necessarily need to be targeted directly to the CNS. Peripheral tissues, such as liver or muscle, could be harnessed as factories to produce therapeutic EVs that circulate and impact tissues throughout the body, including the CNS. This approach could be used for any disease to achieve wide-spread delivery of a therapeutic protein throughout the body.
Conclusion
We have shown that EVs can deliver SMN protein to recipient cells in tissue culture. This delivered SMN protein localized to the nucleus and interacted with normal cellular protein partners, indicating the delivered protein was able to perform in a manner similar to endogenous SMN protein. Our findings highlight a novel approach for delivery of SMN protein to cells, which could be harnessed to develop a new therapeutic strategy for treatment of SMA.
Materials and methods
Cell culture
A459 cells122 were obtained from the American Type Culture Collection (ATCC) (CCL-185, ATCC, Manassas, VA) and were grown in Minimum Essential Medium (MEM) (M2279, Sigma, Oakville, ON) supplemented with 10% (v/v) fetal bovine serum (FBS) (35–077-CV, Corning, Corning, NY), 2 mM GlutaMAX (35,050,061, Gibco, Grand Island, NY), and 1X antimycotic-antibiotic (15,240,062, Gibco). A549:HA-Gemin2 cells stably expressing an N-terminal HA-tagged Gemin2 protein were generated as follows. pRP3268 contains the cytomegalovirus (CMV) immediate early enhancer/promoter driving expression of a HA-tagged human GEMIN2 cDNA linked to a gene for hygromycin resistance through an internal ribosome entry site (IRES). A549 cells were transfected with pRP3268 using lipofectamine 2000 (Invitrogen, Carlsbad, CA), and pooled resistant cells were selected at 200 µg/mL hygromycin (Invitrogen). HepG2 cells67 (HB-8065, ATCC), were grown in Dulbecco’s Modified Eagle Medium (D5671, DMEM, Sigma) supplemented with 10% FBS (Gibco), 2 mM GlutaMAX (Gibco), and 1X antimycotic-antibiotic (Gibco). HepG2:3F-SMN cells stably expressing an N-terminal triple FLAG-tagged SMN protein were generated as follows. pLN103 contains the CMV immediate early enhancer/promoter driving expression of an N-terminal triple FLAG-tagged human SMN1 cDNA linked to a gene for hygromycin resistance through an IRES. HepG2 cells were transfected with pLN103 with Lipofectamine 2000 (Invitrogen), and pooled resistant cells were selected at 400 µg/mL hygromycin (Invitrogen). The human fibroblast cell line GM00232 was obtained from Coriell Institute for Medical Research (Camden, NJ). GM00232 was orginally collected from a 7-month old male diagnosed with SMA type 1 with a homozygous deletion of exons 7 and 8 of SMN1 and 2 copies of SMN2. Cells were maintained in MEM (Sigma) supplemented with 15% (v/v) FBS (Gibco), 2 mM GlutaMAX (Gibco), and 1X antimycotic-antibiotic (Gibco). All cells were incubated at 37˚C, 5% CO2 in a humidified chamber.
Viral infection
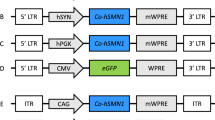
Ad3F-SMN is an adenovirus vector lacking early region 1 (E1) and E3 and possessing an expression cassette containing the CMV immediate early enhancer/promoter driving expression of a triple FLAG-tagged SMN1 cDNA. AdmCherry-SMN is adenovirus vector lacking E1 and E3 and possessing an expression cassette containing the CMV immediate early enhancer/promoter driving expression of an mCherry-tagged SMN1 cDNA. Ad3F-SMN and AdmCherry-SMN were grown, purified, and titered on 293 cells as previously described123.
HepG2 cells were infected with Ad3F-SMN or AdmCherry-SMN at the indicated multiplicity of infection (MOI) or mock infected with an equivalent volume of phosphate buffered saline (PBS) (D8537, Sigma) for 1 h at 37˚C, with rocking to redistribute the virus every 15 min. Cells were then washed three times with PBS to remove unattached virus. Cell lysates and conditioned medium (CM) were collected 72 hpi.
Isolation of extracellular vesicles (EVs)
EVs were isolated from CM to concentrate the particles for immunoblot analysis. Ten 150 mm dishes of HepG2 or HepG2:3F-SMN cells seeded at a density of 5 × 106 cells per dish were used for EV isolation. Seventy-two hours post-plating, CM was collected and EVs isolated by differential ultra-centrifugation, adapted from Théry et al124. The CM was centrifuged at 2,500xg for 15 min to pellet apoptotic bodies and cellular debris. The resulting supernatant was collected and subjected to ultra-centrifugation for 90 min at 120,000xg at 4˚C in a SW32 Ti rotor (Beckman Coulter, Mississauga, ON). The resulting pellets were resuspended in PBS (Sigma), pooled, and ultra-centrifuged at 120,000xg in a SW41 Ti rotor (Beckman Coulter) for 90 min at 4˚C. The resulting pellet was resuspended in 300μL of PBS and stored at -20˚C.
EVs were isolated from HepG2 cells infected with Ad3F-SMN using a polyethylene glycol (PEG)-based approach. HepG2 cells were plated in one 100 mm dish per treatment condition (4.4 × 106 cells per dish) and, next day, infected with Ad3F-SMN as described above. Seventy-two hpi, CM was collected and centrifuged at 2,500xg for 15 min, the resulting supernatant was collected and mixed 1:1 with 16% PEG (w/v) prepared in PBS (Sigma) and incubated at 4˚C overnight. Following incubation, the CM/PEG solution was centrifuged at 1,500xg for 30 min to pellet the EVs. The supernatant was discarded and the pellet was washed with 500 µL of PBS and centrifuged at 1,500xg for 5 min. The supernatant was discarded and the resulting pellet was washed with 500 µL PBS, then resuspended in 300 µL of PBS and stored at -20˚C.
Concentration and diameter of the EVs was determined by nanoparticle tracking analysis (NTA) using a NanoSight NS300 (Malvern Panalytical, Westborough, MA). NanoSight NTA 3.4 software was used to capture videos and analyze isolated particles. Samples were diluted in 0.1 µm filtered PBS immediately before analysis. For each sample, 2 independent analyses were conducted using a syringe pump, each capturing 60 s of video 3 times. Videos were captured using the following settings: syringe pump speed 50, focus 129, screen gain 2.2, camera level 14. Particles were analyzed using the following settings: screen gain 10, detection threshold 6.
Conditioned media (CM) treatments
For all media transfer experiments, the CM was subjected to low-speed centrifugation to remove cell debris and large EVs (e.g. apoptotic bodies) prior to application to the recipient cells, but was not concentrated or further processed. HepG2 cells were plated in 100 mm dishes (4.4 × 106 cells per dish) and, next day, infected with Ad3F-SMN or AdmCherry-SMN as described above at an MOI = 200. Seventy-two hpi, CM was collected and centrifuged at 2,500xg for 15 min to remove apoptotic bodies and cellular debris. CM was either used immediately or frozen at -80˚C until time of use. For frozen CM, the CM was thawed in a 37˚C water bath and centrifuged at 2,500xg for 15 min to pellet residual debris prior to application to the recipient cells.
For recipient cells that were to undergo immunofluorescent staining, cells were seeded at a density of 3 × 104 cells per well in 8-well chambered slides (80,841, Ibidi, Fitchburg, WI). The next day, medium was removed and the cells were pre-treated with 100 µM of 5,6-dichloro-1-β-D-ribofuranosylbenzimidazole (DRB) resuspended in dimethyl sulfoxide (DMSO) or vehicle control, both at a final DMSO concentration of 0.001% v/v for 1 h at 37˚C. Two hundred µL of CM per well was supplemented with 100 µM of DRB or vehicle, both at a final DMSO concentration of 0.001% v/v, and the cells were treated for 2 h at 37˚C.The cells were washed 3 times with PBS and prepared for immunofluorescence staining as detailed below. Parental A549 cells and fibroblasts derived from a patient with SMA underwent the same process without the addition of DRB.
Co-immunoprecipitation
Cells in 150 mm dishes were trypsinized and counted, and 5 × 106 cells were lysed in 500 µL of RIPA buffer (New England Biolabs). Lysates were cleared by centrifugation at 21,130xg for 10 min at 4˚C, and the supernatant transferred to a fresh tube. The cleared lysate was aliquoted into 4 tubes (100 µL/tube), and the volume adjusted to 400 µL with RIPA buffer (New England Biolabs). The remaining portion of cleared lysate was retained to use as the input sample during immunoblot analysis. Four µg of anti-FLAG (F1804, Sigma), mouse IgG isotype control (5415, Cell Signalling, Danvers, MA), anti-HA (ab236632, Abcam), or rabbit IgG isotype control (2729, Cell Signalling) was added to the diluted lysate and mixed by rotation at 4˚C overnight. Forty µL of Dynabeads protein G (10004D, Invitrogen) or Dynabeads protein A (10001D, Invitrogen) were washed in RIPA buffer, then added to each tube of lysate/antibody solution and incubated at 4˚C for 90 min. The bound and unbound fractions were separated using a magnetic tube rack. The bound fraction was washed 3 times with RIPA buffer and resuspended in 40 µL 2 × Laemmli buffer (62.5 mM Tris–HCl pH 6.8, 25% w/v glycerol, 5% v/v β-mercaptoethanol, 2% w/v sodium dodecyl sulphate (SDS), 0.01% w/v bromophenol blue).
Immunoblot
Cells and EVs were either lysed in passive lysis buffer (Promega) at the time of collection then mixed with an equal volume of 2 × Laemmli buffer or lysed directly in 2 × Laemmli buffer, and stored at − 20 °C. Cells cultured in 35 mm, 100 mm, and 150 mm dishes were collected in 200 μL, 500 μL, and 1000 μL final volume of buffer, respectively. Samples were boiled for 10 min prior to protein separation by sodium dodecyl sulphate–polyacrylamide gel electrophoresis (SDS-PAGE). Separated proteins were transferred to an Immobilon-P polyvinylidene difluoride (PVDF) membrane (Millipore, Burlington, MA). Membranes were blocked with Intercept (PBS) Blocking Buffer (927–70,001, LI-COR Biosciences, Nebraska) for 1 h at RT and probed with the following primary antibodies diluted in blocking buffer supplemented with 0.2% Tween 20: SMN (1:5000 1 h at room temperature (RT) for cell lysates, 1:1000 overnight at 4˚C for EVs; BD Transduction, Mississauga, ON), FLAG (1:5000 1 h at RT for cell lysates, 1:1000 overnight at 4˚C for EVs; F1804, Sigma), Tubulin (1:10,000 1 h at RT; ab59670, Abcam, Cambridge, UK or CP06, Millipore), Flotillin-2 (1:1000 overnight at 4˚C; C42A3, Cell Signaling Technologies, Danvers, MA), Gemin2 (1:5000 1 h at RT; ab7084, Abcam), ALIX (1:1000 overnight at 4˚C; ab186429, Abcam), CD29/Integrin beta-1 (1:1000 overnight at 4˚C; 04–1109, Millipore), HA (1:5000 overnight at 4˚C; ab236632, Abcam). Membranes were washed three times in PBS containing 0.1% Tween 20 (PBST), and incubated with the following fluorescently-labelled secondary antibodies in blocking buffer supplemented with 0.2% Tween 20 and 0.01% SDS: IRDye goat anti-mouse 680 (926–68,070, LI-COR), IRDye goat anti-mouse 800 (925–32,210), IRDye goat anti-rabbit 680 (925–68,071, LI-COR), IRDye goat anti-rabbit 800 (926–32,211, LI-COR). Membranes were developed using Odyssey CLx and visualized using LI-COR Image Studio 4.0 software.
Immunofluorescence staining and microscopy
Cells were fixed in 4% paraformaldehyde in PBS for 10 min at RT, washed 3 times with PBS, and permeabilized with 0.25% Triton X-100 (Sigma) in PBS for 10 min at RT. The cells were blocked in 10% donkey serum (S30, Millipore) in PBS for 30 min at RT, and then incubated in 10% donkey serum (Millipore) overnight at 4˚C with the following antibodies: SMN (1:250; BD Transduction), FLAG (1:250; F1804, Sigma), Tubulin (1:500; ab59670, Abcam), Gemin2 (1:250; ab7084, Abcam), HA (1:250, ab236632, Abcam). The cells were washed three times for 5 min with 1% donkey serum (Millipore) in PBS, then incubated with the following secondary antibodies in 10% donkey serum in PBS (Millipore) for 1 h at RT; Alexa Fluor donkey anti-rabbit 488 (1:1000; A21206, Invitrogen, Eugene, OR), Alexa Fluor donkey anti-rabbit 594 (1:1000; A21207, Invitrogen), Alexa Fluor donkey anti-mouse 488 (1:1000; A21202, Invitrogen) or Alexa Fluor donkey anti-mouse 594 (1:1000; A21203, Invitrogen). Following incubation with secondary antibody, the cells were stained with Hoechst 33342 at a concentration of 1 µg/mL (H3570, Life Technologies, Eugene, OR) in 1% donkey serum in PBS (Millipore) for 5 min at RT to visualize nuclei. The cells were washed three times for 5 min each with 1% donkey serum in PBS. Epifluorescence microscopy images were captured with a Zeiss Axio Imager M2 upright microscope, and processed using FIJI software125. Confocal images were captured with a Zeiss LSM 900 inverted confocal microscope, and processed using FIJI. Orthogonal projections were generated from 4–9 z-stacks captured every 1.0 µm using ZEN blue version 3.2 (Carl Zeiss Microscopy, Oberkochen, Germany). Fluorescence intensity in the images was quantified using CellProfiler126.
Nuclear gem quantification was conducted as follows: For the data included in Figs. 1 and 3, the number of nuclear gems per nucleus was counted in three independent fields of view each containing 50–80 cells, and converted to the number of nuclear gems per 100 nuclei for each field of view. Statistical significance was assessed using each independent fields of view as a separate replicate. For the data included in Fig. 5, three independent media transfer experiments were conducted. For each experiment, three images per treatment group were captured. The average number of gems per nucleus was quantified in each image, and the average of the three images, each containing 60–100 nuclei, was calculated to gather each independent replicate. The number of nuclear gems per nucleus was then converted to the number of nuclear gems per 100 nuclei. Statistical significance was assessed using each independent experiment as a separate replicate.
Statistical analysis
All statistical analyses were performed using Prism version 9.1.0, and the test performed is indicated in the figure legend. Parametric tests were chosen to evaluate statistical significance as the data is not ranked or ordinal, and is normally distributed. Data is presented as the mean ± standard deviation. Data in Figs. 4 and 5 was transformed by log transformation to analyze the data in different treatment groups on a similar scale. In all tests, one asterisk (*) indicates p < 0.05, two asterisk (**) indicates p < 0.01, three asterisk (***) indicates p < 0.001, and four asterisk (****) indicates p < 0.0001.
Data availability
The data that support the findings of this study are available on request.
References
Lefebvre, S. et al. Identification and characterization of a spinal muscular atrophy-determining gene. Cell 80, 155–165. https://doi.org/10.1016/0092-8674(95)90460-3 (1995).
Lefebvre, S. et al. Correlation between severity and SMN protein level in spinal muscular atrophy. Nat. Genet. 16, 265–269. https://doi.org/10.1038/ng0797-265 (1997).
Kolb, S. J. & Kissel, J. T. Spinal muscular atrophy. Neurol. Clin 33, 831–846. https://doi.org/10.1016/j.ncl.2015.07.004 (2015).
Kolb, S. J. et al. Natural history of infantile-onset spinal muscular atrophy. Ann. Neurol. 82, 883–891. https://doi.org/10.1002/ana.25101 (2017).
Finkel, R. S. et al. Observational study of spinal muscular atrophy type I and implications for clinical trials. Neurology 83, 810–817. https://doi.org/10.1212/WNL.0000000000000741 (2014).
Burns, J. K., Kothary, R. & Parks, R. J. Opening the window: The case for carrier and perinatal screening for spinal muscular atrophy. Neuromuscul. Disord. 26, 551–559. https://doi.org/10.1016/j.nmd.2016.06.459 (2016).
Bevan, A. K. et al. Early heart failure in the SMNDelta7 model of spinal muscular atrophy and correction by postnatal scAAV9-SMN delivery. Hum. Mol. Genet. 19, 3895–3905. https://doi.org/10.1093/hmg/ddq300 (2010).
Shababi, M. et al. Partial restoration of cardio-vascular defects in a rescued severe model of spinal muscular atrophy. J. Mol. Cell Cardiol. 52, 1074–1082. https://doi.org/10.1016/j.yjmcc.2012.01.005 (2012).
Szunyogova, E. et al. Survival Motor Neuron (SMN) protein is required for normal mouse liver development. Sci. Rep. 6, 34635. https://doi.org/10.1038/srep34635 (2016).
Deguise, M. O. et al. Abnormal fatty acid metabolism is a core component of spinal muscular atrophy. Ann. Clin. Transl. Neurol. 6, 1519–1532. https://doi.org/10.1002/acn3.50855 (2019).
Deguise, M. O. et al. Immune dysregulation may contribute to disease pathogenesis in spinal muscular atrophy mice. Hum. Mol. Genet. 26, 801–819. https://doi.org/10.1093/hmg/ddw434 (2017).
Bowerman, M. et al. Glucose metabolism and pancreatic defects in spinal muscular atrophy. Ann. Neurol. 72, 256–268. https://doi.org/10.1002/ana.23582 (2012).
Bowerman, M. et al. Defects in pancreatic development and glucose metabolism in SMN-depleted mice independent of canonical spinal muscular atrophy neuromuscular pathology. Hum. Mol. Genet. 23, 3432–3444. https://doi.org/10.1093/hmg/ddu052 (2014).
Gombash, S. E. et al. SMN deficiency disrupts gastrointestinal and enteric nervous system function in mice. Hum. Mol. Genet. 24, 5665. https://doi.org/10.1093/hmg/ddv292 (2015).
Thomson, A. K. et al. Survival of motor neurone protein is required for normal postnatal development of the spleen. J. Anat. 230, 337–346. https://doi.org/10.1111/joa.12546 (2017).
Chiriboga, C. A. et al. Results from a phase 1 study of nusinersen (ISIS-SMN(Rx)) in children with spinal muscular atrophy. Neurology 86, 890–897. https://doi.org/10.1212/WNL.0000000000002445 (2016).
Baranello, G. et al. Risdiplam in Type 1 spinal muscular atrophy. N. Engl. J. Med. 384, 915–923. https://doi.org/10.1056/NEJMoa2009965 (2021).
Mendell, J. R. et al. Single-dose gene-replacement therapy for spinal muscular atrophy. N. Engl. J. Med. 377, 1713–1722. https://doi.org/10.1056/NEJMoa170619810.1056/NEJMoa1706198 (2017).
Mercuri, E. et al. Nusinersen versus sham control in later-onset spinal muscular atrophy. N. Engl. J. Med. 378, 625–635. https://doi.org/10.1056/NEJMoa1710504 (2018).
René, C. A. & Parks, R. J. Expanding the availability of onasemnogene abeparvovec to older patients: The evolving treatment landscape for spinal muscular atrophy. Pharmaceutics https://doi.org/10.3390/pharmaceutics15061764 (2023).
Biogen. Spinraza prescribing information, <https://www.spinraza.com/content/dam/commercial/spinraza/caregiver/en_us/pdf/spinraza-prescribing-information.pdf> (2020)
Ratni, H. et al. Discovery of risdiplam, a selective Survival of Motor Neuron-2 ( SMN2) gene splicing modifier for the treatment of Spinal Muscular Atrophy (SMA). J. Med. Chem. 61, 6501–6517. https://doi.org/10.1021/acs.jmedchem.8b00741 (2018).
Chand, D. et al. Hepatotoxicity following administration of onasemnogene abeparvovec (AVXS-101) for the treatment of spinal muscular atrophy. J. Hepatol. 74, 560–566. https://doi.org/10.1016/j.jhep.2020.11.001 (2021).
Yazaki, K., Sakuma, S., Hikita, N., Fujimaru, R. & Hamazaki, T. Child neurology: pathologically confirmed thrombotic microangiopathy caused by onasemnogene abeparvovec treatment for SMA. Neurology 98, 808–813. https://doi.org/10.1212/WNL.0000000000200676 (2022).
Pagliardini, S. et al. Subcellular localization and axonal transport of the survival motor neuron (SMN) protein in the developing rat spinal cord. Hum. Mol. Genet. 9, 47–56. https://doi.org/10.1093/hmg/9.1.47 (2000).
Coovert, D. D. et al. The survival motor neuron protein in spinal muscular atrophy. Hum. Mol. Genet. 6, 1205–1214. https://doi.org/10.1093/hmg/6.8.1205 (1997).
Li, D. K., Tisdale, S., Lotti, F. & Pellizzoni, L. SMN control of RNP assembly: from post-transcriptional gene regulation to motor neuron disease. Semin. Cell Dev. Biol. 32, 22–29. https://doi.org/10.1016/j.semcdb.2014.04.026 (2014).
Lorson, C. L., Hahnen, E., Androphy, E. J. & Wirth, B. A single nucleotide in the SMN gene regulates splicing and is responsible for spinal muscular atrophy. Proc. Natl. Acad. Sci. U S A 96, 6307–6311. https://doi.org/10.1073/pnas.96.11.6307 (1999).
Liu, Q., Fischer, U., Wang, F. & Dreyfuss, G. The spinal muscular atrophy disease gene product, SMN, and its associated protein SIP1 are in a complex with spliceosomal snRNP proteins. Cell 90, 1013–1021. https://doi.org/10.1016/s0092-8674(00)80367-0 (1997).
Fischer, U., Liu, Q. & Dreyfuss, G. The SMN-SIP1 complex has an essential role in spliceosomal snRNP biogenesis. Cell 90, 1023–1029. https://doi.org/10.1016/s0092-8674(00)80368-2 (1997).
Battle, D. J., Kasim, M., Wang, J. & Dreyfuss, G. SMN-independent subunits of the SMN complex. Identification of a small nuclear ribonucleoprotein assembly intermediate. J. Biol. Chem. 282, 27953–27959. https://doi.org/10.1074/jbc.M702317200 (2007).
Carissimi, C., Saieva, L., Gabanella, F. & Pellizzoni, L. Gemin8 is required for the architecture and function of the survival motor neuron complex. J. Biol. Chem. 281, 37009–37016. https://doi.org/10.1074/jbc.M607505200 (2006).
Goulet, B. B., Kothary, R. & Parks, R. J. At the “junction” of spinal muscular atrophy pathogenesis: the role of neuromuscular junction dysfunction in SMA disease progression. Curr. Mol. Med. 13, 1160–1174. https://doi.org/10.2174/15665240113139990044 (2013).
Pellizzoni, L., Baccon, J., Charroux, B. & Dreyfuss, G. The survival of motor neurons (SMN) protein interacts with the snoRNP proteins fibrillarin and GAR1. Curr. Biol. 11, 1079–1088. https://doi.org/10.1016/s0960-9822(01)00316-5 (2001).
Renvoisé, B. et al. The loss of the snoRNP chaperone Nopp140 from Cajal bodies of patient fibroblasts correlates with the severity of spinal muscular atrophy. Hum. Mol. Genet. 18, 1181–1189. https://doi.org/10.1093/hmg/ddp009 (2009).
Bachand, F., Boisvert, F. M., Côté, J., Richard, S. & Autexier, C. The product of the survival of motor neuron (SMN) gene is a human telomerase-associated protein. Mol. Biol. Cell. 13, 3192–3202. https://doi.org/10.1091/mbc.e02-04-0216 (2002).
Poole, A. R. & Hebert, M. D. SMN and coilin negatively regulate dyskerin association with telomerase RNA. Biol. Open 5, 726–735. https://doi.org/10.1242/bio.018804 (2016).
Blackburn, E. H. & Collins, K. Telomerase: an RNP enzyme synthesizes DNA. Cold Spring Harb. Perspect. Biol. https://doi.org/10.1101/cshperspect.a003558 (2011).
Sanchez, G. et al. A novel function for the survival motoneuron protein as a translational regulator. Hum. Mol. Genet. 22, 668–684. https://doi.org/10.1093/hmg/dds474 (2013).
Chaytow, H., Huang, Y. T., Gillingwater, T. H. & Faller, K. M. E. The role of survival motor neuron protein (SMN) in protein homeostasis. Cell. & Mol. life sci. : CMLS 75, 3877–3894. https://doi.org/10.1007/s00018-018-2849-1 (2018).
Lauria, F. et al. SMN-primed ribosomes modulate the translation of transcripts related to spinal muscular atrophy. Nat. cell boil. 22, 1239–1251. https://doi.org/10.1038/s41556-020-00577-7 (2020).
Rossoll, W. et al. Smn, the spinal muscular atrophy-determining gene product, modulates axon growth and localization of beta-actin mRNA in growth cones of motoneurons. J. Cell Biol. 163, 801–812. https://doi.org/10.1083/jcb.200304128 (2003).
Ting, C. H. et al. The spinal muscular atrophy disease protein SMN is linked to the Golgi network. PLoS One 7, e51826. https://doi.org/10.1371/journal.pone.0051826 (2012).
Bowerman, M. et al. SMN, profilin IIa and plastin 3: a link between the deregulation of actin dynamics and SMA pathogenesis. Mol. Cell. Neurosci. 42, 66–74. https://doi.org/10.1016/j.mcn.2009.05.009 (2009).
Bowerman, M., Beauvais, A., Anderson, C. L. & Kothary, R. Rho-kinase inactivation prolongs survival of an intermediate SMA mouse model. Hum. Mol. Genet. 19, 1468–1478. https://doi.org/10.1093/hmg/ddq021 (2010).
Zhao, D. Y. et al. SMN and symmetric arginine dimethylation of RNA polymerase II C-terminal domain control termination. Nature 529, 48–53. https://doi.org/10.1038/nature16469 (2016).
Nash, L. A. et al. Survival Motor Neuron Protein is released from cells in exosomes: A potential biomarker for spinal muscular atrophy. Sci. Rep. 7, 13859. https://doi.org/10.1038/s41598-017-14313-z (2017).
Hurwitz, S. N. et al. Proteomic profiling of NCI-60 extracellular vesicles uncovers common protein cargo and cancer type-specific biomarkers. Oncotarget 7, 86999–87015. https://doi.org/10.18632/oncotarget.13569 (2016).
Skogberg, G. et al. Characterization of human thymic exosomes. PLoS One 8, e67554. https://doi.org/10.1371/journal.pone.0067554 (2013).
Xu, X. et al. Quantitative proteomic analysis of exosomes from umbilical cord mesenchymal stem cells and rat bone marrow stem cells. Proteomics 23, e2200204. https://doi.org/10.1002/pmic.202200204 (2023).
Benedikter, B. J. et al. Ultrafiltration combined with size exclusion chromatography efficiently isolates extracellular vesicles from cell culture media for compositional and functional studies. Sci. Rep. 7, 15297. https://doi.org/10.1038/s41598-017-15717-7 (2017).
Liang, B. et al. Characterization and proteomic analysis of ovarian cancer-derived exosomes. J. Proteom. 80, 171–182. https://doi.org/10.1016/j.jprot.2012.12.029 (2013).
Welsh, J. A. et al. Minimal information for studies of extracellular vesicles (MISEV2023): From basic to advanced approaches. J. Extracell. Vesicles 13, e12404. https://doi.org/10.1002/jev2.12404 (2024).
Mathivanan, S., Ji, H. & Simpson, R. J. Exosomes: extracellular organelles important in intercellular communication. J. Proteom. 73, 1907–1920. https://doi.org/10.1016/j.jprot.2010.06.006 (2010).
Wiklander, O. P. et al. Extracellular vesicle in vivo biodistribution is determined by cell source, route of administration and targeting. J. Extracell. Vesicles 4, 26316. https://doi.org/10.3402/jev.v4.26316 (2015).
Wiklander, O. P. B., Brennan, M., Lötvall, J., Breakefield, X. O. & El Andaloussi, S. Advances in therapeutic applications of extracellular vesicles. Sci. Transl. Med. https://doi.org/10.1126/scitranslmed.aav8521 (2019).
Morad, G. et al. Tumor-Derived Extracellular Vesicles Breach the Intact Blood-Brain Barrier. ACS Nano. 13, 13853–13865. https://doi.org/10.1021/acsnano.9b04397 (2019).
Driedonks, T. et al. Pharmacokinetics and biodistribution of extracellular vesicles administered intravenously and intranasally to. J. Extracell. Biol. https://doi.org/10.1002/jex2.59 (2022).
René, C. A. & Parks, R. J. Delivery of therapeutic agents to the central nervous system and the promise of extracellular vesicles. Pharmaceutics https://doi.org/10.3390/pharmaceutics13040492 (2021).
René, C. A. & Parks, R. J. Bioengineering extracellular vesicle cargo for optimal therapeutic efficiency. Mol. Ther. Methods Clin. Dev. 32, 101259. https://doi.org/10.1016/j.omtm.2024.101259 (2024).
Haney, M. J. et al. Exosomes as drug delivery vehicles for Parkinson’s disease therapy. J. Control. Release 207, 18–30. https://doi.org/10.1016/j.jconrel.2015.03.033 (2015).
Izadpanah, M. et al. Extracellular vesicles as a neprilysin delivery system memory Improvement in alzheimer’s disease. Iran J. Pharm. Res. 19, 45–60. https://doi.org/10.22037/ijpr.2020.112062.13508 (2020).
Goulet, B. B., McFall, E. R., Wong, C. M., Kothary, R. & Parks, R. J. Supraphysiological expression of survival motor neuron protein from an adenovirus vector does not adversely affect cell function. Biochem. Cell Biol. 91, 252–264. https://doi.org/10.1139/bcb-2012-0094 (2013).
Aoto, K., Takabayashi, S., Mutoh, H. & Saitsu, H. Generation of Flag/DYKDDDDK epitope tag knock-in mice using. Int. J. Mol. Sci. https://doi.org/10.3390/ijms231911915 (2022).
Babaylova, E. S. et al. mRNA regions where 80S ribosomes pause during translation elongation in vivo interact with protein uS19, a component of the decoding site. Nucleic Acids Res. 48, 912–923. https://doi.org/10.1093/nar/gkz1145 (2020).
DiDonato, C. J., Parks, R. J. & Kothary, R. Development of a gene therapy strategy for the restoration of survival motor neuron protein expression: implications for spinal muscular atrophy therapy. Hum. Gene. Ther. 14, 179–188. https://doi.org/10.1089/104303403321070874 (2003).
Knowles, B. B., Howe, C. C. & Aden, D. P. Human hepatocellular carcinoma cell lines secrete the major plasma proteins and hepatitis B surface antigen. Science 209, 497–499. https://doi.org/10.1126/science.6248960 (1980).
Bochkov, Y. A. & Palmenberg, A. C. Translational efficiency of EMCV IRES in bicistronic vectors is dependent upon IRES sequence and gene location. Biotechniques 41, 283–284. https://doi.org/10.2144/000112243 (2006).
Feng, W. et al. Gemins modulate the expression and activity of the SMN complex. Hum. Mol. Genet. 14, 1605–1611. https://doi.org/10.1093/hmg/ddi168 (2005).
Carissimi, C. et al. Gemin8 is a novel component of the survival motor neuron complex and functions in small nuclear ribonucleoprotein assembly. J. Biol. Chem. 281, 8126–8134. https://doi.org/10.1074/jbc.M512243200 (2006).
Meier, I. D., Walker, M. P. & Matera, A. G. Gemin4 is an essential gene in mice, and its overexpression in human cells causes relocalization of the SMN complex to the nucleoplasm. Biol. Open https://doi.org/10.1242/bio.032409 (2018).
Ross, P. J. On the role of chromatin in the regulation of adenovirus vector transgene expression Doctorate of Philosophy thesis University of Ottawa (2009).
Glenn, G. M. & Ricciardi, R. P. Detailed kinetics of adenovirus type-5 steady-state transcripts during early infection. Virus Res. 9, 73–91. https://doi.org/10.1016/0168-1702(88)90051-2 (1988).
Yamaguchi, Y., Wada, T. & Handa, H. Interplay between positive and negative elongation factors: drawing a new view of DRB. Genes Cells 3, 9–15. https://doi.org/10.1046/j.1365-2443.1998.00162.x (1998).
Giberson, A. N. et al. Human adenoviral DNA association with nucleosomes containing histone variant H3.3 during the early phase of infection is not dependent on viral transcription or replication. Biochem. Cell Biol. 96, 797–807. https://doi.org/10.1139/bcb-2018-0117 (2018).
Ross, P. J. et al. Assembly of helper-dependent adenovirus DNA into chromatin promotes efficient gene expression. J. Virol. 85, 3950–3958. https://doi.org/10.1128/JVI.01787-10 (2011).
Yeo, C. J. J. & Darras, B. T. Overturning the paradigm of spinal muscular atrophy as just a motor neuron disease. Pediatr. Neurol. 109, 12–19. https://doi.org/10.1016/j.pediatrneurol.2020.01.003 (2020).
Nash, L. A., Burns, J. K., Chardon, J. W., Kothary, R. & Parks, R. J. Spinal muscular atrophy: More than a disease of motor neurons?. Curr. Mol. Med. 16, 779–792. https://doi.org/10.2174/1566524016666161128113338 (2016).
Finkel, R. S. et al. Nusinersen versus Sham control in infantile-onset spinal muscular atrophy. N. Engl. J. Med. 377, 1723–1732. https://doi.org/10.1056/NEJMoa1702752 (2017).
Passini, M. A. et al. Antisense oligonucleotides delivered to the mouse CNS ameliorate symptoms of severe spinal muscular atrophy. Sci. Transl. Med. https://doi.org/10.1126/scitranslmed.3001777 (2011).
Günther, R. et al. Long-term efficacy and safety of nusinersen in adults with 5q spinal muscular atrophy: a prospective European multinational observational study. Lancet Reg. Health Eur. 39, 100862. https://doi.org/10.1016/j.lanepe.2024.100862 (2024).
Cordts, I. et al. Intrathecal nusinersen administration in adult spinal muscular atrophy patients with complex spinal anatomy. Ther. Adv. Neurol. Disord. 13, 1756286419887616. https://doi.org/10.1177/1756286419887616 (2020).
Mercuri, E. et al. Risdiplam in types 2 and 3 spinal muscular atrophy: A randomised, placebo-controlled, dose-finding trial followed by 24 months of treatment. Eur. J. Neurol. 00, 1–12. https://doi.org/10.1111/ene.15499 (2022).
Day, J. W. et al. Onasemnogene abeparvovec gene therapy for symptomatic infantile-onset spinal muscular atrophy in patients with two copies of SMN2 (STR1VE): an open-label, single-arm, multicentre, phase 3 trial. Lancet Neurol. 20(4), 284–293. https://doi.org/10.1016/s1474-4422(21)00001-6 (2021).
Mendell, J. R. et al. Five-Year Extension Results of the Phase 1 START Trial of Onasemnogene Abeparvovec in Spinal Muscular Atrophy. JAMA Neurol. 78, 834–841. https://doi.org/10.1001/jamaneurol.2021.1272 (2021).
Mercuri, E. et al. Onasemnogene abeparvovec gene therapy for symptomatic infantile-onset spinal muscular atrophy type 1 (STR1VE-EU): an open-label, single-arm, multicentre, phase 3 trial. Lancet Neurol. 20, 832–841. https://doi.org/10.1016/S1474-4422(21)00251-9 (2021).
Strauss, K. A. et al. Onasemnogene abeparvovec for presymptomatic infants with two copies of SMN2 at risk for spinal muscular atrophy type 1: the Phase III SPR1NT trial. Nat. Med. 28, 1381–1389. https://doi.org/10.1038/s41591-022-01866-4 (2022).
Strauss, K. A. et al. Onasemnogene abeparvovec for presymptomatic infants with three copies of SMN2 at risk for spinal muscular atrophy: the Phase III SPR1NT trial. Nat. Med. 28, 1390–1397. https://doi.org/10.1038/s41591-022-01867-3 (2022).
Novartis. Novartis to initiate SMART Phase 3b global study of Zolgensma in children up to 21 kg, building on real-world experience <https://www.novartis.com/news/media-releases/novartis-initiate-smart-phase-3b-global-study-zolgensma-children-21-kg-building-real-world-experience> (2021)
Gaillard, J., Gu, A. R. & Neil Knierbein, E. E. Necrotizing enterocolitis following onasemnogene abeparvovec for spinal muscular atrophy: A case series. J. Pediatr. 260, 113493. https://doi.org/10.1016/j.jpeds.2023.113493 (2023).
Silverman, E. Novartis reports two children died from acute liver failure after treatment with Zolgensma gene therapy <https://www.statnews.com/pharmalot/2022/08/11/novartis-zolgensma-liver-failure-gene-therapy-death/> (2022)
Novartis. Zolgensma acute liver failure update <https://www.novartis.com/news/zolgensma-acute-liver-failure-update> (2022).
Francis, J. W. et al. A survival motor neuron:tetanus toxin fragment C fusion protein for the targeted delivery of SMN protein to neurons. Brain Res. 995, 84–96. https://doi.org/10.1016/j.brainres.2003.09.063 (2004).
Anderton, R. S., Meloni, B. P., Mastaglia, F. L. & Boulos, S. Investigation of a recombinant SMN protein delivery system to treat spinal muscular atrophy. Transl. Neurosci. 5, 8–16 (2014).
Pham, T. T. et al. Endosomal escape of nucleic acids from extracellular vesicles mediates functional therapeutic delivery. Pharmacol. Res. 188, 106665. https://doi.org/10.1016/j.phrs.2023.106665 (2023).
Chen, C. C. et al. Elucidation of exosome migration across the blood-brain barrier model in vitro. Cell Mol. Bioeng. 9, 509–529. https://doi.org/10.1007/s12195-016-0458-3 (2016).
Miotto, P. M. et al. Liver-derived extracellular vesicles improve whole-body glycaemic control via inter-organ communication. Nat. Metab. 6, 254–272. https://doi.org/10.1038/s42255-023-00971-z (2024).
Burnett, B. G. et al. Regulation of SMN protein stability. Mol. Cell. Biol. 29, 1107–1115. https://doi.org/10.1128/MCB.01262-08 (2009).
Han, K. J. et al. Ubiquitin-specific protease 9x deubiquitinates and stabilizes the spinal muscular atrophy protein-survival motor neuron. J. Biol. Chem. 287, 43741–43752. https://doi.org/10.1074/jbc.M112.372318 (2012).
Lorenzini, B. et al. Producing vesicle-free cell culture additive for human cells extracellular vesicles manufacturing. J. Control. Release 355, 501–514. https://doi.org/10.1016/j.jconrel.2023.01.073 (2023).
Andriolo, G. et al. methodologies for scalable production of high-quality purified small extracellular vesicles from conditioned medium. Methods Mol. Biol. 2668, 69–98. https://doi.org/10.1007/978-1-0716-3203-1_7 (2023).
Lightner, A. L. et al. Bone marrow mesenchymal stem cell-derived extracellular vesicle infusion for the treatment of respiratory failure from COVID-19: A randomized. Placebo-Control. Dosing Clin. Trial. Chest https://doi.org/10.1016/j.chest.2023.06.024 (2023).
Chu, M. et al. Nebulization Therapy with Umbilical Cord Mesenchymal Stem Cell-Derived Exosomes for COVID-19 Pneumonia. Stem Cell Rev. Rep. 18, 2152–2163. https://doi.org/10.1007/s12015-022-10398-w (2022).
Zhu, Y. G. et al. Nebulized exosomes derived from allogenic adipose tissue mesenchymal stromal cells in patients with severe COVID-19: a pilot study. Stem Cell Res. Ther. 13, 220. https://doi.org/10.1186/s13287-022-02900-5 (2022).
Guo, M. et al. Autologous tumor cell-derived microparticle-based targeted chemotherapy in lung cancer patients with malignant pleural effusion. Sci. Transl. Med. https://doi.org/10.1126/scitranslmed.aat5690 (2019).
Kim, M. S. et al. Development of exosome-encapsulated paclitaxel to overcome MDR in cancer cells. Nanomedicine 12, 655–664. https://doi.org/10.1016/j.nano.2015.10.012 (2016).
Johnson, J. et al. First-in-human clinical trial of allogeneic, platelet-derived extracellular vesicles as a potential therapeutic for delayed wound healing. J. Extracell. Vesicles 12, e12332. https://doi.org/10.1002/jev2.12332 (2023).
Wu, J. Y., Li, Y. J., Hu, X. B., Huang, S. & Xiang, D. X. Preservation of small extracellular vesicles for functional analysis and therapeutic applications: a comparative evaluation of storage conditions. Drug Deliv. 28, 162–170. https://doi.org/10.1080/10717544.2020.1869866 (2021).
Görgens, A. et al. Identification of storage conditions stabilizing extracellular vesicles preparations. J. Extracell. Vesicles 11, e12238. https://doi.org/10.1002/jev2.12238 (2022).
Zhu, X. et al. Comprehensive toxicity and immunogenicity studies reveal minimal effects in mice following sustained dosing of extracellular vesicles derived from HEK293T cells. J. Extracell. Vesicles 6, 1324730. https://doi.org/10.1080/20013078.2017.1324730 (2017).
Servais, L. et al. Real-world outcomes in patients with spinal muscular atrophy treated with onasemnogene abeparvovec monotherapy: findings from the RESTORE registry. J. Neuromuscul. Dis. 11, 425–442. https://doi.org/10.3233/JND-230122 (2024).
Gallotta, I. et al. Neuron-specific knock-down of SMN1 causes neuron degeneration and death through an apoptotic mechanism. Hum. Mol. Genet. 25, 2564–2577. https://doi.org/10.1093/hmg/ddw119 (2016).
Sheller-Miller, S., Choi, K., Choi, C. & Menon, R. Cyclic-recombinase-reporter mouse model to determine exosome communication and function during pregnancy. Am. J. Obstet. Gynecol. 221(502), e501-502.e512. https://doi.org/10.1016/j.ajog.2019.06.010 (2019).
Hagenacker, T. et al. Nusinersen in adults with 5q spinal muscular atrophy: a non-interventional, multicentre, observational cohort study. Lancet Neurol. 19, 317–325. https://doi.org/10.1016/S1474-4422(20)30037-5 (2020).
Darras, B. T. et al. Risdiplam-treated infants with type 1 spinal muscular atrophy versus historical controls. N. Engl. J. Med. 385, 427–435. https://doi.org/10.1056/NEJMoa2102047 (2021).
Poirier, A. et al. Risdiplam distributes and increases SMN protein in both the central nervous system and peripheral organs. Pharmacol. Res. Perspect 6, e00447. https://doi.org/10.1002/prp2.447 (2018).
Thomsen, G. et al. Biodistribution of onasemnogene abeparvovec DNA, mRNA and SMN protein in human tissue. Nat. Med. 27, 1701–1711. https://doi.org/10.1038/s41591-021-01483-7 (2021).
Finkel, R. S. et al. Treatment of infantile-onset spinal muscular atrophy with nusinersen: a phase 2, open-label, dose-escalation study. Lancet 388, 3017–3026. https://doi.org/10.1016/S0140-6736(16)31408-8 (2016).
Povero, D. et al. Circulating extracellular vesicles with specific proteome and liver microRNAs are potential biomarkers for liver injury in experimental fatty liver disease. PLoS One 9, e113651. https://doi.org/10.1371/journal.pone.0113651 (2014).
Achour, B. et al. liquid biopsy enables quantification of the abundance and interindividual variability of hepatic enzymes and transporters. Clin. Pharmacol. Ther. 109, 222–232. https://doi.org/10.1002/cpt.2102 (2021).
Trifunov, S. et al. Full-length SMN transcript in extracellular vesicles as biomarker in individuals with spinal muscular atrophy type 2 treated with nusinersen. J. Neuromuscul. Dis. 10, 653–665. https://doi.org/10.3233/JND-230012 (2023).
Giard, D. J. et al. In vitro cultivation of human tumors: establishment of cell lines derived from a series of solid tumors. J. Natl. Cancer Inst. 51, 1417–1423. https://doi.org/10.1093/jnci/51.5.1417 (1973).
Ross, P. J. & Parks, R. J. Construction and characterization of adenovirus vectors. Cold Spring Harb. Protoc. https://doi.org/10.1101/pdb.prot5011 (2009).
Théry, C., Amigorena, S., Raposo, G. & Clayton, A. Isolation and characterization of exosomes from cell culture supernatants and biological fluids. Curr. Protoc. Cell Biol. https://doi.org/10.1002/0471143030.cb0322s30 (2006).
Schindelin, J. et al. Fiji: an open-source platform for biological-image analysis. Nat. Methods 9, 676–682. https://doi.org/10.1038/nmeth.2019 (2012).
Stirling, D. R. et al. Cell Profiler 4: improvements in speed, utility and usability. BMC Bioinform. 22, 433. https://doi.org/10.1186/s12859-021-04344-9 (2021).
Acknowledgements
The authors are grateful to Kathy Poulin for excellent technical assistance, and to Drs. Rashmi Kothary (Ottawa Hospital Research Institute) and Dylan Burger (Ottawa Hospital Research Institute) for valuable discussion. pLN107, the plasmid used to generate Ad3F-SMN, was constructed by Leslie Nash as a graduate student in the Parks Lab. This work was supported by a collaborative grant from the Canadian Institutes of Health Research (CIHR, PJT-178120) to R.J.P. and Drs. Rashmi Kothary (OHRI), Panayiotis O. Vacratsis (University of Windsor) and Jodi Warman-Chardon (The Ottawa Hospital), and additional research funds to R.J.P. from CIHR (NHG-107767, MOP-136898, PYY-175428) and Cure SMA/Cure SMA Canada. C.A.R. was supported by a Queen Elizabeth II Graduate Scholarship in Science and Technology from the Ontario Provincial Government (Canada).
Author information
Authors and Affiliations
Contributions
Conceptualization: C.A.R., R.J.P.; Formal Analysis: C.A.R., R.J.P.; Funding acquisition: C.A.R., R.J.P.; Investigation: C.A.R.; Methodology: C.A.R., R.J.P.; Project administration: R.J.P.; Supervision: R.J.P.; Visualization: C.A.R., R.J.P.; Writing – original draft: C.A.R.; Writing – review & editing: C.A.R., R.J.P. All authors have read and agreed to the published version of the manuscript
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
René, C.A., Parks, R.J. Extracellular vesicles efficiently deliver survival motor neuron protein to cells in culture. Sci Rep 15, 5674 (2025). https://doi.org/10.1038/s41598-025-90083-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-90083-3