Abstract
Inflammatory Bowel Disease (IBD), Crohn's disease (CD) and ulcerative colitis (UC), requires a combination of procedures and tests in diagnosis and discrimination. This study aimed to delineate specific serum metabolomic biomarkers that diagnose IBD and differentiate IBD subgroups. Serum samples and clinical metadata of the participants, IBD patients and Normal Controls (NC), were collected. Untargeted and targeted metabolomic analyses by high-resolution mass spectrometry and multivariate statistical approaches were applied. Further, Receiver Operating Characteristic (ROC) curves, pathways, and network analyses were conducted. Distinct clustering separated IBD patients from the NC, although the CD and UC subgroups overlapped in the non-targeted profiling. Targeted metabolomics revealed elevated tryptophan and indole-3-acetic acid levels and reduced primary-to-secondary bile acid ratios in both CD and UC patients. The differences in specific tryptophan metabolites between CD and UC were identified. The ROC analysis underscored the discriminatory power of the biomarkers (AUC values: NC vs. CD = 0.9738; NC vs. UC = 0.9887; UC vs. CD = 0.7140). Pathway analysis revealed alterations in glycerolipid metabolism, markedly differentiating UC from CD. Network analysis correlated metabolomic markers with the clinical phenotypes of IBD. Serum metabolomic biomarkers can precisely identify IBD, discriminate IBD subtypes, and further reveal the phenotypes of IBD.
Similar content being viewed by others
Introduction
Inflammatory Bowel Disease (IBD), which includes Crohn’s disease (CD) and Ulcerative Colitis (UC), is a chronic inflammatory condition of the gastrointestinal (GI) tract characterized by pathological responses of both the innate and acquired immune systems. Once thought to be confined primarily to Western countries, IBD has witnessed a marked increase in its incidence in newly industrialized nations over the last two decades, challenging previous geographic assumptions and highlighting the growing global health burden of IBD. This trend not only strains healthcare systems, but it also highlights the calls for urgent re-evaluation of diagnostic and management strategies in order to accommodate the growing diversity of IBD patients worldwide1.
The etiology of IBD is multifactorial and involves a complex interplay between genetic predispositions, microbial interactions within the gut microbiome, immunological responses, environmental exposure, and dietary factors. This complexity not only obscures the full understanding of IBD pathogenesis despite extensive research efforts2,3, but also complicates the clinical management of IBD, affecting patient outcomes and treatment efficacy. In clinical practice, the diagnosis of IBD poses a significant challenge, primarily because of the heterogeneity of its symptoms and overlap with other GI disorders, compounded by the difficulty in distinguishing between the IBD subtypes CD and UC, which is critical for tailoring treatment strategies. The absence of definitive biomarkers necessitates a comprehensive diagnostic framework, integrating clinical assessments with diagnostic modalities such as endoscopy, histology, fecal markers, and imaging4,5. However, despite these efforts, the nuanced nature of these conditions often results in diagnostic uncertainty, underscoring the urgent need for novel biomarkers that can enhance diagnostic accuracy and optimize patient care.
Metabolomics, the comprehensive analysis of small molecules in biological specimens, offers unique advantages for biomarker discovery in IBD6. Serum/plasma metabolomics, by providing a systemic overview of the metabolic status, captures not only the gut-derived metabolites but this method also reflects broader metabolic changes, offering insights into the systemic nature of the disease. This minimally invasive and patient-friendly method, characterized by well-standardized procedures across laboratories, not only facilitates easier sample collection from patients but also minimizes discomfort, making it particularly advantageous for longitudinal studies and routine monitoring.
Previous investigations of IBD using serum or plasma samples have revealed disparities in the metabolite profiles between afflicted individuals and healthy controls7. Studies focusing on specific metabolic pathways, such as bile acid8,9 and tryptophan pathways10, have been pivotal because of their association with disease activity and outcomes. Tryptophan (TRP), an indispensable amino acid, has been noted for its diminished levels in IBD patients. By considering the three major metabolic pathways of TRP within the immune and epithelial cells of the intestine, contemporary research has shed light on the relevance of TRP and its metabolites in the pathogenesis of IBD11,12,13. Similarly, bile acids play a crucial role in intestinal immune system dysregulation and gut homeostasis14, and previous studies have correlated changes in bile acid composition with IBD pathogenesis and disease activity15. However, a systematic review highlights a major limitation of prior research: small sample sizes, particularly in studies utilizing serum and plasma, often limit the statistical significance and generalizability16.
In addressing identified research gaps, our study was conducted with a substantial cohort, incorporating in-depth disease characteristics to establish a foundation for novel biomarker discovery in IBD diagnosis and classification. We utilized comprehensive metabolite profiling, concentrating on crucial pathways such as bile acids and tryptophan metabolites, to differentiate IBD patients from healthy controls. Our objectives encompassed identifying specific serum biomarkers for IBD subtype differentiation and assessing metabolites for their potential value in predicting disease phenotypes.
Methods
Study design and sample collection
The study cohort comprised of patients diagnosed with IBD and normal controls (NC). Patients with IBD were recruited from the IBD center of Kyung Hee University Hospital (Seoul, Republic of Korea) between May 2018 and September 2022. NC who were asymptomatic and free from major medical diseases, including gastrointestinal disorders, and without a family or personal history of IBD, were recruited during the same period. Additional screening, including routine blood tests and a medical history questionnaire, was performed to ensure the health status of the controls. This study was approved by the Institutional Review Board of Kyung Hee University Hospital (Approval No. IRB-2018-03-006) and carried out in accordance with relevant guidelines and regulations. Also, informed consent was obtained from all participants.
For the patient group, the inclusion criteria were patients newly diagnosed (less than 4 weeks before study enrollment) with IBD and also those with an established diagnosis who had undergone medical treatment prior to enrollment. The diagnosis of IBD was confirmed through a comprehensive approach, including clinical assessment, biochemical tests, stool examinations, endoscopic findings, and imaging methods4,17 aligned with the latest clinical guidelines. The exclusion criteria included indeterminate colitis, other significant comorbidities, or an inability to provide informed consent. Serum samples from IBD patients were collected at study enrollment using standardized phlebotomy procedures and processed within 2 h of collection through centrifugation at 4 °C, followed by aliquoting and storage at −80 °C for further analysis. Along with serum samples, detailed data on disease characteristics such as disease behavior and treatment history were systematically recorded. The assessment of disease activity is a critical component and it was conducted meticulously through biochemical tests. Specifically, the biological disease activity was determined using objective biomarkers, including serum C-reactive protein (CRP) and fecal calprotectin. Biological remission was defined as a CRP level less than 0.5 mg/dL and a fecal calprotectin level less than 250 μg/g. Conversely, active disease was identified by a CRP level of 0.5 mg/dL or greater, or fecal calprotectin level of 250 μg/g or higher.
Metabolic workflow and data analysis
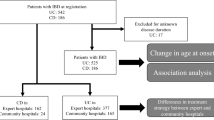
The metabolic workflow of this study, depicted in Fig. 1, entailed the detailed identification and quantification of 78 distinct metabolites in serum samples from 346 participants using high-resolution mass spectrometry techniques. These analyses employed gas chromatography-time-of-flight mass spectrometry (GC-TOF-MS) and liquid chromatography-triple-quadrupole (LC-TQ) MS, which are well-known for their precision and sensitivity in metabolite profiling. Data analysis was strategically oriented towards understanding the variations in metabolomic profiles in relation to IBD subtypes and pertinent clinical variables, as outlined in Table 1. The critical components of our workflow are summarized below, and further details are provided in the Supplementary Data.
Schematic overview of the comprehensive workflow and key methodological steps. This schematic delineates the methodological framework and sequential processes employed in our study. It begins with (1) sample preparation, including sample collection and extraction, followed by (2.1) untargeted metabolite profiling through GC-TOF-MS analysis, and (2.2) targeted metabolite analysis via LC-TO-MS, focusing on bile acids and tryptophan-related metabolites. The subsequent stage (3) encompasses data processing, featuring peak alignment, multivariate statistical analysis, and metabolite identification. Feature selection (4.1) was conducted using the Boruta algorithm, which includes shadow feature creation, random forest modeling, and interative confirmation of important features. Parallelly, (4.2) pathway analysis was performed using MetaboAnalyst 5.0, involving data normalization and auto-scaling for metabolic pathway elucidation. The final stage (5) data interpretation synthesizes the results into ROC curves, PCA/PLS-DA score plots, and pathway analyses, providing a comprehensive understanding of the metabolomic landscape in IBD.
Sample preparation
Serum samples (100 µL) were extracted with an extraction solution (400 µL) in 2 mL microcentrifuge tubes. The choice of solvent—50% methanol for untargeted metabolite profiling and bile acid analysis and 100% methanol for tryptophan metabolite analysis—was guided by their efficacy in extracting a wide range of metabolites while preserving stability. After extraction, the resulting supernatant was filtered and used for bile acid and tryptophan metabolite analyses. For untargeted metabolite profiling, all of the samples were dried using a speed vacuum concentrator and derivatized to enhance the volatility and thermal stability of the compounds for GC-TOF-MS analysis.
Data processing
The raw GC-TOF-MS data were converted to CDF (NetCDF) files using LECO Chroma TOF software (version 5.40, LECO Corp.). After conversion, the MetAlign software package (http://www.metalign.nl) was used for peak detection, retention-time correction, and alignment analysis. Multivariate statistical analysis was performed using the SIMCA P+ software (version 16.0; Umetrics, Umea, Sweden). The LC-TQ-MS data were ionized by electrospray ionization in the negative ion mode and detected in the multiple reaction monitoring (MRM) mode.
Statistical/bioinformatic analyses
We opted for nonparametric tests, specifically the Wilcoxon signed-rank test, because of their robustness in analyzing non-normally distributed data, which is common in metabolomics studies. Furthermore, adjusted p-values for all identified metabolites were calculated using the False Discovery Rate (FDR) method to account for multiple comparisons and ensure the robustness of our statistical findings. Receiver Operating Characteristic (ROC) curves and accuracy measures with 95% confidence intervals (CIs) were calculated using R version 4.3.1. to provide a statistical measure of the diagnostic power of the biomarkers. Additionally, to select biomarkers associated with the subtypes and phenotypes of IBD, we employed Boruta (version 8.0.0 in R), a novel random forest-based feature selection technique within machine learning. Metabolic pathway analysis was performed using functional enrichment and the pathway analysis tool of the free web-based software MetaboAnalyst 5.0, which facilitates the identification of perturbed metabolic pathways in IBD.
Results
Characteristics of the participants
In this study, 346 subjects were analyzed, including 88 healthy volunteers (normal controls, NC) and 258 patients with IBD (134 with CD and 124 with UC). The basic characteristics of the participants are summarized in Table 1. The gender distribution was approximately 78% men in the CD group, 62% in the UC group, and 70% in the NC group. Mean ages were 49.5 years for CD, 42.7 years for UC, and 33.6 years for NC, with mean BMIs of 22.8 kg/ kg/m2 for CD, 22.9 kg/m2 for UC, and 23.5 kg/m2 for NC, respectively. In this study, there were no significant differences in age or sex between the IBD patient group and the NC group. However, the BMI of the IBD patients was significantly lower compared to the NC group. This finding aligns with previous observations that IBD patients often exhibit reduced BMI due to factors such as chronic inflammation, malabsorption, and altered nutritional intake18. Such differences are well-documented in the context of IBD pathophysiology and its impact on overall nutritional status.
Patients with CD were predominantly diagnosed between 16 and 40 years of age (73.1%), while 37.1% of patients with UC received diagnosed after the age of 40 years. The median disease duration was 6 years for CD (range: 0–27 years) and 1 year for UC (range: 0–25 years). The distribution of disease activity was similar between the CD and UC groups, with an equitable distribution among patients with IBD. Approximately half of the patients in each group were classified as having active disease, whereas the other half were in clinical remission. A substantial majority of participants had received treatment, with 94% in the CD group and 87% in the UC group having undergone some form of therapy. The proportion of the treatment-naïve patients was 6% and 13% in the CD and UC groups, respectively.
Comparative metabolic profiling in IBD
In this study, we have conducted a comprehensive analysis of the serum metabolite levels in patients diagnosed with CD, UC, and NC using both targeted and untargeted metabolite profiling strategies. Untargeted metabolite profiling facilitated by GC-TOF-MS analysis revealed distinct clustering of the NC group along principal component 1 (PC1). However, a discernible separation among the UC and CD groups was not evident in Principal Component Analysis (PCA) and Partial Least Squares Discriminant Analysis (PLS-DA) score plots (Fig. 2A and B). The analysis identified 43 metabolites, of which the significantly discriminant metabolites between the experimental groups were selected based on the variable importance in projection (VIP) value (> 0.7) from the PLS-DA model and a p-value (< 0.05) from the one-way ANOVA (Table S1). Normalization of the relative levels of significantly altered metabolites to the NC values, followed by their visualization using a heatmap (Fig. 2C), revealed decreased levels of various amino acids, organic acids, carbohydrates, and fatty acids in the patient groups. Conversely, levels of alanine, proline, ribose, fructose, pelargonic acid, lactic acid, 4-hydroxyphenylacetic acid, inosine, and specific lipids (monoacylglycerides and gamma-tocopherol) were found to be significantly higher in the patient group than in the NC group. Notably, no significant differences were identified between the UC and CD groups, and only minimal variation in metabolite content was observed.
Serum metabolite distributions and discriminatory analysis in inflammatory bowel disease subtypes versus normal controls. (a) Principal Component Analysis (PCA) and (b) Partial Least Squares-Discriminant Analysis (PLS-DA) score plots visualization showcases the metabolic distinctions. (c) A heatmap visualization of the identified serum metabolites derived from Gas Chromatography-Time of Flight Mass Spectrometry (GC-TOF-MS) dataset. (d,e) Boxplots of tryptophan metabolism-related metabolites and ratio of primary and secondary bile acids. Significantly altered serum metabolites indicated by asterisk (*p value < 0.05, ** p value < 0.01, *** p value < 0.001, **** p value < 0.0001).
The concentrations of the metabolites associated with tryptophan metabolism were found to be significantly higher in the patient groups than in the NC group, as shown in Fig. 2D. Notably, both patient groups demonstrated a significant elevation in tryptophan and indole-3-acetic acid levels, whereas only the CD group showed increased levels of kynurenine and indole-3-propionic acid compared with the NC group. Additionally, the UC group exhibited significantly reduced levels of indole-3-acetic acid, serotonin, and acetylcholine compared to the CD group. The ratio of primary to secondary bile acids was significantly decreased in both patient groups relative to that in the NC group in Fig. 2E.
Identification of specific metabolites in IBD subtypes
First, we conducted multivariate statistical analyses for each IBD subtype (Tables S2 and S3). The results indicate that disease location in CD and disease extent in UC poorly fit the model for identifying IBD biomarkers. To further delineate the biomarkers that facilitate the classification of the IBD subtypes and distinguish them from NC, we utilized ROC curves and conducted metabolic pathway analyses. The Boruta feature selection algorithm was applied prior to the ROC curve analysis to identify the most crucial variables for IBD subtype differentiation, as shown in Figures S1-S3. The ROC curve results (Fig. 3A) demonstrated significant discriminatory power, with Area Under the Curve (AUC) values for NC vs. CD (AUC: 0.9738), NC vs. UC (AUC: 0.9887), and UC vs. CD (AUC: 0.7140), highlighting the precision of our identified metabolites in distinguishing between these groups.
Identification of serum metabolites for differentiating inflammatory bowel disease subtypes from normal controls. (A) ROC (Receiver Operating Characteristic) curve of selected serum metabolites by Boruta feature selection through comprehensive metabolic profiles. (B-D) Overview of pathway analysis. The x-axis represents the pathway impact value computed from pathway topologic analysis, and the y-axis is the negative log of the p value obtained from pathway enrichment analysis. The color of each circle is based on p values (darker colors indicate more significant changes in regard to metabolites in the corresponding pathway), whereas the size of the circle corresponds to the pathway impact score.
Additionally, the pathway analysis of the identified metabolites revealed persistent alterations in glyoxylate and dicarboxylate metabolism, alanine, aspartate, and glutamate metabolism, and glycine, serine, and threonine metabolism across all experimental groups (Fig. 3B-D). Specific metabolic pathways, such as beta-alanine metabolism, and arginine and proline metabolism, were altered in the IBD subtypes compared to the NC. Notably, glycerolipid metabolism was uniquely altered, thus distinguishing between UC and CD and underscoring its potential role in the pathophysiology of these conditions.
Identification of specific metabolites in CD and UC phenotypes
After identifying the robust metabolites for NC versus UC (Fig. S1, 33 variables), and NC versus CD (Fig. S2, 45 variables), and UC versus CD (Fig. S3 and Table S4, 14 variables) using the Boruta feature selection algorithm, we assessed their clinical applicability in sub-classifying CD and UC based on their phenotypes and other clinical characteristics. This assessment provides novel insights into the diagnostic and therapeutic management of these conditions.
Network analysis was conducted based on metabolic metabolites identified through Boruta feature selection and ROC curves for each CD and UC subclassification. The selected metabolites demonstrated statistical significance, as confirmed by the Boruta algorithm, and exhibited robust discriminatory power, with an AUC of over 0.7 and a p-value below 0.05 for each IBD subtype (refer to Table S5-7).
In CD, the network analysis revealed that certain metabolites were significantly correlated with pharmacological treatments, as illustrated in Fig. 4A. Patients who received anti-TNF treatment demonstrated elevated levels of inosine, ribose, threonic acid, 2-ethylhexanoic acid, lactic acid, and palmitic acid, whereas those who did not receive anti-TNF treatment showed lower levels of boric acid, glycerol, fumaric acid, lysine, phenylalanine, phosphate, succinic acid, and oleamide. Patients undergoing combined immunosuppressive therapy, which includes two or more steroids, thiopurines, methotrexate, and biologics, such as anti-TNFs, vedolizumab, and ustekinumab, exhibited lower levels of glycerol, cortisol, oleamide, and phosphate, except for an increase in fructose levels, when compared to untreated patients. Moreover, biological disease activity, assessed by serum CRP and fecal calprotectin levels, was closely associated with specific metabolic markers; active disease was correlated with elevated levels of maltose, glycerol, boric acid, phosphate, and succinic acid, while remission featured reduced levels of tryptophan, xanthurenic acid, 2-ethylhexanoic acid, threonic acid, glutamic acid, lactic acid, and phenylalanine (Fig. 4B and Supplementary Table S5-7).
Overview of specific biomarkers in patients with Crohn’s disease. (a) Network analysis illustrating the relationships between significantly altered serum metabolites and clinical factors. Selected serum biomarkers and clinical factors were determined using the Boruta feature selection algorithm, demonstrating good discriminatory power (AUC > 0.7, p-value < 0.05). (b) Bar plots representing the levels of confirmed serum biomarkers associated with each clinical factor.
Network analysis of UC revealed correlations with biological disease activity (active vs. remission), time of diagnosis (newly diagnosed vs. established), and immunosuppressive therapy usage (involving at least one agent among steroids, thiopurines, methotrexate, and biologics such as anti-TNFs, vedolizumab, and ustekinumab), Fig. 5A. Active UC was associated with increased levels of stearic acid, fumaric acid, succinic acid, and phosphate, in contrast to the remission phase, which showed reduced levels of deoxycholic acid (DCA), p-hydroxyphenylacetic acid, and monoglyceride (MG)(18:2(9Z,12Z)/0:0/0:0) (Fig. 5B). Newly diagnosed patients with UC exhibited elevated levels of boric acid, alpha-tocopherol, lysine, phosphate, and specific organic acids (fumaric acid, succinic acid, and urea), unlike those with an established diagnosis, who showed decreased levels of aspartic acid and alanine. Patients who received immunosuppressive therapy demonstrated increased levels of glutamic acid, aspartic acid, gamma-tocopherol, xanthurenic acid, and indole-3-lactic acid, whereas those who did not receive such treatments had lower levels of citric acid and urea.
Overview of specific biomarkers in patients with ulcerative colitis. (a) Network analysis illustrating the relationships between significantly altered serum metabolites and clinical factors. Selected serum biomarkers and clinical factors were determined using the Boruta feature selection algorithm, demonstrating good discriminatory power (AUC > 0.7, p-value < 0.05). (b) Bar plots representing the levels of confirmed serum biomarkers associated with each clinical factor.
Discussion
The current study, carried out in a large cohort and grounded in rigorously validated clinical and biological metadata, adds a novel dimension to the discourse by revealing statistically significant differences in comprehensive serum metabolite profiles between IBD patients and controls. This differentiation underscores the potential of serum metabolomics in IBD as a diagnostic biomarker, suggesting its future use in clinical practice. Importantly, our study identified serum metabolites that exhibited significant differences across IBD subtypes, bridging the translational gap and offering a pathway toward enhancing diagnostic precision in IBD. This advancement is crucial given the historical challenges associated with the overlapping clinical manifestations and the absence of definitive biomarkers.
Currently, there are a limited number of studies on biological biomarkers or distinct observable intestinal pathophysiologies specific to IBD subtypes. A metabolomics approach has been used to gradually identify metabolites in the broader areas of clinical studies, such as to discriminate IBD patients from healthy individuals9,10,11, diet-induced remission in IBD12, and also to provide new insights into the pathophysiology and potential biomarkers of IBD13,14,19. Similar to previous studies20,21, differences in the levels of serum metabolites, including fatty acids, amino acids, carbohydrates, and organic acids, were observed between patients with IBD and the NC group in the present study. These alterations in the metabolic profiles of patients with IBD are widely known to result from gut dysbiosis22.
Following these results, our research demonstrated significant decreases in most amino acids in the patient group compared to those in the control group, except for alanine and proline. The amino acid metabolic status has been related to oxidative stress promotion and cytokine release in the inflammatory response23. In particular, a lower blood glutamine concentration has been associated with increased immune activation in the GI tract24, which is consistent with our pathway analysis results. In contrast, the concentrations of monosaccharides, ribose, and fructose were higher in patients with IBD than those in the NC group. According to a recent study, fructose can induce severe oxidative stress injury that increases interleukin-6 (IL-6) levels, leading to mucosal inflammation of the intestine. Additionally, changes in the gut microbial community derived from fructose were discovered, and subsequent alterations in arginine and proline metabolic pathways were identified25. In agreement with this study, our results showed a significant enrichment of arginine and proline metabolism in the pathway analysis. Moreover, we observed significant alterations in the levels of various fatty acids and lipids. A metabolic pathway analysis comparing UC and CD highlighted glycerolipid metabolism as a high-impact factor. A recent study on lipidomic profiling of serum revealed noteworthy changes in lipids within human CD metabolism influenced by multiple pathogenic mechanisms. These findings also hold promise for the use of lipid biomarkers in diagnosis and prognosis6.
In the targeted analysis of tryptophan metabolites, distinct differences were observed between the IBD and NC groups. A previous study conducted in Germany found that serum tryptophan levels were significantly lower in patients with IBD, showing a negative correlation with the disease activity. Similarly, several studies have reported increased levels of kynurenine and kynurenine-to-tryptophan ratios in patients with IBD compared to controls7,26,27. In contrast to these findings, our study found increased tryptophan levels in patients with CD and UC. However, tryptophan metabolites, such as kynurenine, in CD, and indole metabolites in both CD and UC were also elevated compared with those in the NC group. This suggests that the observed higher levels of tryptophan in patients with IBD may not be due to decreased tryptophan degradation, but rather an initial increase in the metabolic precursor, tryptophan itself. Tryptophan is absorbed through food and then metabolized via three pathways, 90% of which progress to the kynurenine pathway28. Therefore, the consideration of dietary intake in participants could have provided further insight into the observed discrepancies. Additionally, instead of focusing solely on the absolute amounts of metabolites, analyzing the expression of indoleamine 2,3-dioxygenase 1 (IDO1), the first rate-limiting enzyme in tryptophan metabolism, or the kynurenic acid/tryptophan ratio, might offer a more accurate reflection of changes in tryptophan metabolism7. We anticipate that future studies will further elucidate these findings.
Alterations in the composition of gut microbiota in patients with IBD lead to increased levels of primary bile acids (BA) and decreased secondary BA production29. Primary BA, such as cholic acid (CA), are synthesized in the liver, conjugated to taurine or glycine, and secreted into the duodenum. Approximately 95% of primary BA are reabsorbed in the terminal ileum and recycled via the enterohepatic circulation. The unabsorbed primary BA are then deconjugated by bacteria to form secondary BA30. Gut dysbiosis in IBD decreases the deconjugation of unabsorbed BA and subsequently depletes secondary BA in the gut. A shift in BA composition has been reported to be associated with intestinal mucosal inflammation during IBD pathogenesis31.
Previous studies have suggested that alterations in serum BA profiles are correlated with the disease course and activity of IBD. However, these studies often lacked healthy controls, were limited by small sample sizes, and focused exclusively on BA analysis32,33. Our current study, involving a larger cohort of 346 patients, including healthy controls, provides a comprehensive analysis of various metabolites, in addition to BA. We demonstrated significant decreases in the ratios of primary to secondary BA in the sera of patients with both CD and UC when compared with NC (Fig. 2E). In particular, as shown in Figs. S1 and S2, the levels of primary BA and glycine- or taurine-conjugated primary BA were consistently elevated in both CD and UC groups (cholic acid [CA], glycocholic acid [GCA], glycochenodeoxycholic acid [GCDCA], and taurodeoxycholic acid [TDCA] in UC; CA, chenodeoxycholic acid [CDCA], GCA, and GCDCA in CD) relative to NC. Notably, glycodeoxycholic acid (GDCA) levels were lower in both CD and UC patients than in healthy controls, highlighting the need for further analyses to elucidate the implications of this finding. These results underscore the profound influence of altered BA profiles on the pathogenesis of IBD, suggesting a potential interplay between gut dysbiosis, BA composition, and intestinal mucosal inflammation in patients with IBD.
Currently, there is a notable gap in the research focused on identifying metabolomic markers correlated with disease phenotypes and clinical variables of IBD, such as disease severity, location, and extent. Delineating the mechanisms underlying various IBD phenotypes is essential as it could lead to the discovery of novel diagnostic therapeutic targets and enable more personalized management based on patient characteristics. Our analysis revealed that tricarboxylic acid (TCA) cycle intermediates such as succinate and fumarate were increased in the biologically active states of both UC and CD, suggesting their significant roles in regulating cellular immunity34. Succinate has been shown to accumulate under conditions of inflammation and metabolic stress and it plays a crucial role in the immunological regulation of macrophages35,36. Similarly, fumarate levels have been shown to rise following the activation of immune cells, such as macrophages and monocytes37, indicating that an active inflammatory state in IBD leads to TCA cycle deregulation and the accumulation of its intermediates. Our metabolomic pathway analysis not only highlighted glyoxylate and dicarboxylate metabolism related to the TCA cycle but also identified various interconnected amino acid metabolism pathways as key metabolic pathways altered in the serum of patients with IBD. These findings suggest the potential use of succinate and fumarate as markers for predicting disease activity in IBD.
Our network analysis identified serum metabolomic markers that were significantly associated with ongoing pharmacological treatments, particularly biologics (specifically, anti-TNF agents) and immunosuppressive therapies. These findings revealed that patients undergoing such treatments exhibit distinctive serum metabolomic profiles, underscoring the potential of these markers for monitoring treatment efficacy and tailoring therapeutic interventions according to individual patient needs. Discovery of these serum metabolomic markers offers a promising avenue for enhancing personalized medicine for IBD, enabling more precise and effective disease management. However, while these findings mark a significant step forward in the application of metabolomics to IBD treatment, they also highlight the necessity for a deeper analysis of the fundamental mechanisms at play. In addition, the differences in treatment strategies between UC and CD observed in our study suggest the need for further studies to clarify the role of serum metabolites that can be used for differential diagnosis of IBD subtypes. Future research should account for treatment-related confounding factors to ensure the accurate evaluation of serum metabolites as reliable diagnostic biomarkers and to strengthen their discriminatory power between IBD subtypes.
While our findings provide valuable insights into the effects of biologics and immunosuppressants on serum metabolites, the metabolomic impact of 5-ASA—the most commonly prescribed medication for IBD—remains poorly understood. A previous study reported no significant differences in plasma metabolite profiles between treated and untreated UC patients receiving either topical or oral 5-ASA38. Given the widespread use of 5-ASA, it is essential to investigate its potential influence on serum metabolomic profiles to better understand its therapeutic role and optimize treatment strategies. Therefore, we advocate for comprehensive research to elucidate these underlying mechanisms, particularly focusing on the metabolomic effects of 5-ASA and other common IBD medications through integrated analysis of serum and fecal metabolites, to advance personalized therapeutic approaches in IBD patient care.
Our study has several limitations. First, the participant cohort was sourced from a single center, which may have limited the generalizability of the results to broader populations. However, the robustness and size of our sample might have mitigated this issue to some extent. Secondly, although the potential biomarkers we identified show high AUC values, there is a potential risk of overfitting due to the use of the Boruta feature selection method without an independent validation cohort. To address this, we applied multiple rounds of data sampling and feature stability analysis to enhance the reliability of our findings. Nonetheless, further validation in independent, multi-center cohorts is necessary, and we are currently pursuing this through an ongoing nationwide research project to ensure more robust and generalizable results. Additionally, our study predominantly involved previously diagnosed patients and focused solely on the serum metabolome. In contrast, a recent large-scale study exclusively examined newly diagnosed treatment-naïve patients by assessing both serum and urine metabolomes, providing valuable insights that complement the findings of our serum-centric analysis39. We anticipate that subsequent studies will delve into the complex connections between serum metabolites, gut microbiota, and their metabolites, further insights as recently explored in the context of mucosal and plasma metabolomes, and their correlation with disease characteristics in pediatric IBD40. Finally, this study did not include a direct comparison of IBD patients with those suffering from other GI disorders, as the control subjects were healthy volunteers. Although we adjusted for age, sex, and BMI in our multivariate analysis using healthy controls, future studies should incorporate control groups with other intestinal inflammatory diseases to better delineate biomarkers specific to IBD, which is essential for practical clinical application in differential diagnosis. Importantly, our literature review suggests that no studies have yet conducted a comparison of serologic metabolites between IBD and non-IBD gastrointestinal conditions. This gap underscores the need for future research in this area to identify novel serologic metabolomic biomarkers that could significantly improve diagnostic precision and patient outcomes. Nevertheless, it is important to acknowledge that many prior studies investigating serum metabolomic profiles in IBD have similarly compared IBD patients with healthy controls, reflecting a broader methodological challenge within the field. The limited research in this area may also be due to the relatively short disease course and spontaneous resolution observed in conditions like infectious colitis and ischemic colitis, as well as the research focus on pathophysiology in irritable bowel syndrome, rather than on serologic biomarkers.
In conclusion, we combined untargeted and targeted analyses to identify specific serum metabolomic changes associated with IBD and its subtypes. Targeted metabolomic analysis is essential to distinguish between these subtypes. Additionally, the network analysis revealed markers related to IBD phenotypes, providing a critical foundation for future studies. Our findings reinforce the significance of serum metabolomics as a patient-friendly diagnostic marker that may play a crucial role in advancing personalized IBD care.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- IBD:
-
Inflammatory bowel disease
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- UC:
-
Ulcerative colitis
- CD:
-
Crohn’s disease
- NC:
-
Normal controls
- GC-TOF-MS:
-
Gas chromatography-time-of-flight mass spectrometry
- LC-TQ-MS:
-
Liquid chromatography-triple-quadrupole
- PCA:
-
Principal Component Analysis
- PLS-DA:
-
Partial Least Squares Discriminant Analysis
- TRP:
-
Tryptophan
- IDO1:
-
Indoleamine 2,3-dioxygenase 1
- BA:
-
Bile acid
- CRP:
-
C-reactive protein
References
Ng, S. C. et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. Lancet 390(10114), 2769–2778 (2017).
Piovani, D. et al. Environmental risk factors for inflammatory bowel diseases: An umbrella review of meta-analyses. Gastroenterology. 157(3), 647–659 (2019).
Guan, Q. A comprehensive review and update on the pathogenesis of inflammatory bowel disease. J. Immunol. Res. 2019, 1–16 (2019).
Feakins, R. et al. ECCO topical review on clinicopathological spectrum and differential diagnosis of inflammatory bowel disease. J. Crohns Colitis. 16(3), 343–368 (2022).
Lu, Y. et al. Development and validation of a new algorithm model for differential diagnosis between Crohn’s disease and intestinal tuberculosis: A combination of laboratory, imaging and endoscopic characteristics. BMC. Gastroenterol. 21, 1–9 (2021).
Nikolaus, S. et al. Increased tryptophan metabolism is associated with activity of inflammatory bowel diseases. Gastroenterology. 153(6), 1504–1516 (2017).
Sofia, M. A. et al. Tryptophan metabolism through the kynurenine pathway is associated with endoscopic inflammation in ulcerative colitis. Inflamm. Bowel. Dis. 24(7), 1471–1480 (2018).
Ma, R. et al. A novel serum metabolomic panel for the diagnosis of Crohn’s disease. Inflamm. Bowel. Dis. 29(10), 1524–1535 (2023).
Liu, H. et al. Untargeted serum metabolomics reveals specific metabolite abnormalities in patients with Crohn’s disease. Front. Med. 9, 814839 (2022).
Daniluk, U. et al. Untargeted metabolomics and inflammatory markers profiling in children with Crohn’s disease and ulcerative colitis—A preliminary study. Inflamm. Bowel. Dis. 25(7), 1120–1128 (2019).
Ghiboub, M. et al. Metabolome changes with diet-induced remission in pediatric Crohn’s disease. Gastroenterology. 163(4), 922–936 (2022).
Keshteli, A. H. et al. Comparison of the metabolomic profiles of irritable bowel syndrome patients with ulcerative colitis patients and healthy controls: New insights into pathophysiology and potential biomarkers. Aliment. Pharmacol. Ther. 49(6), 723–732 (2019).
Keshteli, A. H. et al. A distinctive urinary metabolomic fingerprint is linked with endoscopic postoperative disease recurrence in Crohn’s disease patients. Inflamm. Bowel. Dis. 24(4), 861–870 (2018).
Probert, F. et al. Plasma nuclear magnetic resonance metabolomics discriminates between high and low endoscopic activity and predicts progression in a prospective cohort of patients with ulcerative colitis. J. Crohns Colitis. 12(11), 1326–1337 (2018).
Clish, C. B. Metabolomics: An emerging but powerful tool for precision medicine. Mol. Case. Stud. 1(1), 000588 (2015).
Gallagher, K., Catesson, A., Griffin, J. L., Holmes, E. & Williams, H. R. Metabolomic analysis in inflammatory bowel disease: A systematic review. J. Crohns Colitis. 15(5), 813–826 (2021).
Maaser, C. et al. ECCO-ESGAR guideline for diagnostic assessment in IBD Part 1: Initial diagnosis, monitoring of known IBD, detection of complications. J. Crohns Colitis. 13(2), 144–164 (2019).
Dong, J. et al. Body mass index is associated with inflammatory bowel disease: A systematic review and meta-analysis. PLoS ONE 10(12), e0144872 (2015).
Hisamatsu, T. et al. Novel, objective, multivariate biomarkers composed of plasma amino acid profiles for the diagnosis and assessment of inflammatory bowel disease. PLOS ONE 7(1), 31131 (2012).
Scoville, E. A. et al. Alterations in lipid, amino acid, and energy metabolism distinguish Crohn’s disease from ulcerative colitis and control subjects by serum metabolomic profiling. Metabolomics. 14, 1 (2018).
Zheng, L., Wen, X. L. & Duan, S. L. Role of metabolites derived from gut microbiota in inflammatory bowel disease. World. J. Clin. Cases. 10(9), 2660–2677 (2022).
Zhenyukh, O. et al. High concentration of branched-chain amino acids promotes oxidative stress, inflammation and migration of human peripheral blood mononuclear cells via mTORC1 activation. Free. Radic. Biol. Med. 104, 165–177 (2017).
Perna, S. et al. The role of glutamine in the complex interaction between gut microbiota and health: A narrative review. Int. J. Mol. Sci. 20(20), 5232 (2019).
Song, G. et al. Fructose stimulated colonic arginine and proline metabolism dysbiosis, altered microbiota and aggravated intestinal barrier dysfunction in DSS-induced colitis rats. Nutrients. 15(3), 782 (2023).
Ferru-Clément, R. et al. Serum lipidomic screen identifies key metabolites, pathways, and disease classifiers in Crohn’s disease. Inflamm. Bowel. Dis. 29(7), 1024–1037 (2023).
Dudzińska, E. et al. Increased expression of kynurenine aminotransferases mRNA in lymphocytes of patients with inflammatory bowel disease. Therap. Adv. Gastroenterol. 12, 1756284819881304 (2019).
Gostner, J. M. et al. Tryptophan metabolism and related pathways in psychoneuroimmunology: The impact of nutrition and lifestyle. Neuropsychobiology. 79(1), 89–99 (2020).
Upadhyay, K. G., Desai, D. C., Ashavaid, T. F. & Dherai, A. J. Microbiome and metabolome in inflammatory bowel disease. J. Gastroenterol. Hepatol. 38(1), 34–43 (2023).
Shapiro, H., Kolodziejczyk, A. A., Halstuch, D. & Elinav, E. Bile acids in glucose metabolism in health and disease. J. Exp. Med. 215(2), 383–396 (2018).
Thomas, J. P., Modos, D., Rushbrook, S. M., Powell, N. & Korcsmaros, T. The emerging role of bile acids in the pathogenesis of inflammatory bowel disease. Front. Immunol. 13, 829525 (2022).
Liu, C. et al. Bile acid alterations associated with indolent course of inflammatory bowel disease. Scand. J. Gastroenterol. 58(9), 988–997 (2023).
Sun, R., Jiang, J., Yang, L., Chen, L. & Chen, H. Alterations of serum bile acid profile in patients with Crohn’s disease. Gastroenterol. Res. Pract. 2022, 1680008 (2022).
Connors, J., Dawe, N. & Van Limbergen, J. The role of succinate in the regulation of intestinal inflammation. Nutrients. 11(1), 25 (2018).
Ryan, D. G. & O’Neill, L. A. Krebs cycle reborn in macrophage immunometabolism. Annu. Rev. Immunol. 38, 289–313 (2020).
Tannahill, G. et al. Succinate is an inflammatory signal that induces IL-1β through HIF-1α. Nature. 496(7444), 238–242 (2013).
Kelly, B. & O’neill, L. A. Metabolic reprogramming in macrophages and dendritic cells in innate immunity. Cell. Res. 25(7), 771–784 (2015).
Colombel, J. F. et al. Adalimumab for maintenance of clinical response and remission in patients with Crohn’s disease: The CHARM trial. Gastroenterology 132(1), 52–65 (2007).
Probert, F. et al. Plasma nuclear magnetic resonance metabolomics discriminates between high and low endoscopic activity and predicts progression in a prospectived cohort of patients with ulcerative colitis. J. Crohns Colitis. 12(11), 1326–1337 (2018).
Aldars-García, L. et al. Serum and urine metabolomic profiling of newly diagnosed treatment-naïve inflammatory bowel disease patients. Inflamm. Bowel. Dis. 30(2), 167–182 (2024).
Nyström, N. et al. Mucosal and plasma metabolomes in new-onset paediatric inflammatory bowel disease: Correlations with disease characteristics and plasma inflammation protein markers. J. Crohns Colitis. 17(3), 418–432 (2023).
Acknowledgements
This study was supported by the Seoul Clinical Laboratories (SCL), Yongin, Korea, for the serum sample collection. The participants with IBD in this study are from a broader cohort of Korean individuals with IBD who have contributed stool, blood, and mucosal tissue specimens for a multi-omics investigation (ClinicalTrials.gov identifier: NCT03589183). All study participants provided informed consent for this study, which was approved by the Institutional Review Board (IRB) of Kyung Hee University Hospital (Approval No. 2018-03-006).
Funding
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare of the Republic of Korea (Grant Number: RS-2023-KH135855), and supported by the Medical Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Science and ICT (NRF-2017R1A5A2014768).
Author information
Authors and Affiliations
Contributions
The study concept and design were developed by CKL, YJ and ESJ. Samples were collected and analyzed by all authors, including CHO, YJK, and WK. DHS, HJK and YJP performed the experiments and data analysis. Analysis and interpretation of the data were conducted by all authors, including JEK, SJO and CKL. JEK and DHS was responsible for the initial draft of the manuscript, while all authors provided critical revisions and ultimately approved the final version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, J.E., Suh, D.H., Park, Y.J. et al. Identifying robust biomarkers for the diagnosis and subtype distinction of inflammatory bowel disease through comprehensive serum metabolomic profiling. Sci Rep 15, 5661 (2025). https://doi.org/10.1038/s41598-025-90160-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-90160-7