Abstract
This study aimed to determine whether ultrasonography can be used to assess the oropharyngeal airway in patients with obstructive sleep apnoea hypopnoea syndrome (OSAHS). 104 patients with OSAHS and 104 sex-, body mass index (BMI)-, and age-matched healthy subjects underwent oropharynx airway assessment using ultrasound. The dimensional changes of the oropharynx were monitored, and sonographic measurements of the airway lumen were obtained during deep breathing. Measurements were compared between groups. All suspected patients underwent Polysomnography in the sleep laboratory. OSAHS was defined as apnea-hypopnea index (AHI) > 5 events/h. Adequate visualization of oropharyngeal dimensional changes was obtained in 95.19% of patients with OSAHS and 100% of healthy subjects. The anteroposterior diameter (AP) and lateral diameter (LAT) of the oropharyngeal airway of patients with OSAHS were smaller than those of healthy subjects at the end of deep inspiration and expiration (all P < 0.05). Patients with OSAHS had greater lateral airway dimensional changes than the anterior-posterior dimension changes (P < 0.001). The AP/LAT ratio of OSAHS at the end of deep inspiration was higher than that of healthy subjects (P = 0.012). Ultrasonography can detect the dimensional changes of the oropharyngeal airway in patients with OASHS during deep breathing. Patients with OASHS have a smaller airway size, a more circular configuration, and a more significant change of diameter in oropharynx airway than healthy subjects.
Similar content being viewed by others
Introduction
OSAHS affects nearly 1 billion young-middle-aged people worldwide1. Obstructive sleep apnoea hypopnoea syndrome (OSAHS) is defined by apnoea and hypopnoea caused by partial or complete obstruction of the upper airways during sleep2. The oropharyngeal airway plays an important role in the pathogenesis of OSAHS, the evaluation of dynamic dimensional changes of the upper airway not only provides the biomechanics and pathophysiology for OSAHS diagnosis, also provides a framework to model its biomechanical properties and propensity to collapse during sleep, and helps doctors to determine treatment strategies for patients with OSAHS3. Many imaging approaches, such as computed tomography (CT) and magnetic resonance imaging (MRI), can provide valuable information about the structure and function of the oropharynx. However, CT involves ionizing radiation, and MRI is expensive and not easily accessible. A previous study indicated that ultrasonography (US) may be useful in providing detailed anatomical information on the oropharynx airway and has numerous potential utilities for clinical applications4. Lun et al. found that sonography was valuable in evaluating the diameter of the oropharyngeal airway in healthy adult subjects which provides a realistic impression of oropharyngeal dimensional changes during deep breathing5,6. However, to the best of our knowledge, the US has not been applied to assess oropharynx airway dimensional changes in individuals with OSAHS. Therefore, this study aimed to use the US to evaluate the oropharyngeal airway dimensional changes during deep breathing in OSAHS.
Materials and methods
This study is approved by the Ethics Committee of the first affiliated hospital of Guangxi Medical University (approval number:2024-E773-01), and all participants provided written informed consent before participating in the study. All methods were performed in accordance with the relevant guidelines and regulations. This study adopted non-randomized, observational study with a control group.
Participants
Participants in this study were categorized into two groups (OSAHS and healthy subjects):
OSAHS group
Patients were enrolled in this study if they met the following inclusion criteria: (1) patients who underwent overnight Polysomnography (PSG) examinations and were diagnosed with OSAHS based on overnight PSG and (2) patients who had not received prior treatment for OSAHS before the ultrasonic examination. The ultrasonic examination was performed the next morning after PSG. The exclusion criteria were as follows: cooperated poorly, definite deformations of head and neck such as retrognathia, history of head and neck surgery and radiotherapy, recent head and neck disease or cancer. After applying these criteria, 104 patients were enrolled in this study.
Healthy subject group
104 body mass index (BMI)-, sex-, and age-matched healthy participants agreed to participate in this study. All of them underwent a thorough history and physical examination. All healthy subjects were free of any symptoms suggesting sleep apnea (such as snoring; frequent feelings of tiredness, fatigue, and drowsiness during the day; cessation of breathing during sleep and hypertension, etc.), other sleep disorders, no history of obstructive upper airway disease, and no history of disease affecting the respiratory system. BMI, sex, and age of healthy subjects were matched with those of patients with OSAHS.
Polysomnography (PSG)
Overnight PSG was performed using a digital EMBLA Titanium™ system (Embla, Broomfield, USA). All suspected patients underwent PSG in the sleep laboratory. The apnea-hypopnea index (AHI) was calculated as the total number of episodes of apnea and hypopnea per hour of sleep based on the PSG results. OSAHS was defined as AHI > 5 events/h. The lowest oxygen saturation (LSAT) was also recorded for each patient.
Ultrasonic examination
The device used was the Resona 70 B (Mindray Medical International Ltd., Shenzhen, China) with a curved transducer in the frequencies of 2–5 MHz. The sonographic examination was performed by a certified sonographer who has 10 years of experience in sonography of the head and neck and was blinded to the polysomnographic data. Visualization rates of the oropharynx airway were detected according to whether the air-tissue interface of the oropharynx airway could be well-recognized.
All participants underwent sonographic examinations in the supine position while fully awake and were instructed to breathe through their noses with their mouths closed. Ultrasonic examinations were performed as described previously5,6. The procedural setup for using a convex array transducer to acquire oropharyngeal airway images is as follows:
-
(1)
Lateral oblique views
The neck was maximally hyperextended, and the maximum turning of the head on the opposite side was examined. The convex array transducer was transversely across the left lateral neck, parallel to the mandible (Fig. 1).
-
(2)
Transverse view
To optimally visualize this area, the participant’s head and neck maintained a neutral position with the neck hyperextended maximally and the chin kept up (position of maximum rise, remain) without a pillow (Fig. 2). The convex array transducer is transverse across the anterior surface of the neck, just above the hyoid bone. Standard planes to view the oropharyngeal airway and the detailed measurement method are shown in Table 1. The oropharynx airway dimensions were obtained based on the deep expiratory and deep inspiratory phases of three deep breaths. The oropharynx airway dimensions were measured across the three deep breaths to obtain the mean value.
Statistical analysis
The data were analyzed using SPSS 25.0 (SPSS Inc., Chicago, IL, USA). Data are expressed as mean ± SD and compared between participants diagnosed with OSAHS and healthy subjects using the two-sample t-test. The US diameters between the end of deep inspiration and deep expiration were compared using a paired-sample t-test. Independent prediction role of ultrasonic parameters was evaluated through a binary logistic regression method. Receiver operating characteristics (ROC) curves were generated to determine the area under the curve (AUC) to evaluate the ability of the ultrasonic parameters as diagnostic markers. Youden’s score was used to detect optimal sensitivity and specificity. Spearman’s correlation test was performed to evaluate the association between AHI, lowest oxygen saturation (LSAT), and airway parameters in patients with OSAHS. For all statistical tests, p ≤ 0.05 indicated statistical significance.
Results
Reliability and reproducibility studies
Interobserver and intraobserver reliabilities were calculated using intraclass correlation coefficients (ICC) for sonographic measurements of the oropharynx in 20 patients with OSAHS. The ICC value was > 0.7, indicating good reproducibility. Good reliability was demonstrated, with internal consistency values (Cronbach’s α) greater than 0.8.
Rate of visualization
In the healthy subject group, the oropharyngeal airway of all participants was easily visualized by sonography, compared to 95.19% (99/104) in patients with OSAHS.
Ultrasound imaging
Lateral oblique views
On lateral oblique scans, the oropharyngeal airway was visualized deep to the lateral pharyngeal wall and ran between the posterior border of the tongue and the anterior border of the rear pharyngeal wall. In the lateral oblique view, the oropharyngeal airway resembled a hyperechoic curvilinear line with typical posterior air artifacts (Fig. 3). After deep inspiration, the tongue moved anteriorly away from the posterior pharyngeal wall and reached its maximum displacement at the end of deep inspiration. The tongue retracted posteriorly toward its initial position during deep expiration. Accompanied by the anterior dimensional changes of the tongue, the oropharyngeal airway gradually expanded during deep inspiration. With the advancement of the tongue, the lateral pharyngeal walls around the tongue move inward during deep inspiration. Figures 3 and 4 show the displacement of these tissues during deep breathing in patients with OSAHS and healthy subjects.
The displacement of tissues during deep breathing in patients with OSAHS in lateral oblique views. (a) Probe location in lateral oblique planes. (b) Sonogram of the oropharynx in patients with OSAHS at the end of deep inspiration. (c) Sonogram of the oropharynx in patients with OSAHS at the end of deep expiration. Lateral oblique images taken in the submandibular region show an oropharynx airway, which appears hyperechoic curvilinear line (small arrows). Hyperechoic echogenicity with ringdown gas artifact (large arrows) suggests the airway origin. 1 and 2, the caliper points show the borders of the airway, and the anterior-posterior diameter (between cursors) of the oropharynx airway was measured in these standard planes. GG indicates genioglossus. (d) Schematic drawing of the internal anatomy of the oropharynx, the transducer position, and illustration of ultrasonic measurements.
The displacement of tissues during deep breathing healthy subjects in lateral oblique views. (a) Probe location in lateral oblique planes. (b) Sonogram of the oropharynx in healthy subjects at the end of deep inspiration. (c) Sonogram of the oropharynx in healthy subjects at the end of deep expiration. Lateral oblique images taken in the submandibular region show the oropharynx airway, which appears hyperechoic curvilinear line (small arrows). 1 and 2, the caliper points show the borders of the airway, and the anterior-posterior diameter (between cursors) of the oropharynx airway was measured in these standard planes. GG indicates genioglossus. (d) Schematic drawing of the internal anatomy of the oropharynx, the transducer position, and illustration of ultrasonic measurements.
Transverse view
The oropharyngeal airway was visible through the genioglossus muscles as a hyperechoic curvilinear line on the transverse view (Fig. 5). Its left and right border were delineated by the lateral pharyngeal walls. The lateral pharyngeal walls move inward to narrow the transverse diameters of the oropharyngeal airway during deep inspiration. During deep expiration, the lateral pharyngeal walls move outward to dilate the transverse diameters of the oropharyngeal airway. Figures 5 and 6 show the displacement of these tissues during deep breathing in healthy subjects and patients with OSAHS.
The displacement of these tissues during deep breathing in healthy subjects in transverse views. (a) Probe location in transverse planes. (b) Sonogram of the oropharynx in healthy subjects at the end of deep inspiration. (c) Sonogram of the oropharynx at the end of deep expiration. A transverse view of the oropharynx airway taken with the probe in the submental area just above the hyoid bone shows the oropharynx airway (arrows) as a bright hyperechoic line. The anterior and lateral walls of the oropharynx airway are formed by the genioglossus (GG) and lateral oropharyngeal wall (triangle), respectively. The lateral diameter (cursors and the number 1,2) of the oropharynx airway was measured in these standard planes. MH indicates mylohyoid; GH, geniohyoid. (d) Schematic drawing of the internal anatomy of the oropharynx, the transducer position, and illustration of ultrasonic measurements.
The displacement of these tissues during deep breathing in patients with OSAHS in transverse views. (a) Probe location in transverse planes. (b) Sonogram of the oropharynx in healthy subjects at the end of deep expiration. (c) Sonogram of the oropharynx at the end of deep inspiration. A transverse view of the oropharynx airway taken with the probe in the submental area just above the hyoid bone shows the oropharynx airway (arrows) as a bright hyperechoic line. The anterior and lateral walls of the oropharynx airway are formed by the genioglossus (GG) and lateral oropharyngeal wall (triangle), respectively. The lateral diameter (cursors and the number 1,2) of the oropharynx airway was measured in these standard planes. MH indicates mylohyoid; GH, geniohyoid. (d) Schematic drawing of the internal anatomy of the oropharynx, the transducer position, and illustration of ultrasonic measurements.
Patient characteristics and US parameters of the oropharynx airway
Table 2 summarizes the clinical characteristics, polysomnographic data, and sonographic measurements of the oropharyngeal airways. Compared with healthy subjects, patients with OSAHS had a significantly smaller oropharyngeal airway. The anterior-posterior diameter (AP) and AP/lateral diameter (LAT) ratios were higher at the end of deep inspiration than at the end of deep expiration in each group (P < 0.001). The LATs were smaller at the end of deep inspiration than deep expiration in each group (P < 0.001 for both).
There were no differences between dimensions’ changes of the anteroposterior and the dimensions’ changes of the lateral airways in the healthy group (t = 1.159, P = 0.249). Patients with OSAHS had greater lateral airway dimensional changes than the anterior-posterior dimension changes (t = − 7.206, P < 0.001).
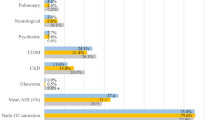
In binary logistic regression analysis, LAT (Ins) and LAT (Expi) were the most important predictive factor for OSAHS (p both < 0.001) (Table 3). ROC curves were applied to determine the sensitivity and specificity of the LAT (Ins) and LAT (Expi). As depicted in Fig. 7, the AUC value of the LAT (Ins) was 0.738 which was significantly higher than LAT (Expi) (0.581). A LAT (Ins) lower than 34.6 had the highest diagnostic value for OSAHS, with a sensitivity of 48.1% and a specificity of 92.3%. A LAT (Expi) lower than 40.4 had the highest diagnostic value for OSAHS, with a sensitivity of 30.8% and a specificity of 89.4%.
In a correlative study of AHI, LSAT, BMI, age, and US parameters in patients with OSAHS, we observed positive and negative correlations, which are presented in Table 4. AHI was positively correlated with AP (Ins) (ρ = 0.202, p = 0.040), AP (Expi) (ρ = 0.197, p = 0.045), and AP/LAT (Expi) (ρ = 0.222, p = 0.023). For the US parameters, the interobserver and intraobserver agreement were excellent (ICC, 0.771–0.879 for interobserver reliability and 0.822–0.907 for intraobserver reliability) (Table 5).
Discussion
The oropharynx’s anterior, posterior, and lateral walls are formed by the following structures: the soft palate, tongue, lingual tonsils, constrictor muscles, and connective tissue. This study used these structures as acoustic windows to evaluate the oropharyngeal airway. A useful landmark in identifying the oropharyngeal airway is the strong echoes of the air-tissue interface, which generally can be demonstrated without difficulty. Furthermore, the change in the relative position of adjacent organs (tongue, lateral pharyngeal wall and posterior pharyngeal wall) and airway gas may allow significantly improved visualization of the oropharyngeal airway. In our study, the rate of visualization of the oropharynx airway in patients with OSAHS was lower than that in healthy subjects. One of the reasons may be that patients with OSAHS have a greater volume of the pharyngeal wall, and the deeper position of the oropharynx airway results in inadequate penetration the poor resolution. Another reason is that, although speculative, an increase in parapharyngeal fat may cause poor ultrasonic penetration (Fig. 8).
Sonogram of the oropharynx in patients with OSAHS. (a) Sonogram of the oropharynx in patients with OSAHS at the end of deep inspiration. (b) Sonogram of the oropharynx in patients with OSAHS at the end of deep expiration. Transverse view of the oropharynx airway in a 37-year-old patient with OSAHS (male; BMI, 34.54; AHI, 107/h; LSAT, 44%) with the probe placed just above the hyoid bone. GG indicates genioglossus; MH, mylohyoid; and GH, geniohyoid.
In this study, in patients with OSAHS and healthy subjects, the tongue moved anteriorly, and the lateral pharyngeal walls moved inward during deep inspiration. During deep expiration, the tongue and the lateral pharyngeal walls return to their initial position. Cheng et al. reported similar results and suggested that the genioglossus moved anteriorly during inspiration and posteriorly during expiration7. Ultrasonography revealed that the oropharynx airway lumen varied with a displacement of its surrounding structure during deep inspiration and expiration. The behavior and activity patterns of the oropharynx airway and its surrounding soft tissue during deep respiration were quite similar between OSAHSs and healthy subjects. However, patients in OSAHS group had a smaller oropharynx airway size and a more significant change in oropharynx airway diameter compared to healthy subjects. This result suggested that the range of pharyngeal wall dimensional changes of the upper airway in patients with OSAHS was higher than that in healthy subjects. Meanwhile, the change of oropharynx airway transverse diameter was greater than the anteroposterior diameter in the OSAHS group but not in the healthy subject group. The increased propensity of the airway to collapse should be reflected by the increased dimensional changes of airway boundary during respiration as negative upper airway intraluminal pressure is increased8,9. Our results support that patients with OSASH have increased variability in airway diameter and tissue movement, consistent with the hypothesis that airway collapsibility plays a crucial role in the pathogenesis of OSAHS. Furthermore, ROC curve analysis indicated that LAT (Ins) and LAT (Expi) could effectively identify OSAHS, with cutoff values of LAT (Ins) = 34.6, and LAT (Expi) = 40.4. Among these parameters, a LAT (Ins) lower than 34.6 had the highest diagnostic value. The sensitivity of LAT (Ins) and LAT (Expi) were low because the upper bound of the measurement values in patients with OSAHS were close to the normal measurement values in healthy subjects. Sonography provides a new and effective reference for the differential diagnosis of OSAHS, especially suitable for distressed area, which had the worst health care. Choosing an appropriate oropharyngeal size is important for effective and timely airway management10. The oropharyngeal examination assessed oropharyngeal airway size and lateral pharyngeal wall dimensional changes may help quantify the degree of oropharyngeal anatomical obstruction for OSAHS patient, which were predictive factors for surgical outcomes. Sonography may be a useful measuring tools for choosing an appropriate oropharyngeal size and assessing the degree of lateral pharyngeal wall dimensional changes to predict the surgical outcomes of OSAHS10,11.
In this study, patients with OSAHS have a significantly higher AP/LAT ratio than healthy subjects at the end of deep inspiration. OSAHS patients had a slightly higher AP/LAT ratio than healthy subjects at the end of deep expiration, although the difference was not significant. Our results show dynamic changes in the airway shape during deep inspiration and expiration, and there was increased variability in airway shape in the inspiration state. These findings are consistent with a previous notion of airway collapse during inspiration in OSASH12,13. Additionally, patients with OSAHS in our study had a more circular configuration of the oropharyngeal airway with the major axis oriented in the LAT than healthy subjects, which is consistent with previous reports by Rodenstein et al. and Mayer et al., which also found that patient with OSAHS had a more circular configuration of upper airway than healthy controls14,15. With aging and increasing BMI, the oropharynx changes shape. The airway lumen became more spherical in patients with OSAHS with a higher BMI. These results further suggest that the AP/LAT ratio is an essential factor associated with the occurrence and development of OSAHS.
In this sample, BMI and AHI had a significant relationship with the AP dimensions in patients with OSAHS; however, there was no significant correlation between BMI (AHI, age) and oropharynx airway transverse diameter. Wang et al. found that weight loss was associated with decreased anterior–posterior distance and increased lateral distance in the retropalatal region16, which is very similar to our results.
The limitation of our study was that no reference standard such as CT, MRI or nasoendoscopy is available for comparison to determine the accuracy of sonographic measurements of the oropharynx airway lumen due to radiation exposure high cost or incursion. Although the reliability (ICC) and internal consistency (Cronbach’s α) were suitable for all measurements in the present study, further validation study of ultrasound oropharynx airway diameter measurements is needed, and gross specimen may be the best reference standard. It is important to note that the OSAHS and normal subjects keep the same posture during ultrasonic examination, but there may be potential alteration of oropharyngeal shape and size due to the neck in the hyperextended position and turned to the side17.
Conclusions
Ultrasonography can detect the dimensional changes of the oropharyngeal airway in patients with OASHS during deep breathing. Patients with OASHS have a smaller airway size, a more circular configuration, and a more significant change of diameter in oropharynx airway than healthy subjects. Sonography provides a new and effective reference for the differential diagnosis of OSAHS as a beneficial noninvasive choice for research applications.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Benjafield, A. V. et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. Lancet Respir Med. 7 (8), 687–698 (2019).
Kapur, V. K. et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep. Med. 13 (3), 479–504 (2017).
Chen, L., Xiao, T. & Ng, C. T. The biomechanical mechanism of upper airway collapse in OSAHS patients using clinical Monitoring data during natural sleep. Sens. (Basel). 21 (22), 7457 (2021).
Abdallah, F. W. et al. Is ultrasound a valid and reliable imaging modality for airway evaluation? An observational computed tomographic validation study using submandibular scanning of the mouth and oropharynx. J. Ultrasound Med. 36 (1), 49–59 (2017).
Lun, H. M., Zhu, S. Y., Liu, R. C., Gong, J. G. & Liu, Y. L. Investigation of the upper airway anatomy with ultrasound. Ultrasound Q. 32 (1), 86–92 (2016).
Lun, H. M., Zhu, S. Y., Hu, Q., Liu, Y. L. & Wei, L. S. Sonographic assessment of oropharynx movement during deep breathing. Ultrasound Med. Biol. 45 (11), 2906–2914 (2019).
Cheng, S., Butler, J. E., Gandevia, S. C. & Bilston, L. E. Movement of the human upper airway during inspiration with and without inspiratory resistive loading. J. Appl. Physiol. (1985). 110 (1), 69–75 (2011).
Schwab, R. J., Gefter, W. B., Hoffman, E. A., Gupta, K. B. & Pack, A. I. Dynamic upper airway imaging during awake respiration in normal subjects and patients with sleep disordered breathing. Am. Rev. Respir Dis. 148 (5), 1385–1400 (1993).
Arens, R. et al. Changes in upper airway size during tidal breathing in children with obstructive sleep apnea syndrome. Am. J. Respir Crit. Care Med. 171 (11), 1298–1304 (2005).
Castro, D. & Freeman, L. A. Oropharyngeal airway. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing (2024). Jan– (2023).
Lai, C. C. et al. Clinical predictors of pediatric obstructive sleep apnea syndrome. Ann. Otol. Rhinol. Laryngol. 127 (9), 608–613 (2018).
Suratt, P. M., Dee, P., Atkinson, R. L., Armstrong, P. & Wilhoit, S. C. Fluoroscopic and computed tomographic features of the pharyngeal airway in obstructive sleep apnea. Am. Rev. Respir Dis. 127 (4), 487–492 (1983).
Stein, M. G. et al. Cine CT in obstructive sleep apnea. AJR Am. J. Roentgenol. 148 (6), 1069–1074 (1987).
Rodenstein, D. O. et al. Pharyngeal shape and dimensions in healthy subjects, snorers, and patients with obstructive sleep apnoea. Thorax 45 (10), 722–727 (1990).
Mayer, P. et al. Relationship between body mass index, age and upper airway measurements in snorers and sleep apnoea patients. Eur. Respir J. 9 (9), 1801–1809 (1996).
Wang, S. H. et al. Effect of weight loss on upper airway anatomy and the apnea-hypopnea index. The importance of tongue fat. Am. J. Respir Crit. Care Med. 201 (6), 718–727 (2020).
Prasad, A. et al. Comparison of sonography and computed tomography as imaging tools for assessment of airway structures. J. Ultrasound Med. 30 (3), 965–972 (2011).
Author information
Authors and Affiliations
Contributions
Yaoli Liu and Haimei Lun wrote the main manuscript text and prepared figures and tables, Qiao Hu, Lisi Wei, Linsong Ye Searched literature and reviewed relevant content, Shangyong Zhu Reviewed and revised the entire text.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
The author(s) declare(s) that they had full access to all the data in this study, and the author(s) take(s) complete responsibility for the integrity of the data and the accuracy of the data analysis.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, Y., Lun, H., Hu, Q. et al. Dynamic behavior of the oropharynx airway during deep breath in patients with obstructive sleep apnoea hypopnoea syndrome observed by ultrasonography. Sci Rep 15, 5585 (2025). https://doi.org/10.1038/s41598-025-90312-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-90312-9