Abstract
The relationship between 25-hydroxyvitamin D (25(OH)D) status and cardiovascular disease (CVD) in the diabetes population still needs to be clarified. This study aimed to explore the association of 25(OH)D with CVD and cardiometabolic risk factors in Chinese population with type 2 diabetes mellitus (T2DM). This cross-sectional study was performed with 1378 hospitalized patients with T2DM. Participants were classified into three groups according to the serum 25(OH)D levels: vitamin D adequate, vitamin D insufficiency and vitamin D deficient. Multivariate logistic regression analysis, stratified analysis and interaction analysis were performed to determine the relationship between serum 25(OH)D levels and CVD outcome. After adjusting for confounders, serum 25(OH)D levels were significantly negatively associated with cardiovascular disease in type 2 diabetic patients [OR: 0.97 (0.94, 0.99), p = 0.0131]. Taking the vitamin D-sufficient group (≥ 20 ng/mL) as a reference, the vitamin D-deficiency group (< 12 ng/mL) was associated with a significantly higher risk of cardiovascular disease, with a 1.25-fold increased risk after adjusting for all potential confounders [OR: 2.25 (1.33, 3.79), p = 0.0023]. Stratification analysis showed that the association between vitamin D deficiency and increased risk of cardiovascular disease was particularly significant in women [OR: 4.32 (1.54, 12.12), p = 0.0055], older adults [OR: 4.14 (1.10, 15.56), p = 0.0355], normal-weight [OR: 4.09 (1.51, 11.10), p = 0.0056] and obese subjects [OR: 3.66 (1.03, 13.05), p = 0.0453]. Vitamin D deficiency was significantly associated with an increased risk of overweight/obesity [OR: 1.57 (1.10, 2.24), p = 0.0134], hypertension [OR: 1.81 (1.30, 2.51), p = 0.0004], hypertriglyceridemia [OR: 1.56 (1.12, 2.16), p = 0.0078] and reduced HDL-C [OR: 1.67 (1.19, 2.35), p = 0.0033]. Serum 25(OH)D levels were significantly negatively associated with CVD in T2DM patients and vitamin D deficiency was significantly associated with an increased risk of overweight/obesity, hypertension and dyslipidemia.
Similar content being viewed by others
Introduction
The number of adults with diabetes is growing rapidly worldwide. In 2021, the International Diabetes Federation (IDF) reported that 537 million adults worldwide suffer from diabetes and this number is predicted to increase to 643 million by 20301. The harm of diabetes primarily depends on its serious complications, particularly CVD. CVD is the leading cause of mortality and disability among people with T2DM, and approximately one in three adults with T2DM already have CVD2. Individuals with diabetes have two to fourfold increased risks of CVD and mortality compared with the normal population after adjustment for conventional risk factors3,4,5. Furthermore, CVD mortality accounts for approximately one-half of all deaths in diabetes6. Despite extensive epidemiological assessment of the growth of diabetes prevalence, the quantification of the disease burden of and variation in diabetes-related complications is lacking7. As China’s population ages, the burden of death and disability caused by diabetes and its complicated CVD will continue to increase. Therefore, identifying modifiable cardiometabolic risk factors in individuals with diabetes is necessary for the prevention of diabetes-related cardiovascular complications6.
Vitamin D is an essential fat-soluble vitamin that regulates calcium and phosphorus metabolism and maintains bone health. In addition, vitamin D plays an important role in the function of various organs and tissues, including the cardiovascular system8. One of the proposed mechanisms of action is renin-angiotensin-aldosterone (RAAS) activation. It was reported that the vitamin D receptor (VDR) knock-out mice have higher blood pressure and develop cardiac hypertrophy due to increased renin expression and subsequent activation of the RAAS9. Besides, Vitamin D has demonstrated a protective role in CVD by suppressing the inflammatory response, and reduces oxidative stress10. Accumulating epidemiologic studies have shown that serum 25(OH)D levels were associated with the incidence and progression of CVD11,12,13. These findings were largely based on general populations. Evidence regarding the relationships among vitamin D status and CVD events among individuals with diabetes is limited. Moreover, such a relationship must be clarified in this group of individuals, in whom vitamin D deficiency is particularly common. Furthermore, discrepancies in the studies on the relationship between serum vitamin D levels and CVD are observed because of various confounding factors. For example, one prospective study of 289 Danish patients with diabetes found that serum 25(OH)D deficiency was associated with an increased risk of all-cause and CVD mortality14, and another study of 698 Swedish patients with diabetes showed a marginally inverse association of serum 25(OH)D with mortality in men, but not in women15. Furthermore, many linear Mendelian randomized analyses have found that serum vitamin D levels are not associated with CVD risks16 and some studies also failed to demonstrate the beneficial effect of vitamin D supplementation on CVD outcomes17,18,19. We speculate that the contradictions may be related to gender, race, region, disease state and dietary habits20,21. Therefore, further studies are necessary to clarify whether serum levels of 25[OH]D are related to the CVD outcome in people with diabetes, particularly in the Chinese diabetic population. China was the country with the most diabetes in the world. From 1990 to 2024, the age-standardized incidence, prevalence and DALYs (Disability-adjusted life years) of overall diabetes in China are on the rise1. The public cognition level of diabetes in China is still at a relatively basic stage. Meanwhile, the age, race, region, eating habits and lifestyle influence the population vitamin D level a lot. At present, the relationship between vitamin D deficiency and CVD in the Chinese population is still unclear. Thus, understanding the relationship between vitamin D deficiency and cardiometabolic risk before the development of the disease is important to establish whether vitamin D supplementation can be used to prevent the development of CVD in patients with diabetes3.
We hypothesized that serum 25(OH)D levels were negatively associated with cardiovascular disease in the Chinese population with type 2 diabetes. In this study, we performed a retrospective analysis of the association of 25(OH)D with CVD and cardiometabolic risk factors in Chinese diabetics.
Methods
Study design
Initially, 2328 participants with T2DM aged over 18 were recruited from the First Affiliated Hospital of Zhengzhou University in China from January 2018 to December 2020. The exclusion criteria were as follows: metabolic syndrome (MetS) who cannot be diagnosed with T2DM, patients with acute diabetic complications such as ketoacidosis and hyperosmolar coma; tumor; acute infection; serious liver and kidney dysfunction; thyroid, parathyroid, and other endocrine gland-related diseases; autoimmune diseases; mental disease, and patients who are taking any medications known to affect vitamin D metabolism. In addition, we excluded participants who had missing laboratory results and questionnaire data. Finally, a total of 1378 patients with T2DM were enrolled (Fig. 1). The study was conducted in accordance with the principles of the Declaration of Helsinki and approved by the ethics committee of First Affiliated Hospital of Zhengzhou University.
Data collection
From the medical records of the individuals selected we collected the relative data: the history of medical conditions, family history of disease, presence of comorbidities associated with TD2M, medication use and other lifestyle factors. Smoking status was categorized into never smoking, current smoker, and previous smoker. Current smoking was defined as having smoked at least 100 cigarettes in one’s lifetime and is currently smoking cigarettes22. Alcohol intake was categorized into never drinking, current drinker and previous drinker. Alcohol drinking was defined as the consumption of alcohol ≥ 18 g during the past month23. In this study, anthropometric measurements were also collected in this study, such as weight, height, and blood pressure level. Weight and height were measured in accordance with the recommendations of the World Health Organization (WHO), with an accuracy to the nearest 0.1 kg and 0.1 cm, respectively, with the participants in light weight clothing without shoes. Body mass index (BMI) was calculated as follows: body weight (kg) divided by height square (m2). Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured using an automatic blood pressure meter after seating for at least 15 min and the average of the three measurements was recorded for calculate the mean BP. Cardiac function was assessed by echocardiography in all patients.
Laboratory measurements
All blood samples from patients who underwent overnight fasting were collected in the morning (around 6–7 a.m) so as to minimized the variation caused by specimen collection factors. An autobiochemical analyzer (Roche Diagnostic GmbH) was used to determine the serum concentrations of total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), fasting blood glucose (FBG), uric acid (UA), alanine aminotransferase (ALT), aspartate aminotransferase (AST), blood urea nitrogen (BUN), creatinine (Cr), γ-glutamyl transferase (GGT), alkaline phosphatase (ALP), total protein (TP), albumin (ALB), total bilirubin (TBIL), direct bilirubin (DBIL), thyroid stimulating hormone (TSH), parathormone (PTH), total triiodothyronine (TT3), free tetraiodothyronine (FT4), fasting plasma insulin, C-peptide and C-reactive protein (CRP). 25(OH)D serum levels were detected by electrochemical method. Glycated hemoglobin (HbA1c) levels were quantified using high-performance liquid chromatography. Insulin resistance was estimated on the basis of the homeostasis model assessment of insulin resistance (HOMAIR) by using the following formula: fasting insulin (mU/L)×FBG (mmol/L)/22.5.
Determination of carotid intima-media thickness (IMT)
Carotid ultrasonography was performed using a color Doppler ultrasonic diagnostic instrument. IMT was defined as the mean of the maximum thickness in the right and left sides of the common carotid artery, and IMT is the distance between the lumen-intima interface and the media adventitia interface. Carotid artery plaque (CAP) was defined as either a focal structure that encroached into the arterial lumen by at least 50% of the surrounding IMT value or a thickness of > 1.5 mm. The presence of CAP was defined as ≥ 1 plaque in any of the carotid arteries.
Definition of diagnostic criteria
T2DM was defined as FBG ≥ 7.0 mmol/L, HbA1c ≥ 6.5%, or the use of any anti-diabetic medication or self-reported history of diabetes based on the American Diabetes Association, as well as exclude other types of diabetes (e.g., Type 1 diabetes, LADA)24.
Sufficient, insufficient and deficient vitamin D statuses were defined as serum concentrations of 25(OH)D > 20.00 ng/mL, between 12.00 and 20.00 ng/mL, and < 12.00 ng/mL, respectively, according to the report released in 2010 by the Institute of Medicine25.
CVD was defined as a positive medical history of a cardiovascular event, including myocardial infarction, angina pectoris, carotid artery diseases, heart failure, and cerebrovascular disease (e.g. cerebral infarction, cerebral hemorrhage, ischemic and hemorrhagic stroke). Overweight is defined as 24 ≤ BMI < 28 kg/m2 and obesity is defined as a BMI26 of ≥ 28 kg/m2. Hypertension was defined as SBP ≥ 130 mmHg and DBP ≥ 85 mmHg or treatment with anti-hypertensive medication27. Osteoporosis was divided into osteopenia and osteoporosis in accordance with the WHO diagnostic criteria28.
For dyslipidemia, high (elevated) TC was defined as ≥ 5.20 mmol/L; high (elevated) TG was defined as > 1.70 mmol/L; high (elevated) LDL-C was defined as ≥ 3.40 mmol/L, and low (reduced) HDL-C was defined as < 1.29 mmol/L for women and < 1.04 mmol/L for men27.
Statistical analysis
Continuous variables with a normal distribution are expressed as the mean [standard deviation (SD)] and those with a non-normal distribution are expressed as the median (IQR: Q1–Q3). In contrast, categorical variables were reported as numbers and percentages (%). Differences in continuous variables among the groups were tested using a one-way analysis of variance for normally distributed variables or a Kruskal-Wallis test for non-normally distributed variables. Differences in categorical variables were analyzed by using a Chi-square test.
Univariate and multivariate logistic regressions were used to estimate the association of serum levels of 25(OH)D with CVD or cardiometabolic risk factors in people with type 2 diabetes. Hosmer-Lemeshow test was used to evaluate the goodness of fit effect of the model. Sensitivity analysis was conducted, and multivariate adjusted models were used to assess confounding variables. Confounding factors were screened on the basis of the p value when introducing different indexes into the regression models, and indexes with p value less than 0.1 were taken as covariates. Trend analyses were also conducted by entering the median value of each category of vitamin D status levels as a continuous variable in the models29. In addition, stratified analyses and interaction analyses by gender (male and female), age (< 45 years, 45–60 years, ≥ 60 years) and BMI (< 24, 24–28, ≥ 28) were further conducted.
Empower (R; www.empowerstats.com, X & Y Solutions Inc., Boston MA) and R (http://www.Rproject.org) were used for all statistical analyses27,30. Two-tailed p values less than 0.05 were considered statistically significant.
Results
Baseline characteristics of the study subjects
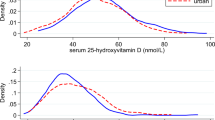
The present study population was composed of 1378 participants, with an average age of 50 years, and consisted of 946 males and 432 females. The median level of 25(OH)D for all subjects was 18.764 (13.20–22.15) ng/mL and we classified all patients into vitamin D adequate (≥ 20 ng/mL), vitamin D insufficiency (12–20 ng/mL) and vitamin D deficient groups (< 12 ng/mL) based on the serum 25(OH)D levels. The basic characteristics of the subjects were shown in Table 1. The sex composition, age, BMI, blood pressure, and alcohol consumption history were significantly different among the three groups (p < 0.05). There were no significant differences among the three groups in the duration of diabetes, the time of onset of diabetes, hypoglycemic treatment and the complications of diabetes (p > 0.05). Moreover, in terms of laboratory indicators, lipid metabolism (TG, HDL-C), blood glucose status (FBG, HbA1c, Insulin 120), renal function (BUN, Cr), liver function (AST, TP, ALB, TBIL, DBIL) and PTH were significantly different in various vitamin D statuses (p < 0.05).
The association between vitamin D status and cardiovascular disease in patients with T2DM
We then analyzed the association between cardiovascular disease and vitamin D status in diabetic patients by univariate and multivariate logistic regression analysis (Table 2). The association of vitamin D status with cardiovascular disease was measured by the odds ratio (OR). The Hosmer-Lemeshow goodness of fit tests was not significant for any of the logistic regression models (all p > 0.05), indicating that the goodness of fit of the models were good. In the analysis of the crude model (model 1), cardiovascular disease did not appear to be significantly associated with vitamin D levels before adjusting for confounders (p > 0.05). However, after adjusting for confounding factors by binary logistic regression, we found that 25(OH)D levels were significantly negatively associated with cardiovascular disease in type 2 diabetic patients [OR: 0.97 (0.94, 0.99), p = 0.0131]. Taking vitamin D-sufficient group (≥ 20 ng/mL) as reference, after adjusting for various confounding factors (model 2, model 3, model 4), the vitamin D-deficiency group (< 12 ng/mL) was still associated with a significantly higher risk of cardiovascular disease, with a 1.25-fold increased risk after adjusting for all potential confounders [OR: 2.25 (1.33, 3.79), p = 0.0023]. Further trend tests showed that the risk of cardiovascular disease in type 2 diabetes patients increased significantly with decreasing of vitamin D levels (p for trend = 0.0076).
We performed stratification analysis and interaction analysis to explore whether the association between vitamin D deficiency and a higher risk of cardiovascular disease was influenced by sex, age and BMI (Table 3). The results showed that after adjusting for relevant confounders, the association between vitamin D deficiency and an increased risk of cardiovascular disease was particularly significant in women [OR: 4.32 (1.54, 12.12), p = 0.0055], older adults (age > 60 years) [OR: 4.14 (1.10, 15.56), p = 0.0355], normal-weight (BMI < 24 kg/m2) [OR: 4.09 (1.51, 11.10), p = 0.0056] and obese subjects (BMI ≥ 28 kg/m2) [OR: 3.66 (1.03, 13.05), p = 0.0453]. Interaction analysis showed that sex, age and BMI did not significantly interfere with the association of vitamin D status and cardiovascular disease in type 2 diabetic patients. (all p > 0.05).
The relationship between vitamin D deficiency and cardiometabolic risk factors in diabetic patients
Finally, we analyzed the association of vitamin D levels with major cardiometabolic risk factors in diabetic patients. The results showed that vitamin D deficiency was strongly associated with a higher risk of cardiometabolic risk factors after adjusting for relevant confounders (Table 4). Compared with normal vitamin D levels, vitamin D deficiency was significantly associated with an increased risk of overweight/obesity [OR: 1.57 (1.10, 2.24), p = 0.0134], hypertension [OR: 1.81 (1.30, 2.51), p = 0.0004], hypertriglyceridemia [OR: 1.56 (1.12, 2.16), p = 0.0078] and reduced HDL-C [OR: 1.67 (1.19, 2.35), p = 0.0033]. However, no significant association was observed between vitamin D deficiency and hypercholesterolemia and higher LDL-C (all p > 0.05).
Discussion
In this cross-sectional study of Chinese adults with type 2 diabetes, we found that the serum 25(OH)D levels was significantly and negatively associated with CVD. The association was independent of traditional risk factors, including sex, age, BMI, lifestyle, and other confounding factors. Furthermore, vitamin D deficiency was strongly associated with a high risk of cardiometabolic risk factors, including overweight/obesity, hypertension, and dyslipidemia.
Vitamin D deficiency and insufficiency are common in people with diabetes. The average 25(OH)D concentration in the present study was 18.764 (13.20–22.15) ng/mL, which was lower than Chinese general population (22.4 ng/mL)31. Consistent with other studies, we found there are sex, age, BMI, blood pressure, and alcohol consumption history differences in various vitamin D statuses. Numerous epidemiological studies have explored the association among vitamin D status, CVD and mortality between older individuals and the general population, which support the association between higher serum 25 (OH)D levels and a lower risk of CVD morbidity and mortality32,33,34,35. Among patients with diabetes, who had a high prevalence of vitamin D deficiency and a high risk of CVD7, evidence is limited and inconclusive. Several large prospective cohort studies found that higher serum 25(OH)D levels were associated with reduced risk of cardiovascular outcomes among participants with diabetes6,21 Consistent with previous studies, we observed that 25(OH)D levels were significantly and negatively associated with CVD in patients with type 2 diabetic after adjusting for confounding factors. Further trend tests showed that the risk of CVD in patients with type 2 diabetes increased significantly with the decrease of vitamin D levels. Our findings indicate the importance of monitoring vitamin D status in the population with diabetes. Several potential mechanisms could explain the observed relationships between serum 25(OH)D levels and high risk of CVD. Vitamin D has anti-inflammatory and anti-mitotic actions that stabilize the endothelium, one of the key explanations for its cardiovascular-protective effects36,37. Furthermore, a previous study indicated that vitamin D is a negative regulator of the renin-angiotensin-aldosterone system (RAAS) in vivo38.
In addition, the significant relationships between vitamin D deficiency and increased risk of CVD was observed in women, older adults, and obese patients with diabetes. In general, vitamin D deficiency status is common among women, people with obesity, and older people. Cross-sectional studies showed that obesity is consistently characterized by lower 25(OH)D serum levels and a higher prevalence of vitamin D insufficiency and deficiency39. Individuals with obesity tend to expose their skin less to sunlight because of less physical activity outdoors, which could explain the high prevalence of hypovitaminosis D40. Another study shows an inverse correlation between the level of 25(OH)D and severity of coronary atherosclerosis in women and men over 70 years old41. Moreover, a negative interference of age with the concentrations of 25(OH)D is observed because the aged skin produces less vitamin D than the skin of younger people42. Vitamin D deficiency is especially common among elderly people, who often have less sun exposure (because of reduced outdoor activity) and limited capacity of the skin to produce vitamin D metabolites. Gender remarkably affects vitamin D status. Women are generally more prone to low 25(OH)D concentrations than men (possibly because of a positive correlation of 25(OH)D with testosterone levels). A study showed that lower 25(OH)D levels observed in females, as compared with males, play a more relevant role in conditioning the severity of coronary artery disease20. Our results of stratified and interaction analysis further confirm the reliable association between vitamin D deficiency and CVD.
Studies have shown that low vitamin D levels were associated with cardiometabolic risk markers such as hypertension43, atherogenic lipid profile44 and obesity45. Our study showed that vitamin D deficiency was strongly associated with a higher risk of cardiometabolic risk factors after adjusting for relevant confounders, which is consistent with some of the studies. Compared with normal vitamin D levels, vitamin D deficiency was remarkably associated with an increased risk of overweight/obesity, hypertension, hypertriglyceridemia, and reduced HDL-C. There is no consensus in the literature regarding the independent effects of 25(OH)D and obesity on cardiometabolic parameters. A study showed that vitamin D status is favorably associated with the cardiovascular risk factors in adults with obesity46. However, other study found no statistical significance in the association between 25(OH)D and body fat percentage47. Palacios observed a negative correlation between 25(OH)D and the percentage of body fat, but not a statistically significant correlation between 25(OH)D and BMI48. Notably, many confounding factors seem to influence these relationships. After adjusting for relevant confounders such as sex, age, BMI, SBP, DBP, smoking status, alcohol intake, new onset, duration of T2DM, hypoglycemic therapy, and osteoporosis, our study confirmed that a low serum 25(OH)D level was markedly associated with increased risk of overweight/obesity.
Hypertension is a serious risk factor for CVD. Our study confirmed that vitamin D deficiency was remarkably associated with an increased risk of hypertension. This result was consistent with previous studies49,50,51. The present study also showed that vitamin D deficiency was markedly associated with an increased risk of hypertriglyceridemia and reduced HDL-C. In addition, no significant association was observed between vitamin D deficiency and hypercholesterolemia, which is different from other studies. Farshad reported that vitamin D deficiency may be a risk factor for hypercholesterolemia, but not for hypertriglyceridemia (low HDL-c)46. The authors excluded patients with obesity resulting from endocrine disorders, which may explain the different results observed between their study and our study.
The strength of our study was that abundant information was available on basic characteristics, lifestyle habits, disease statues, medication and other covariates, which may enhance the validity of the conclusions through adjustment for a lot of potential confounding factors in this study. However, several limitations were worthy of consideration when interpreting our findings. First, as an observational study, this study did not conduct random sampling and causality cannot be determined. The participants of the study were Chinese patients with T2DM in a single center. Therefore, the present results might not be representative of the general T2DM population. Moreover, although many potential confounding factors were adjusted for analyses, we cannot exclude the role of residual confounding factors resulting from errors in the measurement of covariates and other important factors that may influence vitamin D levels (e.g. seasonal information on vitamin D, diet, vitamin D supplement information, physical activity, etc.) that were not assessed in the cohort.
Conclusion
In conclusion, our study suggested that serum 25(OH)D levels were significantly negatively associated with with CVD in Chinese type 2 diabetic patients. Vitamin D deficiency was significantly associated with a increased risk of overweight/obesity, hypertension, hypertriglyceridemia and reduced HDL-C. In the future, prospective multicenter follow-up cohort studies are worthy of implementation, and confounding factors not included in this study are fully considered, so as to further clarify the causal association between vitamin D levels and cardiovascular disease in diabetic population and the potential benefits of vitamin D supplementation for diabetic patients.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Ogurtsova, K. et al. IDF diabetes atlas: global estimates of undiagnosed diabetes in adults for 2021. Diabetes Res. Clin. Pract. 183, 109118 (2022).
Mosenzon, O. et al. CAPTURE: a multinational, cross-sectional study of cardiovascular disease prevalence in adults with type 2 diabetes across 13 countries. Cardiovasc. Diabetol. 20 (1), 154 (2021).
Strain, W. D. & Paldanius, P. M. Diabetes, cardiovascular disease and the microcirculation. Cardiovasc. Diabetol. 17 (1), 57 (2018).
Sarwar, N. et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375 (9733), 2215–2222 (2010).
Rao, K. S. S. et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N. Engl. J. Med. 364 (9), 829–841 (2011).
Zhang, P. et al. Association of serum 25-hydroxyvitamin D with cardiovascular outcomes and all-cause mortality in individuals with prediabetes and diabetes: results from the UK biobank prospective cohort study. Diabetes Care 45 (5), 1219–1229 (2022).
Harding, J. L. et al. Global trends in diabetes complications: a review of current evidence. Diabetologia 62 (1), 3–16 (2019).
Lee, J. H. et al. Vitamin D deficiency an important, common, and easily treatable cardiovascular risk factor? J. Am. Coll. Cardiol. 52 (24), 1949–1956 (2008).
Li, Y. C. et al. 1,25-Dihydroxyvitamin D(3) is a negative endocrine regulator of the renin-angiotensin system. J. Clin. Investig. 110, 229–238 (2002).
Ferder, M., Inserra, F., Manucha, W. & Ferder, L. The world pandemic of vitamin D deficiency could possibly be explained by cellular inflammatory response activity induced by the renin-angiotensin system [Internet]. Am. J. Physiol. Cell. Physiol. 304, C1027 (2013).
Zhang, R. et al. Serum 25-hydroxyvitamin D and the risk of cardiovascular disease: dose-response meta-analysis of prospective studies. Am. J. Clin. Nutr. 105 (4), 810–819 (2017).
Yang, J., Ou-Yang, J. & Huang, J. Low serum vitamin D levels increase the mortality of cardiovascular disease in older adults: A dose-response meta-analysis of prospective studies. Medicine (Baltim). 98 (34), e16733 (2019).
Zittermann, A. et al. Vitamin D and cardiovascular disease: an updated narrative review. Int. J. Mol. Sci. 22 (6) (2021).
Joergensen, C. et al. Vitamin D levels and mortality in type 2 diabetes. Diabetes Care 33 (10), 2238–2243 (2010).
Jennersjo, P. et al. A prospective observational study of all-cause mortality in relation to serum 25-OH vitamin D3 and parathyroid hormone levels in patients with type 2 diabetes. Diabetol. Metab. Syndr. 7, 53 (2015).
Manousaki, D. et al. Mendelian randomization studies do not support a role for vitamin D in coronary artery disease. Circ. Cardiovasc. Genet. 9 (4), 349–356 (2016).
Scragg, R. et al. Effect of monthly high-dose vitamin d supplementation on cardiovascular disease in the vitamin D assessment study: a randomized clinical trial. JAMA Cardiol. 2 (6), 608–616 (2017).
Manson, J. E. et al. Vitamin D supplements and prevention of cancer and cardiovascular disease. N. Engl. J. Med. 380 (1), 33–44 (2019).
Djousse, L. et al. Supplementation with vitamin d and omega-3 fatty acids and incidence of heart failure hospitalization: VITAL-heart failure. Circulation 141 (9), 784–786 (2020).
Verdoia, M. et al. Impact of gender difference on vitamin D status and its relationship with the extent of coronary artery disease. Nutr. Metab. Cardiovasc. Dis. 25 (5), 464–470 (2015).
Wan, Z. et al. Association of serum 25-hydroxyvitamin D concentrations with all-cause and cause-specific mortality among individuals with diabetes. Diabetes Care 44 (2), 350–357 (2021).
Xu, Y. et al. Prevalence and control of diabetes in Chinese adults. JAMA 310 (9), 948–959 (2013).
Xiao, P. et al. Adequate 25-hydroxyvitamin D levels are inversely associated with various cardiometabolic risk factors in Chinese children, especially obese children. BMJ Open Diabetes Res. Care 8 (1) (2020).
Feng, X. et al. Influence of serum albumin on HbA1c and HbA1c-Defined glycemic status: A retrospective study. Front. Med. (Lausanne) 8, 583093 (2021).
Ross, A. C. et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of medicine: what clinicians need to know. J. Clin. Endocrinol. Metab. 96 (1), 53–58 (2011).
Weir, C. B. & Jan, A. BMI Classification Percentile and Cut Off Points (2023).
Feng, X. et al. The association between hyperuricemia and obesity metabolic phenotypes in Chinese general population: a retrospective analysis. Front. Nutr. 9, 773220 (2022).
Prevention and management of osteoporosis. World Health Organ. Tech. Rep. Ser. 921, 1–164, back cover (2003).
Park, S. Y. et al. Association of coffee consumption with total and cause-specific mortality among nonwhite populations. Ann. Intern. Med. 167 (4), 228–235 (2017).
Tang, H. et al. Circulating levels of IL-33 are elevated by obesity and positively correlated with metabolic disorders in Chinese adults. J. Transl. Med. 19 (1), 52 (2021).
Bai, K. et al. Serum 25-hydroxyvitamin D status of a large Chinese population from 30 Provinces by LC-MS/MS measurement for consecutive 3 years: differences by age, sex, season and Province. Eur. J. Nutr. 62 (3), 1503–1516 (2023).
Anderson, J. L. et al. Relation of vitamin D deficiency to cardiovascular risk factors, disease status, and incident events in a general healthcare population. Am. J. Cardiol. 106 (7), 963–968 (2010).
Crowe, F. L. et al. Non-linear associations of 25-hydroxyvitamin D concentrations with risk of cardiovascular disease and all-cause mortality: results from the health improvement network (THIN) database. J. Steroid Biochem. Mol. Biol. 195, 105480 (2019).
Hutchinson, M. S. et al. Low serum 25-hydroxyvitamin D levels are associated with increased all-cause mortality risk in a general population: the Tromso study. Eur. J. Endocrinol. 162 (5), 935–942 (2010).
Virtanen, J. K. et al. Association of serum 25-hydroxyvitamin D with the risk of death in a general older population in Finland. Eur. J. Nutr. 50 (5), 305–312 (2011).
Chen, Y. et al. 1,25-Dihydroxyvitamin D(3) suppresses inflammation-induced expression of plasminogen activator inhibitor-1 by blocking nuclear factor-kappaB activation. Arch. Biochem. Biophys. 507 (2), 241–247 (2011).
Venkatesh, B. & Nair, P. Hypovitaminosis D and morbidity in critical illness: is there proof beyond reasonable doubt? Crit. Care 18 (3), 138 (2014).
Oh, J. et al. 1,25(OH)2 vitamin D inhibits foam cell formation and suppresses macrophage cholesterol uptake in patients with type 2 diabetes mellitus. Circulation 120 (8), 687–698 (2009).
Ekwaru, J. P. et al. The importance of body weight for the dose response relationship of oral vitamin D supplementation and serum 25-hydroxyvitamin D in healthy volunteers. PLoS One 9 (11), e111265 (2014).
Pourshahidi, L. K. Vitamin D and obesity: current perspectives and future directions. Proc. Nutr. Soc. 74 (2), 115–124 (2015).
Dziedzic, E. A., Przychodzen, S. & Dabrowski, M. The effects of vitamin D on severity of coronary artery atherosclerosis and lipid profile of cardiac patients. Arch. Med. Sci. 12 (6), 1199–1206 (2016).
Lips, P. Vitamin D physiology. Prog. Biophys. Mol. Biol. 92 (1), 4–8 (2006).
Ferrario, C. M. & Strawn, W. B. Role of the renin-angiotensin-aldosterone system and proinflammatory mediators in cardiovascular disease. Am. J. Cardiol. 98 (1), 121–128 (2006).
Gagnon, C. et al. Low serum 25-hydroxyvitamin D is associated with increased risk of the development of the metabolic syndrome at five years: results from a National, population-based prospective study (The Australian diabetes, obesity and lifestyle study: AusDiab). J. Clin. Endocrinol. Metab. 97 (6), 1953–1961 (2012).
Lamendola, C. A. et al. Relations between obesity, insulin resistance, and 25-hydroxyvitamin D. Am. J. Clin. Nutr. 95 (5), 1055–1059 (2012).
Amirkhizi, F. et al. Vitamin D status is favorably associated with the cardiovascular risk factors in adults with obesity. Clin. Nutr. ESPEN 46, 232–239 (2021).
Dominoni, L. et al. Vitamin D is associated with body composition and fat intake, but not with cardiometabolic parameters in adults with obesity. Nutr. Res. 105, 97–104 (2022).
Palacios, C. et al. Determinants of vitamin D status among overweight and obese Puerto Rican adults. Ann. Nutr. Metab. 60 (1), 35–43 (2012).
Yilmaz, S. et al. The relationship between vitamin D levels and nondipper hypertension. Blood Press. Monit. 20 (6), 330–334 (2015).
Del, P. R. et al. Vitamin D and blood pressure control among hypertensive adults: results from NHANES 2001–2014. J. Hypertens. 38 (1), 150–158 (2020).
Mokhtari, E., Hajhashemy, Z. & Saneei, P. Serum vitamin D levels in relation to hypertension and pre-hypertension in adults: a systematic review and dose-response meta-analysis of epidemiologic studies. Front. Nutr. 9, 829307 (2022).
Acknowledgements
We would like to thank the participants in this study.
Funding
This work was supported by the National Natural Science Foundation of China (number 82102281), the Natural Scientific Foundation of Hunan Province (Grant Number 2021JJ40867, number 2021JJ40893) and the National Key Research and Development Program of China (2022YFC2505200).
Author information
Authors and Affiliations
Contributions
LT, YW and HT designed and revised the study; YW, WL, DX, RC and NZ conducted the research; HT, HZ and WL analyzed the data; HT and NZ wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the First Affiliated Hospital of Zhengzhou University. Written informed consent to participate was obtained from all participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, N., Wang, Y., Li, W. et al. Association between serum vitamin D level and cardiovascular disease in Chinese patients with type 2 diabetes mellitus: a cross-sectional study. Sci Rep 15, 6454 (2025). https://doi.org/10.1038/s41598-025-90785-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-90785-8
Keywords
This article is cited by
-
Exploring 1,3,4-oxadiazolyl sulfide derivatives as antidiabetic candidates: synthesis, antioxidant activity, SAR-study, molecular docking, and DFT-insights
BMC Chemistry (2025)
-
Weight adjusted waist index is a superior obesity index for predicting arterial stiffness in type 2 diabetes mellitus
Scientific Reports (2025)
-
Optimizing cardiac radiation therapy in left breast cancer patients using an intelligent hybrid fuzzy model and differential genetic evolution
Cluster Computing (2025)
-
The associations of insomnia symptoms and clinical features as well as blood metabolic parameters in adolescents with major depressive disorders
European Archives of Psychiatry and Clinical Neuroscience (2025)
-
Creatinine as a predictor of proliferative diabetic retinopathy among patients with type 2 diabetes mellitus: a systematic review and meta-analysis
International Urology and Nephrology (2025)