Abstract
Late-onset cardiotoxicity induced by anthracyclines occurs years to decades after completion of anti-cancer therapy and is associated with increased morbi-mortality of cancer survivors. Chemotherapy at the time of treatment probably causes cardiac damages for which the juvenile heart compensate. Co-morbidities happening in the adulthood such as type 1 diabetes (DT1), affect the heart and thus can unmask chemotherapy induced cardiotoxicity. To prove our hypothesis, we induced hyperglycemia [Streptozotocin treatment (STZ), 50 mg/kg/day for 5 days] in 11 weeks old mice who previously received doxorubicin treatment (Dox, 3 mg/kg) when they were six-weeks old. Interestingly, streptozotocin-induced hyperglycemia in Dox-pretreated mice (Dox-STZ) induced a higher mortality (p < 0.05) and more severe cardiac dysfunction (p < 0.0001) when compared with mice receiving Dox or STZ alone. Apoptosis evaluated by caspase 3 protein expression and Bax/Bcl2 genes expression was higher in Dox-STZ mice compared to STZ or Dox alone. While Dox and STZ independently induced capillary rarefaction, cardiomyocytes atrophy was only induced by STZ. Furthermore, Sirius-red staining of cardiac sections showed higher fibrosis levels (p < 0.0001) in Dox-STZ compared to Dox or STZ alone. All together, these results demonstrate that STZ precipitates and unmask cardiac dysfunction in previously treated Dox animals.
Similar content being viewed by others
Introduction
Anthracycline-based chemotherapy is one of the most commonly used anti-neoplastic regimens1,2. Although highly effective, anthracyclines are cardio-toxic which may affect up to 39% of cancer patients3. Late-onset anthracycline cardiotoxicity occurs years to decades after anthracycline treatment has been completed4,5 which is a lifelong threat especially in cancer survivors who have a long life-expectancy after successful antineoplastic treatment. Late-onset cardiac failure may be the result of the inability of the reduced number of healthy myocytes to fulfill after a long-term asymptomatic period the demands of additional cardiovascular strain such as diabetic cardiomyopathy.
Moreover, diabetes has been associated with poor outcomes and overall survival in patients with cancer who were treated with anthracyclines-based chemotherapy6,7. It is reasonable to expect that a cancer patient with diabetic cardiomyopathy would be more susceptible to the anthracyclines-induced cardiac damage due to the pre-existing cardiac dysfunction8. However, the role of diabetes in the initiation or unmasking sub-clinical cardiotoxicity and the exact mechanisms on how the additional stress from diabetes, remain largely unexplored.
Few experimental studies showed that doxorubicin pharmacokinetics are impaired in diabetic heart leading to increased fat accumulation and decreased renal clearance9,10,11,12. Other mechanisms involve decrease of antioxidant defense, defective β-oxidation of fatty acids followed by energy depletion13,14. However, the role of diabetes-induced cardiac atrophy and capillary rarefaction in anthracyclines-induced cardiotoxicity has never been explored yet. The pathophysiology of cardiomyocyte injuries by diabetes and anthracyclines-induced cardiotoxicity may be commonly linked to oxidative stress, apoptosis, fibrosis, inflammation and metabolic remodeling15,16,17,18. Doxorubicin undergoes redox cycling by mitochondrial complex I NADH dehydrogenase, leading to oxidative stress, membrane lipid peroxidation, mitochondrial dysfunction, and altered cardiac gene expression collectively leading to cardiomyocyte death19. Diabetic cardiomyopathy involves coronary microcirculation defects, hormonal dysregulation, all leading to a diastolic and then a systolic cardiac dysfunction20,21,22.
We hypothesize that anthracyclines could induce aberrant cell signaling and oxidative stress overlapping with diabetes and leading to a vicious cycle liable to expedite and to exacerbate the process of heart failure. Using an in vivo juvenile mice model of doxorubicin induced cardiotoxicity and streptozotocin induced hyperglycemia together with an in vitro model of cardiomyocytes subjected to doxorubicin and hyperglycemia, we aim to demonstrate that streptozotocin inducing hyperglycemia thus mimicking a type 1 diabetes will unmask doxorubicin induced cardiotoxicity.
Material and methods
Animal experimental procedures
Animal handling practice during experimentation was followed and approved by the Animal Ethics Committee Lariboisière–Villemin according to the guidelines of the Laboratory Animal Ethic Regulation (APAFIS#12111-2017110817428853V3). The ARRIVE rules and guidelines were taken into consideration by the authors.
Mice were housed with a 12/12 h light–dark cycle and with ad libidum access to food and water. All experimental procedures were performed in accordance with the Directive 2010/63/eu of the European Union.
Six-week old male SWISS mice (Janvier) were injected intraperitonealy, four times every 5 days, with either doxorubicin (Sigma-Aldrich, Saint Quentin Fallavier, France; Dox; n = 34) or saline (n = 24). The first 2 doses of doxorubicin were at a concentration of 1 mg/kg, and the last 2 injections were at 0.5 mg/kg23. Control animals were injected with an equivalent volume of saline. Animals were observed daily and weighed weekly. Two weeks after the last injection, streptozotocin-induced hyperglycemia was initiated.
It was induced as previously described21. Saline or Dox treated mice received daily intra-peritoneal injections for 5 days with streptozotocin (STZ) (40 mg/kg/d) dissolved in sodium citrate buffer (Sigma-Aldrich, Saint Quentin Fallavier, France). Control animals received sodium citrate buffer injections. Three days after the last injection, whole-blood glucose was monitored using the Euroflashmonitor (LifeScan, Milpitas, CA, USA) in fasted mice. STZ-treated mice with blood glucose concentration higher than 15 mM were considered diabetic. DT1 was induced for a period of 6 weeks.
At the end of the protocol, mice were sacrificed with an i.p. overdose of pentobarbital (50 mg/kg) injection. The hearts were arrested in diastole by an intravenous injection of saturated KCl, they were quickly removed, weighed and cut transversely at the ventricles equator. The upper parts of the heart were mounted, frozen in isopentane precooled with liquid nitrogen, and kept at -80 °C until use, as previously described24.
Echocardiography
Echocardiography was performed on lightly sedated mice with ketamine (80 mg/kg) as previously described25. The thickness of the left ventricle LV and fractional shortening were measured using a GE Vivid-7 machine (General Electric Medical Systems, Paris, France) equipped with an 8–14 MHz linear transducer. Echocardiography was performed 5 times, before and after treatments (Dox or STZ) and at the end of the protocol (Fig. 1A).
Streptozotocin-induced hyperglycemia aggravates cardiac dysfunction and mortality induced by doxorubicin. (A) Schematic representation of the protocol used in vivo. (B) Kaplan-Meyer plot of mice surviving during the in vivo experimental protocol in the 4 groups of mice treated with saline (Ctl), doxorubicin (Dox), streptozotocin (STZ) or both (Dox-STZ). (C) Cardiac function evaluated by fractional shortening measured by transthoracic echocardiography (TTE) of mice after doxorubicin treatment (represented arrow Dox on the x-axis) and type 1 diabetes (represented by Stz on the x-axis). (D) Cleaved caspase 3 protein expression in the cardiac tissue evaluated by western blot. (E, F) mRNA expression of Bax and Bcl2, respectively measured in the cardiac tissue par RT-qPCR. *p < 0.05, **p < 0.01 and ***p < 0.001.
In vitro studies
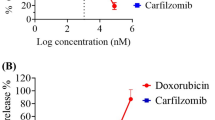
Rat cardiomyocytes H9C2 cells (Sigma-Aldrich, 88092904) were cultured in DMEM (Sigma-Aldrich, Saint Quentin Fallavier, France) supplemented with 10% of fetal bovine serum (Fisher Scientific, Illkirch, France) and 1% of penicillin–streptomycin antibiotics (Sigma-Aldrich, Saint Quentin Fallavier, France), at 37 °C and 5% Co2. Plated cardiomyocytes were starved (2% serum) for 10–12 h before treatment with Dox (1 µM) and/or glucose (33 mM) for 24 h. Cell survival was assessed by counting alive cells using Malassez counting-chamber. The cells were then centrifuged (300 g, 5 min) and the pellet used for protein and RNA preparation. All the treatments were done in triplicates and the experiments were repeated three times.
For cell morphology assessment, cells were grown on coverslips which were fixed at the end of the protocol with 4% paraformaldehyde for 10 min following a thorough wash with 1% sterile phosphate buffered saline (PBS). This was followed by immunofluorescence staining.
RNA preparation and real-time quantitative RT-PCR
RNA were prepared from mice heart tissue using QIAGEN RNeasy Mini Kit (Qiagen, Courtaboeuf, France) according to manufacturer instructions and as previously described26. RNA concentration was determined using the ND-100 spectrophotometer (Nanodrop, Thermo Fischer Scientific Waltham, USA). The cDNA synthesis was performed using the QuantiTect® Reverse Transcription Handbook Kit (Qiagen, Courtaboeuf, France). Real-time quantitative RT-PCR was performed using 1.25 ng cDNA and 10 nmol of specific primers (Supplemental Table 1) for amplification of the genes of interest using the LightCycler 96 thermal cycler (Roche Diagnostics France SAS, Meylan, France).
Protein preparation and western blot
Proteins were prepared from mice heart tissue and H9C2 cells in RIPA lysis buffer (0.02M Tris HCl pH7.5, 0.1M KCl, 1mM EDTA, 1mM EGTA, 1mM DTT, 0.04M Β-glycérophosphate, 2mM sodium Ortho-Vanadate, 1mM PMSF, 0.01Mm NaF) in the presence of anti-proteases and anti-phosphatases (Sigma-Aldrich, Saint Quentin Fallavier, France). Protein yield was measured by spectrophotometry using the Pierce BCA Protein Assay kit (ThermoFischer Scientific, France). Proteins (20µg) were heated at 99 °C for 7 min before being separated by SDS-page electrophoresis using on a 4–20% polyacrylamide gel (Biorad, Hercules, USA) and transferred to 0.2-μm nitrocellulose membrane. Nitrocellulose blots were blocked and incubated with primary and secondary antibodies (Supplemental Table 2). Chemiluminescence was measured using AZURE (Azure Biosystems) and measured using MultiGauge V2.02 software (Fuji).
Immunostaining
Double immunostaining was performed on cryostat heart tissue sections using vinculin and caveolin-1 antibodies. Phalloidin antibody was used for H9C2 immunostaining. All antibodies are listed in Supplemental Table 2.
Cardiac fibrosis
Cardiac cryosections (7 μm) were stained with Sirius red (0.5% in saturated picric acid). Fibrosis was semi-quantified, as previously described24 with a severity scale ranging from slight fibrosis (1) to high collagen accumulation (5). Fibrosis quantification was double-blinded.
Statistical analyses
All values are expressed as mean ± SEM. Statistical comparisons were performed using GraphPad Prism software (version 6.00 for Windows, GraphPad Software, La Jolla California, USA www.graphpad.com). Variables comparison was done using one-way ANOVA and Dunn’s correction or two-way ANOVA with Bonferroni correction. Survival rate was analyzed by the Kaplan–Meier method with the log-rank test. Statistical significance was considered when p < 0.05.
Results
Doxorubicin induces acute cardiac dysfunction and hyperglycemia
One week after the last injection of doxorubicin, mice had an echocardiography to detect early cardiotoxicity, defined as minus 10% in fractional shortening (FS) when compared to the echocardiography done before the onset of doxorubicin treatment. Ten mice (29%) presented with an acute doxorubicin induced cardiotoxicity (Supplemental Figure 1A). Only mice presenting with no cardiac dysfunction were included in the experimental DT1 like induction.
Interestingly, doxorubicin induced an increase in glycaemia (p < 0.05) when compared to saline treated mice (Supplemental Figure 1B). A concomitant decrease of GLUT4 protein expression in the cardiac tissue of doxorubicin treated mice was observed (p < 0.05), with no change in GLUT1 protein expression (Supplemental Figure 1C). However, this hyperglycemia induced by doxorubicin wasn’t exacerbated post STZ treatment (Supplemental Figure 2).
STZ-induced hyperglycemia aggravates cardiac dysfunction and mortality induced by doxorubicin
Doxorubicin and STZ-induced hyperglycemia independently induced mice mortality (Fig. 1B). Interestingly, STZ-induced hyperglycemia induction in doxorubicin pretreated mice induced a higher mortality in mice. STZ-induced hyperglycemia, two weeks after induction, induced a decrease in FS in doxorubicin treated mice (Fig. 1C) probably involved in the highest percentage of death observed in the Dox-STZ experimental group. Diabetes induced a decrease in body weight, heart and liver weight with no added effect due to doxorubicin treatment (Table 1). At the end of the protocol, no significant difference in systolic cardiac function was observed between the four experimental groups (Table 1), probably associated with a bias induced by death of diseased mice. Evolution of echocardiographic parameters from baseline to the end of the protocol are illustrated in Supplemental Table 3 & 4.
We observed an increase in active caspase 3 protein level and the pro-apoptotic Bax mRNA level in the Dox-STZ group compared to control group (p < 0.05, Fig. 1D, E) whereas the anti-apoptotic Bcl2 mRNA levels remained stable (Fig. 1F). All together, these results indicated an increased apoptosis in the cardiac tissue of the Dox-STZ mice group.
Furthermore, in vitro experiments showed that doxorubicin or hyperglycemia treatments induced cardiomyocytes mortality which was further higher when the cells were incubated with both doxorubicin and high glucose concentration (Fig. 2A).
Effect of doxorubicin and glucose on cardiomyocytes survival and size. (A) H9C2 Cardiomyocytes mortality 24h after doxorubicin (Dox), Glucose (Glc) or both (DoxGlc) treatment. (B, C) cross section of cultured H9C2 labeled with phalloidin (green). Ctl represent the non-treated condition. *p < 0.05, **p < 0.01 and ***p < 0.001 compared to the “Ctl” condition. #p < 0.05 compared to the “Dox” condition.
STZ-induced hyperglycemia and not doxorubicin induced cardiomyocytes atrophy
Cardiac cachexia assessed by echocardiography showed that doxorubicin and type 1 diabetes individually decreased intraventricular septum diameter when compared to control mice (Table 1). This decrease was aggravated when doxorubicin treatment was followed by STZ-induced hyperglycemia (p < 0.001) (Table 1).
Interestingly, cardiomyocytes diameter measured on cardiac sections stained with vinculin antibody showed that only diabetes induced cardiomyocytes atrophy (Fig. 3A, B). Whereas no change in Atrogin 1 protein levels was observed between the experimental mice groups (data not shown), an increase of MurF1 protein levels was observed in the cardiac tissue of STZ treated mice (Fig. 3C). These effects of diabetes on cardiomyocyte atrophy is blunted when the mice were pretreated by doxorubicin (Fig. 3A, B).
Effect of streptozotocin-induced hyperglycemia and doxorubicin on cardiomyocytes atrophy and capillary rarefaction. (A) Double immunostaining of vinculin (green) and caveolin-1 (red) proteins on cardiac sections of saline (Ctl), doxorubicin (Dox), streptozotocin (STZ) and both doxorubicin and diabetes (Dox-STZ) treated mice. Histograms indicate the cross-sectional area of myocytes (B) and the capillary/cardiomyocyte ratio (D) measured in the 4 groups. (C,E) protein expression of MuRF-1 and VEGF-A, respectively, measured in the cardiac tissue par western blot. *p < 0.05, **p < 0.01 and ***p < 0.001 compared to the “Ctl” condition or otherwise specified. Scale, 100 µm.
High glucose concentration had the same effect in vitro by inhibiting the trophicity of cultured H9C2 (Fig. 2B, C). However, doxorubicin induced cardiomyocytes atrophy in vitro which was not observed in vivo (Fig. 2B, C).
Doxorubicin and STZ-induced hyperglycemia independently induced capillary rarefaction
Each stress independently induced a decrease in the number of capillaries per cardiomyocyte (Fig. 3A, D) without an aggravation of this effect when the mice were affected with both stresses (Fig. 3D). In addition, a decrease in cardiac VEGF-A protein level was observed in response to doxorubicin and STZ (Fig. 3E).
STZ-induced hyperglycemia aggravates cardiac fibrosis in doxorubicin treated mice
Cardiac fibrosis quantified on Sirius red stained cardiac sections showed that doxorubicin or STZ-induced hyperglycemia induced increased collagen deposition (Fig. 4A). Interestingly, fibrosis was aggravated in STZ-induced hyperglycemia in doxorubicin pretreated mice (Fig. 4B). We also observed an increase in fibronectin protein expression and a decreased laminin protein expression in Dox-STZ mice group (Supplemental Figure 3A & B). Fibronectin upregulation was driven by doxorubicin but not by hyperglycemia as no significant change was observed in STZ group not receiving doxorubicin. Furthermore, we observed an increase in the pro-fibrotic galectin-3 protein levels in the Dox-STZ mice group (Fig. 4C) and no change in CD68 protein level whatever the experimental group (Fig. 4D).
Streptozotocin-induced hyperglycemia aggravates cardiac fibrosis in doxorubicin treated mice. (A) Distribution of fibrillar collagens in the left ventricle of a mouse examined by polarized light microscopy after Sirius Red staining. (B) Semi-quantitative analysis of cardiac fibrosis. (C,D) protein expression of Galectin 3 and CD68, respectively, in the cardiac tissue. *p < 0.05, **p < 0.01 and ***p < 0.001 compared to the “Ctl” condition. Scale, 100 µm.
Discussion
Our study demonstrated that type 1 diabetes unmasks infra-clinical cardiotoxicity induced by doxorubicin treatment. The mechanisms by which type 1 diabetes precipitates doxorubicin induced cardiotoxicity involved to an increased cardiomyocyte death and consequently extracellular matrix remodeling thus inducing contractile cardiac dysfunction and ultimately death (Fig. 5).
Cancer and diabetes mellitus are two leading causes of death in the world representing health and economical concerns (WHO;27). Epidemiological studies have demonstrated a strong link between certain cancers and diabetes mellitus28,29, with cancer increasing diabetes incidence30 and vice versa31,32.
The lifelong risk of cardiotoxicity is complex and multifaceted. Key roles have been attributed to mitochondrial dysfunction33, anthracyclines metabolism34, inflammation and fibrosis35 together with myofibril disorganization36, cardiomyocyte senescence and apoptosis37. Late-onset cardiotoxicity mechanisms are difficult to understand. One can speculate that infra-clinical cardiotoxicity is already present in the heart of patients after the termination of their treatment with anthracyclines as recently confirmed by meta-analysis showing that clinically overt cardiotoxicity occurred in 6% of patients, whereas subclinical cardiotoxicity developed in 18% of patients6. Our study emphasizes the potential association of anthracycline cardiotoxicity with another stressor, here represented by type 1 diabetes, which unmask the infra-clinical toxicity.
Relationship between cancer treatment induced cardiotoxicity and diabetes has been previously investigated. Studies showed that preexisting diabetes in cancer patients who will undergo a chemotherapy treatment will have higher incidence of cardiovascular events38. This was confirmed by an experimental study demonstrating an increased sensitivity of the diabetic heart to doxorubicin treatment7,11.
Our study is novel and shows for the first time the consequence of type 1 diabetes on a pretreated heart with anthracyclines. Importantly, it has been shown that cancer and its treatment can induce later on diabetes mellitus39,40. Furthermore, it has been shown that -Pancreatic cancer increases diabetes incidence41. The relation between cancer, anthracyclines and diabetes is even more complex. Indeed, Type 1 and type 2 Diabetes were shown to be associated with increased risk of cancer incidence42,43 and can worsen mortality induced by cancer44.
In our study, one week after doxorubicin treatment completion, twenty percent of the mice presented with acute cardiotoxicity (decrease of more than 10% of FS). This result is in accordance with what has been published concerning juvenile model of cardiotoxicity23. In addition, doxorubicin acutely induced hyperglycemia which wasn’t aggravated later on when type 1 diabetes was induced, which confirms the acute and transient state of this increase in blood glucose. It has been described that cytotoxic chemotherapy is associated with transient and acute hyperglycemia in patients45,46,47. This increase in blood glucose was assigned to acute beta-cell damage and a drop in protein synthesis causing an increase demand in gluconeogenic precursors45,46.
In accordance with our results, an experimental study showed that doxorubicin induces hyperglycemia and insulin resistance in rats48. Downregulation of the AMPK signaling leading to a decrease in GLUT-4 expression, in the skeletal muscle of doxorubicin treated rats was suggested by the authors to be responsible of doxorubicin induced glucose intolerance. One week after doxorubicin treatment, hyperglycemia was associated with a decreased expression of GLUT4 in mice heart (Supplemental Figure 1) with no change in AKT and insulin receptors expression (data not shown), as previously described48. Together with cardiac atrophy and cachexia, decreased GLUT-4 expression in the heart and probably in skeletal muscles explain doxorubicin induced hyperglycemia even if we cannot exclude any doxorubicin toxic effect on pancreatic cells.
Hyperglycemia itself contributes to cardiac toxicity as demonstrated by increased cardiomyocytes mortality when incubated in vitro with high glucose concentration. High glucose induced cardiotoxicity has previously been described in vitro49 and in vivo50. Furthermore, it has been shown that hyperglycemia increases doxorubicin accumulation in the heart tissue11,51. Even if we didn’t observe a higher glycaemia when type 1 diabetes was induced in doxorubicin pretreated mice compared to doxorubicin treated mice without type 1 diabetes, our findings showed, in vitro and in vivo, that combination of doxorubicin treatment and hyperglycemia aggravated cardiomyocytes apoptosis and cardiac dysfunction.
Furthermore, it has been shown that metformin, an oral antihyperglycemic drug used for type 2 diabetes, reduces the risk of cancer in patients with diabetes mellitus52. Very recently, Metformin combination with neoadjuvant chemotherapy was shown to be safe, tolerable, and to improves non-significantly the clinical and pathological tumor response of breast cancer patients53. Metformin is cardio-protective in a context of myocardial ischemia54 and recently against doxorubicin-induced cardiotoxicity55. The mechanism by which metformin prevent cardiotoxicity induced by doxorubicin seems to be partially linked to decreased inflammation and apoptosis in the heart56,57,58. Unfortunately, none of these studies were done in a context of diabetes which might dysregulates the balance favoring cardio-protection induced by metformin.
Another very promising drugs in this context are the Sodium-glucose cotransporter 2 (SGLT2) inhibitors (e.g., gliflozin, empagliflozin, dapagliflozin), the novel oral glucose-lowering medication, which were shown to be cardioprotective against doxorubicin treatment59,60,61. This cardioprotective effect was also demonstrated in a doxorubicin and diabetic mouse model62. Furthermore, two recent retrospective studies showed a beneficial association between SGLT2 inhibitors use and decreased mortality, cardiovascular events and rehospitalization for cancer patients treated with anthracyclines63,64.
Moreover, preclinical studies evaluating concomitant use of SGLT-2 inhibitors with doxorubicin in cancer models demonstrated a beneficial and synergic effect of SGLT-2 inhibitors on tumor growth65,66. These studies further demonstrated that the use of SGLT2-inhibitors allows for the use of lower doses of doxorubicin thus preventing its side effects.
Another factor precipitating cardiac dysfunction and mortality in mice receiving both doxorubicin and streptozotocine in our study, is cardiac fibrosis. Cardiac fibrosis induced cardiac dysfunction has been largely investigated in the past67. Doxorubicin and streptozotocin induce cardiac fibrosis associated with cardiac dysfunction21,59. Interestingly, cardiac fibrosis induced cardiac dysfunction is a late-onset effect of doxorubicin which can appear during the recovery phase, weeks after treatment termination35. Extracellular matrix proteins profiling evaluated in cardiac tissues was similar to what was previously described with doxorubicin inducing collagen 1, 3 and fibronectin expression but decreasing laminin expression thus disrupting the structural and functional maintenance of cardiac cells68,69.
Interestingly, cardiac dysfunction and mortality in hyperglycemic and doxorubicin treated mice wasn’t associated with cardiomyocytes atrophy. This is surprising as doxorubicin and diabetes alone induce cardiomyocytes atrophy as shown by other studies21,70. We only observed cardiomyocytes atrophy in diabetic mice not receiving doxorubicin. This was associated with increased MuRF1 expression71,72. One can speculate that maintained cardiomyocytes size in diabetic mice receiving doxorubicin is an adaptive response of the resting cardiomyocytes following cardiac apoptosis, and should be further investigated in the future.
Although our study is novel and translational with clinical relevance for cancer survivors presenting higher risk of developing later on cardiovascular comorbidities such as diabetes mellitus which can unmask a subclinical cardiotoxicity induced by chemotherapy treatment, it presents with some limitations. First of all, only type 1 diabetes was mimicked by STZ-induced hyperglycemia despite the fact that it represents less than 10% of diabetes mellitus. Second, only cardiomyocyte cell lines, and not primary cells, were used. Third, our model doesn’t include cancer which itself can induce cardiac changes leading to cardiac dysfunction73. Fourth, insulin resistance and glucose tolerance tests were not performed in this study limiting the evaluation of doxorubicin metabolic effect.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Carvalho, C. et al. Doxorubicin: The good, the bad and the ugly effect. Curr. Med. Chem. 16, 3267–3285 (2009).
Mordente, A., Meucci, E., Silvestrini, A., Martorana, G. E. & Giardina, B. New developments in anthracycline-induced cardiotoxicity. Curr. Med. Chem. 16, 1656–1672 (2009).
Lopez-Sendon, J. et al. Classification, prevalence, and outcomes of anticancer therapy-induced cardiotoxicity: The CARDIOTOX registry. Eur. Heart J. 41, 1720–1729. https://doi.org/10.1093/eurheartj/ehaa006 (2020).
Steinherz, L. J., Steinherz, P. G., Tan, C. T., Heller, G. & Murphy, M. L. Cardiac toxicity 4 to 20 years after completing anthracycline therapy. JAMA 266, 1672–1677 (1991).
Yeung, S. T., Yoong, C., Spink, J., Galbraith, A. & Smith, P. J. Functional myocardial impairment in children treated with anthracyclines for cancer. Lancet 337, 816–818 (1991).
Lotrionte, M. et al. Review and meta-analysis of incidence and clinical predictors of anthracycline cardiotoxicity. Am. J. Cardiol. 112, 1980–1984. https://doi.org/10.1016/j.amjcard.2013.08.026 (2013).
Reinbolt, R. E. et al. Risk factors for anthracycline-associated cardiotoxicity. Support Care Cancer 24, 2173–2180. https://doi.org/10.1007/s00520-015-3008-y (2016).
Barrett-Lee, P. J. et al. Expert opinion on the use of anthracyclines in patients with advanced breast cancer at cardiac risk. Ann. Oncol. 20, 816–827. https://doi.org/10.1093/annonc/mdn728 (2009).
Pei, X. M. et al. S100A8 and S100A9 are associated with doxorubicin-induced cardiotoxicity in the heart of diabetic mice. Front Physiol. 7, 334. https://doi.org/10.3389/fphys.2016.00334 (2016).
Belke, D. D., Swanson, E. A. & Dillmann, W. H. Decreased sarcoplasmic reticulum activity and contractility in diabetic db/db mouse heart. Diabetes 53, 3201–3208 (2004).
Al-Shabanah, O. A., El-Kashef, H. A., Badary, O. A., Al-Bekairi, A. M. & Elmazar, M. M. Effect of streptozotocin-induced hyperglycaemia on intravenous pharmacokinetics and acute cardiotoxicity of doxorubicin in rats. Pharmacol. Res. 41, 31–37. https://doi.org/10.1006/phrs.1999.0568 (2000).
Mitra, M. S., Donthamsetty, S., White, B. & Mehendale, H. M. High fat diet-fed obese rats are highly sensitive to doxorubicin-induced cardiotoxicity. Toxicol. Appl. Pharmacol. 231, 413–422. https://doi.org/10.1016/j.taap.2008.05.006 (2008).
Sayed-Ahmed, M. M. et al. Propionyl-L-carnitine as potential protective agent against adriamycin-induced impairment of fatty acid beta-oxidation in isolated heart mitochondria. Pharmacol. Res. 41, 143–150. https://doi.org/10.1006/phrs.1999.0583 (2000).
Mitra, M. S., Donthamsetty, S., White, B., Latendresse, J. R. & Mehendale, H. M. Mechanism of protection of moderately diet restricted rats against doxorubicin-induced acute cardiotoxicity. Toxicol. Appl. Pharmacol. 225, 90–101. https://doi.org/10.1016/j.taap.2007.07.018 (2007).
Childs, A. C., Phaneuf, S. L., Dirks, A. J., Phillips, T. & Leeuwenburgh, C. Doxorubicin treatment in vivo causes cytochrome C release and cardiomyocyte apoptosis, as well as increased mitochondrial efficiency, superoxide dismutase activity, and Bcl-2: Bax ratio. Cancer Res. 62, 4592–4598 (2002).
Suliman, H. B. et al. The CO/HO system reverses inhibition of mitochondrial biogenesis and prevents murine doxorubicin cardiomyopathy. J. Clin. Invest. 117, 3730–3741. https://doi.org/10.1172/JCI32967 (2007).
Takemura, G. & Fujiwara, H. Doxorubicin-induced cardiomyopathy from the cardiotoxic mechanisms to management. Prog. Cardiovasc. Dis. 49, 330–352. https://doi.org/10.1016/j.pcad.2006.10.002 (2007).
Yang, Y., Zhang, H., Li, X., Yang, T. & Jiang, Q. Effects of PPARalpha/PGC-1alpha on the energy metabolism remodeling and apoptosis in the doxorubicin induced mice cardiomyocytes in vitro. Int. J. Clin. Exp. Pathol. 8, 12216–12224 (2015).
Minotti, G., Menna, P., Salvatorelli, E., Cairo, G. & Gianni, L. Anthracyclines: Molecular advances and pharmacologic developments in antitumor activity and cardiotoxicity. Pharmacol. Rev. 56, 185–229. https://doi.org/10.1124/pr.56.2.6 (2004).
Jia, G., DeMarco, V. G. & Sowers, J. R. Insulin resistance and hyperinsulinaemia in diabetic cardiomyopathy. Nat. Rev. Endocrinol. 12, 144–153. https://doi.org/10.1038/nrendo.2015.216 (2016).
Messaoudi, S., Milliez, P., Samuel, J. L. & Delcayre, C. Cardiac aldosterone overexpression prevents harmful effects of diabetes in the mouse heart by preserving capillary density. FASEB J. 23, 2176–2185. https://doi.org/10.1096/fj.08-125302 (2009).
Fazal, L. et al. Akt-mediated cardioprotective effects of aldosterone in type 2 diabetic mice. FASEB J. 28, 2430–2440. https://doi.org/10.1096/fj.13-239822 (2014).
Huang, C. et al. Juvenile exposure to anthracyclines impairs cardiac progenitor cell function and vascularization resulting in greater susceptibility to stress-induced myocardial injury in adult mice. Circulation 121, 675–683. https://doi.org/10.1161/CIRCULATIONAHA.109.902221 (2010).
Azibani, F. et al. Aldosterone inhibits antifibrotic factors in mouse hypertensive heart. Hypertension 59, 1179–1187. https://doi.org/10.1161/HYPERTENSIONAHA.111.190512 (2012).
Nicol, M. et al. Doxorubicin-induced and trastuzumab-induced cardiotoxicity in mice is not prevented by metoprolol. ESC Heart Fail 8, 928–937. https://doi.org/10.1002/ehf2.13198 (2021).
Azibani, F. et al. Aldosterone inhibits the fetal program and increases hypertrophy in the heart of hypertensive mice. PLoS ONE 7, e38197. https://doi.org/10.1371/journal.pone.0038197 (2012).
Cohen-Solal, A., Beauvais, F. & Logeart, D. Heart failure and diabetes mellitus: Epidemiology and management of an alarming association. J. Card Fail 14, 615–625. https://doi.org/10.1016/j.cardfail.2008.04.001 (2008).
Giovannucci, E. et al. Diabetes and cancer: a consensus report. Diabetes Care 33, 1674–1685. https://doi.org/10.2337/dc10-0666 (2010).
Cannata, D., Fierz, Y., Vijayakumar, A. & LeRoith, D. Type 2 diabetes and cancer: What is the connection?. Mt Sinai J. Med. 77, 197–213. https://doi.org/10.1002/msj.20167 (2010).
Keating, N. L., O’Malley, A. J. & Smith, M. R. Diabetes and cardiovascular disease during androgen deprivation therapy for prostate cancer. J. Clin. Oncol. 24, 4448–4456. https://doi.org/10.1200/JCO.2006.06.2497 (2006).
Larsson, S. C., Mantzoros, C. S. & Wolk, A. Diabetes mellitus and risk of breast cancer: A meta-analysis. Int. J. Cancer 121, 856–862. https://doi.org/10.1002/ijc.22717 (2007).
Zendehdel, K. et al. Cancer incidence in patients with type 1 diabetes mellitus: A population-based cohort study in Sweden. J. Natl. Cancer Inst. 95, 1797–1800. https://doi.org/10.1093/jnci/djg105 (2003).
Lebrecht, D. & Walker, U. A. Role of mtDNA lesions in anthracycline cardiotoxicity. Cardiovasc. Toxicol. 7, 108–113. https://doi.org/10.1007/s12012-007-0009-1 (2007).
Minotti, G., Salvatorelli, E. & Menna, P. Pharmacological foundations of cardio-oncology. J. Pharmacol. Exp. Ther. 334, 2–8. https://doi.org/10.1124/jpet.110.165860 (2010).
Zhu, W., Shou, W., Payne, R. M., Caldwell, R. & Field, L. J. A mouse model for juvenile doxorubicin-induced cardiac dysfunction. Pediatr. Res. 64, 488–494. https://doi.org/10.1203/PDR.0b013e318184d732 (2008).
Maejima, Y., Adachi, S., Ito, H., Hirao, K. & Isobe, M. Induction of premature senescence in cardiomyocytes by doxorubicin as a novel mechanism of myocardial damage. Aging Cell 7, 125–136. https://doi.org/10.1111/j.1474-9726.2007.00358.x (2008).
Garcia Fernandez, M. et al. Early changes in intramitochondrial cardiolipin distribution during apoptosis. Cell Growth Differ. 13, 449–455 (2002).
Arreskov, A. B. et al. The impact of cancer on diabetes outcomes. BMC Endocr. Disord. 19, 60. https://doi.org/10.1186/s12902-019-0377-0 (2019).
Lipscombe, L. L. et al. Incidence of diabetes among postmenopausal breast cancer survivors. Diabetologia 56, 476–483. https://doi.org/10.1007/s00125-012-2793-9 (2013).
Jensen, M. V. et al. Endocrine late effects in survivors of cancer in adolescence and young adulthood: A Danish population-based cohort study. JAMA Netw. Open 1, e180349. https://doi.org/10.1001/jamanetworkopen.2018.0349 (2018).
Sah, R. P., Nagpal, S. J., Mukhopadhyay, D. & Chari, S. T. New insights into pancreatic cancer-induced paraneoplastic diabetes. Nat. Rev. Gastroenterol. Hepatol. 10, 423–433. https://doi.org/10.1038/nrgastro.2013.49 (2013).
Abudawood, M. Diabetes and cancer: A comprehensive review. J. Res. Med. Sci. 24, 94. https://doi.org/10.4103/jrms.JRMS_242_19 (2019).
Vigneri, P., Frasca, F., Sciacca, L., Pandini, G. & Vigneri, R. Diabetes and cancer. Endocr. Relat. Cancer 16, 1103–1123. https://doi.org/10.1677/ERC-09-0087 (2009).
Deng, H. Y. et al. Diabetes mellitus and survival of non-small cell lung cancer patients after surgery: A comprehensive systematic review and meta-analysis. Thorac Cancer 10, 571–578. https://doi.org/10.1111/1759-7714.12985 (2019).
Feng, J. P. et al. Secondary diabetes associated with 5-fluorouracil-based chemotherapy regimens in non-diabetic patients with colorectal cancer: Results from a single-centre cohort study. Colorectal Dis. 15, 27–33. https://doi.org/10.1111/j.1463-1318.2012.03097.x (2013).
Tayek, J. A. & Chlebowski, R. T. Metabolic response to chemotherapy in colon cancer patients. JPEN J. Parenter Enteral Nutr. 16, 65S-71S. https://doi.org/10.1177/014860719201600606 (1992).
Kohne, C. H. et al. Modulation of 5-fluorouracil with methotrexate and low-dose N-(phosphonacetyl)-L-aspartate in patients with advanced colorectal cancer. Results of a phase II study. Eur. J. Cancer 33, 1896–1899. https://doi.org/10.1016/s0959-8049(97)00256-6 (1997).
de Lima Junior, E. A. et al. Doxorubicin caused severe hyperglycaemia and insulin resistance, mediated by inhibition in AMPk signalling in skeletal muscle. J. Cachexia Sarcopenia Muscle 7, 615–625. https://doi.org/10.1002/jcsm.12104 (2016).
Yano, N. et al. Beta-adrenergic receptor mediated protection against doxorubicin-induced apoptosis in cardiomyocytes: The impact of high ambient glucose. Endocrinology 149, 6449–6461. https://doi.org/10.1210/en.2008-0292 (2008).
Feng, C. C. et al. Cardiac apoptosis induced under high glucose condition involves activation of IGF2R signaling in H9c2 cardiomyoblasts and streptozotocin-induced diabetic rat hearts. Biomed. Pharmacother. 97, 880–885. https://doi.org/10.1016/j.biopha.2017.11.020 (2018).
Moroz, L. V., Kabieva, A. O., Donenko, F. V. & Borovkova, N. B. Modification of doxorubicin action with artificial hyperglycemia. Antibiot Khimioter 35, 34–36 (1990).
Evans, J. M., Donnelly, L. A., Emslie-Smith, A. M., Alessi, D. R. & Morris, A. D. Metformin and reduced risk of cancer in diabetic patients. BMJ 330, 1304–1305. https://doi.org/10.1136/bmj.38415.708634.F7 (2005).
Barakat, H. E., Hussein, R. R. S., Elberry, A. A., Zaki, M. A. & Ramadan, M. E. The impact of metformin use on the outcomes of locally advanced breast cancer patients receiving neoadjuvant chemotherapy: An open-labelled randomized controlled trial. Sci. Rep. 12, 7656. https://doi.org/10.1038/s41598-022-11138-3 (2022).
Gong, L., Goswami, S., Giacomini, K. M., Altman, R. B. & Klein, T. E. Metformin pathways: pharmacokinetics and pharmacodynamics. Pharmacogenet. Genomics 22, 820–827. https://doi.org/10.1097/FPC.0b013e3283559b22 (2012).
Argun, M. et al. Cardioprotective effect of metformin against doxorubicin cardiotoxicity in rats. Anatol. J. Cardiol 16, 234–241. https://doi.org/10.5152/akd.2015.6185 (2016).
Kobashigawa, L. C., Xu, Y. C., Padbury, J. F., Tseng, Y. T. & Yano, N. Metformin protects cardiomyocyte from doxorubicin induced cytotoxicity through an AMP-activated protein kinase dependent signaling pathway: an in vitro study. PLoS ONE 9, e104888. https://doi.org/10.1371/journal.pone.0104888 (2014).
Asensio-Lopez, M. C. et al. Involvement of ferritin heavy chain in the preventive effect of metformin against doxorubicin-induced cardiotoxicity. Free Radic. Biol. Med. 57, 188–200. https://doi.org/10.1016/j.freeradbiomed.2012.09.009 (2013).
Ashour, A. E. et al. Metformin rescues the myocardium from doxorubicin-induced energy starvation and mitochondrial damage in rats. Oxid. Med. Cell Longev. 2012, 434195. https://doi.org/10.1155/2012/434195 (2012).
Quagliariello, V. et al. The SGLT-2 inhibitor empagliflozin improves myocardial strain, reduces cardiac fibrosis and pro-inflammatory cytokines in non-diabetic mice treated with doxorubicin. Cardiovasc. Diabetol. 20, 150. https://doi.org/10.1186/s12933-021-01346-y (2021).
Baris, V. O. et al. Empagliflozin significantly prevents the doxorubicin-induced acute cardiotoxicity via non-antioxidant pathways. Cardiovasc. Toxicol. 21, 747–758. https://doi.org/10.1007/s12012-021-09665-y (2021).
Sabatino, J. et al. Empagliflozin prevents doxorubicin-induced myocardial dysfunction. Cardiovasc. Diabetol. 19, 66. https://doi.org/10.1186/s12933-020-01040-5 (2020).
Oh, C. M. et al. Cardioprotective potential of an SGLT2 inhibitor against doxorubicin-induced heart failure. Korean Circ. J. 49, 1183–1195. https://doi.org/10.4070/kcj.2019.0180 (2019).
Abdel-Qadir, H. et al. The association of sodium-glucose cotransporter 2 inhibitors with cardiovascular outcomes in anthracycline-treated patients with cancer. JACC CardioOncol. 5, 318–328. https://doi.org/10.1016/j.jaccao.2023.03.011 (2023).
Gongora, C. A. et al. Sodium-glucose co-transporter-2 inhibitors and cardiac outcomes among patients treated with anthracyclines. JACC Heart Fail 10, 559–567. https://doi.org/10.1016/j.jchf.2022.03.006 (2022).
Eliaa, S. G., Al-Karmalawy, A. A., Saleh, R. M. & Elshal, M. F. Empagliflozin and doxorubicin synergistically inhibit the survival of triple-negative breast cancer cells via interfering with the mTOR pathway and inhibition of calmodulin: In vitro and molecular docking studies. ACS Pharmacol. Transl. Sci. 3, 1330–1338. https://doi.org/10.1021/acsptsci.0c00144 (2020).
Zhong, J. et al. Canagliflozin inhibits p-gp function and early autophagy and improves the sensitivity to the antitumor effect of doxorubicin. Biochem. Pharmacol. 175, 113856. https://doi.org/10.1016/j.bcp.2020.113856 (2020).
Swynghedauw, B. Molecular mechanisms of myocardial remodeling. Physiol. Rev. 79, 215–262. https://doi.org/10.1152/physrev.1999.79.1.215 (1999).
Dudnakova, T. V. et al. Alterations in myocardial cytoskeletal and regulatory protein expression following a single Doxorubicin injection. J Cardiovasc. Pharmacol. 41, 788–794. https://doi.org/10.1097/00005344-200305000-00017 (2003).
Skaggs, C. et al. Effects of doxorubicin on extracellular matrix regulation in primary cardiac fibroblasts from mice. BMC Res. Notes 16, 340. https://doi.org/10.1186/s13104-023-06621-7 (2023).
Willis, M. S. et al. Doxorubicin exposure causes subacute cardiac atrophy dependent on the striated muscle-specific ubiquitin ligase MuRF1. Circ. Heart Fail 12, e005234. https://doi.org/10.1161/CIRCHEARTFAILURE.118.005234 (2019).
Sandri, M. et al. Foxo transcription factors induce the atrophy-related ubiquitin ligase atrogin-1 and cause skeletal muscle atrophy. Cell 117, 399–412. https://doi.org/10.1016/s0092-8674(04)00400-3 (2004).
Chaouat, G. et al. TH1/TH2 paradigm in pregnancy: paradigm lost? Cytokines in pregnancy/early abortion: Reexamining the TH1/TH2 paradigm. Int. Arch. Allergy Immunol. 134, 93–119. https://doi.org/10.1159/000074300 (2004).
Tian, M. et al. Cardiac alterations in cancer-induced cachexia in mice. Int. J. Oncol. 37, 347–353 (2010).
Acknowledgements
We are grateful to Malha Sadoune and Alexis Nguyen for their valuable help.
Funding
This work was supported by Institut National de la Santé et de la Recherche Médicale (INSERM), Fondation pour la recherche médicale, Université Paris Cité and Fondation de France.
Author information
Authors and Affiliations
Contributions
F.A. and A.C.S. designed the experiments. M.N., B.D., R.R., M.G., E.P. and N.A. performed the experiments. F.A., and M.N., prepared the manuscript. All the authors revised the manuscript critically for important intellectual content. All authors confirmed the authenticity of all the raw data, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nicol, M., Deniau, B., Rahli, R. et al. Streptozotocin-induced hyperglycemia unmasks cardiotoxicity induced by doxorubicin. Sci Rep 15, 8104 (2025). https://doi.org/10.1038/s41598-025-91824-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-91824-0
This article is cited by
-
Distinct immunometabolic signatures of type 1 versus type 2 diabetes in a murine model of myocardial infarction
Cardiovascular Diabetology (2026)