Abstract
Multidomain lifestyle interventions can improve cognitive function and mobile health technologies can deliver cost-effective interventions. We developed the smartphone app, Cognitive Evergreenland, to promote cognitive health in people at high risk of dementia, and assessed its usability. Functional modules were selected using a behaviour change wheel (BCW) theory-based method. Target behaviors were assessed by literature review and focus group interviews. Findings were mapped onto the Capability, Opportunity, and Motivation—Behaviour (COM-B) model and Theoretical Domains Framework, identifying behaviors requiring change and linking them to intervention functions. Behavior change techniques (BCTs) considered likely to be effective were selected, and corresponding COM-B components and BCTs translated into application functionalities. The app was optimized based on user feedback collected by interview and evaluated using “Mobile Health App Usability Questionnaire for Standalone mHealth Apps (Patient Version)”. Promoting adherence to multidomain lifestyle interventions required changes in physical and psychological abilities, reflective and automatic motivation reinforcement, and social and physical opportunities provision. We identified seven key intervention functions and selected 16 BCTs. Finalized Cognitive Evergreenland modules included health education, cognitive stimulation, cognitive training, interactive communication, health diary, functional assessment, and personal profile. Target users indicated overall satisfaction with usability. BCW theory application facilitated Cognitive Evergreenland development.
Similar content being viewed by others
Introduction
The need for lifestyle interventions based on mobile health (mHealth)
Cognitive impairment and dementia are major challenges facing the global health sector in the twenty-first century1. To date, there are no effective pharmacological interventions to delay or treat cognitive decline or dementia; therefore, there are increasing efforts to develop methods that can proactively control modifiable risk factors, with the aim of delaying or slowing disease onset and/or progression. Indeed, compelling evidence from an increasing number of observational studies suggests that targeting modifiable risk factors can reduce the incidence of dementia2,3. Approximately one-third of Alzheimer’s disease cases are attributable to modifiable risk factors4, and the authors of a 2014 study calculated that, based on an estimated 10% relative reduction in the contributions of each of seven risk factors per decade, overall Alzheimer’s disease prevalence could be decreased by 8.3% by 20505. Therefore, improving brain health and cognitive function through lifestyle interventions that target risk factors before the onset of dementia may delay, or even prevent, the onset of cognitive decline or dementia6,7.
As lifestyle-related risk factors influencing cognitive function are typically clustered, multidomain strategies to prevent cognitive decline and dementia may be more effective than targeting individual risk factors8,9,10. Indeed, there is growing evidence that targeting multiple lifestyle factors simultaneously may improve the effectiveness of interventions, relative to approaches focused on a single lifestyle factor11. Some large-scale randomized controlled trials have assessed the efficacy of face-to-face multidomain lifestyle interventions in preventing cognitive impairment or dementia; however, the conclusions from these studies are inconsistent. The Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER) trial was a two-year face-to-face multidomain intervention study, including dietary changes, physical exercise, cognitive training, and vascular risk monitoring. In comparison to the control group receiving general health advice, the FINGER trial found that cognitive function was maintained in a group of participants at risk of cognitive decline12; however, two other large-scale, multidomain randomized controlled trials targeting improvements in cognitive function or reduction in dementia incidence primarily reported negative results, with no significant improvements in cognitive function or reduction in dementia incidence across the entire study population13,14. Nevertheless, post-hoc analyses of both studies indicated that the multidomain interventions had positive effects on individuals with a higher risk of dementia, such as those experiencing mild cognitive impairment (MCI) or subjective cognitive decline (SCD)15. In addition, a systematic review concluded that comprehensive analysis of study results was difficult, due to significant heterogeneity among studies in intervention characteristics, such as the combinations of risk factors targeted, lengths of intervention, and participant characteristics16. Based on these results, we infer that multidomain lifestyle interventions have potential, but further research is needed to understand how such approaches can be improved to increase their efficacy in reducing cognitive decline and dementia risk.
Face-to-face intervention programs also face practical barriers, including the need to train appropriate staff and the resources required to deliver the intervention, such as the location and personnel. With the emergence of "Internet + ,” time and space limitations can be eliminated, allowing people to easily obtain information at any place and time. Therefore, an attractive alternative to the face-to-face approach is to deliver lifestyle programs online, taking advantage of the rapidly growing field of mHealth interventions17. mHealth applications are key components of mHealth interventions, and function via software programs on smartphones, tablets, and other mobile devices, to enhance health conditions. A previous systematic review and meta-analysis18 to investigate the effects of multidomain web-based lifestyle programs on brain health reported that such programs have potential to contribute to dementia prevention, although the results of the small number of studies included in the meta-analysis were highly heterogeneous. Additionally, it is undeniable that these innovative mHealth tools facilitate the implementation and monitoring of intervention measures, while also being cost-effective and more broadly applicable, in terms of geographical regions and populations17. Previous studies have also provided insights that can inform the development of such tools; for example, they have demonstrated that populations at high risk of dementia can be prioritized as key targets for interventions, including enhanced lifestyle-based multidomain interventions, and the intervention effects appropriately assessed19,20.
The need for theory in mHealth-based applications
Compliance with long-term participation in lifestyle interventions varies considerably among older adults at increased risk of dementia21. A qualitative study found that it is critical for lifestyle-based, multidomain prevention strategies to be tailored to the needs of key target groups, to maximize their appeal and efficacy22. Specifically, further insights into how a multidomain lifestyle-based approach can be used to reduce the risk of cognitive decline and dementia are needed, as well as details of which preferences and considerations are important for lifestyle-based risk reduction approaches. Simultaneously, optimization of selection of targeted lifestyle-related behaviors is necessary, to better understand the potential inhibitors and facilitators of measures to promote brain health. Lifestyle interventions developed with the participation of patients and local healthcare professionals are more likely to achieve effective outcomes, because they are aligned with local needs, preferences, and priorities, ensuring that the requirements of relevant stakeholders are best met23. Another critical issue for the successful implementation of mHealth approaches is whether interventions are evidence-based and grounded in theory24. Application of relevant theories in mHealth projects is particularly crucial, as it can lead to well-rounded intervention strategies, resulting in improved health outcomes25. In particular, research has highlighted the need for mHealth interventions to develop high levels of health behavioral competencies among participants, to inspire self-motivation and persistence26. Numerous theories and models of behavior change can be used to guide the design of interventions to prompt and sustain behavior change, and the applicability of these theories may vary depending on the specific behaviors involved.
mHealth apps developed using the behaviour change wheel (BCW) theory and related strategies are reported to be particularly effective in initiating and sustaining changes in user behavior27,28,29. BCW theory is based on behavior change theory, closely integrates evidence-based intervention functions, and can guide interventions to target environments and populations. Further, the role of healthcare professionals in application development is crucial. In this study, we particularly emphasized the critical role that healthcare professionals play in using BCW as a theoretical framework for designing lifestyle intervention applications targeting populations at high risk for dementia. The comprehensive and systematic nature of BCW theory makes it a powerful tool for consideration of multiple lifestyle intervention aspects, such as participant preferences and needs, as well as potential barriers and facilitators, thus improving the overall effectiveness of an intervention.
Objectives
In this study, we aimed to make full use of the advantages of the BCW theoretical framework, to more effectively implement an intervention for groups at high risk of dementia, through the participation of healthcare professionals. Further, we sought to provide more innovative and effective solutions for dementia prevention and management. In this report, we describe the design and development of the Cognitive Evergreenland app using the BCW framework to enhance adherence and engagement in lifestyle interventions for individuals at high risk of dementia.
Methods
Setting
The Cognitive Evergreenland app was developed in this study, primarily to target patients at high risk of dementia, defined as older people (aged ≥ 60 years) who are experiencing SCD or MCI. These individuals have not yet progressed to the stage of dementia, according to the Jessen criteria (clinically normal on objective assessment, self/informant reported cognitive decline, and decline not better explained by a major medical, neurological, or psychiatric diagnosis).
Theoretical framework
First, factors influencing adherence to mobile lifestyle interventions for older adults at high risk of dementia, based on the Capability, Opportunity, and Motivation—Behaviour (COM-B) model within the BCW theory, were analyzed30. The COM-B model is a framework for understanding behavior, through analysis of COM as influences on behavior, as well as their potential interactions and resulting behaviors, and forms the core of the BCW. The Theoretical Domains Framework (TDF) was employed to identify drivers and barriers to behavioral change and diagnose behavioral issues, pinpointing key elements and proposing corresponding solutions31. These elements were then mapped to BCW intervention functions based on the relationship matrix between COM-B components and BCW intervention functions. Subsequently, intervention functions were selected according to the APEASE criteria (Affordability, Practicability, Effectiveness, Acceptability, Safety, and Equity)32. Then, appropriate behavior change techniques (BCTs) were filtered for correspondence with the Behavior Change Technique Taxonomy version 1 (BCTTv1) list33. Overall, this comprehensive approach integrated BCW and TDF theories, to provide a systematic and effective framework for understanding and addressing factors affecting adherence to lifestyle interventions for older adults at high risk of dementia. The development process is reported following the Guidance for Reporting Intervention Development Studies in Health Research checklist, consisting of 14-item quality criteria (Additional file 1)34.
Development process
The Cognitive Evergreenland development process referred to the BCW model and was subdivided into three main phases, each containing key sub-steps, to ensure that user needs were systematically understood and met. Detailed descriptions of each stage are provided below.
Stage I: Understanding the problem and user preferences
Step 1: define the problem in behavioral terms
The first step was to identify specific barriers to the implementation of lifestyle interventions for older adults at high risk of dementia. To achieve this, two researchers conducted a comprehensive literature review. The review focused on identifying who performs the behaviors and listing other factors that may influence problem behaviors. The researchers systematically searched eight databases for studies published in the past five years, using search terms such as "dementia OR cognitive decline OR cognitive impairment," "facilitator OR motivat* OR benefit* OR barrier*," and "lifestyle OR lifestyle intervention." The findings were categorized using the COM-B model, which included physical and psychological capability, physical and social opportunity, and automatic and reflective motivation.
Steps 2 and 3: select and specify target behaviors
Data from evidence-based research was incorporated to identify target behaviors of older adults at high risk for dementia. Once a target behavior was selected, specific elements of the selected target behavior were further clarified; for example, who needs to do this, what they need to do differently to elicit change, and when and where it needs to happen, as well as how often and with whom. These specifications were discussed and finalized during a series of research group meetings, where consensus was reached on the final target behaviors. The meetings involved in-depth discussions on the feasibility, relevance, and potential impact of the selected behaviors, ensuring alignment with the needs of the target population and the goals of the intervention.
Step 4: identify what needs to change
Based on a review of the literature, focus group interviews with older people at high risk for dementia, who were interested in participating in a multidomain lifestyle intervention, were organized, with the aim of collecting information about potential barriers and facilitators to adherence to the intervention (Additional file 2). Focus groups concentrated on 14 known barriers to adherence to multidomain lifestyle interventions among older adults at high risk for dementia, mapped on the COM-B model generated in step 1; each session lasted approximately 1 h. At the end of each focus group, one of the researchers provided a summary of the discussion and an opportunity to clarify or add any missing points, and the content of each focus group was recorded in detail.
Stage II: identification of intervention options and policy recommendations
Steps 5 and 6: identify intervention functions and policy categories
Intervention functions most likely to influence primary behavior change were preliminarily identified through a comprehensive review of the findings of COM-B and TDF behavior analysis. To further refine and validate these findings, focus group discussions were conducted. The APEASE criteria were used to guide selection of the relevant intervention functions; these criteria are: (1) Affordability, (2) Practicability, (3) Effectiveness and cost-effectiveness, (4) Acceptability, (5) Side effects/safety, and (6) Equity. Additionally, specific policy categories supporting each intervention function were identified; these were determined using the policy categories provided in the BCW guide (such as marketing, guidelines, service provision, etc.). These policy categories help to support the execution and promotion of an application, ensuring its successful implementation and maximizing its impact on the target user group.
Stage III: Identification of application function modules and usability evaluation
Step 7: selection of BCTs
The BCTTv1, proposed by Michie et al.33, describes how each BCT is associated with various intervention functions. Focus group discussions, providing valuable insights based on their diverse backgrounds and expertise in the field, were used to select the most effective and feasible techniques from the potential list of BCTs, based on the APEASE criteria, to guide dementia-prone older adults in adhering to long-term lifestyle interventions. The focus group discussions were structured such that participants were divided into four groups, with each group responsible for in-depth exploration of one or more intervention functions and their corresponding BCTs. Each group presented their findings and received feedback from both peer groups and the moderator. Following the initial broad categorization of intervention content, we conducted detailed analyses to determine the precise BCTs to be employed.
Step 8: determining the mode of delivery
After selection of BCTs, the next step involved integrating these techniques into the functionalities of the Cognitive Evergreenland app. This process entailed collaboration with mobile app design and development companies, to determine the specific mode of delivery most suitable for Cognitive Evergreenland, such as a mobile app, WeChat Mini Program, or web-based online support, to ensure that users can easily access and use the app.
Step 9: assessment and refinement of app usability
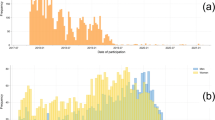
Once the mode of delivery was selected, two rounds of pilot testing were conducted to assess the app’s usability. Through purposive sampling, older adult participants with SCD and MCI were recruited from the Geriatric Medicine Centre in Fujian Province, China, to pilot the application.
The pilot process included online or face-to-face interviews, using the Usability Evaluation Opinions Collection Form (Additional file 3) to assess the completion rate of application users independently or with assistance, and continuously collecting user feedback and modification suggestions until data saturation was achieved, indicated by no new themes or suggestions emerging from the interviews. Based on the feedback received, the application was revised and optimized. After optimization, a second round of pilot testing was conducted with a new group of older adults with SCD and MCI, who were asked to complete the Mobile Health App Usability Questionnaire for Standalone mHealth Apps—Patient Version (MAUQ-SP) to assess usability35. The MAUQ-SP questionnaire comprises three dimensions: usability, interface and satisfaction, and effectiveness, with a total of 18 items. Each item is rated on a scale from “strongly disagree” to “strongly agree” with scores ranging from 1 to 7. The scores of all items are summed and averaged to obtain a total score, with higher scores indicating better usability. Our previous research validated the Chinese version of this questionnaire, showing a Cronbach’s α coefficient of 0.979, a split-half reliability of 0.919, and a test–retest reliability of 0.974, demonstrating good reliability and validity36.
Ethics and consent
This study obtained approval from the Ethics Committee of Fujian Provincial Hospital (K2021-03-029) and was carried out in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants, ensuring that they were informed in advance about the potential benefits and risks of participating in the research. Participants were confident in the confidentiality and anonymity of their information.
Results
Step 1: define the problem in behavioral terms
Research indicates that older adults actively engaged in lifestyle intervention activities exhibit better cognitive trajectories, with the most active participants more likely to observe improvements in their daily lifestyle habits, which are associated with better cognitive outcomes, highlighting the crucial role of persistence in lifestyle interventions in influencing cognition37. Prior to this study, there were no reports addressing the barriers and mechanisms affecting participant adherence to lifestyle intervention activities and lifestyle changes.
To address this gap, two researchers (RL and YJY) conducted a literature review38,39,40, we identified 12 known barriers related to the adherence of older adults at high risk of dementia to multidomain lifestyle intervention measures, based on the COM-B model (Additional file 4). The results of our review indicated that all influences on behavior (physical and psychological capability, physical and social opportunity, and automatic and reflective motivation) may be associated with non-adherence, confirming that factors influencing such behavioral changes are highly complex. Most of these barriers are related to more than one aspect of the COM-B model influencing behavior, with motivation the most prevalent. Based on our analysis, we inferred those social influences, including factors from the social environment and others, such as social support, social pressure, and social norms, can appropriately map to both reflective and automatic motivation. This suggests that promoting social opportunities can enhance motivation behavior, and that this association may even facilitate synergistic induction of compliance.
Steps 2 and 3: select and specify target behaviors
Based on the evidence synthesized from the literature review conducted by RL and YJY, the research team identified high-intensity, long-term lifestyle interventions as the primary target behavior for older adults at risk of dementia. This decision was supported by findings from key studies, such as the FINGER and Multidomain Alzheimer Preventive trials, which demonstrated that sustained engagement in multidomain lifestyle interventions can significantly improve cognitive outcomes.
The research team further specified the target behavior by defining:
-
Who: Older adults with SCD or MCI.
-
What: Daily completion of multidomain lifestyle intervention tasks.
-
Where: Using mobile health technology to overcome location barriers.
-
How Often: Daily engagement.
These specifications were validated during research group meetings, where the team discussed the feasibility and relevance of the selected behaviors. The final target behaviors were aligned with the needs of the target population and the goals of the intervention, as summarized in Table 1.
Step 4: identify what needs to change
Through focus group interviews, we specifically clarified barriers, and analyzed their causes, as well as facilitators, to further understand user preferences and needs (Table 2). This process helped us gain a more comprehensive understanding of the barriers and facilitators faced by seniors at high risk for dementia in adhering to multidomain lifestyle interventions, providing guidance for our subsequent TDF-guided mapping of barrier areas that may affect BCW intervention implementation. Research on intervention functions provided important background information. Overall, the focus groups generated a deeper understanding of factors that need to be changed to achieve the selected target behaviors.
Steps 5 and 6: identify intervention functions and policy categories
Guided by the APEASE criteria, research team members initially identified relevant intervention functions based on a correlation matrix linking the COM-B model, TDF, and potential intervention functions. Subsequently, focus group discussions were conducted to refine and finalize the selection, ultimately determining seven intervention functions: training, enablement, education, persuasion, incentivization, environmental restructuring, and modeling. These functions were then matched with corresponding policy categories using a BCW-based relationship matrix.
Based on this relationship matrix and integrating the results of focus group discussions (Additional file 5), two suitable policy categories were ultimately selected: “Communication” and "Public Service." “Communication” involves the use of various media, such as print, electronic, telephone, or broadcast, to disseminate information about the need for early intervention for dementia prevention to the public and professionals. For example, dissemination of the need for early intervention for dementia prevention to the public and professionals through brochures or looped video playback, emphasizing the serious consequences of non-intervention at this stage. “Public Service” entails providing support services, such as integration of primary and secondary dementia prevention, into the national basic health public service program. The remaining policy categories were not included in the intervention options of this study, due to their inconsistency with the APEASE criteria; however, past intervention studies have indicated that policy categories may have limited effects in individual or small-scale interventions and are more suitable for providing recommendations for policy formulation from a macro perspective. Therefore, the “Communication” and “Public Service” policy categories proposed in this study can serve as reference points for policy recommendations.
Step 7: select behavior change techniques (BCTs)
To select the most applicable BCTs, we incorporated focus group discussions and thoroughly considered the APEASE criteria. Through guided discussion and negotiation under the moderator’s stewardship, a consensus was established on the identification of BCTs and their alignment with the respective intervention functions (Additional file 5). Ultimately, we selected 16 BCTs that were deemed most suitable based on this comprehensive approach (Table 3).
Step 8: determine mode of delivery
After discussions with data engineers and software developers, it was decided to implement Cognitive Evergreenland on a WeChat Mini Program platform to ensure user accessibility and ease of use (Fig. 1). Subsequently, using agile development methodologies, the corresponding COM-B components and BCTs were translated into application functional modules. Through repeated communication with development engineers, the overall architecture of Cognitive Evergreenland was finalized, consisting of five layers: the user layer, application layer, service layer, collection layer, and data source layer (Fig. 2). The user layer and application layer were designed with different functional modules tailored to different user types. On the user interface, these functional modules included Health Education, Cognitive Stimulation, Cognitive Training, Interactive Communication, Health Diary, Functional Assessment, and Personal Profile (see Table 4 for details).
Step 9: assessment and refinement of app usability
Twelve older adults with SCD and MCI, comprising six women and six men, with educational backgrounds spanning from primary education to post-graduate levels, and diverse levels of proficiency in smartphone usage, ranging from “Not proficient” to “Very proficient,” were selected to participate in the first round of pilot testing. The independent or assisted completion rate by users exceeded 90%, and 11 modification suggestions were proposed (Additional file 3). Data saturation was achieved, as no new themes or suggestions emerged from the interviews. Based on the feedback received, the application was revised and optimized.
Next, a further 24 older adults with SCD and MCI were chosen to assess the usability of the platform and complete the MAUQ-SP36. Survey results from the second round indicated that participants rated the usability of the Cognitive Evergreenland app, in terms of the three dimensions of MAUQ-SP (usability, interface and satisfaction, and effectiveness) and overall satisfaction, with scores exceeding 5/7 (Table 5), indicating good usability. The application is currently under registration with the China Copyright Protection Center (Registration Number: 2023SR0526900). The source code for the application can be found in Additional file 6.
Discussion
This study provides a step-by-step illustration of how to integrate evidence, theory, and validated assessment tools into the development of mHealth applications aimed at enhancing the COM for healthy behaviors among individuals at high risk of dementia. The BCW systematically describes the conditions needed in the internal, external social, and physical environments of individuals, to achieve target behaviors. By mapping these conditions to the elements of the COM-B model, intervention measures are linked to behavioral mechanisms, providing a clear and specific practical framework for designing theory-driven applications32. Initially, we identified 12 known barriers related to the persistence of multicomponent lifestyle interventions for older adults at high risk of dementia within the COM-B model, by conducting a literature review. Following the selection and specification of target behaviors, we further elucidated these barrier factors through focus group interviews, by analyzing their underlying reasons, as well as investigating facilitators, and gaining insights into user preferences and needs. We found that older adults face various complex barriers when participating in multicomponent lifestyle interventions, including lack of interest, low self-efficacy, limited resources, time constraints, and skepticism about intervention content, among others. These obstacles reflect the diversity in cognition and behavior among older adults and highlight the need for carefully designed intervention measures to address them. In comparison with previous research38,39,40, we also identified issues of low self-efficacy among older adults participating in multidomain lifestyle interventions, indicating a lack of confidence in their ability to sustain long-term engagement. For example, people may worry about the quantity and burden of intervention tasks and be reluctant to learn new things. Additionally, the appeal of intervention content significantly influences sustained participation, as individuals may perceive intervention tasks as monotonous and dull. These findings underscore the importance of paying particular attention to these factors during the application development process.
We also conducted behavioral analysis of areas requiring change and linked our findings with intervention functions, policy categories, and BCTs, to effect change. This approach allows for the customization of interventions, to meet the preferences and needs of target users. Key elements that influence the participation of older people at high risk of dementia in multidomain lifestyle interventions identified using the TDF framework included: Skills, Knowledge, Beliefs and capabilities, Beliefs about consequences, Intentions, Goals, Reinforcement, Environmental context and resources, and Social influences. Following the main steps and principles of the BCW, we propose an mHealth management strategy for MCI and ultimately identified seven intervention functions, two policy suggestions, and 16 applicable BCTs. Given the interactions among all components of the BCW, the selection of appropriate intervention functions, policy categories, and BCTs is crucial for maximizing the potential for behavior change when designing interventions.
The importance of identifying and analyzing the factors contributing to adherence, and barriers to interventions is often underestimated, particularly in the context of older patients, who are typically retired. Unlike younger age groups, where adherence to treatment may lead to increased health-related productivity, this correlation is less straightforward among older individuals41. In our study, we employed a theory-driven approach to develop the application, similar to the methodology used by Smith et al. in their study to develop the “Stay Active” smartphone application based on the BCW framework, with the aim of increasing physical activity among women with gestational diabetes37; however, our study identified more key intervention functions than those found in their study, which included Enablement, Environmental restructuring, and Modelling. This disparity may be attributable to the greater complexity of barriers to adherence to long-term, intensive lifestyle interventions among older individuals, necessitating a broader range of strategies.
In this work, we successfully integrated BCTs and Intervention functions selected through rigorous scientific steps into Cognitive Evergreenland. By collaborating with data engineers and software developers, we identified WeChat mini programs as the most appropriate delivery method and transformed various BCTs into functional modules of the application. This customized intervention design can better meet the needs of users and improve the acceptability and effectiveness of the intervention. Therefore, it is crucial to work with software developers with experience in commercial application during the development process, to ensure that BCTs can be realistically integrated into application functionality, while maintaining their rigor. Future researchers in the mHealth field should consider adopting this approach, to ensure that theory can be effectively integrated into application functionality, thereby maximizing its potential to promote behavior change.
This study has several limitations. First, there are limitations regarding the sample. The participants primarily consisted of older adults at high risk of dementia, which may have introduced sample selection bias and could restrict the generalizability of the application to a broader population. Second, the involvement of local healthcare professionals and the consideration of local needs during the development of the Cognitive Evergreenland app may further limit the generalizability of our findings to other regions or cultural contexts. Third, it is possible that we did not identify all obstacles and factors potentially driving adherence to the multifaceted lifestyle intervention, as not all key stakeholders (such as family members and government officials) were included in our focus groups. Additionally, there may be variations in the understanding and acceptance of the intervention strategies that necessitate consideration of cultural and linguistic factors. Hence, future studies to validate our findings in different regions and cultural contexts are warranted. The next step involves examination of the feasibility and effectiveness of the multifaceted lifestyle intervention based on Cognitive Evergreenland, along with assessment of its impact on health behaviors.
We present an evidence-informed and systematically developed intervention aimed at enhancing adherence and engagement in lifestyle interventions for individuals at high risk of dementia through the Cognitive Evergreenland app. We describe the process of applying the BCW, TDF, and BCTs to identify and design behavior change intervention components tailored to support the objectives of our application. The processes applied in this study represent a structured approach that can be adopted by researchers to guide the development of mobile applications targeting lifestyle interventions aimed at enhancing adherence and engagement in individuals at high risk of dementia.
Data availability
Data is available on request due to privacy/ethical restrictions. The data that support the findings of this study are available on request from the corresponding author.
References
World Health Organization. Risk reduction of cognitive decline and dementia: WHO guidelines (2019).
An, R. et al. Predictors of progression from subjective cognitive decline to objective cognitive impairment: a systematic review and meta-analysis of longitudinal studies. Int. J. Nurs. Stud. 149, 104629. https://doi.org/10.1016/j.ijnurstu.2023.104629 (2024).
Yu, J. T. et al. Evidence-based prevention of Alzheimer’s disease: systematic review and meta-analysis of 243 observational prospective studies and 153 randomised controlled trials. J. Neurol. Neurosurg. Psychiatry 91, 1201–1209. https://doi.org/10.1136/jnnp-2019-321913 (2020).
Livingston, G. et al. Dementia prevention, intervention, and care. Lancet 390, 2673–2734. https://doi.org/10.1016/s0140-6736(17)31363-6 (2017).
Norton, S., Matthews, F. E., Barnes, D. E., Yaffe, K. & Brayne, C. Potential for primary prevention of Alzheimer’s disease: An analysis of population-based data. Lancet Neurol. 13, 788–794. https://doi.org/10.1016/s1474-4422(14)70136-x (2014).
de Bruijn, R. F. et al. The potential for prevention of dementia across two decades: The prospective, population-based Rotterdam Study. BMC Med. 13, 132. https://doi.org/10.1186/s12916-015-0377-5 (2015).
Yaffe, K. Modifiable risk factors and prevention of dementia: What is the latest evidence?. JAMA Intern. Med. 178, 281–282. https://doi.org/10.1001/jamainternmed.2017.7299 (2018).
Dingle, S. E. et al. Associations between data-driven lifestyle profiles and cognitive function in the AusDiab study. BMC Public Health 22, 1990. https://doi.org/10.1186/s12889-022-14379-z (2022).
Peters, R. et al. Combining modifiable risk factors and risk of dementia: A systematic review and meta-analysis. BMJ Open 9, e022846. https://doi.org/10.1136/bmjopen-2018-022846 (2019).
Dingle, S. E. et al. Data-driven lifestyle patterns and risk of dementia in older Australian women. Alzheimers Dement. 20, 798–808. https://doi.org/10.1002/alz.13467 (2024).
Andrieu, S., Coley, N., Lovestone, S., Aisen, P. S. & Vellas, B. Prevention of sporadic Alzheimer’s disease: Lessons learned from clinical trials and future directions. Lancet Neurol. 14, 926–944. https://doi.org/10.1016/s1474-4422(15)00153-2 (2015).
Ngandu, T. et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. Lancet 385, 2255–2263. https://doi.org/10.1016/s0140-6736(15)60461-5 (2015).
Andrieu, S. et al. Effect of long-term omega 3 polyunsaturated fatty acid supplementation with or without multidomain intervention on cognitive function in elderly adults with memory complaints (MAPT): A randomised, placebo-controlled trial. Lancet Neurol. 16, 377–389. https://doi.org/10.1016/s1474-4422(17)30040-6 (2017).
Moll van Charante, E. P. et al. Effectiveness of a 6-year multidomain vascular care intervention to prevent dementia (preDIVA): A cluster-randomised controlled trial. Lancet 388, 797–805. https://doi.org/10.1016/s0140-6736(16)30950-3 (2016).
Cheng, G. R. et al. Prevalence and risk factors for subjective cognitive decline and the correlation with objective cognition among community-dwelling older adults in China: results from the Hubei memory and aging cohort study. Alzheimers Dement. 19, 5074–5085. https://doi.org/10.1002/alz.13047 (2023).
Hafdi, M., Hoevenaar-Blom, M. P. & Richard, E. Multi-domain interventions for the prevention of dementia and cognitive decline. Cochrane Database Syst. Rev. 11, Cd013572. https://doi.org/10.1002/14651858.CD013572.pub2 (2021).
Angelis, I. et al. Mobile application for monitoring and preventing cognitive decline through lifestyle intervention. Adv. Exp. Med. Biol. 1338, 89–96. https://doi.org/10.1007/978-3-030-78775-2_11 (2021).
Wesselman, L. M. et al. Web-based multidomain lifestyle programs for brain health: Comprehensive overview and meta-analysis. JMIR Ment. Health 6, e12104. https://doi.org/10.2196/12104 (2019).
Rosenberg, A., Mangialasche, F., Ngandu, T., Solomon, A. & Kivipelto, M. Multidomain interventions to prevent cognitive impairment, Alzheimer’s disease, and dementia: from FINGER to World-Wide FINGERS. J. Prev. Alzheimers Dis. 7, 29–36. https://doi.org/10.14283/jpad.2019.41 (2020).
Sindi, S., Mangialasche, F. & Kivipelto, M. Advances in the prevention of Alzheimer’s disease. F1000Prime Rep. 7, 50. https://doi.org/10.12703/p7-50 (2015).
Turunen, M. et al. Computer-based cognitive training for older adults: determinants of adherence. PLoS One 14, e0219541. https://doi.org/10.1371/journal.pone.0219541 (2019).
Dingle, S. E., Milte, C. M., Daly, R. M. & Torres, S. J. Attitudes and considerations for multidomain lifestyle approaches to dementia prevention: a qualitative study. J. Alzheimers Dis. 97, 939–949. https://doi.org/10.3233/jad-230176 (2024).
Smits, S. et al. Development of a behavior change intervention to encourage timely cancer symptom presentation among people living in deprived communities using the behavior change wheel. Ann. Behav. Med. 52, 474–488. https://doi.org/10.1007/s12160-016-9849-x (2018).
Sahin, C. Rules of engagement in mobile health: What does mobile health bring to research and theory?. Contemp. Nurse 54, 374–387. https://doi.org/10.1080/10376178.2018.1448290 (2018).
Cho, Y. M., Lee, S., Islam, S. M. S. & Kim, S. Y. Theories applied to m-health interventions for behavior change in low- and middle-income countries: a systematic review. Telemed. J. E Health 24, 727–741. https://doi.org/10.1089/tmj.2017.0249 (2018).
Düzel, E. & Thyrian, J. R. Mobile everyday-life digital technologies for the prevention of Alzheimer’s dementia: cognitive health and cognitive safety. Nervenarzt. 94, 400–407. https://doi.org/10.1007/s00115-023-01478-4 (2023).
Truelove, S., Vanderloo, L. M., Tucker, P., Di Sebastiano, K. M. & Faulkner, G. The use of the behaviour change wheel in the development of ParticipACTION’s physical activity app. Prev. Med. Rep. 20, 101224. https://doi.org/10.1016/j.pmedr.2020.101224 (2020).
Smith, R. et al. Applying the behaviour change wheel to develop a smartphone application “stay-active” to increase physical activity in women with gestational diabetes. BMC Pregnancy Childbirth 22, 253. https://doi.org/10.1186/s12884-022-04539-9 (2022).
Chu, S. et al. A WeChat mini-program-based approach to smoking cessation behavioral interventions: Development and preliminary evaluation in a single-arm trial. Digit. Health 9, 20552076231208550. https://doi.org/10.1177/20552076231208553 (2023).
Michie, S., van Stralen, M. M. & West, R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement. Sci. 6, 42. https://doi.org/10.1186/1748-5908-6-42 (2011).
Cane, J., O’Connor, D. & Michie, S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 7, 37. https://doi.org/10.1186/1748-5908-7-37 (2012).
Michie, S., Atkins, L. & West, R. The Behaviour Change Wheel. A Guide to Designing Interventions 1st edn, Vol. 1003, 1010 (Silverback Publishing, USA, 2014).
Michie, S. et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 46, 81–95. https://doi.org/10.1007/s12160-013-9486-6 (2013).
Duncan, E. et al. Guidance for reporting intervention development studies in health research (GUIDED): An evidence-based consensus study. BMJ Open 10, e033516. https://doi.org/10.1136/bmjopen-2019-033516 (2020).
Zhou, L., Bao, J., Setiawan, I. M. A., Saptono, A. & Parmanto, B. The mHealth app usability questionnaire (MAUQ): development and validation study. JMIR Mhealth Uhealth 7, e11500. https://doi.org/10.2196/11500 (2019).
Lin, R. et al. Validity and reliability the Chinese version of the standalone mHealth apps usability questionnaire for standalone mHealth apps patient version in older adults. J. Nurs. Sci. 38, 107–111 (2023).
Ngandu, T. et al. The effect of adherence on cognition in a multidomain lifestyle intervention (FINGER). Alzheimers Dement. 18, 1325–1334. https://doi.org/10.1002/alz.12492 (2022).
Kulmala, J. et al. Facilitators and barriers to implementing lifestyle intervention programme to prevent cognitive decline. Eur. J. Public Health 31, 816–822. https://doi.org/10.1093/eurpub/ckab087 (2021).
Coley, N. et al. Adherence to multidomain interventions for dementia prevention: data from the FINGER and MAPT trials. Alzheimers Dement. 15, 729–741. https://doi.org/10.1016/j.jalz.2019.03.005 (2019).
Coley, N. et al. Disparities in the participation and adherence of older adults in lifestyle-based multidomain dementia prevention and the motivational role of perceived disease risk and intervention benefits: an observational ancillary study to a randomised controlled trial. Alzheimers Res. Ther. 13, 157. https://doi.org/10.1186/s13195-021-00904-6 (2021).
Noben, C. Y., Evers, S. M., Nijhuis, F. J. & de Rijk, A. E. Quality appraisal of generic self-reported instruments measuring health-related productivity changes: a systematic review. BMC Public Health 14, 115. https://doi.org/10.1186/1471-2458-14-115 (2014).
Acknowledgements
The authors would like to thank the participants in this study, all the staff and volunteers who participated.
Funding
This study was funded by the National Natural Science Foundation of China (72104050) and the Joint Funds for the Innovation of Science and Technology, Fujian Province (Grant number: 2020Y9021). The research funding was primarily used for data collection and software development.
Author information
Authors and Affiliations
Contributions
RL and YJY were responsible for the study conception and design, data collection/analysis, drafting of manuscript. HL and MFC as a supervision, administrative/critical revisions for important intellectual content. CSH: critical revision/technical/ supervision, technical and material support. JYZ: data analysis and supervision. All authors provided critical feedback and helped shape the research, analysis and manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lin, R., Yan, Y., Huang, C. et al. Development and usability of the “Cognitive Evergreenland” app to engage individuals at high risk of dementia in lifestyle interventions. Sci Rep 15, 9004 (2025). https://doi.org/10.1038/s41598-025-92535-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-92535-2