Abstract
The initiation of tofersen, a new specific antisense oligonucleotide (ASO) for SOD1 pathology, marked a significant turning point for SOD1-ALS patients. While clinical trials and early access program studies reported a significant reduction in plasma and cerebrospinal fluid (CSF) neurofilament levels, neuroinflammation following prolonged treatment was never assessed. In this multicenter study, we evaluated a cohort of 18 SOD1-ALS patients treated with tofersen, analyzing correlations between biomarkers of neurodegeneration/neuroinflammation and clinical variables indicative of disease progression. NfL, NfH, CHI3L1, and Serpina1 levels in serum and CSF were determined by semi-automated immunoassays (Ella™ technology). Generalized linear mixed models were employed to investigate longitudinal trends of these biomarkers. Our data highlighted a progressive decrease in CSF neurofilament levels during tofersen treatment (MR = 0.97, 95% CI 0.94–0.99, p = 0.006 and MR = 0.98, 95% CI 0.95–1.00, p = 0.076 for NfL and NfH in CSF, respectively). Conversely, CSF levels of SerpinA1 and CHI3L1 increased over time (MR = 1.12, 95% CI 1.08–1.16, p < 0.0001 and MR = 1.039, 95% CI 1.015–1.062, p = 0.001 for SerpinA1 and CHI3L1 in CSF, respectively), but these modifications were most apparent after six and twelve months of therapy, respectively. Disease progression rate did not correlate with these biomarker trends. We observed a significant decrease in neurofilament levels during Tofersen treatment, alongside an increase in neuroinflammatory markers, potentially linked to an immune response triggered by ASO treatment. Given the limited data on tofersen’s long-term efficacy in ALS due to its recent introduction, identifying biomarkers that predict clinical outcomes such as diminished therapeutic response or adverse effects is crucial. These biomarkers may help to better understand the underlying pathomechanisms of ALS and tofersen’s role in modulating disease progression.
Similar content being viewed by others
Introduction
Mutations in Cu/Zn superoxide dismutase (SOD1) are detected in approximately 2% of sporadic ALS (sALS) cases1 and 10% of familial ALS (fALS) cases within the European population2. Over 200 distinct SOD1 variants have been reported, displaying highly variable penetrance and geographical distribution2. For instance, the A5V mutation is more prevalent in North America3, D91A is predominantly found in Europe4, and H47R is more common in Japan5. Although the precise mechanisms by which SOD1 gene variants lead to motor neuron degeneration in ALS remain unclear, they are mainly believed to confer a toxic gain of function to the SOD1 protein6, typically resulting in leg weakness with predominantly lower motor neuron signs as the most common clinical presentation7. Tofersen (BIIB067), an intrathecal antisense oligonucleotide (ASO), received accelerated approval from the United States Food and Drug Administration (FDA) in April 2023 for the treatment of SOD1-ALS. This approval was based on its ability to reduce SOD1 protein levels and decrease plasma neurofilament light chain (NfL), a neurodegeneration and prognostic ALS biomarker8. A phase I/II trial (NCT02623699) indicated that the cerebrospinal fluid (CSF) concentrations of SOD1 protein were reduced across four dose cohorts, with the 100 mg-dose Tofersen group exhibiting a slower decline in ALS Functional Rating Scale-Revised (ALSFRS-R) scores compared to the placebo group9. However, in the phase III VALOR study (NCT02623699), no statistically significant difference was observed in the ALSFRS-R score changes between the tofersen and placebo groups, despite reductions in SOD1 protein concentration in CSF and NfL in plasma among Tofersen-treated8. Notably, during the open-label extension (OLE) period, patients who received early access to Tofersen exhibited a slower decline in ALSFRS-R scores compared to those with delayed access8. Based on these findings, an Early Access Program (EAP) was initiated to provide tofersen to ALS patients with SOD1 gene mutations (SOD1-ALS) outside clinical trials.
In Italy, the EAP was approved in November 2021, and in May 2024, the European Medicines Agency (EMA) granted marketing authorization for Tofersen under exceptional circumstances. Following the EAP’s commencement in Europe, several longitudinal studies were conducted, reinforcing the results from the VALOR study and its OLE phase. These studies demonstrated reductions in serum and CSF NfL levels10,11,12 as well as phosphorylated neurofilament heavy chain (NfH) CSF levels10. These findings allowed for the analysis of patients’ clinical progression and biomarker dynamics before and during tofersen treatment. As part of an extended real-world study, this Italian multicenter investigation aimed to explore how, in addition to neurofilaments, other markers of neuroinflammation change during repeated intrathecal administration of tofersen in SOD1-ALS patients, and whether these biomarker changes correspond to variations in clinical measures of ALS.
Results
Demographic and clinical features at baseline
A total of 18 SOD1-ALS patients were enrolled, with recruitment starting on November 21, 2021, and the final clinical and biomarker assessment was conducted on February 29, 2024. This resulted in 140 observations over the study period, with each participant having at least four observations during tofersen administration. The median follow-up time after the first tofersen administration was 19.94 months [IQR: 16.14–29.10]. Supplementary Table 1 details the number of observations and any missing values for each variable. Before the initiation of tofersen, one patient (5.56%) was already receiving PEG feeding, and five patients (29.41%) were on non-invasive ventilation (NIV). None exhibited signs or symptoms of FTD. The primary clinical characteristics of these patients are summarized in Table 1.
Three patients (two males and one female) were classified as fast progressors. Supplementary Table 2 presents the specific SOD1 mutations in our cohort and their correlation with selected clinical variables. The cohort generally exhibited prolonged diagnostic delays and slow disease progression rates at baseline. However, one patient was a carrier of the A5V mutation, associated with a more aggressive form of the disease. During follow-up, 2 out of 17 patients (11.76%) required PEG insertion due to worsening dysphagia, and 1 out of 12 (8.33%) initiated NIV. During tofersen treatment, 3 patients (16.67%) died from respiratory failure, with an average survival of 18.07 ± 2.90 months after the first tofersen infusion.
Regarding adverse events related to tofersen administration, 6 out of 18 patients experienced post-procedural headaches, with 2 developing signs of aseptic meningitis. These cases were managed with a short course of steroid therapy, with no further complications and without discontinuation of tofersen (for further details refer to supplementary materials in the captions of Figs. 1 and 2). Among serious adverse events, two patients experienced prolonged hospitalization due to respiratory insufficiency. One patient recovered following antibiotic and anticoagulant therapy (due to concurrent pulmonary thromboembolism) and NIV, while the other underwent a tracheostomy.
Baseline biomarker concentrations and correlations among biomarkers, demographic, and clinical variables
Biomarker analyses were performed on serum and CSF samples collected from patients undergoing tofersen treatment, with samples taken at baseline (before the first dose) and at subsequent administration time points.
Table 2 shows the serum and CSF concentrations of the biomarkers at baseline. Supplementary Table 3 shows the coefficient of variations for each analyte. We found a strong correlation between CSF levels of NfL and NfH (rho = 0.94, p < 0.001) and between CSF levels of NfL and CHI3L1 (rho = 0.56, p = 0.027) at baseline. Serum-CSF concentrations correlations for each type of biomarker revealed a significant correlation for NfL (rho = 0.87, p < 0.001), while for the other analytes the concentrations in the two compartments tended to differ. This strong correlation was maintained over time during Tofersen administration, particularly at 3, 9, and 15 months (rho = 0.64, p = 0.015; rho = 0.70, p = 0.009; rho = 0.85, p = 0.003, respectively) after the first injection. On the other hand, NfH and CHI3L1 concentrations tended to correlate but without reaching statistical significance only at baseline (rho = 0.50, p = 0.10 and rho = -0.57, p = 0.096 for NfH and CHI3L1, respectively).
Table 3 reports the baseline correlations among biomarkers and demographic and clinical variables.
Changes in biomarkers during tofersen administration
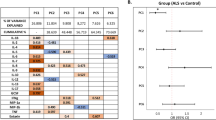
Descriptive statistics for each biomarker concentration at predefined time points is reported in Table 4. During the first 18 months of treatment, we observed a significant and progressive decrease of NfL and NfH in the CSF, especially during the first year of treatment, and a progressive increase in the CSF concentrations of SerpinA1 and CHI3L1 levels. Figure 1 displays the individual and average trends of logarithmic concentrations of biomarkers in CSF over time (expressed as days after the first tofersen infusion). Neurofilaments levels decreased over time, with pronounced reductions in CSF and serum NfL, and less evident changes in NfH, especially during the first year of tofersen treatment. Some subjects later exhibited stabilization or an increase in NfL and NfH concentrations. Baseline NfL concentrations in CSF decreased by an average 3% for every month of tofersen administration (MR = 0.97, 95% CI: 0.94–0.99, p = 0.006), while in serum by an average 5% (MR = 0.95, 95% CI 0.93–0.98, p = 0.002). Neither NfH in CSF (MR = 0.98, 95% CI 0.95–1.00, p = 0.076) nor NfH in serum significantly decreased over time after tofersen administration (MR = 0.95, 95%CI 0.87–1.04, p = 0.29). SerpinA1 increased after tofersen administration by an average of 12% monthly in CSF and, to a lesser extent, in serum. Similarly, CHI3L1 levels rose both in CSF and in serum by an average of 0.39% and 0.17% in CSF and serum respectively. When looking at individual modifications of these two biomarkers, these changes were most apparent after the first year of tofersen treatment.
Clinical features and change in biomarkers levels during tofersen administration
We first evaluated the longitudinal trajectory of ALSFRS-R and DPR during the administration of tofersen (Fig. 2). For each month after the first tofersen administration, ALSFRS-R changed on average of − 0.25 points/month (mean difference: − 0.245, 95%CI − 0.38–0.11, p < 0.001) while DPR did not significantly modify during the observation period (mean difference: − 0.006, 95% CI − 0.013–0.0005, p = 0.068). Subsequently, we evaluated the relationship between the change in DPR, calculated as the difference between the value at six and twelve months (T6 and T12, respectively) compared to the baseline value (T0), and the concentration of each biomarker at the three time-points considered. In particular, we aimed to test whether modifications in biomarkers during tofersen administration reflected how DPR could modify as well during treatment (Table 5).
Then, we evaluated in a multivariable mixed-effect model the effect of all measured CSF biomarkers on ALSFRS-R score changes over time, finding that none of them correlated with the score variations after tofersen administration (mean difference for each pg/ml of NfL increase in ALSFRS-R: − 0.000022, 95% CI − 0.00011–0.000063, p = 0.61).
Factors affecting neurofilaments modifications during tofersen treatment
Next, we sought to determine whether the decrease in neurofilament levels over time with tofersen administration was influenced by other clinical factors and interrogated generalized linear mixed-effects models for that. In our initial multivariable mixed-effects model, we included baseline age, gender, baseline DPR (disease progression rate), and the time from disease onset to the first tofersen administration. The results of this analysis are presented in Table 6.
This analysis showed that the time lag between the onset of the disease and the first tofersen administration was associated with a modest decrease (almost 1% monthly) in baseline serum NfL. NfH concentrations in serum and CSF were better associated with baseline disease progression rates than the duration of treatment per se, though tofersen duration of therapy effect was confirmed in serum NfH, and gender could impact as well on this biomarker. SerpinA1 and CHI3L1 modified over time since the first tofersen administration in line with the trends described in the above paragraphs. Moreover, serum CHI3L1 seemed to positively associate with baseline age and with ALS duration history, while baseline DPR seemed to correlate positively with rises in serum CHI3L1.
Finally, we evaluated how neuroinflammation, represented by SerpinA1 and CHI3L1, could influence neurofilaments over time. In particular, only CHI3L1 was significantly associated with neurofilament levels, with a 0.18% increase in the average concentration of NfL in the CSF for each one ng/ml rise of CSF CHI3L1 (MR = 1.0018, 95% CI 1.000–1.003, p = 0.028).
Discussion
The present study aimed to characterize the clinical and biological features of a small cohort of SOD1-ALS patients undergoing tofersen treatment for up to 18 months. In our exploratory study, a reduction in CSF neurofilaments (NfL and NfH) was confirmed during tofersen treatment, consistent with previous reports10,11,12,13. However, this decline appeared to plateau after one year of therapy. Among the two neurofilament isoforms, NfL showed a more pronounced reduction, with an average monthly decrease of 3% in CSF and 5% in serum following each tofersen administration. On the other hand, longitudinal studies on peripheral concentrations of neurofilaments in ALS patients not receiving any active treatment suggest serum NfL is rather stable during ALS progression14,15, while data on NfH are more contrasting16.
Importantly, we observed that tofersen treatment may be associated with an increase in neuroinflammatory biomarkers, specifically SerpinA1 and CHI3L1, both of which have been previously investigated as prognostic biomarkers in ALS17,18,19. CHI3L1 exhibited a slower rate of increase compared to SerpinA1, reaching significant levels only after 12 months of treatment. Interestingly, CHI3L1 has also been measured in patients with Spinal Muscular Atrophy (SMA) receiving ASO treatment with intrathecal Nusinersen, where its decline was associated with clinical improvements in SMA types 3 and 420. Conversely, CHIT1, another marker of neuroinflammation, showed a progressive increase after repeated lumbar punctures21. Longitudinal studies in untreated ALS patients suggest both plasma and CSF concentrations of CHI3L1 are stable22.
In our model based on 18 ALS-SOD1 patients, CHI3L1—a biomarker associated with chronic neuroinflammation19—appeared to have a mild effect on CSF NfL levels, leading to a modest 0.18% increase for each additional ng/mL of CSF CHI3L1. In our exploratory cohort, CHI3L1 significantly increased after one year of continuous treatment, coinciding with the observed attenuation in the decline of neurofilament levels in CSF. This general rise in neuroinflammatory biomarkers in the CSF could suggest an ongoing inflammatory response, which may be a compensatory mechanism or a side effect of the treatment, i.e. due to physical trauma from repeated lumbar punctures or from ASO administration itself. Alternatively, these changes may reflect a heightened protective neuroinflammatory response to the disease. Given the relatively recent introduction of ASO therapies, our understanding of their impact on neuroinflammation in ALS remains limited. Thus, it is essential to monitor neuroinflammatory patterns closely to enhance our understanding of ALS pathogenesis. Similar considerations apply to nusinersen treatment in SMA20,23.
Several studies have proposed a neuroprotective role for SerpinA1 due to its anti-inflammatory properties, including its capacity to modulate pro-inflammatory microglia and inhibit protein aggregation24,25. Research on mutant SOD1 (mSOD1G93A) mice has shown that microglial activation occurs early in ALS and intensifies as the disease progresses, suggesting that microglia may contribute to disease progression26. This was further corroborated by in vivo PET imaging studies in SOD1 mutation carriers, which demonstrated microglial activation in cortical and subcortical regions during the pre-symptomatic phase, with involvement of the sensorimotor cortex as symptoms emerged27.
Both central and peripheral immune systems undergo dynamic changes during the disease, with early-stage signals from motoneurons attempting to repair damaged tissue. However, in later stages, beneficial immune reactions (involving M2 microglia and regulatory T cells) transition to harmful ones (involving M1 microglia and Th1 cells)28. Given that patients in this study began tofersen treatment approximately 46 months after the onset of symptoms, the elevated CSF concentrations of SerpinA1 and CHI3L1 could reflect the advanced neuroinflammatory state of the disease with microglia likely becoming neurotoxic.
Our findings, like those previously reported17,21,24,29, confirm that DPR was closely correlated with baseline CSF levels of neurofilaments and CHI3L1.
A recent study demonstrated that tofersen treatment increased levels of various selenium species, including neurotoxic species, as well as selenoprotein P, a selenium-transporting enzyme30. These molecules exhibit a dual role, shifting from regulatory functions in redox reactions to neurotoxic effects by altering the cytoskeleton and inducing proteomic changes. This bivalent behaviour dependent on complex environmental factors seems to be a common denominator in ALS-related neuroinflammation.
Moreover, SerpinA1 concentrations increased significantly within the first few months of treatment, indicating a potential early anti-inflammatory response that may eventually transition into a more toxic phase despite the overall increase in neuroinflammation.
ASOs represent an innovative approach to precision therapy for neurodegenerative diseases. However, as evidenced by our data and corroborated in the literature31 they may induce immunological or inflammatory responses that warrant further investigations. For example, 11.11% of our patients developed aseptic meningitis, a complication also reported during the treatment of SMA with nusinersen23,32. Thus, exaggerated intrathecal immune responses during the treatment with ASOs must be carefully monitored, and further research is needed to elucidate the underlying mechanisms and predictive factors for risk stratification.
A major limitation of the present study is its small sample size and the phenotypic heterogeneity, partly related to different SOD1 mutations33, and the variability of disease durations before the first tofersen administration. Additionally, as a real-world study, our dataset included more missing values compared to clinical trials. We cannot rule out the risk of overgeneralization given the small sample size and the heterogeneous nature of SOD1-associated ALS. Therefore, larger studies including a broader range of subjects across the full spectrum of SOD1-ALS are recommended before making further biological hypotheses regarding the effect of tofersen in these patients. Correction with multiple testing, which was not performed in this study, could be employed to partly overcome the limits imposed by the small sample size. Finally, given the observational nature of the study, causality cannot be comprehensively established and should be investigated with pre-clinical models.
Despite these limitations, our study confirmed the significant decrease in neurofilaments in both serum and CSF, as reported by the VALOR study8 and other ‘real world’ studies10,11,12. An added value of our work lies in the evaluation of both systemic and central inflammation markers alongside clinical data and biomarkers of neuroinflammation during tofersen treatment, showing significant increases in SerpinA1 and CHI3L1. No single biomarker can encapsulate all the complex pathological mechanisms at play in a heterogeneous disease like ALS, especially when considering inflammatory markers, which are involved in numerous signalling networks34. Therefore, a panel of multiple biomarkers is likely better suited to capture the dynamic signatures associated with different stages of ALS and to identify optimal treatment strategies for patients most likely to benefit from immunomodulatory therapies.
Our study, though very exploratory in nature, seeks to fill some of the gaps in understanding disease progression and the effects of a new precision therapy. However, these findings require further validation in larger cohorts of patients and with longer follow-ups to mitigate data instability and to better determine the role of these biomarkers in predicting therapeutic response versus potential side effects.
Conclusions
In conclusion, tofersen shows potential as a therapeutic option for SOD1-ALS, with significant effects on neurodegeneration markers. However, the associated observed inflammatory response following prolonged intrathecal treatment requires careful monitoring, and further studies are required to ensure the long-term safety and efficacy of the treatment.
Methods
Study cohort
This retrospective cohort study enrolled 18 SOD1-ALS patients treated with Tofersen under the EAP in four major Italian ALS centers: Padua, Naples, Milan, and Modena. Clinical data along with CSF and serum samples from these patients were collected longitudinally every three months by each center. None of the patients in this cohort participated in the VALOR study. According to the EAP protocol, ALS patients with SOD1 mutations were treated with an intrathecal administration of 100 mg tofersen, beginning with a loading dose on days 1, 14, and 28, followed by a maintenance phase where the drug was administered every 28 days. Following the baseline measurement, coinciding with the first intrathecal tofersen administration, clinical and biomarker assessments were conducted every three months, according to each center clinical practice, until February 29, 2024. The last observation for this study was set at June 30, 2024. Biomarker assessments were contingent upon sample availability from each center. This research was conducted according to the Declaration of Helsinki guidelines.
Ethics
The EAP for tofersen administration in SOD1-ALS patients was priorly approved by the Ethics Committee for all patients enrolled in the participating centers. Before enrolment in the EAP, patients provided written informed consent. Next, this research received approval from the Ethics Committee of Area Vasta Emilia Nord (file number: 63/2022).
Clinical variables
Demographic and clinical variables were recorded at baseline visit, including sex, age at onset, diagnostic latency, family history for ALS and/or frontotemporal dementia (FTD), site of onset (bulbar, upper limb or lower limb, respiratory), and ALS phenotype (classic, bulbar, upper motor neuron predominant, flail arm, flail leg, respiratory and progressive muscular atrophy ALS)35. Anthropometric measurements such as weight, height, and Body Mass Index (BMI) were documented along with baseline weight loss36, defined as the difference in kilograms between body weight before symptom onset and body weight at the first tofersen administration.
At each subsequent administration of tofersen, the ALSFRS-R total score and the disease progression rate (DPR)—defined as the monthly decline in the ALSFRS-R total score over a specific time interval—were calculated37. Respiratory function was assessed by force vital capacity (FVC). Additional clinical data including time to non-invasive ventilation (NIV), invasive ventilation (IV), percutaneous endoscopic gastrostomy (PEG), and death, were also collected.
Patients were classified into slow, intermediate, or fast progressors based on the following DPR cut-offs: less than 0.5 for slow, between 0.5 and 1 for intermediate, and greater than 1 for fast progressors38. Cognitive and behavioural impairment within the FTD spectrum were evaluated according to Strong criteria39. All treatments were recorded, including Riluzole, and other supplementation therapies such as L-acetyl carnitine and vitamins.
SOD1 mutations were classified according to the exon localization, and amino acid sequence conservation was analyzed using ConSurf (https://consurf.tau.ac.il) 40. The functional impact of mutations on the SOD1 protein was interpreted using PredictSNP (https://loschmidt.chemi.muni.cz/predictsnp) as previously reported41,42.
Sample collection and laboratory assays
Serum and CSF samples were obtained by venipuncture and lumbar puncture, respectively, processed as previously reported29,43, and stored in polypropylene tubes at − 80 °C until analysis. All samples were centralized and finally processed for biomarker quantification in Modena laboratory with a semi-automated immunoassay, the Ella™ microfluidic platform (BioTechne, ProteinSimple, San Jose, California, 95,134 USA), which has been already tested for neurofilaments in patients with ALS and other neurodegenerative diseases44,45. NfL, pNfH, SerpinA1, and chitinase 3 like-1 (CHI3L1) levels were determined according to manufacturer’ instructions using the following dilutions: 1:2 for both serum and CSF for NfL, 1:2 for serum and 1:4 for CSF for NfH, 1:200.000 and 1:10.000 for serum and CSF for SerpinA1; 1:10 and1:100 for serum and CSF for CHI3L117. The manufacturer priorly evaluated intra-assay and inter-assay variability for each batch and their values are shown in Supplementary Table 4.
Statistical analysis
Continuous variables were reported as means (standard deviations, SD) or medians [interquartile ranges, IQR], according to their distribution, and categorical variables as absolute numbers (percentages, %). As this was an observational multicenter study, serum samples were not consistently available for all participants at each time point, unlike in controlled clinical trials. Missing values were handled without applying any imputation method.
We evaluated clinical and demographic features by performing two-tailed t-tests and ANOVA for continuous variables between two groups or multiple groups, respectively, and a chi-square test for comparisons between categorical variables. Since all biomarkers had left-skewed, non-parametric tests were used to compare two or multiple groups, with Mann–Whitney U tests or Wilcoxon tests, respectively. Correlations among biomarkers and between biomarkers and clinical variables were assessed by Spearman correlation coefficient. A p-value less than 0.05 was considered statistically significant.
To describe biomarker concentrations after tofersen administration, concentrations were initially considered at defined time points roughly every three months, that is, at T0 (baseline, when first Tofersen administration was performed), T3 (84 days ± 15 since baseline), T6 (168 days ± 18 since baseline), T9 (252 days ± 20 since baseline), T12 (336 days ± 30 since baseline), T15 (420 days ± 30 since baseline) and T18 (504 days ± 30 since baseline). Once we organized the dataset according to this temporal order, we first tested whether differences existed, for each biomarker under investigation, between matched-pairs of observations, that is, between each time-point and baseline, and then between each time point and three months before for each subject for whom these observations were available. Differences were tested by Wilcoxon matched-pairs signed-rank test and a p-value less than 0.05 was considered as statistically significant. To account for a more general trajectory of each biomarker during Tofersen treatment, a generalized mixed-effect model was applied, generalizing previously tested linear regression models for longitudinal trajectories of neurofilaments14. The following biomarkers were considered as the dependent variable in separate models: NfL in CSF and serum (pg/ml), NfH in CSF and serum (pg/ml), SerpinA1 in CSF and serum (µg/ml), CHI3L1 in CSF and serum (ng/ml). Firstly, unadjusted models including time from baseline (months) as the only independent variable were estimated to describe the observed linear trend over time. Next, a multivariable model was used to estimate the effect of clinical and demographic variables on each biomarker longitudinal trajectory, including the following covariates: age at baseline (years)14, time since onset of disease to baseline (one month), gender (males versus females), and DPR at baseline (+ 1 point/months). None of these explanatory variables was time-varying. For both NfL and NfH, a second multivariable model was run to estimate the effect of CHI3L1 and SerpinA1 on their longitudinal course following Tofersen treatment, either in CSF or in serum. An individual random intercept term was included in all models to allow the average value of the outcome to vary between patients; also, an individual random slope term was included for unadjusted models and in multivariable models. Each biomarker was analysed using a multiplicative effect generalized linear mixed model with gamma distribution and log link function; results were reported as the mean ratio (MR) with a 95% confidence interval (CI). A mean ratio equal to one implies the explanatory variable has an estimated average 0% effect on the biomarker; any increase or decrease in the mean ratio over one suggests there is an average percentage increase or decrease in the biomarker compared to reference values. For a better visualization of individual trajectories of CSF neurofilaments, CHI3L1 and SerpinA1 over time, logarithmic transformation was applied to these biomarker values and the confidence intervals of linear regression models estimates were displayed in Fig. 1 as shadowed areas.
Average variations in ALSFRS-R and DPR over time were similarly tested with a generalized linear mixed-effects model with Gaussian distribution and additive effect, with time in months since the first Tofersen administration as the only explanatory variable. To investigate whether any biomarker variations could explain average changes in ALSFRS-R or DPR, each single biomarker in serum and CSF (tested separately) was included in the multivariable model.
Data analysis was performed using STATA statistical package 18 (StataCorp. 2023. College Station, TX: StataCorp LLC).
Data availability
Individual deidentified participant data, including clinical and biological assessments, will be shared with any qualified investigator upon reasonable requests made to the corresponding author.
References
Ruf, W. P. et al. Spectrum and frequency of genetic variants in sporadic amyotrophic lateral sclerosis. Brain Commun. 5, fcad152 (2023).
Zou, Z.-Y. et al. Genetic epidemiology of amyotrophic lateral sclerosis: a systematic review and meta-analysis. J. Neurol. Neurosurg. Psychiatry 88, 540–549 (2017).
Saeed, M. et al. Age and founder effect of SOD1 A4V mutation causing ALS. Neurology 72, 1634–1639 (2009).
Berdyński, M. et al. SOD1 mutations associated with amyotrophic lateral sclerosis analysis of variant severity. Sci. Rep. 12, 103 (2022).
Arisato, T. et al. Clinical and pathological studies of familial amyotrophic lateral sclerosis (FALS) with SOD1 H46R mutation in large Japanese families. Acta Neuropathol. (Berl.) 106, 561–568 (2003).
Sau, D. et al. Mutation of SOD1 in ALS: A gain of a loss of function. Hum. Mol. Genet. 16, 1604–1618 (2007).
Bernard, E. et al. Clinical and molecular landscape of ALS patients with SOD1 mutations: Novel pathogenic variants and novel phenotypes. A single ALS center study. Int. J. Mol. Sci. 21, 6807 (2020).
Miller, T. M. et al. Trial of antisense oligonucleotide tofersen for SOD1 ALS. N. Engl. J. Med. 387, 1099–1110 (2022).
Benatar, M. et al. Design of a randomized, placebo-controlled, phase 3 trial of tofersen initiated in clinically presymptomatic SOD1 variant carriers: The ATLAS study. Neurotherapeutics 19, 1248–1258 (2022).
Wiesenfarth, M. et al. Effects of tofersen treatment in patients with SOD1-ALS in a “real-world” setting—A 12-month multicenter cohort study from the German early access program. eClinicalMedicine 69, 102495 (2024).
Meyer, T. et al. Neurofilament light-chain response during therapy with antisense oligonucleotide tofersen in SOD1-related ALS: Treatment experience in clinical practice. Muscle Nerve 67, 515–521 (2023).
Sabatelli, M. et al. Long-term treatment of SOD1 ALS with tofersen: A multicentre experience in 17 patients. J. Neurol. https://doi.org/10.1007/s00415-024-12437-7 (2024).
Meyer, T. et al. Clinical and patient-reported outcomes and neurofilament response during tofersen treatment in SOD1-related ALS—A multicenter observational study over 18 months. Muscle Nerve (2024).
Benatar, M. et al. Validation of serum neurofilaments as prognostic and potential pharmacodynamic biomarkers for ALS. Neurology 95, e59–e69 (2020).
Meyer, T. et al. Serum neurofilament light chain in distinct phenotypes of amyotrophic lateral sclerosis: A longitudinal, multicenter study. Eur. J. Neurol. 31, e16379 (2024).
Simkins, T. J. et al. Plasma neurofilament analysis in VITALITY-ALS. Amyotroph. Lateral Scler. Front. Degener. 26, 103–112 (2025).
Martinelli, I. et al. SerpinA1 levels in amyotrophic lateral sclerosis patients: An exploratory study. Eur. J. Neurol. 31, e16054 (2024).
Rosén, C. et al. High levels of neurofilament light and YKL-40 in cerebrospinal fluid are related to poor outcome in ALS. J. Neurol. Sci. 463, 123112 (2024).
Xu, A. et al. Chitinases as a potential diagnostic and prognostic biomarker for amyotrophic lateral sclerosis: A systematic review and meta-analysis. Neurol. Sci. 45, 2489–2503 (2024).
De Wel, B., De Schaepdryver, M., Poesen, K. & Claeys, K. G. Biochemical and clinical biomarkers in adult SMA 3–4 patients treated with nusinersen for 22 months. Ann. Clin. Transl. Neurol. 9, 1241–1251 (2022).
Freigang, M. et al. Increased chitotriosidase 1 concentration following nusinersen treatment in spinal muscular atrophy. Orphanet J. Rare Dis. 16, 330 (2021).
Vu, L. et al. Cross-sectional and longitudinal measures of chitinase proteins in amyotrophic lateral sclerosis and expression of CHI3L1 in activated astrocytes. J. Neurol. Neurosurg. Psychiatry 91, 350–358 (2020).
Yao, X. et al. Nusinersen effectiveness and safety in pediatric patients with 5q-spinal muscular atrophy: A multi-center disease registry in China. J. Neurol. 271, 5378–5391 (2024).
Gold, M. et al. α1-antitrypsin modulates microglial-mediated neuroinflammation and protects microglial cells from amyloid-β-induced toxicity. J. Neuroinflammation 11, 165 (2014).
Zsila, F. Inhibition of heat- and chemical-induced aggregation of various proteins reveals chaperone-like activity of the acute-phase component and serine protease inhibitor human α1-antitrypsin. Biochem. Biophys. Res. Commun. 393, 242–247 (2010).
Xiao, Q. et al. Mutant SOD1 G93A microglia are more neurotoxic relative to wild-type microglia. J. Neurochem. 102, 2008–2019 (2007).
Tondo, G. et al. 11 C-PK11195 PET–based molecular study of microglia activation in SOD1 amyotrophic lateral sclerosis. Ann. Clin. Transl. Neurol. 7, 1513–1523 (2020).
Zhao, W., Beers, D. R. & Appel, S. H. Immune-mediated mechanisms in the pathoprogression of amyotrophic lateral sclerosis. J. Neuroimmune Pharmacol. 8, 888–899 (2013).
Zucchi, E. et al. Cerebrospinal fluid neurofilaments may discriminate upper motor neuron syndromes: A pilot study. Neurodegener. Dis. 18, 255–261 (2018).
Vinceti, M. et al. Changes in cerebrospinal fluid concentrations of selenium species induced by tofersen administration in subjects with amyotrophic lateral sclerosis carrying SOD1 gene mutations. Biol. Trace Elem. Res. https://doi.org/10.1007/s12011-024-04311-4 (2024).
Reilich, P. et al. Myelitis as a side effect of tofersen therapy in SOD1-associated ALS. J. Neurol. 271, 2114–2118 (2024).
Moshe‐Lilie, O., Riccelli, L. P. & Karam, C. Possible recurrent aseptic meningitis associated with nusinersen therapy. Muscle Nerve 62, (2020).
Opie-Martin, S. et al. The SOD1-mediated ALS phenotype shows a decoupling between age of symptom onset and disease duration. Nat. Commun. 13, 6901 (2022).
Gaur, N., Perner, C., Witte, O. W. & Grosskreutz, J. The Chitinases as biomarkers for amyotrophic lateral sclerosis: Signals from the CNS and beyond. Front. Neurol. 11, 377 (2020).
Gianferrari, G. et al. Epidemiological, clinical and genetic features of ALS in the last decade: A prospective population-based study in the Emilia Romagna Region of Italy. Biomedicines 10, 819 (2022).
Fasano, A. et al. Percutaneous endoscopic gastrostomy, body weight loss and survival in amyotrophic lateral sclerosis: a population-based registry study. Amyotroph. Lateral Scler. Front. Degener. 18, 233–242 (2017).
Mandrioli, J. et al. Heterogeneity in ALSFRS-R decline and survival: a population-based study in Italy. Neurol. Sci. 36, 2243–2252 (2015).
Lu, C.-H. et al. Neurofilament light chain: A prognostic biomarker in amyotrophic lateral sclerosis. Neurology 84, 2247–2257 (2015).
Strong, M. J. et al. Amyotrophic lateral sclerosis—Frontotemporal spectrum disorder (ALS-FTSD): Revised diagnostic criteria. Amyotroph. Lateral Scler. Front. Degener. 18, 153–174 (2017).
Ashkenazy, H. et al. ConSurf 2016: an improved methodology to estimate and visualize evolutionary conservation in macromolecules. Nucleic Acids Res. 44, W344-350 (2016).
Bendl, J. et al. PredictSNP: robust and accurate consensus classifier for prediction of disease-related mutations. PLoS Comput. Biol. 10, e1003440 (2014).
Martinelli, I. et al. The landscape of cognitive impairment in superoxide dismutase 1-amyotrophic lateral sclerosis. Neural Regen. Res. 18, 1427 (2023).
Simonini, C. et al. CSF heavy neurofilament may discriminate and predict motor neuron diseases with upper motor neuron involvement. Biomedicines 9, 1623 (2021).
Witzel, S. et al. Population-based evidence for the use of serum neurofilaments as individual diagnostic and prognostic biomarkers in amyotrophic lateral sclerosis. Ann. Neurol. 96, 1040–1057 (2024).
Fazeli, B. et al. Quantification of blood glial fibrillary acidic protein using a second-generation microfluidic assay. Validation and comparative analysis with two established assays. Clin. Chem. Lab. Med. 62, 1591–1601 (2024).
Acknowledgements
The authors acknowledge the other members who contributed to data collection and analysis: Nicola Fini, Eleonora Leopizzi, Andrea Ghezzi, Francesca Prompicai, Silvia Parisi, and Roberta Bedin; Giuliana Federico, Aida Molares Zulueta, Camilla Garrè, Riccardo Sideri.
Funding
This study was supported by grants from the Ministero della Salute, Ricerca Finalizzata bando 2021 (RF-2021-12373036), by the University of Modena and Reggio Emilia (bando FAR 2021, Progetti di ricerca Interdisciplinari Mission Oriented, NEURALS project), and by Fondazione Cassa di Risparmio di Modena (Neurobiobanca di Modena).Moreover, the research was supported by the Ricerca Corrente funding scheme of the Italian Ministry of Health.
Author information
Authors and Affiliations
Contributions
C.S, E.Z., and J.M. conceived and designed this study. C.S., E.Z., I.M., G.G., G.M., L.C., S.G., T.F., contributed to the acquisition of the data. E.Z. performed the statistical analysis with the methodological support of F.B., while C.S., E.Z., I.M., G.G., and J.M. all contributed to the data interpretation. C.S. and E.Z. wrote the initial draft of the article, while J.M. and F.B. critically revised the paper; all the authors have read, revised and approved the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Each patient’s EAP for tofersen administration was approved by the local Ethical Committees of all the participating centers prior to enrolment,while this observational study received approval from the Ethics Committee of Area Vasta Emilia Nord (file number: 63/2022).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Simonini, C., Zucchi, E., Martinelli, I. et al. Neurodegenerative and neuroinflammatory changes in SOD1-ALS patients receiving tofersen. Sci Rep 15, 11034 (2025). https://doi.org/10.1038/s41598-025-94984-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-94984-1