Abstract
Numerous studies demonstrate that intestinal microbiota contribute to colorectal cancer (CRC), which is often associated with dysbiosis. Most of the data were obtained from studies on CRC patients, making it challenging to determine whether alterations in microbiota are a consequence of the pathology or whether they actively drive its progression. Several studies using laboratory animals suggest that gut microbiota may be involved in both the onset and progression of CRC. In the present study we utilized the azoxymethane-dextran sulfate sodium (AOM/DSS) mouse model of CRC to investigate the contribution of healthy-state microbiota to inflammation-associated tumorigenesis. Two cohorts of C57BL/6 mice harboring different intestinal microbiota demonstrated different susceptibility to AOM/DSS treatment. Sequencing of 16S rRNA bacterial DNA from fecal samples revealed Akkermansia muciniphila and Bacteroides acidifaciens as marker features in the healthy-state microbiota (before AOM/DSS administration), which showed a strong positive correlation with tumor incidence. Moreover, the healthy-state abundance of these markers, considered beneficial bacteria, was strongly positively correlated with the sulfate-reducing bacteria Desulfovibrio fairfieldensis identified as a marker of chronic colitis-associated microbiota. Furthermore, the abundances of these marker features, associated with CRC outcome, correlated with the expression of interferon gamma and nitric oxide synthase 2 genes in colon tissue during the early stage of DSS-induced intestinal inflammation. In contrast to multiple studies demonstrating the anti-inflammatory properties of A. muciniphila and B. acidifaciens, our results point out their potential adverse effect under specific conditions of genotoxicity and inflammation in the intestine. Taken together, our findings suggest a complex, context-dependent role of commensal microbiota in inflammation-associated dysbiosis and CRC.
Similar content being viewed by others
Introduction
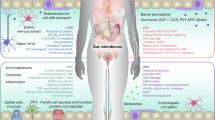
Colorectal cancer (CRC) is the third most common type of cancer and the second leading cause of cancer-related deaths1. The vast majority of CRC cases arise sporadically, suggesting a crucial role of environmental factors in the initiation and progression of tumorigenesis. Furthermore, intestinal inflammation contributes to CRC; in particular, inflammatory bowel diseases (IBD) are risk factors for CRC development2. Chronic inflammation promotes a tumorigenic microenvironment. On the one hand, it leads to DNA damage due to the accumulation of reactive oxygen species; on the other hand, it increases cell proliferative activity through the production of growth factors and angiogenesis3,4. Moreover, disturbances in the gut microbiota, resulting in dysbiosis, contribute to the initiation and progression of CRC5,6,7.
In a normal physiological state, the gut microbiota is relatively stable, although it may vary in response to environmental and dietary changes. It is recognized as playing a significant role in immunity and CRC pathogenesis8. According to some reports, alterations in intestinal microbiome composition and diversity are associated with CRC9,10,11,12. Different studies have revealed an increase or depletion of several gut bacteria contributing to host immunity in CRC patients compared to healthy controls. A number of pro-inflammatory bacteria, including enterotoxigenic Bacteroides fragilis, Fusobacterium spp., Enterococcaceae spp., Porphyromonas, Peptostreptococus, Escherichia coli, Shigella, and Streptococcus spp., were found to be enriched in patients with CRC10,11,13,14,15. Whereas some commensal bacteria known to promote anti-inflammatory responses, such as Faecalibacterium, Blautia, Clostridium, Bifidobacterium, Roseburia, Coprococcus, and Lachnospiraceae, were depleted in patients suffering from CRC10,11,14. It should be noted that most of the data were obtained from studies on CRC patients, which makes it difficult to determine whether dysbiosis results from tumorigenesis or drives the pathology. The investigation of mucosa-associated microbiome communities at different stages of colorectal neoplasm progression revealed distinct microbial signatures, the enrichment of which was confirmed in independent cohorts using publicly available data16. These findings imply dynamic changes of microbial communities during the progression of the pathology. An interesting model explaining the complex role of the microbiota in CRC was proposed by Tjalsma et al., namely, the “bacterial driver-passenger” theory17. This model suggests that the initiation of tumorigenesis is triggered by “driver” bacteria with pro-cancerogenic characteristics, such as genotoxicity and the induction of a robust inflammatory response. The onset and establishment of the tumor microenvironment result in significant physiological and metabolic alterations. “Passenger” bacteria, which typically colonize a healthy intestine poorly, take advantage of these alterations and outcompete “drivers”. This process results in dysbiosis and most likely promotes tumorigenesis17. However, the most microbiome studies in patients are limited to the stage of developed tumors and do not include data on the initial healthy-state microbiota of these patients. Therefore, revealing the role of baseline microbiota along with its dynamic changes during CRC pathogenesis remains to be performed.
Studies utilizing animal models enable the investigation of the role of particular microbes and the overall dynamic changes in microbiota composition throughout tumor development in the colon. There is a body of evidence supporting the role of microbiota in predisposition to colorectal tumorigenesis. It was demonstrated that mice sharing a genetic background, when housed in different rooms within the same animal facility or obtained from different facilities, exhibited distinct susceptibility to inflammation-associated tumorigenesis (AOM/DSS model). This variation is at least partially attributed to differences in immune activation caused by microbiota features18. Moreover, microbiota transfer from CRC patients increased susceptibility to tumor formation in mice after AOM injection19 and enhanced sporadic tumorigenesis in the ApcMin/+ genetic mouse model of CRC20. An interesting finding reported by S. Rosshart et al. revealed that germ-free mice colonized with a more diverse microbiota from wild mice, compared to those from laboratory mice, developed fewer tumors in the AOM/DSS model21. Zackular et al. demonstrated that the outcomes of the AOM/DSS model were influenced by the initial microbiota, as treatment with antibiotics prior to AOM injection decreased the size and number of tumors22. Furthermore, an experiment involving the transplantation of fecal microbiota from CRC patients and healthy donors in germ-free mice showed that the number of tumors was associated with the structure of the microbiota obtained. However, contrary to other studies, this finding did not correlate with the health status of the donors. Moreover, tumor burden was associated with specific features of the commensal microbiome, which were identified as belonging to the genera Bacteroides, Parabacteriodes, Alistipes, and Akkermansia muciniphila23. Therefore, baseline healthy-state commensal microbiota might promote inflammation-associated tumorigenesis by modulating the mucosal immune system and the epithelial cell’s physiology, as well as by shaping microbial communities through competition for nutrients and producing metabolites that are utilized by other microorganisms.
In the current study, we investigated the intestinal microbiota-associated susceptibility to colorectal tumorigenesis using the AOM/DSS mouse model. Two cohorts of C57BL/6 mice, bred in our facility and housed in separate rooms, exhibited distinct initial microbiota compositions and differed in susceptibility to inflammation-associated tumorigenesis. Sequencing of 16S rRNA bacterial DNA from fecal samples revealed marker features of the initial microbiota (before AOM/DSS administration) that were associated with AOM/DSS susceptibility and showed a strong positive correlation with the number of tumors. These features were annotated as common gut commensals Akkermansia muciniphila and Bacteroides acidifaciens. Moreover, the abundance of these markers in the initial microbiota was strongly positively correlated with a feature identified as a marker of chronic colitis-associated microbiota – Desulfovibrio fairfieldensis. Furthermore, the abundance of the observed marker features correlated not only with the number of tumors but also with the expression of interferon gamma and nitric oxide synthase 2 genes in the colon tissue at the early stage of DSS-induced intestinal inflammation. Taken together, our findings demonstrate a relationship between initial microbiota, dysbiosis associated with inflammation-associated tumorigenesis, and CRC outcomes.
Materials and methods
Animals and housing conditions
All procedures were performed under Russian legislation according to the standards of Good Laboratory Practice (directive # 267 from 19 June 2003 of the Ministry of Health of the Russian Federation), institutional Ethical committee guidelines, and the European Convention for the Protection of Vertebrate animals. All the protocols were approved by the Ethics Committee on Animal and Human Research of the Institute of Molecular and Cellular Biology (Novosibirsk, Russia), protocol №02/21, dated 04 August 2021. All animals were tested quarterly according to the Federation of European laboratory animal science association’s (FELASA) recommendations24 and had SPF-status. All results are reported in consistency with ARRIVE (animal research: reporting in vivo experiments) guidelines25.
The study utilized C57BL/6JNskrc mice (local C57BL/6J sub-colony). In the first colorectal cancer (CRC) experiment, two groups of male C57BL/6JNskrc mice were used. The first group (denoted as the “F1” group, n = 10) was the progeny of mice received from the Center for Genetic Resources of Laboratory Animals at the Institute of Cytology and Genetics of the Siberian Branch of the Russian Academy of Sciences (ICG SB RAS, Novosibirsk, Russia) and bred at the Scientific Research Institute of Neurosciences and Medicine (SRINM) for two to three generations, while the second group (denoted as the “F2” group, n = 7) was obtained directly from the Center for Genetic Resources of Laboratory Animals at ICG SB RAS, Novosibirsk, Russia. The animals from both facilities were placed in one room one week before the experiment. All subsequent experiments involved C57BL/6JNskrc male and female mice, all bred at the SRINM. In the second CRC experiment, two groups of male C57BL/6JNskrc mice, both bred in SRINM, but housed in separate rooms in the facility (“R1”, n = 13 and “R2”, n = 8 groups for Room 1 and Room 2) were used. These two groups were obtained as follows: a sub colony of C57BL/6JNskrc mice bred at SRINM was placed in a new room and bred independently for three to four generations. As a result, we obtained two populations of C57BL/6JNskrc mice housed separately in two different rooms of the mouse facility at SRINM. These two groups differed in microbiota composition, specifically, A. muciniphila abundance (Fig. 2A). The animals from both groups were placed in one room one week before the experiment. Animals from Room 1 were not mixed with those from Room 2 and were housed as same-sex siblings. The first CRC experiment also included a control group of the untreated C57BL/6JNskrc male mice (Control, n = 15) of the same age bred at SRINM. Control animals developed no tumors and are only shown in metabolite analysis (n = 15 for blood serum metabolites, n = 5 for intestinal metabolites) (Figure S3).
Two C57BL/6 mouse colonies, bred and housed in distinct rooms within the same facility, exhibited different abundances of A. muciniphila and demonstrated differing responses in the AOM/DSS-induced colorectal cancer model. (A) Experimental design. (B) Tumors in the colon of mice on the day 98 of the experiment. F1 and F2 – indicate two different facilities of origin. (C) Percentage of mice with detectable tumors in the colon for each group (n = 7−10). Differences were tested using the Fisher Exact test. (D) Number of tumors in mice following AOM/DSS treatment * p < 0.05 by the Wilcoxon test (W = 55.5, p = 0.0412, n = 7−10). (E) Alpha diversity of the gut microbiota, assessed by Shannon index (n = 5 per group). No significant differences were identified, as determined by the Wilcoxon test (W = 21, p = 0.095). (F) First two axes of principal coordinate analysis (PCoA) of weighted UniFrac distances (n = 5 per group). Significant differences (p-value = 0.01) between two facilities were identified by PERMANOVA with 1000 permutations. (G) Relative abundance of the gut microbial taxa in mice after AOM/DSS treatment, assessed by 16S rRNA gene sequencing (n = 5 per group). (H) LefSE analysis of OTUs with LDA score ≥ 2.0 and FDR < 0.05 identified in the microbiome of the intestinal content at the “CRC” time point (n = 5 per group). (I) The initial (before AOM injection) A. muciniphila 16S rRNA DNA level in the intestinal contents (normalized to 16S rRNA DNA). * p < 0.05 by the Wilcoxon test (W = 71, p = 0.028, n = 8−11). Value points shown in red indicate outliers. The white arrow points at the tumor. Red lettering represents Akkermansia at different taxonomic levels.
All experiments were conducted in the SRINM animal facility. Animals were housed in same-sex groups of 4–8 mice in individually ventilated cages. The light/dark photoperiod was 14 h/10 h (light off at 12:00 h), with temperatures maintained at 22–24 °C and humidity at 30–60%. Food and drinking water were provided ad libitum.
AOM/DSS colorectal cancer model
The AOM/DSS model was established according to the widely used protocol26,27 utilizing azoxymethane (AOM, A5486, Sigma-Aldrich Co., USA) and dextran sulfate sodium (DSS, MW ~ 40000, 1138, NeoFroxx, Germany). Male mice aged 8–12 weeks received a single intraperitoneal injection of AOM in a dosage of 10 mg/kg body weight. Two days after, the mice were given three rounds of DSS treatment, each lasting for 2 weeks, with 1.8% DSS dissolved in drinking water for 1 week followed by drinking water for the next week (Figs. 1A and 2B). During the experiment, body weight and other clinical signs of colitis were monitored, and the disease activity scores were recorded (listed in Table 1). Mice were euthanized by CO2 inhalation 14 weeks after the first DSS administration. Following euthanasia, the colon was dissected longitudinally, visible tumors in the colon were counted and measured in size, and the area of tissue affected by tumors was further estimated using ImageJ software. No control group was included in either of the CRC experiments; comparisons were made between two groups from different facilities/rooms within each experiment. The schematic of the experiments is summarized in Figure S1.
Two cohorts of C57BL/6 mice bred in two separate facilities differed in the gut microbiota composition and demonstrated different susceptibility to the AOM/DSS colorectal cancer model. (A) A. muciniphila 16S rRNA gene levels in feces of the mice bred in two separate rooms before the AOM/DSS treatment (normalized to 16S rRNA gene). * p < 0.05 by the Wilcoxon test (W = 81, p = 0.037, n = 8−13). Value points shown in red indicate outliers. (B) Experimental design. (C) Tumors in the colon of mice on the day 98 of the experiment. R1 and R2 indicate different mouse colonies. (D) Percentage of mice with detectable tumors in the colon for each group. Differences were tested using the Fisher Exact test (n = 8−13). (E) Number of tumors in mice following AOM/DSS treatment, ** p < 0.01 by the Wilcoxon test (W = 79.5, p = 0.0068, n = 8−13). (F) Colon tissue area (mm2) affected by tumors. ** p < 0.01 by the Wilcoxon test (W = 93, p = 0.0028, n = 8−13). (G) Alpha diversity on the day 98 of the experiment (at the “CRC” time point). No significant differences were identified by the Wilcoxon test (W = 35, p = 0.238, n = 8−13). Value points shown in red indicate outliers. (H) First two axes of principal coordinate analysis (PCoA) of weighted UniFrac distances at the “CRC” time point (n = 8−13). No difference was found with PERMANOVA with 1000 permutations. (I) Relative abundance of the top 15 taxa at the genus level in mice at the “CRC” time point, assessed by 16S rRNA amplicon sequencing (n = 8−13). (J) Body weight loss during three rounds of DSS, expressed as a percentage of the initial body weight (before AOM injection). Differences between groups on each day were tested using pairwise t-test with Benjaminni-Hochberg p-value correction (t = −2.9, df = 18.9, p = 0.017, n = 8−13). * p-value < 0.05.
Intragastric treatment with Akkermansia muciniphila
Akkermansia muciniphila (CCUG 64013T) was cultured on chocolate agar plates (938500183805215, BioMedia, Russia) in an anaerobic jar (AnaeroJar, AG0025A, Oxiod; USA) supplemented with an anaerobic generator (AnaeroGen, AN0025A, ThermoScientific, USA) and an anaerobic indicator (BR0055B, ThermoScientific, USA) for 5 days at 37 °C. The identity of the colonies was checked by PCR with the primers specific to A. muciniphila (primer sequences are presented in supplementary Table S1). Bacterial cells were washed from the agar plates with PBS in a sterile environment and diluted to 5 × 108 CFU/ml. Bacterial counts were calculated by plating serial dilutions on the agar plates. Male mice aged 8–12 weeks (n = 7) were orally administered A. muciniphila in sterile PBS (108 CFU/200 µl per mouse) three times a week for 4 weeks. Control mice (n = 7) were given an equivalent volume of sterile PBS (supplementary Figure S4). Fecal samples were collected three days after the final gavage in order to assess A. muciniphila colonization and other changes of the microbiome using 16S rRNA amplicon sequencing (described below).
Acute DSS colitis model
Acute DSS colitis was induced following a previously published protocol28. Female mice aged 8–10 weeks with different A. muciniphila levels (“Amuc high” n = 12 and “Amuc low” n = 8) were treated with 1.8% DSS (DSS, MW ~ 40000, 1138, NeoFroxx, Germany) in drinking water for 7 days, followed by drinking water for 2 days. After this, the animals were euthanized by CO2 inhalation. Control group mice (n = 8) with mixed levels of A. muciniphila received drinking water only. Similar to the AOM/DSS model, body weight and other physical signs were monitored, and disease activity scores were recorded during DSS treatment. Following euthanasia, colon length was measured.
Histology
Colon and tumor tissues fixed in 4% paraformaldehyde were embedded in paraffin, sectioned at 4 μm thickness, and stained with hematoxylin and eosin. Sections were examined in a blinded manner, and morphological features were observed. Images were captured with an AxioImager.M2 microscope using an Axiocam 305 color camera (Zeiss, Germany).
DNA extraction from feces and intestinal content
DNA was extracted using QIAamp Fast DNA Stool Mini Kit (51604, Qiagen, Germany) according to the manufacturer’s instructions. Briefly, 2–4 fecal droppings or intestinal contents (the content of the small intestine, cecum, colon, and a fecal sample) were homogenized and lysed in Inhibitex Buffer at 70 °C for 30 min, then centrifuged at 10,000 rpm for 5 min. The supernatant was transferred to a clean tube and mixed with Proteinase K and AL Buffer, then incubated at 70 °C for 10 min. Next, 96% ethanol was added, the samples were mixed, applied to spin columns, and washed with AW1 and AW2 buffers. Purified DNA was eluted, quantified using a NanoDrop 2000 spectrophotometer (ThermoScientific, USA), and stored at − 20 °C until PCR analysis or library preparation.
16S rRNA amplicon sequencing and Microbiome analysis
DNA library preparation and sequencing were performed by Novogene (https://en.novogene.com). Briefly, 16S rRNA V3-V4 regions were amplified with barcoded primers using Phusion®High-Fidelity PCR Master Mix (M0531, New England Biolabs, USA). PCR products were purified and libraries were prepared using TruSeq® DNA PCR-Free Sample Preparation Kit (20015963, Illumina, USA) according to the manufacturer’s recommendations. Libraries were pooled in equal ratios and sequenced on a paired-end Illumina platform to generate 250 bp paired-end raw reads.
Raw demultiplexed reads were processed with QIIME2 (version 2023.5.1)29. Paired-end reads were merged, filtered, and denoised with Deblur30. The obtained ASVs were clustered to OTUs with vsearch cluster-features-de-novo plugin (identity 0.99), taxonomy annotation was performed with q2-feature-classifier using classifier trained on SILVA SSU 138 database31,32. Further taxonomy visualization and diversity analysis were performed using MicrobiomeAnalyst 2.033 and R (version 4.1.2). OTUs with low abundance were filtered out, and counts were scaled with Cumulative-Sum Scaling. To identify marker features Linear discriminant analysis Effect Size (LefSE) analysis34 was performed, and features with LDA scores ≥ 2.0 and FDR < 0.05 were filtered for abundance and correlation analysis.
Microbiome real-time PCR
The level of bacteria of interest in fecal samples was evaluated by the amount of specific 16S rRNA DNA normalized to conservative 16S rRNA DNA of bacteria. PCR contained PCR Master Mix HS-qPCR SYBR Blue (MHC030, Biolabmix, Russian Federation), specific primers with a final concentration of 250 nM each (all primer sequences are presented in supplementary Table S1), and 25–100 ng of DNA extracted from feces. Real-time PCR was performed in a CFX96 real-time PCR Detection System (BioRad Laboratories, USA) according to the following protocol: 95 °C for 3 min; 40 cycles of: 95 °C for 15 s, 62 °C for 25 s, 72 °C for 25 s; melt curve 65–95 °C. Relative amount of bacterial DNA was calculated by formula: 2[Ct(concerv.16 S rRNA)−Ct(specific 16 S rRNA)].
RNA extraction and gene expression analysis
The gene expression analysis was performed as follows. Total RNA was isolated from colon tissue samples using QIAzol lysis reagent (79306, Qiagen, Germany) and genomic DNA was removed by DNaseI (04716728001, Roche, Germany) according to the recommendations of the manufacturers. RNA concentration was analyzed using a NanoDrop 2000 spectrophotometer (ThermoScientific, USA). Reverse transcription was performed using 7–10 µg of purified RNA, a mix of random hexa-deoxyribonucleotide and Oligo-dT primers, and M-MuLV reverse transcriptase (E318, SibEnzyme, Russian Federation) according to the manufacturer’s recommendations. The cDNA obtained was five times diluted with ultrapure water and used for real-time PCR. Real-time PCR was performed using PCR Master Mix HS-qPCR SYBR Blue (MHC030, Biolabmix, Russian Federation), 5 µL of cDNA, and 250 nM specific primers (listed in supplementary Table S2). The reaction was performed in a CFX96 real-time PCR Detection System (BioRad Laboratories, USA) according to the following protocol: 95 °C for 3 min; 40 cycles of: 95 °C for 15 s, 62 °C for 25 s, 72 °C for 25 s; melt curve 65–95 °C. Expression of the target gene was normalized to Tubb5 level using the formula: 2[Ct(Tubb5 mRNA)−Ct(gene of interest mRNA)].
NMR spectroscopy
The metabolomic profile of the sample was analyzed at the Center for Collective Use “Mass Spectrometric Investigations,” SB RAS (Novosibirsk, Russia), utilizing high-resolution 1H NMR spectroscopy. Metabolite extraction from serum was conducted using a sample preparation protocol previously validated for quantitative NMR-based metabolomics35. Briefly, 100 µL of ice-cold methanol and 100 µL of ice-cold chloroform were added to 100 µL of serum, followed by vortexing for 30 s, incubation on ice for 10 min, and further incubation at − 20 °C for 30 min. The resulting mixtures were centrifuged at 12,000 rpm and 4 °C for 30 min to precipitate proteins. The upper hydrophilic fraction was then transferred to fresh vials and lyophilized using a vacuum concentrator.
Protein-free metabolite extracts from mouse distal intestine were obtained as described previously35. Briefly, intestinal fragments were harvested, frozen in liquid nitrogen, and stored in 1.5 mL Eppendorf tubes at − 70 °C. The frozen tissue was weighed and homogenized with a glass homogenizer in a cold (− 20 °C) mixture of water/methanol/chloroform in a 1:2:2 (v/v) ratio, using 1600 µL of solvent mixture per 150 mg of wet tissue. The mixture was vortexed for 30 s, kept on ice for 10 min, and incubated at − 20 °C for 20 min. Centrifugation at 12,000 rpm and 4 °C for 30 min facilitated protein precipitation. The upper hydrophilic fraction was then collected into fresh vials and lyophilized.
Dried extracts were reconstituted in 600 µL of D2O containing 6 × 10− 6 M sodium 3-(trimethylsilyl)propane-1-sulfonate as an internal standard, along with a 20 mM deuterated phosphate buffer to maintain a pH of 7.4. 1H NMR measurements were performed using the AVANCE III HD 700 MHz NMR spectrometer equipped with a 16.44 T Ascend cryomagnet.
Proton NMR spectra for each sample were acquired with 128 accumulations, maintaining a sample temperature of 25 °C during data acquisition. The detection pulse utilized a 90-degree angle, and a repetition time of 25 s was implemented to allow complete relaxation of all spins. Low-power radiation at the water resonance frequency was applied prior to acquisition to presaturate the water signal, employing the zgpr pulse sequence.
NMR spectra were manually phased and baseline-corrected. Signal processing and integration were conducted using MestReNova V.12 software. Sodium 3-(trimethylsilyl)propane-1-sulfonate was used as a reference at a concentration of 6 µM. Metabolite resonance assignments were in accordance with the Human Metabolome Database. Raw blood and intestine NMR metabolomic data are shared in a public repository36 with IDs 292 and 293.
Statistical data analysis
All statistical tests were performed with R (version 4.1.2) using various packages and visualized using ggplot2. Normal distribution of the data was assessed using the Shapiro-Wilk test. Fisher’s Exact Test was used to analyze categorical variables. ANOVA (Analysis of Variance) was applied to analyze the effect of multiple factors for normally distributed data. The Wilcoxon Test was applied to assess differences in microbiota relative abundances and other data that do not follow a normal distribution. PERMANOVA (Permutational Multivariate Analysis of Variance) was used to assess differences in beta diversity among groups based on weighted UniFrac distances. Spearman correlation was used to analyze the association between two ranked variables, such as taxa abundances and tumor counts. The Benjamini-Hochberg correction was applied for multiple comparisons (p < 0.05 were considered statistically significant differences, unless otherwise specified). Paired and unpaired versions of statistical tests were applied to dependent and independent data, respectively, where applicable.
Results
Mice bred in two facilities showed different susceptibility to AOM/DSS treatment
We established the AOM/DSS colorectal cancer model using C57BL/6 male mice (n = 17) that originated from two different facilities. The cohorts included mice bred in-house (“F1”, n = 10) and those obtained from an external facility (“F2”, n = 7). Two days after AOM injection (10 mg/kg of body weight), mice received three rounds of 1.8% DSS in drinking water (the experimental design is shown in Fig. 1A). Ninety-eight days after the first DSS administration, the mice were sacrificed and examined for tumors in the colon. Representative photographs are shown in Fig. 1B, and representative microphotographs demonstrating distal colon histology are shown in supplementary Figure S2. The results indicated that the mice developed tumors in the distal colon in a manner dependent on their facility of origin, 8 of 10 “F1” mice had visible tumors in the colon, whereas only 2 of 7 “F2” mice developed 1 or 2 tumors (Fig. 1C,D; difference between groups was tested with the Fisher exact test, p = 0.058, and Wilcoxon test, p = 0.041, respectively).
According to several findings, differences in susceptibility to AOM/DSS treatment in mice of the same strain may result from differences in gut microbiota composition18,21,22,23. Since the mice in the current experiment were obtained from different facilities, we hypothesized that the observed differences in AOM/DSS susceptibility might be due to some microbiota features. We analyzed the microbiota of the mice at the end of the experiment using 16S rRNA gene sequencing of DNA extracted from the intestinal contents. For this analysis, 5 samples per group were selected: mice with 2–8 tumors from the “F1” and mice with no tumors from the “F2” group, in order to analyze the most pronounced differences between the groups. No differences were found in alpha diversity (Fig. 1E), but significant differences were observed in beta diversity, as tested with weighted UniFrac (Fig. 1F). This indicates differences in microbiome composition between the “F1” and “F2” groups after AOM/DSS treatment (p < 0.01, tested with PERMANOVA).
The microbiotas of the two groups differed in the abundance of several bacterial taxa (Akkermansia genus, Lachnospiraceae family, Prevotalleceae genus, Fig. 1G). To identify specific features associated with the “F1” and “F2” microbiomes, we applied LefSE analysis. Features annotated to Akkermansia muciniphila and its higher taxonomy proved to be strongly associated with the “F2” group resistant to AOM/DSS treatment (Fig. 1H). As the AOM/DSS model is driven by inflammation26,27, our findings align with the reported anti-inflammatory role of this bacterium in DSS-induced colitis37,38. We further analyzed the metabolomic profiles of the intestinal samples collected from both experimental groups using NMR spectrometry. For this analysis, serum and fragments of distal intestine were used. We found no difference between the test groups in several dozen of small metabolites in both serum and intestinal tissue (supplementary Figure S3A, B, E, F). There were significant changes in some serum metabolites in both groups as compared to the control samples from the untreated animals (supplementary Figure S3C, D), while no differences were found in intestinal tissue metabolites (supplementary Figure S3G, H). These changes were similar across both test groups, so we attribute them to tumorigenesis itself rather than any differences in the microbiota.
We propose that the observed difference in A. muciniphila abundance between the test groups at the point of cancer development originates from the initial differences in its levels. To test this hypothesis, we employed qPCR with species-specific primers to analyze A. muciniphila in fecal samples collected prior to AOM injection. Surprisingly, the abundance of this bacterium in the initial microbiotas was inversely related to that at the “CRC” time point; specifically, A. muciniphila was found to be more abundant in the AOM/DSS susceptible “F1” group (Fig. 1I). This suggests that certain bacterial species may undergo dynamic changes during cancer progression. Despite this, A. muciniphila remained our primary candidate bacterium associated with CRC development, supported by its highest LDA score (Fig. 1H) and existing literature linking it to cancer.
Healthy-state baseline Akkermansia muciniphila defines susceptibility to CRC
To determine whether higher abundance of A. muciniphila before the treatment affects the AOM/DSS model outcomes, we attempted to increase the colonization of this bacterium in mice bred in our facility. The animals were gavaged with A. muciniphila (CCUG64013T) three times a week for 4 weeks. The experimental design is shown in supplementary Figure S4A. To identify changes in microbiota composition, we analyzed DNA from feces collected 3 days after the last gavage using 16S rRNA sequencing. Contrary to expectations, gavage with A. muciniphila did not increase the abundance of the bacterium (supplementary Figure S4D) and did not alter the overall diversity and composition of the gut microbiota (supplementary Figure S4B, C, D).
Since the straightforward approach to increase A. muciniphila failed, we tested C57BL/6Nskrc mice housed in separate rooms within our facility to identify the animal groups with the natural differences in A. muciniphila abundance. We identified a pair of rooms (“R1” and “R2”) that significantly differed in A. muciniphila abundance, as determined by qPCR with specific primers (p < 0.05, the Wilcoxon test, Fig. 2A). To verify our hypothesis, we treated these two groups with AOM and DSS as in the first experiment (experimental design is shown in Fig. 2B). Consistent with the previous results, mice with higher A. muciniphila abundance (from Room-1, group “R1”) developed significantly more tumors in the colon than those from Room-2 (group “R2”), representative photographs are shown in Fig. 2C. The difference between the groups for the presence of tumors (yes/no) was tested with the Fisher exact test, p = 0.056 (Fig. 2D). We found 2–6 visible tumors in 11 of 13 “R1” mice, whereas there were only 1–2 tumors in 3 of 8 “R2” mice (p < 0.01, the Wilcoxon test, Fig. 2E). The affected tissue area was also greater in “R1” mice (p < 0.01, the Wilcoxon test, Fig. 2F). No cage effect was found for the number of tumors and the affected area of the intestine (Figure S5). DNA samples were extracted from intestinal contents at the “CRC” point (referring to the endpoint of the experiment) and analyzed for microbiome diversity. No significant differences in alpha and beta diversity were observed between the two rooms at the “CRC” point (Fig. 2G, H, I), microbiota diversity and composition were indistinguishable between the two cohorts. A two-way ANOVA revealed a significant interaction between Group and Day factors on the body weight dynamics (F(63, 1197) = 2.06, p < 0.001). Nevertheless, there were no differences in the body weight loss during the experiment, except for day 9, when “R1” mice lost significantly more weight than “R2” mice (Fig. 2J).
Thus, the results obtained support the hypothesis regarding the association between the baseline healthy-state levels of A. muciniphila and outcomes of the AOM/DSS model. Our findings align with those of Baxter et al., which demonstrated that the initial abundance of A. muciniphila was associated with tumor burden in the AOM/DSS mouse model23. Next, we analyzed dynamic changes in the gut microbiota during the development of the AOM/DSS model and attempted to reveal other bacterial features that might be involved in CRC outcomes.
Chronic colitis mitigates baseline microbiota diversity between two mouse colonies
The dynamic changes in the intestinal microbiota were analyzed using 16S rRNA sequencing of DNA extracted from feces collected at different time points during the experiment. The “Before” time point refers to the period before AOM injection, “cDSS” to the time after the third round of DSS treatment. DNA samples were extracted from feces at the “Before” and “cDSS” time points. The most significant differences in both alpha and beta diversity between the two colonies occurred at the initial “Before” time point. At this stage, the “R2” microbiome was characterized by higher Shannon diversity compared to the “R1” (p < 0.001, the Wilcoxon test, Fig. 3A). However, three rounds of DSS treatment decreased alpha diversity in the “R2” group (p < 0.01, the Wilcoxon test, Fig. 3A). Chronic inflammation induced by DSS following AOM injection caused beta diversity shifts in both colonies. In a two-way PERMANOVA analysis, the interaction between the Experimental point and Room factors was found to be marginally significant (F = 60.81, p = 0.058). Significant differences were observed between the “Before” and “cDSS” points within each group, as identified by weighted UniFrac (p < 0.01 and p < 0.05, pairwise comparisons were made using PERMANOVA, Fig. 3B). Moreover, DSS treatment mitigated the differences in diversity observed at the “Before” point. These findings suggest that the most crucial differences occur prior to and during the pathological process.
Dynamic changes of the microbiome composition during AOM/DSS-induced tumorigenesis in two mouse colonies. (A) Alpha diversity before AOM injection and after AOM injection followed by three rounds of DSS treatment. ** - p < 0.01; *** p < 0.001, the Wilcoxon test (R1 vs. R2 Before: W = 5, p = 0.00075, n = 8−13, R2 Before vs. cDSS: W = 59, p = 0.009, n = 8−13). (B) First two axes of principal coordinate analysis (PCoA) of weighted UniFrac distances before AOM injection and after three rounds of DSS (n = 8−13). * - p < 0.05; ** p < 0.01, pairwise comparisons were performed using PERMANOVA with 1000 permutations. (C) Relative abundance of the top 15 bacterial taxa at the genus level in mice before AOM injection and after three rounds of DSS treatment, assessed by 16S rRNA amplicon sequencing (n = 8−13).
Baseline healthy-state and chronic colitis-associated microbiota are characterized by different bacterial features that correlate with tumor burden
Since microbiome taxonomy profiles differed before AOM injection and after three rounds of DSS treatment (Fig. 3C), we performed LefSE analysis to identify “marker” features in the microbiota associated with high and low susceptibility to AOM/DSS-induced tumorigenesis. Features with an LDA score ≥ 2 and FDR < 0.05 were selected for subsequent analysis. The features of the initial microbiotas (“Before”) identified as colony-specific markers included Akkermansia muciniphila, Bacteroides acidifaciens and OTUs annotated to the genera Muribaculaceae, Prevotellaceae and Lachnospiraceae (Fig. 4A). Akkermansia muciniphila, Bacteroides acidifaciens, and two OTUs from Muribaculaceae were prevalent in Room-1, whereas Lachnospiraceae and other OTUs from Muribaculaceae were commonly found in Room-2 (Fig. 4A,C). In the context of DSS-induced chronic inflammation (“cDSS”), Desulfovibrio fairfieldensis and OTUs annotated to Muribaculaceae, Lachnospiraceae and Bacteroides were identified as marker microbiome features (Fig. 4B). Desulfovibrio fairfieldensis and Muribaculaceae were more abundant in Room-1, while Lachnospiraceae, and Bacteroides were more prevalent in Room-2 (Fig. 4B,D).
Identification of “marker” features specific to the microbiotas of the two mouse colonies before AOM injection (the “Before” time point) and after three rounds of DSS treatment (the “cDSS” time point). (A,B) LefSE analysis of the marker features at the “Before” and “cDSS” time points (n = 8−13), LDA score ≥ 2 and adjusted p-value < 0.05. Features are named by their taxonomy with unique feature identifiers. (C,D) Heatmap showing the abundance of marker features at the “Before” and “cDSS” time points (n = 8−13). Samples are clustered by Bray-Curtis distances. (E,F) Correlation heatmap representing the Spearman correlation (ρ > |0.5|) between the abundance of the identified markers at the “Before” and “cDSS” time points with the number of tumors observed at the “CRC” time point. Correlations that are not significant are crossed out. *, **, *** Benjaminni-Hochberg adjusted ρ-value < 0.05, 0.01 and 0.001.
To find associations between microbiome features and tumor burden, we analyzed correlations between normalized OTUs counts and tumor counts. Features exhibiting significant moderate and strong correlations (ρ > |0.5|, the Spearman test) were selected for subsequent analysis. Interestingly, features from both “Before” and “cDSS” time points correlated with tumor burden. In line with our previous findings, A. muciniphila showed a moderate positive correlation with tumor number, and B. acidifaciens strongly correlated with tumor counts (ρ = 0.53, p < 0.01 and ρ = 0.76, p < 0.001 respectively, the Spearman test, Fig. 4E). In the “cDSS” microbiome, D. fairfieldensis positively correlated with tumor counts, while Lachnospiraceae and Bacteroides demonstrated negative correlations (ρ = − 0.60, ρ =̶ 0.63, ρ =̶ − 0.57 respectively, p < 0.01, the Spearman test, Fig. 4F). Thus, among more than 600 features, we identified 5 microbiome markers associated with tumor burden.
Bacterial markers before colitis correlate with chronic inflammation-associated species and tumor burden
Since the microbiome alterations occur throughout the course of CRC development, it is important to trace the changes associated with different stages of the process. Therefore, we analyzed the dynamic changes of the identified markers at two points of the experiment, as well as the correlation between key bacterial features. We applied Spearman correlation analysis to the normalized OTU counts of the selected features at the “Before” and “cDSS” points. In the initial microbiota, a correlation was found only between abundances of A. muciniphila and B. acidifaciens (ρ = 0.79, p < 0.001, Fig. 5A). Interestingly, the initial abundances of features at the “Before” time point significantly correlated with those specific to the “cDSS” chronic inflammation point. The correlations were positive for D. fairfieldensis (ρ = 0.6, p < 0.05, Fig. 5A) and negative for the Lachnospiraceae NK4A136 group (ρ = − 0.68 and ρ =̶ − 0.75, p < 0.01, Fig. 5A). Remarkably, no correlations were found in the abundances of the same feature at the “Before” and “cDSS” time points, confirming profound microbiota alterations during the establishment of chronic inflammation.
Correlation between the identified “marker” features in the microbiotas of two mouse colonies at two experimental time points: before AOM injection (the “Before” time point) and after three rounds of DSS (the “cDSS” time point). (A) Correlation heatmap representing the Spearman correlation (ρ > 0.5) between the abundances of the identified markers at the “Before” and “cDSS” time points. Correlations that are not significant are crossed out. Correlations with Benjaminni-Hochberg adjusted p-value < 0.05 are marked significant. (B–E) Abundances of selected marker features at the “Before” and “cDSS” time points (n = 8−13). * p < 0.05, ** - p < 0.01, *** p < 0.001 by the Wilcoxon test with Benjaminni-Hochberg correction (f14f4_Akkermansia_muciniphila: Before_R1 vs. Before_R2 W = 95, p = 0.002; Before_R2 vs. cDSS_R2 W = 2, p = 0.002; 80130_Bacteroides_acidifaciens: Before_R1 vs. Before_R2 W = 96, p = 0.003; c5aa3_Desulfovibrio_fairfieldensis: Before_R1 vs. cDSS_R1 W = 4, p = 0.00016; Before_R2 vs. cDSS_R2 W = 8, p = 0.014; cDSS_R1 vs. cDSS_R2 W = 100, p = 0.00023; Lachnospiraceae_NK4A136_group: cDSS_R1 vs. cDSS_R2 W = 2, p = 0.001). Value points shown in red indicate outliers. (F–H) The Spearman correlation between selected features and tumor burden in mice with developed tumors. Correlations and Benjaminni-Hochberg adjusted p-value are presented in pictures.
In terms of changes in abundance, the baseline normalized counts of A. muciniphila and B. acidifaciens were significantly lower in Room-2 compared to Room-1 (p < 0.01, the Wilcoxon test, Fig. 5B,C). However, upon chronic inflammation, the abundance of A. muciniphila in the “R2” group increased (p < 0.01, the Wilcoxon test, Fig. 5B). As a result, the differences between the groups diminished at the “cDSS” time point (Fig. 5B,C). The abundance of D. fairfieldensis did not differ between Room-1 and Room-2 before AOM injection. However, it increased in both groups upon chronic inflammation (p < 0.001 for “R1” and p < 0.05 for “R2”, the Wilcoxon test, Fig. 5D). Additionally, the increase observed in Room-1 was significantly greater than that in Room-2 (p < 0.001, the Wilcoxon test, Fig. 5D). Lachnospiraceae NK4A136 count differed between the two rooms only at the “cDSS” point (p < 0.01, the Wilcoxon test, Fig. 5E). These results suggest that the initial composition of the microbiota may influence its alterations during intestinal inflammation through complex interactions within the microbial community. Next, we validated the results obtained with NGS by qPCR using primers specific to A. muciniphila, B. acidifaciens, and D. fairfieldensis (primer sequences are listed in Table S1). Since Lachnospiraceae NK4A136 and unidentified Bacteroides were annotated only at the genus level, it was not possible to design species-specific primers to quantify these features by qPCR. Therefore, we further analyzed only three species mentioned above. As shown by qPCR, the normalized OTU counts obtained in NGS analysis highly correlated with the qPCR measurements of the species abundances (supplementary Figure S6A, B, C), so we used these primers for subsequent analysis.
Thereby, we selected three significant bacterial features from both the “Before” and “cDSS” points that strongly correlate with tumor burden (Fig. 5F,G,H). The positive correlation of the baseline healthy-state A. muciniphila and B. acidifaciens with tumor counts is consistent with findings of Baxter et al., which demonstrated an association between AOM/DSS-induced tumor incidence and the abundance of A. muciniphila and Bacteroides spp23. Moreover, Wang et al. reported that gavage with A. muciniphila exacerbated tumorigenesis in the AOM/DSS model, probably through modulation of cell proliferation39. As for the association between D. fairfieldensis and tumors, the role of sulfate-reducing bacteria (SRB) Desulfovibrio spp. in both intestinal inflammation and colorectal cancer has been suggested in a number of studies40. The most thought-provoking observation is the correlation between the baseline abundance of A. muciniphila and B. acidifaciens and the subsequent increase of D. fairfieldensis in the context of chronic inflammation.
The initial abundance of Akkermansia muciniphila positively correlates with the expression of inflammatory cytokines in acute colitis
To further explore the role of the identified markers in inflammation that may contribute to AOM/DSS-induced tumorigenesis, we examined changes in the gut microbiome and gene expression in colon tissue during the early stage of DSS-induced colitis. In the previous experiment, the only significant difference in body weight loss was observed on the 9th day, two days after the first DSS round (Fig. 2G). Therefore, we analyzed mice with distinct initial levels of A. muciniphila (“Amuc high” and “Amuc low”, p < 0.001, the Wilcoxon test, Fig. 6E) that were treated with DSS in drinking water for 7 days, followed by 2 days of regular drinking water (experimental design is shown in Fig. 6A). In this experiment, most animals demonstrated rectal bleeding and diarrhea, but clinical scores did not differ between the groups (Fig. 6B). As expected, DSS treatment resulted in colon shortening (Fig. 6C). Moreover, there was a significant effect of DSS treatment on body weight loss in both groups (p < 0.001 by repeated measures ANOVA), but there were no differences attributed to A. muciniphila abundance (Fig. 6D).
The role of A. muciniphila and other marker features in DSS-induced acute colitis. (A) Experimental design. (B) Disease activity score (DAI) on day 9 of the experiment (n = 7−11). No significant difference was identified with the Wilcoxon test (W = 26, p = 0.16). (C) Colon length on the day 9 of the experiment (n = 8−12). *** – p < 0.001, the Wilcoxon test (Cont vs. Amuc_high_aDSS W = 86.5, p = 0.0031; Cont vs. Amuc_low_aDSS W = 59, p = 0.005). (D) Body weight loss during DSS treatment, expressed as a percentage of initial body weight (n = 8−12). (E–G) 16S rRNA DNA levels of marker features in feces of the mice before and after DSS treatment (n = 8−12). **, *** p < 0.01 and p < 0.001, the Wilcoxon test with Benjaminni-Hochberg correction (A. muciniphila: Before_Amuc_high vs. Before_Amuc_low W = 96, p = 0.00006, Before_Amuc_high vs. aDSS_Amuc_high W = 11, p = 0.0002, Before_Amuc_low vs. aDSS_Amuc_low W = 0, p = 0.0002; B. acidifaciens: Before_Amuc_high vs. aDSS_Amuc_high W = 118, p = 0.007). Value points shown in red indicate outliers. (H–K) Relative mRNA levels of Tnfa, Ifng, Il1b, Nos2 (normalized to Tubb5) in colon tissue. * p < 0.05, ** – p < 0.01, the Wilcoxon test with Benjaminni-Hochberg correction (Tnfa: Cont vs. DSS_Amuc_high W = 14, p = 0.022; Nos2 Cont vs. DSS_Amuc_high W = 9, p = 0.005). Value points shown in red indicate outliers. (L) The Spearman correlation between the abundance of fecal DNA of the identified markers at the “Before” (A. muciniphila and B. acidifaciens) and “aDSS” (D. fairfieldensis) time points and expression of Tnfa, Ifng, Nos2 in colon tissue. Correlations and Benjaminni-Hochberg adjusted p-value are highlighted in red.
Analysis of the gut microbiota using qPCR with specific primers revealed an increase of A. muciniphila in both groups (p < 0.001, the Wilcoxon test, Fig. 6E). This result is in line with our earlier observation at the “cDSS” time point (Fig. 5B). Despite the dynamic changes observed in the previous experiment (Fig. 5C, D), the abundance of two other markers, B. acidifaciens and D. fairfieldensis, did not increase (Fig. 6F, G). Interestingly, gene expression analysis through mRNA assessment in colon tissue showed a significant increase in the expression of Tnfa and Nos2 in mice with a “high” level of initial A. muciniphila, whereas no such increase was observed in the low A. muciniphila group (p < 0.05 by the Wilcoxon test, compared to the control group with no treatment, Fig. 6H,K). In contrast, there was no significant effect on Il1b expression (Fig. 6J). There was also a trend towards increased Ifng expression in the “Amuc high” group, although these changes were not significant (Fig. 6I). Remarkably, we revealed positive correlations between the initial abundance of A. muciniphila and B. acidifaciens and the expression levels of Ifng and Nos2 genes (ρ > 0.5, p < 0.05, the Spearman correlation, Fig. 6L). Thus, these results suggest that high initial colonization by A. muciniphila may be associated with more intense DSS-induced inflammation, which could result in increased susceptibility to AOM/DSS treatment.
Discussion
In the current study, we took advantage of two C57BL/6 mouse colonies harboring distinct gut microbiota and demonstrated that mice with a higher baseline abundance of A. muciniphila and B. acidifaciens were more susceptible to inflammation-induced tumorigenesis in the AOM/DSS model. Moreover, the initial abundances of these candidate bacteria were positively correlated with the increase of sulfate-reducing bacteria (SRB) D. fairfieldensis during the establishment of chronic intestinal inflammation. All these bacteria showed a significant positive correlation with the number of tumors, implying a complex dynamic interplay between the microbial species that results in susceptibility to tumorigenesis. Although A. muciniphila and B. acidifaciens are known as beneficial commensals, our results suggest that under certain conditions, they can be associated with the severity of CRC. Apparently, the dual role of A. muciniphila and B. acidifaciens depends on the structure of the intestinal microbial community. Specifically, our data suggest that these bacteria are associated with an increase of D. fairfieldensis in the context of inflammation, which could contribute to tumorigenesis. It should be noted that our results are limited to the analysis of fecal microbiota, as the study was designed to correlate the baseline healthy state and inflammation-associated microbiota with the number of tumors. Characterization of the mucosal microbiome might reveal additional candidates associated with tumor burden.
The gut microbiota is a complex, dynamic ecosystem that is regulated by the host through various factors, including the repertoire of mucin glycans, diet, and the mucosal immune system41. At the same time, it is, to some extent, a self-regulating community. Microbiota composition is shaped by different microbe-microbe interactions, including competition for energy sources and cross-feeding, when metabolites of one bacterium are consumed by others42. A number of studies comparing the gut microbiota of patients with healthy controls revealed dysbiosis in CRC10,11,13,14,15. Although certain bacterial species have been identified as being associated with CRC (Bacteroides fragilis, Fusobacterium spp., Enterococcaceae spp., etc.), there is no consistency across different reports, suggesting a large variation in the microbiota between individuals. Apart from this, one possible explanation of the inconsistency is that microbiota composition is profoundly altered during tumorigenesis. This may also pose an obstacle to the identification of specific bacteria involved in CRC pathogenesis. For instance, according to the “bacterial driver-passenger” CRC model, bacteria that “drive” the pathology are subsequently replaced by more adapted “passengers”, which benefit from an inflammatory and tumorigenic microenvironment17,43. Our research supports the idea of such dynamic changes, as the most profound differences between microbiotas of two mouse colonies with distinct susceptibility to tumorigenesis were observed in the baseline healthy state and during chronic inflammation, while microbiotas at the final “CRC” point were nB. acidifaciensot significantly different.
Interestingly, in our study, the tumor burden was associated with the baseline abundance of common symbionts A. muciniphila and , which are known as anti-inflammatory bacteria. This association has been demonstrated in a number of studies utilizing the DSS-induced colitis model37,38,44,45. Moreover, certain experiments indicate the alleviating effect of A. muciniphila and its membrane protein on inflammation-associated tumorigenesis in mice46,47. It should be noted that in all these studies, mice were treated with the bacteria or their membrane proteins and by-products during the experiment, which means that the baseline microbial community was not taken into account. Furthermore, there is a report that contradicts the anti-inflammatory and anti-tumor properties of A. muciniphila, where this bacterium was shown to exacerbate inflammation and tumorigenesis in a mouse model used in the study39. Altogether, this highlights the importance of considering the initial microbiota as well as its alterations during the establishment of the pathology. In consistency with our results, Baxter et al. demonstrated that the initial microbiota, notably A. muciniphila and Bacteroides spp., were positively correlated with the number of tumors in the AOM/DSS model. Since the research utilized germ-free mice colonized with fecal microbiota from CRC patients and healthy controls, the results reflect the effects of the established baseline microbial community in tumorigenesis23.
One of the possible explanations of these correlations is that both A. muciniphila and B. acidifaciens are mucin-degrading bacteria48,49,50. Their high abundances in the context of colitis could exacerbate inflammation via degradation of the mucosal barrier. It is worth noting that, in our study, although A. muciniphila abundance increased after three rounds of DSS, its level at the point of chronic inflammation did not correlate with the tumor burden. This further highlights the importance of baseline bacterial levels. Moreover, our analysis of gene expression in colon tissue in acute colitis revealed a moderate positive correlation between baseline abundances of both A. muciniphila and B. acidifaciens and the expression of Ifng, Nos2, suggesting an association between the initial microbiota and the inflammatory response.
The mechanistic basis of immune modulation by A. muciniphila and B. acidifaciens in the context of colorectal cancer necessitates further investigation. High-quality studies have demonstrated the effects of A. muciniphila and its fractions on various immune cell types. For instance, Bae et al. (2022) provided compelling evidence that A. muciniphila, particularly its phospholipid cell membrane component, activates a TLR2-TLR1 heterodimer in murine bone marrow-derived dendritic cells, thereby triggering a pro-inflammatory response51. Another study examined the effects of both live and pasteurized A. muciniphila on murine macrophages and human monocytes, revealing complex immunological impacts. Specifically, A. muciniphila induced a robust pro-inflammatory immune response upon acute treatment while shifting to an anti-inflammatory reaction in A. muciniphila-trained (pre-exposed) cells52.
Several studies have investigated the effects of A. muciniphila in vivo, particularly in inflammation and cancer models. It is widely accepted that colonization by A. muciniphila (given its high colonization rate) leads to partial alleviation of colitis in mouse models of inflammatory bowel disease53,54. However, the impact of A. muciniphila on inflammation can vary depending on the context, as evidenced by Ganesh et al., who reported opposing effects using a model of experimental infection with Salmonella typhimurium55. Additionally, the effects of A. muciniphila are influenced by the specific strain utilized56. While the mechanisms of action of (A) muciniphila concerning immune modulation have been extensively studied, they have yielded contradictory results. Similar opposing findings have been observed with B. acidifaciens, although in vitro data regarding this bacterium is markedly poorer than that concerning Akkermansia57,58,59. For these reasons, it is possible that either of the bacterial species could serve as a pro-inflammatory stimulus. At the same time, both A. muciniphila and B. acidifaciens could just associate with other unknown factors that drive inflammation and CRC in our model.
Baseline abundances of A. muciniphila and B. acidifaciens correlated with the increase of D. fairfieldensis during chronic colitis. D. fairfieldensis, an SRB species linked to IBD and CRC40,60, produces hydrogen sulfide (H2S), which plays a complex role in colonocyte physiology61. While increased H2S-producing bacteria are observed in adenoma and CRC patients62,63,64,65, H2S also promotes CRC pathogenesis by stimulating mitochondrial function and glycolysis, enhancing tumor cell proliferation, migration, and invasion66. Exogenous H2S has been shown to stimulate colon cancer cell proliferation67 and enhance mitochondrial function68. Therefore, a rise in D. fairfieldensis may elevate H2S levels in the colon, fostering inflammation and tumorigenesis. Additionally, outer membrane vesicles from D. fairfieldensis can damage the epithelial barrier and activate macrophages, promoting intestinal inflammation69. From a mechanistic point of view, the observed increase of SRB D. fairfieldensis in association with the healthy-state baseline abundance of A. muciniphila and B. acidifaciens is of great interest. Both our healthy-state candidate bacteria are known as acetate and propionate (short-chain fatty acids, SCFAs) producers70,71,72, which could potentially provide H2 in the intestinal lumen.
However, in this report we do not directly test the causative relationship between A. muciniphila and B. acidifaciens and D. fairfieldensis experimentally. Thus, the cross-feeding theory is just one of the possible explanations of the observed association between A. muciniphila, B. acidifaciens, D. fairfieldensis, and tumor count, which needs to be studied further. Alternatively, either or both of our potential driver bacteria could contribute to inflammation and tumor growth, while D. fairfieldensis simply associates with the severity of the disease state.
A considerable limitation of this study is that it only includes male mice, but not females. It has been shown that female mice exhibit different incidence and slower development of tumors in CRC models in mice, a phenomenon that has been linked to estradiol production in females73,74. This sex difference complicates the use of mixed-sex animal groups. At the same time, estradiol production in female mice may affect the role of microbiota in CRC progression. Consequently, the findings of this study should be interpreted with caution, taking this limitation into account.
In conclusion, our data suggest a complex, context-dependent role of the commensal microbiota in inflammation-associated dysbiosis and CRC. The key microbial features include A. muciniphila recognized as a promising probiotic75,76, as well as the commensal B. acidifaciens, both of which correlate with the increase of SRB D. fairfieldensis in chronic colitis and tumor burden in CRC. In contrast to multiple studies demonstrating the anti-inflammatory properties of these two bacteria, our results point out potential adverse effects under specific conditions of genotoxicity and inflammation in the intestine. The relationship between these bacteria is particularly intriguing, given the cross-feeding metabolic interactions among commensals, which are often overlooked in the design of probiotics. Thus, our research emphasizes the need for deeper investigation into the complex interactions among commensal microbiota and the crosstalk between the microbiota and the host throughout disease development.
Data availability
The 16S rRNA gene sequencing datasets presented in this study can be found in the online repository https://www.ncbi. nlm.nih.gov/ under the following accession numbers: PRJNA1187488 and PRJNA1187527. The NMR spectrometry datasets presented in this study can be found in the online repository Animal metabolite database (AMDB) by following links: https://amdb.online/amdb/experiments/292/ and https://amdb.online/amdb/experiments/293/.
References
Bray, F. et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 74, 229–263 (2024).
Keum, N. & Giovannucci, E. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat. Rev. Gastroenterol. Hepatol. 16, 713–732 (2019).
Meira, L. B. et al. DNA damage induced by chronic inflammation contributes to colon carcinogenesis in mice. J. Clin. Invest. 118, 2516–2525 (2008).
Mangerich, A. et al. Infection-induced colitis in mice causes dynamic and tissue-specific changes in stress response and DNA damage leading to colon cancer. Proc. Natl. Acad. Sci. 109, E1820–E1829 (2012).
Dzutsev, A., Goldszmid, R. S., Viaud, S., Zitvogel, L. & Trinchieri, G. The role of the microbiota in inflammation, carcinogenesis, and cancer therapy. Eur. J. Immunol. 45, 17–31 (2015).
Sánchez-Alcoholado, L. et al. The role of the gut Microbiome in colorectal cancer development and therapy response. Cancers (Basel) 12, 1406 (2020).
Artemev, A., Naik, S., Pougno, A., Honnavar, P. & Shanbhag, N. M. The association of Microbiome dysbiosis with colorectal cancer. Cureus 14, e22156 (2022).
Wong, S. H. & Yu, J. Gut microbiota in colorectal cancer: Mechanisms of action and clinical applications. Nat. Rev. Gastroenterol. Hepatol. 16, 690–704 (2019).
Chen, W., Liu, F., Ling, Z., Tong, X. & Xiang, C. Human intestinal lumen and mucosa-associated microbiota in patients with colorectal cancer. PLoS ONE 7, e39743 (2012).
Wang, T. et al. Structural segregation of gut microbiota between colorectal cancer patients and healthy volunteers. ISME J. 6, 320–329 (2012).
Ahn, J. et al. Human gut Microbiome and risk for colorectal cancer. JNCI J. Natl. Cancer Inst. 105, 1907 (2013).
Mira-Pascual, L. et al. Microbial mucosal colonic shifts associated with the development of colorectal cancer reveal the presence of different bacterial and archaeal biomarkers. J. Gastroenterol. 50, 167–179 (2015).
Kostic, A. D. et al. Genomic analysis identifies association of Fusobacterium with colorectal carcinoma. Genome Res. 22, 292 (2012).
Wu, N. et al. Dysbiosis signature of fecal microbiota in colorectal cancer patients. Microb. Ecol. 66, 462–470 (2013).
Saffarian, A. et al. Crypt- and mucosa-associated core microbiotas in humans and their alteration in colon cancer patients. MBio 10, e01315-19 (2019).
Nakatsu, G. et al. Gut mucosal Microbiome across stages of colorectal carcinogenesis. Nat. Commun. 6, 8727 (2015).
Tjalsma, H., Boleij, A., Marchesi, J. R. & Dutilh, B. E. A bacterial driver-passenger model for colorectal cancer: beyond the usual suspects. Nat. Rev. Microbiol. 10, 575–582 (2012).
Yu, A. I. et al. Gut microbiota modulate CD8 T cell responses to influence colitis-associated tumorigenesis article gut microbiota modulate cd8 t cell responses to influence colitis-associated tumorigenesis. Cell Rep. 31, 107471 (2020).
Wong, S. H. et al. Gavage of fecal samples from patients with colorectal cancer promotes intestinal carcinogenesis in Germ-Free and conventional mice. Gastroenterology 153, 1621–1633 (2017).
Li, L. et al. Gut microbiota from colorectal cancer patients enhances the progression of intestinal adenoma in Apc(min/+) mice. EBioMedicine 48, 301–315 (2019).
Rosshart, S. P. et al. Wild mouse gut microbiota promotes host fitness and improves disease resistance. Cell 171, 1015–1028e13 (2017).
Zackular, J. P. et al. The gut Microbiome modulates colon tumorigenesis. MBio 4, e00692-13 (2013).
Baxter, N. T., Zackular, J. P., Chen, G. Y. & Schloss, P. D. Structure of the gut Microbiome following colonization with human feces determines colonic tumor burden. Microbiome 2, 20 (2014).
Mähler, M. et al. FELASA recommendations for the health monitoring of mouse, rat, hamster, Guinea pig and rabbit colonies in breeding and experimental units. Lab. Anim. 48, 178–192 (2014).
du Sert, N. P. et al. The ARRIVE guidelines 2.0: Updated guidelines for reporting animal research. PLoS Biol. 18, e3000410 (2020).
Thaker, A. I., Shaker, A., Suprada Rao, M. & Ciorba, M. A. Modeling Colitis-Associated cancer with azoxymethane (AOM) and dextran sulfate sodium (DSS). J. Vis. Exp. https://doi.org/10.3791/4100 (2012).
Parang, B., Barrett, C. W. & Williams, C. S. AOM/DSS model of Colitis-Associated cancer. Methods Mol. Biol. 1422, 297 (2016).
Borisova, M. A. et al. Fucose ameliorates tryptophan metabolism and behavioral abnormalities in a mouse model of chronic colitis. Nutrients 12, 445 (2020).
Bolyen, E. et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat. Biotechnol. 37, 852–857 (2019).
Amir, A. et al. Deblur rapidly resolves single-nucleotide community sequence patterns. mSystems 2, e00191-16 (2017).
Quast, C. et al. The SILVA ribosomal RNA gene database project: Improved data processing and web-based tools. Nucleic Acids Res. 41, D590 (2013).
Bokulich, N. A. et al. Optimizing taxonomic classification of marker-gene amplicon sequences with QIIME 2’s q2-feature-classifier plugin. Microbiome 6, 1–17 (2018).
Lu, Y. et al. MicrobiomeAnalyst 2.0: Comprehensive statistical, functional and integrative analysis of Microbiome data. Nucleic Acids Res. 51, W310–W318 (2023).
Segata, N. et al. Metagenomic biomarker discovery and explanation. Genome Biol. 12, R60 (2011).
Morozova, M. V. et al. Colitis-associated intestinal microbiota regulates brain Glycine and host behavior in mice. Sci. Rep. 2022. 121 (12), 1–18 (2022).
Yanshole, V. V. et al. Animal metabolite database: Metabolite concentrations in animal tissues and convenient comparison of quantitative metabolomic data. Metab. 2023. 13, 1088 (2023).
Bian, X. et al. Administration of Akkermansia muciniphila ameliorates dextran sulfate Sodium-Induced ulcerative colitis in mice. Front. Microbiol. 10, 2259 (2019).
Zhai, R. et al. Strain-specific anti-inflammatory properties of two Akkermansia muciniphila strains on chronic colitis in mice. Front. Cell. Infect. Microbiol. 9, 239 (2019).
Wang, F. et al. Akkermansia muciniphila administration exacerbated the development of colitis-associated colorectal cancer in mice. J. Cancer. 13, 124 (2022).
Carbonero, F., Benefiel, A. C., Alizadeh-Ghamsari, A. H. & Gaskins, H. R. Microbial pathways in colonic sulfur metabolism and links with health and disease. Front. Physiol. 3, 448 (2012).
Crouch, L. I. et al. The role of glycans in health and disease: Regulators of the interaction between gut microbiota and host immune system. Semin Immunol. 73, 101891 (2024).
Culp, E. J. & Goodman, A. L. Cross-feeding in the gut microbiome: ecology and mechanisms. Cell. Host Microbe. 31, 485–499 (2023).
Avril, M. & DePaolo, R. W. Driver-passenger bacteria and their metabolites in the pathogenesis of colorectal cancer. Gut Microbes 13, 1941710 (2021).
Liu, Q. et al. Akkermansia muciniphila exerts Strain-Specific effects on DSS-Induced ulcerative colitis in mice. Front. Cell. Infect. Microbiol. 11, 698914 (2021).
Zheng, C. et al. Bacteroides acidifaciens and its derived extracellular vesicles improve DSS-induced colitis. Front. Microbiol. 14, 1304232 (2023).
Wang, L. et al. Original research: A purified membrane protein from Akkermansia muciniphila or the pasteurised bacterium blunts colitis associated tumourigenesis by modulation of CD8 + T cells in mice. Gut 69, 1988 (2020).
Ma, X. et al. The alleviating effect of Akkermansia muciniphila PROBIO on AOM/DSS-induced colorectal cancer in mice and its regulatory effect on gut microbiota. J. Funct. Foods. 114, 106091 (2024).
Derrien, M., Vaughan, E. E., Plugge, C. M. & de Vos, W. M. Akkermansia muciniphila gen. Nov., Sp. Nov., a human intestinal mucin-degrading bacterium. Int. J. Syst. Evol. Microbiol. 54, 1469–1476 (2004).
Martens, E. C., Chiang, H. C. & Gordon, J. I. Mucosal glycan foraging enhances fitness and transmission of a saccharolytic human gut bacterial symbiont. Cell. Host Microbe. 4, 447 (2008).
Crouch, L. I. et al. Prominent members of the human gut microbiota express endo-acting O-glycanases to initiate mucin breakdown. Nat. Commun. 11, 1–13 (2020).
Bae, M. et al. Akkermansia muciniphila phospholipid induces homeostatic immune responses. Nature 608, 168–173 (2022).
Peña-Cearra, A. et al. Akkermansia muciniphila-induced trained immune phenotype increases bacterial intracellular survival and attenuates inflammation. Commun. Biol. 7, 192 (2024).
Wang, B. et al. Stable colonization of Akkermansia muciniphila educates host intestinal microecology and immunity to battle against inflammatory intestinal diseases. Exp. Mol. Med. 55, 55–68 (2023).
Wade, H. et al. Akkermansia muciniphila and its membrane protein ameliorate intestinal inflammatory stress and promote epithelial wound healing via CREBH and miR-143/145. J. Biomed. Sci. 30, 38 (2023).
Ganesh, B. P. et al. Commensal Akkermansia muciniphila exacerbates gut inflammation in Salmonella Typhimurium-infected gnotobiotic mice. PLoS ONE. 8, e74963 (2013).
Liu, Y. et al. Akkermansia muciniphila exerts strain-specific effects on DSS-induced ulcerative colitis in mice. Front. Cell. Infect. Microbiol. 11, 698914 (2021).
Wu, Y. et al. Galactooligosaccharides and Limosilactobacillus reuteri synergistically alleviate gut inflammation and barrier dysfunction by enriching Bacteroides acidifaciens for Pentadecanoic acid biosynthesis. Nat. Commun. 15, 9291 (2024).
Zheng, Y. et al. Bacteroides acidifaciens and its derived extracellular vesicles improve DSS-induced colitis. Front. Microbiol. 14, 1304232 (2023).
Mitchell, C. et al. Regulation of Bacteroides acidifaciens by the Aryl hydrocarbon receptor in IL-22-producing immune cells has sex-dependent consequential impact on colitis. Front. Immunol. 15, 1444045 (2024).
Singh, S. B., Carroll-Portillo, A. & Lin, H. C. Desulfovibrio in the Gut: The enemy within? Microorganisms 11, 1772 (2023).
Blachier, F. et al. Production of hydrogen sulfide by the intestinal microbiota and epithelial cells and consequences for the colonic and rectal mucosa. Am. J. Physiol. - Gastrointest. Liver Physiol. 320, G125–G135 (2021).
Feng, Q. et al. Gut microbiome development along the colorectal adenoma–carcinoma sequence. Nat. Commun. 6, 1–13 (2015).
Hale, V. L. et al. Shifts in the fecal microbiota associated with adenomatous polyps. Cancer Epidemiol. Biomarkers Prev. 26, 85–94 (2017).
Hale, V. L. et al. Synthesis of multi-omic data and community metabolic models reveals insights into the role of hydrogen sulfide in colon cancer. Methods 149, 59 (2018).
Wolf, P. G. et al. Diversity and distribution of sulfur metabolic genes in the human gut Microbiome and their association with colorectal cancer. Microbiome 10, 1–16 (2022).
Szabo, C. et al. Tumor-derived hydrogen sulfide, produced by cystathionine-β-synthase, stimulates bioenergetics, cell proliferation, and angiogenesis in colon cancer. Proc. Natl. Acad. Sci. U S A. 110, 12474–12479 (2013).
Cai, W., Wang, M., Ju, L., Wang, C. & Zhu, Y. Hydrogen sulfide induces human colon cancer cell proliferation: role of Akt, ERK and p21. Cell. Biol. Int. 34, 565–572 (2010).
Untereiner, A. A., Oláh, G., Módis, K., Hellmich, M. R. & Szabo, C. H2S-induced S-sulfhydration of lactate dehydrogenase a (LDHA) stimulates cellular bioenergetics in HCT116 colon cancer cells. Biochem. Pharmacol. 136, 86–98 (2017).
Nie, Y. et al. Desulfovibrio fairfieldensis-Derived outer membrane vesicles damage epithelial barrier and induce inflammation and pyroptosis in macrophages. Cells 12, 89 (2023).
Miyamoto, Y. & Itoh, K. Bacteroides acidifaciens Sp. nov., isolated from the caecum of mice. Int. J. Syst. Evol. Microbiol. 50 Pt 1, 145–148 (2000).
Reichardt, N. et al. Phylogenetic distribution of three pathways for propionate production within the human gut microbiota. ISME J. 86 (8), 1323–1335. 2014 (2014).
Ghotaslou, R. et al. The metabolic, protective, and immune functions of Akkermansia muciniphila. Microbiol. Res. 266, 127245 (2023).
Song, C. H. et al. Combination treatment with 17β-estradiol and anti-PD-L1 suppresses MC38 tumor growth by reducing PD-L1 expression and enhancing M1 macrophage population in MC38 colon tumor model. Cancer Lett. 543, 215780 (2022).
Lee, S. M. et al. The effect of sex on the azoxymethane/dextran sulfate Sodium-treated mice model of colon cancer. J. Cancer Prev. 21 (4), 271–278 (2016).
Al-Fakhrany, O. M. & Elekhnawy, E. Next-generation probiotics: the upcoming biotherapeutics. Mol. Biol. Rep. 51, 505 (2024).
Zhao, Y. et al. Akkermansia muciniphila: A promising probiotic against inflammation and metabolic disorders. Virulence 15, 2375555 (2024).
Acknowledgements
This research was funded by the Russian Science Foundation, grant number 23-75-01094.
Author information
Authors and Affiliations
Contributions
Formal analysis, K.M.A. and E.N.K.; Funding acquisition, A.K.M.; Investigation, K.M.A., O.A.S., K.E.C., M.V.M. and E.N.K., Methodology, K.M.A., O.A.S., and E.N.K.; Supervision, E.N.K.; Writing—original draft, K.M.A. and E.N.K.; Writing—review & editing, K.M.A., O.A.S., K.E.C, M.V.M., Y.P.T, and E.N.K. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Achasova, K.M., Snytnikova, O.A., Chanushkina, K.E. et al. Baseline abundance of Akkermansia muciniphila and Bacteroides acidifaciens in a healthy state predicts inflammation associated tumorigenesis in the AOM/DSS mouse model. Sci Rep 15, 12241 (2025). https://doi.org/10.1038/s41598-025-96514-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-96514-5