Abstract
The removal of titanium plates after maxillofacial trauma is influenced by various patient- and plate-related factors. Understanding these factors can help improve surgical outcomes and minimize complications associated with plate retention or removal. The study employed a prospective cohort design and was conducted over a period of 16 months, from June 2023 to October 2024 included 420 patients who underwent titanium plate removal following maxillofacial trauma. Patients were followed up at intervals of 1 week, 1 month, and 3 months postoperatively to evaluate surgical outcomes, functional recovery, and any long-term complications. Data on demographics, trauma characteristics, plate type, anatomical location, and postoperative outcomes were statistically evaluated using chi-square tests. Persistent pain (70%), infection (91%), and plate exposure (28%) were the most common reasons for plate removal. Gender (p < 0.001), occupation (p < 0.001), and trauma etiology (p < 0.001) significantly influenced outcomes. Mandibular plates (63%) and titanium alloy plates (70%) exhibited higher complication rates. Postoperative satisfaction was reported by 56% of patients, though 84% required additional surgeries (p < 0.001). This study identifies key factors influencing titanium plate removal and highlights the need for individualized treatment strategies to optimize patient outcomes and satisfaction.
Similar content being viewed by others
Introduction
The use of titanium bone plates has revolutionized the management of maxillofacial trauma by providing stability and facilitating bone healing in complex fractures1. However, the need for plate removal due to complications such as infection, discomfort, and other associated issues remains a significant concern in clinical practice2. Despite advancements in plate design and surgical techniques, a substantial number of patients still undergo secondary surgeries for plate removal, raising questions about the factors influencing these outcomes3,4. Understanding these factors is critical for improving patient care, optimizing treatment strategies, and minimizing the need for reoperations5.
Maxillofacial trauma frequently results from high-impact events such as road traffic accidents, physical assaults, falls, and sports injuries. These injuries are often severe, requiring surgical intervention to restore both functional and aesthetic aspects of the facial skeleton6. Titanium plates, due to their biocompatibility, strength, and resistance to corrosion, are the material of choice for fixation in such cases. However, postoperative complications such as plate exposure, infection, and patient discomfort can necessitate removal6,7,8. Identifying the underlying causes and associated factors leading to these complications is essential for refining surgical approaches and improving long-term outcomes.
The use of titanium bone plates has revolutionized the management of maxillofacial trauma by providing stability and facilitating bone healing in complex fractures1,9. However, the need for plate removal due to complications such as infection, discomfort, and other associated issues remains a significant concern in clinical practice10. Despite advancements in plate design and surgical techniques, a substantial number of patients still undergo secondary surgeries for plate removal, raising questions about the factors influencing these outcomes. Understanding these factors is critical for improving patient care, optimizing treatment strategies, and minimizing the need for reoperations.
Previous studies have highlighted the importance of infection control, anatomical considerations, and patient-specific factors in the management of maxillofacial trauma11,12,13,14. However, comprehensive analyses integrating these variables into a single framework are limited. This gap in the literature underscores the need for a detailed evaluation of the frequency and causes of titanium plate removal, as well as the associated complications and outcomes.
This study aims to address this gap by exploring the demographic, clinical, and surgical factors influencing the removal of titanium bone plates in patients with maxillofacial trauma. By examining a large dataset and employing statistical analyses, the research aims to elucidate patterns and associations that may inform clinical decision-making. Specifically, the study investigates variables such as patient demographics, etiology of trauma, anatomical location and type of titanium plates, and reasons for plate removal. Additionally, it examines the impact of these factors on postoperative complications and patient satisfaction.
The findings of this study are expected to contribute to the development of evidence-based guidelines for the management of titanium plates in maxillofacial trauma, ultimately improving patient care and quality of life.
Methods and materials
Study setting and ethical approval
This study was conducted in the Department of Oral and Maxillofacial Surgery at Lady Reading Hospital, Peshawar, Pakistan. Ethical clearance was granted by the Research Ethical Committee of Iqra National University, Department of Allied Health Sciences, Peshawar, Pakistan (Ref: INU/AHS/157 − 23). The study adhered to the principles outlined in the Declaration of Helsinki for conducting research involving human participants.
Study design and duration
The research employed a prospective cohort study design and was carried out over a period of 16 months, from June 2023 to October 2024.
Study population
The study population comprised patients requiring oral and maxillofacial surgical interventions i.e., plate removal. Participants were selected based on the inclusion and exclusion criteria outlined below:
Inclusion criteria:
-
1.
Patients aged 4–65 years undergoing oral and maxillofacial surgery.
-
2.
Individuals who provided written informed consent to participate in the study.
-
3.
Patients with no significant medical comorbidities (diabetes, chest infection and cardiac problems etc.) that could interfere with the outcomes.
Exclusion criteria:
-
1.
Patients with systemic illnesses contraindicating surgical procedures.
-
2.
Individuals unable to provide informed consent.
-
3.
Pregnant or lactating women.
Sample size and sampling technique
The sample size was calculated based on an expected proportion of the target outcomes and a 95% confidence interval with a 5% margin of error. A total of 420 participants were recruited using a consecutive sampling technique to ensure a representative sample of the study population.
Language correction
ChatGPT 3.5 was used for language correction and clarity of purpose. Moreover, all the manuscript was proofread after the use of ChatGPT.
Data collection
Data were collected using a structured pro forma that included patient demographics, clinical history, diagnostic findings, and procedural details. The data collection tool was piloted on a subset of patients (n = 100) to ensure its validity and reliability before full-scale implementation. The study utilized a structured questionnaire to collect data on various aspects, including patient demographics, clinical history, reasons for plate removal, and postoperative outcomes. Patient satisfaction was assessed through binary questions and open-ended responses, focusing on quality of life improvements, recommendations for the procedure, and additional comments. The questionnaire was designed to capture both quantitative and qualitative data to provide a comprehensive evaluation of the outcomes associated with titanium plate removal.
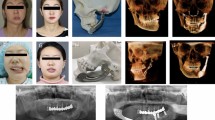
Diagnostic modalities
All patients underwent diagnostic workups tailored to their clinical presentations, including imaging modalities such as:
-
1.
Magnetic Resonance Imaging (MRI): For assessing soft tissue involvement.
-
2.
Computed Tomography (CT) Scans: For evaluating bony structures.
-
3.
Magnetic Resonance Spectroscopy (MRS): For detecting metabolic alterations indicative of neoplastic or inflammatory processes, when applicable.
Surgical procedures
Patients underwent standard oral and maxillofacial surgical procedures based on their diagnoses. Surgical interventions included but were not limited to:
-
1.
Tumor excision with appropriate margins.
-
2.
Reconstructive surgery using autologous or alloplastic materials.
-
3.
Management of maxillofacial trauma using rigid fixation techniques.
Postoperative care and Follow-up
Postoperative care was standardized across all patients, including:
-
1.
Monitoring for immediate complications such as infection or hemorrhage.
-
2.
Pain management using nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids as needed.
-
3.
Wound care protocols to prevent infection and ensure optimal healing.
Patients were followed up at 1-week, 1-month, and 3-month intervals postoperatively to evaluate surgical outcomes, functional recovery, and any long-term complications. Moreover, postoperative infections were managed using a standardized antibiotic regimen consisting of amoxicillin with clavulanic acid and metronidazole (Flagyl) for 5 days. This approach effectively controlled infections in the majority of cases, minimizing the need for prolonged antibiotic use or additional interventions. The regimen was adjusted in cases of clinical non-response or based on microbiological findings.
Data analysis
The collected data were analyzed using SPSS (version 28.0). Descriptive statistics were used to summarize demographic and clinical characteristics. Continuous variables were expressed as means and standard deviations, while categorical variables were presented as frequencies and percentages. Inferential statistical tests, such as the chi-square test for categorical variables. A p-value of < 0.05 was considered statistically significant.
Results
Table 1 presents the descriptive statistics for the demographic characteristics of the participants, including age, height, and weight. The mean age of the participants was 29.87 ± 8.79 years, with a minimum of 4.9 years and a maximum of 55 years, indicating a relatively wide age range in the study population. The mean height was 1.561 ± 0.201 m, with a minimum of 0.948 m and a maximum of 1.83 m, reflecting a moderate variation in height. The mean weight was 76.07 ± 18.33 kg, with a minimum of 43 kg and a maximum of 107 kg, showing a broad distribution of body weights among the participants.
Table 2 provides an overview of the distribution of participants based on gender, occupation, and time relapse since maxillofacial trauma. Regarding gender, the sample was predominantly male, with 301 males (71.67%) compared to 119 females (28.33%). Regarding occupation, most participants were unemployed, accounting for 168 individuals (40%). The next largest group was employed participants, comprising 119 individuals (28.33%), followed by students (112 participants, or 26.67%). A smaller proportion of participants were retired, with only 21 individuals (5%) reporting this occupation. Lastly, the time relapse since maxillofacial trauma indicates that a significant proportion of participants (224, or 53.33%) experienced their trauma less than 6 months ago. This relatively short time frame suggests that the study may be focused on more acute cases of maxillofacial injuries, which could have implications for the surgical interventions and recovery outcomes being studied. The remaining participants experienced trauma more than 6 months ago, though the exact percentages for these groups are not provided here.
Table 3 presents the distribution of participants based on the anatomical location of titanium plates and the type of titanium plate used in the maxillofacial surgeries.
Regarding the anatomical location, most titanium plates were placed in the mandible bone, with 161 participants (38.33%) receiving plates in this area. The zygomatic bone was the second most common location, with 105 participants (25%). The maxilla followed closely with 98 participants (23.33%), while the orbital bone and nasal bone accounted for smaller proportions, at 35 participants (8.33%) and 21 participants (5%), respectively. These findings suggest that mandible and zygomatic bones are the most common sites for titanium plate placement, likely due to the higher incidence of fractures in these areas in maxillofacial trauma cases.
Regarding the type of titanium plate used, most patients received microplates, with 224 participants (53.33%) undergoing this procedure. The next most commonly used type was the miniplate, applied to 150 participants (35.33%), while other plate types (such as larger plates or customized implants) were used in a smaller proportion of cases as shown in Table 3.
Factors influencing titanium plate removal in maxillofacial trauma management
The removal of titanium plates in maxillofacial surgery is a multifactorial decision influenced by patient demographics, trauma characteristics, and surgical factors. The association of these variables with the reasons for plate removal, providing insights into clinical decision-making processes and potential areas for optimization is illustrated in Table 3.
Gender was significantly associated with the reasons for titanium plate removal (p < 0.001). Male participants were more likely to report persistent pain (50.17%), infection (65.22%), and plate exposure (30.1%), while female participants had lower frequencies across these categories. Occupation also played a significant role (p < 0.001), with unemployed individuals more likely to request plate removal due to discomfort (14%), persistent pain (35%), and infection (35%). In contrast, students reported plate removal primarily due to growing age (77%), reflecting the need for plate removal in pediatric or adolescent patients to accommodate skeletal growth. The time elapsed since maxillofacial trauma and the etiology of the injury were significantly associated with plate removal (p < 0.001). Plates were most commonly removed within six months of trauma due to infection (42%), persistent pain (28%), and plate palpability (35%). In contrast, plate removal more than two years post-trauma was often linked to growing age (77%) or surgeon recommendations (7%).
The etiology of maxillofacial trauma also influenced (p < 0.001) removal reasons. Road Traffic Accidents were the most frequent cause, accounting for persistent pain (42%) and infection (35%), likely due to the severity and complexity of such injuries. Physical assault and falls were associated with varied reasons, including plate exposure (21%) and surgeon recommendations (28%), underscoring the individualized nature of plate removal decisions. The anatomical location of titanium plates significantly influenced removal reasons (p < 0.001). Plates in the mandible were more likely to be removed due to infection (63%) and persistent pain (21%), consistent with the high mechanical loads and functional demands in this region. Plates in the maxilla and zygomatic bones were associated with discomfort (21%) and plate exposure (21%), reflecting the aesthetic and structural challenges in these areas. The type of titanium plate also played a role, with manipulates being associated with infection (63%) and persistent pain (21%), while microplates were more often removed due to plate exposure (35%) and growing age (42%). Reconstruction plates, though used less frequently, were associated with surgeon recommendations (7%) and specific complications such as bone healing difficulties as shown in Table 4.
Titanium alloy plates (p < 0.001) were more frequently removed due to infection (70%) and plate exposure (35%), possibly due to their widespread use in high-stress areas like the mandible. Pure titanium plates, while less common, were associated with patient requests for removal (42%) and allergic reactions (7%). The duration since plate insertion also influenced removal (p < 0.001), with plates in place for less than six months being removed primarily due to infection (42%) and persistent pain (28%). Plates retained for over two years were more likely to be removed (p < 0.001) due to growing age (77%), highlighting the temporal considerations in maxillofacial plate management. The history of previous surgeries was another significant factor (p < 0.001). Post-removal complications varied, with infection (70%) and persistent pain (21%) being the most common. However, a notable proportion of participants (38.33%) experienced no complications, indicating the potential for successful outcomes with proper management. Despite the challenges, patient satisfaction with plate removal was high, with 71.67% reporting satisfaction or high satisfaction (p < 0.001). Improvements in quality of life were reported by 76.67%, and 68.33% of participants would recommend plate removal to others with similar issues as depicted in Table 4.
The analysis in Fig. 1 evaluates the strength of associations between various factors and the removal of titanium plates in maxillofacial trauma cases using Cramér’s V coefficient, which ranges from 0 (no association) to 1 (perfect association). The strength of association is interpreted as follows: 0.0–0.1 indicates negligible association, 0.1–0.3 weak association, 0.3–0.5 moderate association, and above 0.5 strong association.
Key findings reveal a strong association (Cramér’s V > 0.5) for the primary reason for titanium plate removal (0.545). Moderate associations (0.3–0.5) were observed for factors such as the time lapse since maxillofacial trauma (0.432), the duration since plate insertion (0.432), and the etiology of trauma (0.332). Weak associations (0.1–0.3) were identified for occupation (0.283), history of previous surgery (0.277), anatomical location of the plate (0.166), type of titanium plate used (0.160), and the plate material (0.147). Gender demonstrated a negligible association (0.056) as shown in Fig. 1.
Discussion
The multifactorial nature of titanium plate removal following maxillofacial trauma underscores the complexity of treatment outcomes. Our study aimed to investigate the factors influencing the removal of titanium plates in patients with maxillofacial trauma, with the hypothesis that specific demographic, clinical, and surgical variables are associated with plate removal. The findings of the study support this hypothesis, as significant associations were observed between plate removal and variables such as infection, discomfort, and anatomical location of the plates.
Gender differences in plate removal
The study highlighted a significant association between gender and reasons for plate removal (p< 0.001). Male patients exhibited higher rates of persistent pain (50.17%), infection (65.22%), and plate exposure (30.1%). These results mirror findings by Alpert et al. (2011), where males showed increased removal rates due to higher trauma severity, often linked to RTAs15. Female patients reported fewer complications, with patient requests (19.83%) being the most common cause of removal, potentially reflecting different aesthetic concerns or pain thresholds16,17. The gender-based differences in reasons for plate removal highlight the need for a more nuanced understanding of the underlying factors. While the higher rates of complications in male patients may be linked to the severity of trauma, as suggested by Alpert et al. (2011), the role of gender-specific pain perception and aesthetic concerns in driving removal requests among female patients requires further investigation15.
Occupational influence
Occupation significantly impacted plate removal reasons (p< 0.001). Unemployed patients had higher rates of discomfort (14%) and infection (35%), which could relate to delayed medical attention and suboptimal postoperative care, as noted by Schortinghuis et al. (2005)18. Conversely, employed individuals experienced lower rates of infection (35%) and requested fewer removals due to palpability (28%). Students reported plate removal predominantly for growing age concerns (77%), consistent with Sauerbier et al. (2008), who emphasized age-specific considerations in titanium plate use19.
Time elapsed since trauma
The duration since maxillofacial trauma significantly influenced removal factors (p< 0.001). Plates removed within six months were primarily associated with infection (42%) and pain (28%), reflecting acute complications. These findings align with Choi et al. (2010), who identified early postoperative infection as a primary driver for hardware removal20. Plates retained for over two years were often removed due to surgeon recommendations (7%) or growing age (77%), corroborating Schneider et al. (2019), who highlighted long-term considerations in pediatric and adolescent patients21.
Etiology of maxillofacial trauma
The trauma’s etiology was significantly associated with removal factors (p< 0.001). Road Traffic Accidents accounted for the highest removal rates due to persistent pain (42%) and infection (35%), consistent with Ellis et al. (1996), who found that high-impact injuries often lead to complications requiring plate removal22. Physical assaults and falls were associated with varying causes, including plate exposure (21%) and surgeon recommendations (28%), suggesting individualized outcomes based on trauma mechanisms, as highlighted by Rai et al. (2018)23,24.
Anatomical location of plates
The anatomical site of plate placement significantly impacted removal factors (p< 0.001). Mandibular plates were predominantly removed for infection (63%) and pain (21%), reflecting the mandible’s high mechanical load and susceptibility to complications10. Plates in the maxilla and zygomatic bone were more often removed for discomfort (21%) and exposure (21%), consistent with Bagán et al. (2010), who emphasized the structural and aesthetic challenges in these areas25. The significant impact of anatomical site on plate removal reflects the unique challenges associated with different facial regions. Mandibular plates were predominantly removed for infection and pain, likely due to the mandible’s high mechanical load and susceptibility to complications, consistent with findings by Bagán et al. (2010). In contrast, plates in the maxilla and zygomatic bone were more often removed for discomfort and exposure, emphasizing the structural and aesthetic challenges in these areas25.
Type and material of titanium plates
The type of titanium plate used significantly influenced removal factors (p< 0.001). Manipulates were associated with infection (63%) and pain (21%), while microplates showed higher removal rates due to exposure (35%) and growing age (42%). These findings align with Bhatt et al. (2014), who highlighted exposure risks with microplates in thin soft tissue areas26. Titanium alloy plates were predominantly removed due to infection (70%) and plate exposure (35%), whereas pure titanium plates were more frequently removed at the patient’s request (42%), reflecting their superior biocompatibility but increased palpability awareness, as noted by Gear et al. (2004)27.
History of previous surgeries and postoperative complications
A history of prior surgeries significantly influenced removal reasons (p< 0.001). Patients without previous surgeries had higher removal rates for pain (50.17%) and infection (65.22%), while those with prior surgeries reported fewer complications, possibly due to enhanced surgical precision or experience. Chronic infection and bone healing complications were notable in patients with prior surgeries, consistent with findings from Jang et al. (2018)28.
Post-removal complications, such as infection (70%) and non-healing wounds (28%), underscore the challenges associated with titanium plate removal. However, 49% of patients reported no complications post-removal, reflecting improved surgical techniques and postoperative care protocols29. Additional surgeries were required in 70% of cases with persistent pain or infection, emphasizing the need for comprehensive pre-removal planning.
Patient satisfaction and quality of life
Satisfaction with the removal surgery outcome was generally high (56% satisfied, 21% very satisfied), with improvements in pain and discomfort being the primary reasons. These findings align with Lim et al. (2015), who reported significant quality-of-life improvements following plate removal. However, dissatisfaction was noted in 14% of cases, primarily due to postoperative complications or unmet expectations, highlighting areas for further improvement16. The generally high levels of patient satisfaction and reported improvements in quality of life following plate removal are encouraging, aligning with the existing literature. However, the persistent dissatisfaction in a notable proportion of cases, primarily due to postoperative complications or unmet expectations, underscores the need for a more comprehensive approach to patient counseling, surgical decision-making, and postoperative care to optimize outcomes16. The higher rates of infection and pain observed in this study compared to European population is attributed to differences in patient populations, healthcare settings, and trauma severity30. Factors such as limited healthcare resources, variations in infection control protocols, and more severe trauma cases in the study population likely contributed to these findings31. Additionally, socioeconomic and cultural factors, including access to healthcare, compliance with postoperative care, and beliefs about pain management, may have influenced the outcomes. These differences highlight the need for further comparative studies to better understand and address these disparities. Due to the limited availability of studies specifically addressing titanium plate removal in maxillofacial trauma, some references in this discussion are derived from orthopedic literature. While these studies provide valuable insights into the biomechanical and clinical factors influencing implant outcomes, their applicability to maxillofacial implants may be limited. This highlights the need for further research specifically focused on titanium plates in maxillofacial trauma to strengthen the evidence base and provide more directly applicable findings.
Conclusion
This study demonstrated the multifactorial reasons influencing the removal of titanium plates following maxillofacial trauma, emphasizing the interplay of patient demographics, trauma characteristics, plate types, and anatomical considerations. Persistent pain, infection, and discomfort emerged as the most common factors necessitating plate removal, with gender, occupation, and time elapsed since trauma playing significant roles. Anatomical location and plate material also significantly influenced outcomes, with mandibular plates and titanium alloy plates exhibiting higher rates of complications.
While most patients reported satisfaction following plate removal, postoperative complications, such as infection and the need for additional surgeries, underscore the challenges in managing such cases.
Future research should focus on developing advanced biomaterials and techniques to reduce complications and improve long-term outcomes. Additionally, a standardized approach to patient counseling, surgical decision-making, and postoperative care is essential to optimize patient satisfaction and quality of life. Addressing these factors comprehensively will enhance treatment protocols and provide better healthcare outcomes for patients undergoing maxillofacial trauma management. Moreover, future studies should consider performing a comparative analysis of different titanium plate systems to evaluate the impact of plate design, material, and other characteristics on complication rates, infections, and mechanical failure, which could provide valuable insights for improving patient outcomes.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- MRI:
-
Magnetic Resonance Imaging
- CT:
-
Computed Tomography
- MRS:
-
Magnetic Resonance Spectroscopy
- NSAIDs:
-
Nonsteroidal Anti-Inflammatory Drugs
- RTA:
-
Road Traffic Accident
- SPSS:
-
Statistical Package for the Social Sciences
References
Gilardino, M. S., Chen, E. & Bartlett, S. P. Choice of internal rigid fixation materials in the treatment of facial fractures. Craniomaxillofac. Trauma. Reconstr. 2 (1), 49–60 (2009).
Abd-Elaziem, W., Darwish, M. A., Hamada, A. & Daoush, W. M. Titanium-Based alloys and composites for orthopedic implants applications: A comprehensive review. Mater. Design. 241, 112850 (2024).
Yadav, A. Principles of Internal Fixation in Maxillofacial Surgery. In: Oral and Maxillofacial Surgery for the Clinician. edn. Edited by Bonanthaya K, Panneerselvam E, Manuel S, Kumar VV, Rai A. Singapore: Springer Nature Singapore; : 1039–1051. (2021).
Cho, R-Y. et al. Patient-specific plates for facial fracture surgery: A retrospective case series. J. Dent. 137, 104650 (2023).
Ahmad, W. et al. Fixation in Maxillofacial Surgery—Past, Present and Future: A Narrative Review Article. FACE 5(1):126–132. (2024).
Fama, F. et al. Maxillofacial and concomitant serious injuries: an eight-year single center experience. Chin. J. Traumatol. 20 (1), 4–8 (2017).
Agnihotry, A., Fedorowicz, Z., Nasser, M. & Gill, K. S. Resorbable versus titanium plates for orthognathic surgery. Cochrane Database Syst. Rev. 10 (10), Cd006204 (2017).
Bandyopadhyay, A., Mitra, I., Goodman, S. B., Kumar, M. & Bose, S. Improving biocompatibility for next generation of metallic implants. Prog. Mater. Sci. 133, 101053 (2023).
Kaur, N. et al. Efficacy of titanium mesh osteosynthesis in maxillofacial fractures. J. Maxillofac. Oral Surg. 17 (4), 417–424 (2018).
Shah, K. V. et al. Risk factors for plate infection, exposure, and removal in mandibular reconstruction. Otolaryngol. Head Neck Surg. 171 (6), 1705–1714 (2024).
Jose, A., Nagori, S. A., Agarwal, B., Bhutia, O. & Roychoudhury, A. Management of maxillofacial trauma in emergency: an update of challenges and controversies. J. Emerg. Trauma. Shock. 9 (2), 73–80 (2016).
Cicuttin, E. et al. Antibiotic prophylaxis in torso, maxillofacial, and skin traumatic lesions: A systematic review of recent evidence. Antibiotics (Basel). 11(2), 139 (2022).
Chouinard, A-F., Troulis, M. J. & Lahey, E. T. The acute management of facial fractures. Curr. Trauma. Rep. 2 (2), 55–65 (2016).
Kumar, N., Choudhary, R. S., Malhotra, K. & Kathariya, R. Maxillofacial nursing: assessing the knowledge and awareness of nurses in handling maxillofacial injuries through a comprehensive survey. J. Oral. Maxillofac. Surg. 19 (1), 136–142 (2020).
Alodhayani, A. et al. Gender difference in pain management among adult cancer patients in Saudi Arabia: A Cross-Sectional assessment. Front. Psychol. 12, 628223 (2021).
Berkowitz, R. et al. The impact of complications and pain on patient satisfaction. Ann. Surg. 273 (6), 1127–1134 (2021).
Gómez-Barrachina, R. et al. Titanium plate removal in orthognathic surgery: prevalence, causes and risk factors. A systematic literature review and meta-analysis. Int. J. Oral Maxillofac. Surg. 49 (6), 770–778 (2020).
Boyd, B. et al. Risk Factors for Surgical Site Infection after Operative Management of Pilon Fractures, vol. 7; (2022).
Kagaruki, G. B. et al. Barriers to the implementation, uptake and scaling up of the healthy plate model among regular street food consumers: a qualitative inquiry in Dar-es-Salaam City, Tanzania. BMC Nutr. 8 (1), 110 (2022).
Sarraj, M. et al. Management of deep surgical site infections of the spine: a Canadian nationwide survey. J. Spine Surg. 8 (4), 443–452 (2022).
Bottini, G. B., Roccia, F. & Sobrero, F. Management of pediatric mandibular condyle fractures: A literature review. J. Clin. Med. 13(22), 6921 (2024).
Zakeri, H. et al. The etiology of trauma in geriatric traumatic patients refer to an academic trauma center: A cross sectional study. Bull. Emerg. Trauma. 12 (3), 124–129 (2024).
Khurana, B., Bayne, H. N., Prakash, J. & Loder, R. T. Injury patterns and demographics in older adult abuse and falls: A comparative study in emergency department settings. J. Am. Geriatr. Soc. 72 (4), 1011–1022 (2024).
Zohrevandi, B., Shahrestani, M. F., Mohammadnia, H., asadi, K. & Khodadadi-Hassankiadeh, N. Characteristics of blunt and penetrating trauma among victims of physical violence: A retrospective study. BMC Public. Health. 24 (1), 2073 (2024).
Präger, T. M., Brochhagen, H. G., Mischkowski, R., Jost-Brinkmann, P. G. & Müller-Hartwich, R. Bone condition of the maxillary zygomatic process prior to orthodontic anchorage plate fixation. J. Orofac. Orthop. 76 (1), 3–13 (2015).
Khandelwal, P. et al. Miniplate removal in operated cases of maxillofacial region in a dental Institute in Rajasthan, India. Med. Pharm. Rep. 92 (4), 393–400 (2019).
Prestat, M. & Thierry, D. Corrosion of titanium under simulated inflammation conditions: clinical context and in vitro investigations. Acta Biomater. 136, 72–87 (2021).
Torensma, B., Hany, M., Bakker, M. J. S. & van Velzen, M. Veld BA, Dahan A, Swank DJ: Cross-sectional E-survey on the Incidence of Pre- and Postoperative Chronic Pain in Bariatric Surgery. Obes Surg 33(1):204–210. (2023).
Almusallam, W. A. L. et al. Etiologies of orthopedic implant removal among patients who underwent orthopedic fixation surgeries in King Abdulaziz medical City. Cureus 15 (8), e43809 (2023).
Asya, O. et al. A retrospective epidemiological analysis of maxillofacial fractures at a tertiary referral hospital in Istanbul: a seven-year study of 1,757 patients. Maxillofac. Plast. Reconstr. Surg. 46 (1), 37 (2024).
Tan, F. Y. et al. Length of hospital stay among oral and maxillofacial patients: a retrospective study. J. Korean Assoc. Oral Maxillofac. Surg. 47 (1), 25–33 (2021).
Author information
Authors and Affiliations
Contributions
MG; Article Conceptualization, Article writing, Data Collection and Proofreading, MG; Article Conceptualization, Article writing, and Data Analysis, FI; Article Conceptualization, Article writing, Data Analysis, Review for Language Check, Formatting the Article, MJU; Data Collection, Data Analysis, and Proofreading, MM; Article Conceptualization, Article writing, Proof Reading, Software Analysis, Supervising the Study, NJ; Conceptualization, Writing, Proofreading, Data Analysis, Data Collection, Administrating, NK; Article Conceptualization, Article writing, Data Analysis, Review for Language Check, Formatting the Article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
All the author have given the consent for publication for submission and publication in this journal.
Ethical approval
This study was conducted in the Department of Oral and Maxillofacial Surgery at Lady Reading Hospital, Peshawar, Pakistan. Ethical clearance was granted by the Research Ethical Committee of Iqra National University, Department of Allied Health Sciences, Peshawar, Pakistan (Ref: INU/AHS/157 − 23). The study adhered to the principles outlined in the Declaration of Helsinki for conducting research involving human participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gul, M., Gul, M., Inayat, F. et al. Analysis of factors influencing the removal of titanium bone plates in maxillofacial trauma patients. Sci Rep 15, 27733 (2025). https://doi.org/10.1038/s41598-025-96586-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-96586-3