Abstract
Pulmonary hypertension (PH) associated with chronic obstructive pulmonary disease (COPD) contributes to mortality. Existing epidemiological research is limited in scale, leading to varied prevalence estimates. Hereby, we aim to evaluate the prevalence and impact of COPD-related PH in individuals with COPD. We used medical-claims data from the national health insurance database (NHIRD) of Taiwan (2009 to 2018). The index date was defined as the initial hospitalization for COPD. We identified patients above 40 year-old with a COPD diagnosis from inpatient claims data and stratified rates of COPD-related PH by gender, age, and COPD severity. We compared short- and long-term mortality between COPD patients with and without PH. To ensure the reliability of our findings, we performed a sensitivity analysis by excluding patients who had not undergone echocardiography. Among 215,292 patients hospitalized primarily for COPD, we found an average COPD-related PH prevalence of 39.9 per 1000 individuals. The annual trend significant declined in prevalence among men but was comparable among women. Furthermore, a higher frequency of COPD-related hospitalization or emergency department visits correlated with an elevated COPD-related PH prevalence, irrespective of age. In comparison to COPD patients without PH, those with this condition exhibited notably higher one-year, three-year, and five-year mortality rates. Collectively, despite a declining trend in COPD-related PH prevalence among COPD patients, its development is closely linked to the severity of COPD. Given the significantly increased mortality rates in COPD patients with PH, early detection of this condition and the implementation of related interventions should be prioritized.
Similar content being viewed by others
Introduction
As the second leading cause of pulmonary hypertension (PH), chronic lung disease related pulmonary hypertension (PH) is associated with increasing morbidity and mortality1,2,3. It is closely linked to chronic obstructive pulmonary disease (COPD) and has become a significant contributor to hospitalization and mortality4,5. Kessler et al. reported that COPD patients with PH demonstrated a markedly reduced survival rate compared to COPD patients without PH6. Conditions directly associated with PH in patients with COPD include loss of the vascular bed and chronic hypoxic pulmonary vasoconstriction caused by alveolar wall destruction7. The severity of PH is correlated with hypoxemia, hypercarbia, and the degree of airway obstruction8,9,10. While the 4-year survival rate for COPD stands at 75%, this rate declines to 50% in cases where COPD is compounded by PH11. Thus, early detection of PH among patients with COPD is critical for reducing the mortality and morbidity associated with the disease2,3. However, a definite diagnosis of PH requires right-heart catheterization (RHC)1. As RHC is an invasive procedure, it is not widely performed1. This limitation may lead to an underdiagnosis of PH1,2,3. Alternatively, echocardiography is the most commonly used noninvasive method for screening PH12. However, even with the growing recognition of PH, the scope of earlier epidemiological investigations remains constrained due to their limited sample sizes. As a result, the reported prevalence rates fluctuate significantly, spanning from 20 to 91%, contingent upon the specific demographics studied8,13. Remarkably, comprehensive nationwide cohort studies that delve into the extent and repercussions of PH within the COPD patient population remain conspicuously absent. This glaring research gap propels the purpose of this cross-sectional study: to meticulously gauge the prevalence of COPD-related PH among individuals afflicted with COPD in Taiwan. To fulfill this aim, we leveraged a population-based longitudinal database from 2009 to 2018, enabling a thorough and illuminating investigation.
Materials and methods
The database
Using the medical-claims data from the national health insurance database (NHIRD), we conducted a cross-sectional study to investigate the prevalence of PH in patients with COPD. The NHIRD covers all healthcare services for approximately 99% of Taiwan’s residents14,15. The NHIRD includes data on age, sex, medications, procedures, and all medical diagnoses from Taiwan’s Single-Payer National Health Insurance program16. Diseases were diagnosed using the International classification of diseases, Ninth Revision Clinical Modification (ICD-9-CM) and Tenth Revision Clinical Modification (ICD-10-CM) codes14,17. The diagnostic accuracy of several diseases, including COPD, in the NHIRD has also been validated16,17. On January 28th, 2022, this study has been reviewed and approved by the Institutional Review Board (IRB:11101-013; entitled “Establishing Chi-Mei cor pulmonale research database- to investigate the prevalence and outcomes of cor pulmonale”) in Chi-Mei Medical Center, Tainan, Taiwan. All methods were performed in accordance with the relevant guidelines and regulations.
Study design
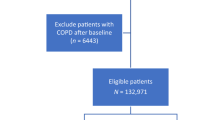
The study design was illustrated in (Fig. 1). We identified patients above 40 year-old with a COPD diagnosis from inpatient claims data from 2009 to 201818,19. We included hospitalized patients with COPD (ICD-9-CM codes 490–492, 496 and ICD-10-CM codes J40-J44) and who were admitted at least once for the principal diagnosis of COPD17. The principal diagnosis is defined as “the condition established after study to be most responsible for the patient’s admission to the hospital”20. The index date was set as the first hospitalization date for COPD. This study estimated the prevalence of COPD-related PH using the number of identified PH cases (ICD-9-CM codes 415.0, 416.8, and 416.9; and ICD-10-CM codes I26.09, I27.2, I27.81, I27.89, and I27.9) from a population of hospitalized patients with COPD in the NHIRD16,17. As addressed in our previous study, using both medical record review and sensitivity tests the accuracy of ICD code for the diagnosis of PH was validated with a specificity of 96.7%21. Patients who had pulmonary hypertension (PH) due to causes other than those listed in (Supplemental Table 1) were not included in the study. Mortality rates were calculated at 1, 3, and 5 years of follow-up from the date during the 9-year study period.
The disease severity was stratified based on the number of admissions and emergency department (ED) visits in the year before the index date. The annual number of hospitalizations is currently considered to reflect the underlying severity of COPD22,23. The prevalence of COPD-related PH was stratified by sex and age categories: ≦50 years, 51–64 years, 65–79 years and ≧ 80 years, ED visits, and hospital admissions. Data on comorbidities were collected for each patient from both the inpatient and outpatient claims databases, covering a period of one year prior to and during the index hospitalization. The severity of comorbid diseases was scored according to the charlson comorbidity index (CCI), updated by Glasheen et al.24. In addition, the differences in the mortality rates at 1, 3, and 5 years between COPD patients with and without PH were analyzed.
Statistics
Yearly trends in the prevalence of COPD-related PH were calculated using a linear trend test and stratified according to sex. The difference in the COPD-related PH rate in patients with COPD according to the number of admissions and ED visits stratified by sex and age group was represented as a percentage. The trend in the rate of COPD-related PH in each group was tested using the Cochran-Armitage trend test. The baseline information, including age, sex, mortality, and CCI of COPD patients with and without PH is shown as a percentage, and the p-value was derived from Pearson’s chi-square test. Also, as echocardiography has been widely used as a screening and follow-up tool to evaluate the severity of PH, as a sensitivity test, we strictly re-defined the diagnosis of COPD-related PH to patients who not only fulfilled ICD codes but also received echocardiography (Procedure Code: 18005, 18006, 18007). The results, including the prevalence of COPD-related PH between sexes and disease severity, will be compared with our main results to verify whether there were any significant differences between the overall population and those who underwent echocardiography. Echocardiography was performed during hospital admission with a principal diagnosis of COPD. The results including the prevalence of COPD-related PH between sexes and disease severity, were compared with our main results to verify whether there were any significant differences between the overall population and those who underwent echocardiography. SAS 9.4 (version 9.4; SAS Institute, Inc., Cary, NC, USA) was used to perform statistical analyses. The resulting data were visualized with Python version 3.8.8 and Matplotlib version 3.3.4 in a Jupyter Notebook environment (version 6.3.0). The significance level (p-value) was set less than 0.05.
Results
The prevalence of COPD-related PH in patients with COPD
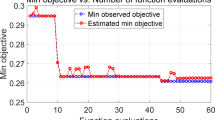
A total of 215,292 patients hospitalized for the first time with a principal diagnosis of COPD were identified. The overall prevalence of COPD-related PH was 39.9 per 1000 person-year among patients hospitalized for COPD (Table 1). Along with the declining prevalence of COPD, a decreasing trend in the prevalence of COPD-related PH was identified from 2009 to 2018 (from 44.8 in 2009 to 33.1 in 2018 per 1000 person-year, p < 0.05). Notably, a significant decrease in the yearly prevalence trend was observed in males (p < 0.05), whereas the yearly prevalence in females was comparable during this period. Focusing on patients with COPD who had more than two admissions in the year before the index date, we also observed a decreasing trend of the ratio of COPD-related PH in (Fig. 2).
Yearly trend of COPD-related PH prevalence according to the severity of COPD
Interestingly, a higher prevalence of COPD-related PH was observed with a higher number of COPD-related admissions (p < 0.01, the Cochran-Armitage trend test) (Table 2). For patients admitted with COPD in the year before the index date, the prevalence of COPD-related PH was 3.03%. In contrast, in patients admitted for three or more times, the prevalence increased to 9.18%. Similarly, the higher the number of emergency room visits for COPD, the higher the prevalence. For patients with COPD who had one ER visit in the past year, the prevalence of COPD-related PH was 4.65%. For patients with COPD who had three or more ER visits in the past year, the prevalence of COPD-related PH was 8.99%. In terms of sex, there was no significant difference in the prevalence of COPD-related PH between male and female patients with COPD with the same number of admissions and ED visits.
Morbidity in patients with COPD-related PH
Although the number of patients hospitalized for COPD increased with age, the highest overall prevalence of COPD-related PH (4.51%) was observed in COPD patients aged 65–79 years-old (Table 3). Similar to our previous findings, the prevalence of COPD-related PH increased with an increase in the number of admissions and ED visits. Depending on age, with the same number of admissions and ED visits, the trends in COPD-related PH prevalence were not significantly different between the different age groups.
Demographic characteristics of COPD patients with and without PH
Demographic characteristics showed no significant differences in the distribution of age and sex between COPD patients with and without PH. Notably, compared with COPD patients free from PH, those with PH had a higher percentage of patients with CCI score ≥ 1, experienced longer hospital stays (days), and had a higher prevalence of obstructive sleep apnea (0.36% vs. 0.15%). Overall, the 1-year, 3-year and 5-year mortality rates were significantly higher in COPD patients with PH than in those without (Table 4).
Sensitivity test (restricting the dataset to patients receiving echocardiography)
To examine the robustness of the outcomes, we performed a sensitivity test by excluding patients who did not undergo echocardiography from the study population. Among the re-defined 4072 patients, the overall prevalence of COPD-related PH was 103.4 per 1000 person-year (Supplemental Table 2). Similarly, with the decreasing prevalence of COPD, the prevalence of COPD-related PH decreased over time in both sexes. Similarly, the prevalence of COPD-related PH increased with the number of admissions and emergency room visits (Supplemental Table 3). The main results, including the prevalence of COPD-related PH between sexes and disease severity, were similar between the overall population and those who underwent echocardiography examinations.
Discussion
In this nationwide study, our findings highlighted that among hospitalized patients with COPD, the overall prevalence of COPD-related PH was 39.9 per 1000 persons. With the declining prevalence of COPD, the incidence of COPD-related PH has decreased in the year before the index date. Nevertheless, the ratio of COPD-related PH increased proportionally with the severity of COPD. Most importantly, compared with COPD patients without PH, those with PH had higher short- and long-term mortality risks. After excluding patients who did not undergo echocardiography, the sensitivity test supported our main findings. To the best of our knowledge, this is the largest nationwide population-based study to estimate the prevalence of COPD-related PH in patients with COPD. Corresponding to previous studies, this study also highlighted a positive correlation between the prevalence of COPD-related PH and the severity of COPD.
Although COPD-related PH has emerged as a major cause of disability and death25, its prevalence of COPD-related PH remains largely unknown. Given the small population and heterogeneous study design, the prevalence of COPD-related PH has varied widely in previous epidemiologic studies26. Thabut et al. reported that among advanced COPD candidates for lung transplantation, the prevalence of pulmonary hypertension was approximately 50%27. Likewise, the organ procurement and tissue network (OPTN) database of 4,930 COPD patients listed for transplantation indicated a similar prevalence of PH (47.6%)28. In contrast, among patients with stage IV disease categorized by the Global Initiative for Chronic Obstructive Lung Disease (GOLD), only 3–5% present with mPAP > 35–40 mmHg29,30. In the work of Scharf et al., among the enrolled 120 COPD patients, the FEV1 was 27.0 ± 7.0, indicating that the majority of them had a very severe degree of obstruction31. The findings derived from their right heart catheterization revealed that 90.8% of the patients demonstrated moderate to severe PH based on their average pulmonary artery (PA) pressures31. Thus, the exact prevalence of COPD-related PH in patients with COPD is difficult to determine.
Compared to interstitial lung diseases and obstructive sleep apnea, COPD is a more prevalent and frequent cause of PH32. In this study, the prevalence of COPD-related PH is estimated 39.9 per 1000 persons among hospitalized patients with COPD. Compared with some small-scale cohorts33, the ratio of PH diagnoses in patients with COPD was relatively low. For instance, among 50 COPD patients in Nepal, 68% were diagnosed with COPD-related PH using echocardiography33. In a study conducted on 507 patients with COPD admitted to medical wards, Shrestha et al. reported a 56.3% prevalence of COPD-related PH34. In contrast to previous studies that have mainly focused on a small number of patients with high-grade disease, our study broadly investigated the prevalence of COPD-related PH in patients of various ages, sexes, and disease severities. A larger sample size of the studied population is likely to yield a more accurate assessment of the prevalence of COPD-related PH.
Notably, we observed a decreasing prevalence of both COPD and PH from 2007 to 2018. In another Taiwanese cohort study, proportion of patients with COPD per 10,000 ICU patients decreased from 2003 to 201335. Similarly, the age-standardized mortality rate of COPD in China decreased significantly between 2005 and 202036. With the advancement of drug and healthcare systems, improving COPD management may suppress the prevalence patterns. In contrast to the decreasing trend in the prevalence of COPD-related PH in males, the yearly prevalence in females did not change significantly. Using the WHO database between 2005 and 2007 and between 2015 and 2017, despite the overall COPD mortality decreased in EU men (-16.3%), it increased in women (12.7%)37. Similarly, in the United States, mortality has declined in men but increased in women38. The potential link between sex specific development of COPD-related PH and survival requires more investigations37.
The outcome of COPD-related PH depends on the underlying cause of PH and the severity of the condition18,32,33. If left untreated or poorly managed, COPD-related PH can lead to serious complications such as heart failure, arrhythmias, and even sudden death32,33,38,39. In this study, we observed that the more frequent the admission or ED visits for COPD, the higher the prevalence of COPD-related PH. Compared to COPD patients without PH, those with PH had higher short- and long-term mortality. This highlights the importance of healthcare providers in monitoring cardiovascular conditions and adjusting treatment in patients with COPD, especially those with more severe disease. A special attention to early detection and intervention for COPD-related PH is necessary.
Strength and limitations
The present study had some limitations. First, in the design of an administrative claims database, clinical information, including blood tests, pulmonary function tests and 6-min walking distances, was missing. Second, as the severity of COPD, such as GOLD stage, which is typically categorized based on post-bronchodilator FEV1, could not be directly assessed from the claims data, we categorized the disease severity of COPD using the number of admissions or emergency department visits. There was a significant correlation between the prevalence of COPD-related PH and severity of COPD. Nevertheless, no effective therapeutic options currently exist for PH secondary to COPD. Third, to ensure the accuracy of claims data, this study included only hospitalized COPD patients. As a result, COPD patients with less severe disease who had never been hospitalized were not included, potentially limiting the generalizability of our findings to the broader COPD population. Fourth, as shown in (Table 4), compared with COPD patients without PH, those with PH had a higher prevalence of obstructive sleep apnea, which may contribute to the development of pulmonary hypertension in some patients. To address the aforementioned limitations and validate our findings, we redefined the study population to include individuals who underwent echocardiographic examinations, conducted a sensitivity analysis, and obtained similar results (Supplemental Figs. 1, 2). While this finding supports the study’s reliability, limitations remain regarding the accuracy of ICD-based diagnosis of PH. Additionally, given that echocardiography was primarily performed during hospital admissions for COPD, the measurement of pulmonary pressures during acute COPD exacerbations may have contributed to the higher incidence of PH among COPD patients.
Collectively, with a decreasing trend in COPD diagnoses, the prevalence of COPD-related PH in patients also declined between 2009 and 2018 in Taiwan. Nevertheless, the development of COPD-related PH was positively correlated with the severity of COPD. In an age-independent manner, COPD patients with PH had higher mortality rates than those without PH. Additional studies are necessary to identify other factors associated with the prevalence of PH in patients with COPD.
Data availability
The datasets generated during the current study are not publicly available due to the requirement for the application to NHIRD, Taiwan. For further information, please contact the corresponding author, Wei-Ting Chang (cmcvecho2@gmail.com).
References
Humbert, M. et al. 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur. Respir. J. 61. (2023).
Yogeswaran, A. et al. Relevance of Cor pulmonale in COPD with and without pulmonary hypertension: A retrospective cohort study. Front. Cardiovasc. Med. 9, 826369 (2022).
Sakao, S. Chronic obstructive pulmonary disease and the early stage of Cor pulmonale: A perspective in treatment with pulmonary arterial hypertension-approved drugs. Respir. Investig. 57, 325–329 (2019).
Sabit, R. et al. Sub-clinical left and right ventricular dysfunction in patients with COPD. Respir. Med. 104, 1171–1178 (2010).
VS, J. & SR, M. S J and P J. Echocardiographic findings in chronic obstructive pulmonary disease and correlation of right ventricular dysfunction with disease severity. Int. J. Adv. Med. ;4, (2017).
Kessler, R., Faller, M., Fourgaut, G., Mennecier, B. & Weitzenblum, E. Predictive factors of hospitalization for acute exacerbation in a series of 64 patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 159, 158–164 (1999).
Rubin, L. J. Cor pulmonale revisited. J. Am. Coll. Cardiol. 62, 1112–1113 (2013).
Shujaat, A., Bajwa, A. A. & Cury, J. D. Pulmonary hypertension secondary to COPD. Pulm Med. 2012, 203952 (2012).
Zangiabadi, A., De Pasquale, C. G. & Sajkov, D. Pulmonary hypertension and right heart dysfunction in chronic lung disease. Biomed. Res. Int. 2014, 739674 (2014).
Weir-McCall, J. R., Struthers, A. D., Lipworth, B. J. & Houston, J. G. The role of pulmonary arterial stiffness in COPD. Respir. Med. 109, 1381–1390 (2015).
Weitzenblum, E. et al. Prognostic value of pulmonary artery pressure in chronic obstructive pulmonary disease. Thorax 36, 752–758 (1981).
Naeije, R. & Torbicki, A. More on the noninvasive diagnosis of pulmonary hypertension: doppler echocardiography revisited. Eur. Respir. J. 8, 1445–1449 (1995).
Opitz, I. & Ulrich, S. Pulmonary hypertension in chronic obstructive pulmonary disease and emphysema patients: prevalence, therapeutic options and pulmonary circulatory effects of lung volume reduction surgery. J. Thorac. Dis. 10, S2763–S2774 (2018).
Cheng, C. L. et al. Validation of acute myocardial infarction cases in the National health insurance research database in Taiwan. J. Epidemiol. 24, 500–507 (2014).
Yang, Y. H. et al. Statin use and the risk of cirrhosis development in patients with hepatitis C virus infection. J. Hepatol. 63, 1111–1117 (2015).
Hsieh, C. Y. et al. Taiwan’s National health insurance research database: past and future. Clin. Epidemiol. 11, 349–358 (2019).
Ho, T. W. et al. Validity of ICD9-CM codes to diagnose chronic obstructive pulmonary disease from National health insurance claim data in Taiwan. Int. J. Chron. Obstruct. Pulmon. Dis. 13, 3055–3063 (2018).
Lindenauer, P. K. et al. Outcomes associated with invasive and noninvasive ventilation among patients hospitalized with exacerbations of chronic obstructive pulmonary disease. JAMA Intern. Med. 174, 1982–1993 (2014).
Yang, H. H. et al. Severe exacerbation and pneumonia in COPD patients treated with fixed combinations of inhaled corticosteroid and long-acting beta2 agonist. Int. J. Chron. Obstruct. Pulmon. Dis. 12, 2477–2485 (2017).
Lee, H. & Kim, S. Impact of the ICD-11 on the accuracy of clinical coding in Korea. Health Inf. Manag. 52, 221–228 (2023).
Chang, W. T. et al. Prognostic factors in patients with pulmonary hypertension—A nationwide cohort study. J. Am. Heart Assoc. 5. (2016).
Calverley, P. M. et al. Investigators T. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl. J. Med. 356, 775–789 (2007).
Tashkin, D. P. et al. A 4-year trial of Tiotropium in chronic obstructive pulmonary disease. N Engl. J. Med. 359, 1543–1554 (2008).
Glasheen, W. P. et al. Charlson comorbidity index: ICD-9 update and ICD-10 translation. Am. Health Drug Benefits 12, 188–197 (2019).
Budev, M. M., Arroliga, A. C., Wiedemann, H. P. & Matthay, R. A. Cor pulmonale: an overview. Semin Respir Crit. Care Med. 24, 233–244 (2003).
Celli, B. R., MacNee, W. & Force, A. E. T. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur. Respir. J. 23, 932–946 (2004).
Weitzenblum, E. Chronic Cor pulmonale. Heart 89, 225–230 (2003).
Thabut, G. et al. Pulmonary hemodynamics in advanced COPD candidates for lung volume reduction surgery or lung transplantation. Chest 127, 1531–1536 (2005).
Cuttica, M. J. et al. Categorization and impact of pulmonary hypertension in patients with advanced COPD. Respir. Med. 104, 1877–1882 (2010).
Andersen, K. H. et al. Prevalence, predictors, and survival in pulmonary hypertension related to end-stage chronic obstructive pulmonary disease. J. Heart Lung Transpl. 31, 373–380 (2012).
Seeger, W. et al. Pulmonary hypertension in chronic lung diseases. J. Am. Coll. Cardiol. 62, D109–D116 (2013).
Scharf, S. M. et al. And National emphysema treatment trial G. Hemodynamic characterization of patients with severe emphysema. Am. J. Respir. Crit. Care Med. 166, 314–322 (2002).
Wiedemann, H. P. & Matthay, R. A. Cor pulmonale in chronic obstructive pulmonary disease. Circulatory pathophysiology management. Clin. Chest Med. 11, 523–545 (1990).
Sayami, M., Baral, S., Shrestha, R. & Karki, D. B. Prevalence of chronic Cor pulmonale in chronic obstructive pulmonary disease patients in a teaching hospital in Nepal. J. Inst. Med. Nepal. 41, 15–19 (2019).
Shrestha, B., Dhungel, S. & Chokhani, R. Echocardiography based cardiac evaluation in the patients suffering from chronic obstructive pulmonary disease. Nepal. Med. Coll. J. 11, 14–18 (2009).
Liao, K. M., Chen, Y. C., Cheng, K. C., Wang, J. J. & Ho, C. H. Trends in intensive care unit admissions of COPD patients from 2003 to 2013 in Taiwan. Int. J. Chron. Obstruct. Pulmon. Dis. 13, 2007–2012 (2018).
Liu, W. et al. Trend of mortality and years of life lost due to chronic obstructive pulmonary disease in China and its provinces, 2005–2020. Int. J. Chron. Obstruct. Pulmon. Dis. 16, 2973–2981 (2021).
Mei, F. et al. La Vecchia C and Malvezzi M. Chronic obstructive pulmonary disease (COPD) mortality trends worldwide: an update to 2019. Respirology 27, 941–950 (2022).
Shujaat, A., Minkin, R. & Eden, E. Pulmonary hypertension and chronic Cor pulmonale in COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 2, 273–282 (2007).
Funding
This study was support by Chi-Mei Medical Center, Tainan, Taiwan. Wei-Ting Chang is granted by Ministry of Science and Technology (MOST 109-2326-B-384-001-MY3) and National Health Research Institute (NHRI-EX111-11138SI).
Author information
Authors and Affiliations
Contributions
W.T. Chang, the guarantor of this manuscript, W.T. Chang and T.C. Chang contributed to the conception and design of the study, C.H. Ho and Y.C. Chen analyzed and interpreted the data, T.C. Chang, W.T. Chang and C.T. Liao drafted the manuscript. All authors reviewed and revised this article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study has been reviewed and approved by the Institutional Review Board (IRB: 11101-013) in Chi-Mei Medical Center, Tainan, Taiwan. Inform consent was waived given that NHIRD is a retrospective database with de-identification.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chang, TC., Wang, CM., Ho, CH. et al. A prevalence study focusing on hospitalized COPD related pulmonary hypertension. Sci Rep 15, 12426 (2025). https://doi.org/10.1038/s41598-025-96629-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-96629-9