Abstract
Prostate cancer is a leading cause of morbidity and mortality worldwide, with incidence rates projected to double between 2020 and 2040. This growing health challenge highlights the need for improved diagnostic strategies and risk assessment tools to better understand disease etiology and progression. Among environmental factors, heavy metals have been implicated in inflammation and carcinogenesis, yet their specific role in prostate disease remains insufficiently explored. This novel study analyses the relationship between heavy metal concentrations in plasma and urine of patients with benign prostatic hyperplasia, precancerous lesions and prostate cancer. In addition to evaluating key clinical parameters, including age, total PSA levels, hemoglobin concentrations and monocyte/lymphocyte ratio, it aims to determine whether specific heavy metals contribute to the progression of prostate disease and whether they can serve as potential biomarkers for early diagnosis. Our findings reveal significant differences in vanadium and antimony concentrations in plasma, suggesting a potential role in prostate disease pathophysiology. Notably, lower plasma antimony concentrations are associated with an increased risk of PC, while plasma vanadium concentrations are significantly higher in the PL group. Regression analysis further supports the association between heavy metal concentrations and the risk of PL and PC, highlighting the potential of vanadium and copper as biomarkers or therapeutic targets for prostate health. The study also explores the impact of lead exposure on prostate cancer risk, revealing a significant association between urine lead concentration and PC. These findings underscore the complex interaction between heavy metal concentrations and prostate disease risk, emphasizing the need for further research to elucidate underlying mechanisms and explore therapeutic interventions.
Similar content being viewed by others
Introduction
Prostate cancer (PC) is the second most common cancer in men, with over a million cases diagnosed globally in 2018, representing 15% of all cancers1,2,3. The Lancet Commission has recently published projections indicating a significant increase in PC cases from 1.4 million in 2020 to 2.9 million by 2040, particularly in low and middle-income countries4. This increase cannot be prevented with lifestyle changes or public health interventions only, highlighting the need for alternative strategies5,6. The Commission also emphasizes the importance of improving early diagnosis and developing more effective treatments7,8,9.
The burden of PC is mainly attributed to several factors, including family history, hormones, ethnicity, aging, and inflammatory states10,11,12,13. Chronic inflammation plays a critical role in the development of PC. Exposure to heavy metals may favour chronic inflammation14,15. Heavy metals are not univocally defined, as their classification can be also based on their physical–chemical properties16. Broadly speaking, they include the d- and f-block transition elements, together with p-block metals and some non-metals like selenium and arsenic17. Their biological role can vary from essential to toxic. Essential trace elements, like iron, copper, cobalt, manganese, zinc and chromium, are crucial for enzyme activity, immune regulation, protection from oxidative damage, genomic stability, apoptosis, and cell signalling. Other metals such as cadmium18, mercury and lead are toxic19 (included in Group 1 substances carcinogenic to humans, or suspected to be). However, even essential metals can be toxic if present in high concentrations20. These elements can accumulate in the body through exposure to industrial, environmental, or food substances21. The accumulation of heavy metals can lead to oxidative damage, which has been associated with a range of diseases, including cancer22.
Besides inflammation and oxidative damage, epidemiological studies have shown that exposure to heavy metals can influence the endocrine system, which regulates growth, development, metabolism, and reproduction23,24,25. This can impact the progression of cancer, including PC. Literature reports a number of studies carried out to identify and quantify heavy elements in biological samples of cancer patients (blood, urine, hair, nail, biopsies, etc.) in order to clarify the relationship between the presence of these pollutants in the organism and the risk of developing the disease. We have recently examined these studies and reunited them in a review15 that shows how the results obtained are not always univocal, as the possibility of sound conclusions is limited by the heterogeneity of the data collected in terms of biological samples examined, methodologies, and cohorts of patients selected. Therefore, we decided to add further evidence to these findings by carrying out our own research on this topic.
Our review of the literature on prostate cancer and heavy metals revealed a limited number of articles, with biological samples varying from serum to tissue, hair and nails, blood and urine. In the latter case, the focus was on patients with abnormal PSA values but without a diagnosis of prostate cancer. Generally, only a few metals were examined in each study. In contrast, our research aimed to quantify the concentrations of fourteen heavy metals in blood and urine samples from individuals undergoing diagnostic assessments for prostate pathology. Specifically, we investigated the associations between these metal concentrations and various types of prostate disease, including benign prostatic hyperplasia (BPH), precancerous lesions (PL), and of course prostate cancer (PC). To the best of our knowledge, this is the first study of this kind. Our research, conducted with patients from the Urology Clinic at the University Hospital of Sassari (Italy), aims to provide critical insights into the potential role of heavy metal exposure in the aetiology and progression of prostate disorders, thereby advancing our understanding of its implications for prostate health and disease management.
Materials and methods
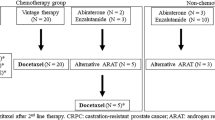
Male subjects with prostate cancer, precancerous lesions, or benign prostatic hypertrophy were recruited from the Urology Department of the University Hospital of Sassari. A total of 93 cases (PC and PL) and 78 controls (BPH) were initially recruited, meeting the calculated sample size required for sufficient statistical power.
The power calculation was based on an expected mean difference (ΔΔ) of 5 μg/L (difference in metal levels between cases and controls) and a standard deviation (σσ) of 10 μg/L, as derived from preliminary data and literature. Using these parameters, the study achieved > 80% power to detect a medium effect size (Cohen’s d = 0.5) at a significance level of α = 0.05/3, adjusted for Bonferroni correction for the three tested metals.
However, due to incomplete data or missing measurements for some metals, the final analysis included data from 61 controls (BPH). Despite this limitation, the available data ensured sufficient power (> 75%) to detect the expected effect size, supporting the validity of this exploratory biomarker study.
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Independent Ethics Committee of the University Hospital of Cagliari (P.O. San Giovanni di Dio: via Ospedale 54, 09124 Cagliari) under Approval Code Prot. PG/2022/4985, dated March 30, 2022. Written informed consent was obtained from all participants prior to their inclusion in the study.
Patient selection and study criteria
This study was conducted at the Urology Clinic of the University Hospital of Sassari between September 2021 and December 2022. Participants were enrolled if they were referred for initial diagnostic evaluation. All patients underwent ultrasound-guided prostate biopsy, and classification into benign prostatic hyperplasia, precancerous lesions, or prostate cancer groups was determined based on histopathological assessment.
Patients were eligible for inclusion if they met at least one of the following criteria: abnormal Digital Rectal Examination (DRE) findings suggestive of prostate pathology or age-related elevated prostate-specific antigen (PSA) levels, in accordance with established clinical guidelines. To minimise confounding factors and ensure the accuracy of heavy metal concentration assessments, individuals with a prior diagnosis of any malignancy, including prostate cancer, were excluded, as systemic cancer can influence metal metabolism and immune responses. Renal and hepatic function are critical in the clearance and metabolism of heavy metals; therefore, participants with significant renal or hepatic dysfunction were excluded from the study. Specifically, individuals with stage III–V chronic kidney disease (CKD), liver failure, or a history of cirrhosis were deemed ineligible. Additionally, acute or chronic inflammatory conditions, including urinary tract infections (UTIs), prostatitis, or systemic infections, were exclusion criteria due to their potential impact on inflammatory markers and heavy metal homeostasis. In order to collect comprehensive patient data, each participant completed a questionnaire that covered demographic characteristics, medical history, family history of cancer, prior prostate cancer screenings, urological health status, and lifestyle factors such as smoking history and physical activity levels.
Heavy metals serum analysis using ICP-MS
Total metals and metalloids in plasma (aluminium, antimony, arsenic, barium, beryllium, cadmium, chromium, cobalt, copper, iron, lead, lithium, manganese, mercury, nickel, molybdenum, selenium, silver, thallium, tin, vanadium and zinc) and urine (antimony, arsenic, barium, cadmium, cobalt, copper, iron, lead, manganese, mercury, molybdenum, selenium, vanadium and zinc) were determined by inductively coupled plasma mass spectrometry (ICP-MS) in accordance with the US EPA 6020B method26. Biological fluids were analysed directly after dilution of 0.5 mL of sample in 5 mL with 2% nitric acid (J.T. Baker, Phillipsburg, NJ, USA) solution. The analysis was performed with an inductively coupled plasma mass spectrometer ICP-MS/MS (Agilent 8800 QQQ, Santa Clara, CA, USA) equipped with a collision cell and two quadrupole mass analyzers. In comparison to a single quadrupole ICP-MS system, the triple quadrupole system significantly increases the accuracy of mass separation. To compensate for the matrix effect and signal drift, a solution of internal standards was used. The calibration curve was verified at the start of each analytical batch using the initial calibration verification (ICV) with a different lot standard, while the instrumental sensitivity was verified using the continuous calibration verification (CCV) at or near midrange. The LOQs testing was 0.001 ng/mL for all elements analysed. The quality control of the data was verified and controlled using Certified Reference Materials ClinChek® Urine Control, and ClinChek® Plasma Control for Trace Elements, (RECIPE Chemicals, München). Laboratory was intercalibrated through successful participation in internationally organized proficiency tests (OELM). The method is accredited according to UNI EN ISO 17025/201727,28.
Statistical analysis
Differences in subject characteristics, including age, ethnicity, education, marital status, family cancer history, were compared between PC cases and BPH or PL using the chi-squared test. To ensure that there was no selection bias when samples for the assay were chosen, the chi-squared test was used to compare background characteristics of the corresponding subjects between groups. The Shapiro–Will test of normality was used to test the statistical distribution of each variable. Data are presented as mean and standard deviation (SD) or median and interquartile range (IQR), and T or U test were used accordingly to test for the presence of any difference between two parametric or non-parametric distributions. The Kruskall–Wallis test was used to assess differences of more than two non-parametric distributed variables. Probit regression models to estimate odds ratio (OR) with 95% confidence intervals (CI) for univariate linear regression analysis of each heavy metal concentration in plasma and urine, and its association with pre-cancerous lesion or prostate cancer. The models were also adjusted in bivariate linear regression analyses for age, total PSA, and the following haematological parameters: WBC, RBC, HBG, neutrophils, lymphocytes, monocytes, and LUC). Statistical analyses were performed using Stata 14 (STATA Corp., College Station, TX, USA). The R heatmap package was used to create the heatmaps.
The inclusion of haematological parameters (WBC, RBC, HBG, neutrophils, lymphocytes, monocytes, and LUC) as confounders in the regression models was driven by their established relevance in the pathophysiology of prostate diseases. Chronic inflammation plays a central role in prostate carcinogenesis, and WBC levels, as a marker of systemic inflammation, can influence tumour progression and the tumour microenvironment. Similarly, RBC and HBG are indicative of anaemia or disruptions in erythropoiesis, which are frequently observed in cancer patients and can affect the systemic transport and bioavailability of heavy metals. Parameters such as neutrophils and lymphocytes, key components of the immune response, are closely tied to the inflammatory milieu and immune modulation in cancer. By adjusting for these variables, the analysis aimed to reduce confounding effects and isolate the specific associations between heavy metal concentrations and prostate pathology. These adjustments improve the robustness of the findings by accounting for potential interactions between systemic inflammation, haematological status, and metal bioaccumulation.
Results
Subject characteristics
From September 2021 to December 2022, a total of 154 participants, all from Sardinia (Italy), were enrolled. The cohort included 61 subjects with BPH, 15 with PL, and 78 with confirmed PC. Age and total PSA, according to the guidelines29, were significantly different across the three groups, with PC patients being older (BPH median age = 68; PL = 69; PC = 74; p = 0.002) and having higher total PSA concentrations than the other two groups (BPH median total PSA = 5.9 ng/mL; PL = 4.4 ng/mL; PC = 7.5 ng/mL; p = 0.0002). Hemoglobin concentrations were also significantly lower in PL and PC patients (BPH median RBC = 15 g/dL; PL = 14 g/dL; PC = 14 g/dL; p = 0.019), while other CBC parameters did not differ across the study groups. Among the CBC inflammatory indices, only the monocytes-to-lymphocytes ratio (MLR) was increased in PL and PC patients (BPH mean MLR = 0.22; PL mean MLR = 0.3; PC mean MLR = 0.25; Table 1).
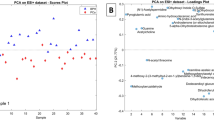
Statistically significant differences were observed in plasma concentrations of manganese and antimony across the three groups (p = 0.049 and 0.034, respectively), while no between-group differences were observed in urinary concentrations of any heavy metal. These findings were also illustrated in heat maps depicting heavy metal concentrations in plasma and urine (Table 2, Figs. 1 and 2).
Heatmap of plasmatic heavy metal concentrations. Each row represents an individual subject (grouped as BPH, PL, and PC, and annotated in green, yellow, and red, respectively) and heavy metal concentration values are scaled from − 10 to 10 (blue to red). The data matrix uses a range of colors to represent values, with darker or more intense colors indicating higher values and lighter or less intense colors indicating lower values.
Heatmap of urinary heavy metal concentrations. Each row represents an individual subject (grouped as BPH, PL, and PC, and annotated in green, yellow, and red, respectively) and heavy metal concentration values are scaled from − 10 to 10 (blue to red). The data matrix uses a range of colors to represent values, with darker or more intense colors indicating higher values and lighter or less intense colors indicating lower values.
Additionally, urinary iron, copper, zinc, selenium, arsenic, molybdenum, cadmium, and antimony concentrations were significantly lower than plasma concentrations in all three groups. By contrast, barium urinary concentrations were significantly lower than plasmatic ones only in the BPH group, as reflected in Table 2. No significant differences were observed for manganese concentrations between plasma and urine across the groups (Table 2).
Adjusted probit regression analysis of metal concentrations in plasma and urine and their associations with prostate pathologies
Probit regression analyses were conducted to evaluate the odds ratio (OR) and 95% confidence interval (CI) for the association between plasma or urinary concentrations of individual heavy metals and the presence of precancerous lesions or prostate cancer, with the benign prostatic hyperplasia group serving as a control (Tables 3 and 4).
Elevated plasma vanadium concentrations were significantly associated with PL (OR 11.67; 95% CI 0.72–22.63; p = 0.04), with a non-significant trend for a similar association in PC patients (OR 7.92; 95% CI − 1.04 to 16.87; p = 0.08). In contrast, lower plasma antimony concentrations were significantly associated with PC (OR − 0.25; 95% CI − 0.43 to − 0.08; p < 0.001). No significant associations were observed between urinary heavy metal concentrations and PL, but there was a trend for an association between urinary copper and PC (OR 0.03; 95% CI 0.00–0.07; p = 0.06) and a significant association for urinary lead and PC (OR 0.28; 95% CI 0.02–0.54; p = 0.03).
Significant or trend-level associations observed in single-metal regression models were further evaluated in bivariate probit regression analyses adjusted for potential confounders, including age, total PSA, and CBC parameters.
Plasma vanadium and PL
After adjustment, elevated plasma vanadium concentrations remained significantly associated with PL when corrected for RBC (OR 13.10; 95% CI 1.39–24.81; p = 0.03), HGB (OR 11.93; 95% CI 0.69–23.17; p = 0.04), lymphocytes (OR 11.87; 95% CI 0.58–23.16; p = 0.04), and age (OR 12.35; 95% CI 0.99–23.70; p = 0.03; Table S1). No significant associations were observed after adjustments for systemic inflammatory indices such as MLR or SIRI (p > 0.10). These results suggest a robust relationship between plasma vanadium and PL.
Plasma vanadium and PC
In contrast, no significant associations were observed between plasma vanadium and PC after adjustment for confounders (Table S2). Adjustment for age (OR 5.40; 95% CI − 3.85 to 14.65; p = 0.25), PSA (OR 6.96; 95% CI − 3.27 to 17.19; p = 0.18), and hematological parameters such as RBC (OR 7.75; 95% CI − 2.05 to 17.54; p = 0.12) did not yield significant results.
Plasma antimony and PC
Plasma antimony concentrations were consistently and significantly associated with PC across all adjusted models (Table S3). The association remained significant after adjustment for age (OR − 0.28; 95% CI − 0.46 to − 0.09; p < 0.001), PSA (OR − 0.26; 95% CI − 0.45 to − 0.06; p = 0.01), and combined age and PSA (OR − 0.26; 95% CI − 0.47 to − 0.06; p = 0.01). The association persisted after adjustments for inflammatory markers such as MLR (OR − 0.22; 95% CI − 0.40 to − 0.04; p = 0.02) and SIRI (OR − 0.24; 95% CI − 0.42 to − 0.06; p = 0.01).
Urinary copper and PC
Urinary copper concentrations showed weak trends toward significance across all adjusted models (Table S4). Adjustments for age (OR 0.04; 95% CI 0.00–0.08; p = 0.07), PSA (OR 0.03; 95% CI − 0.01 to 0.07; p = 0.11), and combined age and PSA (OR 0.03; 95% CI − 0.01 to 0.07; p = 0.17) did not yield significant associations.
Urinary lead and PC
Urinary lead concentrations remained significantly associated with PC after adjustment for demographic factors (Table S4). Adjustment for age yielded an OR of 0.31 (95% CI 0.04–0.57; p = 0.03), while PSA adjustment resulted in an OR of 0.31 (95% CI 0.03–0.58; p = 0.03). Combined adjustment for age and PSA strengthened the association (OR 0.33; 95% CI 0.04–0.61; p = 0.02). Borderline significance was observed for adjustments involving hematological parameters and inflammatory indices, with p values ranging from 0.06 to 0.08.
Comparative analysis of metal concentrations in prostate disorders: insights into biomarkers and disease progression
The statistical analysis of metal concentrations in benign prostatic hyperplasia, precancerous lesions, and prostate cancer groups was conducted using the Mann–Whitney U test, a non-parametric method appropriate for comparing independent groups where data may not follow a normal distribution. The test allowed pairwise comparisons between BPH vs. PL, BPH vs. PC, and PL vs. PC, identifying statistically significant differences in metal concentrations across the groups. The box plots illustrate the distribution of these metal concentrations in serum, Fig. 3, with medians, interquartile ranges (IQR), and whiskers representing the full range of data. A gray zone indicating the mean ± standard deviation (SD) for each group further facilitated comparison across the clinical conditions. The results revealed that plasma manganese concentrations showed a marginally significant difference (p = 0.049) in the PC group compared to BPH and PL, suggesting a potential, but inconclusive role in prostate cancer progression. No significant differences were observed in urinary manganese concentrations (p = 0.919). In contrast, antimony levels were significantly lower in the PC group, aligning with previous findings that associate reduced antimony concentrations with prostate cancer risk. Elevated vanadium levels in the PL group indicate its potential role in precancerous processes, possibly serving as a diagnostic biomarker for early disease stages. For urine samples, manganese concentrations were consistent across groups, while vanadium and copper concentrations were elevated in the PL group. Furthermore, lead concentrations were significantly higher in the PC group, suggesting a link between lead exposure and prostate cancer risk. Importantly, the reference values used for comparison were taken from Tables 11 and 12 of the ISTISAN Report 17/3330, which provides diagnostic reference levels for heavy metals in biological samples. These diagnostic reference levels offer a benchmark for evaluating the observed metal concentrations within the context of prostate health and disease. The results underscore the potential of metals such as vanadium and lead as biomarkers for prostate disease progression and highlight the value of using established diagnostic reference levels in interpreting clinical biochemistry data, Fig. 4.
Discussion
The role of environmental factors, including heavy metal exposure, in the genesis and progression of prostate disease has been widely debated31. Systematic reviews and meta-analyses have indicated that elevated levels of heavy metals in biological samples, such as cadmium, arsenic and lead, are associated with an increased risk of PC, although the underlying mechanisms remain poorly understood32. Our findings align with this evidence, demonstrating that specific heavy metals may influence prostate disease progression. In particular, we observed significantly lower plasma levels of antimony in PC patients and elevated vanadium levels in those with precancerous lesions, suggesting a potential role in early disease development. Furthermore, urinary lead concentrations were significantly associated with PC. These results are consistent with previous studies indicating that certain metals may influence carcinogenesis through oxidative stress, immune dysregulation, and epigenetic modifications33,34,35,36. Additionally, we observed an increase in the monocyte-to-lymphocyte ratio (MLR) in PL and PC patients, reinforcing the link between chronic inflammation and prostate disease progression37.
Overall, the results of our study provide valuable insights into the relationship between heavy metal concentrations in plasma and urine and key components of the clinical continuum linking benign states with precancerous and cancerous prostate pathologies. This continuum was further supported by the observed differences in median age and total PSA concentrations across the three groups. Additionally, the reduction in haemoglobin concentrations and the increase in the monocyte-to-lymphocyte ratio (MLR) in PL and PC patients can be interpreted as indicators of potential immunological alterations in these groups, as well as anaemia associated with preneoplastic or neoplastic states. The MLR is a measure of the balance between the body’s innate immune response (monocytes) and adaptive immune response (lymphocytes). An increased MLR may indicate, in the context of cancer, a shift from adaptive immunity (which relies on specific immune responses to pathogens) to innate immunity (which provides rapid and nonspecific defence against pathogens)38. Additionally, a high MLR may also reflect an ongoing inflammatory response, which is common in cancer and precancerous conditions39. While these changes provide insights into the body’s defense mechanisms, they also highlight the complexity of the immune response in cancer patients.
The evaluation of heavy metal concentrations revealed significant differences for antimony, with lower plasma levels associated with PC, while manganese showed marginally significant differences in plasma across groups, suggesting potential roles of these metals in the pathophysiology of prostate diseases.
According to the International Agency for Research on Cancer (IARC), antimony trioxide (Sb2O3) has been classified as a possible carcinogenic to humans (Group 2B), while antimony trisulfide (Sb2S3) has not been classified with respect to its carcinogenicity (Group 3)40. There are indications of neoplastic or preneoplastic effects of antimony species in animal models across various tissues and organs. Two new studies suggested that antimony acts as an endocrine disruptor through interactions with oestrogen and androgen receptors, potentially promoting tumour growth in the reproductive system, although its relevance for in vivo carcinogenesis in rodents and humans remains unclear41,42. Moreover, recent research demonstrated that low-dose antimony exposure enhances the proliferation and invasion of prostate cancer cells by inhibiting ferroptosis via the Nrf2-SLC7A11-GPX4 pathway43. This suggests that antimony may actively contribute to prostate carcinogenesis. Our finding of lower plasma antimony levels in PC patients may not indicate a protective role but rather reflect altered metal homeostasis in cancer progression. Further research is needed to confirm the mechanistic role of antimony in prostate carcinogenesis and its potential implications as a biomarker of disease progression.
The observed marginal significance for plasma manganese levels in PC aligns with its known roles in cellular metabolism and oxidative stress. However, further studies are needed to confirm its association with prostate cancer risk and its potential as a biomarker. The absence of significant differences in urinary heavy metal concentrations across the groups suggests that the potential impact of heavy metals on prostate health and disease states is more closely related to systemic exposure rather than renal excretion patterns44.
Regression analysis provided additional evidence for the association between heavy metal concentrations and the presence of PL and PC. Plasma vanadium concentrations were significantly higher in the PL group, with a similar but non-significant trend observed in PC patients. This finding suggests that vanadium may play a role in the early stages of prostate neoplasia. In the literature, the pro-tumor effect of vanadium refers to the potential adverse effects of vanadium exposure on tumor progression and/or the promotion of cancerous conditions45,46.
Although vanadium has been studied for its anti-tumor properties, the lack of a significant association with PC in this study indicates that its role might be more relevant in precancerous states47. The analysis also revealed a trend toward a significant association between urinary copper concentration and PC. Variations in copper concentrations or copper/zinc ratios (Cu/Zn) are associated with several tumors, including those of the bladder, breast, colon-rectum, and prostate48. However, in this study, copper showed only weak trends toward significance, suggesting its limited utility as a biomarker in the current cohort.
Another interesting finding concerns the significant association between urinary lead concentration and PC. Previous studies have suggested a potential link between environmental lead exposure and the risk of developing prostate diseases49. Higher blood lead concentrations have been reported in PC cases, suggesting that environmental lead exposure may influence prostate pathology risk. The consistent association of urinary lead with PC, even after adjustment for confounders, highlights its potential as a robust biomarker for prostate cancer risk50,51.
Adjusting for potential confounding factors such as age, total PSA, and complete blood count (CBC) did not alter the significant association between higher plasma vanadium concentrations and PL, reinforcing the possible role of vanadium in prostate health. However, the trend toward an association between copper concentration and PC did not persist after adjustment, suggesting that its role might be secondary or confounded by other variables52.
Globally, these results underscore the importance of exploring plasma antimony and vanadium as potential biomarkers for prostate pathologies, while highlighting the need for further research to confirm the roles of manganese, copper, and lead in prostate cancer progression53,54.
Comparison with literature and the role of heavy metals in prostate pathophysiology
A necessary remark should be dedicated to the comparison of our results to those present in the literature for the same type of cancer15,32. In the previous studies examined, the heterogeneity in the type of biological samples used for the determination of metal concentrations (serum, tissue, hair and nails, blood and urine) and patients enrolled, unfortunately, does not allow us any sound comparison and conclusion. We can only report that in general the metals showing altered concentrations in the case of PC are mainly zinc, selenium, arsenic, cadmium, iron, lead, and to a lesser extent copper, manganese, mercury and antimony. Especially zinc seems to have a protective role against development of PC, as confirmed in different studies where PC patients show low levels of this essential metal. In ours, zinc does not correlate to any prostate pathology. Instead, we have found strong evidence that vanadium is, while the involvement of this element was never reported before. This indicates that further studies are needed to clarify such correlations, together with the need of a common and shared methodology for a better comparison of the results.
The findings of our study highlight the complementary role of heavy metals as plasma and urinary biomarkers in the assessment of prostate health55. Plasma and urine are the most commonly analyzed biofluids for determining metal concentrations56, but their interpretative value differs based on factors such as metabolism, bioavailability, and excretion pathways57. In particular, plasma concentrations provide insight into ongoing pathophysiological mechanisms, while urinary levels reflect long-term exposure and the balance between accumulation and elimination58.
As for the possible mechanisms through which heavy metals can affect the prostate health, we should point out that the contribution of these elements to the pathogenesis of prostate diseases can occur through multiple biological pathways, including oxidative stress, immune dysregulation, endocrine dysfunction, and epigenetic modifications59. It is well established that metals such as lead, cadmium, and vanadium are involved in the generation of reactive oxygen species (ROS), which can induce oxidative stress and DNA damage32,60. This is closely linked to cancer development, including PC, as it promotes genomic instability, mutations, and uncontrolled cell proliferation61. In particular, vanadium has been shown to interfere with cellular redox homeostasis, leading to increased oxidative stress, which may contribute to early-stage neoplastic transformation62. Moreover, chronic inflammation is a recognized hallmark of prostate carcinogenesis. Heavy metals can disrupt immune homeostasis by modulating the production of pro-inflammatory cytokines and altering immune cell function63. Our study found an increase in the monocyte-to-lymphocyte ratio in patients with PL and PC, supporting the hypothesis that heavy metals may influence prostate disease progression through immune dysregulation63. Lead exposure has been associated with increased inflammatory markers, contributing to the establishment of an inflammatory microenvironment that promotes tumour growth64,65. Certain heavy metals, including antimony and cadmium, interfere with androgen and oestrogen receptor signalling66. The prostate is highly dependent on androgen regulation, and disruptions in these pathways can alter cellular proliferation and differentiation67. Antimony compounds have also been found to interact with sex hormone receptors, potentially affecting prostate tissue homeostasis and increasing susceptibility to cancerous transformation40. Scientific evidence suggests that heavy metals may influence gene expression through DNA methylation, histone modifications, and microRNA regulation. These alterations can lead to the activation of oncogenes or the silencing of tumour suppressor genes. Additionally, the accumulation of heavy metals in plasma and urine suggests that they may be differentially eliminated or stored, generating systemic effects rather than being efficiently excreted. The association between urinary lead concentration and PC highlights the potential role of long-term environmental exposure in prostate pathology68. Lead bioaccumulation may affect cellular metabolism, mitochondrial function, and apoptosis regulation, ultimately contributing to prostate disease progression69. Our findings, along with existing literature, confirm the role of heavy metals in carcinogenesis through a combination of oxidative stress, inflammation, endocrine disruption, and epigenetic changes. It is evident that further mechanistic studies are necessary to elucidate the precise molecular pathways involved and to inform the management of prostate disease.
Advantages and limitations of the study
This study presents several strengths and limitations that should be considered when interpreting the findings. One of the key strengths lies in the comprehensive assessment of heavy metal concentrations in both plasma and urine, allowing for a dual perspective on systemic exposure and potential long-term accumulation70. The range of heavy metals analyzed is broader than in previous studies, providing a more detailed overview of their potential role in prostate disease71. Moreover, patient classification into benign prostatic hyperplasia, precancerous lesions, and prostate cancer was based on histopathological confirmation, ensuring the reliability of disease differentiation72. Another strength of the study is its exploration of the relationship between heavy metal exposure and inflammatory markers, particularly the monocyte-to-lymphocyte ratio, which offers insights into the mechanisms underlying prostate disease progression73. Additionally, the inclusion of only native Sardinian participants minimized genetic variability, strengthening the internal validity of the findings. However, certain limitations must be acknowledged. The cross-sectional design prevents establishing causality between heavy metal exposure and prostate disease risk, limiting the ability to infer temporal relationships74. Additionally, while the overall sample size was adequate, the small number of patients with precancerous lesions may have reduced the statistical power for detecting significant associations in this subgroup. The use of Probit regression helped stabilize estimates, but future studies with larger cohorts would enhance reliability75,76. Although individuals with documented occupational exposure to heavy metals were excluded to minimize confounding, detailed dietary data were not collected, potentially affecting the accuracy of exposure assessment77. Given that dietary intake is a major source of metal exposure, future studies should incorporate nutritional profiling to better account for dietary contributions78. Similarly, renal function variability among participants may have influenced urinary metal concentrations, introducing a confounding factor in exposure assessment79. Another notable limitation is the lack of direct measurements of heavy metal accumulation in prostate tissue, which would provide more precise insights into localized effects. While plasma concentrations reflect recent systemic exposure and ongoing metabolic interactions, they may not fully capture the bioaccumulation of metals in prostate tissue. Certain metals, such as vanadium and antimony, demonstrated significant plasma-level variations depending on prostate condition, suggesting a possible role in early-stage disease detection80. Conversely, urinary excretion serves as a marker of long-term exposure. The correlation between urinary lead concentration and PC highlights urine analysis as a potential non-invasive tool for assessing chronic environmental exposure81. This advantage makes urine biomarkers particularly useful in large-scale epidemiological studies, facilitating risk assessment and early screening strategies. However, urine analysis also has limitations, including high variability in individual renal function, which complicates data interpretation, particularly in elderly patients or those with suboptimal hydration82. Additionally, not all metals are efficiently excreted in urine. Cadmium and lead, for example, tend to accumulate in bones and soft tissues, which may reduce the correlation between urinary levels and total body burden83. Another constraint is the short half-life of certain metals, such as arsenic and mercury, limiting their reliability in evaluating chronic exposure and its association with disease risk. To overcome these limitations, future studies should adopt an integrated approach using multiple biological matrices, including plasma, urine, prostate tissue, and hair, to provide a more comprehensive understanding of the role of heavy metals in prostate disease pathogenesis. This strategy would allow for a more accurate assessment of exposure, metabolism, and biological effects, ultimately improving the identification of biomarkers for disease detection and progression monitoring.
Conclusions
This study provides compelling evidence of the complex interaction between heavy metal concentrations and the risk of developing prostate diseases. The significant associations between plasma vanadium concentrations and the risk of PL and PC, as well as the inverse association of antimony with PC, highlight the need for further research to clarify the underlying mechanisms and explore the potential of heavy metals as biomarkers or therapeutic targets for prostate health. The results also emphasize the importance of considering systemic exposure to heavy metals in the context of prevention and management strategies for prostate diseases.
Data availability
The datasets generated and analyzed during this study are available from the corresponding author upon reasonable request. Researchers seeking access may be required to provide a brief proposal outlining the intended use and agree to confiden-tiality terms as per institutional policies.
References
Rawla, P. Epidemiology of prostate cancer. World J. Oncol. 10, 63 (2019).
Kensler, K. H. & Rebbeck, T. R. Cancer progress and priorities: Prostate cancer. Cancer Epidemiol. Biomark. Prev. 29, 267–277 (2020).
Bray, F. et al. Global cancer statistics 2022: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 74, 229–263 (2021).
James, N. D. et al. The lancet commission on prostate cancer: Planning for the surge in cases. Lancet 403, 1683–1722 (2024).
Tesfai, A., Norori, N., Harding, T. A., Wong, Y. H. & Hobbs, M. D. Variation in harms and benefits of prostate-specific antigen screening for prostate cancer by socio-clinical risk factors: A rapid review. BJUI Compass 5, 531–546 (2024).
Coradduzza, D. et al. A preliminary study procedure for detection of polyamines in plasma samples as a potential diagnostic tool in prostate cancer. J. Chromatogr. B 1162, 122468 (2021).
Horgan, D., Van den Bulcke, M., Malapelle, U., Normanno, N., Capoluongo, E. D., Prelaj, A., Rizzari, C., Stathopoulou, A., Singh, J. & Kozaric, M. Aligning Cancer Research Priorities in Europe with Recommendations for Conquering Cancer: A Comprehensive Analysis. Presented at Healthcare. MDPI, 12, 259 (2024).
Farabi, H. et al. A cost-benefit analysis of mass prostate cancer screening. Cost Eff. Resour. Alloc. 22, 37 (2024).
Coradduzza, D. et al. Plasma polyamine biomarker panels: Agmatine in support of prostate cancer diagnosis. Biomolecules 12, 514 (2022).
Berenguer, C. V., Pereira, F., Câmara, J. S. & Pereira, J. A. Underlying features of prostate cancer—Statistics, risk factors, and emerging methods for its diagnosis. Curr. Oncol. 30, 2300–2321 (2023).
Coradduzza, D. et al. Role of nano-mirnas in diagnostics and therapeutics. Int. J. Mol. Sci. 23, 6836 (2022).
Wigle, D. T., Turner, M. C., Gomes, J. & Parent, M.-E. Role of hormonal and other factors in human prostate cancer. J. Toxicol. Environ. Health Part B 11, 242–259 (2008).
Guo, J. et al. Aging and aging-related diseases: From molecular mechanisms to interventions and treatments. Signal Transduct. Target. Ther. 7, 391 (2022).
Budi, H. S. et al. Source, toxicity and carcinogenic health risk assessment of heavy metals. Rev. Environ. Health 39, 77–90 (2024).
Coradduzza, D. et al. Heavy metals in biological samples of cancer patients: A systematic literature review. Biometals 37, 1–15 (2024).
Tchounwou, P. B., Yedjou, C. G., Patlolla, A. K. & Sutton, D. J. Heavy metal toxicity and the environment. Mol. Clin. Environ. Toxicol. 3, 133–164 (2012).
Jones, C. J. & Thornback, J. R. Medicinal Applications of Coordination Chemistry (Royal Society of Chemistry, 2007).
Peana, M. et al. Biological effects of human exposure to environmental cadmium. Biomolecules 13, 36 (2022).
Peana, M. et al. Metal toxicity and speciation: A review. Curr. Med. Chem. 28, 7190–7208 (2021).
Coradduzza, D. et al. Ferroptosis and senescence: A systematic review. Int. J. Mol. Sci. 24, 3658 (2023).
Mishra, P., Poddar, A. & Sahu, B. Assessment of Heavy Metal Toxicity in Humans.
Xu, J. et al. Dual roles of oxidative stress in metal carcinogenesis. J. Environ. Pathol. Toxicol. Oncol. 36, 345–376 (2017).
Liu, D., Shi, Q., Liu, C., Sun, Q. & Zeng, X. Effects of endocrine-disrupting heavy metals on human health. Toxics 11, 322 (2023).
Apostoli, P. & Catalani, S. Effects of metallic elements on reproduction and development. In Handbook on the Toxicology of Metals, 399–423 (Elsevier, 2015).
Pan, J., Liu, P., Yu, X., Zhang, Z. & Liu, J. The adverse role of endocrine disrupting chemicals in the reproductive system. Front. Endocrinol. 14, 1324993 (2024).
EPA, U. Method 6020b (sw-846): Inductively Coupled Plasma-Mass Spectrometry. Washington, DC: 2015-12 (2014).
Piras, P. et al. A representative sampling of tuna muscle for mercury control. Ital. J. Food Saf. 9, 9055 (2020).
Anastasopoulos, G. The new ISO/IEC 17025: 2017. CAL LAB Int. J. Metrol. 30–35 (2017).
Tikkinen, K. A. et al. Prostate cancer screening with prostate-specific antigen (PSA) test: A clinical practice guideline. BMJ 362, k3581 (2018).
Padovani, R. et al. Livelli diagnostici di riferimento nazionali per la radiologia diagnostica e interventistica. Ist. Super. Sanità Roma Rapporti ISTISAN 17, 33 (2017).
Bray, F. et al. Global cancer statistics 2022: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 74, 229–263 (2024).
Devi, V. et al. Serum levels of heavy metals in patients with prostate cancer: A systematic review and meta-analysis. Biol. Trace Elem. Res. https://doi.org/10.1007/s12011-024-04510-z (2025).
Stepanyan, A. et al. Correction: Long-term environmental metal exposure is associated with hypomethylation of CpG sites in NFKB1 and other genes related to oncogenesis. Clin. Epigenet. 15, 143 (2023).
Nail, A. N. et al. Arsenic and human health: New molecular mechanisms for arsenic-induced cancers. Curr. Pollut. Rep. 9, 784–797 (2023).
Beega, F. G. et al. Epigenetic mechanisms of metal carcinogenicity: Exploring associated therapeutic options for individualised treatments. Int. Res. J. Oncol. 7, 153–169 (2024).
Zhao, L., Islam, R., Wang, Y., Zhang, X. & Liu, L.-Z. Epigenetic regulation in chromium-, nickel-and cadmium-induced carcinogenesis. Cancers 14, 5768 (2022).
Xiang, Q., Liu, Y., Xiao, J., Ou, L. & Du, J. Prognostic value of lymphocyte-to-monocyte ratio (LMR) in patients with prostate cancer: A systematic review and meta-analysis. Am. J. Mens Health 18, 15579883241234748 (2024).
Zhu, Z.-F. et al. Predictive role of the monocyte-to-lymphocyte ratio in advanced hepatocellular carcinoma patients receiving anti-PD-1 therapy. Transl. Cancer Res. 11, 160 (2022).
Chen, X., Li, Y., Xia, H. & Chen, Y. H. Monocytes in tumorigenesis and tumor immunotherapy. Cells 12, 1673 (2023).
Saerens, A., Ghosh, M., Verdonck, J. & Godderis, L. Risk of cancer for workers exposed to antimony compounds: A systematic review. Int. J. Environ. Res. Public Health 16, 4474 (2019).
Guarnotta, V., Amodei, R., Frasca, F., Aversa, A. & Giordano, C. Impact of chemical endocrine disruptors and hormone modulators on the endocrine system. Int. J. Mol. Sci. 23, 5710 (2022).
Lacouture, A., Lafront, C., Peillex, C., Pelletier, M. & Audet-Walsh, É. Impacts of endocrine-disrupting chemicals on prostate function and cancer. Environ. Res. 204, 112085 (2022).
Shi, J. et al. Low-dose antimony exposure promotes prostate cancer proliferation by inhibiting ferroptosis via activation of the Nrf2-SLC7A11-GPX4 pathway. Chemosphere 339, 139716 (2023).
Kwon, J.-Y. et al. Association between levels of exposure to heavy metals and renal function indicators of residents in environmentally vulnerable areas. Sci. Rep. 13, 2856 (2023).
Ferretti, V. A. & León, I. E. An overview of vanadium and cell signaling in potential cancer treatments. Inorganics 10, 47 (2022).
Fortoul, T. et al. Overview of environmental and occupational vanadium exposure and associated health outcomes: An article based on a presentation at the 8th international symposium on vanadium chemistry, biological chemistry, and toxicology, washington dc, august 15–18, 2012. J. Immunotoxicol. 11, 13–18 (2014).
Irving, E. & Stoker, A. W. Vanadium compounds as PTP inhibitors. Molecules 22, 2269 (2017).
Mukherjee, B. et al. Vanadium—An element of atypical biological significance. Toxicol. Lett. 150, 135–143 (2004).
Guo, C.-H., Chen, P.-C., Yeh, M.-S., Hsiung, D.-Y. & Wang, C.-L. Cu/Zn ratios are associated with nutritional status, oxidative stress, inflammation, and immune abnormalities in patients on peritoneal dialysis. Clin. Biochem. 44, 275–280 (2011).
Tang, X. et al. Copper in cancer: From limiting nutrient to therapeutic target. Front. Oncol. 13, 1209156 (2023).
Wang, Y. et al. Cuproptosis: A novel therapeutic target for overcoming cancer drug resistance. Drug Resist. Updates 72, 101018 (2023).
Karunasinghe, N. Zinc in prostate health and disease: A mini review. Biomedicines 10, 3206 (2022).
Tyagi, B. et al. Exposure of environmental trace elements in prostate cancer patients: A multiple metal analysis. Toxicol. Appl. Pharmacol. 479, 116728 (2023).
Fu, H., Murali, A. & Damodaran, C. Exposure of Environmental Trace Elements in Prostate Cancer Patients: Risk Analysis in Multiple Levels. Presented at Urologic Oncology: Seminars and Original Investigations, 42, S88 (Elsevier, 2024).
Coradduzza, D., Congiargiu, A., Sanna, A., Lorenzo, B., Marra, S., Cossu, M., Tedde, A., Miglio, M. R., Zinellu, A. & Mangoni, A. A. Heavy metals and prostate cancer: A new study with new findings (2025):
Ashrap, P. et al. Predictors of urinary and blood metal (loid) concentrations among pregnant women in Northern Puerto Rico. Environ. Res. 183, 109178 (2020).
Martinez-Morata, I. et al. A state-of-the-science review on metal biomarkers. Curr. Environ. Health Rep. 10, 215–249 (2023).
Mizuno, Y. et al. Associations between urinary heavy metal concentrations and blood pressure in residents of Asian countries. Environ. Health Prev. Med. 26, 1–11 (2021).
Jomova, K., Alomar, S. Y., Nepovimova, E., Kuca, K. & Valko, M. Heavy metals: Toxicity and human health effects. Arch. Toxicol. 99, 1–57 (2024).
Pizent, A. et al. Environmental exposure to metals, parameters of oxidative stress in blood and prostate cancer: Results from two cohorts. Antioxidants 11(10), 2044 (2022).
Sarkar, B. Metals and Genetics (Springer, 2012).
Aureliano, M., De Sousa-Coelho, A. L., Dolan, C. C., Roess, D. A. & Crans, D. C. Biological consequences of vanadium effects on formation of reactive oxygen species and lipid peroxidation. Int. J. Mol. Sci. 24, 5382 (2023).
Zhang, Y. Toxic Effects of Heavy Metals on the Immune System: Evidence from Population and In Vitro Studies (University of Groningen, 2021).
Tripathi, S., Sharma, Y. & Kumar, D. Unveiling the link between chronic inflammation and cancer. Metab. Open 25, 100347 (2025).
Santos-de-Frutos, K. & Djouder, N. When dormancy fuels tumour relapse. Commun. Biol. 4, 747 (2021).
Bimonte, V. M. et al. The endocrine disruptor cadmium modulates the androgen–estrogen receptors ratio and induces inflammatory cytokines in luminal (a) cell models of breast cancer. Endocrine 83, 798–809 (2024).
Chen, B. et al. Cellular zinc metabolism and zinc signaling: From biological functions to diseases and therapeutic targets. Signal Transduct. Target. Ther. 9, 6 (2024).
Barlow, N. L. & Bradberry, S. M. Investigation and monitoring of heavy metal poisoning. J. Clin. Pathol. 76, 82–97 (2023).
Dai, Y., Xu, X., Huo, X., Schuitemaker, J. H. & Faas, M. M. Differential effect of lead and cadmium on mitochondrial function and NLRP3 inflammasome activation in human trophoblast. J. Physiol. https://doi.org/10.1113/JP286755 (2024).
Wondmie, G. F. & Ahmed, Z. Comprehensive human health risk assessment of heavy metal. In E-Waste and Heavy Metals: Health Hazards and Environmental Impact (eds Tabassum, B. et al.) 35 (Frontiers Media, 2024).
Khoshakhlagh, A. H., Mohammadzadeh, M. & Gruszecka-Kosowska, A. The preventive and carcinogenic effect of metals on cancer: A systematic review. BMC Public Health 24, 2079 (2024).
Anract, J. et al. Incidental prostate cancer in patients undergoing surgery for benign prostatic hyperplasia: A predictive model. Eur. Urol. Oncol. 8, 145–151 (2025).
Wang, L., Li, X., Liu, M., Zhou, H. & Shao, J. Association between monocyte-to-lymphocyte ratio and prostate cancer in the US population: A population-based study. Front. Cell Dev. Biol. 12, 1372731 (2024).
Nag, R., O’Rourke, S. M. & Cummins, E. Risk factors and assessment strategies for the evaluation of human or environmental risk from metal (loid) s—A focus on Ireland. Sci. Total Environ. 802, 149839 (2022).
Liaqat, M., Khan, R. A. & Kamal, S. Comprehensive modelling of prostate cancer progression: Integrating continuous and binary biomarkers with event time data and missing covariates. Discov. Appl. Sci. 6, 71 (2024).
Rijnhart, J. J., Twisk, J. W., Eekhout, I. & Heymans, M. W. Comparison of logistic-regression based methods for simple mediation analysis with a dichotomous outcome variable. BMC Med. Res. Methodol. 19, 1–10 (2019).
Cao, Z., Bakulski, K. M., Paulson, H. L. & Wang, X. Exposure to heavy metals, obesity, and stroke mortality in the united states. MedRxiv 98, e14872 (2023).
Munir, N. et al. Heavy metal contamination of natural foods is a serious health issue: A review. Sustainability 14, 161 (2021).
Huang, Y. et al. The association between urinary metals/metalloids and chronic kidney disease among general adults in Wuhan, China. Sci. Rep. 13, 15321 (2023).
Salcedo-Bellido, I. et al. Toxic metals in toenails as biomarkers of exposure: A review. Environ. Res. 197, 111028 (2021).
Bocca, B. & Battistini, B. Biomarkers of exposure and effect in human biomonitoring of metal-based nanomaterials: Their use in primary prevention and health surveillance. Nanotoxicology 18, 1–35 (2024).
Li, S., Xiao, X. & Zhang, X. Hydration status in older adults: Current knowledge and future challenges. Nutrients 15(11), 2609 (2023).
Chang, L., Shen, S., Zhang, Z., Song, X. & Jiang, Q. Study on the relationship between age and the concentrations of heavy metal elements in human bone. Ann. Transl. Med. 6, 320 (2018).
Funding
This project and D.C. were supported by the Autonomous Region of Sardinia, pursuant to Regional Law August 7, 2007, No. 7 "Promotion of Scientific Research and Technological Innovation in Sardinia—Project UGOV RAS_CRP2023 CARRU: “Role of Circulating Biomarkers in the Management of Patients Affected by Prostate Carcinoma”. National LILT Program—5 per thousand years 2022, Scientific-Sanitary Research Call LILT 2023: “Study of the Heterogeneity of Prostate Carcinoma as a Key for Dissecting Cellular Subtypes That Characterize It”, Number: LILT—Protocol Number 2024U0001294 dated March 29, 2024. Se.M. was funded by Fondazione di Sardegna, MEDICI 2017 Project "Nuclear Magnetic Resonance Studies: Toxic Metals and Carcinogens and Their Interactions with Cellular Targets" and MEDICI 2024 Project “Metalli Pesanti e Tumori: Comprendere l’Impatto Ambientale sulla Salute Umana”.
Author information
Authors and Affiliations
Contributions
Conceptualization: D.C. and Se.M., C.C.; methodology: D.C., C.C., Se.M.; software: A.S., M.C., B.D.L.; validation, D.C., B.D.L., Se.M.; formal analysis: A.S., M,C., D.C.; investigation: Se.M., B.D.L, A.T., D.C.; re-sources: So.M., A.T..; data curation: A.C., M.R.D.M., A.Z.; writing-original draft preparation: D.C., Se.M..; writing-review and editing: Se.M, C.C, M.M., A.A.M.; visualization: M.M., C.C., Se.M., A.A.C.; supervision: Se.M, C.C..
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee COMITATO ETICO INDIPENDENTE—Azienda Ospedaliero Universitaria di Cagliari P.O. San Giovanni di Dio: via Ospedale 54-09124 Cagliari. Approval Code: Prot. PG/2022/4985. Approval Date: 30/03/2022.
Informed consent
Written informed consent has been obtained from the patients to publish this paper.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Coradduzza, D., Sanna, A., Di Lorenzo, B. et al. Associations between plasma and urinary heavy metal concentrations and the risk of prostate cancer. Sci Rep 15, 14274 (2025). https://doi.org/10.1038/s41598-025-97682-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-97682-0