Abstract
Oral cavity squamous cell carcinoma (SCC) is the most common head and neck region tumor. The pathologic T4a classification is defined tumor invasion by three distinctive subgroups with skin, bone marrow, or a depth of invasion (DOI) > 10 mm and tumor size > 40 mm, as specified in the revised AJCC 8th edition staging manual. We examined these three subgroups’ different survival outcomes and explored factors influencing survival in patients with pT4a gingivobuccal SCC, and further investigate the discriminatory capacity among these three subgroups. All patients (n = 120) were treated from January 2010 to December 2021 for pT4a gingivobuccal SCC. Sixty-six (55%) exhibited bone invasion, 62 (51.7%) had skin invasion, and 44 (36.7%) had a deep DOI (DOI > 10 mm and tumor size > 40 mm). The median follow-up period for all patients was 93.6 months. The median overall survival (OS) was 48.1 months for patients with shallow (≤ 10 mm) vs. 25.1 months for those with deep DOIs (p = 0.03). The study found that deep DOI tumors were the primary factor influencing poorer OS in patients classified as pT4a after conducting a subgroup analysis. Three independent factors predicted poor prognosis: deep DOI (hazard ratio [HR] = 2.08, 95% confidence interval [CI] 1.00–4.31), extranodal extension (HR = 2.35, 95% CI 1.16–4.79), and positive resection margin (HR = 2.96, 95% CI 1.14–17.73). Deep DOI predicted worse outcomes and outperformed the risks of bone/skin invasion among these patients with pT4a gingivobuccal SCC.
Similar content being viewed by others
Introduction
Squamous cell carcinoma (SCC) is the most common type of malignant tumor found in the oral cavity, accounting for nearly 95% of all oral cancer cases. Oral cavity cancer is a leading cause of cancer-related deaths in developing countries. In the United States, oral cavity and pharyngeal cancers rank as the ninth most common cancer, while in Taiwan, they are the seventh most prevalent1,2. In Southeast Asia and Taiwan, where the main risk factors like areca nut chewing and smoking are predominant, the common sites for SCC in the oral cavity include the buccal mucosa, gingiva, tongue, hard palate, and retromolar trigone. In Taiwan, the buccal mucosa is the most frequently affected tumor site3.
The staging of primary tumors for oral cavity cancer has undergone regular revisions since the American Joint Committee on Cancer (AJCC) published the first edition of the Manual for Staging of Cancer in 1977. Traditionally, the largest dimension of the tumor has been the most significant characteristic of the Tumor (T) category in oral cavity cancer. Before 2017, pathologic (p) T4 categorized tumors based on their extension to the skin or bone marrow as pT4a. Meanwhile, tumors extending to the masticator space, pterygoid plates, skull base, and involving the internal carotid artery were classified as T4b. Numerous studies have validated that deeper tumor invasion correlates with an increased risk of nodal metastases and unfavorable outcomes. Depth of invasion (DOI) has been identified as having the worst prognostic significance4,5,6. The AJCC 8th edition significantly revised the T-category for oral cavity cancer by incorporating the DOI feature in 20177. The 2018 update specifies that tumor size > 40 mm and with a DOI > 10 mm should be classified as pT4a tumors8,9,10. Bone marrow and skin invasion are established criteria for classifying pT4a tumors linked to poor prognoses. It is now also plausible that the DOI and tumor size might influence prognosis as well. A prominent collaborative study has also demonstrated that DOI is significantly associated with worse outcomes. However, among these T4a subgroup’s tumors, it was impossible to further distinguish these subgroups based on these features5. In the revised 8th edition of the AJCC staging, pT4a oral cavity SCC now includes three subgroups characterized by DOI > 10 mm and tumor size > 40 mm and features with bone invasion or facial skin invasion in the resected specimen.
Given that gingivobuccal squamous cell carcinoma (SCC) is the most common type of oral cavity tumor, it could be suitable to perform radical excision, even in advanced stages3,11,12,13. Gingivo-buccal squamous cell carcinoma (SCC) is located in close proximity to the alveolar bones and skin, making it more susceptible to early invasion compared to other sub-sites of tongue and oral tumors. The existing literature has not thoroughly explored comparative outcomes in differentiating between those with tumor size > 40 mm and DOI > 10 mm and pT4a tumors with bone or skin invasion in resected oral cavity SCC11,12,13,14,15,16,17,18. We retrospectively reviewed our cancer database to analyze the differences in prognostic outcomes among these three subgroups patients with pT4 gingivobuccal SCC. Our primary goal was to evaluate whether these subgroups exhibit varying risks in terms of prognosis. Additionally, we aimed to identify the most significant factors influencing the prognosis of gingivobuccal patients with pT4a tumors, and further investigated the discriminatory capacity among these three subgroups.
Results
Patients’ characteristics
One hundred twenty patients with resected pT4a gingivobuccal SCC met our inclusion criteria. The study cohort consisted predominantly of men, with 118 males and 2 females. The median age was 57, ranging from 31 to 80, and 88.3% of participants were under 65. The most common subsites of oral cavity SCC were the bucca, gingiva, and lips (87.5%), followed by the retromolar (7.5%). Among the patients, 45 (37.5%) had confirmed positive neck metastases, and only 6 (5%) underwent neck node excision without neck dissection. The pN3 was observed in 22 patients and all pN3 patients exhibited the feature of extranodal extension (ENE) (18.3%), and positive resected margins were reported in 9 patients (7.5%). A total of 36 patients (30%) exhibited perineural invasion (PNI), while 14 patients (11.7%) showed evidence of lymphovascular invasion (LVI) in their pathological specimens. All patients underwent surgery aimed at curative treatment. Additionally, 104 patients (86.7%) received adjuvant radiotherapy alone or in combination with chemotherapy. All adjuvant radiotherapy doses prescribed to our patients were ≥ 60 Gy. A summary of the relevant demographic and clinicopathological details can be found in Table 1.
Distribution of subgroups of pT4a patients
In a study involving 120 patients with resected pT4a tumors, 66 (55%) exhibited bone marrow invasion, while 62 (51.7%) showed skin invasion. Additionally, 44 patients (36.7%) had tumor size > 40 mm and DOI > 10 mm. It was common for these pT4a tumors to overlap in features, meaning that some patients exhibited more than one characteristic. Due to this overlap, statistical analysis was not applied to compare the three subgroups. The T4a subgroup displayed a similar distribution in terms of age and gender. Notably, patients with a deep DOI (tumor size > 40 mm and DOI > 10 mm) were more likely to be younger, with 95.5% under 65 years old and 52% having neck lymph node metastasis. Table 2 summarizes the distribution of these subgroups among patients with pT4a tumors.
Survival outcomes among the pT4a subgroups
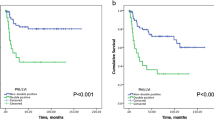
The median follow-up period for all patients was 93.6 months (standard deviation = 42 months; range = 26.4–164.4 months). The median overall survival (OS) for the entire cohort was 38 months, with a comparison showing 48.1 months for patients with shallow DOI tumors versus 25.1 months for those with deep DOI tumors. Additionally, the median disease-free survival (DFS) was 28 months for the whole cohort, with 36.6 months for shallow DOI tumors compared to 18 months for deep DOI tumors.
There was a statistically significant difference in OS favoring shallow DOI tumors (p = 0.03), as determined by the log-rank test (see Fig. 1a). However, for DFS, only a trend was observed favoring shallow DOI tumors with a p-value of 0.07 (see Fig. 2a). Additionally, the subgroup analysis of bone marrow or skin invasion did not show a statistically significant difference in OS with p-values of 0.1 for bone and 0.39 for skin, as determined by the log-rank test (see Fig. 1b,c). For DFS, no significant differences were found in the subgroup analyses of patients with bone (p = 0.1) or skin invasion (p = 0.41), again using the log-rank test (see Fig. 2b,c).
Overall survival analysis in patients with pT4a gingivobuccal squamous cell carcinoma: influence of tumor characteristics. Kaplan–Meier survival curves illustrating the 5-year overall survival rates of patients diagnosed with pT4a gingivobuccal squamous cell carcinoma. Panel (a) compares survival based on the presence vs. absence of tumor size > 40 mm and depth of invasion > 10 mm. Panels (b) and (c) assess the impact of bone invasion (presence vs. absence) and skin invasion (presence vs. absence) on overall survival. Statistical significance was assessed using the log-rank test, with p-values indicated.
Disease-free survival analysis of patients with pT4a gingivobuccal squamous cell carcinoma based on tumor characteristics. Kaplan–Meier survival curves illustrating 5-year disease-free survival rates in patients with pT4a gingivobuccal squamous cell carcinoma. Panel (a) compares survival outcomes based on the presence vs. absence of tumor size > 40 mm and depth of invasion > 10 mm. Panels (b) and (c) delineate survival based on the presence vs. absence of bone and skin invasion, respectively. Statistical significance was assessed using the log-rank test, with p-values indicated.
Stratification of deep DOI > 10 mm and tumor > 40 mm against shallow DOI ≤ 10 mm in pT4a patients
Following pathological review, 116 patients with pT4a tumors had documented DOI reports. Of these, 44 (38.0%) were classified in the deep DOI group. The median age of patients in the deep DOI group was 55, while 58 for those with shallow DOI (p = 0.27).
When compared to patients with shallow DOI tumors, those with deep DOI tumors showed a higher likelihood of being under 65 years of age (p = 0.052), having tumors located in the gingivobuccal subsite (p = 0.046), exhibiting ENE (p = 0.046), and having positive neck nodes (p = 0.048). However, the clinicopathological characteristics, such as positive resection margin, PNI, LVI, and postoperative adjuvant treatment, showed similar distributions between the deep and shallow DOI tumors. The clinicopathological features related to deep and shallow DOI of pT4a are summarized in Table 3.
Univariate and multivariate analyses of OS outcomes in patients with pT4a disease
Univariate analyses identified six critical predictors of OS. Among these, five factors were associated with a worse OS: deep DOI tumor (HR = 1.96, 95% CI 1.11–3.46), ENE (HR = 2.86, 95% CI 1.54–5.31), pathologic nodal status (HR = 2.68, 95% CI 1.54–4.65), positive resection margin (HR = 5.4, 95% CI 2.47–11.8), and LVI (HR = 2.08, 95% CI 2.08–4.28). Conversely, male sex was linked to a favorable OS (HR = 0.1, 95% CI 0.02–0.42).
We identified that both pN + and ENE significantly impact survival; however, pN + is strongly correlated with ENE. In our cohort, all pN3 patients exhibited the feature of ENE, making ENE a reasonable representative of pathologic nodal status in the study. Consequently, we included only the ENE factor in the multivariate analysis, based on the principle that independent variables should be independent of each other in such analyses. When these five variables were analyzed in a multivariate Cox proportional hazards model, three factors emerged as independent predictors of poorer prognosis: deep DOI tumor (HR = 2.08, 95% CI 1.00–4.31), ENE (HR = 2.35, 95% CI 1.16–4.79), and positive resection margin (HR = 2.96, 95% CI 1.14–17.73). For additional details, please refer to Table 4.
Discussion
According to the Global Cancer Statistics 2020, two-thirds of oral cavity cancer patients are in developing countries. The age-standardized mortality rate for cancer of the lip and oral cavity is 2.8 per 100,000 for men and 1.0 per 100,000 for women worldwide. In Taiwan, the age-standardized incidence rates for men rose significantly from 4.19 per 100,000 population in 1980 to 27.19 per 100,000 population in 2019, resulting in a man-to-woman ratio 9.5:11,2. Gingivobuccal SCC is strongly associated with the chewing of betel quid and the consumption of tobacco and alcohol2,3. A population-based study found a clear link between the rise in oral cancer incidence and cigarette/alcohol consumption, along with areca nut production in Taiwan2. Our cohort primarily consisted of males, with a median age of 57 years, and 86% of the patients were under 65. This aligns with a previous study on patients with pT4a tumors in Taiwan, which also reported a predominantly male population and a similar age distribution3,8.
Surgery with adequate margins, neck dissection, and adjuvant radiation or chemoradiation is essential for treating patients with oral cavity SCC5,6,8,11,12,13,14. There has been increased interest in the outcomes of resected pT4a patients based on different types of involvement, such as invasion through the bone cortex, skin, or deep DOI > 10 mm and tumors > 40 mm. Gingivobuccal SCC has a marked propensity to invade the mandible or maxilla cortical bone and facial skin. Patients exhibiting both invasion characteristics tend to have a higher likelihood of distant metastases and local recurrence11,13,16,17,18. In a retrospective analysis of 590 patients with pT4a oral cavity SCC, it was found that single bone involvement was not an independent prognostic marker after adjusting for margin positivity, tumor differentiation, PNI, and positive nodal involvement in a multivariable analysis16. Patients with pT4a oral cavity SCC with pathologic skin invasion have significantly worse survival outcomes as compared to controls without skin invasion17.
The International Consortium for Outcome Research in Head and Neck Cancer emphasizes that DOI is an independent negative factor affecting survival outcomes. Therefore, including DOI is foundational for revising the AJCC 8th edition5. While invasion of the bone or skin is the criterion for classifying tumors as T4a, the DOI may also affect prognosis. However, few studies have independently examined the interactions among these factors or assessed their discriminatory impact within specific subgroups. Our study found that deep DOI tumors were the primary factor influencing poorer OS in patients classified as pT4a after conducting a subgroup analysis. Liao et al. identified three unfavorable risk factors that impact OS in patients with pT3-4 oral cavity SCC. These factors include tumor size > 40 mm with a DOI > 10 mm, a DOI > 20 mm, and invasion through the bone cortex or skin. While all three criteria are significant, the authors further evaluated their ability to discriminate between outcomes. They found that the criteria related to DOI > 20 mm and invasion through the bone cortex/skin provided a better discriminative capability than the criterion of tumor size > 40 mm and DOI > 10 mm. Consequently, the authors recommended that tumors exhibiting a DOI > 20 mm be classified as T4a8. The literature consistently shows that the DOI correlates well with the risk of nodal metastasis and an increased likelihood of locoregional recurrence5,6,8,12,14,19,20,21. These studies found an increased DOI even in the negative neck node, revealing a significant cumulative risk that had a profound and negative impact on prognosis20,21,22. Our study found that patients with deep DOI tumors had a higher rate of positive nodal disease (52.3% compared to 30.6%) and ENE (29.5% compared to 12.5%) than those without deep DOI.Positive neck metastasis associated with ENE has long been recognized as an independent unfavorable prognostic factor for oral cancer23,24.
Our results indicate that pT4a is associated with a poor prognosis. Our cohort’s 2-year and 5-year OS rates align with those reported in the literature, with 2-year survival ranging from 70 to 80% and 5-year survival ranging from 31 to 65%8,11,12,13,16,17,18. A population study conducted in Taiwan reported the following survival rates for patients with pT3–T4 oral cavity SCC according to the AJCC 8th edition staging system: the 2-year cancer-specific survival rate was 71.8%, while the OS rate was 63.6%. The 5-year cancer-specific survival rate was 68.4%, and the OS rate was 57.9%18. Venkatesh et al. studied pT4a patients with bone invasion, reporting a 3-year DFS rate of 63.7% and an OS rate of 78.1%16. In comparison to the study by Diebolt et al., our findings revealed lower OS and DFS rates. For patients with pT4a tumors, those with skin invasion had a 2-year OS of 30.8% compared to 53.3% for those without skin invasion. The 5-year OS rates were 16.4% for patients with skin invasion and 42.2% for those without. Additionally, the DFS for patients with skin invasion was 23.7% at 2 years and 15.8% at 5 years, while patients without skin invasion had DFS rates of 47.7% at 2 years and 41.4% at 5 years17.
Our study identified four independent unfavorable prognostic factors for OS in pT4a patients, including tumor size > 40 mm and DOI > 10 mm, positive surgical margins, positive neck lymphatic metastasis, and ENE. Additionally, the literature indicates that other factors influencing the survival of T4a patients include age, histological features (such as differentiation, PNI, and LVI), ENE, treatment modality, and genetic characteristics3,4,11,12,13,16,17,18. Liao et al. identified the presence of ENE and positive nodes as independent unfavorable factors impacting survival outcomes in patients with pT4a tumors11,13. In a population study concerning pT4 oral cavity SCC in Taiwan, the authors identified four significant unfavorable prognostic variables: age ≥ 65 years, pN+, moderate-to-poor differentiation, positive resected margins, and treatment with surgery alone12. A cancer registry study conducted in Taiwan revealed that many patients with T3–4 tumors, characterized by their positive margins alone, surpassed most other risk factors associated with poor outcomes. This included factors such as advanced nodal stage, higher T stage, and age 65 years or older18.
Our primary study aimed to examine the impact of discrimination among subgroups of pT4a disease. However, there may be an inherent limitation in the new AJCC criterion concerning DOI in the literature, as these data are not consistently available in all pathologic reports. This inconsistency may complicate the transition between staging systems before 2016. Nevertheless, to adhere to the “long form” format and to prospectively gather cancer information for the Taiwan Cancer Registry (TCR) Database on oral cancer since 2011 in Taiwan, we have been collecting data regarding DOI, ENE, resected margin status, and detailed therapy18. The data provided information on whether the invasion was through DOI or cortex/skin. This allowed us to reclassify all pT4a patients according to the new AJCC staging guidelines. There is a concern that this revision in staging might lead to the underuse or unnecessary use of adjuvant therapies. However, 87% of our pT4a patients received adjuvant radiotherapy following NCCN treatment guidelines. Therefore, it is reasonable to hypothesize that most subgroups with a tumor > 40 mm and DOI > 10 mm before implementing the AJCC 8th edition likely received adjuvant therapies.
The study has some limitations. First, we only included patients classified as pT4 and did not examine all stages of gingivobuccal SCC in the database. Previous research has indicated that patients with pT3 may be reclassified as T4a based on DOI criteria, leading to migration or upstaging between the two different editions of the TNM classification (7th and 8th editions)25,26,27,28. Riemenschnitter et al. studied the reclassification of tumor stage using DOI in 2118 patients with oral SCC. They found that 14.4% of patients were upstaged due to the inclusion of DOI in the T-category25. Cramer et al. compared the 7th and 8th editions of the AJCC guidebook and found that 10.0% of all patients were upstaged, with 14.2% upstaged to stage III and 25.2% to stage IV disease27.
Despite the limitations of its retrospective design, the study revealed that deep DOI, along with a positive section margin and ENE, led to poor OS after adjusting for other prognostic factors. In summary, a DOI > 10 mm and a tumor size > 40 mm was identified as a significant prognostic factor in the T4a subgroup. The criteria of deep DOI and tumor size > 40 mm has been identified and outperform the risks of bone/skin invasion. So the topic should be further investigated and might be reflected in further revisions of pT4a classification in gingivobuccal SCC. As this is a retrospective study with a limited sample size obtained from a single tertiary academic center, further stratification on pathologic nodal group, adjuvant treatment, and doses of radiation and chemotherapy might not be feasible. Our findings may prompt further research involving a larger cohort or utilizing the Taiwan Cancer Registry (TCR) database, which has prospectively gathered detailed clinicopathologic data on oral cancer patients, for validation. Furthermore, despite having a substantial sample size for these evaluations, the study did not assess multiple important factors, such as histologic differentiation or lifestyle habits like smoking and/or areca nut consumption.
Materials and methods
Patients and data collection
This retrospective study focuses on patients with pT4 SCC of the oral cavity, treated between January 2010 and December 2021. Tumor locations were identified using the ICD coding for Oncology, third edition, specifically about gingivobuccal (C06.0), retromolar (C06.2), and unspecified areas (C06.8–06.9). Clinicopathological information was gathered from the oral cancer registry database at Chi Mei Medical Center. We confirmed that all methods were performed in accordance with relevant guidelines and regulations. Informed consent was waived due to the retrospective nature of the study, and the analysis used anonymized clinical data with the approval of the Chi Mei Medical Center Institutional Review Board (IRB No. 11309-008).
All patients underwent radical tumor surgery, which included therapeutic neck dissection. Our exclusion criteria were stringent, including the absence of follow-up data, perioperative mortality, or incomplete information regarding primary tumor characteristics or nodal status, which are essential for accurate staging. Patients were also excluded if they had not undergone surgery at our hospital, were treated solely with palliative intent, or had previous head and neck radiotherapy. This ensured the reliability and accuracy of our findings.
All included patients completed their treatment, which was determined by a multidisciplinary head and neck cancer treatment team, and were followed at a cancer center at regular intervals posttreatment. Adjuvant therapy was administered to our pT4a patients showing ENE, multiple lymph node metastases, or positive margins (when a second surgical operation was infeasible) in the study and radiation doses, with a consensus of 60–66 Gy, were prescribed according to NCCN treatment guidelines29. Follow-up data up to December 2023 were collected through chart reviews. A flowchart illustrating the selection process for study participants is provided in Supplemental Fig. 1.
DOI and pathologic features
Taiwan hospitals must report all cases of oral cancer to the TCR database. The database includes demographics, clinical information, pathological features, and details about cancer treatment. The Health and Welfare Data Science Center of the Taiwanese Ministry of Health and Welfare oversees the TCR. As of 2011, certain variables—such as ENE, resected margin status, and DOI—must adhere to the “long form” cancer data format18. The definitions of pT4a subgroup tumors differ between the 7th and 8th editions of the AJCC staging manual. In the 8th edition, pT4a is reclassified into subgroups based on bone marrow invasion, skin invasion, or tumors > 40 mm with a DOI > 10 mm. Each case was reviewed individually. Additionally, the ENE of the dissected lymph nodes should be extracted from the pathology reports on a case-by-case basis. The cohort of pT4a patients was then re-categorized based on DOI, with tumors further classified as shallow DOI (DOI ≤ 10 mm) or deep DOI (DOI > 10 mm and tumor > 40 mm).
Statistical analysis
Patients were categorized into two groups based on shallow pT4a or deep pT4a tumors. We assessed both groups’ OS and DFS. For OS, patients were censored at the time of death or the last follow-up, measured from the date of cancer diagnosis. For DFS, patients were censored upon experiencing locoregional or metastatic recurrence or death from any cause, starting from the date following radical surgery.
Using the log-rank test, we employed Kaplan–Meier analyses for survival comparisons and evaluated differences between the survival curves. Continuous variable differences were assessed with the Student’s t-test or the Wilcoxon rank sum test, while differences in categorical variables were evaluated using the chi-square test. To identify independent survival factors, we utilized multivariate Cox proportional hazard models that included variables with p-values less than 0.05 from the univariate analyses. We calculated hazard ratios (HR) and 95% confidence intervals (CI). A two-tailed p-value of < 0.05 was considered statistically significant. All analyses were performed using the statistical package SPSS version 25 for Windows (SPSS, Chicago, IL, USA).
Data availability
The datasets used and/or analysed during the current study are unable to openly reported due to protect study participant privacy, and only available from the corresponding author on reasonable request.
References
Siegel, R. L., Giaquinto, A. N. & Jemal, A. Cancer statistics, 2024. CA Cancer J. Clin. 74, 12–49 (2024).
Chou, C. W., Lin, C. R., Chung, Y. T. & Tang, C. S. Epidemiology of oral cancer in Taiwan: A population-based cancer registry study. Cancers 15, 2175. https://doi.org/10.3390/cancers15072175 (2023).
Lin, N. C., Hsien, S. I., Hsu, J. T. & Chen, M. Y. C. Impact on patients with oral squamous cell carcinoma in different anatomical subsites: A single-center study in Taiwan. Sci. Rep. 11, 15446. https://doi.org/10.1038/s41598-021-95007-5 (2021).
Pillai, V. et al. Prognostic determinants of locally advanced buccal mucosa cancer: Do we need to relook the current staging criteria? Oral Oncol. 95, 43–51 (2019).
Ebrahimi, A. et al. Primary tumor staging for oral cancer and a proposed modification incorporating depth of invasion: An international multicenter retrospective study. JAMA Otolaryngol. Head Neck Surg. 140, 1138–1148 (2014).
Pentenero, M., Gandolfo, S. & Carrozzo, M. Importance of tumor thickness and depth of invasion in nodal involvement and prognosis of oral squamous cell carcinoma: A review of the literature. Head Neck. 27, 1080–1091 (2005).
Lydiatt, W. M. et al. Head and neck cancers-major changes in the American joint committee on cancer eighth edition cancer staging manual. CA Cancer J. Clin. 67, 122–137 (2017).
Liao, C. T. et al. Tumor depth of invasion (tumor > 4 cm/depth > 10 mm and depth > 20 mm) and through cortex/skin invasion are both valid criteria for classifying tumors as pT4a in AJCC 2018 oral cavity cancer staging system. Ann. Surg. Oncol. 26, 3663–3672 (2019).
Zanoni, D. K., Patel, S. G. & Shah, J. P. Changes in the 8th edition of the American joint committee on cancer (AJCC) staging of head and neck cancer: Rationale and implications. Curr. Oncol. Rep. 21, 52. https://doi.org/10.1007/s11912-019-0799-x (2019).
Mattavelli, D. et al. The 8th TNM classification for oral squamous cell carcinoma: What is gained, what is lost, and what is missing. Oral Oncol. 111, 104937. https://doi.org/10.1016/j.oraloncology.2020.104937 (2020).
Liao, C. T. et al. Comparative outcomes in oral cavity cancer with resected pT4a and pT4b. Oral Oncol. 49, 230–236 (2013).
Kang, C. J. et al. Clinical outcomes of patients with pT4a and pT4b oral cavity squamous cell carcinoma who had undergone surgery: Results from a Taiwanese registry-based, nationwide cohort study. Oral Oncol. 126, 105750. https://doi.org/10.1016/j.oraloncology.2022.105750 (2022).
Liao, C. T. et al. Surgical outcome of T4a and resected T4b oral cavity cancer. Cancer 107, 337–344 (2006).
Piazza, C., Bresciani, L. & Giannini, L. Depth of invasion for prognostic stratification in oral cavity cancer: Do we need further validation? Ann. Transl. Med. 7, S84. https://doi.org/10.21037/atm.2019.04.19 (2019).
Yokota, Y. et al. Comparison of the 8th edition of TNM staging of oral cancer with the 7th edition and its prognostic significance using clinical depth of invasion and extranodal extension. Oral Oncol. 145, 106519. https://doi.org/10.1016/j.oraloncology.2023.106519 (2023).
Venkatesh, B. et al. Challenges in the assessment of medullary bone invasion in oral cavity cancers and its prognostic significance. Head Neck Pathol. 18, 37 (2024).
Diebolt, J. H. et al. Prognostic implications of skin invasion in locally advanced oral cavity squamous cell carcinoma. Otolaryngol. Head Neck Surg. 169, 69–75 (2023).
Lin, M. C. et al. Adequate surgical margins for oral cancer: A Taiwan cancer registry National database analysis. Oral Oncol. 119, 105358 (2021).
Shinn, J. R. et al. Cumulative incidence of neck recurrence with increasing depth of invasion. Oral Oncol. 87, 36–42 (2018).
Chang, B. et al. A prognostic nomogram incorporating depth of tumor invasion to predict long-term overall survival for tongue squamous cell carcinoma with R0 resection. J. Cancer. 9, 2107–2115 (2018).
Jain, P. V. et al. Clinicopathologic determinants of outcome in pathologic T4a (pT4a) squamous cell carcinoma of the gingivobuccal subsite of the oral cavity. Indian J. Surg. Oncol. 10, 594–599 (2019).
Huang, S. H., Hwang, D., Lockwood, G., Goldstein, D. P. & O’Sullivan, B. Predictive value of tumor thickness for cervical lymph-node involvement in squamous cell carcinoma of the oral cavity: A meta-analysis of reported studies. Cancer 115, 1489–1497 (2009).
Yanamoto, S. et al. Multicenter retrospective study of adjuvant therapy for patients with pathologically lymph node-positive oral squamous cell carcinoma: Analysis of covariance using propensity score. Ann. Surg. Oncol. 22, S992–S999 (2015).
Shaw, R. J. et al. Extracapsular spread in oral squamous cell carcinoma. Head Neck. 32, 714–722 (2010).
Riemenschnitter, C. E. et al. Need for adjuvant radiotherapy in oral cancer: Depth of invasion rather than tumor diameter. Eur. Arch. Otorhinolaryngol. 280, 339–346 (2023).
Mercante, G. et al. TNM classifications for oral cavity tumors in the 8th editions and following versions. Eur. Arch. Otorhinolaryngol. 279, 527–531 (2022).
Cramer, J. D., Reddy, A., Ferris, R. L., Duvvuri, U. & Samant, S. Comparison of the seventh and eighth edition American joint committee on cancer oral cavity staging systems. Laryngoscope 128, 2351–2360 (2018).
Jain, D., Dravid, C., Singla, A., Kumari, S. & Grover, R. K. Comparison of the seventh and eighth editions of the American joint committee on cancer pT and pN classifications as predictors of survival in patients with oral squamous cell carcinoma. Am. J. Clin. Pathol. 151, 292–301 (2019).
National Comprehensive Cancer Network. Head and neck cancer. Version 1.2025.
Acknowledgements
The authors acknowledge the Department of Cancer Registry of Chi Mei Medical Center, Tainan, Taiwan, and Enago® for the English language review.
Funding
This work was supported by grants from the Ministry of Science and Technology (Taiwan) (MOST 111-2314-B-384-006-MY3) and Chi Mei Medical Center (Tainan, Taiwan) (CMMOST11106).
Author information
Authors and Affiliations
Contributions
Conceptualization: S-Y H. Data curation: C-Y Y, C-Y L, M-T C, H-C Y, C-H L, L-C L. Statistical analysis: L-T S. Supervision: S-Y H. Writing–original draft: W-J H and S-Y H. Writing, review, and editing: S-Y H.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Research ethics
This study was conducted in compliance with the Declaration of Helsinki. The research project was approved by the Chi Mei Medical Center Institutional Review Board (IRB No. 11309-008). The authors are accountable for all aspects of the work and ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Following the journal’s patient consent policy, written informed consent was obtained from the patients to publish this report.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hong, WJ., Shieh, LT., Yen, CY. et al. The significance of the depth of invasion and tumor size in resected pathologic T4a gingivobuccal squamous cell carcinoma. Sci Rep 15, 14618 (2025). https://doi.org/10.1038/s41598-025-98222-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-98222-6