Abstract
Bladder cancer therapy remains challenging due to poor efficacy and frequent recurrence. Mannose, a naturally occurring monosaccharide, has demonstrated antitumor effects in various cancers, yet its mechanism of action in bladder cancer is unclear. This study explored the inhibitory effects of mannose on bladder cancer. We found mannose significantly inhibited the growth of bladder cancer cells, xenografts, and organoids. Mannose directly binds to PKM2, inhibiting its enzymatic activity and reducing lactate production. This reduction in lactate led to decreased PKM2 lactylation and increased acetylation, causing PKM2 to translocate to the nucleus. Nuclear PKM2 activated the NF-κB pathway, inducing NLRP1/Caspase-1/GSDMD/IL-1β-dependent pyroptosis. Additionally, mannose promoted antitumor immune responses by inducing pyroptosis and enhancing the efficacy of immune checkpoint inhibitors. These findings highlight the use of mannose as a potent antitumor agent and a promising therapeutic strategy for bladder cancer.
Similar content being viewed by others
Introduction
Bladder cancer, as the most common malignancy of the urinary system, is classified into muscle-invasive (MIBC) and nonmuscle-invasive (NMIBC) subtypes. NMIBC accounts for ~75% of new diagnoses, with ~20% progressing to MIBC1. Post-treatment recurrence occurs in 50–70% of NMIBC patients, while up to 50% of MIBC patients relapse within 5 years post-cystectomy2. Current first-line platinum-based chemotherapy achieves 36–65% response rates but fails to improve overall survival3. Although immunotherapies such as Bacillus Calmette–Guérin (BCG) instillation and immune checkpoint inhibitors show promise, the urgent need for more effective drugs to curb tumor recurrence and progression remains4.
Mannose, a natural monosaccharide found in various plants and fruits, exists at low concentrations in human body fluids5. It is primarily excreted through the urinary system and accumulates in the bladder, directly impacting bladder cells, a unique advantage in treating urinary tract diseases. Recent studies have demonstrated the effectiveness of mannose against urinary tract infections caused by Escherichia coli and other bacteria, underscoring its safety and biocompatibility6,7. Mannose exhibits diverse antitumor effects across different cancers: In osteosarcoma and fibrosarcoma cells lacking the essential mannose metabolism enzyme phosphomannose isomerase (PMI), mannose-induced metabolite accumulation disrupts glucose metabolism, causing energy deficits, nucleic acid metabolism disorders, genomic instability, and ultimately cancer cell death8,9. In breast cancer, due to increased mannose metabolism, it regulates cellular glycosylation to inhibit PD-L1 expression and enhance immunotherapy efficacy10. Additionally, mannose impacts key signaling pathways, including the PI3K/AKT, ERK, and AMPK pathways, in other cancers11. These findings position mannose as a promising therapeutic candidate for bladder tumors, warranting further exploration of its role in cancer therapy.
Lactylation, a recently discovered protein post-translational modification, was initially noted in histones12. This process involves the addition of lactyl groups to lysine residues, thereby linking the metabolic byproduct lactate with gene expression regulation. Lactylation has been shown to activate oncogenes and promote cell proliferation, angiogenesis, and immune evasion13. Emerging evidence shows that nonhistone proteins such as metabolic enzymes and transcription factors also undergo lactylation, which can alter their activity, stability, or interactions with other molecules, thereby affecting tumor cell proliferation, migration, and metabolism14. Therefore, further investigation of abnormal lactylation in bladder cancer is critical for elucidating the mechanisms of its development and progression.
Cellular pyroptosis, a caspase-dependent form of programmed cell death, is characterized by inflammatory caspase activation and significant proinflammatory mediator release, morphologically and mechanistically distinct from apoptosis and necrosis15. It plays pivotal roles in various diseases, including infections, neurodegenerative disorders, and cancers16. Pyroptosis commences when inflammasomes detect stimulatory signals, leading to caspase-1 recruitment and activation. The activated caspase-1 cleaves and activates both the pyroptosis effector gasdermin D (GSDMD) and the cytokine IL-1β, resulting in cell membrane pore formation that triggers cell death and inflammatory mediator release17. Consequently, induction of cancer cell pyroptosis represents a target for antitumor therapy.
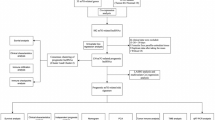
In this study, we investigated the regulatory effects of mannose on bladder cancer growth and analyzed its targets and downstream signaling pathways in bladder cancer cells. We discovered that mannose significantly inhibits bladder cancer growth by inducing pyroptosis and synergistically enhances the efficacy of chemotherapy and immunotherapy. Specifically, in bladder cancer cells, mannose targets PKM2, inhibits its lactylation, and promotes its nuclear translocation to activate NF-κB pathway-dependent pyroptosis and foster an antitumor immune environment.
Results
Mannose inhibits tumor growth in bladder cancer
We first evaluated the intrinsic levels of PMI across various cancer cell lines and urothelial cells (Fig. 1A) and assessed the impact of mannose on these cells (Fig. 1B and Supplementary Fig. 1D). Mannose significantly inhibited the growth of bladder cancer cell lines, independent of endogenous PMI expression levels. We selected 5637 and UMUC3 cells for detailed analysis. The IC50 values for mannose in 5637 and UMUC3 cells were 45 mM and 25 mM, respectively (Fig. 1C). The results of the cell cycle analysis indicated that mannose treatment increased in the proportion of cells in the G1 phase while reducing the S-phase population, suggesting G1/S-phase arrest (Fig. 1D). PCR analysis revealed significant downregulation of CCNA2 in both cell lines, further supporting the induction of G1/S phase arrest by mannose (Fig. 1E). Flow cytometry with PI staining showed that mannose promoted cell death (Fig. 1F). However, no activation of apoptosis-related proteins was observed, indicating cell death occurred independently of the apoptotic pathway (Fig. 1G, K). Mannose also inhibited the growth of patient-derived bladder cancer organoids (Fig. 1H). In vivo experiments confirmed that mannose suppressed bladder cancer xenograft growth in nude mice (Fig. 1I, J). Consistent with previous findings, mannose synergistically enhanced cisplatin- and THP-induced apoptosis (Fig. 1K, L).
A Western blot analysis of PMI expression in urinary epithelial cells and bladder cancer cells (SVHUC1, 5637, T24, UMUC3). B Colony formation assay assessing the effects of mannose on the proliferation of urinary epithelial cells (SVHUC1) and cancer cells. C A CCK-8 assay was used to determine the duration of mannose treatment and the IC50 at 48 h, with values of ~45 mM for UMUC3 cells and 20 mM for 5637 cells. D Cell cycle analysis following mannose treatment in UMUC3 and 5637 cells. E PCR analysis of cyclin expression in UMUC3 and 5637 cells treated with mannose. F Flow cytometry analysis of UMUC3 and 5637 cell death induced by mannose treatment. G Assessment of apoptosis pathway activation in mannose-treated UMUC3 and 5637 cells. H Evaluation of the ability of mannose to inhibit the growth of bladder tumor organoids. I Assessment of the growth inhibition effect of mannose in nude mice bearing transplanted bladder tumors. J Immunohistochemistry (Ki-67 staining) confirming the inhibitory effect of mannose on bladder cancer tissue. K Detection of PARP cleavage in cells treated with mannose combined with cisplatin (CDDP) or pirarubicin (THP). L Analysis of the combined effects of mannose and cisplatin or pirarubicin on UMUC3 cells, with drug combination indices calculated via ZIP scores.
Mannose binds to PKM2 and inhibits its enzymatic activity
Through biotin-labeled mannose pull-down and mass spectrometry analysis, we identified PKM2, a critical glycolytic regulator, as a high-abundance binding target (Fig. 2A, B and Supplementary Data 2). Enrichment analysis revealed strong association of the identified proteins with glycolytic pathways (Fig. 2C). Fluorescence colocalization, small molecule pull-down, and CETSA confirmed specific binding between mannose and PKM2 (Fig. 2D–F). Molecular docking revealed that mannose binds to PKM2 active pocket, forming hydrogen bonds with Asp296, a crucial catalytic site, indicating competitive inhibition of PKM2 enzymatic function (Fig. 2G, H). Molecular dynamics simulations demonstrated that mannose stabilizes PKM2 conformational changes (Fig. 2I, J). We also confirmed mannose inhibits pyruvate kinase activity in bladder cancer cells (Fig. 2K).
A Schematic of mannose with biotin modification. B List of proteins bound to biotinylated mannose identified via a pull-down assay and mass spectrometry. C KEGG analysis showing the enrichment of mannose-bound proteins in glycolytic and other metabolic pathways. D Immunofluorescence staining indicating the colocalization of biotinylated mannose with PKM2 in cells. E Confirmation of the binding of mannose to PKM2 via a biotinylated mannose pull-down assay. F CETSA confirming the increased thermal stability of PKM2 in the presence of mannose. G, H Molecular docking results showing that mannose binds to the active pocket of PKM2 and forms hydrogen bonds with the catalytic site K296. I, J Molecular dynamics simulation of PKM2 in complex with mannose, analyzing changes in RMSD and RMSF. K Analysis of the effects of mannose on pyruvate kinase activity in bladder cancer cells.
Mannose inhibits lactate production and lactylation
We further investigated the effects of mannose on cellular glucose metabolism. Mannose significantly reduced culture medium acidification and cellular glycolytic capacity (Fig. 3A, B). Metabolomic analysis revealed that the altered metabolites enriched in pyruvate metabolism pathway (Fig. 3C, D, Supplementary Data 3). While glucose, glucose-6-phosphate (G6P), and glucose-1-phosphate (G1P) levels remained unchanged, mannose markedly decreased lactate and pyruvate levels (Fig. 3E). Additionally, mannose significantly reduced pyruvate kinase activity, pyruvate content, and lactate content without affecting lactate dehydrogenase activity (Figs. 3F–H and 2N). Furthermore, mannose suppressed cellular ATP production, which was rescued by lactate supplementation (Fig. 3I, J). Finally, we demonstrated that mannose inhibited the overall lactylation level in bladder cancer cells and xenografts (Fig. 3K, L). Collectively, these results indicate that mannose inhibits cellular glycolytic activity, lactate production, and overall lactylation levels by inhibiting PKM2 enzymatic activity.
A Measurement of the pH of the culture medium of bladder cancer cells following mannose treatment. B Seahorse analysis of the impact of mannose on the glycolytic capacity of UMUC3 and 5637 cells. C PLS-DA validation of the effects of mannose on the metabolic profile of UMUC3 bladder cancer cells. D KEGG pathway enrichment analysis of significantly altered metabolic pathways in UMUC3 cells treated with mannose. E Changes in glycolytic products in mannose-treated UMUC3 cells analyzed via metabolomics. F Analysis of LDH enzyme activity in bladder cancer cells treated with mannose. G Measurement of lactate levels in bladder cancer cells following mannose treatment. H Analysis of pyruvate levels in bladder cancer cells treated with mannose. I Assessment of ATP production in mannose-treated bladder cancer cells. J Restoration of ATP production by lactate supplementation in mannose-treated bladder cancer cells. K Western blot analysis of lactylation levels in mannose-treated bladder cancer cells. L Immunohistochemistry was used to assess the effects of mannose on protein lactylation levels in xenograft tumor tissues from nude mice.
Mannose promotes PKM2 nuclear translocation by regulating K433 lactylation
To identify proteins that undergo lactylation in bladder cancer cells, we conducted lactylation-immunoprecipitated protein mass spectrometry identified PKM2 K433 as a lactylation site (Fig. 4A, Supplementary Fig. S1A, and Supplementary Data 4). Further analysis confirmed that mannose treatment reduced PKM2 lactylation (Fig. 4B, C). A PKM2 K433R mutation abolished PKM2 lactylation and impaired pyruvate generation, highlighting its role in enzymatic activity (Fig. 4D, E). We also established that p300, a primary lactyltransferase, interacts with PKM2 (Fig. 4F), and that p300 knockdown reduced PKM2 lactylation and enzymatic activity (Fig. 4G, H). Given that p300 also regulates PKM2 K433 acetylation, we hypothesized that lactylation and acetylation compete at this site18. Further tests revealed that mannose decreased PKM2 lactylation and increased acetylation, whereas lactate supplementation increased PKM2 lactylation and inhibited acetylation (Fig. 4I). PKM2 Y105 phosphorylation, which is critical for PKM2 nuclear translocation following acetylation19, was significantly enhanced by mannose (Fig. 4J). Immunofluorescence and cellular compartment analysis demonstrated that mannose treatment increased PKM2 nuclear translocation (Fig. 4K, L). Exogenous lactate, but not glucose, reversed mannose-induced PKM2 nuclear translocation (Fig. 4M). In summary, mannose inhibits PKM2 K433 lactylation, suppresses its enzymatic activity, and promotes PKM2 nuclear translocation.
A MS identification of K433 on PKM2 as a potential lactylation site in bladder cancer cells. B Immunoprecipitation validation of lactylation of PKM2 identified by mass spectrometry. C Validation of the regulatory effects of mannose on the identified lactylation of PKM2 in bladder cancer cells. D Introduction of exogenous wild-type PKM2 and K433R mutant PKM2 in bladder cancer cells, comparing lactylation levels with those of lactate supplementation. E Comparison of pyruvate production by wild-type PKM2 and K433R mutant PKM2 in bladder cancer cells. F Immunoprecipitation validation of the interaction between PKM2 and p300 in bladder cancer cells. G Changes in PKM2 lactylation levels in bladder cancer cells after p300 was knocked down with two different siRNAs. H Effects of p300 knockdown on pyruvate kinase activity in bladder cancer cells. I Effects of mannose and lactate supplementation on the lactylation and acetylation levels of PKM2 in bladder cancer cells. J Validation of PKM2 phosphorylation in mannose-treated bladder cancer cells. K Fluorescence detection of PKM2 localization following mannose treatment. L Analysis of nuclear and cytoplasmic PKM2 expression in bladder cancer cells. M Examination of the effects of mannose, glucose, and lactate supplementation on nuclear PKM2 expression in bladder cancer cells.
Mannose regulates PKM2 nuclear translocation to activate the NF-κB pathway and promote pyroptosis
Nuclear PKM2 can further activate other transcription factors and signaling pathways20. Using RNA sequencing and transcription factor analysis of bladder cancer cells treated with mannose, we found that the differentially expressed genes (DEGs) were significantly related to the NF-κB transcription factors RELA (p65) and NFKB1 (p50) (Fig. 5A and Supplementary Data 5). Further validation revealed that mannose treatment and exogenous nuclear PKM2 expression significantly activated p50 and p65 in bladder cancer cells (Fig. 5B). Mannose treatment also increased p50 and p65 in vivo (Fig. 5C). Fluorescence colocalization and immunoprecipitation confirmed that PKM2 colocalized and bound with p50 and p65, with stronger binding to p65 (Fig. 5D, E). Furthermore, lactate supplementation inhibited mannose-induced p65 activation (Fig. 5F). As mannose promoted nonapoptotic cell death, activated the inflammatory NF-κB pathway, and DEGs were enriched in programmed necrosis pathways, we propose that mannose may promote pyroptosis (Fig. 5G). To confirm this hypothesis, further tests revealed that mannose treatment increased LDH release (Fig. 5H) and lipid peroxidation (Fig. 5I). Morphologically, the mannose-treated cells exhibited typical pyroptotic features (Fig. 5J and Supplementary Fig. S1B). These results suggest that mannose activates the NF-κB pathway and promotes pyroptosis.
A RNA sequencing of mannose-treated UMUC3 cells with transcription factor analysis exploring key transcription factors associated with differentially expressed genes, highlighting the significant associations with NFKB1 and RELA. B Construction of bladder cancer cell lines with nuclear-specific expression of PKM2 to assess the effects of mannose treatment and nuclear PKM2 on the expression levels of p50 and p65. C Immunohistochemistry was used to assess the impact of mannose treatment on NF-κB transcription factor expression in xenograft tumor tissues from nude mice. D Fluorescence colocalization evaluation of p50 or p65 with PKM2 in UMUC3 cells. E Immunoprecipitation of p50 or p65 combined with PKM2 in UMUC3 and 5637 cells. F Analysis of the effects of mannose and lactate on p50 and p65 expression levels in different bladder cancer cell lines. G KEGG pathway enrichment analysis of significantly altered pathways in UMUC3 cells treated with mannose identified through RNA sequencing, highlighting pathways related to pyroptosis. H Measurement of LDH release induced by mannose-induced pyroptosis in bladder cancer cells. I Analysis of lipid peroxidation levels in bladder cancer cells treated with mannose by measuring the MDA content. J Examination of morphological changes in UMUC3 and 5637 cells via scanning electron microscopy (SEM) following mannose treatment.
Mannose activates NF-κB and NLRP1/Caspase-1/GSDMD/IL-1β dependent pyroptosis
We studied changes in the expression of NF-κB downstream inflammatory genes. We found that the expression levels of the pyroptosis-related factors IL1B, IL18, and TNF significantly increased after mannose treatment, whereas the IL6 levels remained unchanged (Fig. 6A). Additionally, mannose enhanced the transcription of the pyroptosis effector GSDMD (Fig. 6B). Among the upstream caspases, only CASP1 expression notably increased with mannose treatment (Fig. 6C). Our analysis also revealed that mannose increased both the expression and cleavage of Caspase-1, GSDMD, and IL-1β (Fig. 6D). Among the NOD-like receptor family members21, mannose activated the expression and cleavage of NLRP1 but not that of NLRP3 (Fig. 6E). Lactate supplementation inhibited the mannose-induced activation of NLRP1 and Caspase-1, as well as LDH release (Fig. 6F, G). Specifically, mannose treatment and nuclear PKM2 expression promoted p65 binding to the promoters of NLRP1, CASP1, GSDMD, and IL1B (Fig. 6H–K). In nude mouse xenografts, mannose significantly increased the expression of GSDMD and IL-1β, confirming its role in promoting NF-κB and NLRP1/Caspase-1/GSDMD/GSDMD/IL-1β-dependent pyroptosis (Fig. 6L).
A PCR analysis of NF-κB-induced cytokine expression in mannose-treated bladder cancer cells. B PCR analysis of pyroptosis-induced gasdermin gene expression in mannose-treated bladder cancer cells. C PCR analysis of genes upstream of GSDMD in mannose-treated bladder cancer cells. D Examination of the activation of pyroptosis pathways in response to mannose in bladder cancer cells. E Examination of the activation of NOD-like receptor pathways in response to mannose in bladder cancer cells. F Examination of the activation of NLRP1 and Caspase-1 by supplementation with lactate in mannose-treated bladder cancer cells. G Examination of LDH release by the addition of lactate to mannose-treated bladder cancer cells. Analysis of the transcriptional regulation of pyroptosis genes by the NF-κB transcription factor p65: H IL-1β, I GSDMD, J Caspase-1, K NLRP1. L. Immunohistochemistry was used to assess the impact of mannose treatment on pyroptosis-related protein expression levels in xenograft tumor tissues from nude mice.
Mannose activates antitumor immune responses through pyroptosis
Our findings also highlight the role of mannose in activating antitumor immunity. In C57BL/6 mice, mannose treatment significantly reduced MB49 xenograft growth (Fig. 7A, B) without affecting body weight or blood glucose levels (Fig. 7C, D). RNA sequencing and immune infiltration scoring revealed that mannose treatment led to T-cell activation (increased number of cytotoxic CD8⁺ T cells and decreased number of exhausted and regulatory T cells), enhanced humoral responses (B-cell activation and increased number of plasma cells), and proinflammatory responses (upregulated M1 macrophages and increased number of neutrophils) (Fig. 7E, Supplementary Fig. S1C, and Supplementary Data 6). IHC staining further confirmed the increase in CD8a and Gzmb (markers of cytotoxic CD8⁺ T cells) and CD11b (a monocyte marker) expression, coupled with a decrease in Pd-l1 expression (Fig. 7F). PCR analysis revealed that mannose increased IL-1B expression in xenografts (Fig. 7G). Immunofluorescence assays confirmed an increase in GSDMD expression (Fig. 7H). Finally, the combination of mannose with an anti-Pd-1 antibody demonstrated significantly greater antitumor efficacy than treatment with mannose or the anti-Pd-1 antibody alone (Fig. 7I, J). These results underscore that mannose activates antitumor immune responses through pyroptosis and synergistically enhances the efficacy of immunotherapy.
A Impact of mannose feeding on the growth of MB49 subcutaneous transplant tumors in C57BL/6 mice on day 23. B Tumor growth curves of the mannose-supplemented subcutaneous transplant tumors. C Effects of mannose supplementation on the body weights of C57BL/6 mice on day 23. D Effects of mannose feeding on the blood glucose levels of C57BL/6 mice on day 23. E Immune infiltration analysis in mannose-supplemented transplant tumors harvested on day 23 via RNA sequencing, with a heatmap showing the fold changes in immune cell infiltration scores between the two groups. F IHC was used to assess the impact of mannose exposure on the infiltration levels of CD8+ T cells, cytotoxic CD8+ T cells (Gzmb), and CD11b+ innate immune cells, and Pd-l1 expression in mouse tumors harvested on day 23. G PCR analysis of immune-related interleukins in mouse tumors harvested on day 23. H Fluorescence evaluation of GSDMD expression in mouse tumors harvested on day 23. I Effects of the combination of mannose and an anti-Pd-1 antibody on the growth of MB49 subcutaneous transplant tumors in C57BL/6 mice. J Tumor growth curves of subcutaneously transplanted tumors treated with mannose combined with an anti-Pd-1 antibody.
Discussion
In this study, we demonstrate that mannose exerts direct antitumor effects by inducing pyroptosis while synergizing with chemotherapy and immunotherapy. Mannose, a natural monosaccharide abundant in plants such as cranberries, is clinically utilized in cranberry extracts to prevent urinary tract infections22. Following oral administration, mannose undergoes renal excretion and accumulates in the bladder before urinary elimination. This pharmacokinetic profile confers unique therapeutic advantages for urinary system diseases23. Moreover, as a natural compound, mannose exhibits superior biocompatibility and safety compared to synthetic small molecules, enhancing its clinical translatability24. Although structurally analogous to glucose, mannose minimally impacts blood glucose levels. Consistent with previous reports8, our animal studies revealed that chronic mannose administration did not alter physiological parameters (e.g., body weight, blood glucose) in mice, suggesting potential safety for diabetic populations8.
Through chemoproteomics, small molecule pull-down, molecular docking, and dynamics simulations, we identified PKM2 as a direct binding target of mannose. PKM2, a critical glycolytic enzyme catalyzing phosphoenolpyruvate (PEP)-to-pyruvate conversion with ATP generation, is highly expressed in embryonic and neoplastic cells, positioning it as a strategic therapeutic target25. Our findings further revealed that mannose suppresses PKM2 K433 lactylation while promoting K433 acetylation. This observation aligns with prior reports of competitive post-translational modifications at identical residues26. For example, methylation of histone H3K9 is associated with gene silencing, whereas acetylation at the same site is linked to gene activation, with these modifications competing to determine chromatin conformation and gene expression27. Mechanistically, mannose binding inhibits PKM2 enzymatic activity, reducing lactate production and establishing a self-reinforcing cycle: diminished PKM2 lactylation further reduces enzymatic activity while promoting acetylation-driven nuclear translocation and activating the NF-κB pathway.
Nuclear PKM2 functions as a transcriptional coactivator, enhancing NF-κB, HIF1α, and STAT3 activity28. We confirmed nuclear PKM2 binding to NF-κB transcription factors p50 and p65 in bladder cancer cells, thereby driving pyroptosis-related gene transcription. We observed that mannose activated the NLRP1/Caspase-1/GSDMD/IL-1β pyroptosis pathway, as evidenced by increased protein cleavage, upregulated total protein expression, and elevated mRNA levels. Taken together, these findings demonstrate that mannose can activate the pyroptosis pathway and upregulate its expression at the transcriptional level via the nuclear localization of PKM2.
During pyroptosis, gasdermin D forms membrane pores, releasing proinflammatory cytokines, such as IL-1β and IL-18, and damage-associated molecular patterns (DAMPs), into the tumor microenvironment29. These signals recruit and activate neighboring immune cells, initiating antitumor immune responses30. Our data demonstrate that mannose synergizes with immunotherapy by eliciting tumor cell pyroptosis, highlighting its clinical translation potential. Future studies will employ single-cell sequencing to dissect mannose-immune cell crosstalk within the tumor microenvironment via inflammatory signaling.
While conventional chemotherapy for cancer patients typically employs intravenous administration, bladder cancer patients uniquely benefit from intravesical chemotherapy through bladder perfusion. Compared to systemic intravenous delivery, intravesical chemotherapy not only enhances local drug concentration and prolongs chemotherapeutic agent exposure to bladder cancer cells, but also demonstrates reduced systemic side effects31. Mannose, a natural monosaccharide, exhibits excellent biocompatibility and safety profiles in humans. Notably, experimental animals maintained on 20% mannose-supplemented drinking water displayed no significant adverse effects, suggesting its promising potential as a intravesical therapeutic agent8. Following oral administration, mannose undergoes urinary excretion with prolonged bladder retention, thereby extending contact duration with bladder cancer cells and potentiating its cytotoxic effects7. Furthermore, mannose demonstrates substantial cost-effectiveness compared to currently available clinical chemotherapeutic agents, coupled with markedly reduced toxicity profiles, indicating its dual advantages in alleviating both economic and physiological burdens for bladder cancer patients. These findings underscore the scientific imperative for subsequent clinical investigations exploring the therapeutic efficacy of combined oral mannose administration and mannose solution intravesical perfusion in bladder cancer management.
Recent studies have revealed that mannose enhances antitumor immunity through T-cell differentiation remodeling and promotes PD-L1 degradation in breast cancer cells10,32. Our published research further demonstrates mannose-mediated inhibition of inflammatory microenvironment formation in lung cancer33. These collective findings highlight the robust immunomodulatory properties of mannose, suggesting potential synergistic effects when combined with immune checkpoint inhibitors to augment tumoricidal activity34. Building upon the proposed investigation of oral mannose combined with intravesical mannose perfusion, future research could explore the therapeutic potential of triple therapy incorporating immune checkpoint inhibitors for bladder cancer treatment. This innovative therapeutic paradigm warrants comprehensive preclinical and clinical evaluation to assess its efficacy in multimodal cancer management.
In summary, we demonstrate that mannose directly targets PKM2 in bladder cancer cells, suppressing its enzymatic activity and inhibiting glycolysis and lactate production. This metabolic reprogramming leads to suppression of PKM2 lactylation while promoting its nuclear translocation. Nuclear-localized PKM2 subsequently activates the NF-κB inflammatory signaling pathway, inducing pyroptosis-mediated tumor suppression and fostering an antitumor immune microenvironment.
Methods
Cell culture
Bladder cancer cell lines and control urothelial cells were cultured in high-glucose Dulbecco’s modified Eagle’s medium (DMEM) or RPMI 1640 medium supplemented with 10% fetal bovine serum (FBS) and 1% penicillin‒streptomycin. The cultures were maintained at 37 °C in a humidified atmosphere with 5% CO2.
Clonal formation assay
Cells were seeded in 6-well plates at a density of 1000 cells per well and treated under specified experimental conditions. After incubation, the colonies were fixed with paraformaldehyde, stained with crystal violet, and visualized. The clonal area was quantified using imaging software.
Cell Counting Kit-8 (CCK-8) assay
Cells were seeded in 96-well plates and treated according to the experimental protocol. Ten milliliters of CCK-8 solution was added to each well, and the cells were incubated for an additional period. The absorbance was measured using a microplate reader. Cell viability, inhibition rates, and IC50 values were calculated using GraphPad Prism software. The ZIP score was determined using the R package SynergyFinder35.
Patient-derived organoid culture
The study was approved by the Ethics Committee of Liaoning Cancer Hospital & Institute (GZR20240373). Informed consent was obtained for all participants. All ethical regulations relevant to human research participants were followed. Bladder tumor tissues were collected, minced, and enzymatically digested with a mixture of collagenase and dispase. Following digestion, the cell suspension was filtered, resuspended in Matrigel, and seeded into culture plates. Organoid culture medium was added once the droplets solidified, and the medium was changed every 3 days. Organoids were confirmed to be tumor components by immunohistochemistry after two passages.
Cell cycle analysis by flow cytometry cells
For cell cycle analysis by flow cytometry, the cells were trypsinized, collected, and fixed in ice-cold 70% ethanol overnight at 4 °C. Following fixation, the cells were washed with phosphate-buffered saline (PBS) and treated with RNase A. Propidium iodide (PI) staining was conducted to label the cellular DNA, and the stained cells were analyzed via flow cytometry. The DNA histograms were processed using FlowJo software.
Cell death analysis by flow cytometry
For cell death analysis by flow cytometry, both adherent and floating cells were collected, washed, and resuspended in binding buffer. The cells were stained with PI for 15 min in the dark at room temperature and analyzed using a flow cytometer, which acquired data for at least 10,000 events per sample. The percentage of PI-positive cells, indicative of cell death, was quantified using FlowJo software.
Western blotting (WB)
Cell lysates or immunoprecipitated samples were resolved by SDS‒PAGE based on the target protein’s molecular weight. Proteins were transferred onto nitrocellulose or PVDF membranes, which were then blocked with nonfat milk and incubated with primary antibodies overnight at 4 °C. After washing, the membranes were probed with HRP-conjugated secondary antibodies. The protein bands were visualized using an enhanced chemiluminescence (ECL) substrate and captured via a chemiluminescence imaging system.
Coimmunoprecipitation (co-IP)
Cells were resuspended in RIPA buffer supplemented with protease inhibitors and lysed; and the lysates were precleared with control IgG and protein G/A magnetic beads, followed by centrifugation. The supernatants were incubated with specific antibodies overnight at 4 °C and then with magnetic beads for 4 h. The immunoprecipitates were collected, washed with PBS, and eluted by boiling in SDS sample buffer.
Nuclear protein extraction
For nuclear protein extraction, the cells were harvested, washed, and resuspended in ice-cold hypotonic buffer containing protease inhibitors. After incubation on ice and homogenization, the cytoplasmic fraction was separated by centrifugation, and the nuclear pellet was resuspended in hypertonic buffer. Nuclei were lysed using a nonionic detergent, and centrifugation yielded a supernatant containing nuclear proteins. The extracted proteins were quantified and assessed via gel electrophoresis.
Biotinylated mannose synthesis and pull-down
Biotinylated mannose was synthesized through an esterification reaction between biotin and mannose, followed by purification using column chromatography or HPLC. Biotinylated mannose was added to the cell lysates, which were then incubated with streptavidin magnetic beads and washed to remove nonspecific proteins. The affinity of the target protein complexes for biotinylated mannose was analyzed via western blotting.
4D label-free mass spectrometry
After electrophoresis, 4D label-free mass spectrometry proteins extracted from gels were enzymatically digested into peptides. Peptides were separated through multidimensional chromatography, which combines high-pH and low-pH reversed-phase separations. The separated peptides were analyzed via mass spectrometry and identified and quantified on the basis of mass–charge ratios (m/z). The data were processed via bioinformatics tools to reveal proteome alterations.
Cellular thermal shift assay (CETSA)
CETSAs were conducted36: UMUC3 cell cultures were transiently transfected with EPL-epitope-tagged PKM2 constructs. Following transfection, cells were diluted to working concentration and treated with 50 mM mannose in a 5% CO2 humidified atmosphere at 37 °C for 60 min. A controlled thermal denaturation protocol was subsequently implemented, with microplates undergoing progressive temperature elevation from 40 °C to 68 °C using 2 °C increments. Cellular lysates were prepared through detergent-mediated membrane disruption followed by the addition of chemiluminescent detection substrates. Signal quantification was performed using a multimode plate reader with integrated luminescence detection capabilities. Thermal denaturation profiles were analyzed through non-linear regression analysis employing Boltzmann sigmoidal curve fitting in GraphPad Prism.
Molecular docking and molecular dynamics simulation
AutoDock was used for molecular docking between mannose and PKM2, and GROMACS was employed for molecular dynamics simulations. Molecular dynamics simulations of the complex were performed via Amber14. The general AMBER force field (GAFF) was used for mannose, and the ff14SB force field was used for PKM2. Molecular mechanics optimization and molecular dynamics simulation of all compounds were conducted via the Sander procedure in Amber14.
Enzyme activity assays
Metabolic enzyme activity assays were conducted using activity assay kits according to the manufacturer’s instructions. Cell lysates were prepared, and reactions containing lysate, assay buffer, and substrates were incubated. Substrate conversion was monitored by the absorbance corresponding to NADH production. Enzyme activity was calculated based on absorbance changes over time, and standard curves were used for quantification.
Seahorse XF glycolysis stress test
Cells were seeded in XF96 cell culture microplates and equilibrated in Seahorse XF Base Medium. The extracellular acidification rate (ECAR) was measured at baseline and in response to specific inhibitors, including glucose, oligomycin, and 2-deoxy-D-glucose (2-DG). The glycolytic capacity was calculated by subtracting the ECAR after oligomycin from that with glucose.
Metabolome
Metabolites were extracted from cells and analyzed using mass spectrometry to obtain their mass–charge ratios (m/z) and retention times. Data processing included peak detection, alignment, normalization, and the generation of metabolic profiles. Multivariate statistical analyses, such as partial least squares discriminant analysis (PLS-DA), were used to identify significant metabolites. Metabolites were extracted from cells and analyzed using mass spectrometry to obtain their mass–charge ratios (m/z) and retention times.
Metabolite detection
Metabolite contents, such as pyruvate and lactate contents, were measured via detection assay kits according to the manufacturer’s instructions. Cell lysates were prepared, and reactions containing lysate, assay buffer, and substrates were incubated. Substrate conversion was monitored by absorbance changes, and standard curves were used for quantification.
Plasmid transfection and lentiviral infection
293T cells were seeded and transfected with packaging plasmids and plasmids containing target DNA using Lipofectamine 3.0. After incubation, the virus-containing medium was collected and concentrated. Target cell lines were infected with the viral medium, and stable cell lines were established through puromycin selection or alternative methods.
RNA sequencing
Total RNA was extracted using TRIzol reagent and assessed for quality. mRNA was enriched, fragmented, and reverse-transcribed into cDNA. cDNA underwent end repair, A-tailing, and adapter ligation. Libraries were amplified, quality-checked, and sequenced on an Illumina platform. The data were subjected to quality control, alignment, and gene expression quantification for transcriptome analysis.
Real-time quantitative PCR (RT‒qPCR)
Total RNA was isolated and reverse-transcribed into cDNA via a reverse transcription kit. PCR was performed using specific primers and SYBR Green master mix. Gene expression levels were normalized to internal controls, and relative expression was calculated via the 2−ΔΔCT method.
Scanning electron microscopy (SEM) imaging
Samples were fixed, dehydrated through an ethanol series, critically point-dried, mounted on stubs, and sputter-coated with gold-palladium. SEM images were acquired to visualize the surface morphology.
Confocal immunofluorescence imaging
Cells were fixed, permeabilized, blocked, and incubated with primary antibodies overnight. After washing, they were incubated with fluorochrome-conjugated secondary antibodies and counterstained with DAPI. Images were acquired via a confocal microscope.
Lactate dehydrogenase (LDH) assay
Culture supernatants were collected, and LDH activity was measured via an LDH assay kit according to the manufacturer’s instructions. The reaction mixture was added to the samples, and the absorbance was measured at 490 nm.
Malondialdehyde (MDA) assay
Cell lysates were prepared, and supernatants were collected. After adding thiobarbituric acid (TBA) reagent, the mixtures were heated, cooled, and their absorbance was measured at 532 nm. MDA concentration was calculated using a standard curve.
Xenograft mice model
Animal studies were approved by the Animal Care and Use Committee of China Medical University (IACUC Issue No. KT2023184). We have complied with all relevant ethical regulations for animal use. BALB/c nude mice or C57BL/6 mice were subcutaneously inoculated with 10 million cells resuspended in Matrigel. Mice were fed water containing 0%, 10%, or 20% mannose. Pd-1 antibody was administered via tail vein injection. The tumor size was monitored for 23 days, and the tumor volume was measured. Tissues harvested on day 23 were further analyzed by IHC and RNA-seq.
Immunohistochemistry (IHC)
Formalin-fixed, paraffin-embedded tissues were sectioned, deparaffinized, and subjected to antigen retrieval. Sections were incubated with primary antibodies overnight, followed by HRP-conjugated secondary antibodies. Immunoreactivity was visualized using DAB chromogen, counterstained with hematoxylin, and examined under a microscope.
Statistics and reproducibility
The data were analyzed using GraphPad Prism 8.0 software. Triple biological replications were made. Unpaired/paired t-tests were used for comparing differences between two groups, and one-way/two-way ANOVA tests were used for comparing multiple groups. Significance levels were defined as not significant (ns), p < 0.05 (*), p < 0.01 (**), and p < 0.001 (***). The source data behind the graphs in the paper are provided as Supplementary Data 1. Drug combination scores were calculated via the SynergyFinder package in R35, pathway enrichment analysis via clusterProfiler37, and immune cell infiltration scoring via ImmuCellAI38.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
References
Siegel, R. L., Miller, K. D., Wagle, N. S. & Jemal, A. Cancer statistics, 2023. CA Cancer J. Clin. 73, 17–48 (2023).
Seiler, R. et al. Impact of molecular subtypes in muscle-invasive bladder cancer on predicting response and survival after neoadjuvant chemotherapy. Eur. Urol. 72, 544–554 (2017).
Liu, S., Chen, X. & Lin, T. Emerging strategies for the improvement of chemotherapy in bladder cancer: Current knowledge and future perspectives. J. Adv. Res. 39, 187–202 (2022).
Facchini, G. et al. Advanced/metastatic bladder cancer: current status and future directions. Eur. Rev. Med. Pharmacol. Sci. 24, 11536–11552 (2020).
Watkins, C. B. & Frenkel, C. Inhibition of pear fruit ripening by mannose. Plant Physiol. 85, 56–61 (1987).
Salvatore, S. et al. A randomized controlled trial comparing a new D-mannose-based dietary supplement to placebo for the treatment of uncomplicated Escherichia coli urinary tract infections. Eur. Urol. Focus 9, 654–659 (2023).
Hayward, G. et al. d-mannose for prevention of recurrent urinary tract infection among women: a randomized clinical trial. JAMA Intern Med. 184, 619–628 (2024).
Gonzalez, P. S. et al. Mannose impairs tumour growth and enhances chemotherapy. Nature 563, 719–723 (2018).
Harada, Y. et al. Metabolic clogging of mannose triggers dNTP loss and genomic instability in human cancer cells. eLife 12, e83870 (2023).
Zhang, R. et al. D-mannose facilitates immunotherapy and radiotherapy of triple-negative breast cancer via degradation of PD-L1. Proc. Natl. Acad. Sci. USA 119, e2114851119 (2022).
Jin, H., Liu, X. & Liu, H. X. Biological function, regulatory mechanism, and clinical application of mannose in cancer. Biochim. Biophys. Acta Rev. Cancer 1878, 188970 (2023).
Zhang, D. et al. Metabolic regulation of gene expression by histone lactylation. Nature 574, 575–580 (2019).
Yao, W., Hu, X. & Wang, X. Crossing epigenetic frontiers: the intersection of novel histone modifications and diseases. Signal. Transduct. Target Ther. 9, 232 (2024).
Yang, Z., Zheng, Y. & Gao, Q. Lysine lactylation in the regulation of tumor biology. Trends Endocrinol. Metab. 35, 720–731 (2024).
Burdette, B. E., Esparza, A. N., Zhu, H. & Wang, S. Gasdermin D in pyroptosis. Acta Pharm. Sin. B 11, 2768–2782 (2021).
Wei, X. et al. Role of pyroptosis in inflammation and cancer. Cell Mol. Immunol. 19, 971–992 (2022).
Arre, V. et al. The ‘speck’-tacular oversight of the NLRP3-pyroptosis pathway on gastrointestinal inflammatory diseases and tumorigenesis. J. Biomed. Sci. 30, 90 (2023).
Bhardwaj, A. & Das, S. SIRT6 deacetylates PKM2 to suppress its nuclear localization and oncogenic functions. Proc. Natl. Acad. Sci. USA 113, E538–E547 (2016).
Lv, L. et al. Mitogenic and oncogenic stimulation of K433 acetylation promotes PKM2 protein kinase activity and nuclear localization. Mol. Cell 52, 340–352 (2013).
Zhang, S., Liao, Z., Li, S. & Luo, Y. Non-metabolic enzyme function of PKM2 in hepatocellular carcinoma: a review. Medecine 102, e35571 (2023).
Robinson, K. S. et al. ZAKalpha-driven ribotoxic stress response activates the human NLRP1 inflammasome. Science 377, 328–335 (2022).
Russo, E. et al. Cranberry, D-mannose and anti-inflammatory agents prevent lower urinary tract symptoms in women undergoing prolapse surgery. Climacteric 23, 201–205 (2020).
Maalouf, N. et al. High mannose level in bladder cancer enhances type 1 fimbria-mediated attachment of uropathogenic E. coli. Front. Cell Infect. Microbiol. 12, 968739 (2022).
Dalle Vedove, E., Costabile, G. & Merkel, O. M. Mannose and mannose-6-phosphate receptor-targeted drug delivery systems and their application in cancer therapy. Adv. Health. Mater. 7, e1701398 (2018).
Liao, M. et al. Targeting the Warburg effect: a revisited perspective from molecular mechanisms to traditional and innovative therapeutic strategies in cancer. Acta Pharm. Sin. B 14, 953–1008 (2024).
Hunter, T. The age of crosstalk: phosphorylation, ubiquitination, and beyond. Mol. Cell 28, 730–738 (2007).
Allis, C. D. & Jenuwein, T. The molecular hallmarks of epigenetic control. Nat. Rev. Genet. 17, 487–500 (2016).
Wang, D., Liu, X., Li, M., Ning, J. HIF-1alpha regulates the cell viability in radioiodine-resistant papillary thyroid carcinoma cells induced by hypoxia through PKM2/NF-kappaB signaling pathway. Mol. Carcinog. 63, 238–252 (2023).
Li, N., Wang, Y., Wang, X., Sun, N. & Gong, Y. H. Pathway network of pyroptosis and its potential inhibitors in acute kidney injury. Pharm. Res. 175, 106033 (2022).
Man, S. M. & Kanneganti, T. D. Innate immune sensing of cell death in disease and therapeutics. Nat. Cell Biol. 26, 1420–1433 (2024).
Lee, H. W. et al. Clinical efficacy of neoadjuvant intravesical mitomycin-c therapy immediately before transurethral resection of bladder tumor in patients with nonmuscle-invasive bladder cancer: preliminary results of a prospective, randomized phase II study. J. Urol. 209, 131–139 (2023).
Qiu, Y. et al. Mannose metabolism reshapes T cell differentiation to enhance anti-tumor immunity. Cancer Cell 43, 103–121.e108 (2025).
Jin, H. et al. Mannose inhibits NSCLC growth and inflammatory microenvironment by regulating gut microbiota and targeting OGT/hnRNP R/JUN/IL-8 Axis. Int. J. Biol. Sci. 21, 1566–1584 (2025).
Xing, Y. et al. A bifunctional lysosome‐targeting chimera nanoplatform for tumor‐selective protein degradation and enhanced cancer immunotherapy. Adv. Mater. 37, e2417942 (2025).
Malyutina, A. et al. Drug combination sensitivity scoring facilitates the discovery of synergistic and efficacious drug combinations in cancer. PLoS Comput. Biol. 15, e1006752 (2019).
Romero, C. et al. A cellular target engagement assay for the characterization of SHP2 (PTPN11) phosphatase inhibitors. J. Biol. Chem. 295, 2601–2613 (2020).
Yu, G., Wang, L. G., Han, Y. & He, Q. Y. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS 16, 284–287 (2012).
Miao, Y. R. et al. ImmuCellAI: a unique method for comprehensive T-cell subsets abundance prediction and its application in cancer immunotherapy. Adv. Sci. 7, 1902880 (2020).
Acknowledgements
This work was supported by National Natural Science Foundation of China (82002669), Natural Science Foundation of Liaoning (2020-ZLLH-39), The doctoral research start-up fund project of Natural Science Foundation of Liaoning (2021-BS-045), Key Research and Development Program of Liaoning Province (2023JH2/101300060), Natural Science Foundation of Liaoning (2022-MS-086), Natural Science Foundation of Liaoning (2023-MS-056), Natural Science Foundation of Liaoning (2023-BSBA-213), National Natural Science Foundation of China (82403330).
Author information
Authors and Affiliations
Contributions
Haoyi Jin: Investigation, Visualization, Writing—Original Draft. Pingeng Wu: Investigation, Validation. Chengcheng Lv: Data Curation, Formal analysis. Shouyi Zhang: Validation, Data Curation. Yunchao Zhang: Validation, Data Curation. Changqi Li: Validation, Data Curation. Ruxu Gao: Supervision. Guangyi Shan: Supervision. Huan Bi: Project administration. Hong Chang: Resources, Supervision. Xi Liu: Conceptualization, Writing—Review and Editing. Yu Zeng: Resources, Funding acquisition. All data were generated in-house, and no paper mill was used. All authors agree to be accountable for all aspects of work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The animal studies were approved by the Animal Care and Use Committee of China Medical University (IACUC Issue No. KT2023184, date: 04/03/2024), and all the animal handling procedures were conducted in accordance with the Basel Declaration. Organoid culture was approved by the local ethics committee of Liaoning Cancer Hospital& Institute (GZR20240373, date: 07/03/2024) based on the Helsinki Declaration, and written informed consent was obtained from all subjects.
Consent for publication
All authors consent for publication.
Peer review
Peer review information
Communications Biology thanks Zhenyu Nie and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editors: Mengtan Xing and Johannes Stortz.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jin, H., Wu, P., Lv, C. et al. Mannose inhibits PKM2 lactylation to induce pyroptosis in bladder cancer and activate antitumor immune responses. Commun Biol 8, 689 (2025). https://doi.org/10.1038/s42003-025-08130-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s42003-025-08130-8
This article is cited by
-
Lactylation at the crossroads of immune metabolism and epigenetic regulation: revealing its role in rheumatic immune diseases
Journal of Translational Medicine (2025)
-
Lactate at the crossroads of tumor metabolism and immune escape: a new frontier in cancer therapy
Journal of Translational Medicine (2025)