Abstract
Background
Cell therapy, particularly using cardiomyocytes, shows significant promise for treating heart failure. Direct reprogramming of somatic cells into cardiomyocytes using small molecules is advantageous due to its efficiency and cost-effectiveness.
Methods
Human urine-derived cells (hUCs) were transdifferentiated into functional cardiomyocyte-like cells (hCiCMs) using a cocktail of 15 small molecules under xeno-free conditions. Various Characterizations were performed, including immunofluorescence, transmission electron microscopy (TEM), qPCR, single-cell RNA sequencing, patch-clamp recordings, and intracellular Ca²+ measurements. The therapeutic potential was tested in both mouse and porcine models of myocardial infarction (MI).
Results
Reprogramming efficiency achieves 15.08% on day 30, with purity reaching 96.67% on day 60. hCiCMs display cardiomyocyte markers, sarcomeric structures, and abundant mitochondria. Electrophysiological analysis confirms ventricular-like action potentials and regular calcium transients. Single-cell RNA sequencing reveals cardiomyocyte subpopulations resembling 13-week embryonic human heart cells, with gene ontology analysis indicating successful maturation. In the MI model, hCiCM transplantation improves cardiac function, increasing ejection fraction and fractional shortening while reducing fibrosis.
Conclusions
This study demonstrates the successful reprogramming of hUCs into functional hCiCMs using small molecules under xeno-free conditions, offering a scalable, autologous cell source for cardiac repair with significant potential for regenerative therapies.
Plain language summary
Cardiomyocytes are the muscle cells within the heart that enable the heart to contract and pump blood. We aimed to develop a method to generate cardiomyocytes from cells derived from human urine. We used a combination of 15 small molecules to transform human urine-derived cells into cardiomyocyte-like cells. The cells were tested in mouse and porcine models of heart damage, where they were found to enhance heart function. This approach could be further developed as a possible safe, efficient, and scalable solution for producing heart cells that could be transplanted into people with heart disease as a treatment.
Similar content being viewed by others
Introduction
Heart failure occurs when the myocardium experiences cardiomyocyte loss or dysfunction1. However, cardiomyocytes are terminally differentiated cells that cannot self-proliferate in the adult mammalian heart. When myocardial infarction occurs, activated fibroblasts proliferate extensively at the infarct site, causing the continuous death of cardiomyocytes, the formation of scars, and the induction of irreversible damage. Currently available cardiac therapies focus primarily on preserving remaining cardiomyocytes and preventing fibrosis without effectively replenishing lost cardiomyocytes. Conversely, cell therapy aims to restore cardiac function after severe injury2. Although pioneering research has shown that transplanting cardiac stem/progenitor cells or cardiomyocytes can significantly improve cardiac function, the limited availability of cell sources and the risk of rejection after allogenic transplantation hinder the widespread clinical application of this approach3,4,5. Currently, embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) are two main cell sources used to obtain cardiomyocytes in vitro6. However, challenges remain related to the efficiency of cardiac differentiation and the functional integration of converted cells7. Additionally, concerns about immune compatibility and the risk of tumor formation persist8.
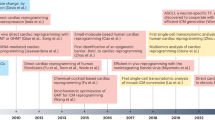
Recent advancements in the direct reprogramming of somatic cells into functional cardiomyocytes, bypassing the pluripotent state, offer new opportunities for obtaining cardiomyocytes from various sources9. Reprogramming of somatic fibroblasts into cardiomyocyte-like (CM-like) cells can be achieved by overexpressing cardiac genes, both in vivo and in vitro10,11,12,13. The discovery of fibroblast transdifferentiation into myocardial cells can be traced back to Yamanaka’s finding that exogenous transcription of Oct4, Sox2, Klf4, and c-Myc can induce the transdifferentiation of fibroblasts into pluripotent stem cells14. As research on this topic progressed, scientists discovered that the exogenous introduction of related transcription factors could promote the transdifferentiation of somatic cells into other cell types without the need to pass through a pluripotent stage. In the field of heart regeneration, scientists have reported that forced expression of myocardial cell-related transcription factors (Gata4, Mef2c, and Tbx5, GMT) in fibroblasts can promote their direct transdifferentiation into myocardial cells15. Related studies have shown that the efficiency of the GMT method for transdifferentiating cardiac fibroblasts into myocardial cells is relatively low, and the induced myocardial cells are morphologically different from endogenous myocardial cells, with lower signaling efficiency and an inability to form good end-to-end contacts with surrounding myocardial cells11,16. Previous studies also indicated that adult cardiac fibroblasts have some tolerance to exogenous Gata4, Mef2c, and Tbx5, resulting in low transdifferentiation efficiency, and that the transdifferentiated myocardial cells are in a relatively immature state with weak beating performance16. In addition, reprogramming of somatic fibroblasts via genetic manipulation carries a high risk of causing retrovirus-related insertional mutagenesis and genetic/epigenetic aberrations, limiting the clinical application of such approaches17,18,19,20,21,22,23. In comparison, chemical reprogramming of somatic fibroblasts using small molecules has emerged as a better alternative and has attracted significant attention in recent research24. Chemical reprogramming uses small molecules to modulate endogenous factors in the starting cells, eliminating the need to target cell-type-specific proteins25,26,27,28,29. This approach offers several advantages, including ease of manipulation, efficient cellular delivery, greater temporal control, non-immunogenicity, and cost-effectiveness, making it more suitable for clinical development30. Moreover, the reprogramming process can be finely tuned by adjusting the concentrations and combinations of small molecules used19,31.In 2013, Deng et al. successfully reprogrammed mouse somatic cells via complete chemical induction. The induced pluripotent stem cells (iPSCs) obtained through this method are known as chemically induced pluripotent stem cells (CiPSCs)32. The discovery of CiPSCs technology circumvents the need to introduce exogenous genes, thereby reducing the associated safety risks and increasing the suitability of the obtained cells for further development and clinical application. In 2016, Cao et al. used full small-molecular compounds to induce the reprogramming of human foreskin fibroblasts into cardiomyocytes29. Subsequently, in 2023, Cao et al. developed another xeno-free and full chemical induction method to reprogram human foreskin fibroblasts into expandable cardiovascular progenitor cells25. Moreover, these cardiovascular progenitor cells were demonstrated to have very good therapeutic effects in the context of myocardial infarction in mice, which verifies the promise of using a fully chemical induction system to develop advanced cell therapies. Currently, fibroblasts and mesenchymal stem cells are the main cell types used for transdifferentiation2,11,25,33,34. Although these cells are present in human body, the invasive extraction process needed for their isolation poses challenges for repeated sampling, limiting large-scale industrial application and impeding widespread clinical adoption. In contrast, the use of human urine cells (hUCs) for transdifferentiation offers unique advantages, including non-invasive collection from the patient and a painless and inexpensive extraction process35. These cells can also be collected repeatedly, eliminating the limitations of donor cells. Most importantly, urine cells collected from the patient reduce the risk of immune rejection and provide an ideal foundation for reprogramming36,37.
In this study, we demonstrate the feasibility of using hUCs as a viable source for generating cardiomyocyte-like cells. Reprogramming of hUCs into cardiomyocytes is realized by using small molecule cocktails in xeno-free conditions. As far as we are aware, our findings reveal a new, autologous, and scalable cardiac cell source for regenerative therapies and cardiac repair, without the need for foreign genetic materials.
Methods
Isolation of urine cells from human urine
To isolate cells from urine, fresh urine samples (average amount of 50 ml per sample, four subjects) were immediately transferred to the laboratory under sterile conditions at 4 °C. Each sample was centrifuged at 500 × g for 5 min, and the cell pellets were gently resuspended in sterile phosphate buffer saline (PBS) solution. After the cell suspension was centrifuged at 500 × g for 5 min, the cell pellets were resuspended in 3 ml of medium composed of 1:1 mixture of DMEM/F12 (ThermoFisherScientific) and keratinocyte serum free medium (KSFM, ThermoFisher Scientific), containing 5% fetal bovine serum (FBS; ThermoFisher Scientific) and 1% penicillin/streptomycin (Welgene, Deagu, Korea). The cells were seeded (1 × 104 cells/well) onto 24-well plates (Falcon, USA), and incubated at 37 °C in a 5% CO2 and air humidified incubator (Heraeus HeraCell 150, Thermo). Culture medium was changed every two days until the cells formed colonies. Each colony was transferred to individual wells of 24-well plate and cultured. The cells were split when they reached 70–80% confluency. Individuals who provided their urine samples did so with full awareness and agreement, as documented by signed informed consent forms.
Cell culture
hUCs were seeded at 1 × 104 cells/well in 6-well culture plates. hUCs were maintained in hUCs culture medium (DMEM/F12:keratinocyte SFM (1:1, v/v, ThermoFisher Scientific) medium containing 10% FBS (ThermoFisher Scientific), 1% penicillin/streptomycin, 10 ng/mL EGF(sigma)). The cells were incubated in a humidified incubator with 5% CO2. All cell lines used in this study, including human umbilical cord stem cells (hUCs) and derived human cardiac-induced cardiomyocytes (hCiCMs), were routinely tested for mycoplasma contamination to ensure culture integrity. Additionally, cell authentication was conducted to verify the identity of hUCs prior to differentiation. Short tandem repeat (STR) profiling was performed using the PowerPlex 16 System (Promega) and compared against reference profiles to confirm cell line authenticity. All procedures were carried out in accordance with established laboratory protocols to maintain the quality and reliability of cell cultures.
The hiPSCs were obtained from the Stem Cell Platform of the Shanghai Institute of Biochemistry and Cell Biology, Chinese Academy of Sciences. All studies involving these cell lines were conducted in compliance with the ethical guidelines and regulations approved by the Ethics Review Committee of the Sixth People’s Hospital of Shanghai. The cells were cultured under standard conditions for induced pluripotent stem cells, maintained in a humidified incubator at 37 °C with 5% CO2. They were grown on Matrigel-coated plates in a defined, feeder-free medium suitable for iPSCs, with daily medium (StemFit 03 Kit) changes. The cells were passaged every 4–5 days using a gentle dissociation reagent to preserve their undifferentiated state.
Small molecule libraries
To induce cardiac reprogramming of human fibroblasts, a collection of 100 small molecules known to facilitate reprogramming was initially screened (Supplementary Data 1). Small molecules in these libraries were purchased from Sigma, Tocris Bioscience, Merck, Cayman, Selleckchem, and Stemgent.
Chemical induction of CMs from human urine cells
hUCs were seeded onto 12-well, matrigel-coated plates at a density of 10,000 cells/well in hUCs culture medium. When cells achieved 80–90% confluence (usually about 3–4 d after seeding, daily monitoring is necessary) (day 0), the medium was replaced with chemical reprogramming medium 4 (CRM4) (knockout DMEM(Gibco), 2% xenofree B27 supplement without insulin (Gibco), 10% knockout serum replacement (Gibco), 500 ug/mL human serum albumin (oryzogen), 200 ng/mL bFGF (R&D), 50 /mL Lascorbic acid 2-phosphate (Sigma), 0.1 mM β-mercaptoethanol (Sigma), 2 mM Glutamax(Gibco), and 1% nonessential amino acids(Gibco)) containing the small-molecule cocktail 15 C. This medium was renewed every 2 days. During each medium change, gently rock the plate back and forth to get cell debris into suspension, ensuring that the cell debris will be discarded via aspiration. After 20 days, the cells were washed twice with phosphate-buffered saline (PBS), and the medium was changed to chemical reprogramming medium 5 (CRM5) (low-glucose DMEM(Gibco), 1% xenofree B27 supplement (Gibco), 2 mM Glutamax(Gibco), 0.1 mM β-mercaptoethanol (Sigma), 50 μg ml−1 Lascorbic acid 2-phosphate (Sigma), 500ug/mL human serum albumin (oryzogen), 4 mM DL- lactate (Sigma)) containing the small-molecule cocktail 15 C. This medium was renewed every 2 days. After 30 days, the cells were dissociated into single cells by triple Express (Gibco) and then replated onto 12-well Matrigel (Corning, 354277)-coated plates at a density of 500,000 cells/well and incubated in cardiac maintain medium (CMM) containing RPMI 1640(Gibco), 2% xeno-free B27 supplement (Gibco), 2 mM Glutamax (Gibco), 50 μg/mL Lascorbic acid 2-phosphate, 500 ug/mL human serum albumin (oryzogen), and 1% nonessential amino acids (Gibco). The medium was changed every 2 days. Unless indicated otherwise, all cytokines were of human origin.
Chemical reprogramming medium 1 (CRM1) contains high-glucose DMEM(Gibco), 5% FBS(Gibco), 1% insulin-transferrin-sodium selenium (Sigma), 10% knockout serum replacement(Gibco), 50/mL Lascorbic acid 2-phosphate (Sigma), 0.1 mM β-mercaptoethanol (Sigma), 2 mM Glutamax(Gibco), and 1% nonessential amino acids(Gibco). Chemical reprogramming medium 2 (CRM2) contains knockout DMEM(Gibco), 1% insulin-transferrin-selenium(Gibco), 10% knockout serum replacement(Gibco), 10 ng/mL bFGF (R&D), 50/mL Lascorbic acid 2-phosphate (Sigma), 0.1 mM β-mercaptoethanol (Sigma), 500 μg/mL human serum albumin(oryzogen), 2 mM Glutamax(Gibco), 1% lipid mixture (Gibco), and 1% nonessential amino acids(Gibco). Chemical reprogramming medium 3 (CRM3) contains DMEM/F12(Gibco), 1% insulin-transferrin-sodium selenium (Gibco), 10% knockout serum replacement(Gibco), 50/mL Lascorbic acid 2-phosphate (Sigma), 0.1 mM β-mercaptoethanol (Sigma), 500 μg/mL human serum albumin(oryzogen), 2 mM Glutamax(Gibco), 1% lipid mixture (Gibco), and 1% nonessential amino acids (Gibco).
Flow cytometry analysis
hCiCMs were dissociated with TrypLE Express (Gibco) and washed with phosphate-buffered saline (PBS). Cells were then fixed in 4% paraformaldehyde (PFA) for 10 min, permeabilized with 0.1% Triton X-100 for 10 min, and incubated with 1:200 mouse anti-cTnt (Invitrogen) at 4 °C overnight. Secondary staining was performed with a secondary antibody conjugated to Alexa Fluor 488 (1:1000; Invitrogen) for 1 h at room temperature. Samples were analyzed with an ACEA NovoCyte flow cytometer.
Quantitative real-time polymerase chain reaction (qRT-PCR) analysis
Total mRNA was isolated using TRIzol (Invitrogen), and 1 μg mRNA was used to synthesize cDNA using the PrimeScript RT Master Mix reagent kit (Takara) according to the manufacturer’s protocol. Real-time PCR was performed using 2× SYBR Green qPCR Master Mix (Biotool) and a Stratagene Mx 3000 P thermal cycler. Samples were normalized using GAPDH as a housekeeping gene. The sequences of the primers are listed in Supplementary Data 4.
Immunofluorescent staining
Immunofluorescence staining analysis was performed as described. Briefly, to detect intracellular markers, cells were fixed with 4% paraformaldehyde, permeabilized with PBS containing 0.3% (v/v) Triton X-100 (Sigma), and blocked with 3% IgG-free bovine serum albumin (BSA, Solarbio) in PBS with 0.3% Triton X-100. Then, cells were incubated with primary antibodies at 4 °C overnight and stained with isotype-matched secondary antibodies conjugated with Alexa-488, Alexa-549, or Alexa-647 (Life Technologies; 1:1000). Nuclei were counterstained with Hoechst 33342 (Sigma-Aldrich). Images were captured by an Olympus FV10i confocal microscope.The following antibodies were used: Gata4 (Clone: G-4, sc-25310, Santa Cruz Biotechnology; 1:400); Mef2c (Clone: D80C1, 5030, Cell Signalling Technology; 1:200); Nkx2–5 (Clone: A-3, sc-376565, Santa Cruz Biotechnology; 1:50); cTnT (Clone: 13–11, MA5-12960, Thermo; 1:500); cTnI (Clone: H-170, sc-15368, Santa Cruz Biotechnology; 1:400); MLC2v (Clone: Polyclonal, 10906-1-AP, ProteinTech Group; 1:200); α-actinin (Clone: EA-53, A7732, Sigma; 1:1000).
Transmission electron microscopy (TEM)
On Day 60, hCiCMs were detached by TrypLE Express (Gibco) and centrifuged into pellets. The cell pellet was washed in PBS 3 times and fixed with 2.5% glutaraldehyde for 2 h. Then, the pellet was washed again, then fixed in 1% osmium tetroxide, followed by dehydration in acetone, and finally embedded in epoxy resin (EPON). Next, 70 nm thin sections, cut with a diamond knife, were mounted on copper slot grids coated with Formvar. Subsequently, these sections were stained with uranyl acetate and lead citrate for following examinations on a Talos L120C transmission electron microscope at 120 kV.
Patch-clamp recording
On Day 60, hCiCMs were dissociated with TrypLE Express (Gibco) and replated at a density of 100,000 cells per well on a 24-well plate with glass cover slips coated with Matrigel. Patch-clamp recording was performed in a temperature-controlled room (approximately 37 °C). The Giga-Ohm seal was achieved under voltage-clamp mode, and the action potentials (APs) were recorded under the current-clamp configuration using a Multiclamp 700B (Axon, USA). The pipette solution contained 140 mM KCl, 1 mM MgCl2, 10 mM EGTA, and 10 mM HEPES (pH 7.2 with KOH). During the recording process, constant perfusion of extracellular solution was maintained using a BPS perfusion system (ALA Scientific Instruments, USA). The extracellular solution contained 140 mM NaCl, 5 mM KCl, 1 mM CaCl2, 1.25 mM MgCl2, 10 mM HEPES and 10 mM glucose (pH 7.4 with NaOH). Signals were filtered at 1 kHz and digitized using DigiData 1440 with pClamp9.2 software (Molecular Devices, USA).
Intracellular Ca2+ measurement
To record calcium transients, the hCiCMs were incubated with 2 μM Fluo-4 AM in cell culture medium at 37 °C for 30 min. After removing excess dye in the medium, spontaneous Ca2+ transients were recorded at 37 °C using a high-resolution living cell imaging system (GE Healthcare, USA). The recording lasted for at least 30 s for each field. The peak time and decay time of each beat were recorded and analyzed with Prism 9.0.1 (GraphPad Software, USA).
Single-cell RNA sequencing (scRNA-seq)
The cells were collected by trypsinization. The ascites samples went through filtering by 40-micron sterile strainers and were centrifuged at 350 × g for 5 min. Then the supernatant was discarded, and the sediment was resuspended in 1 ml PBS (HyClone). Finally, the samples were stained with Trypan Blue, and the cell viability was evaluated microscopically. Single-cell suspensions (2 × 105 cells/mL) with PBS (HyClone) were loaded onto microwell chip using the Singleron Matrix® Single Cell Processing System. Barcoding beads are subsequently collected from the microwell chip, followed by reverse transcription of the mRNA captured by the Barcoding Beads and to obtain cDNA, and PCR amplification. The amplified cDNA is then fragmented and ligated with sequencing adapters. The scRNA-seq libraries were constructed according to the protocol of the GEXSCOPE® Single Cell RNA Library Kits (Singleron)38. Individual libraries were diluted to 4 nM, pooled, and sequenced on Illumina Novaseq 6000 with 150 bp paired end reads. 0oiRaw reads were processed to generate gene expression profiles using CeleScope v1.5.2 (Singleron Biotechnologies) under default settings. Briefly, Barcodes and UMIs were extracted from R1 reads and corrected. Adapter sequences and poly A tails were trimmed from R2 reads, and the trimmed R2 reads were aligned against the Homo_sapiens_ensembl_92 transcriptome using STAR(v2.6.1b). Uniquely mapped reads were then assigned to exons with FeatureCounts(v2.0.1). Successfully Assigned Reads with the same cell barcode, UMI and gene were grouped together to generate the gene expression matrix for further analysis.
Quality control, dimension-reduction, and clustering
Scanpy v1.8.1 was used for quality control, dimensionality reduction, and clustering under Python 3.7. For each sample dataset, we filtered expression matrix by the following criteria: 1) cells with gene count less than 200 or with top 2% gene count were excluded; 2) cells with top 2% UMI count were excluded; 3) cells with mitochondrial content \( > \)20% were excluded; 4) genes expressed in less than 5 cells were excluded. The raw count matrix was normalized by total counts per cell and logarithmically transformed into normalized data matrix. Top 2000 variable genes were selected by setting flavor = “seurat”. Principle Component Analysis (PCA) was performed on the scaled variable gene matrix, and top 20 principle components were used for clustering and dimensional reduction. Cell clusters were visualized by using Uniform Manifold Approximation and Projection (UMAP)39.
Differentially expressed genes (DEGs) analysis
To identify differentially expressed genes (DEGs), we used the scanpy.tl.rank_genes_groups() function based on Wilcoxon rank sum test with default parameters, and selected the genes expressed in more than 10% of the cells in either of the compared groups of cells and with an average log (Fold Change) value greater than 1 as DEGs. Adjusted p-value was calculated by Benjamini-Hochberg correction, and the value 0.05 was used as the criterion to evaluate the statistical significance.
Pathway enrichment analysis
To investigate the potential functions of reprogramming cells, Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) analysis were used with the “cluster Profiler” R package v 3.16.140. Pathways with p_adj value less than 0.05 were considered as significantly enriched. Selected significant pathways were plotted as bar plots. Gene Ontology gene sets including molecular function (MF), biological process (BP), and cellular component (CC) categories, were used as reference.
Cell-type recognition with cell-ID
The cell type identification of each cluster was determined according to the expression of canonical markers from the reference database SynEcoSysTM (Singleron Biotechnology). SynEcoSysTM contains collections of canonical cell type markers for single-cell seq data, from CellMakerDB, PanglaoDB, and recently published literatures41.
Cell cycle analysis
Cell Cycle score of each cell was calculated using the Cell Cycle Scoring function implemented in the Seurat v 3.1.2 package42.
UCell gene set scoring
Gene set scoring was performed using the R package UCell v 1.1.043. UCell scores are based on the Mann-Whitney U statistic by ranking query genes in order of their expression levels in individual cells. Because UCell is a rank-based scoring method, it is suitable to be used in large datasets containing multiple samples and batches.
Measurement of human cytokines
300,000 hUCs-derived hCiCMs were plated onto a well of a 24-well plate. The supernatant was collected after 2 days of culture (N = 3). Human cytokines from the hUCs-derived hCiCMs in each well were measured using the VEGF assay kit (Multi Sciences, EK183EGA) following the manufacturer’s protocol.
Mice
NOD-SCID-beige (CBySmn.CB17-Prkdcscid/J) were purchased from The Jackson Laboratory. The number of animals per experimental group is presented in each figure. Mice received humane care in compliance with the Guide for the Principles of Laboratory Animals. Animal experiments were approved by the Shanghai Sixth People’s Hospital Affiliated to Shanghai Jiao Tong University School of Medicine Institutional Animal Care and Use Committee and performed according to local guidelines. In our research, we utilized mouse models across four distinct experiments to validate our findings. The primary experiment, presented in Fig. 5, constructed an MI model using two groups: a vehicle-treated group with 7 mice and a cell-injected group with 8 mice. These sample sizes were carefully selected based on previous studies and statistical requirements to ensure reliable and significant outcomes. In a supplementary experiment (Fig. S10), we tracked luciferase-labeled cells in the hearts of 3 mice to assess retention time, opting for a smaller cohort for initial method validation. Similarly, a tumorigenicity study involving 3 mice provided a preliminary evaluation of tumor formation potential. Additionally, Fig. S11 explored the impact of non-cardiomyocyte injections on cardiac function in MI mice, using another group of 3 mice for early verification of results. We applied rigorous inclusion and exclusion criteria across all experiments. Only healthy mice meeting predefined experimental standards were included, while those that died during surgery were excluded to uphold ethical and scientific integrity. No other animals, experimental units, or data points were omitted, and the exact number of surgery-related exclusions will be confirmed from our records. Randomization was employed to allocate mice to different groups. Specifically, mice were randomly assigned to either the cell-injected group or the vehicle group using a double-blind randomization procedure. Cage locations were systematically rotated to control environmental influences, and measurements were conducted at consistent times to avoid diurnal variations. Experimenters were blinded during data collection to prevent measurement bias. These strategies comprehensively addressed all key confounders, including treatment order, measurement timing, and animal/cage location, ensuring none were left uncontrolled. Male mice were exclusively used for all experiments. This choice was made to eliminate the potential confounding effects of estrogen, which is present in female mice and known to influence cardiovascular physiology. By using only male mice, we ensured consistency and reduced variability in results, aligning with common practices in cardiovascular research. All procedures adhered strictly to animal ethics guidelines and standardized protocols.
Mouse MI model
Permanent ligation of the left anterior descending coronary artery (LAD) in the left ventricle was conducted on 12-week-old NOD scid gamma mice. The mice were anesthetized using a mixture of 2.4% isoflurane and 97.6% oxygen and placed in a supine position. Thoracotomy was performed at the third intercostal space, and self-retaining micro-retractors were inserted to separate the third and fourth ribs, allowing for visualization of the LAD. Surgical ligation of the LAD was performed 1.5 mm distal to the left atrial appendage, carefully avoiding damage to the pericardial sac. Following ligation, the retractors were removed, and the chest cavity was closed.
Measurement of scar area
The fibrotic scar formation in the hearts after myocardial infarction (MI) was visualized by trichrome staining of cryosections with a Masson’s trichrome staining kit (Sigma, HT15–1) in accordance with the manufacturer’s instructions. The scar size was measured using ImagePro software, and the scar area (stained blue) was distinguished from the healthy area (stained red) on transections taken at four levels spanning from the ligation site to the apex of the heart. The distance between adjacent levels was approximately 0.5 mm, with the first level starting just below the ligation. Three slides of heart tissue were measured at each level, resulting in a total number of 15 sections per heart.
Echocardiography
All mice were lightly anesthetized by 1.5-3% isoflurane inhalation. Heart function was evaluated by transthoracic echocardiography using a Vevo 2100 instrument, and data were analyzed with Vevo 2100 software package. Echocardiography, performed 2–3 days post MI, demonstrated a significant reduction in ejection fraction before cell transplantation. Echocardiography was also performed 4 weeks after cell transplantation.
Quantitative analysis of cell engraftment and retention in mice
hUCs-derived hCiCMs/Venus-luciferase were generated by transduction with pCSII-EF-dVenusLuc2, a lentiviral vector encoding Venus and luciferase. These hUCs-derived hCiCMs/Venus-luciferase were transplanted into the hearts of NOD mice (N = 3). The mice received intravenous administration of luciferin (200 mg/kg BW). Bioluminescence imaging was captured immediately after luciferin administration using the AniView 100 system.
Tumorigenicity assay
The HiPSC H1 line (2 × 106 cells/100 μl/administration) and hUCs-derived hCiCMs (2 × 106 cells/100 μl/administration) were resuspended in DMEM (Gibco, 11960-044) and subcutaneously injected into NOD mice, respectively. At the end of the experiment, the mice were euthanized and dissected. The skin tissue and subcutaneous space, particularly at the transplantation site, were carefully inspected.
Swine MI model
All animal experiments adhered to the Guide for the Principles of Laboratory Animals and were approved by the Institutional Animal Care and Use Committee (IACUC) of the Shanghai Sixth People’s Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, ensuring humane care and compliance with local guidelines. Male Bama miniature pigs (10–15 kg) were selected to establish a swine myocardial infarction (MI) model via chemical glue occlusion, as previously described44, with the exclusive use of males eliminating potential estrogen-related confounding effects. Rigorous inclusion and exclusion criteria were enforced: only healthy pigs meeting predefined standards were included, while those dying during surgery or exhibiting illness were excluded, with exact surgery-related exclusion numbers available in our records; no additional animals, experimental units, or data points were omitted. Pigs were randomly assigned to either the cell-injected or vehicle control group using a double-blind randomization procedure, with pen locations systematically rotated and measurements timed consistently to control environmental and diurnal variations. At week 1 post-MI, a second thoracotomy exposed the infarction site, where human chemically induced cardiomyocytes (hCiCMs) were injected into the myocardial layer of the test group at 2 × 10^6 cells/kg (0.1 mL per point, 15 points per animal) using a microinjector, while the control group received solvent alone. Post-injection, the pericardium was sutured, and the chest closed in layers. To mitigate immune rejection, immunosuppressants were administered three days pre- and post-intervention: intravenous cyclosporine at 8 mg/kg (pre-administration) and 5 mg/kg (post-administration), adjusted for body surface area, alongside oral mycophenolate mofetil (500 mg/day) and prednisone acetate (20 mg/day) mixed with feed. The number of animals per group is detailed in each figure.
Blinding
A double-blind randomization procedure was employed to allocate mice to treatment groups. A computer-based tool generated an independent randomization sequence, assigning mice to either the cell-injected group or the vehicle group with equal probability. Treatments were coded as “Treatment A” and “Treatment B,” and group assignments were concealed from all study personnel.
Statistics and reproducibility
Values are reported as the Means ± SD. P and calculated by Student’s t-test, P < 0.05 was considered statistically significant. All graphs were plotted with GraphPad Prism 9.0 software.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Chemical induction of spontaneously contracting cell clusters from hUCs
The detailed isolation procedure for hUCs is summarized in the Materials and Methods section. The cells obtained from the urine were small, compact, separated, and had a rice grain-like shape. They formed colonies within 5–7 days after initial seeding and grew larger at approximately day 14 (Fig. S1a). These colonies could be dissociated and cultured for several passages (data not shown). We initiated chemical induction of human cardiomyocyte-like cells (hCiCMs) from hUCs at passage 1 (Fig. S1b). Characterization of hUCs was performed before induction. Immunofluorescence results indicated that these hUCs expressed CD44, CD73, CD90, PAX8, and SSEA4, but did not express HLA-DR, CD34, or CD45 (Fig. S1c). The flow cytometry results revealed that hUCs did not express the cardiomyocyte marker CTNT (Fig. S1d). We also evaluated the effect of storage time on the yield of urinary cells after preservation at 4 °C. The results demonstrated that, as the storage time at 4 °C increased, the yield of urinary cells progressively decreased (Fig. S1e). To avoid the genetic insertion and carcinogenicity of cardiomyocytes generated by virus-based methods, we started with a combination of nine compounds (9 C, CHIR99021, A8301, BIX01294, AS8351, SC1, Y27632, OAC2, SU16F, and JNJ10198409) to reprogram hUCs into cardiomyocytes. This combination has been tested by Cao et al., who successfully induced cardiomyocytes from human somatic fibroblasts29. However, significant cell death occurred in our experiments, and beating clones were only observed in very few experiments (Fig. 1a). To increase the cell survival rate and improve reprogramming efficiency, we conducted a large-scale screening of 100 compounds related to stem cell regulation and epigenetics25,28,29,45 (Supplementary Data 1), and seven positive compounds were found to significantly increase the number of beating cell clusters and were added to the 9 C combination mentioned above (Fig. 1b). This updated 16 C combination significantly improved the cell survival rate during reprogramming. In particular, the Bmi1 inhibitor PTC209 greatly increased the number of clusters, whereas the other six compounds significantly improved the transdifferentiation efficiency. Next, we tried to identify the specific small molecule in 16 C that was critical for inducing hCiCMs by removing individual compounds from 16 C in subsequent experiments. The removal of CHIR99021, A8301, BIX01294, AS8351, Y27632, and OAC2 results in failure to induce beating clusters, whereas the removal of SC1 not only reduced cell death rate but also increased the number of beating clusters (Fig. 1c). We also assessed the impact of different basal media on induction efficiency (refer to the Materials and Methods). Compared with non-animal-derived additives, the original cardiac reprogramming medium (CRM1), which contains animal-derived components such as FBS and insulin-transferrin-sodium selenium, was less effective in improving consistency and reproducibility. Moreover, CRM5, a low-glucose medium that inhibits fibroblast proliferation, was found to reduce the number of contaminant cells and promote cardiomyocyte maturation. Furthermore, testing of various induction protocols with different basal media (Fig. 1d) revealed that Scheme 6 significantly increased the number of beating clusters (Fig. 1e). After performing different combinations and optimizations, we finalized a combination of 15 compounds (15 C) comprising CHIR99021, A8301, BIX01294, AS8351, Y27632, OAC2, SU16F, JNJ10198409, PTC209, AKT inhibitor, CX4945, SGC-CBP30, EPZ5676, Dorsomorphin, and SET2-IN-1 for hCiCMs induction; this combination was used as the standard induction protocol in subsequent experiments. With this standard 15 C induction protocol, the number of beating colonies steadily increased over time, reaching a plateau approximately day 30 (Fig. 1f). We conducted induced differentiation tests using urinary cells extracted from urine samples from three different donors, each with three independent collections, as starting cells for reprogramming. The reprogramming efficiency after approximately 30 days of differentiation ranged from 4.62% to 28.87% (Fig. S2a). Subsequently, we replaced the cells after 30 days and tested the optimal number of days for the addition of the appropriate purification medium. The testing protocol is shown in Fig. S2b. The results revealed that after approximately six days of purification, the cardiomyocyte purity exceeded 90% around day 60 (Fig. S2c). Finally, we established the induced differentiation protocol shown in Fig. 1g. The morphology of hCiCMs at passage 1 on day 30 of induction strongly resembled that of embryonic-stage cardiomyocytes (Fig. 1h, Supplementary Movie 2 and Supplementary Movie 3). Flow cytometry results showed that the induction efficiency of P0 on day 30 was about 15.08%, and after replating and purification, the efficiency increased to 96.67% on day 60 (Fig. 1i).
a A representative contracting cluster induced by 9 C on reprogramming day 30, n = 3. See also Supplementary Movie 1. Scale bars, 200 µm. b Screening for compounds promoting for contracting clusters induction. Number of beating clusters at day 30 is shown. Data are means ± SD, n = 3. *P < 0.05; **P < 0.01;***P < 0.001. Exact p-values are provided in a file named Supplementary Data 5. c Screening for compounds essential for contracting clusters induction. Number of beating clusters on day 30 are shown, n = 3. Exact p-values are provided in a file named Supplementary Data 5. d Schemes of different combinations of different reprogramming mediums. e Induction of beating clusters with 15 C under different schemes, n = 3. f Induction of beating clusters with 15 C under scheme 6 on different day, n = 3. g The scheme of direct cardiac reprogramming from hUCs with small molecule cocktails. hUCs are plated in urine cell growth medium for one day, and then the medium is changed into cardiac reprogramming medium (CRM) containing the small molecule cocktails. On day 30, the medium was changed into cardiomyocyte-purified medium for 4 days. After purification, the medium was changed into cardiomyocyte-maintaining medium (CMM). The first beating clusters could be observed on day 15–20, n = 3. h Morphology of the representative contracting clusters induced by 15 C, n = 9. See also Supplementary Movie 2 and Supplementary Movie 3. Scale bars, 100 µm. i Flow cytometry analyses of the percentage of cTnt+ cells on day 30 and day 60. Dot plots represent data from 23,546 events for hCiCMs-P0 and 85,627 events for hCiCMs-P1. The gating strategy is detailed in Supplementary Fig. S3.
Structural and functional characterization of hCiCMs
To evaluate the differentiation status and functional properties of hCiCMs, immunofluorescence techniques were used to detect the expression of cardiomyocyte-specific markers in hCiCMs. The immunofluorescence staining results revealed that the hCiCMs significantly expressed various cardiomyocyte markers, including cardiac troponin T (cTnT), GATA4 (a transcription factor crucial for cardiac development), cardiac troponin I (cTnI), and Nkx2.5 (a cardiac-specific transcription factor), indicating successful differentiation of hUCs into cardiomyocytes (Fig. 2a). Additionally, the ultrastructure of the hCiCMs was examined in detail via transmission electron microscopy (TEM). The TEM images revealed the presence of linear Z bands within the hCiCMs (Fig. 2b). Z bands represent the typical structure in cardiomyocytes; they are located at the junctions between adjacent sarcomeres and are responsible for connecting the sarcomeres, ensuring the uniform transmission of force during myocardial contraction. Therefore, the well-aligned Z bands observed in the TEM images indicated that these hCiCMs possess the structural characteristics of mature cardiomyocytes. Moreover, numerous oval and round electron-dense structures in the TEM images indicated the abundance of mitochondria within the hCiCMs (Fig. 2b). Mitochondria are vital energy production centers in cardiomyocytes, providing ATP to meet the high energy demands during cellular contraction and other metabolic activities. The observed abundance of mitochondria suggested that the hCiCMs may be highly metabolically active, showing a high degree of similarity to mature cardiomyocytes. To gain a deeper insight into these hCiCMs, quantitative PCR (qPCR) was also performed to analyze the gene expression profile of the hCiCMs comprehensively. As shown in the qPCR results, the hCiCMs did not express pluripotency genes (Oct4 and Nanog) and presented very low expression levels of the mesodermal marker gene T, indicating their full differentiation from a stem cell state (Fig. 2c). We were intrigued by the observation that many colonies or cell patches formed before the initiation of beating and examined whether the generation of hCiCMs went through an iPSC stage as previously reported. Quantitative RT-PCR analysis revealed that the expression of pluripotency genes such as Oct4, Sox2, Nanog, and Rex1 remained very low during 15C-mediated cardiac reprogramming (Fig. S7a). In addition, the hCiCMs exhibited significant expression of multiple cardiomyocyte-specific genes, which are essential for cardiac functions, such as cardiomyocyte differentiation, development, contractile function, signal transduction, electrical activity, calcium signaling, and metabolic regulation (Fig. 2c). We conducted immunofluorescence staining for the proliferation markers Ki67 and EdU on cells on day 60 of reprogramming and performed statistical analysis. The findings demonstrated that ~15–20% of cTnT-positive cells expressed the proliferation markers Ki67 and EdU (Fig. S4a, b). Furthermore, we assessed hCiCMs on days 30, 45, 60, and 90 of differentiation using immunofluorescence staining for the myocardial-specific sarcomere marker cTnT (Fig. S4c). The fluorescence intensity was then quantified for each cell, with the fluorescence intensity on day 30 serving as the baseline (set to 1) for comparison. The results revealed that the fluorescence intensity increased from day 30 to day 60, with the fluorescence values reaching a plateau after day 60 (Fig. S4d).
a Immunofluorescence analyses of CM markers, n = 3. Scale bars, 50 µm. b Transmission electron microscopy images of hCiCMs derived from hUCs at day 60, n = 3. MF myofibrils, Z Z-bands, Mit mitochondria. c RT-qPCR analysis of mRNA levels of genes related to pluripotency markers, cardiac structure, ion channels, and mitochondrial functions of hCiCMs derived from hUCs on day 60, n = 3. d Representative action potentials (AP) of hCiCMs derived from hUCs on day 60, n = 15. Em, membrane potential in millivolts. e AP parameters of hCiCMs including AP frenquency, AP amplitude (APA), minimum diastolic potential (MDP), AP durations (APDs) at the level of 30% (APD30), AP durations (APDs) at the level of 50% (APD50) and 90% repolarization (APD90), n = 15. Data are means ± SD. f Representative calcium flux in human cardiac-induced cardiomyocytes (hCiCMs) derived from human umbilical cord stem cells (hUCs) at day 60 of induction, n = 6. g Measurement of the maximum calcium transient amplitude, maximum upstroke velocities, and maximum decay velocities of calcium transients in hCiCMs derived from hUCs on day 60 of induction (n = 6). Data are presented as means ± SD.
Action potential (AP) measurements were conducted on hCiCMs to eliminate the possibility of myoblast or smooth muscle contamination, which might result in similar calcium transients and contractility. In single-cell patch clamp assays, APs were recorded from spontaneously beating cells at approximately day 60 of reprogramming (Fig. 2d). Most of the hUCs-hCiCMs (n = 15) generated ventricular-like action potentials (APs), whereas a subset of the hUCs-hCiCMs (n = 4) exhibited atrial-like APs (Fig. 2d, e). Fluo-4 was used to trace the calcium transients underlying the contraction and relaxation of spontaneously beating cardiomyocytes in hCiCMs (Fig. 2f, g, and Supplementary Movie 4).
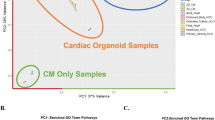
Single-cell RNA-seq analysis to identify cell types among reprogrammed cells derived from hUCs on day 60
By using single-cell transcriptomics analysis combined with UMAP dimensionality reduction, cell cluster identification, and gene function enrichment analysis, we systematically identified the gene expression profiles of the cells obtained after cardiomyocyte reprogramming. A total of 12,826 high-quality single cells were analyzed in this study, and the results are shown in Fig. 3. The UMAP plot (Fig. 3a) depicts the distribution of various cell clusters, including cardiomyocytes (CM1-CM6), fibroblasts, and neurons. The proportion of each cell cluster within the samples is depicted in Fig. 3b, with cardiomyocytes making up a significant portion of the cells (86.15% of the total cells). Specifically, CM1 comprises 25.48%, CM2 accounts for 19.87%, CM3 represents 10.62%, CM4 constitutes 10.59%, CM5 makes up 9.96%, and CM6 comprises 9.63% of the total cells. Fibroblasts represented 11.99% of the total cells, whereas neurons accounted for 1.86% (Fig. 3b). The CM1 cell cluster was characterized by high expression of the CEL, BANCR, and MYH7 genes, which are crucial for lipid metabolism and myocardial contraction. The CM2 cluster was characterized by high expression of the NPPB, ANKDR1, and ACTA1 genes, which are associated with cardiac function and muscle activity. The CM3 cluster highly expressed the PSMA4, BUD23, and TMEM106C genes, which are vital for protein turnover and ribosome biogenesis. The CM4 cluster was distinguished by high expression of the CDC6, FAM111B, and MCM10 genes, which are involved in DNA replication and cell cycle regulation. CM5 cells highly expressed the SHOX2, AC011365.1, and MYBPHL genes, which play significant roles in cardiac development, particularly during developmental stages and muscle maintenance. The CM6 cluster marker genes KIF20A, PTTG1, and PLK1 are closely linked to cell division and mitosis (Fig. S5).
a Uniform manifold approximation and projection (UMAP) delineate 8 clusters and 3 cell types in the reprogrammed cells derived from hUCs on day 60 (n = 3). b Distributions of different cell clusters populations. c Gene ontology analyses reveals the enriched terms of each cardiomyocytes clusters(CM1 and CM2). d UMAP analysis of UCell scores of overall cardiac gene expression of the 13-week embryonic stages matched with different cardiomyocyte clusters. e UCell scores of left/right ventricular and atrial gene expressions of different embryonic stages matched with different cardiomyocyte clusters.
Figures 3c, S6 show the results of gene ontology (GO) analysis of the six cardiomyocyte clusters (CM1-CM6), which differed in significantly enriched biological processes (BP), cell components (CC), and molecular functions (MF). CM1 showed enrichment of muscle contraction and regulation, including processes such as striated muscle contraction, with key components including sarcomeres, myofibrils, and contractile fibers, and key functions including myosin and actin binding. CM2 showed enrichment of muscle development and function, including muscle tissue development and myofibril assembly, with critical components including the myosin complex and sarcomeres, and functions including actin binding and calcium-dependent protein binding. CM3 showed enrichment of muscle structure and function, including muscle tissue development and heart contraction, with key components including sarcomeres and contractile fibers, and functions including actin filament binding. CM4 showed enrichment of DNA replication and cell cycle regulation, including processes such as DNA replication and the G1/S phase transition, and key components such as the replication fork and CMG complex, which are involved in helicase activity. CM5 showed enrichment of muscle function and development, including muscle tissue development and contraction, with components such as the sarcomere and collagen-containing extracellular matrix, and functions such as ion channel regulator activity. CM6 showed enrichment of cell division and chromosome organization, including mitotic nuclear division and chromosome segregation, with components such as the spindle and kinetochore and functions such as microtubule binding and kinase regulator activity (Figs. 3c, S6). To investigate the degree of maturity and cell types of the reprogrammed cardiomyocytes, we compared their expression data with single-cell sequencing data obtained during human embryonic heart development46. Comparative transcriptome analysis revealed that the hCiCMs clusters closely resemble the 13-week embryonic stage of human heart development (Fig. 3e and Supplementary Data 2). Further comparison of the U scores of cardiomyocytes from various regions and stages of human embryonic heart development revealed that CM1, CM2, and CM4 are most similar to the 13-week left ventricle, CM3 resembles the 7-week right ventricle, and CM5 and CM6 are most similar to the left atrium (Fig. 3e and Supplementary Data 3).
Analyses of oncogene and tumor suppressor gene (TSG) expression and cell cycle status in reprogrammed cells derived from hUCs on day 60
To investigate the expression profiles of oncogenes and tumor suppressor genes in reprogrammed hCiCMs, ONGene and TSGene DATABASE 2.0 were used. Uniform manifold approximation and projection (UMAP) visualizations were generated to display the distinct expression patterns of each cell cluster47,48. The UMAP visualizations revealed distinct expression patterns for both oncogenes and tumor suppressor genes (Fig. 4a). The TSGs presented relatively high U scores in CM1, CM2, CM4, and neurons, suggesting a robust mechanism to prevent carcinogenesis and maintain cellular homeostasis. In contrast, the oncogenes displayed higher U scores in CM6 and neurons, indicating increased oncogene expression in these cells. Boxplot analyses supported these findings, revealing significant variations in U scores among different cell types (Fig. 4b). Importantly, the CM groups consistently presented higher U scores for tumor suppressor genes than for oncogenes, suggesting that hCiCMs have an intrinsic safety mechanism favoring TSG expression, thus reducing the risk of carcinogenesis (Fig. 4b). This expression profile is highly favorable for the use of hCiCMs in cell therapy, suggesting a low likelihood of cancerous transformation post-transplantation. To elucidate the expression patterns of pluripotency genes during hCiCMs reprogramming, we analyzed the expression profiles of key stemness-associated genes. These genes, including NANOG, NR5A2, REX1, DPPA2, SOX2, POU5F1, KLF4, TDGF1, ESRRB, and MYC, are crucial for maintaining pluripotency and self-renewal in stem cells. Our analysis focused on expression levels across different cell types, including CM1 to CM6, neurons, and fibroblasts. The data revealed that NANOG, NR5A2, REX1, and DPPA2 were expressed at very low levels in the CM groups, indicating a significant reduction in iPS-related gene expression (Fig. S7b). Similarly, SOX2, POU5F1, KLF4, TDGF1, and ESRRB exhibited low expression levels in the CM groups, with MYC showing slightly higher but still low expression (Fig. S7c). These findings suggest that hCiCMs have low tumorigenicity and teratogenicity, enhancing their safety for use in potential therapeutic applications.
a UMAP analysis of overall oncogenes and tsgenes expression in the reprogrammed cells derived from hUCs on day 60 (n = 3). b UCELL scores of overall oncogenes and tsgenes expression of different cell type clusters in the reprogrammed cells derived from hUCs on day 60. c UMAP analysis of cell cycle status (n = 3). d UCELL scores of cell cycle related genes expression of different cell type clusters. e PCA of all single cells color-coded by cell-cycle states. f Comparison of the percentage of CCA and CCI in different cell types. CCA cell-cycle active, CCI cell-cycle inactive.
In terms of the cell phase, the CM1, CM2, and CM3 clusters were concentrated mainly in the G0/G1 phase, whereas the CM4, CM5, and CM6 clusters were distributed in the S and G2M phases (Fig. 4c). Neurons and fibroblasts showed similar distribution trends, with fibroblasts predominantly in the G0/G1 phase and neurons in the S and G2M phases (Fig. 4c). According to the cell cycle gene scores, the CM1, CM2, CM3, and CM5 clusters scored lower, indicating lower expression of cell cycle-related genes (Fig. 4d). Conversely, the CM4 and CM6 clusters scored higher, suggesting higher cell cycle activity (Fig. 4d). According to the PCA plot, the distributions of different cell populations at each stage were as follows: cells in the cell cycle inactive (CCI) stage were mainly concentrated in the high-value region of the PC1 axis, whereas those in the cell cycle active (CCA) stage were distributed more broadly (Fig. 4e). The CM1, CM2, CM3, and CM5 cell clusters were distributed in the low-value region of the PC1 axis, indicating lower activity; CM4 and CM6 were distributed in the high-value region, indicating higher activity. Neurons and fibroblasts exhibited decreased cell cycle activity (Fig. 4e). Hierarchical clustering (HC) analysis of the top 70 PCA genes revealed that the CM6 and CM4 cell populations presented the highest gene expression levels, with notable upregulation of cell cycle-related genes such as HMGB2, CDK1, and UBE2C (Fig. S8). In comparison, the CM1, CM2, CM3, and CM5 clusters, as well as neurons and fibroblasts, presented lower gene expression levels (Fig. S8). The fibroblast population was almost entirely in the CCI stage, with 100% of the total fibroblasts, indicating extremely low CCA activity (Fig. 4f). The neuron population was entirely in the CCA stage, with 100% of the total neurons, indicating high activity in the CCA stage (Fig. 4f). The hCiCMs population exhibited a mixed distribution, with 76.53% in the CCI stage and 23.47% in the CCA stage (Fig. 4f).
hCiCMs improve cardiac function after myocardial infarction (MI) in mice
We next investigated whether the generated hCiCMs could improve cardiac function in a chronic MI model. To test this hypothesis, we purposely induced cardiac injury via coronary artery ligation in 12-week-old immunodeficient mice. These MI model mice were divided into a treatment group and a vehicle group. One week after MI induction, a second thoracotomy was performed in the treatment group for the administration of hCiCMs (2 million per dose per mouse) (Fig. 5a). Echocardiographic evaluation, conducted 28 days after cell injection, revealed an improvement in cardiac systolic function (Fig. 5b). Specifically, the left ventricular ejection fraction (EF%) and left ventricular fractional shortening (FS%) were significantly improved in the hCiCMs-treated group compared to the vehicle control group on day 28 (Fig. 5c). Histological analyses via Masson staining revealed a significant reduction in fibrotic area in the hCiCMs-treated group compared with the vehicle control group (Figs. 5d, e, S9). Therefore, hCiCMs treatment not only significantly improved cardiac function but also effectively reversed fibrosis in a chronic MI model.
a Schematic drawing of the experimental procedure. Myocardial infarction (MI) was induced by LAD ligation. b Representative cardiac ultrasound images of baseline and 4 W in MI-NOD mice from vehicle control group and hCiCMs transplantation group. Mice were subjected to sham operation or MI by LAD ligation (sham = 4, vehicle = 7, hCiCMs = 8). c Evaluation of cardiac functions with echocardiography. Ejection fraction (EF), fractional shortening (FS), left ventricular volume at systole (LV vol, S), left ventricular volume at diastole (LV vol, d), and left ventricular mass(LV mass) were assessed in pre- and post-treatment mice. Statistical analysis was performed by two-tailed unpaired t test. Exact p values are provided in a file named Supplementary Data 5 (sham = 4, vehicle = 7, hCiCMs = 8). d Images of Masson trichrome staining of the heart sections (as presented in (c, d) (from the MI mice treated with hCiCMs or vehicle. Scale bar =1 mm. e Quantitative analysis of infarct size of (d). Statistical analysis was performed by two-tailed unpaired t test. Exact p values are provided in a file named Supplementary Data 5.
To further investigate the mechanisms underlying the therapeutic effects of hCiCMs, we examined their paracrine effects, specifically their secretion of VEGF, a key angiogenic factor49,50,51. The results demonstrated that as the culture period increased, the amount of VEGF secreted by the cells gradually increased. These findings suggest that hCiCMs may contribute to angiogenesis and enhance cardiac function by releasing angiogenic factors through paracrine signaling upon transplantation (Fig. S10a). Additionally, a significant increase in the number of micro vessels was observed at the edge of the injected cells (Fig. S10b, c). We also assessed the extent of hCiCMs engraftment post-transplantation. Prior to transplantation, we labelled the hCiCMs with luciferase and continuously monitored the luciferase signal in the mice following hCiCMs injection (Fig. S10d). The results revealed that, up to approximately day 28 post-injection, the luciferase signal remained at 30–50% of the baseline value (Fig. S10e). On the basis of these findings, we hypothesize that hCiCMs may engraft within the heart and supplement new myocardial cells, thereby enhancing myocardial contractility and overall heart function. To evaluate potential safety concerns, including the risk of tumor formation, we transplanted hCiCMs subcutaneously into NOD mice, with human pluripotent stem cells used as a positive control. The results indicated that the transplantation of hCiCMs did not lead to significant tumor formation (Fig. S10f).
To determine whether a small subset of noncardiomyocytes derived from reprogramming has the potential to repair cardiac function, we performed cell sorting on day 60 of reprogramming. The cells were infected with an AAV9 virus carrying the cTnT-promoter-GFP construct, with cardiomyocytes being GFP positive and noncardiomyocytes being GFP negative. By using flow cytometry, we differentiated cardiomyocytes (GFP-positive) and noncardiomyocytes (GFP-negative) and subsequently labelled the noncardiomyocytes with luciferase (Fig. S11a). These luciferase-labelled noncardiomyocytes were then transplanted into the hearts of myocardial infarction (MI) model mice. Luciferase fluorescence was tracked in vivo on days 0, 14, and 28 (Fig. S11b, c), and cardiac function was evaluated on day 28. The results indicated that the transplantation of noncardiomyocytes did not lead to significant improvements in cardiac function (Fig. S11d).
hCiCMs provide functional benefits in swine with ischemic heart injury
A swine ischemia model was established via chemical glue occlusion to simulate clinical scenarios, followed by hCiCMs administration (Fig. 6a). The success of the chemical glue occlusion surgery was confirmed by angiography (Fig. 6b, Supplementary Movie 5). Changes in heart condition were also reflected in the ECG results. During surgery, ST-segment elevation and hyperacute T waves were typical manifestations of acute ischemia (Fig. 6c), suggesting successful occlusion of the left anterior descending artery. The left ventricular (LV) ejection fraction and LV fractional shortening were measured via M-mode echocardiography to assess ventricular contractility (Fig. 6d). Overall, LV function in the hCiCMs group was better than that in the vehicle group (Fig. 6e), indicating the significant therapeutic efficacy of the cells. Additionally, hCiCMs treatment significantly reduced fibrotic tissue (Fig. 6f, g), suggesting that hCiCMs mitigate cardiac fibrosis and adverse remodeling following MI.
a Schematic showing the swine study design. b Angiography of swine during myocardial infarction surgery through chemical glue occlusion procedure. c Representative ECG during MI surgery. d Representative M-mode images of echocardiography measurement of cardiac function. e Evaluation of cardiac functions with echocardiography. Ejection fraction (EF), left ventricular fractional shortening (LVFS), left ventricular posterior wall in diastole (LVPWd), left ventricular posterior wall in systole (LVPWs), Interventricular septum in diastole (IVSd), and interventricular septum in systole (IVSs) were presented of swine treated with hCiCMs or vehicle (n = 4, exact p values are provided in a file named Supplementary Data 5). f Images of Masson trichrome staining of the heart sections from the MI swine treated with hCiCMs or vehicle (n = 4), Scale bar =5 mm. g Quantitative analysis of infarct size of h. Statistical analysis was performed by two-tailed unpaired t test. Exact p values are provided in a file named Supplementary Data 5.
With respect to the biosafety of hCiCMs in swine, all animals survived until the study’s endpoint (day 28), and no obvious abnormalities were noted following cell delivery. There was no significant difference in body weight between the vehicle-treated and cell-treated groups (Fig. S12a). In routine blood tests, as determined by several indices (white blood cell count, red blood cell count, hemoglobin, etc.), there were no notable differences between the vehicle- and cell-treated groups (Fig. S12b). In serum biochemical tests, liver and kidney function in the swine after cell treatment was not significantly different from that in the vehicle group (Fig. S12c), demonstrating a lack of side effects. Overall, hCiCMs treatment was safe in a clinically relevant large animal model, indicating high translational potential for cell therapy in clinical applications.
Discussion
Urine-derived cells are a rare adherent cell type that can be repeatedly collected in a noninvasive manner and subsequently expanded on a large scale in vitro, making them a promising source for cardiac regeneration therapies52,53. In contrast to other cell types, urine-derived cells are collected through a simple and noninvasive process, which is particularly advantageous in clinical settings where patient comfort and safety are paramount36,54. This noninvasive method permits multiple sample collections from the patient, allowing comprehensive evaluation and much better-quality control of the therapeutic cells. Furthermore, urine-derived cells exhibit robust proliferative capabilities in vitro, allowing large-scale cultivation for a variety of cell therapy applications, including cardiac repair. Additionally, urine-derived cells are autologous and avoid immune rejection associated with allogeneic transplantation55. Moreover, this personalized treatment can be customized to meet individual needs, improving the precision and effectiveness of therapy.
To optimize the chemical reprogramming efficiency, we incorporated the key compound PTC209 to significantly promote the transdifferentiation of hUCs into hCiCMs. Research has shown that pretreatment with PTC209 improves the efficiency of converting mouse embryonic fibroblasts (MEFs) and adult cardiac fibroblasts (CFs) into induced cardiomyocytes (iCMs)56. Additionally, studies have identified BMI1 as a significant epigenetic barrier during the initial stages of iCMs transdifferentiation57. Therefore, inhibiting BMI1 can alleviate the suppression of cardiac genes such as Gata457.
To further enhance the yield of hCiCMs following the initial transdifferentiation step, we employed a purification strategy utilizing a glucose-free medium supplemented with sodium lactate. This approach exploits the distinct metabolic profiles of cardiomyocytes compared to other cell types. Cardiomyocytes efficiently metabolize lactate by converting it into pyruvate, which subsequently enters the tricarboxylic acid (TCA) cycle to generate ATP. In contrast, many non-cardiomyocyte cells, including stem cells and fibroblasts, exhibit a strong dependence on glucose for energy production and exhibit reduced viability in its absence58. Consequently, in a glucose-deprived environment enriched with high lactate concentrations, non-cardiomyocyte cells undergo progressive cell death, while cardiomyocytes survive and proliferate, enabling effective purification. This purification step proves particularly valuable when initial transdifferentiation efficiency is suboptimal, as it allows for the enrichment of hCiCMs, achieving a higher proportion of cardiomyocytes by day 60.
The evidence suggests that hUC-derived hCiCMs are comparable to the developmental stage of a 13-week-old human embryo, exhibiting typical characteristics of cardiomyocytes, including the expression of cardiac-specific markers and spontaneous contractile function. Moreover, during the transdifferentiation process, the resulting cardiomyocytes form multiple subpopulations, with CM4 and CM6 demonstrating notable proliferative capacity. These findings suggest that the transdifferentiated cells could be expanded in vitro to provide sufficient quantity of cells for clinical applications.
.In myocardial infarction (MI) mouse and swine models, the transplantation of hCiCMs led to marked improvements in cardiac function and a significant reduction in cardiac fibrosis. These findings suggest that hCiCMs have a strong ability to promote myocardial repair and mitigate fibrotic tissue formation. Furthermore, the use of patient-specific urine-derived cells as a source for cardiomyocytes could increase integration rates and prolong retention. Compared with allogeneic cell transplantation, autologous cell transplantation can effectively circumvent immune rejection, enhancing cell survival and functional integration within the host tissue. This approach not only improves therapeutic outcomes but also reduces the need for long-term immunosuppressive therapy, thus lowering treatment costs and patient burden. Consequently, autologous urine-derived hCiCMs represent a promising strategy for the treatment of MI.
Despite these promising findings, our study has limitations that should be addressed in future research. The intrinsic molecular mechanisms underlying transdifferentiation have not been thoroughly elucidated. While chemical small molecules have been shown to induce the conversion of urine cells into cardiomyocytes, the specific molecular pathways and signaling mechanisms involved remain unclear. A deeper understanding of these mechanisms is crucial for optimizing the induction process, increasing the efficiency of hCiCMs conversion, and achieving greater functional maturity of hCiCMs. This will enable better control and regulation of the cell differentiation process, thereby yielding higher quality hCiCMs. Although the hCiCMs generated here exhibit some cardiomyocyte characteristics, their insufficient maturity may impact their integration and long-term functionality within the host tissue. Future research should focus on refining culture conditions or employing auxiliary factors to further increase the maturity of the hCiCMs, thus improving their therapeutic efficacy.
To the best of our knowledge, we present the first evidence of chemically mediated direct conversion of human urine-derived cells into cells of the cardiomyocyte lineage. This protocol for generating xeno-free chemically induced autologous cardiomyocytes represents a significant advancement in cardiac regenerative medicine. Fully chemical approaches are more suitable for clinical use, avoiding potential complications such as tumor formation, tissue rejection, and issues with the homing ability of injected cells in cell transplantation therapy for cardiac diseases. Compared with cardiomyocytes derived from patient-specific induced pluripotent stem cells, hUC-CiCMs provide a more expedited process and circumvent the necessity for multiple transformation stages. Consequently, the overall production cost of hUC-CiCMs is lower, rendering them a more cost-effective alternative. While hCiCMs are functionally comparable to pluripotent stem cell-derived cardiomyocytes, generating fully mature cardiomyocytes remains a critical challenge for cardiac regenerative therapies.
Data availability
All original data and materials used for this study are available from the corresponding authors upon reasonable request. The accession numbers for the single-cell RNA sequencing in this study are available in the NCBI GEO dataset. Single-cell RNA sequencing data: GSE272220. Additionally, the numerical data used to generate the figures in this study, including the source data for Figs. 1–6, are provided in the Supplementary Data files available at figshare: https://doi.org/10.6084/m9.figshare.29046968.
Abbreviations
- hUCs:
-
human urine cells
- hCiCMs:
-
chemical-induced human cardiomyocyte-like cells
- ESCs:
-
embryonic stem cells
- iPSCs:
-
induced pluripotent stem cells
- CM:
-
cardiomyocyte
- GMT:
-
Gata4, Mef2c, and Tbx5
- CiPSCs:
-
chemically induced pluripotent stem cells
- CRM:
-
cardiac reprogramming medium
- cTnT:
-
cardiac troponin T
- TEM:
-
electron microscopy
- qPCR:
-
quantitative polymerase chain reaction
- APs:
-
action potentials
- APA:
-
action potential amplitude
- APD:
-
action potential duration
- GO:
-
gene ontology
- BP:
-
biological processes
- CC:
-
cell components
- MF:
-
molecular functions
- TSGs:
-
tumor suppressor genes
- EF:
-
ejection fraction
- FS:
-
fractional shortening
- MEFs:
-
mouse embryonic fibroblasts
- CFs:
-
cardiac fibroblasts
- iCMs:
-
induced cardiomyocytes
- MI:
-
myocardial infarction
- DEGs:
-
Differentially expressed genes
- UMAP:
-
Uniform Manifold Approximation and Projection
- LAD:
-
left anterior descending coronary artery
- CCI:
-
cell cycle inactive
- CCA:
-
cell cycle active
References
Martin, S. S. et al. 2024 Heart Disease and Stroke Statistics: a report of US and global data from the American Heart Association. Circulation 149, e347–e913 (2024).
Chien, K. R. et al. Regenerating the field of cardiovascular cell therapy. Nat. Biotechnol. 37, 232–237 (2019).
van Berlo, J. H. et al. c-kit+ cells minimally contribute cardiomyocytes to the heart. Nature 509, 337–341 (2014).
Neidig, L. E. et al. Evidence for minimal cardiogenic potential of stem cell antigen 1-positive cells in the adult mouse heart. Circulation 138, 2960–2962 (2018).
Li, Y. et al. Genetic lineage tracing of nonmyocyte population by dual recombinases. Circulation 138, 793–805 (2018).
Hsiao, L. C., Carr, C., Chang, K. C., Lin, S. Z. & Clarke, K. Stem cell-based therapy for ischemic heart disease. Cell Transplant. 22, 663–675 (2013).
Liu, C., Han, D., Liang, P., Li, Y. & Cao, F. The current dilemma and breakthrough of stem cell therapy in ischemic heart disease. Front. Cell. Dev. Biol. 9, 636136 (2021).
Vagnozzi, R. J. et al. An acute immune response underlies the benefit of cardiac stem cell therapy. Nature 577, 405–409 (2020).
Xu, J., Du, Y. & Deng, H. Direct lineage reprogramming: strategies, mechanisms, and applications. Cell Stem Cell 16, 119–134 (2015).
Ieda, M. Direct reprogramming into desired cell types by defined factors. Keio. J. Med. 62, 74–82 (2013).
Bektik, E. & Fu, J. D. Production of cardiomyocyte-like cells by fibroblast reprogramming with defined factors. Methods Mol. Biol. 2239, 33–46 (2021).
Wada, R. et al. Induction of human cardiomyocyte-like cells from fibroblasts by defined factors. Proc. Natl. Acad. Sci. USA 110, 12667–12672 (2013).
Tani, H. et al. Direct reprogramming improves cardiac function and reverses fibrosis in chronic myocardial infarction. Circulation 147, 223–238 (2023).
Takahashi, K. & Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126, 663–676 (2006).
Ieda, M. et al. Direct reprogramming of fibroblasts into functional cardiomyocytes by defined factors. Cell 142, 375–386 (2010).
Wang, L. et al. Stoichiometry of Gata4, Mef2c, and Tbx5 influences the efficiency and quality of induced cardiac myocyte reprogramming. Circ. Res. 116, 237–244 (2015).
Li, J., Song, W., Pan, G. & Zhou, J. Advances in understanding the cell types and approaches used for generating induced pluripotent stem cells. J. Hematol. Oncol. 7, 50 (2014).
Barrachina, L., Arshaghi, T. E., O’Brien, A., Ivanovska, A. & Barry, F. Induced pluripotent stem cells in companion animals: How can we move the field forward. Front. Vet. Sci. 10, 1176772 (2023).
Yamakawa, H. Heart regeneration for clinical application update 2016: from induced pluripotent stem cells to direct cardiac reprogramming. Inflamm. Regen. 36, 23 (2016).
Lai, M. I. et al. Advancements in reprogramming strategies for the generation of induced pluripotent stem cells. J. Assist. Reprod. Genet. 28, 291–301 (2011).
Luo, T. A small-molecule approach towards the Fountain of Youth: chemically induced pluripotent stem cells. Natl. Sci. Rev. 9, nwac181 (2022).
Liu, Z., Zhou, J., Wang, H., Zhao, M. & Wang, C. Current status of induced pluripotent stem cells in cardiac tissue regeneration and engineering. Regen. Med. Res. 1, 6 (2013).
Jacobs, B. M. A dangerous method? The use of induced pluripotent stem cells as a model for schizophrenia. Schizophr. Res. 168, 563–568 (2015).
Budniatzky, I. & Gepstein, L. Concise review: reprogramming strategies for cardiovascular regenerative medicine: from induced pluripotent stem cells to direct reprogramming. Stem Cells Transl. Med. 3, 448–457 (2014).
Wang, J. et al. Reprogramming of fibroblasts into expandable cardiovascular progenitor cells via small molecules in xeno-free conditions. Nat. Biomed. Eng. 6, 403–420 (2022).
Huang, C., Tu, W., Fu, Y., Wang, J. & Xie, X. Chemical-induced cardiac reprogramming in vivo. Cell Res. 28, 686–689 (2018).
Fu, Y. et al. Direct reprogramming of mouse fibroblasts into cardiomyocytes with chemical cocktails. Cell Res. 25, 1013–1024 (2015).
Zhang, Y. et al. Expandable cardiovascular progenitor cells reprogrammed from fibroblasts. Cell Stem Cell 18, 368–381 (2016).
Cao, N. et al. Conversion of human fibroblasts into functional cardiomyocytes by small molecules. Science 352, 1216–1220 (2016).
Wang, J., Sun, S. & Deng, H. Chemical reprogramming for cell fate manipulation: Methods, applications, and perspectives. Cell Stem Cell 30, 1130–1147 (2023).
Li, X., Xu, J. & Deng, H. Small molecule-induced cellular fate reprogramming: promising road leading to Rome. Curr. Opin. Genet. Dev. 52, 29–35 (2018).
Hou, P. et al. Pluripotent stem cells induced from mouse somatic cells by small-molecule compounds. Science 341, 651–654 (2013).
Liuyang, S. et al. Highly efficient and rapid generation of human pluripotent stem cells by chemical reprogramming. Cell Stem Cell 30, 450–459 (2023).
Guan, J. et al. Chemical reprogramming of human somatic cells to pluripotent stem cells. Nature 605, 325–331 (2022).
Zhang, Y. et al. Urine derived cells are a potential source for urological tissue reconstruction. J. Urol. 180, 2226–2233 (2008).
Pavathuparambil, A. M. N., Al-Hawwas, M., Bobrovskaya, L., Coates, P. T. & Zhou, X. F. Urine-derived cells for human cell therapy. Stem Cell Res. Ther. 9, 189 (2018).
Zhou, T. et al. Generation of human induced pluripotent stem cells from urine samples. Nat. Protoc. 7, 2080–2089 (2012).
Dura, B. et al. scFTD-seq: freeze-thaw lysis based, portable approach toward highly distributed single-cell 3’ mRNA profiling. Nucleic Acids Res. 47, e16 (2019).
Wolf, F. A., Angerer, P. & Theis, F. J. SCANPY: large-scale single-cell gene expression data analysis. Genome Biol. 19, 15 (2018).
Yu, G., Wang, L. G., Han, Y. & He, Q. Y. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS 16, 284–287 (2012).
Cortal, A., Martignetti, L., Six, E. & Rausell, A. Gene signature extraction and cell identity recognition at the single-cell level with Cell-ID. Nat. Biotechnol. 39, 1095–1102 (2021).
Scialdone, A. et al. Computational assignment of cell-cycle stage from single-cell transcriptome data. Methods 85, 54–61 (2015).
Andreatta, M. & Carmona, S. J. UCell: Robust and scalable single-cell gene signature scoring. Comp. Struct. Biotechnol. J. 19, 3796–3798 (2021).
Lang, N. et al. A blood-resistant surgical glue for minimally invasive repair of vessels and heart defects. Sci. Transl. Med. 6, 218ra6 (2014).
Wang, J., Wang, Q. & Cao, N. Generation of expandable cardiovascular progenitor cells from mouse and human fibroblasts via direct chemical reprogramming. STAR Protoc. 3, 101908 (2022).
Cui, Y. et al. Single-cell transcriptome analysis maps the developmental track of the human heart. Cell Rep. 26, 1934–1950 (2019).
Liu, Y., Sun, J. & Zhao, M. ONGene: a literature-based database for human oncogenes. J. Genet. Genomics 44, 119–121 (2017).
Zhao, M., Kim, P., Mitra, R., Zhao, J. & Zhao, Z. TSGene 2.0: an updated literature-based knowledgebase for tumor suppressor genes. Nucleic Acids Res. 44, D1023–D1031 (2016).
Breier, G. Functions of the VEGF/VEGF receptor system in the vascular system. Semin. Thromb. Hemost. 26, 553–559 (2000).
Zhao, T., Zhao, W., Chen, Y., Ahokas, R. A. & Sun, Y. Vascular endothelial growth factor (VEGF)-A: role on cardiac angiogenesis following myocardial infarction. Microvasc. Res. 80, 188–194 (2010).
Henning, R. J. Therapeutic angiogenesis: angiogenic growth factors for ischemic heart disease. Future Cardiol. 12, 585–599 (2016).
Bharadwaj, S. et al. Multipotential differentiation of human urine-derived stem cells: potential for therapeutic applications in urology. Stem. Cells 31, 1840–1856 (2013).
Sun, B. et al. Differentiation of human urine-derived stem cells into interstitial cells of Cajal-like cells by exogenous gene modification: a preliminary study. Biochem. Biophys. Res. Commun. 523, 10–17 (2020).
Zou, Y., Li, S., Chen, W. & Xu, J. Urine-derived stem cell therapy for diabetes mellitus and its complications: progress and challenges. Endocrine 83, 270–284 (2024).
Manaph, N., Al-Hawwas, M., Bobrovskaya, L., Coates, P. T. & Zhou, X. F. Correction to: urine-derived cells for human cell therapy. Stem Cell Res. Ther. 9, 222 (2018).
Zhou, Y. et al. Bmi1 is a key epigenetic barrier to direct cardiac reprogramming. Cell Stem Cell 18, 382–395 (2016).
Testa, G. et al. Bmi1 inhibitor PTC-209 promotes chemically-induced direct cardiac reprogramming of cardiac fibroblasts into cardiomyocytes. Sci. Rep. 10, 7129 (2020).
Tohyama, S. et al. Distinct metabolic flow enables large-scale purification of mouse and human pluripotent stem cell-derived cardiomyocytes. Cell Stem Cell 12, 127–137 (2013).
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (31900518 to CH) and Science and Technology Commission of Shanghai Fengxian District (20211603). We thank Singelon Co., Ltd. for their support with single-cell sequencing. Cell culture dishes/plates were obtained from Guangzhou Jet Bio-Filtration Co., Ltd. Centrifuge tubes were obtained from NEST Biotechnology Co., Ltd. (Wuxi, China).
Author information
Authors and Affiliations
Contributions
C.H. and J.Z. designed the study. C.H., Y.C., A.L. (Aoli Li), and A.L. (Aijie Liu) conducted experiments, collected data, and assessed outcomes. W.Z. and H.F. analyzed the data. C.H., J.Z., W.Z. and H.F. wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Medicine thanks Shugo Tohyama and the other anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, Y., Li, A., Liu, A. et al. Reprogramming of human urine cells into cardiomyocytes via a small molecule cocktail in xeno-free conditions. Commun Med 5, 266 (2025). https://doi.org/10.1038/s43856-025-00963-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s43856-025-00963-y