Abstract
Sudden Cardiac Death (SCD) is responsible for at least 180,000 deaths a year and incurs an average cost of $286 billion annually in the United States alone. Herein, we present a novel discrete event simulation model of SCD, which quantifies the chains of events associated with the formation, growth and rupture of atheroma plaques and the subsequent formation of clots, thrombosis and on-set of arrhythmias within a population. The predictions generated by the model are in good agreement both with results obtained from pathological examinations on the frequencies of three major types of atheroma and with epidemiological data on the prevalence and risk of SCD. These model predictions allow for identification of interventions and importantly for the optimal time of intervention leading to high potential impact on SCD risk reduction (up to 8-fold reduction in the number of SCDs in the population) as well as the increase in life expectancy.
Similar content being viewed by others
Introduction
The formation and growth of atheromatous material within the lumen of arterial vessels is a common and prevalent cause of cardiovascular disease (CVD) and accounts for 80% of sudden cardiac death (SCD)1. Annually in the United States, the cost of CVD exceeds $286 billion, while SCD alone is accountable for 180,000–450,000 deaths2. Though numerous approaches have been implemented to prevent SCD through the treatment of CVD, the use of simulation modeling has been limited to applications such as cost of anti-CVD treatment3. In this work, we have developed a discrete event simulation (DES) model which has been designed to predict the occurrence of SCD within a simulated population, allowing for predictive means of intervention and/or treatment to reduce both the incidence and cost associated with SCD. The use of this DES approach allows for the modeling of the complicated chains of random events within individuals or within a population. This is, thus, beneficial for the description of disease evolution. Additionally, the extensive available data from epidemiological1,2,3,4,5,6 and pathological7,8,9,10 studies allow for highly accurate refinement and verification of the model results. The model parameters chosen to fit these data, including frequency and distribution of atheromas, were drawn from a pathological study10, while data on the age of individuals at the time of first atheroma formation were drawn from the Bruneck study5. Predicted estimations of annual SCD risk generated by the model were then compared with the available epidemiological data. Finally, we looked at predictors of SCD and modeled the impact on the life expectancy of simulated patients for two types of interventions: (i) non-invasive methodologies for highly specific and selective identification of coronary atheroma, coupled with atherosclerosis treatment in a certain ‘at risk’ group of the population and (ii) highly efficient medications which decrease the growth rate of atheromas and clots, administered to the whole population after a certain age, which was predicted to reduce the number SCDs up to 8-fold. The important advantage of the model is its ability to predict the optimal time window of the intervention. Another advantage of the model is its ability to integrate data from pathological, clinical and epidemiological studies. If implemented in a clinical setting, predictions on treatment and intervention from this model would not only reduce CVD-associated costs, they could also increase the average life spans of given populations and, more critically, save lives.
Results
Brief model description
Following the data from the pathological studies and the simplified scheme for classification of atherosclerotic lesions8,9,10, we assumed that SCD caused by coronary artery disease could occur due to three major chains of events: (i) thin-cap fibrous atheroma formation→growth→rupture→clot formation→growth→thrombosis→arrhythmia→SCD; (ii) mid-cap fibrous atheroma formation→growth→erosion→clot formation→growth→thrombosis→arrhythmia→SCD; (iii) thick-cap atheroma formation→growth→stenosis→arrhythmia→SCD.
Our software, SCD-Predict, simulates the progression of atherosclerosis in an individual, starting with the formation of the first atheroma and ending either with SCD or with the “simulation stop time.” This can represent either the end of the clinical study, or a non-cardiac death, depending on the objective of the simulation. To model a population or a cohort of such individuals, SCD-Predict is queried multiple times from the parent program specifying the properties of the population. Software is available from the authors upon request.
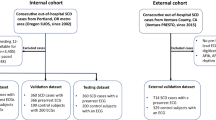
Comparison of the numbers of atheromas simulated with SCD-Predict model and observed in the pathological studies
SCD-Predict was fit with the data drawn from the pathological study of 50 whole human hearts as previously mentioned10. This study reported the number of ruptured and non-ruptured thin-, mid- and thick cap atheromas found in the coronary arteries of these hearts obtained from patients who had died of cardiovascular (n = 33), non-cardiovascular (n = 13) and unknown (n = 4) causes. Table 1 presents comparisons of our simulation results with these observations. Exact values of all simulation parameters can be found in Supplementary Table 1 (Supplementary Materials). To obtain this comparison, SCD-Predict analyzed 100 “simulated-men” and 100 “simulated-women.” Individuals in this “simulated cohort” were either modeled to have died of SCD or determined to have died of non-SCD by reaching the “simulation stop time.” This endpoint was modeled as a normal distribution with an average 72.8 ± 8 years, simulating the age distribution found in10. As seen in Table 1, the simulated numbers of ruptured, non-ruptured thin-cap, mid-cap and thick-cap atheromas are in good agreement with the numbers observed for both men (n = 32) and women (n = 18), as well as the total group in the study (root mean squared error of 13.5% for men, 21.8% for women and 8.6% for the total group). It is, however, important to note that while some parameter fitting was performed, minimization of the mean error was not considered a major goal. We preferred to avoid over-fitting, instead keeping parameter values of initial atheroma size, time to rupture and degree of stenosis consistent with the body of publications5,8,9,10,11,12,13,14,15,16,17. Detailed explanations on the rationale of parameter selection can be found in the Methods section. As an illustration of this aversion to over-fitting, we did not change the parameters of the model when going from “sim-men” to “sim-women,” but used the same parameters in Supplementary Table 1 for both cohorts. Therefore, the only difference in modeling male and female cohorts was found in the normal age distributions of first atheroma formation (mean 55 ± 12 years for men and 61 ± 12 years for women). As shown in the Methods section, these values were in agreement with the Bruneck study5. The rationale for changing only initial distributions and preserving the model parameters is that the protection against atherosclerosis in women is known to be lost within a 5-year period post-menopause5. Thus, a model with identical parameters and a time shift of 6 years should work for both men and women, as proved to be the case (see Table 1).
Additionally, Table 1 contains the results for both men and women who died of SCD and non-SCD causes separately. Here, the comparison with the findings in10 is complicated by the fact that the CV group in10 includes all cases of cardiovascular-related deaths (including myocardial infarction, cardiomyopathy, etc.), while the SCD group from SCD-Predict contained only those who had died of SCD caused by coronary artery disease. This explains why the mean numbers of atheromas in the simulated SCD-Predict group are higher than those observed in the CV group, though there remains good agreement between the numbers for the two groups (numbers for non-CV and non-SCD have even better correlation). Finally, Table 1 presents the number of arrhythmias caused by each of the three types of atheromas within each of the simulated groups, as well as the total mean arrhythmias in the simulated cohort.
Next, comparisons of plaque morphology were explored. We compared the results of SCD-Predict with the observations from Ref. 7 that 73% of SCD cases involved plaque ruptures associated with thrombosis, 8% plaque fissures with intra-plaque fibrin deposition and hemorrhage and 19% possessed no evidence of thrombi. The comparison of these results can be found in Table 2, illustrating that percentages observed in Ref. 7 are very close to the average between “men” and “women” simulated by SCD-Predict. As shown, our average predicted percentage of rupture is also 73%. The predicted percentage of cases possessing thrombi/no rupture is 11% and no thrombus is 16%. These percentage values are quite close to those observed in Ref. 7. Importantly, no parameter fitting to this data was involved. Therefore, the similarity of SCD-Predict's generated data and the independently observed prevalence of lesions of different types confirms the validity of the model.
Figure 1 provides a graphical summary of the simulated patient data via histograms of the distributions of total atheromas, vulnerable atheromas, arrhythmias and age at death for the aforementioned simulated cohorts. While the maximum numbers of atheromas (10), vulnerable atheromas (4) and arrhythmias (3) are the same in “sim-men” and “sim-women,” the mean numbers are substantially higher for men than for women, as expected and reflected by both Table 1 and Figure 1.
Using SCD-Predict, cohorts of 100 men (blue) and 100 women (red) were simulated and analyzed.
The findings visualized above show (a) simulated age at time of death, (b) total number of atheroma, (c) total vulnerable atheroma and (d) number of arrhythmias. These results are compared to findings of10 in Table 1. While the maximum numbers of atheromas, vulnerable atheromas and arrhythmias are the same in “sim-men” and “sim-women” cohorts, the mean numbers are substantially higher for “sim-men” than for “sim-women” as expected and as reflected both in Table 1 and Figure 1. Age at death distributions are to a large extent predetermined by the “stop simulation time” = (72.8 + 8 randn) years, where randn is a MATLAB function for random numbers normally distributed with mean = 0 and std = 1.
Predictions of the SCD-Predict model for the SCD cumulative and annual risk
Because of the nature of the SCD-Predict model and its demonstrated coherence to known pathological and epidemiological data, it is possible to use it as a predictive tool. First, the model was used to predict the age-dependent cumulative risk of SCD in the general population. Multiple cohorts (1,000 “sim-persons” in each) using identical parameters to those above and with the “simulation stop time” varying from 45 to 95 years, were simulated. The number of persons dead due to SCD in each cohort, divided by the total number of persons, yielded the simulated cumulative risk of SCD (Figure 2a). After curve fitting the cumulative risk data points (MATLAB, Curve Fitting Tool), the time derivatives of the fits were calculated, providing the annual SCD risk versus time (Figure 2b). The peaks of annual risk for SCD at age 80 are predicted by our model to be 3.3% and 1.8% for men and women, respectively. This finding is in agreement with the published observations of the age-dependent incidence of SCD4, where the peak of SCD is observed for the age group 75–84 years. Our model predictions are also in agreement with the findings of annual incidence of death from coronary heart disease (CHD) in the Framingham study, where 30 CHD deaths per 1,000 in men (3% annual risk) and 15 CHD deaths per 1,000 in women (1.5% annual risk) were reported for the same age group18. Importantly, the epidemiological data from the Framingham study or from study4 was neither used in the development of the SCD-Predict model, nor in the parameter fitting process. Therefore, the high degree of agreement of annual SCD risk predicted by our model with observed epidemiological data provides additional confirmation of the validity of our model.
Graphical representations of the (a) cumulative and (b) annual risk of SCD for both men (blue) and women (red).
Each point in the cumulative risk curves was generated by running SCD-Predict for the cohort of 1,000 “sim-persons” with fixed “stop simulation time.” Annual risk curves were generated by calculating the derivative of the cumulative risk. Of note are the evident peaks in the generated annual risk curves (at approximately 78 and 95 years of age for men and women, respectively). The annual risk of 3.5% (men) and 1.8% (women) at age 78 is in agreement with the annual 30 CHD deaths per 1,000 in men and 15 CHD deaths in women reported for the age group 75–84 in the Framingham study12.
The detailed quantitative comparison, however, is complicated by the fact that epidemiological studies present the combined data for SCD from the entire spectrum of etiologies: coronary artery disease (~80%), cardiomyopathies (10–15%) and others including congenital cardiac conditions, Brugada and long QT syndromes (5–10%)4. Our model represents only the most common etiology of SCD, i.e. coronary artery disease. Other etiologies will be introduced in the second generation of our SCD-Predict.
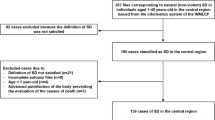
Predictions of the SCD-Predict model for the number of atheromas in SCD and non-SCD subpopulations
A comparison of the predicted number of atheromas in the simulated SCD and non-SCD subpopulations is presented in Figure 3. The most obvious difference between these groups is that in non-SCD, the number of atheromas is quite low at age 45–50 (~0.5 total atheromas) and then increases 12-fold by age 85–90; in contrast, the number of atheromas is already high by age 45–50 in the SCD group (~5 total atheromas) and then increases only by about 1.5-fold in the SCD individuals at 85–90. Similarly, the numbers of ruptures, thin-, mid- and thick-cap atheromas are much less age-dependent for the SCD individuals than for the non-SCD group. With regard to the number of atheromas, the individual modeled to suffer from SCD is, at age 50, much more similar to the SCD individual at age 90 than to the non-SCD individual at age 50.
(a–b) Numbers of ruptured (red), thin-cap (green), mid-cap (black), thick-cap (purple) and total atheroma (blue) for both men (solid lines) and women (dashed lines).
A comparison of simulated individuals (a) without SCD and (b) with SCD demonstrates that for both men and women, the number of atheroma in those who suffer SCD are largely independent of age. (c) Box plots illustrating the difference in total number of atheroma in the simulated male (blue) and female (red) cohorts (box plot data includes minimum, 1st quartile, mean, 3rd quartile, maximum and relative number of patients represented as width). A clear distinction exists between the subpopulations of those simulated patients suffering from SCD and those who did not (the Welch's t-test, with T-statistics: 22.25 and 24.49; df: 992 and 833, for men and women, results in rejection of the null hypothesis with the p-value below 10−6).
We also compared the distributions of the total number of atheromas in the SCD and non-SCD subpopulations of men and women (1,000 individuals each). The age-dependent death incidence for non-SCD individuals was calculated based on Mortality Tables19. Figure 3c presents box plots illustrating that the total number of atheromas is significantly (p-value < 10−6) higher in SCD than in non-SCD subpopulations in both “sim-men” and “sim-women.”
The predictive power of SCD-Predict and the combination of the obtained results – (i) that a high number of atheromas discriminates between SCD and non-SCD groups and (ii) that the number of atheromas in the SCD is relatively independent of the age at death – allows us to hypothesize that the number of atheromas could serve as a useful predictor or biomarker of SCD.
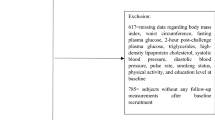
SCD-Predict model predicts high impact of coronary screening and atherosclerosis treatment
Based on the hypothesis of the previous section, we used our model to estimate the impact of early diagnosis and treatment of atherosclerosis. First, 1,000 men at age 45 and 1,000 women at age 55 were simulated and screened for treatment of patients with five or more atheromas. In this case, eight “sim-men” were treated and saved from SCD -- they would have otherwise died between the ages of 45.2 and 66.1. Similarly, we treated 13 “sim-women” and, of these, saved 11 from SCD (the remaining two would not have died of SCD even without treatment). The 11 “sim-women” saved from SCD would have otherwise died between the ages of 55.2 and 77.8.
Next, we explored how the number of treated and saved patients would change if screenings were performed at different ages and if we had used a number of atheromas other than 5 as the threshold for treatment. Obviously, using a lower threshold would save more patients; however, it would also increase the percentage of unnecessarily treated patients and could raise healthcare costs. Therefore, the use of modeling could be beneficial for determination of the optimal age of screening and threshold for treatment. The survival curves for the treated groups are presented in Figure 4a (men) and 4c (women). The difference between the treated and non-treated survival curves (area between the curves) illustrates the number of years of life added to the treated subpopulations. As seen in Figure 4 (for both genders), the average increase in life duration due to treatment is maximized in the case of an early scan (45-men, 55-women) and high threshold of 4 atheromas for treatment. However, the total number of treated/saved patients in this case is quite low, about 20–50 out of 1,000, i.e. 2–5% of the population. Using lower thresholds for treatment and/or older scanning ages leads to smaller increases in life duration per patient, but also leads to larger life duration increases for the treated subpopulation.
Survival curves illustrating the impact of intervention on treated male population (a), treated female population (c), the entire male population (b) and the entire female population (d) based on intervention parameters of age and number of atheromas.
(a) Survival curves for groups of treated and non-treated men using different scan ages (45 and 60) and different numbers of atheroma threshold. (b) Population survival curves for male populations with various intervention parameters. (c) Survival curves for groups of treated and non-treated women using different scan ages (55 and 65) and different numbers of atheroma thresholds. (d) Population survival curves for female populations with various intervention parameters. See text for additional explanations of intervention parameters.
Figures 4b and 4d illustrate the impact of the scanning and atherosclerotic treatment for the entire population. As expected, scans at earlier ages (45, 55) allow saving more people of younger age (<75), while scanning at later ages (60, 65) allows for saving more elderly people. The overall life expectancy of the entire male population is predicted to increase from 75.4 to (i) 75.9 (scan age 45, threshold 4), (ii) 78.6 (scan age 45, threshold 1), (iii) 78.7 (scan age 60, threshold 3). Notably, life expectancy for the treated subpopulation is predicted to increase from 59.9 to 83.3, 69.5 to 88.6 and 72.9 to 89.1 for the first, second and third screening strategies above, respectively. Similarly for women, overall life expectancy is modeled at 78.2 without treatment, 78.9 with the first strategy (scan age 55, threshold 4) and 80.6 years with both the second (scan age 55, threshold 1) and third (scan age 65, threshold 2) strategies. For the treated subpopulation of women, life expectancy is predicted to increase from 69.8 to 86.9, 77.2 to 90.8 and 79.3 to 91.8 for the three strategies, respectively. Note that treated subpopulations are different for different strategies and as a consequence, younger people who would benefit from atherosclerosis treatment are missed in the case of late screening strategies. The data regarding the treated subpopulations are truly compelling and show that early screening with low thresholds seems to be the preferable strategy, leading to the likely saving of lives and increased life spans for individuals.
SCD-Predict model predicts high impact of medications reducing the growth rate of atheromas and clots
Next, SCD-Predict was used to model the effects of disease intervention via the administration of two medications targeted toward reducing growth rates of atheromas and clots. While numerous medications are used in clinical practice today, for the sake of simplicity we focus only on the effects of various highly efficient medications, rather than the implication of specific compounds. Thus we assumed that medication #1 reduces the growth rate of all types of atheromas by a factor of two, while medication #2 reduces the growth rate of all clots by a factor of two. Figure 5 illustrates the change in the number of SCDs, arrhythmias and time to rupture in men and women treated with medication #1, or the combination of medication #1 and #2, relative to the case of no treatment. To ensure a common scale, we normalized all the values by their corresponding values for men without treatment. These were equal to: SCD = 20.5% of population, mean number of arrhythmias per person = 0.631, mean time to rupture = 12.23 years. As seen in Figure 5, the mean time to rupture is increased by 50–60% when treatment is started at 45 and by 30–40% when it is started at age 65. The mean number of arrhythmias is reduced more than 3-fold in the case of medications #1 and #2 being used in combination starting at age 45. Most importantly, the number of sudden cardiac deaths is reduced 4-fold in both men and women when medication #1 is started at age 45 and even more dramatically (i.e. 9-fold in men and 8-fold in women) by the combination of medications #1 and #2. Starting this drug combination at the later age of 65 is 2-fold less effective in men, while in women the difference due to a later start of medication is negligible.
Comparisons of untreated and treated male (blue) and female (red) populations with various intervention parameters (medications reducing atheroma and clot growth rates).
Normalized data show that for both genders, the percentage of SCD within a given population is decreased for the treated subpopulations compared to the untreated. Likewise, the mean number of arrhythmias is also reduced, while the mean number of years to atheroma rupture is increased across both sexes and all intervention parameters. Raw data values printed above bars for comparison. Simulated cohorts contained 5000 individuals for both male and female groups.
Discussion
In this study, we developed a discrete event simulation model of sudden cardiac death by fitting pathological data for the number of ruptured and non-ruptured vulnerable atheromas, as well as the number of erosive and thick-cap atheromas from a study of 50 whole, human hearts10. Application of this model to the general population predicted the age-dependent cumulative and annual risk of SCD which is in compliance with established epidemiological data4,7,18. Analysis of the data on the number of atheromas in the SCD and non-SCD subpopulations led to the hypothesis that the total number of atheromas could serve as an early predictor, or biomarker, of SCD.
Based on this hypothesis and the documented improvements in the efficiency and safety of existing non-invasive atheroma detection techniques, we suggest that early screening of the general population by such approaches in coordination with treatment of atherosclerosis would substantially increase the life expectancy of all population groups. We also modeled the impact of statin- and aspirin-like medications reducing the growth rate of atheromas and clots and predicted that the use of a combination of medications such as these starting at age 45 might result in an 8- to 10-fold reduction of the number of sudden cardiac deaths.
The important advantage of the discrete event simulation approach is that it allows integrating data at multiple scales and levels: microscopic, mesoscopic and macroscopic, pathological clinical and epidemiological. It allows combining blocks describing processes at various levels of details, depending on the importance of the process for the whole model and on the availability of the data. Based on these properties, our SCD model can be easily upgraded as the new data of the mechanism of SCD emerge.
There are several directions to further enhance our current SCD-Predict model. We can introduce the additional chains of events representing other etiologies (cardiomyopathies, Brugada, etc.) that contribute to the annual risk of SCD, especially in the earlier age groups. While modeling SCD in young adults, it is important to take into account the high prevalence of atherosclerosis in the age groups between 15–34 years. Data regarding this aspect of the disease have been extensively studied by Strong et al.20, though by design, none of the individuals studied died of SCD, instead being victims of accidents, homicide, or suicide. Nonetheless, within these young age groups, it was found that the majority of the individuals had at least one lesion in the right coronary artery, though the average number of raised lesions was several fold lower for these age groups and no ruptures were reported. This finding confirms that repair mechanisms are more effective in young adults than in older individuals. We plan to further enhance the SCD-Predict model by adding the blocks which stimulate this healing/repair process which, in turn, makes the model more applicable to young adults.
Also, as more data become available, we will consider including separate chains of events representing disorders such as depression, diabetes and obesity, which are known to be comorbid with cardiovascular disease. Another important avenue is to include the blocks, representing the models of the pathways, like cholesterol metabolism, that are crucial for several of the comorbidities involved. This interaction of diseases and comorbidities could, in turn, provide this model with the capability of assessing complex burden of disease for a given population. One of the major metrics by which the World Health Organization (WHO) analyzes burden of disease involves the measure of Disability-Adjusted Life Years (DALYs)21. This standard combines the Years of Life Lost (YLL) to disease with the Years Lived with Disability (YLD) in the simple formula DALY = YLL + YLD. Certain diseases, such as SCD, cause a significant amount of early death, while having a relatively low amount of resultant disability, while others (such as blindness or diabetes) cause varying degrees of early death with relatively high amounts of resultant disability. Therefore, this DALY metric allows distinctly different diseases to be compared directly as to their impact on a given population (one DALY effectively equals one year of healthy life lost). SCD-Predict, though not specifically designed at this time to account for this, does provide information pertaining to the number of YLL and could be upgraded to include YLD (which can be extracted by comparing initial incidence of atheromatous rupture/cardiovascular event and its associated effects with the onset of SCD). Thus, with these in place, interactions between the various chains of events would provide a more holistic representation of the steps leading to SCD as well as the disease's impact on individuals and populations.
Although these enhancements of the model would enable more personalized prediction of the risk of SCD for a given individual, more than likely they would not change the general conclusions of our study, which are based on average non-stratified data. The most important practical result of our study is the prediction of the high impact on the population's life expectancy of early non-invasive atheroma detection screening and subsequent atherosclerosis treatment. We believe that the next logical step is, therefore, the clinical verification of this finding.
Methods
The SCD-Predict software was developed with the SimEvents simulation engine, which is part of the MATLAB 2011b (Mathworks, Natick, MA) family of software tools. The structure of the model is presented in the Suppl. Figure 1, while Suppl. Figure 2 presents the “arrhythmia to SCD” block.
Age of first atheroma formation
The age distribution of the first atheroma formation was estimated from the data of the high resolution ultrasound study of 826 subjects in the age range 40–84 years: the Bruneck study5. The cumulative risk of atherosclerosis observed in this study was approximated by the integrals of the normal distributions with mean of 55 years for men and 61 years for women and standard deviation of 12 years (Suppl. Fig. 3a). We anticipate that both the size of the detectable atheroma and the age at which it was first observed depend on the sensitivity of diagnostic procedure; therefore it is important to use the data on the initial size and time of formation of atheromas from the same study, as in our case5, so that errors due to the limited sensitivity in the initial size and time of formation distributions compensate for each other.
Formation of the lesions
Following Ref. 5, the size of the atheroma at formation was assumed to have the mean diameter of 1.3 mm for all types of lesions. The mean diameter of the coronary arteries was assumed to be 3.57 ± 0.84 mm, according to the electron beam computer tomographic angiography study17. Therefore, the mean normalized initial size of atheroma (ratio of diameters of atheroma and coronary artery) was set to 0.36.
Both normalized initial sizes of atheromas and the time intervals (inter-generation time values) between the events of formation of atheromas of each type were simulated as random numbers with the probability density function described by the Weibull distribution22:

which describes the family of distributions starting from highly asymmetrical exponential type (0 < k ≤ 1) to Rayleigh (k = 2), to nearly normal symmetrical probability density function (k = 5). Following the above data of5,17, the normalized initial atheroma size distribution was described by the Weibull function with λ = 0.36 and k = 4.5 which results in the standard deviation (σ/λ = 0.23) consistent with the above relative standard deviation (0.84/3.57) of the coronary arteries' diameters17. The distributions of the inter-generation time values were modeled with the Weibull function with parameters λ and k which differed for different types of atheroma (Suppl. Table 1). Suppl. Figures 3b and 3c present the Weibull probability density functions both for inter-generation time intervals and initial sizes of atheromas and clots.
Growth
We used a simple model to describe the growth of lesions:

where x-diameter of the lesion, a-diameter of the blood vessel and r-growth rate. This logistic growth model is widely used within biology to model the growth of some generic object (e.g. population, tumor, lesion) which is being fed by an external resource (and hence grows at rate r) while being constrained due to a finite available space (and hence stops growing as x approaches a). Given its widespread use to describe biological growth in the literature, this same growth model (2) was used for all atheromas and clots -- however the initial sizes, growth rates and thresholds at which rupture of thin-cap atheroma or erosion of mid-cap atheroma occurred, were allowed to vary (Suppl. Figure 3d). The typical atheroma growth time is 15–20 years according to Zohdi et al.23. When the threshold is reached, the clot is formed and starts growing as described by (2); however the growth rate of the clot in the case of a ruptured atheroma is much faster (months) than in the case of erosive atheroma (years). Arrhythmia is assumed to occur as soon as the diameter of an artery lumen is reduced to the threshold value due to the growth of the clot (thrombosis) or due to the growth of thick-cap atheroma (stenosis).
The relation of the artery lumen narrowing and occurrence of ventricular arrhythmia has been a topic of several studies and discussions. The 1996 study9 of 160 atherosclerotic coronary plaques obtained from 31 subjects who died from SCD concluded that “two major determinants of plaque vulnerability, core size and cap thickness are not statistically related. Neither of these two factors that confer vulnerability are related to absolute plaque size or to the degree of stenosis”. The same study demonstrated that “twenty two of these 31 patients (71%) had major thrombus occluding more than 30% of the lumen cross-sectional area at that point”. The 2001 review on coronary thrombosis11 stated: “It is accepted by convention that the presence of a cross sectional luminal narrowing of at least 75%, even in the absence of thrombus, is a potential cause of sudden death.” Another study from the same group12 demonstrated that the mean percentage of stenosis in the arteries of 142 victims of SCD was associated with the number of prior plaque ruptures. This mean varied from 56% in the case of one healed rupture site to 83% in the case of four healed ruptures. The pathological study13 of the hearts of 72 men and 18 women who died of sudden cardiac death demonstrated that the percentage of stenosis differed from 78 ± 12 in the case of plaque rupture, to 70 ± 11 in the case of plaque erosion, to 50 ± 10 in the case of calcified nodule. Another study of 38 hearts from the same research group14,15 reported that “the mean luminal narrowing was least in sections with thin cap atheroma (59.6%), intermediate for hemorrhage into a plaque (68.8%) and highest in plaque rupture (73.3%) or healed plaque rupture (72.8%). The authors of the recent review on sudden cardiac death6 emphasized the difference in the lumen narrowing caused by different types of lesions by stating that “although postmortem examination might reveal an apparent ≥90% culprit lesion in a given coronary vessel, the presence of active plaques elsewhere in the coronary vasculature makes the definition of the culprit vessel responsible for an SCD, in the absence of acute thrombosis or anatomical evidence of an acute myocardial infarction, a challenging chore. It should not be assumed from postmortem anatomy that a stable high grade coronary artery lesion is any more likely to be the culprit vessel in a SCD than an unstable plaque that is occluding only 30% to 50% of the vessel lumen at the postmortem examination.” However, the recently published study of the causes of sudden unexpected death of adult hospital patients16 reported that “the majority 36 of the 58 patients (62%), with sudden death judged due to arrhythmias, had 75% or greater stenosis of 1 or more coronary arteries (average 2),” which supported the conventional statement of 75% stenosis in SCD in Ref. 11.
As seen above, the reported percentage of stenosis varies from 30% to 83% and depends on multiple factors including the type of lesion. Importantly, however, even for the given type of lesion there is no consensus between the studies, likely because of the multiple unreported factors involved. Nevertheless, the majority of the cases gravitate to 50–75% reduction of the arteries lumen cross section area in SCD. Given the fact that not all arrhythmias are fatal, the threshold for arrhythmia likely is lower than the observed stenosis percentage in the postmortem analysis of SCD arteries. Based on these considerations, we used the threshold of 56% reduction of lumen cross section which corresponded to the radius of the lesion equal to 0.75 of the radius of the artery.
Likelihood of arrhythmic cardiac death
Previous cardiac arrest is among the risk factors of SCD, as reported in Ref. 24. To reflect this observation, we assumed that the likelihood to survive L(n) each next arrhythmia is lower than the previous one and is described by the function:

where p–the probability to survive the first arrhythmia, n-number of arrhythmias in a given patient, ln(n)-natural logarithm function. The existing data on the arrhythmia survival rate are contradictory. While anticipating that survival rate depends on multiple factors including type of arrhythmia, age of the patient and the promptness of advanced life support2,24,25, we have not introduced it into our minimal model at this stage, but have instead used the compromise average value of 22% for the probability p to survive the first arrhythmia.
The three chains of events leading to SCD were assumed to be independent in our current version of SCD-Predict. The only interaction between the chains of events is the “competition” for ending the simulation process: as soon as the condition of SCD is reached in one of three chains, the simulation is stopped and the data on age at death, number of arrhythmias and atheromas for the given individual are returned to the parent program.
References
Farb, A., Burke, A. P., Kolodgie, F. D. & Virmani, R. New insights in the pathology of sudden cardiac death. CEPR 5, 373–378 (2001).
Roger, V. L. et al. Heart disease and stroke statistics – 2011 update: A report from the American Heart Association. Circulation 123, e18–e209 (2011).
Cooper, K. et al. The development of a simulation model of the treatment of coronary heart disease. Health Care Manag Sci 5 (4), 259–67 (2002).
Cugh, S. S. et al. Epidemiology of sudden cardiac death: clinical and research implications. Prog Cardiovasc Dis 51, 213–228 (2008).
Kiechl, S. & Willet, J. The natural course of atherosclerosis. Part I: Incidence and progresssion. Atheroscler Thromb Vasc Biol 19, 1484–1490 (1999).
Myerburg, R. J. & Junttila, J. Sudden cardiac death caused by coronary heart disease. Circulation 125, 1043–1052 (2012).
Davies, M. J. Anatomic features in victims of sudden coronary death: coronary artery pathology. Circulation 85, 119–124 (1992).
Kolodgie, F. D., Burke, A. P., Farb, A. & Schwartz, S. M. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Atheroscler Thromb Vasc Biol 20, 1262–1275 (2000).
Mann, J. M. & Davies, M. J. Vulnerable plaque. Relation of characteristics to degree of stenosis in human coronary arteries. Circulation 94, 928–931 (1996).
Cheruvu, P. V. et al. Frequency and distribution of thin-cap fibroatheroma and ruptured plaques in human coronary arteries: a pathologic study. J Am Coll Cardiol 50, 940–949 (2007).
Burke, A. P., Farb, A. & Virmani, R. Coronary thrombosis: whats new? Path Case Rev 6, 244–252 (2001).
Burke, A. P., Kolodgie, F. D., Farb, A., Weber, D. K., Malcom, G. T., Smialek, J. & Virmani, R. Healed plaque rupture and sudden cardiac death: evidence that subclinical rupture has a role in plaque progression. Circulation 103, 934–940 (2001).
Virmani, R., Burke, A. P., Farb, A. & Kolodgie, F. D. Pathology of unstable plaque. Prog Cardiovasc Dis 44, 349–356 (2002).
Virmani, R., Burke, A. P., Kolodgie, F. D. & Farb, A. Vulnerable plaque: the pathology of unstable coronary lesions. J Interven Cardiol 15, 439–446 (2002).
Virmani, R., Burke, A. P., Farb, A. & Kolodgie, F. D. Pathology of the vulnerable plaque. J Am Coll Cardiol 47, C13–C18 (2006).
Nichols, L. & Chew, B. Causes of sudden unexpected death of adult hospital patients. J Hosp Med 7, 706–708 (2012).
Funabashi, N., Kobayashi, Y., Perlroth, M. & Rubin, G. D. coronary artery: quantitative evaluation of normal diameter determined with electron-beam CT compared with cine coronary angiography – initial experience. Radiology 226, 263–271 (2003).
Kannel, W. B. & Vokonas, P. S. Demographics of the prevalence, incidence and management of coronary heart disease in the elderly and in women. Ann Epidemiol 2, 5–14 (1992).
Mortality Tables: http://www.cdc.gov/nchs/data/nvsr/nvsr58/nvsr58_19.pdf
Strong, J. P. Prevalence and Extent of Atherosclerosis in Adolescents and Young Adults: Implications for Prevention from the Pathobiological Determinants of Atherosclerosis in Youth Study. JAMA 281, 727–735 (1999).
World Health Organization. Metrics: Disability-Adjusted Life Year (DALY): Quantifying the Burden of Disease from mortality and morbidity. http://www.who.int/healthinfo/global_burden_disease/metrics_daly/en/. Accessed 03-01-2013
Weibull, W. A statistical distribution of wide applicability. J. Appl. Mech.-Trans. ASME 18, 293–297 (1951).
Zohdi, T. I., Holzapfel, G. A. & Berger, S. A. A phenomenological model for atherosclerotic plaque growth and rupture. J. Theor. Biol. 227, 437–443 (2004).
Sovari, A. A. Sudden cardiac death. December 5, 2011. http://emedicine.medscape.com/article/151907-overview#a0199
Cobb, L. A., Fahrenbruch, C. E., Olsufka, M. & Copass, M. K. Changing incidence of out-of hospital ventricular fibrillation, 1980–2000. JAMA 288, 3008–3013 (2002).
Acknowledgements
The authors would like to thank the National Science Foundation grant CHE-0748648 (SKD) and the National Institute of Health grant 5R01GM047915-18 (SD) for support. S.D. is grateful to the Miller School of Medicine of the University of Miami for the Lucille P. Markey Chair in Biochemistry and Molecular Biology. T.H. would like to thank the National Science Foundation Integrative Graduate Education Research Traineeship (grant DGE-0653710).
Author information
Authors and Affiliations
Contributions
The overall project idea was from P.J.G. and S.D. Conceptual design of the computational model system was provided by V.P.A. and N.J. Relevant cardiovascular input to the model was provided by P.J.G. Data collection was performed by T.H. with model output data interpretation and analysis by V.P.A., T.H., S.K.D., S.D. and P.J.G. The manuscript was prepared by T.H. and V.P.A. with assistance of all other co-authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
odelDiscrete Event Simulation M of Sudden Cardiac Death Predicts High Impact of Preventive Interventions Supplemental Information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareALike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Andreev, V., Head, T., Johnson, N. et al. Discrete Event Simulation Model of Sudden Cardiac Death Predicts High Impact of Preventive Interventions. Sci Rep 3, 1771 (2013). https://doi.org/10.1038/srep01771
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep01771
This article is cited by
-
Surface Chest Motion Decomposition for Cardiovascular Monitoring
Scientific Reports (2014)