Abstract
Histiocytic sarcoma and tumors with dendritic cell differentiation (HDT) are uncommon neoplasms often with an aggressive clinical course that may occur in association with another hematologic malignancy or mediastinal germ cell tumor (secondary HDT, sHDT). Previous studies have shown mutations in the RAS/MAPK pathway in HDT and have demonstrated a clonal relationship between HDT and associated lymphoid malignancies through common translocations or identical immunoglobulin or T-cell receptor gene rearrangements. We performed whole exome sequencing on 16 cases of sHDT to further evaluate the spectrum of mutations that occur in sHDT in the context of an associated lymphoid malignancy, including cases associated with follicular lymphoma (FL), chronic lymphocytic leukemia/small lymphocytic lymphoma, B- and T-cell acute lymphoblastic leukemia/lymphoma and peripheral T-cell lymphoma, NOS. In addition, we assessed the clonal relationship between the HDT and the associated lymphoid malignancy in three cases for which matched samples were available. We found mutations in RAS/MAPK pathway genes in 14/16 cases of sHDT associated with diverse mature and precursor B-cell and T-cell neoplasms, involving KRAS (8/16), BRAF (2/16), NRAS (2/16), MAP2K1 (1/16), and NF1 (1/16). In addition, we note that FL-associated sHDT frequently shares a similar mutational profile to the associated malignancy, identifying mutations in CREBBP or KMT2D in all cases and “aberrant” somatic hypermutation in 5/6 cases. Our study confirms the role of the RAS/MAPK pathway in the pathogenesis of sHDT, provides further evidence of a common neoplastic precursor and, in the case of FL, gives additional insight into the stage in lymphomagenesis at which transdifferentiation may occur.
Similar content being viewed by others

Introduction
The clonal relationship between co-occurring lymphoid and histiocytic/dendritic neoplasms is a well-documented phenomenon, most often in relation to low grade B-cell lymphoma (BCL) including follicular lymphoma (FL) [1, 2] and chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) [3], but is also described in cases of B- and T-acute lymphoblastic leukemia/lymphoma [4,5,6]. Although rare, in these cases, the histiocytic/dendritic neoplasm and the associated lymphoid tumor have been shown to share identical structural rearrangements (such as the IGH/BCL2 translocation) [1, 2], clonal immunoglobulin or T-cell receptor (TRG) gene rearrangements [1,2,3,4,5,6] or in some cases, identical pathogenic mutations [7, 8].
Several theories have been proposed to explain the origin and evolution of these related neoplasms of seemingly different lineage, including origin from a common neoplastic progenitor, transdifferentiation of a mature lymphoid cell to one of myeloid lineage or alternatively dedifferentiation of a lymphoid cell to an immature progenitor with subsequent differentiation along the myeloid/dendritic lineage [1, 9]. Despite these hypotheses, the mechanism by which this process occurs remains poorly understood.
With the advent of next generation sequencing, mutational analysis has given insight into the molecular pathogenesis of histiocytic and dendritic cell tumors and has shown a central role for driving alterations in genes of the RAS/MAPK pathway. This also holds true for histiocytic/dendritic tumors that arise in association with lymphoid neoplasia, with case reports documenting responses to MEK inhibition in MAP2K1-mutated histiocytic sarcoma associated with FL [10], as well as mutations in KRAS [11], BRAF [12], NF1 [13], and NRAS [8, 14]. With this in mind, we sought to further the understanding of the mutational landscape of secondary histiocytic/dendritic neoplasms, firstly by performing whole exome sequencing on a cohort of cases associated with diverse lymphoid malignancies of both B-cell and T-cell origin, and secondly by evaluating the clonal relationship between the lymphoid and histiocytic/dendritic tumors in three cases for which a matched sample of the associated lymphoid malignancy was available.
Materials and methods
Case selection
Sixteen cases of secondary histiocytic/dendritic tumors (sHDT) comprising 15 histiocytic sarcomas (HS) and 1 indeterminate dendritic cell tumor (IDCT) were identified from the files of the Hematopathology Section of the National Cancer Institute under an IRB approved protocol. Associated hematologic malignancies included FL, aggressive BCL, CLL/SLL, T-lymphoblastic leukemia/lymphoma (T-ALL), B-lymphoblastic leukemia/lymphoma (B-ALL) and peripheral T-cell lymphoma, NOS (PTCL). Several of these cases have been previously reported in the literature with limited molecular analysis and clonality studies (Table 1); however, none have had mutational analysis performed prior to the current study. Material from the associated lymphoid malignancy was available in 3 cases (1 FL and 2 T-ALL).
DNA extraction, BCL2 translocation and clonality studies
DNA was extracted from formalin-fixed paraffin embedded (FFPE) tissue sections using QIAGEN QIAamp DNA FFPE Tissue Kit on a QIAcube robotic system according to the manufacturer’s protocol (QIAGEN, Germantown, MD, USA). In cases with composite components, the histiocytic/dendritic component was macrodissected. BCL2 translocations were detected in two cases using a break-apart FISH probe (described later) or by PCR for the IGH/BCL2 (MBR) translocation as described elsewhere [15]. Four of six FL-associated cases were previously published and had IGH/BCL2 status determined according to methods described at that time [1]. Clonality studies were performed as previously described [15] or as described at initial publication [1, 3, 4, 6].
Whole exome sequencing, variant annotation, and filtration
Exome libraries were prepared in 17 cases (14 HDT and 3 paired lymphoid malignancies) using Agilent SureSelectXT reagents (Agilent, Santa Clara, CA, USA) and in 2 cases using Accel-NGS 2 S Hyb DNA library Kit (Swift Biosciences, Ann Arbor, MI, USA). Targets were captured using SureSelect Human All Exon V5 + UTR target enrichment kit and sequenced on an Illumina HiSeq3000 with TruSeq V2 chemistry (Illumina, San Diego, CA, USA). Alignment and variant calling were performed utilizing the Center for Cancer Research Collaborative Bioinformatics Resource (CCBR) Pipeliner workflow (https://github.com/CCBR/Pipeliner). Reads were trimmed using Trimmomatic v0.33 [16] and mapped to the hs37d5 human reference genome (ftp://ftp.1000genomes.ebi.ac.uk/vol1/ftp/technical/reference/phase2_reference_assembly_sequence/hs37d5.fa.gz) using BWA-mem v0.7.15 [17]. Resulting BAM files were then sorted using Samtools v1.3 (http://www.htslib.org/) [18] and PCR duplicates were marked using Picard v2.1.1 (https://broadinstitute.github.io/picard/). Indel realignment and base recalibration was performed using GATK v3.7 [19]. Read- and alignment-level quality was assessed using MultiQC v1.7 (http://multiqc.info/) to aggregate QC metrics from FastQC (http://www.bioinformatics.babraham.ac.uk/projects/fastqc/), FastQ Screen (https://www.bioinformatics.babraham.ac.uk/projects/fastq_screen/), Qualimap (http://qualimap.bioinfo.cipf.es/) [20], Bamtools (http://github.org/pezmaster31/bamtools) [21], and Trimmomatic [16].
Variant calling was performed on each sample using two variant callers (MuTect 1.1.7 and MuTect2) [22]. An internal panel of normals developed from >400 normal germline samples accumulated at CCBR was used to remove sequencing artifacts and common variants at > 0.001 frequency in ExAC (excluding the TCGA) r0.3.1 [23], 1000 Genomes Project [24] or gnomAD [23]. Variants were annotated using vcf2maf v1.6.17 (https://github.com/mskcc/vcf2maf) and Ensembl VEP 92 [25], followed by CADD GRCh37-v1.4 [26], ClinVar [27] and the COSMIC database v88 (http://cancer.sanger.ac.uk) [28].
At final filtration, variants were further filtered for >20x total coverage, ≥6 reads supporting the mutant allele, and >0.05 and <0.99 frequency in the tumor sample. In order to exclude germline mutations, we retained only those variants present in gnomAD at a frequency of <0.0001 and with a CADD score of >20. We also used a targeted gene list (Supplementary Table 1) to reduce the number of variants for assessment. The methods used in the filtering and generation of the targeted gene list has been described in detail elsewhere [15]. Genes associated with clonal hematopoiesis were not rescued. Variants in the targeted gene list meeting one of the following criteria were considered significant:
-
(1)
Present in a recurrently mutated gene (gene mutated in ≥4 samples).
-
(2)
Splice site, nonsense mutation or frameshift/in-frame insertion or deletion.
-
(3)
Variant present ≥2 times in the COSMIC database v88 (http://cancer.sanger.ac.uk) [28], or designated as pathogenic/likely pathogenic in ClinVar [27].
-
(4)
Variant present once in the COSMIC database v88 (http://cancer.sanger.ac.uk) [28], but occurring within a known hotspot, or domain as described in the literature.
Assessment of “aberrant” somatic hypermutation
Coverage statistics were reviewed for the top 20 most frequently mutated genes reported to be targeted by “aberrant” somatic hypermutation (aSHM) [13, 29,30,31], and genes with an average of >90% of nucleotides in the first 2000 base pairs covered at >20x in 14 or more samples were retained for evaluation (BCL2, TMSB4X, and LTB). Variants in these 3 genes were retained if present in ≥6 reads, at a depth of >20 reads. To remove potential germline events, variants that were present in gnomAD or at an allele frequency of ≥0.4 were excluded. The number of mutations involving RGYW/WRCY motifs, transitions, and transversions were quantified. The RGYW/WRCY motif bias ratio was calculated by dividing the observed number of mutations by the expected number of mutations occurring within these motifs.
Copy number analysis
Copy number was estimated from the exome sequencing data using default settings for CNVkit v0.8.5 [32]. Calls from CNVkit were also exported in nexus.ogt format for review and annotation in Nexus 9.0 Software (BioDiscovery, Hawthorne, CA).
Fluorescent in-situ hybridization (FISH)
FISH was performed to test for CDKN2A deletion using the Vysis LSI CDKN2A SpectrumOrange Probe (9p21) (Abbott Molecular, Des Plaines IL, USA) with Vysis CEP 9 (9p11-q11 Alpha Satellite DNA) Aqua Probe (Abbott Molecular) as a reference. FISH for the BCL2 translocation was performed using BCL2 FISH DNA probe, Split Signal, Code no: Y5407 (Dako, Carpinteria, CA, USA). The hybridization procedure and additional methods have been described in detail elsewhere [15].
Evaluation of the clonal relationship between lymphoid and histiocytic/dendritic tumors
The clonal relationship between three HDT and paired lymphoid malignancies was assessed using the variants identified following variant filtration. In order to identify additional mutations that may have been filtered, and to examine models for the clonal architecture of the samples, SuperFreq version 1.2.6 [33] was used. Non-synonymous, exonic mutations were prioritized as per the default algorithm. The resulting clonal structures were revised in the context of tumor purity, variant allele frequencies, and copy number alterations.
Results
Cohort features: histology, immunohistochemistry and clonality studies
The 16 HDT cases in the cohort comprised HS (15/16) or IDCT (1/16) with a male predominance (13/16 cases, 81.25%). The associated malignancies were FL (6/16 cases), BCL (1/16 cases), CLL/SLL (2/16 cases), B-ALL (2/16 cases), T-ALL (4/16 cases), and PTCL NOS (1/16 cases) (Table 1). In fifteen cases, the HDT developed either concurrently or subsequently to the associated lymphoid malignancy. In one case, the HDT was diagnosed three years prior to the associated aggressive BCL. Seven cases have been previously published in the literature without sequencing data [1, 3, 4, 6], Table 1 and Supplementary Table 2.
Clonality studies were performed or had results available in all cases. Immunoglobulin (IG) or TRG gene rearrangements were detected in 15/16 HDT. Two cases (one CLL-associated and one B-ALL associated) had both IG and TRG rearrangements. In 9 cases with available information, the clonal IG or TRG rearrangement identified was similar to the associated lymphoid malignancy, either by PCR product size or by sequence similarity as previously published; however, in 4 cases the HDT was macrodissected from the associated lymphoid malignancy or the possibility of small volume residual lymphoid tumor was considered, and therefore contamination, though minimized, cannot be entirely excluded (Supplementary Table 3). All cases associated with FL had a BCL2 translocation confirmed either by FISH or PCR. In the case with negative clonality analysis, sequence similarity between the IGH/BCL2 breakpoints in the FL and HDT had been previously demonstrated [1].
Secondary histiocytic/dendritic neoplasms associated with diverse lymphoid malignancies have frequent alterations of the RAS/MAPK pathway
Whole exome sequencing was performed on 16 histiocytic/dendritic cell tumors and 3 matched lymphoid malignancies. Median coverage ranged from 223x to 417x. In the absence of matched germline samples, stringent variant filtration was performed as described above. All variants discovered are listed in Supplementary Table 4. Consistent with previous studies, we found a high frequency of mutations in the RAS/MAPK pathway, with mutations present in 14/16 cases (87.5%). The mutations were present independent of the associated lymphoid malignancy, although the two cases without RAS pathway mutations were both associated with T-ALL. The most frequently mutated gene was KRAS, occurring in 8 cases including 4/6 FL cases (p.Q61H [HDT02, HDT11, HDT13]; p.G12D [HDT12]), 2/4 T-ALL cases (p.K117N [HDT08]; p.G12D [HDT15]), 1/1 PTCL-associated case (p.G12A [HDT05]) and 1/2 CLL-associated cases (p.G12A [HDT14]). Mutations in BRAF and NRAS were each present in two cases. A BRAF p.V600E was present in a case associated with BCL [HDT06] and a p.D594G mutation was present in 1/6 FL-associated cases [HDT10]. NRAS mutations were present in 1/2 CLL-associated cases (p.Q61K [HDT03]) and 1/2 B-ALL-associated cases (p.G12D [HDT16]). Single mutations were identified in MAP2K1 in 1/6 FL-associated cases (p.F53L [HDT01]) and NF1 in 1/2 B-ALL- associated cases (p.C2223* [HDT04]).
With the exception of the NF1 mutation, all RAS pathway mutations discovered occur in well-described oncogenic hotspots. The NF1 alteration is a nonsense mutation and therefore predicted to be inactivating, and in the context of a tumor suppressor gene, significant. The mutational profile of the cases is detailed in Fig. 1.
Follicular lymphoma-associated histiocytic sarcoma and follicular lymphoma share a common mutational profile
In view of the known clonal relationship between lymphoid and histiocytic/dendritic tumors, we specifically assessed each case for alterations in genes that are known to be mutated in lymphoid malignancies (Supplementary Table 1). All FL-associated cases had mutations that occur early in the pathogenesis of FL, with 5/6 cases harboring mutations in CREBBP (p.S1436N [HDT02]; p.I1483F [HDT10]; p.R1446H [HDT11]; p.S1680del [HDT12 and HDT13] and p.R1446C [HDT13]) and 5/6 cases with mutations in KMT2D (p.Q3570* [HDT01]; p.W4730* and p.W4377* [HDT10]; c.14644-2 A > C and p.Q773* [HDT11] and p.R2801* [HDT12] and p.Q3394* [HDT13]). Additional mutations associated with FL/DLBCL were also present at lesser frequencies, including in TNFRSF14 (p.W12* [HDT12]; c.460 + 2 T > G [HDT13]), POU2AF1 (c.16 + 2 T > C [HDT01]; c.16 + 1 G > A [HDT12]), FOXO1 (p.R21H [HDT01]; p.E9* [HDT10]), B2M (p.L85fs [HDT10]); SGK1 (p.Q125* [HDT12]), PIK3CD (p.E1021K [HDT10]), CARD11 (p.G126D [HDT01]), and MYD88 (p.M240T [HDT01]), Fig. 1 and Supplementary Tables 4 and 5 [34]. Consistent with their relationship to the associated FL, all six cases had a BCL2 translocation documented by FISH or PCR and clonal IG gene rearrangements were demonstrated in all but one case.
We were able to evaluate the clonal relationship of one case of HS to an associated grade 3B FL [HDT01]. In this case, the diagnostic biopsy showed FL and HDT, and a biopsy taken 7 months later showed only HDT. We sequenced the FL component of the diagnostic biopsy and the HDT from the biopsy at 7 months. Both tumors shared identical IGK gene rearrangements (IGH rearrangement was not detected in either tumor), harbored identical mutations in KMT2D, BCL2 and POU2AF1, and a BCL2 translocation was identified in the HDT by FISH. The FL had additional mutations in BIRC3, MDM2 and PIM1 that were not present in the HS (Supplementary Table 6). Interestingly, the HS showed multiple additional “B-cell lymphoma” mutations that were not present in the associated FL, including in MYD88, WHSC1, CARD11, FOXO1, WAS, and P2RY8, as well as homozygous deletion of CDKN2A and a mutation in the RAS pathway gene, MAP2K1. These findings are consistent with origin of the HS and FL from a common neoplastic B-cell and suggest a pathogenic role for the RAS pathway in the development of the HS. MAP2K1 mutations, although associated with pediatric-type FL [35], are not common in adult-type FL [34] (Fig. 2).
a Histological features of FL grade 3B (H&E, original magnification ×40) and HS, biopsy composite with FL (left) and the sequenced biopsy at 7 months (right) (original magnification ×200). The FL is positive for PAX5 (original magnification ×100) and negative for CD68 (original magnification ×100). Both HS biopsies are negative for PAX5 (original magnification ×100) and positive for CD68, which is more focal in the biopsy at 7 months (original magnification ×100, left; original magnification ×200, right). b The FL and HS share identical clonal IG arrangements. c Comparison of the mutational profiles of clonally related FL and HS.
HDT associated with other mature B-cell malignancies may also have a mutational profile that is reminiscent of the associated lymphoid tumor. We identified mutations in CREBBP (p.S1680del and p.Q1209fs), GNA13 (p.Q27* and p.S9fs), IRF4 (p.C99R) and IRF8 (p.Q46*) in the single case of HS associated with aggressive BCL [HDT06]. In addition, 1/2 cases associated with CLL [HDT03] had mutations in NOTCH1 (p.P2514fs) and TP53 (p.R280G), both described in CLL. Neither CLL-associated case in this study had mutations in CREBBP, KMT2D, or other mutations typically associated with FL/DLBCL.
Histiocytic/dendritic neoplasms associated with lymphoblastic leukemia/lymphoma
The two cases associated with B-ALL had RAS pathway mutations as described above. In addition, both had clonal IG rearrangements and one case also had a clonal TRG gene rearrangement [HDT16]. Co-occurring NF1 and SETD2 mutations were present in case [HDT04] involving the GI tract, a finding that has previously been noted in a subset of primary HS [15].
Of the 4 T-ALL-associated sHDT, two did not have RAS pathway mutations; however, both had TRG rearrangements detected by PCR. No significant oncogenic activating mutations were detected in either of these cases. The remaining two cases associated with T-ALL both had mutations in KRAS and FBXW7 and identical TRG gene rearrangements to the associated T-ALL, which was analyzed separately. In the first case [HDT08], both T-ALL and HS samples had the same KRAS (p.K117N), FBXW7 (p.R465C), and PIK3CA (p.E542K) mutations as well as identical TRG gene rearrangements and loss of heterozygosity (LOH) at chromosome 9p; however, copy number analysis showed differences between the tumors, with LOH present at chromosome 4q in the T-ALL and not in the HS, and a gain of chromosome 20 present in the HS and not in the T-ALL confirming a clonal relationship between the two tumors and subsequent divergent evolution (Fig. 3). In addition, exome copy number calling suggested loss of CDKN2A in the T-ALL and not in the HDT; however, the loss was focal and we were unable to confirm by FISH.
a Copy number analysis of T-ALL showing LOH at chromosome 4q. (BAF: B allele frequency). b Copy number analysis of HS showing gain of chromosome 20. Both cases have LOH at chromosome 9p. c Mutational and copy number comparison for clonally related T-ALL and HS. d Photomicrograph of the T-ALL and HS (original magnification ×400).
The second case, [HDT15], showed substantially different mutational and copy number profiles between the two tumors. The T-ALL had TP53 (p.C242S) and FBXW7 (p.R465H) mutations, gain of chromosome 18 and a 17p deletion that were not present in the IDCT, and the IDCT had KRAS (p.G12D), FBXW7 (p.R479Q) and RB1 (p.E440K) mutations, as well as a gain of chromosome 12 that were not present in the T-ALL. Despite this, both tumors were clonally related by the same TRG rearrangement and LOH at chromosome 9p with deletion of CDKN2A (Fig. 4). In addition, we identified shared mutations in SETD1B (p.D458fs) and CARD11 (p.D200N) that were subclonal in the T-ALL, but present at a significant allele frequency in the IDCT. The significance of this finding is unclear.
Copy number analysis
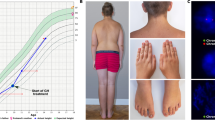
Copy number calling performed on exome sequencing data showed recurrent alterations in chromosome 9p, with LOH in 7 cases. Nine cases with likely losses of 9p21 were called, of which 6 had associated LOH of chromosome 9p. We confirmed homozygous deletions of CDKN2A in 7 of these cases by FISH (Fig. 5). In total, 9 cases had either confirmed deletion of CDKN2A or LOH of chromosome 9p.
a Copy number alterations across entire cohort, with recurrent losses of chromosome 9p at CDKN2A. b Illustrative example of FISH in two cases confirming homozygous deletion of CDKN2A (CEP 9 – Aqua; chromosome 9p.21 – Orange). c View of chromosome 9 in a case with homozygous deletion of CDKN2A (arrow). Copy number alterations are represented in the top panel and B-allele frequencies in the bottom panel (Nexus 9.0, BioDiscovery).
Aberrant somatic hypermutation
We performed a limited assessment to evaluate the presence of aSHM in the sHDT cases (Supplementary Table 7). This analysis was restricted to BCL2, TMSB4X, and LTB, due to limited coverage of intronic regions in our exome sequencing. BCL2 is a well described target of aSHM in both FL and diffuse large BCLs, while TMSB4X and LTB are more recently described aSHM targets found at high frequency in diffuse large BCL [31]. A total of 59 mutations were identified in the 16 sHDT cases. All mutations occurred in cases associated with FL (n = 5) or BCL (n = 1) and were not present in cases associated with any other lymphoid malignancy. Forty-eight of the 59 mutations involved the BCL2 gene, 9 were present in TMSB4X gene, and 2 were present in LTB. The ratio of transitions to transversions was 1.36 and 20/59 mutations were present in RGYW/WRCY motifs, the latter representing an RGYW/WRCY mutational motif bias of 5.95x of expected. These data are characteristic of an activation induced cytidine deaminase (AID)-associated somatic hypermutation signature that is characteristic of germinal center and post-germinal center BCLs, providing further support for the relationship between the FL and the associated HS. Of particular interest, we were also able to compare the spectrum of aSHM in one case of FL with the associated HS [HDT01], and importantly this FL showed a nearly identical spectrum of aSHM as the HS (12/15 identical; Supplementary Table 7).
Discussion
Our study provides new data and insights into the molecular pathogenesis of secondary histiocytic/dendritic neoplasms. Through whole exome sequencing of 16 cases, we reaffirm the significance of the RAS/MAPK pathway in these lesions and propose models of clonal divergence for three cases in which a matched lymphoid malignancy was available.
We report a high frequency of RAS/MAPK pathway mutations, with well-known pathogenic mutations identified in 14/16 cases (87.5%). This finding is consistent with previous series and case reports describing the importance of the RAS pathway in the pathogenesis of histiocytic and dendritic tumors [13, 15, 36,37,38,39]. All cases of sHDT, regardless of the associated lymphoma subtype, had evidence of a clonal relationship to the associated lymphoid tumor through clonal IG or TRG gene rearrangements, or IGH/BCL2 sequence similarity as documented in this study or in our previous reports [1, 3, 4, 6]. Strikingly, although the paired associated lymphoma was not available in most cases, the mutational profiles of eight of the nine cases associated with mature B-cell neoplasms contained many characteristic mutations of the associated BCL subtype. Finally, in the one case in which the paired FL was available, multiple shared mutations were detected, including most of the mutations attributable to aSHM, further substantiating a clonal relationship between the associated BCL and the HS.
Transdifferentiation has been proposed as a mechanism by which tumors of diverse lineages are derived from a common clonal origin [1, 2, 40]. Although it has been thought that mature lymphoid cells lack lineage plasticity, it has been shown that B cells and committed T-cell progenitors can be reprogrammed into macrophage/dendritic cells under the influence of transcription factors including C/EBPα, C/EBPβ, and PU.1 [41,42,43]. In B cells, loss of PAX5 expression is thought to be important in this process, as forced expression of C/EBPα results in the downregulation of PAX5 and activation of the myeloid/macrophage differentiation programs [42]. Furthermore, under appropriate conditions CRE-mediated PAX5 gene deletion alone can allow pro-B cells regain the capacity to differentiate into macrophages [44]. In accordance with these experimental data, loss of immunohistochemical expression of PAX5 was seen in all our cases studied and has been documented in other cases of sHDT [1, 3].
Investigators have also speculated as to the precise nature and stage of development of the common neoplastic cell from which these clonally related tumors originate [4, 5, 45, 46]. Dedifferentiation of the lymphoid malignancy to an uncommitted progenitor with subsequent differentiation along the myeloid/dendritic lineage has been considered[1, 3, 45]; however, evidence of an uncommitted, immature progenitor cell population has not been found. In cases associated with FL, origin from a common precursor cell that has at least reached a pre-B-cell stage of differentiation was considered by Feldman et al. in showing that FL-associated HS harbored IG rearrangements and IGH/BCL2 translocations [1]. More recently Geyer et al. showed evidence for a common precursor in a case of B-ALL associated HS which had IGH/MYC translocations in both histiocytic and lymphoid tumors but clonal divergence and acquisition of BRAF and likely KRAS mutations in the HS [12]. In support of the potential for transdifferentiation to occur at a relatively late stage of B-cell development, somatically hypermutated IGH genes, considered a marker of B-cell maturity, have been found in HDT associated with FL and SMZL [40, 47], and an aberrant somatic hypermutation signature has been reported in a subset of HS cases that were enriched for cases with a history of B-cell malignancy [13]. We also found evidence of aSHM (a characteristic of BCL that have passed through a germinal center stage of differentiation) in 6 sHDT associated with germinal center-derived BCL (5 FL and 1 aggressive BCL), while sHDT cases associated with other hematopoietic tumors (CLL, B-ALL, PTCL and T-ALL) showed no evidence of aSHM.
Other studies have also emphasized clonal divergence demonstrated by the acquisition of additional abnormalities in the associated lymphoid malignancy that are not present in the HDT, including those by Brunner et al, in which the FL and HS shared the IGH/BCL2 translocation but the FL had additional cytogenetic abnormalities [9] and Buser et al, who reported an early T-cell precursor LBL that had an NRAS p.G13D mutation not present in the HDT [46]. Similarly, in our three cases with matched lymphoid and histiocytic/dendritic neoplasms it is notable that while the lymphoid and histiocytic/dendritic tumors shared common structural or mutational alterations, each case showed abnormalities within the lymphoid malignancy that were not present in the HDT, in keeping with origin of the HDT from a common late stage neoplastic precursor or an undetected subclone of the lymphoid tumor, with subsequent clonal divergence.
The larger number of sHDT cases associated with FL allows us to make some observations regarding the relationship between the two tumors. In considering the evolutionary relationship between HDT and FL it is important to take into account the multiple studies that have elegantly shown the stepwise clonal evolution and pathogenesis of FL, with the initial IGH/BCL2 translocation, followed by mutations in genes including CREBBP, KMT2D, and EZH2 [48,49,50]. In our series, all HDT cases associated with FL had a similar mutational profile to FL, including the BCL2 translocation, IG gene rearrangement, mutations in CREBBP and/or KMT2D, and 5/6 had evidence of AID-associated aSHM. All cases also had alterations in RAS/MAPK pathway genes rarely seen in adult-type FL and not present in one matched associated FL, indicating the crucial importance of the RAS/MAPK pathway in the pathogenesis of the HDT in these cases. Consistent with our findings, a Langerhans cell sarcoma in a patient with a history of FL was recently shown to have the IGH/BCL2 translocation, CREBBP and KRAS mutations [11], and HS occurring in two patients with histories of FL and DLBCL were shown to have mutations in KRAS, CREBBP, and KMT2D; and BRAF, KRAS, KMT2D, and EP300, respectively [13]. Based on our data and data from the literature, we surmise that FL-associated HDT arises from a relatively late stage neoplastic B-cell complete with IGH/BCL2 translocation, IG gene rearrangement, and a spectrum of gene mutations that are characteristic of the mutational profile of mature FL, including those associated with AID induced aSHM. The critical “transdifferentiation” step to HDT appears to be associated with the acquisition of RAS/MAPK pathway alterations. While the FL-associated sHDT and the FL share many abnormalities, both tumors may have distinct mutations, as exemplified by the single matched FL-associated HDT in our study, indicating further mutational divergence of each tumor.
Similarly, the non-FL associated HDT cases also possessed mutations commonly found in the associated BCL. One CLL-associated case in our study had a mutation in NOTCH1 at a site previously described as mutated in CLL, and a second case associated with aggressive BCL showed striking similarity to the FL-associated cases with mutations in CREBBP, but also in IRF4, IRF8, and GNA13 frequently reported in DLBCL [51, 52]. While the number of cases studied for these B-lymphoma subtypes are small, these data are also consistent with transdifferentiation of the sHDT from the associated BCL.
While similarities at a genomic level between B-cell neoplasms and sHDT arising in the context of a B-cell malignancy are perhaps not surprising, it is notable that mutational overlap between HS and BCL has also been described in cases of HS occurring in patients without a history of BCL (so-called primary HS) [13, 15]. Analogous to our secondary cases associated with BCL, a subset of primary HS cases have been shown to harbor mutations in genes such as KMT2D, CREBBP, PIK3CD, MYD88, TNFRSF14, or POU2AF1 and/or to have clonal IG rearrangements [13, 15, 53]. In addition, as previously mentioned, one study demonstrated an aberrant somatic hypermutation signature in HS, including cases of primary HS [13] and rare instances of HS preceding a diagnosis of lymphoid malignancy have also been described [54], including one such case in the current series. These data suggest that a proportion of primary HS develop from a progenitor with B-lineage differentiation potential or possibly through transdifferentiation from a preexisting occult B-cell neoplasm, similar to the majority of B-cell related secondary HS described in the current study.
The identification of RAS pathway mutations in 14/16 of our sHDT cases, and the extensive literature on the importance of the RAS pathway in the pathogenesis of primary HS and other dendritic cell tumors is consistent with the notion that alterations in this pathway are likely to play a role in the transformation to sHDT. For the two T-ALL-associated cases without RAS pathway mutations, we cannot discount the possibility that another mechanism may underlie transformation to sHDT. In addition, in one case in our study, the same RAS pathway mutation was present in both the HDT and the associated T-ALL, indicating that other mechanisms for transformation may be at play. The absence of matched lymphoid malignancy in most cases prevents us from definitively associating the RAS/MAPK pathway mutations with transformation to sHDT; however, at least for the FL associated sHDT, the rarity of RAS pathway alterations in FL suggests RAS/MAPK mutations are critical in the pathogenesis of this type of sHDT.
In conclusion, our study highlights the importance of the RAS/MAPK pathway and provides further insight into the pathogenesis of the rare sHDT associated with diverse lymphoid malignancies. We show that in addition to RAS mutations, BCL-associated HDT may share a mutational profile with the associated lymphoid neoplasm. In particular, we show that FL-associated cases have mutational hallmarks of FL beyond the IGH/BCL2 translocation, in keeping with origin from a common neoplastic B-cell.
Data availability
All genomic data from this study will be deposited in the dbGaP database (www.ncbi.nlm.nih.gov/gap).
References
Feldman AL, Arber DA, Pittaluga S, Martinez A, Burke JS, Raffeld M, et al. Clonally related follicular lymphomas and histiocytic/dendritic cell sarcomas: evidence for transdifferentiation of the follicular lymphoma clone. Blood 2008;111:5433–9.
West DS, Dogan A, Quint PS, Tricker-Klar ML, Porcher JC, Ketterling RP, et al. Clonally related follicular lymphomas and Langerhans cell neoplasms: expanding the spectrum of transdifferentiation. Am J Surg Pathol. 2013;37:978–86.
Shao H, Xi L, Raffeld M, Feldman AL, Ketterling RP, Knudson R, et al. Clonally related histiocytic/dendritic cell sarcoma and chronic lymphocytic leukemia/small lymphocytic lymphoma: a study of seven cases. Mod Pathol. 2011;24:1421–32.
Feldman AL, Minniti C, Santi M, Downing JR, Raffeld M, Jaffe ES. Histiocytic sarcoma after acute lymphoblastic leukaemia: a common clonal origin. Lancet Oncol. 2004;5:248–50.
Kumar R, Khan SP, Joshi DD, Shaw GR, Ketterling RP, Feldman AL. Pediatric histiocytic sarcoma clonally related to precursor B-cell acute lymphoblastic leukemia with homozygous deletion of CDKN2A encoding p16INK4A. Pediatr Blood Cancer. 2011;56:307–10.
Feldman AL, Berthold F, Arceci RJ, Abramowsky C, Shehata BM, Mann KP, et al. Clonal relationship between precursor T-lymphoblastic leukaemia/lymphoma and Langerhans-cell histiocytosis. Lancet Oncol. 2005;6:435–7.
Facchetti F, Pileri SA, Lorenzi L, Tabanelli V, Rimsza L, Pittaluga S, et al. Histiocytic and dendritic cell neoplasms: what have we learnt by studying 67 cases. Virchows Arch. 2017;471:467–89.
Xerri L, Adelaide J, Popovici C, Garnier S, Guille A, Mescam-Mancini L, et al. CDKN2A/B deletion and double-hit mutations of the MAPK pathway underlie the aggressive behavior of Langerhans cell tumors. Am J Surg Pathol. 2018;42:150–9.
Brunner P, Rufle A, Dirnhofer S, Lohri A, Willi N, Cathomas G, et al. Follicular lymphoma transformation into histiocytic sarcoma: indications for a common neoplastic progenitor. Leukemia. 2014;28:1937–40.
Gounder MM, Solit DB, Tap WD. Trametinib in Histiocytic Sarcoma with an Activating MAP2K1 (MEK1) Mutation. N Engl J Med. 2018;378:1945–7.
Choi SM, Andea AA, Wang M, Behdad A, Shao L, Zhang Y, et al. KRAS mutation in secondary malignant histiocytosis arising from low grade follicular lymphoma. Diagn Pathol. 2018;13:78.
Geyer JT, Yigit N, Miyaguchi A, Cheng S, Casano J, Mathew S, et al. Histiocytic Sarcoma Following B-Lymphoblastic Leukemia/Lymphoma. Am J Clin Pathol. 2019;152:486–94.
Shanmugam V, Griffin GK, Jacobsen ED, Fletcher CDM, Sholl LM, Hornick JL. Identification of diverse activating mutations of the RAS-MAPK pathway in histiocytic sarcoma. Mod Pathol. 2019;32:830–43.
Thakral B, Khoury JD. Histiocytic sarcoma: secondary neoplasm or “transdifferentiation” in the setting of B-acute lymphoblastic leukemia. Blood. 2016;128:2475.
Egan C, Nicolae A, Lack J, Chung HJ, Skarshaug S, Pham TA, et al. Genomic profiling of primary histiocytic sarcoma reveals two molecular subgroups. Haematologica. 2020;105:951–60.
Bolger AM, Lohse M, Usadel B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics 2014;30:2114–20.
Li H. Aligning sequence reads, clone sequences and assembly contigs with BWA-MEM. arXiv:13033997v1 [q-bioGN]. 2013.
Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, et al. The sequence alignment/map format and SAMtools. Bioinformatics 2009;25:2078–9.
McKenna A, Hanna M, Banks E, Sivachenko A, Cibulskis K, Kernytsky A, et al. The genome analysis toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 2010;20:1297–303.
Garcia-Alcalde F, Okonechnikov K, Carbonell J, Cruz LM, Gotz S, Tarazona S, et al. Qualimap: evaluating next-generation sequencing alignment data. Bioinformatics. 2012;28:2678–9.
Barnett DW, Garrison EK, Quinlan AR, Stromberg MP, Marth GT. BamTools: a C++ API and toolkit for analyzing and managing BAM files. Bioinformatics. 2011;27:1691–2.
Cibulskis K, Lawrence MS, Carter SL, Sivachenko A, Jaffe D, Sougnez C, et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat Biotechnol. 2013;31:213–9.
Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, Fennell T, et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature. 2016;536:285–91.
Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, Korbel JO, et al. A global reference for human genetic variation. Nature. 2015;526:68–74.
McLaren W, Gil L, Hunt SE, Riat HS, Ritchie GR, Thormann A, et al. The ensembl variant effect predictor. Genome Biol. 2016;17:122.
Rentzsch P, Witten D, Cooper GM, Shendure J, Kircher M. CADD: predicting the deleteriousness of variants throughout the human genome. Nucleic Acids Res. 2019;47:D886–d894.
Landrum MJ, Lee JM, Benson M, Brown GR, Chao C, Chitipiralla S, et al. ClinVar: improving access to variant interpretations and supporting evidence. Nucleic Acids Res. 2018;46:D1062–d1067.
Forbes SA, Beare D, Boutselakis H, Bamford S, Bindal N, Tate J, et al. COSMIC: somatic cancer genetics at high-resolution. Nucleic Acids Res. 2017;45:D777–d783.
Burkhard R, Bhagat G, Cogliatti SB, Rossi D, Gaidano G, Pasqualucci L, et al. BCL2 mutation spectrum in B-cell non-Hodgkin lymphomas and patterns associated with evolution of follicular lymphoma. Hematol Oncol. 2015;33:23–30.
Pasqualucci L, Neumeister P, Goossens T, Nanjangud G, Chaganti RS, Kuppers R, et al. Hypermutation of multiple proto-oncogenes in B-cell diffuse large-cell lymphomas. Nature. 2001;412:341–6.
Khodabakhshi AH, Morin RD, Fejes AP, Mungall AJ, Mungall KL, Bolger-Munro M, et al. Recurrent targets of aberrant somatic hypermutation in lymphoma. Oncotarget. 2012;3:1308–19.
Talevich E, Shain AH, Botton T, Bastian BC. CNVkit: Genome-Wide Copy Number Detection and Visualization from Targeted DNA Sequencing. PLoS Comput Biol. 2016;12:e1004873.
Flensburg C, Sargeant T, Oshlack A, Majewski I. SuperFreq: Integrated mutation detection and clonal tracking in cancer. bioRxiv. 2018;380097.
Krysiak K, Gomez F, White BS, Matlock M, Miller CA, Trani L, et al. Recurrent somatic mutations affecting B-cell receptor signaling pathway genes in follicular lymphoma. Blood. 2017;129:473–83.
Louissaint A Jr., Schafernak KT, Geyer JT, Kovach AE, Ghandi M, Gratzinger D, et al. Pediatric-type nodal follicular lymphoma: a biologically distinct lymphoma with frequent MAPK pathway mutations. Blood. 2016;128:1093–1100.
Diamond EL, Durham BH, Haroche J, Yao Z, Ma J, Parikh SA, et al. Diverse and targetable kinase alterations drive histiocytic neoplasms. Cancer Discov. 2016;6:154–65.
Emile JF, Diamond EL, Helias-Rodzewicz Z, Cohen-Aubart F, Charlotte F, Hyman DM, et al. Recurrent RAS and PIK3CA mutations in Erdheim-Chester disease. Blood. 2014;124:3016–9.
Chakraborty R, Hampton OA, Shen X, Simko SJ, Shih A, Abhyankar H, et al. Mutually exclusive recurrent somatic mutations in MAP2K1 and BRAF support a central role for ERK activation in LCH pathogenesis. Blood. 2014;124:3007–15.
Badalian-Very G, Vergilio JA, Degar BA, MacConaill LE, Brandner B, Calicchio ML, et al. Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood. 2010;116:1919–23.
Wang E, Hutchinson CB, Huang Q, Sebastian S, Rehder C, Kanaly A, et al. Histiocytic sarcoma arising in indolent small B-cell lymphoma: report of two cases with molecular/genetic evidence suggestive of a ‘transdifferentiation’ during the clonal evolution. Leuk Lymphoma. 2010;51:802–12.
Laiosa CV, Stadtfeld M, Xie H, de Andres-Aguayo L, Graf T. Reprogramming of committed T cell progenitors to macrophages and dendritic cells by C/EBP alpha and PU.1 transcription factors. Immunity. 2006;25:731–44.
Xie H, Ye M, Feng R, Graf T. Stepwise reprogramming of B cells into macrophages. Cell. 2004;117:663–76.
Cirovic B, Schonheit J, Kowenz-Leutz E, Ivanovska J, Klement C, Pronina N, et al. C/EBP-induced transdifferentiation reveals granulocyte-macrophage precursor-like plasticity of B cells. Stem Cell Rep. 2017;8:346–59.
Mikkola I, Heavey B, Horcher M, Busslinger M. Reversion of B cell commitment upon loss of Pax5 expression. Science. 2002;297:110–3.
Ratei R, Hummel M, Anagnostopoulos I, Jahne D, Arnold R, Dorken B, et al. Common clonal origin of an acute B-lymphoblastic leukemia and a Langerhans’ cell sarcoma: evidence for hematopoietic plasticity. Haematologica. 2010;95:1461–6.
Buser L, Bihl M, Rufle A, Mickys U, Tavoriene I, Griskevicius L, et al. Unique composite hematolymphoid tumor consisting of a pro-T lymphoblastic lymphoma and an indeterminate dendritic cell tumor: evidence for divergent common progenitor cell differentiation. Pathobiology. 2014;81:199–205.
Wang E, Papalas J, Hutchinson CB, Kulbacki E, Huang Q, Sebastian S, et al. Sequential development of histiocytic sarcoma and diffuse large b-cell lymphoma in a patient with a remote history of follicular lymphoma with genotypic evidence of a clonal relationship: a divergent (bilineal) neoplastic transformation of an indolent B-cell lymphoma in a single individual. Am J Surg Pathol. 2011;35:457–63.
Green MR, Gentles AJ, Nair RV, Irish JM, Kihira S, Liu CL, et al. Hierarchy in somatic mutations arising during genomic evolution and progression of follicular lymphoma. Blood. 2013;121:1604–11.
Okosun J, Bodor C, Wang J, Araf S, Yang CY, Pan C, et al. Integrated genomic analysis identifies recurrent mutations and evolution patterns driving the initiation and progression of follicular lymphoma. Nat Genet. 2014;46:176–81.
Green MR, Kihira S, Liu CL, Nair RV, Salari R, Gentles AJ, et al. Mutations in early follicular lymphoma progenitors are associated with suppressed antigen presentation. Proc Natl Acad Sci USA. 2015;112:E1116–1125.
Karube K, Enjuanes A, Dlouhy I, Jares P, Martin-Garcia D, Nadeu F, et al. Integrating genomic alterations in diffuse large B-cell lymphoma identifies new relevant pathways and potential therapeutic targets. Leukemia. 2018;32:675–84.
Schmitz R, Wright GW, Huang DW, Johnson CA, Phelan JD, Wang JQ, et al. Genetics and pathogenesis of diffuse large B-cell lymphoma. N Engl J Med. 2018;378:1396–407.
Chen W, Lau SK, Fong D, Wang J, Wang E, Arber DA, et al. High frequency of clonal immunoglobulin receptor gene rearrangements in sporadic histiocytic/dendritic cell sarcomas. Am J Surg Pathol. 2009;33:863–73.
Fernandez-Pol S, Bangs CD, Cherry A, Arber DA, Gratzinger D. Two cases of histiocytic sarcoma with BCL2 translocations and occult or subsequent follicular lymphoma. Hum Pathol. 2016;55:39–43.
Funding
This work was supported by the Intramural Research Program of the National Institutes of Health, Center for Cancer Research, National Cancer Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Egan, C., Lack, J., Skarshaug, S. et al. The mutational landscape of histiocytic sarcoma associated with lymphoid malignancy. Mod Pathol 34, 336–347 (2021). https://doi.org/10.1038/s41379-020-00673-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41379-020-00673-x
This article is cited by
-
Synchronous clonally related anaplastic large cell lymphoma and malignant histiocytosis
Diagnostic Pathology (2025)
-
Establishment of human histiocytic sarcoma organoids dependent on the SHH/YAP pathway
Human Cell (2025)
-
Plasmacytoid dendritic cell proliferations, malignant histiocytic (macrophage/dendritic cell) neoplasms and follicular dendritic cell neoplasms: report from the 2024 Joint CSHP/EA4HP/SH workshop
Virchows Archiv (2025)
-
Pathologic characteristics of histiocytic and dendritic cell neoplasms
Blood Research (2024)
-
NF1 mutation and TUBB3 amplification in gastric histiocytic sarcoma: a case report and literature review
Medical Molecular Morphology (2024)