Abstract
BDNF plays a crucial role in shaping the structure and function of neurons. In rodents, BDNF signaling in the dorsolateral striatum (DLS) is part of an endogenous pathway that protects against the development of phenotypes associated with alcohol use. Dysregulation of BDNF levels in the cortex or dysfunction of BDNF/TrkB signaling in the DLS of rodents results in the escalation of alcohol drinking and compulsive alcohol intake. The major source of BDNF in the striatum is the prefrontal cortex. We identified a small ensemble of BDNF-positive neurons in the mouse ventrolateral orbitofrontal cortex (vlOFC), a region implicated in alcohol use disorder (AUD), that extend axonal projections to the DLS, which is associated with alcohol drinking behaviors. We speculated that BDNF in vlOFC-to-DLS circuit may play a role in limiting alcohol drinking and that heavy alcohol intake disrupts this protective pathway. We found that BDNF expression is reduced in the vlOFC of male but not female mice after long-term cycles of binge alcohol drinking and withdrawal. We further discovered that overexpression of BDNF in vlOFC-to-DLS but not in vlOFC-to-dorsomedial striatum (DMS) or M2 motor cortex-to-DLS circuit reduces alcohol but not sucrose intake and preference. We further showed that BDNF in vlOFC-to DLS reduces alcohol self-administration, alcohol seeking, and relapse. Finally, we found that systemic administration of BDNF receptor TrkB agonist, LM22A-4, dampens habitual alcohol seeking. Together, our data suggest that BDNF in a small ensemble of vlOFC-to-DLS neurons may gate alcohol drinking behaviors by attenuating habitual alcohol seeking.
Similar content being viewed by others
Introduction
The brain-derived neurotrophic factor (BDNF) belongs to the neurotrophins family [1]. BDNF plays a vital role in neuronal differentiation and maturation [2], synaptic plasticity, learning, and memory [3]. BDNF is highly expressed in the adult rodent brain [4, 5]. The majority of BDNF is stored in presynaptic dense core vesicles and is released in an activity-dependent manner upon neuronal depolarization [6]. BDNF binds to tropomyosin receptor kinase B (TrkB) receptor, which activates PI3K/AKT, and/or PLC/PKC, and/or ERK1/2 signaling, leading to the activation of transcription [7] or translation [8]. Dysregulation of BDNF signaling has been implicated in psychiatric disorders, such as depression [9], schizophrenia [9], and addiction [10].
Only 10–15% of alcohol users develop AUD [11], implying that there are protective mechanisms that prevent the development of the disorder in the majority of the population. Using rodents as a model system, we and others, presented data to suggest that BDNF is part of a protective mechanism that gates the development of heavy alcohol intake and abuse (reviews [12,13,14]). For example, we found that the activation of BDNF/TrkB/ERK1/2 but not PI3K/AKT, or PLC/PKC signaling in the DLS, a region involved in habitual behavior [15], keeps alcohol intake in moderation by activating the transcription machinery [16,17,18,19].
The prefrontal cortex (PFC) is the major source of BDNF in the striatum [20,21,22,23], and we and others, reported that escalation of alcohol intake results from a breakdown in BDNF signaling. Specifically, chronic high alcohol consumption attenuates BDNF expression in corticostriatal regions of rodents [24,25,26], which is mediated by the microRNA machinery in the medial prefrontal cortex (mPFC) [25, 26], resulting in escalation of alcohol consumption [25, 26]. We further found that the transition from moderate to heavy alcohol intake is also mediated by the alterations in the membranal localization of the BDNF receptors, TrkB and p75NTR in the DLS of rats [27]. Finally, we reported that transgenic mice carrying a polymorphism within the BDNF gene that disrupts BDNF release [28], compulsively drink alcohol, exhibit a reduction in the anxiolytic actions of alcohol and an increase in alcohol preference over social interaction in mice [29, 30]. Together, these data suggest that BDNF in corticostriatal regions gates alcohol drinking behaviors, and that AUD-like phenotypes develop in part when BDNF signaling ceases to function.
The cortical regions that release BDNF into the DLS have not been carefully mapped out. Using a combination of transgenic mouse lines together with a viral-mediated retrograde tracing strategy, we characterized BDNF-expressing cortical neurons that project to the DLS [23]. We found that a small ensemble of BDNF-positive neurons in the vlOFC extend axonal projections to the DLS [23]. The OFC plays a critical role in decision-making, reward-prediction error [31,32,33], reward information [34], and stimulus-outcome behaviors [35,36,37]. The OFC has also been identified as a critical region in AUD [38, 39]. Specifically, in humans, alcohol dependence reduces white matter and neuronal density in the OFC [40,41,42], and the connectivity between OFC and striatum is altered in abstinent subjects [43]. In rodents, alcohol affects the activity of OFC neurons [44, 45]. Furthermore, OFC lesions or chemogenetic inhibition increase alcohol drinking [46,47,48] and decrease context and cue-induced reinstatement [49, 50]. Together, these data suggest that the OFC is an important target of alcohol. However, whether BDNF in vlOFC-to-DLS projecting neurons affects alcohol drinking behaviors is unknown. We report that BDNF expression is reduced in the vlOFC of mice following 7 weeks of intermittent access to 20% alcohol in a 2-bottle choice procedure (IA20%2BC). We further show that overexpression of BDNF in vlOFC-to-DLS circuit limits alcohol intake, seeking, and relapse. Finally, we show that the systemic administration of a TrkB agonist reverts habitual to goal-directed alcohol seeking.
Materials and methods
Reagents, preparation of solutions, collection of brain samples, real-time PCR, purchasing of viruses, stereotaxic viral infection, confirmation of viral expression, and behavioral procedures can be found in the supplementary material.
Animals
Male (152) and female (38) C57BL/6J mice (6–8 weeks) were purchased from Jackson Laboratory and were allowed one week of habituation before experiments began. Mice were individually housed on paper-chip bedding, under a reverse 12-h light-dark cycle. Temperature and humidity were kept constant at 22 ± 2°C, and relative humidity was maintained at 50 ± 5%. Mice were allowed access to food and tap water ad libitum. All animal procedures were approved by the University’s Institutional Animal Care and Use Committee (IACUC) and were conducted in agreement with the Association for Assessment and Accreditation of Laboratory Animal Care.
Behavioral procedures
Intermittent access to 20% alcohol two-bottle choice (IA20%2BC)
IA20%2BC was conducted as previously described [51]. Briefly, mice were given one bottle of 20% alcohol (v/v) in tap water and one bottle of water for 24 h on Monday, Wednesday, and Friday, with 24 or 48-h (weekend) of alcohol withdrawal periods during which mice consumed only water. The placement of water or alcohol bottles was alternated between each session to avoid side preference. Alcohol and water bottles were weighed at the beginning and end of each alcohol drinking session, and alcohol intake (g/kg of body weight), water intake (ml/kg) and total fluid intake (ml/kg) were calculated. Two bottles containing water and alcohol in an empty cage were used to evaluate the spillage. Alcohol preference ratio was calculated by dividing the volume of alcohol consumed to the total volume of fluid intake.
Operant alcohol self-administration
Alcohol operant self-administration training and habitual alcohol seeking training was performed as described previously [52]. First, mice underwent 7 weeks IA20%2BC. Mice drinking more than 12.5 g/kg were selected for the experiment. Alcohol operant self-administration training was initiated under a fixed-ratio (FR) 1 schedule, i.e., one lever press resulted in the delivery of one reward, for four 6-h FR1 sessions, followed by four 4-h FR1 sessions, and finally four 2-h FR1 sessions. Reward deliveries were paired with a 3-s tone and illumination of a cue light. All remaining sessions lasted 2 h. Mice were then trained on a random-interval (RI) schedule, during which rewards were delivered with random delays following active lever presses according to previous studies [53,54,55]. Timepoints were pseudo-randomly assigned by the computer program. Mice first underwent 5 sessions on an RI30 schedule (delays averaging 30 s after lever press, with intervals ranging from 0 to 60 s). Mice were then subjected to 5 sessions of RI60 training (intervals ranging from 30 to 90 s). Mice were divided into 2 groups with similar numbers of active lever presses (106.41 ± 40.78 and 116.35 ± 58.35), port entries (96.35 ± 45.73 and 72.61 ± 14.36), and amount of self-administered alcohol (2.55 ± 0.70 and 2.46 ± 0.79 g/kg/2 h). Three mice were excluded from the operant self-administration procedure due to low pressing numbers. BDNF or mCherry control was then overexpressed in the vlOFC-to-DLS circuit. Three weeks following surgery, RI30 was resumed for 5 sessions, followed by RI60 until the end of the experiment. The number of active lever presses and reward port entries, as well as the number of reward deliveries, were recorded during each session.
LM22A-4 administration: Thirty minutes prior to a degradation session, mice received intraperitoneal (i.p.) administration of saline or LM22A-4 (100 mg/kg) [29].
Contingency degradation
Contingency degradation was used as previously described [56, 57] to test the sensitivity of mice to changes in the response-outcome association. The procedure was conducted across nondegraded (ND) and degraded (D) sessions. During the 2-h degraded session, a lever was extended, but lever presses produced no consequences. In total, 2-3 degradation sessions were performed. During the nondegraded sessions, alcohol deliveries occurred at a rate that was determined based on each animal’s average reward rate during the four RI60 schedules of nondegraded sessions, prior to degradation.
Extinction and reacquisition
Extinction and reacquisition procedures were conducted following completion of the RI training phase and contingency degradation test. Mice underwent 13 daily extinction sessions (2-h each), during which both levers were available, but lever presses were not paired with alcohol deliveries and no cues associated with reward delivery were presented.
The first extinction session was used to assess alcohol-seeking behavior in the absence of reinforcement, as measured by the number of active lever presses and port entries. Subsequent extinction sessions continued until responding stabilized across sessions and decreased to at least half of lever presses compared to previous RI sessions.
Following the last extinction session, reacquisition training (2-h) was conducted during which lever presses were paired with cues and alcohol deliveries to evaluate the reinstatement of operant responding. The session parameters were identical to FR1 schedule.
Statistical analysis
D’Agostino–Pearson normality test, Shapiro–Wilk normality test and F-test/Levene tests were used to verify the normal distribution of variables and the homogeneity of variance, respectively. Data were analyzed using the appropriate statistical test, including two-tailed unpaired t-test, one-way ANOVA, two-way ANOVA with and without repeated measures followed by post-hoc test. GraphPad Prism 9 was used for statistical analyses. All data are expressed as mean +/− SEM. Significance was set at p < 0.05.
Results
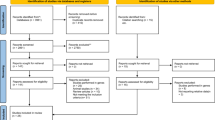
High alcohol drinking reduces BDNF expression in the vlOFC
We identified a small ensemble of vlOFC neurons expressing BDNF that project to the DLS of mice [23]. Since BDNF signaling in the DLS is a locus for keeping alcohol drinking in moderation [18, 19], we hypothesized that normal levels of BDNF in the OFC are required to control the development of heavy alcohol intake. We further hypothesized that breakdown in BDNF signaling in OFC-to-DLS circuit promotes the escalation of alcohol intake. To address these hypotheses, we first tested whether high alcohol drinking alters BDNF levels in the vlOFC. Mice underwent 7 weeks of IA20%-2BC procedure [52] (Fig. 1a). Male mice consumed an average of 14.47 ± 1 g/kg/24 h (Supplementary Fig. 1a–c; Supplementary Table 1), and female mice drank an average of 19.27 ± 1.1 g/kg/24 h (Supplementary Fig. 1d–f; Supplementary Table 1). Mice were sacrificed 4 h after the beginning of the last drinking session (“binge”) and 24 h after the last drinking session (“withdrawal”), and BDNF expression was measured. We found that BDNF mRNA in the vlOFC was significantly decreased in male mice that were subjected to 7 weeks of IA20%2BC during both binge and withdrawal as compared to mice consuming water only (Fig. 1b) (One-way ANOVA: effect of treatment, F(2,15) = 5.705, p = 0.014; Post hoc Dunnett’s multiple comparison test indicates significant differences between water and binge drinking and between water and withdrawal). We further discovered that alcohol-mediated reduction in BDNF mRNA levels is localized to the vlOFC since no changes in BDNF expression were detected in the medial OFC (mOFC) (Fig. 1c) (One-way ANOVA: effect of treatment, F(2,15) = 0.846, p = 0.448). As BDNF neurons in M2 motor cortex send dense projections to the DLS [23], we examined the level of BDNF mRNA in this region in response to high alcohol consumption. As shown in Fig. 1d, BDNF mRNA levels in M2 motor cortex of male mice were unchanged by alcohol (One-way ANOVA: effect of treatment, F(2,15) = 0.354, p = 0.707). Interestingly, the alterations of BDNF levels were sex specific as BDNF mRNA levels in the vlOFC, mOFC or M2 of female mice were unaltered after binge drinking and withdrawal from 7 weeks of IA20%2BC (Fig. 1e–g) (one-way ANOVA: vlOFC, effect of treatment, F(2,16) = 1.13, p = 0.347; mOFC, effect of treatment, F(2,15) = 2.88, p = 0.087; M2 motor cortex, effect of treatment, F(2,17) = 0.484, p = 0.624). Together, these data suggest that chronic alcohol consumption reduces BDNF expression specifically in the vlOFC of male mice. As a result, all subsequent experiments were performed in male mice.
a Timeline of experiments: Female and male mice underwent 7 weeks of IA20%2BC or water only (Supplementary Table 1). Four hours after the beginning of the last drinking session (“binge”) and 24 h after the last drinking session (“withdrawal”), the vlOFC, mOFC and motor cortex M2 were dissected and harvested. The expression of BDNF was measured by RT-qPCR using GAPDH an internal control. Data are presented as the average ratio of BDNF to GAPDH ± SEM and are expressed as percentage of water control. BDNF mRNA in the vlOFC (b), mOFC (c) and M2 motor cortex (d) of male mice. BDNF mRNA in the vlOFC (e), mOFC (f) and M2 motor cortex (g) of female mice. *p < 0.05; ns non-significant. n = 6–8 per group.
DIO-Cre-dependent overexpression of BDNF in vlOFC neurons projecting to the DLS
As described above, high alcohol drinking downregulates BDNF expression in the vlOFC. If BDNF in vlOFC-to-DLS circuit is gating alcohol intake, then replenishing its levels in this circuitry will revert high alcohol intake to moderate levels. To test this possibility, we utilized a circuit-specific strategy to overexpress BDNF in vlOFC neurons that project to the DLS by using the DIO/Cre system, enabling BDNF expression only in the presence of Cre recombinase (Fig. 2a) [23]. AAV2-DIO-BDNF-mCherry virus (1 ×1012 gc/ml) was bilaterally infused into the vlOFC and AAVretro-Cre-GFP virus (3 ×1012 vg/ml) was bilaterally infused into the DLS (Fig. 2b, c). This allowed Cre expression in vlOFC neurons projecting to the DLS visualized by GFP (Fig. 2c), thereby activating Cre-mediated expression of BDNF visualized by mCherry in the vlOFC (Fig. 2c). We further analyzed BDNF signal in vlOFC neurons that project to the DLS in the presence of Cre recombinase (Supplementary Fig. 2a–d). In addition, we assessed the spread of both viruses in the DLS and OFC. As shown in Supplementary Fig. 3, the AAVretro-Cre-GFP virus is localized 1 mm from bregma on the AP axis in the DLS. The AAV2-DIO-BDNF-mCherry virus infection site is localized at 2.1 mm from bregma on the AP axis in the vlOFC, confirming that BDNF is overexpressed in the vlOFC to DLS circuit. Control Mice were bilaterally infected with AAV2-DIO-mCherry in the vlOFC and AAVretro-Cre-GFP in the DLS. Finally, we tested whether BDNF mRNA levels are elevated over baseline in vlOFC neurons that project to the DLS. As shown in Fig. 2d, there was a significant increase of BDNF mRNA levels in the vlOFC of mice infected with AAV2-DIO-BDNF-mCherry as compared to mice infected with AAV2-DIO-mCherry (Unpaired t-test: t (13) = 2.990, p = 0.010).
a Viral strategy of Cre-dependent overexpression of BDNF: BDNF and mCherry coding sequences are floxed by a pair of loxP (blue triangles) and lox2272 (red triangles) sites. In the absence of Cre recombinase, the BDNF and mCherry coding sequences are inverted relative to the EF1a promoter. When expressed, Cre recombinase inverts the BDNF and mCherry sequences into a correct orientation, allowing their expression. b Schematic representation of BDNF overexpression in vlOFC-to-DLS circuit. Mice received bilateral injections of AAV2-DIO-BDNF-mCherry or AAV2-DIO-mCherry in the vlOFC and AAVretro-Cre-GFP in the DLS. c Representative images depicting targeting of AAV2-DIO-BDNF-mCherry (red) in the vlOFC and AAVretro-Cre-GFP (green) in the DLS. Red signal indicates expression of Cre and infection of AAV2-DIO-BDNF-mCherry, confirming the overexpression of BDNF in vlOFC neurons projecting to the DLS. Top left panel depicts mCherry (red) and DAPI (cyan). Bottom left panel depicts GFP (green) and DAPI (cyan). Top and bottom right panels depict mCherry (red) and GFP (green). d The vlOFC was dissected 10 weeks after the infusion of AAV2-DIO-BDNF-mCherry or AAV2-DIO-mCherry in the vlOFC and retroAAV-Cre-GFP in DLS and BDNF expression was measured by RT-qPCR. GAPDH was used as an internal control. Data are presented as the average ratio of BDNF to GAPDH ± SEM and expressed as the percentage of water control. e Timeline of experiments: Three weeks after the surgery, mice underwent IA20%2BC for 7 weeks in the home cage (Supplementary Table 1). f Alcohol intake was recorded. g Alcohol preference was calculated as the ratio of alcohol intake relative to total fluid intake. h Timeline of experiments: Mice received a bilateral injection of AAV2-DIO-BDNF-mCherry or AAV2-DIO-mCherry in the vlOFC and AAVretro-Cre-GFP in the DLS and three weeks after the viral injection, mice were subjected to 2-bottle choice with 0.3% sucrose drinking for 7 sessions in the home cage (Supplementary Table 1). i Sucrose intake was recorded. j Sucrose preference was calculated as the ratio of sucrose intake relative to total fluid intake. Data are represented as mean ± SEM. *p < 0.05, ns: non-significant. n = 6–8 per group.
BDNF in vlOFC-to-DLS projecting neurons gates alcohol but not sucrose intake
Three weeks following viral infection enabling maximal BDNF expression, mice were subjected to 7 weeks of IA20%2BC or water only (Fig. 2e). We found that overexpression of BDNF in vlOFC to DLS projecting neurons significantly reduces alcohol drinking and preference as compared to control mice (Fig. 2f, g, Supplementary Table 1) (Alcohol intake: Two-Way mixed-effect ANOVA, effect of BDNF overexpression, F(1, 13) = 5.89, p = 0.030, effect of session, F(5.873, 73.71) = 3.016, p = 0.011, main effect of interaction, F(20,251) = 0.925, p = 0.554. Alcohol preference: effect of BDNF overexpression, F(1, 13) = 5.91, p = 0.020, effect of session, F(20,240) = 4.35, ****p < 0.0001, effect of interaction, F(20, 240) = 0.96638, p = 0.507). Furthermore, alcohol intake of control mice escalated over time, whereas progressive increase of intake was not detected in mice infected with BDNF in vlOFC neurons projecting to the DLS (Fig. 2f, g). Overexpression of BDNF in vlOFC to DLS projecting neurons did not affect water and total fluid intake (Supplementary Fig. 4a, b) (Water consumption: Two-Way mixed-effect ANOVA, effect of BDNF overexpression, F(1, 13) = 2.906, p = 0.11, effect of session, F(20, 245) = 4.437, ****p < 0.0001, effect of interaction F(20,245) = 0.92, p = 0.55; Total intake consumption: effect of BDNF overexpression, F(1, 13) = 1.168, p = 0.2994, effect of session, F(20, 245) = 1.875, *p = 0.0148, effect of interaction F(20,245) = 1.536, p = 0.0701). Together, these data indicate that escalation of alcohol intake is due in part to the attenuation of BDNF levels in the vlOFC, which is rescued by replenishing BDNF in vlOFC-to-DLS projecting neurons. Our data further suggests that BDNF in OFC to DLS circuitry gates escalation of high alcohol intake.
Next, we set out to determine whether BDNF in vlOFC-to-DLS circuit gates the consumption of sucrose, a natural rewarding substance. To do so, a new cohort of mice was subjected to bilateral injections of AAV2-DIO-BDNF-mCherry in the vlOFC and AAVretro-Cre-GFP in the DLS. Control mice were infected with AAV2-DIO-mCherry in the vlOFC and AAVretro-Cre-GFP in the DLS. Three weeks post-viral infusion, mice underwent intermittent access to 0.3% sucrose 2BC procedure for 2 weeks (Fig. 2h). We found that BDNF overexpression in vlOFC-to-DLS circuit does not alter sucrose intake and preference compared to control mice (Fig. 2i, j, Supplementary Table 1) (Sucrose intake: Two-Way ANOVA, effect of BDNF overexpression, F(1, 11) = 0.233, p = 0.638, effect of session, F(6, 63) = 1.426, p = 0.218, effect of interaction, F(6,63) = 1.605, p = 0.160; Sucrose preference: effect of BDNF overexpression, F(1, 11) = 0.011, p = 0.915, effect of session, F(6, 58) = 1.333, p = 0.257, effect of interaction, F(6, 58) = 3.069, p = 0.012). BDNF overexpression in vlOFC-to-DLS circuit did not alter water consumption and total fluid consumption (Supplementary Fig. 4c, d) (Water intake: Two-Way mixed-effect ANOVA, effect of BDNF overexpression, F(1, 11) = 0.2527, p = 0.62, effect of session, F(6, 58) = 0.8752, p = 0.51, effect of interaction, F(6, 58) = 2.479, *p = 0.03; Total fluid consumption: effect of BDNF overexpression, F(1, 11) = 2.491, p = 0.1428, effect of session, F(6, 58) = 1.541, p = 0.1811, effect of interaction, F(6, 58) = 0.4101, p = 0.8694). Thus, the attenuation of alcohol drinking by BDNF in the vlOFC-to-DLS circuit is not due to changes in palatability and is specific to alcohol. As the striatum plays a role in motor skills [58], we determined whether overexpression of BDNF in vlOFC-to-DLS projecting neurons is due to attenuation of locomotion. As shown in Supplementary Fig. 5, total distance traveled (Supplementary Fig. 5b, c) and velocity (Supplementary Fig. 5d) were similar in the two groups (Total distance traveled: Mann–Whitney Test: U = 15, p = 0.445; Average velocity: Mann–Whitney Test: U = 15, p = 0.445). These results indicate that the behavioral difference in alcohol consumption is not due to changes in motor behavior.
BDNF in vlOFC-to-DMS or M2-to-DLS projecting neurons does not moderate alcohol intake
A small population of BDNF projecting neurons from the vlOFC also projects to the DMS [23]. Therefore, we investigated whether BDNF in vlOFC-to-DMS projecting neurons modulates alcohol consumption. We used the same circuit-specific viral approach, consisting of a bilateral infusion of AAV2-DIO-BDNF-mCherry in the vlOFC and AAVretro-Cre-GFP in the DMS (Fig. 3a), enabling overexpression of BDNF specifically in vlOFC-DMS projecting neurons (Fig. 3b). Control mice were infected with AAV2-DIO-mCherry in the vlOFC and AAVretro-Cre-GFP in the DMS. Three weeks post-viral administration, mice underwent IA20%2BC for 7 weeks, and alcohol intake was assessed. We found no significant difference in alcohol (Fig. 3c, Supplementary Table 1), water, total fluid intake (Supplementary Fig. 6a, b), and alcohol preference (Fig. 3d) between BDNF-overexpressing mice and control groups (Alcohol intake: Two-Way mixed-effect ANOVA, effect of BDNF overexpression, F(1, 17) = 1.033, p = 0.323, effect of session, F(20, 330) = 3.750, ****p < 0.0001, effect of interaction, F(20,330) = 1.592, p = 0.052; Alcohol preference: effect of BDNF overexpression, F(1, 17) = 2.577, p = 0.1268, effect of session, F(20, 327) = 6.605, ****p < 0.0001, effect of interaction, F(20,327) = 0.5599, p = 0.9377; Water consumption: effect of BDNF overexpression, F(1, 17) = 2.14, p = 0.16, effect of session, F(20, 329) = 7.296, ****p < 0.0001, effect of interaction, F(20, 329) = 0.38, p = 0.99; Total fluid consumption: effect of BDNF overexpression, F(1, 17) = 0.2219, p = 0.6436, effect of session, F(20, 324) = 4.744, ****p < 0.0001, effect of interaction, F(20, 324) = 1.523, p = 0.0713). Together, our results suggest that BDNF in vlOFC-to-DLS but not vlOFC-to-DMS circuit moderates alcohol drinking.
a–d Overexpression of BDNF in vlOFC-to-DMS projecting neurons. a Schematic representation of BDNF overexpression in vlOFC-to-DMS circuit. Mice received bilateral injections of AAV2-DIO-BDNF-mCherry or AAV2-DIO-mCherry in the vlOFC and AAVretro-Cre-GFP in the DMS. b Representative image depicting targeting of AAV2-DIO-BDNF-mCherry in vlOFC and AAVretro-Cre-GFP in the DMS. Red cells indicate the expression of Cre and infection of AAV2-DIO-BDNF-mCherry, confirming the overexpression of BDNF in vlOFC neurons projecting to the DMS. Top left panel depicts mCherry (red) and DAPI (cyan). Bottom left panel depicts GFP (green) and DAPI (cyan). Top and bottom right panels depict mCherry (red) and GFP (green). c Three weeks after the surgery, mice underwent IA20%2BC for 7 weeks in the home cage (Supplementary Table 1), and alcohol intake was recorded. d Alcohol preference was calculated as the ratio of alcohol intake relative to total fluid intake. e–h Overexpression of BDNF in M2-to-DLS projecting neurons. e Schematic representation of BDNF overexpression in M2-to-DLS circuit. Mice received bilateral injections of AAV2-DIO-BDNF-mCherry or AAV2-DIO-mCherry in M2 and AAVretro-Cre-GFP in the DLS. f Representative image depicting targeting of AAV2-DIO-BDNF-mCherry in M2 and AAVretro-Cre-GFP in the DLS. Red cells indicate expression of the Cre and infection with AAV2-DIO-BDNF-mCherry confirming the overexpression of BDNF in M2 neurons projecting to the DLS. Top left panel depicts mCherry (red) and DAPI (cyan). Bottom left panel depicts GFP (green) and DAPI (cyan). Top and bottom right panels depict mCherry (red) and GFP (green). g) Three weeks after the surgery, mice underwent IA20%2BC for 7 weeks in the home cage (Supplementary Table 1), and alcohol intake was recorded. h Alcohol preference was calculated as the ratio of alcohol intake relative to total fluid. Data are represented as mean ± SEM. n = 8–10 per group.
BDNF-expressing neurons in M2, a region essential for motor learning and behaviors [59], extend dense projections to the DLS [23]. We, therefore, assessed whether BDNF in M2-to-DLS projecting neurons alters alcohol consumption. To do so, AAV2-DIO-BDNF-mCherry was infused into the M2 and AAVretro-Cre-GFP into the DLS (Fig. 3e, f). Control mice were infected with AAV2-DIO-mCherry in the M2 and AAVretro-Cre-GFP in the DLS. We found that BDNF overexpression in M2 neurons that project to the DLS does not alter alcohol intake (Fig. 3g, Supplementary Table 1) and preference (Fig. 3h) (Alcohol intake: Two-Way mixed-effect ANOVA, effect of BDNF overexpression, F(1, 16) = 0.8408, p = 0.372, effect of session, F(19, 294) = 5.445, ****p < 0.0001, effect of interaction, F(19,294) = 0.709, p = 0.809; Alcohol preference: effect of BDNF overexpression, F(1, 16) = 0.0001175, p = 0.991, effect of session, F(19, 299) = 5.541, ****p < 0.0001, effect of interaction, F(19,299) = 0.918, p = 0.560). Water and total fluid consumption were unchanged between the groups (Supplementary Fig. 6c, d) (Water consumption: Two-Way mixed-effect ANOVA, effect of BDNF overexpression, F(1, 16) = 0.5373, p = 0.47, effect of session, F(19, 298) = 6.149, ****p < 0.0001, effect of interaction, F(19, 298) = 0.6853, p = 0.83; Total fluid consumption: effect of BDNF overexpression, F(1, 16) = 3.591, p = 0.0763, effect of session, F(19, 299) = 4.755, ****p < 0.0001, effect of interaction, F(19, 299) = 0.5461, p = 0.9399). These data indicate that, unlike BDNF in vlOFC-to-DLS circuitry, BDNF in neurons that project from M2-to-DLS do not contribute to mechanisms regulating alcohol drinking.
BDNF in vlOFC-to-DLS projecting neurons gates alcohol self-administration, alcohol seeking and relapse
The DLS as well as the OFC have been implicated in habit formation and habitual drug seeking [55, 57, 60,61,62,63]. We therefore investigated the role of BDNF in the vlOFC-to-DLS circuit in habitual alcohol seeking. We utilized a contingency degradation procedure to examine habitual alcohol seeking [52]. Mice first underwent IA20%2BC for 7 weeks (Supplementary Fig. 7a–d, Supplementary Table 1) and were then trained to operantly self-administer alcohol by lever pressing for 20% alcohol using a random interval (RI) training of reinforcement (Timeline, Fig. 4a), which biases lever responding toward habitual actions [53,54,55]. Alcohol lever presses were similar in mice that were pre-assigned to be infected with AAV2-DIO-BDNF-mCherry or AAV2-DIO-mCherry in the vlOFC and AAVretro-Cre-GFP in the DLS (Supplementary Fig. 7e) (Two-way RM ANOVA: effect of virus F(1,8) = 0.1851, p = 0.6783; effect of session F(2.538,12.3) = 0.7956, p = 0.4422; effect of interaction F3,24) = 0.2797, p = 0.8395). Following the initial training, mice were bilaterally infused with AAV2-DIO-BDNF-mCherry or AAV2-DIO-mCherry in the vlOFC and AAVretro-Cre-GFP in the DLS (Fig. 4a). Three weeks after the surgery, mice underwent 5 additional sessions of RI30 training followed by 5 sessions of RI60 training. First, we examined whether overexpression of BDNF in vlOFC to DLS neurons alters operant self-administration as compared to control mice. Similar to vlOFC BDNF overexpressing mice consuming alcohol in their home cage (Fig. 2) BDNF overexpression in vlOFC-to-DLS circuit robustly decreased alcohol self-administration shown by a reduction in active lever presses (Fig. 4b), alcohol rewards (Fig. 4c) and frequency of active lever presses (Fig. 4d) (Average active lever presses: Two-way RM ANOVA: effect of virus F(1,8) = 8.696, p = 0.0185; effect of session F(2.067,16.53) = 1.234, p = 0.3178; effect of interaction F(4,32) = 2.647, p = 0.0514; Rewards: effect of virus F(1,8) = 5.676, p = 0.0444; effect of session F(2.595,20.76) = 0.4482, p = 0.6943; effect of interaction F(4,32) = 2.684, p = 0.049; Frequency: effect of virus F(1,8) = 8.696, p = 0.0185; effect of session F(2.067,16.53) = 1.234, p = 0.3178; effect of interaction F(4,32) = 2.647, p = 0.0514). These data suggest that BDNF in vlOFC neurons projecting to the DLS moderates alcohol self-administration.
a Experimental timeline: mice underwent 7 weeks of IA20%2BC alcohol in their home cage (Supplementary Table 1). Mice were then trained to operant self-administer 20% alcohol for four weeks on an FR1 schedule followed by an initial habitual alcohol seeking training using random interval (RI) training schedule. Mice were pseudo-randomly assigned to two groups. Control group received bilateral infusions of AAV2-DIO-mCherry in the vlOFC and AAVretro-Cre-GFP in the DLS. The second group received AAV2-DIO-BDNF-mCherry in the vlOFC and AAVretro-Cre-GFP in the DLS. Three weeks after surgery, RI training was resumed followed by contingency degradation testing. Mice then underwent extinction. Lever presses were recorded during the first extinction session and during a reinstatement session. b–d Operant self-administration. Average of active lever presses (b), rewards (c) frequency of active lever presses (d) during the operant training sessions 3 weeks after surgery. e Contingency degradation test: non degraded (ND) and degraded (D). During ND sessions, rewards were delivered on an RI schedule. During D sessions, alcohol rewards were delivered at a rate equal to the average of the last week of training. f, g Average of active lever presses (f) during ND and D testing sessions in RI schedule of reinforcement of AAV-DIO-mCherry infected and AAV-DIO-BDNF-mCherry infected mice. g Cumutative active lever presses of AAV-DIO-mCherry infected and AAV-DIO-BDNF-mCherry infected mice during the 2 hr degradation session. Extinction: the total number of lever presses (h), cumulative number of lever presses (i), port entries (j), and the latency to the first active lever press (k) were recorded. Reacquisition: the total number of lever presses (l), cumulative number of lever presses (m), port entries (n), and the latency to the first active lever press (o) were recorded. Data represented as mean ± SEM. *p < 0.05. n = 5 per group.
With the caveat that BDNF overexpression in vlOFC to DLS circuit robustly decreases alcohol lever presses, we attempted to determine if the reduction in alcohol self-administration was due to an alteration in habitual alcohol seeking. Mice trained to self-administer alcohol in a goal-directed manner are sensitive to contingency degradation, while habitually trained mice are not [53,54,55]. We conducted a contingency degradation procedure and tested whether habitually trained mice continue to press a lever previously paired with alcohol reward delivery (Fig. 4e). During degradation sessions, mice received alcohol at a rate equal to their average reward rate during the 4 nondegraded self-administration sessions immediately preceding the degradation session. As shown in Fig. 4f, the control AAV2-DIO-mCherry infected mice pressed similarly during nondegraded and degraded sessions, indicating habitual responding (Two-way RM ANOVA: effect of virus F(1,8) = 20.90, p = 0.0018; effect of session F(1,8) = 2.084, p = 0.1868; effect of interaction F(1,8) = 0.01386, p = 0.9092). Unfortunately, however, we were unable to assess habitual and goal-directed behavior using a contingency degradation test, as AAV2-DIO-BDNF-mCherry infected mice reduced active lever pressing during nondegraded and degraded sessions compared to control mice (Fig. 4f, g) (cumulative presses during degradation: Two-way RM ANOVA: effect of virus F(1,8) = 5.639, p = 0.0449; effect of session F(1.356,10.85) = 10.90, p = 0.0047; effect of interaction F(11,88) = 5.542, p < 0.0001).
As alcohol seeking precedes alcohol drinking, we examined whether BDNF expressed in this circuitry controls alcohol seeking. To do so, we examined lever presses that were previously associated with alcohol rewards during an extinction session (Fig. 4a). As shown in Fig. 4h, i, overexpression of BDNF in vlOFC to DLS circuit significantly decreases the total number of lever presses as well as the cumulative lever presses (Average active lever presses: Mann–Whitney Test: U = 1, p = 0.0159; Cumulative presses: Two-way RM ANOVA: effect of virus F(1,8) = 5.897, p = 0.0413; effect of session F(1.081,8.645) = 17.13, p = 0.0025; effect of interaction F(11,88) = 5.023, p < 0.0001).
Relapse to alcohol and drug seeking can be modeled by a reacquisition test in which animals first go through a period of extinction in which alcohol deliveries are no longer paired with active lever presses. During the reacquisition test, mice reacquire operant responding [64]. We determined whether overexpressing BDNF in the vlOFC to DLS circuitry alters alcohol lever presses during a reacquisition session. To do so, mice self-administering alcohol underwent 13 extinction sessions during which lever presses were not associated with alcohol deliveries and alcohol cues. During the test session, active lever presses were paired with alcohol deliveries, and lever presses were examined. We found that overexpression of BDNF in vlOFC to DLS neurons reduced total active lever presses (Fig. 4l), cumulative lever presses (Fig. 4m) and port entries (Fig. 4n) following a period of extinction (Average active lever presses: Mann–Whitney Test: U = 2, p = 0.0317; Cumulative presses: Two-way RM ANOVA: effect of virus F(1,8) = 10.42, p = 0.0121; effect of session F(1.642,13.14) = 17.13, p = 0.0004; effect of interaction F(11,88) = 5.006, p < 0.001; Port entries: Mann–Whitney Test: U = 2, p = 0.0317). These behavioral changes were not due to an alteration in locomotion, as shown in Supplementary Fig. 6f (Mann–Whitney Test: U = 20, p = 0.396). Together, these data suggest that BDNF in vlOFC to DLS projecting neurons plays a role in alcohol seeking and relapse.
Systemic administration of a TrkB agonist reverses habitual alcohol seeking
Finally, to examine the translational utility of the findings, and to determine if BDNF sigmaling alters alcohol habits, we utilized the BDNF receptor TrkB agonist, LM22A-4 which selectively binds and activates TrkB [65,66,67,68] (Fig. 5a) and tested its ability to suppress habitual alcohol seeking. A new cohort of mice underwent 7 weeks of IA20%2BC. Following the 7 weeks of IA20%2BC, mice were trained to self-administer 20% alcohol in operant chambers. After 7 initial training sessions on an FR1 schedule, mice began operant training using an RI schedule [53,54,55, 57] (Timeline, Fig. 5b, Supplementary Table 1). Mice were subjected to 5 sessions of RI30 and RI60 training followed by contingency degradation as described above (Timeline, Fig. 5b). Mice received an intraperitoneal (i.p.) administration of saline or a TrkB agonist, LM22A-4 (100 mg/kg) [29], 30 min prior to the degradation session, in a counterbalanced manner. As shown in Fig. 5c, RI-trained mice treated with saline showed no significant differences in lever pressing between non-degraded and degraded sessions. However, RI-trained mice treated with LM22A-4 exhibited a reduction in lever presses during contingency degradation, compared with non-degraded sessions (Fig. 5c) (Two-Way RM ANOVA, main effect of degradation F (1, 26) = 13.52, p = 0.0011, effect of treatment F(1,28) = 0.93, p = 0.342, effect of interaction F(1,26) = 16.08, p = 0.0005). Taken together, these data show that treatment with a TrkB agonist biases mice trained to habitually self-administer alcohol toward a goal-directed action selection strategy, suggesting that BDNF plays a role in moderating habitual alcohol. Furthermore, these results indicate the potential of utilizing a TrkB agonist to prevent habitual drug seeking.
a LM22A-4 mechanism of action: LM22A-4 binds to and activates TrkB, leading to the activation of downstream signaling pathways [65]. b Timeline of operant self-administration training. Following 7 weeks of IA2BC-20% alcohol in the home cage (Supplementary Table 1), mice began operant training for alcohol (20%) self-administration. Mice were trained on FR1 schedule followed by an initial habitual alcohol seeking training using random interval (RI) training schedule followed by contingency degradation testing. Mice were pseudo-randomly assigned and received an i.p. administration of saline or LM22A-4 (100 mg/kg) 30 min prior to the first contingency degradation. c Average lever presses of saline and LM22A-4 treated mice during ND and D testing sessions in RI schedule of reinforcement. Data are represented as mean ± SEM; **p < 0.01, ns: non-significant, n = 14.
Discussion
Here, we investigated the potential role of BDNF in vlOFC-to-DLS circuit in alcohol-drinking and seeking behaviors. We found that chronic high alcohol intake decreases BDNF levels in the vlOFC but not in mOFC or M2 of male but not female mice. We further discovered that BDNF in a small ensemble of vlOFC neurons projecting to the DLS gates alcohol intake, seeking, and relapse. Finally, we showed that systemic administration of a TrkB agonist biases habitual alcohol seeking to goal-directed behavior, suggesting the utility of TrkB agonist to dampen habitual alcohol seeking.
Long-term high levels of alcohol intake decrease BDNF levels in the vlOFC of males but not female mice
The rodent OFC is a complex brain region containing several functionally distinct subregions, with different neuronal populations extending axonal projections throughout the brain [35]. We recently showed that the vlOFC sends projections to the DLS [23]. In rodents, primates, and humans, the vlOFC is an anatomically separate subregion, with distinct corticostriatal circuits linked to specific behavioral functions [35, 69]. We found a significant decrease in BDNF mRNA levels in the vlOFC after high alcohol drinking in male mice. The mechanism responsible for the attenuation of BDNF levels in the vlOFC following long-term binge drinking and withdrawal remains unknown. BDNF mRNA is regulated in part by the microRNA (miR) machinery which promotes mRNA degradation or translation repression [70]. We, and others, previously showed that repeated cycles of high alcohol intake or alcohol vapor exposure and withdrawal decrease BDNF expression in the medial PFC (mPFC) of mice and rats [25, 26] which correlates with increased levels of miR-30a-5p and miR-206 both targeting BDNF mRNA [25, 26]. Overexpression of these miRs in the mPFC of rodents led to an escalation of alcohol intake while their inhibition reduced high drinking [25, 26]. These studies were conducted on male mice; however, evidence suggests sex-specific patterns of miR expression in response to various stimuli [71, 72]. Therefore, it would be of interest to identify the BDNF-targeting miRs increased in the vlOFC after high alcohol intake in male vs. female mice, which could be one of the mechanisms underlying the sexual dimorphism we identified in this study.
BDNF in vlOFC to DLS circuitry controls alcohol drinking behaviors
We found that BDNF overexpression in vlOFC-to-DLS projecting neurons decreases alcohol drinking, seeking, and relapse. The OFC is implicated in motivation [35, 53] and modifying stimulus-outcome associations [35, 53, 56, 73, 74], along with reward seeking [35, 53]. Gourley and colleagues reported that BDNF in the vlOFC is involved in goal-directed decision-making in mice [56, 75]. Specifically, the authors showed that the knockdown of BDNF in OFC interferes with stimulus-outcome and response-outcome associations and that systemic administration of BDNF agonists rescues action-selection associations [76]. In addition, Pitts and colleagues found BDNF to be involved in the balance between action and habit [77] by showing that overexpressing truncated inactive TrkB in vlOFC impedes goal-directed action [77]. These findings, together with ours, suggest that BDNF in the vlOFC-to-DLS circuit may bias mice towards goal-directed alcohol seeking and that BDNF in vlOFC-to-DLS circuit may gate alcohol intake by altering decision-making. However, further work is required to address this question.
Axonal release of BDNF activates TrkB receptors in the target region. We previously reported that BDNF-positive vlOFC neurons form synapses with DLS neurons in mice [23], suggesting that TrkB signaling in the DLS is activated by overexpression of BDNF in vlOFC-to-DLS neurons. TrkB activation promotes the activation of ERK1/2, PLC/PKC, or PI3K/AKT signaling [6, 78]. We previously found that BDNF-mediated activation of TrkB in the DLS gates alcohol intake in a mechanism that depends on ERK1/2 but not PI3K/AKT or PLC/PKC signaling [19], suggesting that BDNF from vlOFC neurons promotes the activation of TrkB/ERK1/2 leading to transcriptional and/or translational modifications that in turn gate alcohol drinking behaviors. This line of research will be explored in future studies.
The majority of DLS neurons are dopamine D1 receptors (D1) or dopamine D2 receptors (D2)-expressing medium spiny neurons (MSN) [79]. Both D1 and D2 MSN express TrkB receptors [80]. Within the DLS, it is plausible that BDNF signaling via TrkB is differentially regulated depending on the target cell i.e. D1 or D2 MSNs [80,81,82]. Work from Nestler and colleagues suggests that activation of BDNF-TrkB signaling in D1 or D2 MSN in the nucleus accumbens generates opposite effects on cocaine and morphine-dependent rewarding behaviors in mice [80, 81]. Further studies are required to gain insight into BDNF-TrkB signaling in behavioral responses to alcohol in subpopulations of DLS neurons.
The vlOFC extends projections to several other brain regions, including the hippocampus, substantia nigra, ventral tegmental area, and several cortical subregions [83, 84]. In addition, work from Gourley and colleagues suggest that the vlOFC projections to the ventrolateral striatum, which includes the nucleus accumbens, regulate goal-directed food and cocaine seeking [56] and Saunders and colleagues recently reported a role of the vlOFC to basolateral amygdala circuit is critical during reward seeking [85]. Thus, we cannot exclude the possibility that BDNF originating from the vlOFC activates TrkB signaling in one or more of these brain regions and may also play a role in alcohol-mediated behaviors.
Translational implications
We previously reported that administration of LM22A-4 converts compulsive alcohol drinking of Met68BDNF mutant mice to moderate levels of intake [29]. We show herein that LM22A-4 reverses habitual alcohol seeking. Although it is likely that the reduction in habitual alcohol behavior by LM22A-4 is due to its stimulatory actions in the DLS, we cannot exclude the possibility that the attenuation of habit is mediated by TrkB in brain regions other than the DLS. LM22A-4 has been shown to have promising effects in preclinical studies for the treatment of several neurological diseases [86,87,88,89]. Thus, our data give rise to the potential use of LM22A-4 in AUD.
Together, our data highlight the importance of a small neuronal ensemble in regulating high alcohol intake, seeking, and relapse. Our findings also provide evidence for a potentially new drug target to combat AUD phenotypes, including habit.
Data availability
Any data not contained in the paper are available on request with appropriate agreements. Source data are provided with this paper.
References
Miranda M, Morici JF, Zanoni MB, Bekinschtein P. Brain-Derived Neurotrophic Factor: A Key Molecule for Memory in the Healthy and the Pathological Brain. Front Cell Neurosci. 2019;13:363 https://doi.org/10.3389/fncel.2019.00363.
Waterhouse EG, An JJ, Orefice LL, Baydyuk M, Liao GY, Zheng K, et al. BDNF promotes differentiation and maturation of adult-born neurons through GABAergic transmission. J Neurosci. 2012;32:14318–30. https://doi.org/10.1523/JNEUROSCI.0709-12.2012.
Colucci-D’Amato L, Speranza L, Volpicelli F. Neurotrophic Factor BDNF, Physiological Functions and Therapeutic Potential in Depression, Neurodegeneration and Brain Cancer. Int J Mol Sci. 2020;21, https://doi.org/10.3390/ijms21207777.
Hofer M, Pagliusi SR, Hohn A, Leibrock J, Barde YA. Regional distribution of brain-derived neurotrophic factor mRNA in the adult mouse brain. EMBO J. 1990;9:2459–64. https://doi.org/10.1002/j.1460-2075.1990.tb07423.x.
Timmusk T, Palm K, Metsis M, Reintam T, Paalme V, Saarma M, et al. Multiple promoters direct tissue-specific expression of the rat BDNF gene. Neuron. 1993;10:475–89. https://doi.org/10.1016/0896-6273(93)90335-o.
Huang EJ, Reichardt LF. Trk receptors: roles in neuronal signal transduction. Annu Rev Biochem. 2003;72:609–42. https://doi.org/10.1146/annurev.biochem.72.121801.161629.
Reichardt LF. Neurotrophin-regulated signalling pathways. Philos Trans R Soc Lond B Biol Sci. 2006;361:1545–64. https://doi.org/10.1098/rstb.2006.1894.
You H, Lu B. Diverse Functions of Multiple Bdnf Transcripts Driven by Distinct Bdnf Promoters. Biomolecules. 2023;13, https://doi.org/10.3390/biom13040655.
Autry AE, Monteggia LM. Brain-derived neurotrophic factor and neuropsychiatric disorders. Pharmacol Rev. 2012;64:238–58. https://doi.org/10.1124/pr.111.005108.
Barker JM, Taylor JR, De Vries TJ, Peters J. Brain-derived neurotrophic factor and addiction: Pathological versus therapeutic effects on drug seeking. Brain Res. 2015;1628:68–81. https://doi.org/10.1016/j.brainres.2014.10.058.
National Survey on Drug Use and Health. https://www.samhsa.gov/data/sites/default/files/reports/rpt42728/NSDUHDetailedTabs2022/NSDUHDetailedTabs2022/NSDUHDetTabsSect5pe2022.html.
Ron D, Barak S. Molecular mechanisms underlying alcohol-drinking behaviours. Nat Rev Neurosci. 2016;17:576–91. https://doi.org/10.1038/nrn.2016.85.
Egervari G, Siciliano CA, Whiteley EL, Ron D. Alcohol and the brain: from genes to circuits. Trends Neurosci. 2021;44:1004–15. https://doi.org/10.1016/j.tins.2021.09.006.
Ron D, Berger A. Targeting the intracellular signaling “STOP” and “GO” pathways for the treatment of alcohol use disorders. Psychopharmacology. 2018;235:1727–43. https://doi.org/10.1007/s00213-018-4882-z.
Lipton DM, Gonzales BJ, Citri A. Dorsal Striatal Circuits for Habits, Compulsions and Addictions. Front Syst Neurosci. 2019;13:28. https://doi.org/10.3389/fnsys.2019.00028.
Jeanblanc J, He DY, McGough NN, Logrip ML, Phamluong K, Janak PH, et al. The dopamine D3 receptor is part of a homeostatic pathway regulating ethanol consumption. J Neurosci. 2006;26:1457–64. https://doi.org/10.1523/JNEUROSCI.3786-05.2006.
Logrip ML, Janak PH, Ron D. Dynorphin is a downstream effector of striatal BDNF regulation of ethanol intake. FASEB J. 2008;22:2393–404.
Jeanblanc J, He DY, Carnicella S, Kharazia V, Janak PH, Ron D. Endogenous BDNF in the dorsolateral striatum gates alcohol drinking. J Neurosci. 2009;29:13494–502. https://doi.org/10.1523/JNEUROSCI.2243-09.2009.
Jeanblanc J, Logrip ML, Janak PH, Ron D. BDNF-mediated regulation of ethanol consumption requires the activation of the MAP kinase pathway and protein synthesis. Eur J Neurosci. 2013;37:607–12. https://doi.org/10.1111/ejn.12067.
Altar CA, Cai N, Bliven T, Juhasz M, Conner JM, Acheson AL, et al. Anterograde transport of brain-derived neurotrophic factor and its role in the brain. Nature. 1997;389:856–60. https://doi.org/10.1038/39885.
Baquet ZC, Gorski JA, Jones KR. Early striatal dendrite deficits followed by neuron loss with advanced age in the absence of anterograde cortical brain-derived neurotrophic factor. J Neurosci. 2004;24:4250–8. https://doi.org/10.1523/JNEUROSCI.3920-03.2004.
Baydyuk M, Xu B. BDNF signaling and survival of striatal neurons. Front Cell Neurosci. 2014;8:254. https://doi.org/10.3389/fncel.2014.00254.
Ehinger Y, Soneja D, Phamluong K, Salvi A, Ron D. Identification of Novel BDNF-Specific Corticostriatal Circuitries. eNeuro 2023;10. https://doi.org/10.1523/ENEURO.0238-21.2023.
Logrip ML, Janak PH, Ron D. Escalating ethanol intake is associated with altered corticostriatal BDNF expression. J Neurochem. 2009;109:1459–68. https://doi.org/10.1111/j.1471-4159.2009.06073.x.
Darcq E, Warnault V, Phamluong K, Besserer GM, Liu F, Ron D. MicroRNA-30a-5p in the prefrontal cortex controls the transition from moderate to excessive alcohol consumption. Mol Psychiatry. 2015;20:1219–31. https://doi.org/10.1038/mp.2014.120.
Tapocik JD, Barbier E, Flanigan M, Solomon M, Pincus A, Pilling A, et al. microRNA-206 in rat medial prefrontal cortex regulates BDNF expression and alcohol drinking. J Neurosci. 2014;34:4581–8. https://doi.org/10.1523/JNEUROSCI.0445-14.2014.
Darcq E, Morisot N, Phamluong K, Warnault V, Jeanblanc J, Longo FM, et al. The Neurotrophic Factor Receptor p75 in the Rat Dorsolateral Striatum Drives Excessive Alcohol Drinking. J Neurosci. 2016;36:10116–27. https://doi.org/10.1523/JNEUROSCI.4597-14.2016.
Egan MF, Kojima M, Callicott JH, Goldberg TE, Kolachana BS, Bertolino A, et al. The BDNF val66met polymorphism affects activity-dependent secretion of BDNF and human memory and hippocampal function. Cell. 2003;112:257–69. https://doi.org/10.1016/s0092-8674(03)00035-7.
Warnault V, Darcq E, Morisot N, Phamluong K, Wilbrecht L, Massa SM, et al. The BDNF Valine 68 to Methionine Polymorphism Increases Compulsive Alcohol Drinking in Mice That Is Reversed by Tropomyosin Receptor Kinase B Activation. Biol Psychiatry. 2016;79:463–73. https://doi.org/10.1016/j.biopsych.2015.06.007.
Moffat JJ, Sakhai SA, Hoisington ZW, Ehinger Y, Ron D. The BDNF Val68Met polymorphism causes a sex specific alcohol preference over social interaction and also acute tolerance to the anxiolytic effects of alcohol, a phenotype driven by malfunction of BDNF in the ventral hippocampus of male mice. Psychopharmacology. 2023;240:303–17. https://doi.org/10.1007/s00213-022-06305-3.
Bromberg-Martin ES, Matsumoto M, Hikosaka O. Dopamine in motivational control: rewarding, aversive, and alerting. Neuron. 2010;68:815–34. https://doi.org/10.1016/j.neuron.2010.11.022.
Schultz W. Dopamine reward prediction-error signalling: a two-component response. Nat Rev Neurosci. 2016;17:183–95. https://doi.org/10.1038/nrn.2015.26.
Schultz W. Reward prediction error. Curr Biol. 2017;27:R369–R371. https://doi.org/10.1016/j.cub.2017.02.064.
Wallis JD. Orbitofrontal cortex and its contribution to decision-making. Annu Rev Neurosci. 2007;30:31–56. https://doi.org/10.1146/annurev.neuro.30.051606.094334.
Ostlund SB, Balleine BW. Orbitofrontal cortex mediates outcome encoding in Pavlovian but not instrumental conditioning. J Neurosci. 2007;27:4819–25. https://doi.org/10.1523/JNEUROSCI.5443-06.2007.
Rolls ET, Critchley HD, Mason R, Wakeman EA. Orbitofrontal cortex neurons: role in olfactory and visual association learning. J Neurophysiol. 1996;75:1970–81. https://doi.org/10.1152/jn.1996.75.5.1970.
Stalnaker TA, Cooch NK, Schoenbaum G. What the orbitofrontal cortex does not do. Nat Neurosci. 2015;18:620–7. https://doi.org/10.1038/nn.3982.
Moorman DE. The role of the orbitofrontal cortex in alcohol use, abuse, and dependence. Prog Neuropsychopharmacol Biol Psychiatry. 2018;87:85–107. https://doi.org/10.1016/j.pnpbp.2018.01.010.
Bracht T, Soravia L, Moggi F, Stein M, Grieder M, Federspiel A, et al. The role of the orbitofrontal cortex and the nucleus accumbens for craving in alcohol use disorder. Transl Psychiatry. 2021;11:267. https://doi.org/10.1038/s41398-021-01384-w.
Pfefferbaum A, Sullivan EV. Disruption of brain white matter microstructure by excessive intracellular and extracellular fluid in alcoholism: evidence from diffusion tensor imaging. Neuropsychopharmacology. 2005;30:423–32. https://doi.org/10.1038/sj.npp.1300623.
Atmaca M, Tabara MF, Koc M, Gurok MG, Baykara S, Korkmaz S, et al. Cortical Thickness of the Orbitofrontal Cortex in Patients with Alcohol Use Disorder. Brain Sci. 2023:13. https://doi.org/10.3390/brainsci13040552.
Miguel-Hidalgo JJ, Overholser JC, Meltzer HY, Stockmeier CA, Rajkowska G. Reduced glial and neuronal packing density in the orbitofrontal cortex in alcohol dependence and its relationship with suicide and duration of alcohol dependence. Alcohol Clin Exp Res. 2006;30:1845–55. https://doi.org/10.1111/j.1530-0277.2006.00221.x.
Volkow ND, Wang GJ, Telang F, Fowler JS, Logan J, Jayne M, et al. Profound decreases in dopamine release in striatum in detoxified alcoholics: possible orbitofrontal involvement. J Neurosci. 2007;27:12700–6. https://doi.org/10.1523/JNEUROSCI.3371-07.2007.
Nimitvilai S, Lopez MF, Mulholland PJ, Woodward JJ. Chronic Intermittent Ethanol Exposure Enhances the Excitability and Synaptic Plasticity of Lateral Orbitofrontal Cortex Neurons and Induces a Tolerance to the Acute Inhibitory Actions of Ethanol. Neuropsychopharmacology. 2016;41:1112–27. https://doi.org/10.1038/npp.2015.250.
Gioia DA, Woodward JJ. Altered Activity of Lateral Orbitofrontal Cortex Neurons in Mice following Chronic Intermittent Ethanol Exposure. eNeuro. 2021;8:ENEURO.0503–20.2021. https://doi.org/10.1523/ENEURO.0503-20.2021.
den Hartog C, Zamudio-Bulcock P, Nimitvilai S, Gilstrap M, Eaton B, Fedarovich H, et al. Inactivation of the lateral orbitofrontal cortex increases drinking in ethanol-dependent but not non-dependent mice. Neuropharmacology. 2016;107:451–9. https://doi.org/10.1016/j.neuropharm.2016.03.031.
Schuh KM, Sneddon EA, Nader AM, Muench MA, Radke AK. Orbitofrontal cortex subregion inhibition during binge-like and aversion-resistant alcohol drinking. Alcohol. 2022;99:1–8. https://doi.org/10.1016/j.alcohol.2021.11.004.
Ray MH, Hanlon E, McDannald MA. Lateral orbitofrontal cortex partitions mechanisms for fear regulation and alcohol consumption. PLoS One. 2018;13:e0198043. https://doi.org/10.1371/journal.pone.0198043.
Bianchi PC, Carneiro de Oliveira PE, Palombo P, Leão RM, Cogo-Moreira H, Planeta C, et al. Functional inactivation of the orbitofrontal cortex disrupts context-induced reinstatement of alcohol seeking in rats. Drug Alcohol Depend. 2018;186:102–12. https://doi.org/10.1016/j.drugalcdep.2017.12.045.
Hernandez JS, Binette AN, Rahman T, Tarantino JD, Moorman DE. Chemogenetic Inactivation of Orbitofrontal Cortex Decreases Cue-induced Reinstatement of Ethanol and Sucrose Seeking in Male and Female Wistar Rats. Alcohol Clin Exp Res. 2020;44:1769–82. https://doi.org/10.1111/acer.14407.
Ehinger Y, Zhang Z, Phamluong K, Soneja D, Shokat KM, Ron D. Brain-specific inhibition of mTORC1 eliminates side effects resulting from mTORC1 blockade in the periphery and reduces alcohol intake in mice. Nat Commun. 2021;12:4407. https://doi.org/10.1038/s41467-021-24567-x.
Hoisington ZW, Salvi A, Laguesse S, Ehinger Y, Shukla C, Phamluong K, et al. The Small G-Protein Rac1 in the Dorsomedial Striatum Promotes Alcohol-Dependent Structural Plasticity and Goal-Directed Learning in Mice. J Neurosci. 2024;44:e1644232024. https://doi.org/10.1523/JNEUROSCI.1644-23.2024.
Gremel CM, Costa RM. Orbitofrontal and striatal circuits dynamically encode the shift between goal-directed and habitual actions. Nat Commun. 2013;4:2264. https://doi.org/10.1038/ncomms3264.
Gremel CM, Chancey JH, Atwood BK, Luo G, Neve R, Ramakrishnan C, et al. Endocannabinoid Modulation of Orbitostriatal Circuits Gates Habit Formation. Neuron. 2016;90:1312–24. https://doi.org/10.1016/j.neuron.2016.04.043.
Corbit LH, Nie H, Janak PH. Habitual alcohol seeking: time course and the contribution of subregions of the dorsal striatum. Biol Psychiatry. 2012;72:389–95. https://doi.org/10.1016/j.biopsych.2012.02.024.
Gourley SL, Olevska A, Zimmermann KS, Ressler KJ, Dileone RJ, Taylor JR. The orbitofrontal cortex regulates outcome-based decision-making via the lateral striatum. Eur J Neurosci. 2013;38:2382–8. https://doi.org/10.1111/ejn.12239.
Morisot N, Phamluong K, Ehinger Y, Berger AL, Moffat JJ, Ron D. mTORC1 in the orbitofrontal cortex promotes habitual alcohol seeking. Elife. 2019;8. https://doi.org/10.7554/eLife.51333.
Calabresi P, Picconi B, Tozzi A, Ghiglieri V, Di Filippo M. Direct and indirect pathways of basal ganglia: a critical reappraisal. Nat Neurosci. 2014;17:1022–30. https://doi.org/10.1038/nn.3743.
Barthas F, Kwan AC. Secondary Motor Cortex: Where ‘Sensory’ Meets ‘Motor’ in the Rodent Frontal Cortex. Trends Neurosci. 2017;40:181–93. https://doi.org/10.1016/j.tins.2016.11.006.
Belin D, Belin-Rauscent A, Murray JE, Everitt BJ. Addiction: failure of control over maladaptive incentive habits. Curr Opin Neurobiol. 2013;23:564–72. https://doi.org/10.1016/j.conb.2013.01.025.
Everitt BJ. Neural and psychological mechanisms underlying compulsive drug seeking habits and drug memories-indications for novel treatments of addiction. Eur J Neurosci. 2014;40:2163–82. https://doi.org/10.1111/ejn.12644.
Luscher C. The Emergence of a Circuit Model for Addiction. Annu Rev Neurosci. 2016;39:257–76. https://doi.org/10.1146/annurev-neuro-070815-013920.
Schoenbaum G, Shaham Y. The role of orbitofrontal cortex in drug addiction: a review of preclinical studies. Biol Psychiatry. 2008;63:256–62. https://doi.org/10.1016/j.biopsych.2007.06.003.
Di Ciano P, Robbins TW, Everitt BJ. Differential effects of nucleus accumbens core, shell, or dorsal striatal inactivations on the persistence, reacquisition, or reinstatement of responding for a drug-paired conditioned reinforcer. Neuropsychopharmacology. 2008;33:1413–25. https://doi.org/10.1038/sj.npp.1301522.
Massa SM, Yang T, Xie Y, Shi J, Bilgen M, Joyce JN, et al. Small molecule BDNF mimetics activate TrkB signaling and prevent neuronal degeneration in rodents. J Clin Invest. 2010;120:1774–85. https://doi.org/10.1172/JCI41356.
Kajiya M, Takeshita K, Kittaka M, Matsuda S, Ouhara K, Takeda K, et al. BDNF mimetic compound LM22A-4 regulates cementoblast differentiation via the TrkB-ERK/Akt signaling cascade. Int Immunopharmacol. 2014;19:245–52. https://doi.org/10.1016/j.intimp.2014.01.028.
Todd D, Gowers I, Dowler SJ, Wall MD, McAllister G, Fischer DF, et al. A monoclonal antibody TrkB receptor agonist as a potential therapeutic for Huntington’s disease. PLoS One. 2014;9:e87923 https://doi.org/10.1371/journal.pone.0087923.
Flores-Bonilla A, Richardson HN. Sex Differences in the Neurobiology of Alcohol Use Disorder. Alcohol Res. 2020;40:04 https://doi.org/10.35946/arcr.v40.2.04.
Leal G, Comprido D, Duarte CB. BDNF-induced local protein synthesis and synaptic plasticity. Neuropharmacology. 2014;76:639–56. https://doi.org/10.1016/j.neuropharm.2013.04.005.
Gebert LFR, MacRae IJ. Regulation of microRNA function in animals. Nat Rev Mol Cell Biol. 2019;20:21–37. https://doi.org/10.1038/s41580-018-0045-7.
Sharma S, Eghbali M. Influence of sex differences on microRNA gene regulation in disease. Biol Sex Differ. 2014;5:3. https://doi.org/10.1186/2042-6410-5-3.
Lusardi TA, Murphy SJ, Phillips JI, Chen Y, Davis CM, Young JM, et al. MicroRNA responses to focal cerebral ischemia in male and female mouse brain. Front Mol Neurosci. 2014;7:11. https://doi.org/10.3389/fnmol.2014.00011.
Rhodes SE, Murray EA. Differential effects of amygdala, orbital prefrontal cortex, and prelimbic cortex lesions on goal-directed behavior in rhesus macaques. J Neurosci. 2013;33:3380–9. https://doi.org/10.1523/JNEUROSCI.4374-12.2013.
Fiuzat EC, Rhodes SE, Murray EA. The Role of Orbitofrontal-Amygdala Interactions in Updating Action-Outcome Valuations in Macaques. J Neurosci. 2017;37:2463–70. https://doi.org/10.1523/JNEUROSCI.1839-16.2017.
Gourley SL, Zimmermann KS, Allen AG, Taylor JR. The Medial Orbitofrontal Cortex Regulates Sensitivity to Outcome Value. J Neurosci. 2016;36:4600–13. https://doi.org/10.1523/JNEUROSCI.4253-15.2016.
DePoy LM, Zimmermann KS, Marvar PJ, Gourley SL. Induction and Blockade of Adolescent Cocaine-Induced Habits. Biol Psychiatry. 2017;81:595–605. https://doi.org/10.1016/j.biopsych.2016.09.023.
Pitts EG, Li DC, Gourley SL. Bidirectional coordination of actions and habits by TrkB in mice. Sci Rep. 2018;8:4495. https://doi.org/10.1038/s41598-018-22560-x.
Chao MV. Neurotrophins and their receptors: a convergence point for many signalling pathways. Nat Rev Neurosci. 2003;4:299–309. https://doi.org/10.1038/nrn1078.
Gerfen CR, Engber TM, Mahan LC, Susel Z, Chase TN, Monsma FJ Jr, et al. D1 and D2 dopamine receptor-regulated gene expression of striatonigral and striatopallidal neurons. Science. 1990;250:1429–32. https://doi.org/10.1126/science.2147780.
Lobo MK, Covington HE, Chaudhury D, Friedman AK, Sun H, Damez-Werno D, et al. Cell type-specific loss of BDNF signaling mimics optogenetic control of cocaine reward. Science. 2010;330:385–90. https://doi.org/10.1126/science.1188472.
Koo JW, Lobo MK, Chaudhury D, Labonté B, Friedman A, Heller E, et al. Loss of BDNF signaling in D1R-expressing NAc neurons enhances morphine reward by reducing GABA inhibition. Neuropsychopharmacology. 2014;39:2646–53. https://doi.org/10.1038/npp.2014.118.
Engeln M, Song Y, Chandra R, La A, Fox ME, Evans B, et al. Individual differences in stereotypy and neuron subtype translatome with TrkB deletion. Mol Psychiatry. 2020;26:1846–59. https://doi.org/10.1038/s41380-020-0746-0.
Izquierdo A. Functional Heterogeneity within Rat Orbitofrontal Cortex in Reward Learning and Decision Making. J Neurosci. 2017;37:10529–40. https://doi.org/10.1523/JNEUROSCI.1678-17.2017.
Hoover WB, Vertes RP. Projections of the medial orbital and ventral orbital cortex in the rat. J Comp Neurol. 2011;519:3766–801. https://doi.org/10.1002/cne.22733.
Ottenheimer DJ, Vitale KR, Ambroggi F, Janak PH, Saunders BT. Basolateral amygdala population coding of a cued reward seeking state depends on orbitofrontal cortex. bioRxiv. 2024. https://doi.org/10.1101/2023.12.31.573789.
Schmid DA, Yang T, Ogier M, Adams I, Mirakhur Y, Wang Q, et al. A TrkB Small Molecule Partial Agonist Rescues TrkB Phosphorylation Deficits and Improves Respiratory Function in a Mouse Model of Rett Syndrome. J Neurosci. 2012;32:1803–10. https://doi.org/10.1523/JNEUROSCI.0865-11.2012.
Simmons DA, Belichenko NP, Yang T, Condon C, Monbureau M, Shamloo M, et al. A small molecule TrkB ligand reduces motor impairment and neuropathology in R6/2 and BACHD mouse models of Huntington’s disease. J Neurosci. 2013;33:18712–27. https://doi.org/10.1523/JNEUROSCI.1310-13.2013.
Escher T, Mittleman G. Schedule-induced alcohol drinking: non-selective effects of acamprosate and naltrexone. Addict Biol. 2006;11:55–63. https://doi.org/10.1111/j.1369-1600.2006.00004.x.
Kipnis PA, Sullivan BJ, Carter BM, Kadam SD. TrkB agonists prevent postischemic emergence of refractory neonatal seizures in mice. JCI Insight. 2020:5. https://doi.org/10.1172/jci.insight.136007.
Acknowledgements
We sincerely thank Dr. Stefan Massa (University of California San Francisco) and Dr. Frank Longo (Stanford University) for generously providing the LM22A4 compound used in this study.
Funding
This study was funded by NIH/NIAAA R37 AA016848 (DR) and NIH/NIAAA R01 AA031832 (DR).
Author information
Authors and Affiliations
Contributions
DR and YE conceived the project. DR and YE provided oversight and guidance. SG, YE, JM and DR designed the experiments. SG, KP, JM, JE and YE conducted the experiments. SG, JM and YE analyzed the data. SG, YE and DR wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gunasekaran, S., Moffat, J.J., Epstein, J.D. et al. BDNF in ventrolateral orbitofrontal cortex to dorsolateral striatum circuit moderates alcohol consumption, seeking and relapse. Neuropsychopharmacol. 51, 565–576 (2026). https://doi.org/10.1038/s41386-025-02274-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41386-025-02274-1
This article is cited by
-
Orbitofrontal BDNF puts the brakes on alcohol intake and relapse
Neuropsychopharmacology (2026)