Abstract
Current psychiatric neuroimaging supports the view that major depressive disorder (MDD) is a dysconnection syndrome, characterized by structural brain dysconnectivity. Recent studies investigating this question, however, did not evaluate the involvement of comorbid disorders, of which anxiety disorders (ANX) are particularly prevalent. Here, we investigated the structural connectivity alterations observed in MDD with and without comorbid ANX. To this end, we reconstructed structural brain networks of n = 781 individuals with a diagnosis of MDD who had at least one diagnosis of an ANX (n = 249) and those without any diagnosis of ANX (n = 532), as well as n = 906 healthy controls (HC) from structural and diffusion-weighted MRI. The network-based statistic (NBS) toolbox was employed to evaluate network-level differences in structural connectivity among the three groups. Transdiagnostic analyses were conducted to explore the dimensional relationship between anxiety and structural connectivity. NBS revealed decreased structural connectivity in MDD patients without comorbid ANX and increased structural connectivity in MDD patients with comorbid ANX relative to HC, with both effects found in spatially overlapping white matter connections. Transdiagnostic analyses suggested that increases in anxiety were associated with increased structural connectivity across all groups. Our finding that hyperconnectivity rather than hypoconnectivity characterizes the structural connectome of MDD patients with comorbid ANX challenges the applicability of the dysconnection syndrome hypothesis to MDD with comorbid ANX, warranting symptom-based investigations of brain changes in mental disorders.
Similar content being viewed by others
Introduction
For over a decade, major depressive disorder (MDD) and anxiety disorders (ANX) have ranked among the ten most debilitating diseases worldwide [1], with lifetime prevalences of 16–20% and 14–29%, respectively [2,3,4,5]. Importantly, these disorders also frequently co-occur: up to 75% of individuals with a primary lifetime diagnosis of MDD also report a history of ANX [6] and up to 81% of those with primary ANX also experience comorbid MDD [7,8,9]. While overlapping diagnostic criteria may inflate this comorbidity [10, 11], its clinical significance is undeniable given its substantial contribution to the overall burden of illness [12]. Individuals with comorbid MDD and ANX (MDD + ANX) exhibit an earlier disease onset, more severe depressive symptoms, higher levels of suicidal ideation, greater functional impairments, and lower remission rates [4, 6, 7, 13,14,15]. Understanding the biological, psychological, and social factors underlying MDD + ANX is therefore crucial to advance mental health care for this severely affected population. The present study aims to contribute to this objective by investigating brain structural alterations in individuals with MDD and MDD + ANX.
From a neurobiological perspective, mental disorders have long been conceptualized as dysconnection syndromes [16,17,18]. This conceptualization suggests that symptoms arise from aberrant information transmission within the network of brain regions and their connecting white matter fiber tracts, collectively referred to as the human connectome [19, 20]. Previous research supports this by showing significant alterations in the structural connectome across MDD, bipolar disorder, and schizophrenia [21,22,23,24,25]. For instance, studies from our group revealed that, in MDD, dysconnectivity in the structural connectome typically presents as subtle yet widespread hypoconnectivity, particularly in individuals with earlier onset and more severe depressive symptoms [23, 26]. These findings reinforce the conceptualization that MDD may manifest as a dysconnection syndrome [27].
While connectome alterations in MDD have been thoroughly investigated, corresponding examinations in MDD + ANX are notably less common [28, 29]. Previous studies on connectome alterations in MDD, including our own, usually did not distinguish between MDD and MDD + ANX. This is problematic, as meta-analyses show that including participants with MDD + ANX significantly increases variability within the MDD-white matter association [30]. Moreover, individuals with MDD + ANX exhibit clinically distinct profiles compared to those with MDD alone, including earlier age of onset, more severe depressive symptoms, and higher rates of hospitalization [12]. These clinical markers have been associated with white matter alterations in prior research [23, 26, 31], suggesting that the neurobiological substrate may differ meaningfully between MDD and MDD + ANX.
To provide more precise insights, it is therefore necessary to distinguish between MDD and MDD + ANX. However, studies that made this distinction yielded inconsistent findings. Some reported reduced connectivity in white matter tracts in MDD + ANX compared to MDD and healthy controls (HC; [32, 33]), while others did not [34, 35]. These discrepancies may be attributed to methodological limitations: First, these studies involved small sample sizes of around 100 participants. While such samples may adequately power analyses of specific a priori hypotheses within predefined regions, they are likely insufficient for detecting reliable brain-wide associations when examining numerous tracts across the whole brain [36, 37]. Second, these studies employed tract-based frameworks (e.g., TBSS) that focus on localized alterations, potentially overlooking broader network-level changes [38]. Network-based frameworks, such as Network-Based Statistics (NBS; [39]), offer a different approach by simultaneously modeling the entire structural connectome within a graph-theoretical framework, enabling identification of spatially distributed subnetworks that may be more sensitive to subtle, widespread alterations across multiple pathways.
To overcome these limitations, the present study uses network analysis to investigate structural connectome differences in a large sample of HCs and individuals with MDD and MDD + ANX. While previous white matter studies in MDD + ANX yielded mixed results, the predominant pattern suggests reduced connectivity compared to HCs [32, 33]. We therefore hypothesize to find structural hypoconnectivity in MDD and MDD + ANX relative to HCs. For differences between MDD and MDD + ANX, existing evidence provides limited guidance. Given the more pronounced structural hypoconnectivity found in individuals with earlier disease onset and more severe depressive symptoms [23, 26], and given that individuals with MDD + ANX exhibit precisely these clinical characteristics [12], we anticipate that, compared to individuals with MDD, individuals with MDD + ANX will exhibit more pronounced hypoconnectivity.
Extending this diagnosis-based perspective, additional transdiagnostic analyses are conducted to explore the relationship between structural connectivity and dimensional measures of anxiety across HC, MDD, and MDD + ANX. These analyses provide a more nuanced, symptom-specific understanding of anxiety-related structural connectome alterations, potentially identifying alterations across the anxiety spectrum. We anticipate that individuals with higher levels of anxiety will show more pronounced structural hypoconnectivity regardless of diagnosis.
Materials and methods
Study procedures
Data were collected as part of the Marburg-Münster Affective Disorders Cohort Study (MACS, see [40] for a study protocol and [41] for an MRI quality assurance protocol). The study procedures received approval from the ethics committees at the Universities of Marburg and Münster, Germany. HCs, as well as in- and outpatients aged 18–65 years were recruited through newspaper advertisements or local psychiatric hospitals. All participants provided written informed consent and received financial compensation. Exclusion criteria are detailed in Supplementary 1.
Clinical assessments
The Structured Clinical Interview for DSM-IV-TR Axis I (SCID-I; [42]) was administered to establish lifetime diagnoses of mental disorders. Participants were categorized into three groups: HC were included if they had no history of mental disorders. Individuals with MDD were included if they met criteria for a lifetime diagnosis of MDD but had no comorbid diagnoses for ANX. Individuals with MDD + ANX were included if they met criteria for a lifetime diagnosis of MDD and at least one comorbid ANX. Remission status was assessed according to SCID-I criteria.
Disease course information was collected through a semi-structured interview, including age of onset of first psychiatric symptoms, number of depressive episodes, and number of psychiatric hospitalizations.
Self-report measures
Self-reported anxiety was assessed using the State-Trait Anxiety Inventory (STAI; [43]), a questionnaire comprising two 20-item scales measuring state anxiety and trait anxiety. State and trait sum scores were calculated, with higher scores indicating greater anxiety levels.
Current depressive symptoms were assessed using the Beck Depression Inventory-I (BDI-I; [44]) sum score for descriptive purposes.
Acquisition and processing of MRI data
Two MR scanners were used for MRI data acquisition (see Supplement 2 for acquisition parameters and Supplementary 3 for preprocessing of diffusion-weighted images). We employed the CATO toolbox [45] to reconstruct the anatomical connectome by obtaining the nodes (114 cortical brain regions, depicted by the Cammoun subdivision of Freesurfer’s Desikan-Killiany atlas [46, 47]) from T1-weighted MRI and reconstructing the edges from diffusion-weighted MRI, defined as the number of reconstructed white matter streamlines between two nodes. See Supplementary 4 and 5 for details on the reconstruction and quality control procedures, respectively.
Statistical analysis
Data analysis was conducted using Python 3.7.9 [48] and Matlab 2019b [49]. Figures were created using BrainNet Viewer [50], Simple Brain Plot [51], and Raincloud plots [52]. Statistical tests were conducted at a two-sided significance level of α = 0.05.
Structural connectome differences among diagnostic groups
To assess between-group differences in structural connectivity, we employed network-based statistic (NBS; [39]) analyses. NBS estimated a family-wise error (FWE)-corrected analysis of covariance to test for between-group differences (HC vs. MDD vs. MDD + ANX) in edge-wise connectivity (i.e., number of white matter streamlines) while correcting for age, sex, and scanner site. A primary NBS threshold of F = 4.0 was chosen in these analyses (see Supplementary 6 for details on NBS thresholds) and permutation tests (5000 permutations) were used to evaluate the significance of an identified network. In case of a significant effect, post-hoc t-tests were conducted to explore the pattern of between-group differences. In these post-hoc t-tests, we adjusted the significance level based on the false discovery rate (FDR) to account for multiple comparisons [53].
The topology of networks identified with NBS was characterized using two approaches. First, we identified network nodes with the highest number of affected edges. Second, we quantified the proportion of edges within the identified network connecting frontal, temporal, parietal, occipital, and insular brain regions and compared this to the respective proportions of edges in the entire connectome (derived by counting all edges present in at least 5% of the sample). Third, to assess whether identified networks involved predominantly short-range or long-range connections, we computed the average white matter fiber length within each identified network. This was calculated as the mean total fiber length across participants, where each participant’s total fiber length represented the sum of individual fiber lengths across all edges within the identified network. Using a permutation test, we compared this observed average total fiber length against the distribution of average total fiber lengths from 1000 topology-preserving random networks of identical size.
To verify that observed group differences were not driven by methodological artifacts, we conducted several robustness checks. We evaluated consistency across (1) sexes by repeating analyses separately for males and females; (2) study sites by conducting site-specific analyses; and (3) remission status by separately analyzing acutely depressed individuals and those with partially or fully remitted episodes. We further assessed potential confounds by (4) controlling for non-linear age effects (age²); (5) including head motion parameters (from FSL’s eddy output) as covariates; and (6) excluding connectome outliers identified using established quality control procedures for structural connectivity matrices (see Supplementary 5) [54]. Finally, we verified findings using (7) an alternative connectivity measure (streamline volume density corrected for gray matter volumes) and (8) the original Desikan-Killiany atlas including subcortical regions.
Brain-wide distribution of structural connectivity differences
To examine structural connectivity differences between HC, MDD, and MDD + ANX beyond the identified subnetworks, we calculated age-, sex-, and site-corrected tvalues for nodal estimates of structural connectivity (i.e., the mean number of streamlines connected to a given brain region). We computed t-values for the contrasts between HC and MDD and between HC and MDD + ANX. The resulting t-values were then mapped onto the brain surface for visualization.
Additionally, we conducted meta-analyses of these t-values using two approaches: First, we evaluated the proportion of brain regions showing hypoconnectivity (t < 0) versus hyperconnectivity (t > 0) for each contrast using chi-square tests. Second, we compared the t-values from the HC vs. MDD contrast to those from the HC vs. MDD + ANX contrast using a paired t-test.
Transdiagnostic associations between structural connectivity and anxiety
Continuous associations between structural connectivity and anxiety were tested exploratorily using NBS. Here, NBS estimated two FWE-corrected generalized linear models to test the association between structural connectivity and either state or trait anxiety while correcting for age, sex, and scanner site across HC, and individuals with MDD and MDD + ANX. Permutation tests were used to evaluate network significance, and p-values were adjusted for multiple comparisons based on the FDR. If either of the two undirected generalized linear models identified a network of white matter tracts associated with either state or trait anxiety, a corresponding directed linear regression model was estimated in NBS to explore the primary direction of that association.
Results
Demographic and clinical characteristics of the sample
Our sample consisted of n = 906 HC, n = 532 individuals with MDD, and n = 249 individuals with MDD + ANX (see Table 1). Comorbid anxiety diagnoses (according to DSM-IV) included agoraphobia (n = 7), generalized anxiety disorder (n = 31), obsessive-compulsive disorder (n = 23), panic disorder (n = 65), posttraumatic stress disorder (n = 62), social anxiety disorder (n = 90), and specific phobias (n = 56), with n = 112 (45%) individuals being diagnosed with more than one anxiety disorder.
Diagnostic groups differed in mean age, sex, and site distribution (see Table 1). Individuals with MDD + ANX were predominantly female and reported an earlier disease onset, a higher number of depressive episodes, and more severe depressive symptoms (according to the BDI-I) compared to those with MDD. The latter was also reflected in a higher proportion of acutely depressed individuals in the MDD + ANX group and a higher proportion of individuals in full remission in the MDD group. Details on patient medications and comorbid disorders are provided in Supplementary 7 and 8.
Network-based differences in structural connectivity among diagnostic groups
Our NBS analysis identified significant components of the structural connectome capturing differences in edge-wise structural connectivity between HC, MDD, and MDD + ANX (NBS F-threshold F = 4.0, pFWE = 0.008, partial η²=0.009). Post-hoc t-tests revealed that these differences were driven by significant decreases in structural connectivity in individuals with MDD (NBS t-threshold t = –1.962, pFWE,FDR < 0.05, 42 edges, Cohen’s d = –0.467) and significant increases in structural connectivity in individuals with MDD + ANX (NBS t-threshold t = 1.962, pFWE,FDR < 0.05, 170 edges, Cohen’s d = 0.759) relative to HC. Consequently, we also identified a subnetwork characterized by significant increases in structural connectivity in individuals with MDD + ANX as compared to those with MDD, though at a lower threshold (NBS t-threshold t = 1.9, pFWE,FDR < 0.05, 126 edges, Cohen’s d = 0.735).
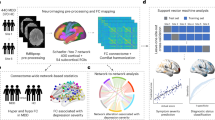
To explore whether these decreases and increases in structural connectivity were detectable within an interconnected subnetwork of edges, we performed an additional, directed NBS analysis specifically testing for the observed pattern of MDD < HC < MDD + ANX. This analysis identified a subnetwork that precisely matched this pattern (NBS t-threshold t = 1.962, pFWE = 0.028, 109 edges, see Fig. 1A, B), meaning that in each edge of that network, individuals with MDD exhibited decreased connectivity and individuals with MDD + ANX exhibited increased connectivity compared to HC. Nodes with the highest number of affected edges of that network were localized within the right insula, right superior temporal gyrus, left rostral middle-frontal gyrus, left superior temporal gyrus, right parahippocampal gyrus, and right temporal pole. The network mainly comprised fronto-frontal, fronto-parietal, and temporo-parietal edges (14.7%, 15.6%, and 12.8% of network edges, respectively). However, comparisons of the identified network with the distribution of edges present in the entire connectome also revealed a disproportionately high number of affected edges connecting frontal and occipital brain regions (11%; \(\chi\)2 = 43.70, p < 0.001, see Fig. 1C), suggesting a particular involvement of long-range connections. This was corroborated by a significantly higher average white matter fiber length within the identified network compared to the average white matter fiber lengths from 1000 topology-preserving random networks of identical size (pperm = 0.006, see Fig. 1D).
Network of white matter fiber tracts capturing differences among healthy controls (HC) as well as depressed individuals without (MDD) and with comorbid anxiety disorder (MDD + ANX). A Axial view of the network identified via NBS. Node size represents the number of affected edges connected to each region, with larger nodes indicating hub regions within the network. Nodes with the highest number of affected edges are labeled with their anatomical region names. Edge thickness reflects the effect size (t statistic) for each connection, with thicker edges indicating stronger group differences. B Between-group differences in the identified network, with effect sizes shown as Cohen’s d. C Frequency of edges connecting frontal, temporal, parietal, occipital, and insular regions in the identified network, compared to the frequency of the respective edges in the full connectome. D Individual estimates of total fiber length across all edges in the identified network versus the first of 1000 size- and topology-matched random networks, with comparison of mean total fiber length (averaged across individuals) in the identified network to mean total fiber lengths in all 1000 randomly selected networks (upper right corner). E Pattern of between-group differences in robustness checks (see Supplementary 9 for effect sizes). Robustness checks included: (1) separate analyses for males and females; (2) separate analyses for participants from either study site; (3) separate analyses for participants with acute, partially remitted or remitted depressive episode; (4) correcting for non-linear age effects; (5) including head motion as a covariate (derived from FSL’s eddy output); (6) excluding connectome outliers; (7) using an alternative measure of structural connectivity (streamline volume density) corrected for gray matter volumes; and (8) using the original Desikan-Killiany atlas that includes subcortical regions. See online version for colored figures.
In robustness checks, we verified that the observed pattern of increased and decreased connectivity in individuals with MDD and MDD + ANX was not driven by (1) sex-specific differences in structural connectivity; (2) differences between study sites; (3) the participants’ remission status; (4) non-linear age effects; (5) the participants’ head movements during MRI acquisition; (6) outliers in structural connectivity; (7) differences in gray matter volume of the connected brain regions; or (8) our decision of excluding subcortical brain regions from our analysis; None of these approaches changed the pattern of results (see Fig. 1E), with effect sizes across robustness checks ranging between Cohen’s d = −0.33 to –0.23 (HC vs. MDD), d = 0.23 to 0.60 (HC vs. MDD + ANX), and d = 0.46 to 0.83 (MDD vs. MDD + ANX; see Supplementary 9). Furthermore, we examined the extent to which the choice of the primary NBS threshold influenced our results (see Supplementary 10). As expected, less stringent thresholds yielded more widespread networks; however, the overall pattern of findings remained consistent, with effect sizes ranging between Cohen’s d = −0.30 to −0.41 (HC vs. MDD), d = 0.27 to 0.42 (HC vs. MDD + ANX), and d = 0.65 to 0.72 (MDD vs. MDD + ANX).
Brain-wide distribution of structural connectivity differences
We examined the spatial distribution of structural connectome alterations across the entire brain by analyzing nodal estimates of structural connectivity (see Fig. 2A–C). Descriptively, structural hypoconnectivity (i.e., reductions in connectivity relative to HC) was less prevalent in the structural connectome of individuals with MDD + ANX (53% of brain regions) than in those with MDD (67% of brain regions). Conversely, increases in connectivity were found more widespread across the structural connectome of individuals with MDD + ANX (47% of brain regions) than in those with MDD (33% of brain regions, \(\chi\)2 = 4.67, p = .031). These differences resulted in a substantial proportion of the structural connectome of individuals with MDD + ANX showing increased structural connectivity compared to individuals with MDD (59% of brain regions). Meta-analytical comparisons revealed that node-wise t-values were indeed significantly lower in the HC vs. MDD contrast as compared to the HC vs. MDD + ANX contrast (paired ttest t = –2.942, p = 0.002, Cohen’s d = 0.333), with particular differences in the connectivity of occipital and insular brain regions (see Fig. 2D).
Spatial distribution of between-group differences (t-values) in nodal structural connectivity (mean number of streamlines connected to a given node). A Differences between healthy controls (HC) and individuals with depression but without comorbid anxiety disorder (MDD). B Differences between HC and individuals with depression and comorbid anxiety disorder (MDD + ANX). C Differences between MDD and MDD + ANX. D Comparison of t-values for nodal structural connectivity differences between HC and MDD to those between HC and MDD + ANX across all 114 nodes (“whole-brain”), and separately within frontal, temporal, parietal, occipital, and insular brain regions. See online version for colored figures.
Transdiagnostic associations between structural connectivity and anxiety
Our transdiagnostic analyses identified subnetworks of edges where structural connectivity was significantly associated with state and trait anxiety across all participants (state anxiety: NBS F-threshold F = 4.0, pFWE,FDR < 0.05, 186 edges; trait anxiety: NBS F-threshold F = 4.0, pFWE,FDR < 0.05, 162 edges). Post-hoc directed linear regression models revealed that these associations predominantly followed a positive direction (state anxiety: NBS t-threshold t = 1.962, pFWE < 0.05, 154 edges, partial η2 = 0.005; trait anxiety: NBS t-threshold t = 1.962, pFWE < 0.05, 118 edges, partial η2 = 0.005; see Fig. 3), indicating that higher levels of anxiety were associated with increases in structural connectivity across HC, MDD, and MDD + ANX.
Node size represents the number of affected edges connected to each region (degree), with larger nodes indicating hub regions within the network. Nodes with the highest number of affected edges are labeled with their anatomical region names. Edge thickness reflects the effect size (F-statistic) for each connection, with thicker edges indicating stronger group differences. See online version for colored figures.
Discussion
Individuals with MDD + ANX experience earlier disease onset, more severe depressive symptoms, and greater functional impairments than those with MDD alone. Despite this significant clinical burden, the neurobiological underpinnings of MDD + ANX remain poorly understood. The present study investigated structural connectome alterations in a large sample of HC and individuals diagnosed with MDD or MDD + ANX. Contrary to our hypotheses, our analyses revealed that the structural connectome in individuals with MDD + ANX is at least partially defined by hyperconnectivity rather than hypoconnectivity. Transdiagnostic analyses indicated that this pattern even extends to HCs and individuals with MDD with elevated levels of anxiety but without ANX. In the following, we will discuss these findings and explore broader implications for future network neuroscience research in mental health.
Previous research on connectome alterations in mental disorders has identified marked patterns of structural hypoconnectivity, i.e., reduced connectivity, particularly in those with an earlier age of onset and more severe depressive symptoms [21, 23, 26]. In the present study, individuals with MDD indeed exhibited this expected pattern of hypoconnectivity. However, those with MDD + ANX displayed a contrasting pattern of structural hyperconnectivity, which was unexpected given their earlier onset and higher depressive symptom severity. To ensure the robustness of this finding, we conducted several analyses to rule out potential confounding factors, such as sex differences or methodological artifacts. Across all these analyses, the hyperconnectivity in individuals with MDD + ANX persisted. Importantly, this pattern was consistently found across different analytical approaches, such as subnetwork-specific and brain-wide analyses, and across observer-rated diagnoses as well as self-reported anxiety data. Post hoc analyses further revealed that these alterations converged on long-range connections and particularly affected insular brain regions. The robustness and spatial consistency of these results suggest that they are not merely artifacts of specific methods or assessments.
Our finding of hyperconnectivity associated with elevated trait and state anxiety raises the question of whether these results reflect stable trait characteristics or rather transient state effects. While our diagnosis-based analysis might suggest a trait effect, there is evidence that sustained elevations in current affective symptoms can indeed be linked with alterations in structural connectivity [26]. However, in the present study, a definitive examination of state versus trait effects of anxiety was limited by the high intercorrelation between these measures, which precludes clear separation of their unique contributions. Moreover, cross-sectional DWI studies are inherently constrained in their ability to distinguish between state and trait effects [55]. To determine whether the observed hyperconnectivity is attributable primarily to trait factors that precede disease onset or to (potentially sustained) state effects emerging during illness progression, longitudinal designs with repeated assessments are required [55].
The mechanisms underlying the identified pattern of structural hyperconnectivity remain speculative, given the lack of large-scale studies on structural connectivity alterations in MDD + ANX. Hypotheses on these mechanisms may be drawn from other modalities, such as functional connectivity. One possibility involves a compensatory mechanism, wherein hyperconnectivity in certain connections offsets hypoconnectivity elsewhere in the connectome [38, 56]. However, the higher disease severity in individuals with MDD + ANX questions the effectiveness of this compensation. An alternative explanation may lie in hyperconnectivity resulting from anxiety-related hypervigilance and heightened threat response: For instance, previous studies have linked increased functional connectivity to early life adversity in rodents [57] and heightened threat response in generalized anxiety disorder [58], as well as hyperactivation of the fear circuit in social anxiety disorder [59]. Given the known relationship between functional and structural connectivity [60, 61], functional hyperconnectivity may, over time, translate into structural hyperconnectivity through Hebbian plasticity [62]. Future large-scale studies could examine whether functional hyperconnectivity following dysfunctional threat response precedes structural hyperconnectivity in MDD + ANX.
While our findings suggest that the nature of dysconnectivity in MDD—whether reduced or increased—depends on the individual clinical profile, we do not propose that these patterns could serve as reliable biomarkers for differential diagnosis. Consistent with prior studies, the effect sizes observed in our study are small, rendering our findings insufficient for differentiating between diagnoses at the individual level [23, 63, 64]. This limited effect size may reflect individual deviations from group-level patterns, for instance, due to comorbidity with other mental disorders, heterogeneity in depressive symptom profiles, and the individually diverse locations of neurobiological alterations in mental disorders [65,66,67,68]. Given this variability, reliably detecting structural connectome differences across all combinations of diagnoses and comorbidities would require enormous sample sizes, rendering traditional group comparisons impractical.
To advance psychiatric network neuroscience, future studies should focus on identifying transdiagnostic biomarkers for specific symptoms rather than relying on diagnostic categories [69], embedded in frameworks such as the Research Domain Criteria [70, 71]. Our transdiagnostic analysis of anxiety-related connectome alterations exemplifies this approach. In future research, this strategy should be expanded to address multiple symptom dimensions simultaneously, thereby identifying alterations that are truly symptom-specific. Integrating individual symptom networks, which model the individual co-occurrence of psychiatric symptoms [72], with brain networks in multi-layer networks may offer a promising avenue for this line of research [73]. Such approaches may help determine if structural hyperconnectivity is linked to specific symptom clusters or biological profiles, such as immuno-metabolic depression [74]. Normative modeling may further enhance these strategies by identifying brain structural alterations relative to normative variations at the subject-level [75]. This combination of methods may help unravel the neurobiological basis of specific symptoms, ultimately paving the way for symptom-tailored interventions rooted in neurobiology [76, 77].
Several limitations should be noted. First, our analyses focused on anxiety as a broad syndrome without further differentiation. Future research should investigate whether different symptoms exhibit distinct structural connectome signatures. Second, our study lacks a group of patients with ANX but without MDD. Based on our findings, we would expect an even more pronounced pattern of structural hyperconnectivity in this group. Third, field maps for distortion correction were not available for this dataset, which may have affected the precision of our tractography results, particularly in regions prone to susceptibility-induced distortions such as orbitofrontal and anterior temporal areas. Fourth, the relatively smaller sample size of the MDD + ANX group may raise concerns. However, it is unlikely to account for the observed pattern of hyperconnectivity, as increases in structural connectivity were also observed in our transdiagnostic analysis covering the entire sample. Finally, this study was not pre-registered, and findings should therefore be interpreted as exploratory and require replication in independent samples.
In conclusion, our findings shed light on the nature of structural connectome alterations in MDD and MDD + ANX, challenging the traditional narrative of dysconnectivity as a linear marker of depressive symptom severity. The unexpected discovery of hyperconnectivity in individuals with MDD + ANX, a group with more severe depressive symptoms, underscores the need for a paradigm shift in psychiatric network neuroscience that prioritizes individualized, symptom-specific research.
Data availability
All data are available in the main text or the supplementary materials. Participant data used in this study, informed consent forms, and scripts employed for analysis will be made available upon reasonable request to the corresponding author.
References
Ferrari AJ, Santomauro DF, Aali A, Abate YH, Abbafati C, Abbastabar H, et al. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403:2133–61.
Bijl RV, Ravelli A, van Zessen G. Prevalence of psychiatric disorder in the general population: results of The Netherlands Mental Health Survey and Incidence Study (NEMESIS). Soc Psychiatry Psychiatr Epidemiol. 1998;33:587–95.
Ebmeier KP, Donaghey C, Steele JD. Recent developments and current controversies in depression. Lancet Lond Engl. 2006;367:153–67.
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:593–602.
Somers JM, Goldner EM, Waraich P, Hsu L. Prevalence and incidence studies of anxiety disorders: a systematic review of the literature. Can J Psychiatry Rev Can Psychiatr. 2006;51:100–13.
Kessler RC, Sampson NA, Berglund P, Gruber MJ, Al-Hamzawi A, Andrade L, et al. Anxious and non-anxious major depressive disorder in the World Health Organization World Mental Health Surveys. Epidemiol Psychiatr Sci. 2015;24:210–26.
ter Meulen WG, Draisma S, van Hemert AM, Schoevers RA, Kupka RW, Beekman ATF, et al. Depressive and anxiety disorders in concert–A synthesis of findings on comorbidity in the NESDA study. J Affect Disord. 2021;284:85–97.
Brawman-Mintzer O, Lydiard RB, Emmanuel N, Payeur R, Johnson M, Roberts J, et al. Psychiatric comorbidity in patients with generalized anxiety disorder. Am J Psychiatry. 1993;150:1216–8.
Dunner DL. Management of anxiety disorders: the added challenge of comorbidity. Depress Anxiety. 2001;13:57–71.
Boschloo L, van Borkulo CD, Rhemtulla M, Keyes KM, Borsboom D, Schoevers RA. The Network Structure of Symptoms of the Diagnostic and Statistical Manual of Mental Disorders. PloS One. 2015;10:e0137621.
Forbes MK, Neo B, Nezami OM, Fried EI, Faure K, Michelsen B, et al. Elemental psychopathology: distilling constituent symptoms and patterns of repetition in the diagnostic criteria of the DSM-5. Psychol Med. 2024;54:886–94.
Kalin NH. The critical relationship between anxiety and depression. Am J Psychiatry. 2020;177:365–7.
Fava M, Alpert JE, Carmin CN, Wisniewski SR, Trivedi MH, Biggs MM, et al. Clinical correlates and symptom patterns of anxious depression among patients with major depressive disorder in STAR*D. Psychol Med. 2004;34:1299–308.
Kessler RC, Akiskal HS, Ames M, Birnbaum H, Greenberg P, Hirschfeld RMA, et al. Prevalence and effects of mood disorders on work performance in a nationally representative sample of U.S. workers. Am J Psychiatry. 2006;163:1561–8.
Penninx BWJH, Nolen WA, Lamers F, Zitman FG, Smit JH, Spinhoven P, et al. Two-year course of depressive and anxiety disorders: results from the Netherlands Study of Depression and Anxiety (NESDA). J Affect Disord. 2011;133:76–85.
Friston K, Brown HR, Siemerkus J, Stephan KE. The dysconnection hypothesis (2016). Schizophr Res. 2016;176:83–94.
Geschwind N. Disconnexion syndromes in animals and man. Brain. 1965;88:237.
van den Heuvel MP, Sporns O. A cross-disorder connectome landscape of brain dysconnectivity. Nat Rev Neurosci. 2019;20:435–46.
Hagmann P. From diffusion MRI to brain connectomics. [Lausanne]: EPFL; 2005.
Sporns O, Tononi G, Kötter R. The human connectome: a structural description of the human brain. PLOS Comput Biol. 2005;1:e42.
de Lange SC, Scholtens LH, van den Berg LH, Boks MP, Bozzali M, Cahn W, et al. Shared vulnerability for connectome alterations across psychiatric and neurological brain disorders. Nat Hum Behav. 2019;3:988–98.
Perry A, Roberts G, Mitchell PB, Breakspear M. Connectomics of bipolar disorder: a critical review, and evidence for dynamic instabilities within interoceptive networks. Mol Psychiatry. 2019;24:1296–318.
Repple J, Gruber M, Mauritz M, de Lange SC, Winter NR, Opel N, et al. Shared and Specific Patterns of Structural Brain Connectivity Across Affective and Psychotic Disorders. Biol Psychiatry. 2023;93:178–86.
Van Den Heuvel MP, Sporns O, Collin G, Scheewe T, Mandl RCW, Cahn W, et al. Abnormal rich club organization and functional brain dynamics in schizophrenia. JAMA Psychiatry. 2013;70:783–92.
van Velzen LS, Kelly S, Isaev D, Aleman A, Aftanas LI, Bauer J, et al. White matter disturbances in major depressive disorder: a coordinated analysis across 20 international cohorts in the ENIGMA MDD working group. Mol Psychiatry. 2020;25:1511–25.
Repple J, Mauritz M, Meinert S, de Lange SC, Grotegerd D, Opel N, et al. Severity of current depression and remission status are associated with structural connectome alterations in major depressive disorder. Mol Psychiatry. 2020;25:1550–8.
Li BJ, Friston K, Mody M, Wang HN, Lu HB, Hu DW. A brain network model for depression: From symptom understanding to disease intervention. CNS Neurosci Ther. 2018;24:1004–19.
Sindermann L, Redlich R, Opel N, Böhnlein J, Dannlowski U, Leehr EJ. Systematic transdiagnostic review of magnetic-resonance imaging results: Depression, anxiety disorders and their co-occurrence. J Psychiatr Res. 2021;142:226–39.
van Tol MJ, van der Wee NJA, Veltman DJ. Fifteen years of NESDA Neuroimaging: An overview of results related to clinical profile and bio-social risk factors of major depressive disorder and common anxiety disorders. J Affect Disord. 2021;289:31–45.
Xu EP, Nguyen L, Leibenluft E, Stange JP, Linke JO. A meta-analysis on the uncinate fasciculus in depression. Psychol Med. 2023;53:2721–31.
Meinert S, Leehr EJ, Grotegerd D, Repple J, Förster K, Winter NR, et al. White matter fiber microstructure is associated with prior hospitalizations rather than acute symptomatology in major depressive disorder. Psychol Med. 2020;52:1166–74.
Heij GJ, Penninx BWHJ, van Velzen LS, van Tol MJ, van der Wee NJA, Veltman DJ, et al. White matter architecture in major depression with anxious distress symptoms. Prog Neuropsychopharmacol Biol Psychiatry. 2019;94:109664.
Lai CH, Wu YT. The white matter microintegrity alterations of neocortical and limbic association fibers in major depressive disorder and panic disorder: the comparison. Med (Balt). 2016;95:e2982.
Canu E, Kostić M, Agosta F, Munjiza A, Ferraro PM, Pesic D, et al. Brain structural abnormalities in patients with major depression with or without generalized anxiety disorder comorbidity. J Neurol. 2015;262:1255–65.
Delaparte L, Yeh FC, Adams P, Malchow A, Trivedi MH, Oquendo MA, et al. A comparison of structural connectivity in anxious depression versus non-anxious depression. J Psychiatr Res. 2017;89:38–47.
Helwegen K, Libedinsky I, van den Heuvel MP. Statistical power in network neuroscience. Trends Cogn Sci. 2023;27:282–301.
Marek S, Tervo-Clemmens B, Calabro FJ, Montez DF, Kay BP, Hatoum AS, et al. Reproducible brain-wide association studies require thousands of individuals. Nature. 2022;603:654–60.
Fornito A, Zalesky A, Breakspear M. The connectomics of brain disorders. Nat Rev Neurosci. 2015;16:159–72.
Zalesky A, Fornito A, Bullmore ET. Network-based statistic: Identifying differences in brain networks. NeuroImage. 2010;53:1197–207.
Kircher T, Wöhr M, Nenadic I, Schwarting R, Schratt G, Alferink J, et al. Neurobiology of the major psychoses: a translational perspective on brain structure and function—the FOR2107 consortium. Eur Arch Psychiatry Clin Neurosci. 2019;269:949–62.
Vogelbacher C, Möbius TWD, Sommer J, Schuster V, Dannlowski U, Kircher T, et al. The Marburg-Münster Affective Disorders Cohort Study (MACS): a quality assurance protocol for MR neuroimaging data. NeuroImage. 2018;172:450–60.
Wittchen H, Wunderlich U, Gruschwitz S, Zaudig M., Skid I. Strukturiertes Klinisches Interview für DSM-IV. Achse I: Psychische Störungen. Interviewheft und Beurteilungsheft. Göttingen, Germany: Hogrefe; 1997.
Spielberger C, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983.
Beck AT, Steer RA, Carbin MG. Psychometric properties of the beck depression inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100.
de Lange SC, Helwegen K, van den Heuvel MP. Structural and functional connectivity reconstruction with CATO - A Connectivity Analysis TOolbox. NeuroImage. 2023;273:120108.
Cammoun L, Gigandet X, Meskaldji D, Thiran JP, Sporns O, Do KQ, et al. Mapping the human connectome at multiple scales with diffusion spectrum MRI. J Neurosci Methods. 2012;203:386–97.
Desikan RS, Ségonne F, Fischl B, Quinn BT, Dickerson BC, Blacker D, et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. NeuroImage. 2006;31:968–80.
Van Rossum G, Drake FL. Python 3 Reference Manual. Scotts Valley, CA: CreateSpace. Scotts Valley, CA: CreateSpace; 2019.
MATLAB. 9.7.0.1190202 (R2019b). Natick, Massachusetts: The MathWorks Inc.; 2019.
Xia M, Wang J, He Y. BrainNet Viewer: A Network Visualization Tool for Human Brain Connectomics. PLoS One. 2013;8:e68910.
Scholtens LH, de Lange SC, van den Heuvel MP. Simple brain plot [Internet]. Zenodo; 2021 [cited 2024 Aug 19]. Available from: https://zenodo.org/records/5346593.
Allen M, Poggiali D, Whitaker K, Marshall TR, Kievit RA. Raincloud plots: a multi-platform tool for robust data visualization. Wellcome Open Res. 2019;4:63.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol. 1995;57:289–300.
Van Den Heuvel MP, Scholtens LH, Van Der Burgh HK, Agosta F, Alloza C, Arango C, et al. 10kin1day: a bottom-up neuroimaging initiative. Front Neurol. 2019;10:425.
Schmaal L, van Velzen LS. Deficits in white matter microstructure in major depressive disorder: cause, consequence, or correlate?. Biol Psychiatry. 2019;86:734–5.
Hillary FG, Grafman JH. Injured Brains and Adaptive Networks: The Benefits and Costs of Hyperconnectivity. Trends Cogn Sci. 2017;21:385–401.
Johnson FK, Delpech JC, Thompson GJ, Wei L, Hao J, Herman P, et al. Amygdala hyper-connectivity in a mouse model of unpredictable early life stress. Transl Psychiatry. 2018;8:49.
Buff C, Brinkmann L, Neumeister P, Feldker K, Heitmann C, Gathmann B, et al. Specifically altered brain responses to threat in generalized anxiety disorder relative to social anxiety disorder and panic disorder. NeuroImage Clin. 2016;12:698–706.
Brühl AB, Delsignore A, Komossa K, Weidt S. Neuroimaging in social anxiety disorder—A meta-analytic review resulting in a new neurofunctional model. Neurosci Biobehav Rev. 2014;47:260–80.
Honey CJ, Sporns O, Cammoun L, Gigandet X, Thiran JP, Meuli R, et al. Predicting human resting-state functional connectivity from structural connectivity. Proc Natl Acad Sci. 2009;106:2035–40.
Suárez LE, Markello RD, Betzel RF, Misic B. Linking Structure and Function in Macroscale Brain Networks. Trends Cogn Sci. 2020;24:302–15.
Lazari A, Salvan P, Cottaar M, Papp D, Rushworth MFS, Johansen-Berg H. Hebbian activity-dependent plasticity in white matter. Cell Rep. 2022;39:110951.
Winter NR, Leenings R, Ernsting J, Sarink K, Fisch L, Emden D, et al. Quantifying deviations of brain structure and function in major depressive disorder across neuroimaging modalities. JAMA Psychiatry. 2022;79:879–88.
Winter NR, Blanke J, Leenings R, Ernsting J, Fisch L, Sarink K, et al. A systematic evaluation of machine learning-based biomarkers for major depressive disorder. JAMA Psychiatry. 2024;81:386–95.
Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:617–27.
Fried EI, Nesse RM. Depression is not a consistent syndrome: An investigation of unique symptom patterns in the STAR*D study. J Affect Disord. 2015;172:96–102.
Segal A, Parkes L, Aquino K, Kia SM, Wolfers T, Franke B, et al. Regional, circuit and network heterogeneity of brain abnormalities in psychiatric disorders. Nat Neurosci. 2023;26:1613–29.
Spiller TR, Duek O, Helmer M, Murray JD, Fielstein E, Pietrzak RH, et al. Unveiling the structure in mental disorder presentations. JAMA Psychiatry. 2024;81:1101–7.
Segal A, Tiego J, Parkes L, Holmes AJ, Marquand AF, Fornito A. Embracing variability in the search for biological mechanisms of psychiatric illness. Trends Cogn Sci. 2025;29:85–99.
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–51.
Insel TR. The NIMH research domain criteria (RDoC) Project: precision medicine for psychiatry. Am J Psychiatry. 2014;171:395–7.
Borsboom D. A network theory of mental disorders. World Psychiatry J World Psychiatr Assoc WPA. 2017;16:5–13.
Blanken TF, Bathelt J, Deserno MK, Voge L, Borsboom D, Douw L. Connecting brain and behavior in clinical neuroscience: a network approach. Neurosci Biobehav Rev. 2021;130:81–90.
Penninx BWJH, Lamers F, Jansen R, Berk M, Khandaker GM, De Picker L, et al. Immuno-metabolic depression: from concept to implementation. Lancet Reg Health Eur. 2025;48:101166.
Marquand AF, Rezek I, Buitelaar J, Beckmann CF. Understanding heterogeneity in clinical cohorts using normative models: beyond case-control studies. Biol Psychiatry. 2016;80:552–61.
Siddiqi SH, Taylor SF, Cooke D, Pascual-Leone A, George MS, Fox MD. Distinct symptom-specific treatment targets for circuit-based neuromodulation. Am J Psychiatry. 2020;177:435–46.
Tozzi L, Bertrand C, Hack LM, Lyons T, Olmsted AM, Rajasekharan D, et al. A cognitive neural circuit biotype of depression showing functional and behavioral improvement after transcranial magnetic stimulation in the B-SMART-fMRI trial. Nat Ment Health. 2024;2:987–98.
Acknowledgements
This work is part of the German multicenter consortium “Neurobiology of Affective Disorders. A translational perspective on brain structure and function”, and the LOEWE Center DYNAMIC. Principal investigators (PIs) with respective areas of responsibility in the FOR2107 consortium are: Work Package WP1, FOR2107/MACS cohort and brainimaging: Tilo Kircher (speaker FOR2107), Udo Dannlowski (co-speaker FOR2107), Axel Krug, Igor Nenadic, Carsten Konrad. CP1, biobank: Petra Pfefferle, Harald Renz. CP2, administration. Tilo Kircher, Udo Dannlowski, Carsten Konrad. Data access and responsibility: All PIs take responsibility for the integrity of the respective study data and their components. All authors and coauthors had full access to all study data. Acknowledgements and members by Work Package (WP): WP1: Henrike Bröhl, Katharina Brosch, Bruno Dietsche, Rozbeh Elahi, Jennifer Engelen, Sabine Fischer, Jessica Heinen, Svenja Klingel, Felicitas Meier, Tina Meller, Torsten Sauder, Simon Schmitt, Frederike Stein, Annette Tittmar, Dilara Yüksel (Dept. of Psychiatry, Marburg University). Mechthild Wallnig, Rita Werner (Core-Facility Brainimaging, Marburg University). Carmen Schade-Brittinger, Maik Hahmann (Coordinating Center for Clinical Trials, Marburg). Michael Putzke (Psychiatric Hospital, Friedberg). Rolf Speier, Lutz Lenhard (Psychiatric Hospital, Haina). Birgit Köhnlein (Psychiatric Practice, Marburg). Peter Wulf, Jürgen Kleebach, Achim Becker (Psychiatric Hospital Hephata, Schwalmstadt-Treysa). Ruth Bär (Care facility Bischoff, Neunkirchen). Matthias Müller, Michael Franz, Siegfried Scharmann, Anja Haag, Kristina Spenner, Ulrich Ohlenschläger (Psychiatric Hospital Vitos, Marburg). Matthias Müller, Michael Franz, Bernd Kundermann (Psychiatric Hospital Vitos, Gießen). Christian Bürger, Katharina Dohm, Fanni Dzvonyar, Verena Enneking, Stella Fingas, Katharina Förster, Janik Goltermann, Dominik Grotegerd, Hannah Lemke, Susanne Meinert, Nils Opel, Ronny Redlich, Jonathan Repple, Kordula Vorspohl, Bettina Walden, Dario Zaremba (Dept. of Psychiatry, University of Münster). Harald Kugel, Jochen Bauer, Walter Heindel, Birgit Vahrenkamp (Dept. of Clinical Radiology, University of Münster). Gereon Heuft, Gudrun Schneider (Dept. of Psychosomatics and Psychotherapy, University of Münster). Thomas Reker (LWL-Hospital Münster). Gisela Bartling (IPP Münster). Ulrike Buhlmann (Dept. of Clinical Psychology, University of Münster). CP1: Julian Glandorf, Fabian Kormann, Arif Alkan, Fatana Wedi, Lea Henning, Alena Renker, Karina Schneider, Elisabeth Folwarczny, Dana Stenzel, Kai Wenk, Felix Picard, Alexandra Fischer, Sandra Blumenau, Beate Kleb, Doris Finholdt, Elisabeth Kinder, Tamara Wüst, Elvira Przypadlo, Corinna Brehm (Comprehensive Biomaterial Bank Marburg, Marburg University). This work was funded by the German Research Foundation (DFG, Work Package WP1, FOR2107/MACS cohort and brainimaging: Tilo Kircher (DFG grant numbers KI 588/14-1, KI 588/14-2, HA7070/2-2, HA7070/3, HA7070/4), Udo Dannlowski (DA 1151/5-1, DA 1151/5-2), Axel Krug (KR 3822/5-1, KR 3822/7-2), Igor Nenadic (NE 2254/1-2), Carsten Konrad (KO 4291/3-1). CP1, biobank: Petra Pfefferle (PF 784/1-1, PF 784/1-2), Harald Renz (RE 737/20-1, 737/20-2). CP2, administration. Tilo Kircher (KI 588/15-1, KI 588/17-1), Udo Dannlowski (DA 1151/6-1), Carsten Konrad (KO 4291/4-1)), the Interdisciplinary Center for Clinical Research (IZKF) of the medical faculty of Münster (grant Dan3/012/17 to UD), IMF Münster RE 22 17 07 to JR and the Deanery of the Medical Faculty of the University of Münster. MP was supported by an ERC Consolidator grant (101001062 CONNECT) and a NWO VICI grant (VI.C.241.074 BrainDiversity) from the Netherlands Organization for Scientific Research. The DYNAMIC center is funded by the LOEWE program of the Hessian Ministry of Science and Arts (Grant Number: LOEWE1/16/519/03/09.001(0009)/98).
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Conceptualization: MG, JS, KFA, PR, NvW, HS, SF, FT, JR Methodology: MG, JS, MM, IL, MvdH, JR Investigation: MG, JS, KFA, PR, NvW, HS, SF, FT, PG, LMB, JG, NRW, KT, AW, TB, MK, HM, JH, JK, CJ, FTO, PU, LT, LS, JB, SM, DG, FS Visualization: MG, JS, MM, JR Supervision: MP, KF, LS, JB, SM, DG, FS, VJ, NA, HJ, AJ, IN, NO, TH, JB, MvdH, AR, TK, EJL, UD, JR Writing—original draft: MG, JS, JR Writing—review & editing: MG, JS, MM, KFA, PR, NvW, HS, SF, FT, IL. PG, LMB, JG, NRW, KT, AW, TB, MK, HM, JH, JK, CJ, FTO, PU, LT, MP, KF, LS, JB, SM, DG, FS, BS, NA, HJ, AJ, IN, NO, TH, JB, MvdH, AR, TK, EJL, UD, JR.
Corresponding author
Ethics declarations
Competing interests
MG and KFA received remuneration from Janssen for consultancy services. JR received speaker’s honoraria from Janssen, Hexal, Neuraxpharm, and Novartis. TK received unrestricted educational grants from Servier, Janssen, Recordati, Aristo, Otsuka, neuraxpharm. This cooperation has no relevance to the work that is covered in the manuscript. The other authors declare no financial interests or competing interests.
Ethical
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gruber, M., Schulte, J., Mauritz, M. et al. Network-based analysis of differential white matter connectivity in major depressive disorder with and without comorbid anxiety. Neuropsychopharmacol. (2026). https://doi.org/10.1038/s41386-025-02312-y
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41386-025-02312-y