Abstract
Background
Prostate Cancer (PCa) is a leading cause of cancer-related mortality globally. Clinically significant PCa (CsPCa) is associated with more aggressive disease, making accurate diagnosis crucial. Multiparametric Magnetic Resonance Imaging (Mp-MRI) is a well-established tool for PCa detection, but the dynamic contrast-enhanced (DCE) sequence raises concerns due to cost, risks, and patient experience. Biparametric MRI (Bp-MRI) has emerged as an alternative, but its diagnostic performance compared to Mp-MRI has not been thoroughly examined through a systematic review and meta-analysis in recent years.
Methods
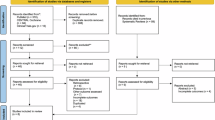
A systematic review and meta-analysis were conducted to compare the diagnostic accuracy of Bp-MRI and Mp-MRI for detecting CsPCa by assessing the databases MEDLINE/PubMed, CENTRAL Cochrane, and ClinicalTrials.gov. Studies published between 2012 and 2024 that compared Bp-MRI and Mp-MRI using histopathological analysis as the reference standard were included. Data were extracted to obtain diagnostic test accuracy measurements (sensitivity, specificity, diagnostic odds ratio, positive and negative likelihood ratios) and study characteristics. Statistical analysis involved two bivariate random-effects models, a summary Receiver Operating Characteristic (sROC) curve, and meta-regression models assessing the comparison of both diagnostic test accuracies and the interaction of different study-level covariates.
Results
Nineteen studies involving 5,173 patients were included. Mp-MRI demonstrated a pooled sensitivity of 0.90 (95% CI: 0.87–0.93) and a specificity of 0.64 (95% CI: 0.50–0.76), while Bp-MRI showed a pooled sensitivity of 0.89 (95% CI: 0.85–0.92) and a specificity of 0.73 (95% CI: 0.62–0.82). Both modalities showed similar diagnostic performance with overlapping sROC curves. Meta-regression revealed no statistically significant difference between the two tools, and the study-level covariates did not influence the results.
Conclusion
Bp-MRI is a viable alternative to Mp-MRI for detecting CsPCa, with comparable diagnostic accuracy, especially when contrast agents are a concern. Further prospective randomized studies are needed to confirm these findings.
Registry
PROSPERO (CRD42024552125).
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
All data analyzed or generated during the development of this study are included in this published article and its supplementary data file.
References
Bergengren O, Pekala KR, Matsoukas K, Fainberg J, Mungovan SF, Bratt O, et al. 2022 Update on Prostate Cancer Epidemiology and Risk Factors-A Systematic Review. Eur Urol. 2023;84:191–206.
Gandaglia G, Leni R, Bray F, Fleshner N, Freedland SJ, Kibel A, et al. Epidemiology and Prevention of Prostate Cancer. Eur Urol Oncol. 2021;4:877–92.
Rawla P. Epidemiology of Prostate Cancer. World J Oncol. 2019;10:63–89.
Matoso A, Epstein JI. Defining clinically significant prostate cancer on the basis of pathological findings. Histopathol enero de. 2019;74:135–45.
Lavery HJ, Droller MJ. Do Gleason patterns 3 and 4 prostate cancer represent separate disease states?. J Urol. 2012;188:1667–75.
Kovtun IV, Cheville JC, Murphy SJ, Johnson SH, Zarei S, Kosari F, et al. Lineage relationship of Gleason patterns in Gleason score 7 prostate cancer. Cancer Res. 2013;73:3275–84.
Sopyllo K, Erickson AM, Mirtti T. Grading evolution and contemporary prognostic biomarkers of clinically significant prostate cancer. Cancers. 2021;13.
Franiel T, Stephan C, Erbersdobler A, Dietz E, Maxeiner A, Hell N, et al. Areas suspicious for prostate cancer: MR-guided biopsy in patients with at least one transrectal US-guided biopsy with a negative finding-multiparametric MR imaging for detection and biopsy planning. Radiol abril de. 2011;259:162–72.
Hambrock T, Somford DM, Hoeks C, Bouwense SAW, Huisman H, Yakar D, et al. Magnetic resonance imaging guided prostate biopsy in men with repeat negative biopsies and increased prostate specific antigen. J Urol. 2010;183:520–7.
Sciarra A, Panebianco V, Ciccariello M, Salciccia S, Cattarino S, Lisi D, et al. Value of magnetic resonance spectroscopy imaging and dynamic contrast-enhanced imaging for detecting prostate cancer foci in men with prior negative biopsy. Clin Cancer Res J Am Assoc Cancer Res. 2010;16:1875–83.
Polascik TJ, Passoni NM, Villers A, Choyke PL. Modernizing the diagnostic and decision-making pathway for prostate cancer. Clin Cancer Res J Am Assoc Cancer Res. 2014;20:6254–7.
Ahmed HU, El-Shater Bosaily A, Brown LC, Gabe R, Kaplan R, Parmar MK, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet Lond Engl. 2017;389:815–22.
Kasivisvanathan V, Rannikko AS, Borghi M, Panebianco V, Mynderse LA, Vaarala MH, et al. MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis. N Engl J Med. 2018;378:1767–77.
Mottet N, Cornford P, Van Den Bergh RCN, Briers E, De Santis M, Fanti S EAU guidelines on prostate cancer. Update April. 2014.
Mason BR, Eastham JA, Davis BJ, Mynderse LA, Pugh TJ, Lee RJ, et al. Current Status of MRI and PET in the NCCN Guidelines for Prostate Cancer. J Natl Compr Cancer Netw JNCCN. 2019;17:506–13.
De Perrot T, Sadjo Zoua C, Glessgen CG, Botsikas D, Berchtold L, Salomir R, et al. Diffusion-Weighted MRI in the Genitourinary System. J Clin Med.2022;11.
Wibmer AG, Vargas HA, Hricak H. Role of MRI in the diagnosis and management of prostate cancer. Future Oncol Lond Engl. 2015;11:2757–66.
Verma S, Turkbey B, Muradyan N, Rajesh A, Cornud F, Haider MA, et al. Overview of dynamic contrast-enhanced MRI in prostate cancer diagnosis and management. Am J Roentgenol. 2012;198:1277–88.
Weinreb JC, Barentsz JO, Choyke PL, Cornud F, Haider MA, Macura KJ, et al. PI-RADS Prostate Imaging – Reporting and Data System: 2015, Version 2. Eur Urol. 2016;69:16–40.
Faccioli N, Santi E, Foti G, Curti P, D’Onofrio M. Cost-effectiveness analysis of short biparametric magnetic resonance imaging protocol in men at risk of prostate cancer. Arch Ital Urol E Androl. 2022;94:160–5.
Huh JS, Park KK. A Cost-Benefit Comparison of Biparametric Magnetic Resonance Imaging Versus Conventional Prostate Cancer Screening. J Urol Oncol. 2023;21:121–7.
Pockros B, Davenport MS, Stensland K, Sekar R, Morgan T. Prostate Mri Without Contrast: Opportunity To Reduce Financial Toxicity And Improve Access For Patients With Prostate Cancer. Urol Oncol Semin Orig Investig. 2024;42:S96–7.
Porter KK, King A, Galgano SJ, Sherrer RL, Gordetsky JB, Rais-Bahrami S. Financial implications of biparametric prostate MRI. Prostate Cancer Prostatic Dis. 2020;23:88–93.
Fraum TJ, Ludwig DR, Bashir MR, Fowler KJ. Gadolinium-based contrast agents: A comprehensive risk assessment. J Magn Reson Imaging. 2017;46:338–53.
Rudnick MR, Wahba IM, Leonberg-Yoo AK, Miskulin D, Litt HI. Risks and Options With Gadolinium-Based Contrast Agents in Patients With CKD: A Review. Am J Kidney Dis J Natl Kidney Found. 2021;77:517–28.
Bass EJ, Pantovic A, Connor M, Gabe R, Padhani AR, Rockall A, et al. A systematic review and meta-analysis of the diagnostic accuracy of biparametric prostate MRI for prostate cancer in men at risk. Prostate Cancer Prostatic Dis. 2021;24:596–611.
Alabousi M, Salameh JP, Gusenbauer K, Samoilov L, Jafri A, Yu H, et al. Biparametric vs multiparametric prostate magnetic resonance imaging for the detection of prostate cancer in treatment-naïve patients: a diagnostic test accuracy systematic review and meta-analysis. BJU Int. 2019;124:209–20.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.
Zwinderman AH, Glas AS, Bossuyt PM, Florie J, Bipat S, Stoker J. Statistical models for quantifying diagnostic accuracy with multiple lesions per patient. Biostatistics. 2008;9:513–22.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13.
QUADAS-2: A Revised Tool for the Quality Assessment of Diagnostic Accuracy Studies., Annals of Internal Medicine. 2011. Vol. 155 p. 529-36.
Reitsma JB, Glas AS, Rutjes AWS, Scholten RJPM, Bossuyt PM, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol. 2005;58:982–90.
Viechtbauer W. Bias and Efficiency of Meta-Analytic Variance Estimators in the Random-Effects Model. J Educ Behav Stat. 2005;30:261–93.
Holling H, Böhning W, Masoudi E, Böhning D, Sangnawakij P. Evaluation of a new version of I2 with emphasis on diagnostic problems. Commun Stat-Simul Comput. 2020;49:942–72.
Gatsonis C, Paliwal P. Meta-Analysis of Diagnostic and Screening Test Accuracy Evaluations: Methodologic Primer. Am J Roentgenol. 2006;187:271–81.
DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28:105–14.
Ost DE Interpretation and Application of the Likelihood Ratio to Clinical Practice in Thoracic Oncology. J Bronchol Interv Pulmonol [Internet]. 2022;29. Disponible en: https://journals.lww.com/bronchology/fulltext/2022/01000/interpretation_and_application_of_the_likelihood.10.aspx
Glas AS, Lijmer JG, Prins MH, Bonsel GJ, Bossuyt PMM. The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol. 2003;56:1129–35.
Assel M, Sjoberg D, Elders A, Wang X, Huo D, Botchway A, et al. Guidelines for reporting of statistics for clinical research in urology. BJU Int. 2019;123:401–10.
Kattan MW, Vickers AJ. Statistical Analysis and Reporting Guidelines for CHEST. CHEST. 2020;158:S3–11.
Donegan S, Williams L, Dias S, Tudur-Smith C, Welton N. Exploring treatment by covariate interactions using subgroup analysis and meta-regression in cochrane reviews: a review of recent practice. PloS One. 2015;10:e0128804.
Hamza TH, van Houwelingen HC, Heijenbrok-Kal MH, Stijnen T. Associating explanatory variables with summary receiver operating characteristic curves in diagnostic meta-analysis. J Clin Epidemiol. 2009;62:1284–91.
Sánchez-Meca J, Botella J. Moderators analysis in meta-analysis: Meta-regression and subgroups analyzes. Cirugia Espanola. 2024;102:446–7.
Russo F, Mazzetti S, Regge D, Ambrosini I, Giannini V, Manfredi M, et al. Diagnostic accuracy of single-plane biparametric and multiparametric magnetic resonance imaging in prostate cancer: a randomized noninferiority trial in Biopsy-naïve Men. Eur Urol Oncol. 2021;4:855–62.
Thaiss WM, Moser S, Hepp T, Kruck S, Rausch S, Scharpf M, et al. Head-to-head comparison of biparametric versus multiparametric MRI of the prostate before robot-assisted transperineal fusion prostate biopsy. World J Urol. 2022;40:2431–8.
Kuhl CK, Bruhn R, Krämer N, Nebelung S, Heidenreich A, Schrading S. Abbreviated biparametric prostate MR imaging in men with elevated prostate-specific antigen. Radiology. 2017;285:493–505.
Pesapane F, Acquasanta M, Meo RD, Agazzi GM, Tantrige P, Codari M, et al. Comparison of sensitivity and specificity of biparametric versus multiparametric prostate MRI in the detection of prostate cancer in 431 men with elevated prostate-specific antigen levels. Diagnostics. 2021;11.
Brembilla G, Giganti F, Sidhu H, Imbriaco M, Mallett S, Stabile A, et al. Diagnostic accuracy of abbreviated bi-parametric MRI (a-bpMRI) for prostate cancer detection and screening: a multi-reader study. Diagnostics. 2022;12.
Xu L, Zhang G, Shi B, Liu Y, Zou T, Yan W, et al. Comparison of biparametric and multiparametric MRI in the diagnosis of prostate cancer. Cancer Imaging. 2019;19:90.
Zawaideh JP, Sala E, Shaida N, Koo B, Warren AY, Carmisciano L, et al. Diagnostic accuracy of biparametric versus multiparametric prostate MRI: assessment of contrast benefit in clinical practice. Eur Radio. 2020;30:4039–49.
van der Leest M, Israël B, Cornel EB, Zámecnik P, Schoots IG, van der Lelij H, et al. High Diagnostic Performance of Short Magnetic Resonance Imaging Protocols for Prostate Cancer Detection in Biopsy-naïve Men: The Next Step in Magnetic Resonance Imaging Accessibility. Eur Urol. 2019;76:574–81.
Thestrup KCD, Logager V, Baslev I, Møller JM, Hansen RH, Thomsen HS. Biparametric versus multiparametric MRI in the diagnosis of prostate cancer. Acta Radio Open. 2016;5:2058460116663046.
Zhang J, Xu L, Zhang G, Zhang X, Bai X, Ji Z, et al. Comparison between biparametric and multiparametric MRI diagnosis strategy for prostate cancer in the peripheral zone using PI-RADS version 2.1. Abdom Radio. 2022;47:2905–16.
Mahajan M, Gupta V, Gupta P, Sharma P, Abrol D. Evaluation of clinically significant prostate cancer using biparametric magnetic resonance imaging: An evolving concept. J Cancer Res Ther. 2022;18:1640–5.
Tamada T, Kido A, Yamamoto A, Takeuchi M, Miyaji Y, Moriya T, et al. Comparison of biparametric and multiparametric MRI for clinically significant prostate cancer detection with PI-RADS Version 2.1. J Magn Reson Imaging. 2021;53:283–91.
Bao J, Zhi R, Hou Y, Zhang J, Wu CJ, Wang XM, et al. Optimized MRI assessment for clinically significant prostate cancer: A STARD-compliant two-center study. J Magn Reson Imaging. 2021;53:1210–9.
Choi MH, Kim CK, Lee YJ, Jung SE. Prebiopsy biparametric MRI for clinically significant prostate cancer detection with PI-RADS Version 2: A multicenter study. Am J Roentgenol. 2019;212:839–46.
Gatti M, Faletti R, Calleris G, Giglio J, Berzovini C, Gentile F, et al. Prostate cancer detection with biparametric magnetic resonance imaging (bpMRI) by readers with different experience: performance and comparison with multiparametric (mpMRI). Abdom Radio. 2019;44:1883–93.
De Visschere P, Lumen N, Ost P, Decaestecker K, Pattyn E, Villeirs G. Dynamic contrast-enhanced imaging has limited added value over T2-weighted imaging and diffusion-weighted imaging when using PI-RADSv2 for diagnosis of clinically significant prostate cancer in patients with elevated PSA. Clin Radio. 2017;72:23–32.
Barth BK, De Visschere PJL, Cornelius A, Nicolau C, Vargas HA, Eberli D, et al. Detection of clinically significant prostate cancer: short dual–pulse sequence versus standard multiparametric MR Imaging—A multireader study. Radiology. 2017;284:725–36.
Radtke JP, Boxler S, Kuru TH, Wolf MB, Alt CD, Popeneciu IV, et al. Improved detection of anterior fibromuscular stroma and transition zone prostate cancer using biparametric and multiparametric MRI with MRI-targeted biopsy and MRI-US fusion guidance. Prostate Cancer Prostat Dis. 2015;18:288–96.
Van Nieuwenhove S, Saussez TP, Thiry S, Trefois P, Annet L, Michoux N, et al. Prospective comparison of a fast 1.5-T biparametric with the 3.0-T multiparametric ESUR magnetic resonance imaging protocol as a triage test for men at risk of prostate cancer. BJU Int. 2019;123:411–20.
Cuocolo R, Verde F, Ponsiglione A, Romeo V, Petretta M, Imbriaco M, et al. Clinically significant prostate cancer detection with biparametric MRI: A systematic review and meta-analysis. Am J Roentgenol. 2021;216:608–21.
Asif A, Nathan A, Ng A, Khetrapal P, Chan VWS, Giganti F, et al. Comparing biparametric to multiparametric MRI in the diagnosis of clinically significant prostate cancer in biopsy-naive men (PRIME): a prospective, international, multicentre, non-inferiority within-patient, diagnostic yield trial protocol. BMJ Open. 2023;13:e070280.
Wen L, Badgett R,Cornell J.Number needed to treat: A descriptor for weighing therapeutic options.Am J Health Syst Pharm.2005;62:2031–6.
Funding
This study received no specific grant from any funding agency.
Author information
Authors and Affiliations
Contributions
CAGB and CMGG conceived and designed the study. CAGB, VSM, CMGG, and JEJG acquired the data. CAGB and MIAG analyzed and interpreted the data. CAGB, CMGG, JEJG, NGB, MIAG, LFPC, MIRR, and VSM drafted the manuscript. CAGB, CMGG, JEJG, NGB, MIAG, LFPC, MIRR, and VSM critically revised the manuscript for important intellectual content. CAGB and CMGG supervised the study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
This study did not involve the direct participation of human subjects; thus, an informed consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Garcia-Becerra, C.A., Arias-Gallardo, M.I., Juarez-Garcia, J.E. et al. Head-to-head comparison of diagnostic test accuracy between biparametric and multiparametric MRI: an updated systematic review and bivariate meta-analysis. Prostate Cancer Prostatic Dis 28, 993–1004 (2025). https://doi.org/10.1038/s41391-025-00999-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41391-025-00999-0
This article is cited by
-
Comparative diagnostic accuracy of multiparametric-MRI and Micro-ultrasound for clinically significant prostate cancer—a bivariate meta-analysis of prospective studies
Prostate Cancer and Prostatic Diseases (2026)
-
Best of 2025 in prostate cancer and prostatic diseases
Prostate Cancer and Prostatic Diseases (2026)
-
AI-aided diagnostic performance for prostate MRI: systematic review and meta-analysis
Prostate Cancer and Prostatic Diseases (2025)
-
Clarifying the clinical role of biparametric MRI: reflections on diagnostic equivalence and patient-level stratification
Prostate Cancer and Prostatic Diseases (2025)