Abstract
Introduction COVID-19 emergency and associated measures across the UK and Ireland during the first and third waves of the pandemic disrupted mainstream dental services and training across all specialties.
Aims Investigate the effect of COVID-19 pandemic on training, mental health and wellbeing of specialty trainees (STs) in restorative dentistry and associated mono-specialities across the United Kingdom and Ireland.
Materials and methods A cross-sectional survey was conducted exploring experiences of STs in restorative dentistry, prosthodontics, endodontics and periodontics (n = 101) across the United Kingdom and Ireland during the first (March 2020) and third (July 2021) waves of the pandemic. Results were analysed quantitatively and qualitatively.
Results In total, 28 postgraduate trainees responded, yielding a 28% response rate. STs reported perceived impact on their training in March 2020 and July 2021, with some redeployed to urgent dental care duties in this time period. STs reported reduction in speciality-level clinical activities and a negative impact on mental health and wellbeing in both March 2020 and July 2021. A total of 12 STs felt COVID-19 negatively impacted their future careers.
Conclusion The COVID-19 pandemic negatively impacted clinical training and mental health of STs in restorative dentistry and associated mono-specialities across the United Kingdom and Ireland. Increased flexibility and accounting for lost clinical activities could have improved ST morale and wellbeing.
Key points
-
Highlights the immediate and delayed impact of COVID-19 and its associated restrictions on restorative trainees in the UK and Ireland.
-
Provides insights into the wellbeing and thoughts of restorative trainees.
-
Provides suggestions and recommendations for management of speciality trainees in future, similar pandemic situations.
Similar content being viewed by others
Introduction
The COVID-19 pandemic of 2020 resulted in significant disruption to dentistry across the United Kingdom.1 The first wave of the pandemic was estimated to have started in February/March 2020 and ended September 2020. During this wave, the UK moved from the containment phase to the delay phase of the response to COVID-19, with very similar responses occurring in Ireland.2,3,4 During this period, all routine dental care in the UK and Ireland stopped and only those requiring urgent treatment were able to access care, with dental staff being redeployed to other key services to aid the management of the pandemic.5,6 Several urgent dental centre hubs were set up across the UK to carry out aerosol generating procedures (AGPs) where staff had access to appropriate personal protective equipment (PPE). These centres were staffed by dentists ranging from generalists, postgraduate trainees and specialists. Other postgraduate trainees were redeployed to other clinical areas (often non-dental) to help in the response to COVID-19.5,6 The third wave of the pandemic was defined as starting May 2021 and ending in December 2021 and was caused by a surge in the Delta variant.3 During the third wave, due to well-established vaccination programmes and uptake across the UK and Ireland, restrictions were being lifted, resulting in a phased return of dental services to a resumption of full clinical practice.4,7,8
In the UK, postgraduate specialist training pathways within restorative dentistry and its mono-specialities (endodontics/prosthodontics/periodontics) exist based on different funding streams. Those that hold contractual NHS positions of training are called specialty trainees (STs) and those who are self-funded (typically clinical Master's students) are specialist, mono-specialty, self-funded trainees.9
A previous survey conducted across Wales demonstrated that the first wave of the pandemic impacted postgraduate training and self-perceived mental health for both dental core trainees (DCTs) and STs.10 Both cohorts experienced differing proportions of redeployment (DCTs = 44%; STs = 32%) and expressed concern on the negative impact of COVID-19 on their training (DCTs = 84%; STs = 74%), and extreme disruption to clinical and educational activities (DCTs = 92%; STs = 79%).10 Similar issues were also reported by oral surgery STs in the UK, with 74% expressing concern over the impact of COVID-19 on their speciality training, with 59% stating they were either already or were due to be redeployed to other roles.11
However, there is limited evidence in the literature on how training was affected for STs during the first and third waves of the pandemic and it is assumed that during third wave, training would not have been as affected as during the first wave. To the authors' knowledge, there are no surveys that have considered the immediate (first wave) and later (third wave) impact of COVID-19 on postgraduate training of restorative dentistry and mono-speciality trainees in endodontics, prosthodontics and periodontics across the UK and Ireland.
Aims and objectives
To investigate the impact of the COVID-19 pandemic and its associated waves on STs in restorative dentistry and associated mono-specialities, and determine any perceived impact on:
-
Training experiences
-
Trainee mental health and wellbeing
-
Trainees' future careers.
Materials and methods
A cross-sectional study was performed based upon a previously published and peer-reviewed study.10 This consisted of an initial pilot study to determine suitability of the method and questionnaire which was sent to six STs in different specialties across the UK. Feedback and suggestions were collated on all aspects of the proposed method and survey questions. This allowed the finalisation of the method and electronic survey for the main study.
Ethical approval for this study was granted by Cardiff University Dental School Research Ethics Committee (DSREC no. 2033a) and was reviewed by the UK Committee of Postgraduate Dental Deans and Directors (COPDEND) Secretariat. An email was sent to all restorative and mono-speciality trainees in the UK and Ireland via COPDEND and Specialty Registrars in Restorative Dentistry Group distribution lists. This email contained an invitation to participate in the survey, a participant information sheet and a link to the electronic survey. A maximum of two reminder emails were sent one month after beginning the survey.
The online survey consisted of a 20-item questionnaire created using internet-based software (Online Surveys, https://www.onlinesurveys.ac.uk) developed by Bristol University12 and based upon a previously validated questionnaire10. The questions asked were categorised into demographic and redeployment, perceptions of training experience, impact on education, and mental health and wellbeing. For training experiences and impact on education, multiple responses could be given based on clinical roles within redeployment and only single answers for perceptions on mental health and wellbeing.
Eligibility criteria were any ST in restorative dentistry, prosthodontics, periodontics and endodontics that were in post during the first wave (March 2020) and third wave (July 2021) of the COVID-19 pandemic, and training in the UK and/or Ireland.
Consent was obtained in a previously published two-step process requiring participants to read the required participant information and clicking ‘next' and to complete and submit all responses for the questionnaire.10
Non-identifiable information was collected and participant anonymity was maintained throughout the data collection process, and all data analysis was done using descriptive statistics and in aggregate to ensure no traceability to institutions with small ST cohort sizes. Additionally, all free-text responses were analysed using an inductive thematic approach to determine any common themes on an iterative process until no new themes emerged. All participants were provided with up-to-date information on services available for mental health and wellbeing across each Health Education organisation (or equivalent) in the UK and Ireland.
Results
Demographic and redeployment data
In total, 101 postgraduate trainees were invited to participate, with 28 responding, yielding a 28% total response rate: 19 restorative dentistry, three prosthodontic, three periodontic and three endodontic trainees. Figure 1 indicates the age groups, post type and training grade.
a) Age range of specialty trainees that responded. b) Distribution of responses according to post type. c) Distribution of responses according to training year (* = other restorative specialty training grades not otherwise listed, which are out-of-programme and post-completion of specialist training)
Figure 2 indicates the clinical roles for respondents in the first and third waves of the pandemic, with most (n = 28) stating they worked in dental hospital in March 2020 and July 2021 (n = 26). Only ten STs were asked to redeploy at any point between March 2020 (n = 8) and July 2021 (n = 2), with six of eight STs agreeing to take part in March 2020 redeployment and all STs agreeing in July 2021. Figure 3a indicates the roles undertaken during redeployment, with STs stating being redeployed in March 2020 to urgent dental care centres within the same training unit (n = 7) and/or different training unit (n = 3), while in July 2021, STs were redeployed to critical care and/or COVID testing (n = 2) centres.
Figure 3b indicates the tasks STs were undertaking during redeployment. In March 2020, most (n = 8) STs performed either emergency dental care and/or telephone/remote consultations (n = 6). In July 2021, two STs performed ‘other tasks' associated with COVID vaccination and testing, and one performed ventilation tasks on general medical wards.
Perceived impact on specialty training
More STs felt concerned or extremely concerned about the impact of COVID-19 and associated measures in March 2020 (n = 22) than in July 2021 (n = 18). Additionally, with regards to workload change and allocation, a larger proportion (n = 14) of STs in July 2021 reported either a somewhat or significant increase in workload compared to March 2020 (n = 8), while in March 2020, 13 STs reported a somewhat or significant decrease in workload compared to July 2021 (n = 8).
Figure 4a indicates the different ways in which the COVID-19 pandemic negatively affected specialty training. In March 2020, the most commonly reported activities that were affected were: reduction in logbook procedures (n = 21); reduction in patient contact/clinical time (n = 21); cancellation/postponement of courses (n = 20); and inability to complete portfolio work-based assessments (n = 19). While in July 2021, these were: reduction in logbook procedures (n = 18); reduction in patient contact/clinical time (n = 13); cancellation/postponement of courses (n = 10); and cancelled/postponement of study days (n = 9).
Figure 4b indicates how the COVID-19 pandemic positively impacted specialty training. In March 2020, STs indicated an increase in time and opportunities for: clinical governance activities (n = 9); portfolio write-up (n = 9); ‘other' activities, including research time (n = 7); and dealing with stressful situations (n = 7). However, in July 2021, STs stated an increase in opportunities for: research (n = 9); dealing with stressful situations (n = 8); leadership skills (n = 8); and portfolio write-up (n = 6).
Figure 4c indicates the perceived impact of COVID-19 pandemic on future careers, with 12 STs indicating a somewhat or significantly negative impact, and only four indicating a somewhat or significantly positive impact. Box 1 provides insights into how STs described their feelings to expand on the perceived impact on their careers. Inductive thematic analysis revealed two common themes to describe the impact of COVID-19 and its associated measures, which were clinical training exposure and mental health/wellbeing.
Perceived impact on mental health, wellbeing and support
Most STs in March 2020 (n = 15) and July 2021 (n = 16) reported a somewhat or significant negative impact of the COVID-19 pandemic on their mental health and wellbeing, with 22 describing feeling slightly or significantly more stressed in March 2020 compared to 19 in July 2021.
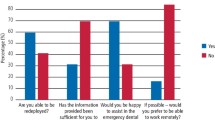
Figure 5a and Figure 5b provide insights into the perception of support provided to STs during both the first and third waves of the pandemic, respectively. In March 2020, the majority of STs felt very well or somewhat supported for appropriate PPE (n = 21) and that they had a safe working environment (n = 19); adequate supervision (n = 17); access to COVID-19 testing (n = 17); correct distribution of workload (n = 17); guidelines on patient management (n = 17); and regular communication and updates (n = 16). In July 2021, STs reported they felt very well or somewhat supported for appropriate PPE (n = 23) and that they had access to COVID-19 testing (n = 22); a safe working environment (n = 19); adequate supervision (n = 17); correct distribution of workload (n = 16); guidelines on patient management (n = 16); and regular communication and updates (n = 15).
Trainee thoughts on preparedness for future pandemics
When asked which actions/activities would have the perceived impact of the pandemic on their training, the most to least common responses were as follows: extending training post (n = 8); increased departmental teaching (n = 7); using study budget the following year (n = 6); increased opportunity for e-learning (n = 5); and ‘other' (n = 3), including better timetabling and option for flexibility in training.
Discussion
The response rate obtained was 28% (n = 28) from 101 eligible STs across UK and Ireland, which is lower than the previous Welsh-based survey (73%) completed by the same research group.10 This is owing to a much larger and organisationally diverse cohort for questionnaire dissemination across the UK and Ireland compared to Wales.
The survey indicated that COVID-19 pandemic and associated measures had both an immediate effect (March 2020) and late effect (July 2021) on speciality training for the restorative and mono-speciality trainees. In March 2020, participants' main issues were concerning clinical contact time (and therefore clinical experience), their increased stress levels and reduced mental health and wellbeing, while in July 2021, this decreased. Additionally, there were differences in redeployment of STs between March 2020 and July 2021, with eight being asked during the first wave compared to only two in the third wave. This in an indicator of the differences in response by the NHS to the first and third pandemic waves, with all non-essential services being cancelled during the first wave and then reinstated to almost full capabilities by the third wave, meaning there were fewer requirements for redeployment of staff in the third wave as compared to the first. Additionally, vaccination rates across the UK and Ireland were significantly higher for all adults by the third wave, which helped significantly lower infection rates, deaths due to COVID-19 and severe infection hospitalisations.3,12 As a result of the national vaccination programme altering the course of the COVID-19 pandemic, NHS policy and strategy evolved to the reduce requirement for redeployment of dentists by the third wave.8
First-wave redeployment rates across the UK and Ireland differed according to geographic region and speciality. In this study of UK and Irish restorative and mono-speciality trainees, 75% of those asked to redeploy took part, while a combined 32% of all Welsh STs took part (oral surgery, oral medicine, orthodontics, oral and maxillofacial surgery [OMFS], dental public health, paediatric dentistry, and special care dentistry),10 and 59% of oral surgery STs across the UK.11 Differences in redeployment rates across the UK reflect differences across different NHS trusts and the relative differences in patient hospital admission rates, which varied across the UK, with England being the most affected compared with Wales, Scotland and Northern Ireland.6 However, there were no studies published which considered third wave pandemic redeployment of dental postgraduate trainees in comparison to the existing study.
For those STs that were redeployed in either first wave, the duties they performed were similar to those reported by other studies of other specialty trainees in other dental specialties, with emergency dental care (n = 8) and remote/telephone-based consultations (n = 6) being most commonly reported in this study, which were similar to reported similar rates of 50% (n = 3) of STs in Wales,10 while for oral surgery STs, this was lower, at 29%, with most (41%) being redeployed to oral and maxillofacial units.11This reflects the skill sets of different specialty trainees with redeployments suited to each trainee - oral surgery STs being mostly deployed to OMFS-related duties and restorative STs to emergency dental duties. In the third wave of the pandemic, most restorative and mono-speciality trainees were redeployed to vaccination-based duties, which is a reflection of the changing demand and need on the whole NHS workforce in this period.
Regarding impact on specialty training, more STs in this study indicated they were concerned or extremely concerned about the impact of COVID on their training in March 2020 (81%) compared with July 2021 (64%). This reduction by the third pandemic wave is likely due to better NHS response to the pandemic by this point, more established services for trainee wellbeing, and better clarity on requirements for redeployment of NHS personnel.6,12
There were similarities between this study and previous studies on the types of activities affected by the pandemic and associated measures taken during the first wave. In this study, STs in March 2020 described the most commonly affected activities were: a reduction in logbook procedures (75%) and patient contact/clinical time (75%); cancellation/postponement of courses (71%); and inability to complete portfolio work-based assessments (68%). This is similar to a previous UK-based study on oral surgery STs during the first wave, which stated the most commonly affected activities were: cancellation or postponement of study days (94%); reduction in logbook procedures (85%); and cancelled or postponed courses (75%).11 This perceived reduction in activities related to ST portfolio and curriculum activities was likely due to STs being asked to perform other ‘non portfolio' or ‘non-curriculum' activities.
When comparing March 2020 with July 2021, we can see a reduction in the perceived impact of COVID-19 on issues reported in the first wave: reduction in logbook procedures (75% versus 64%) and patient contact/clinical time (75% versus 46%), cancellation/postponement of courses (71% versus 36%) and study days (57% versus 32%). This therefore clearly indicates that UK preparedness improved overall as the pandemic progressed, with far more courses being offered either remotely or returning to face-to-face, plus a shift in overall health policy for dentistry, with services returning to normality by the third wave. Additionally, it is unknown (and beyond scope of this study) whether the reduction in clinical logbook procedures and patient contact time in March 2020 and July 2021 had also led to adverse outcomes in their respective review process for clinical training progression, such as the Annual Review of Clinical Progress process for restorative STs.
STs reported a similar impact of COVID on stress levels in March 2020 (54%) and July 2021 (57%), and rates for the first wave were similar for STs in Wales (53%)10 and oral surgery STs in the UK (62%).11 These results were also in agreement with a recent general survey of UK dentists, with 41%13 stating their mental health suffered during the first wave of the pandemic and 82%14 of Welsh dentists reporting increased stress levels during the same period of the pandemic. As a result, it is clear that the first wave had a nation-wide impact on dentists and by the third wave, results of this study indicated similar stress levels, which suggests either a lasting effect of the pandemic, or a possible lack of suitable provision for trainee support or other methods to allow reduction in stress levels.
With regard to restorative and mono-speciality STs' perception of support, it could be seen that most STs felt they were well-supported in key areas during the pandemic. When comparing perception of support between first and third waves, there were no differences reported between safe working environment (68% versus 68%) and adequate supervision (61% versus 61%), indicating consistency in support across UK and Ireland. There was increased perception of support in the third wave for appropriate PPE (75% versus 82%) and access to COVID-19 testing (61% versus 79%), which was likely due to the initial UK-wide shortages in PPE supplies during the first wave, as well as a well-established COVID-19 testing infrastructure by the third wave.3 However, STs reported a reduction in support for distribution of workload (61% versus 57%), guidelines on patient management (61% versus 57%) and regular communication and updates (57% versus 54%) - these reductions were only by one ST response and thus not deemed as significant reductions from first to third wave.
In preparedness for future pandemics, it is important to consider both immediate and late complications of any policies that may impact on trainee clinical activities and their subsequent mental health. STs in this study suggested increasing length of training periods (30%), departmental teaching activities (25%) and financial flexibility (21%) may help alleviate issues associated with stress and anxiety caused by reduction in clinical activity. However, it is important to also consider constraints in budgeting and workforce allocation and planning in future pandemics to determine whether such suggestions can be implemented.
Limitations of the study
The response rate for this survey was lower at 28% (n = 28) compared with a previous survey of STs in Wales at 73% (n = 19). This was due to differences in communication and distribution of the online survey to both cohorts. Only one organisation was required for distribution among Welsh trainees, while input from multiple organisations was required for distribution throughout UK and Ireland.
Given the limited number of restorative and mono-speciality trainees across the UK and Ireland, it was not possible to ask questions related to trainee location, as this would almost certainly compromise the anonymity of responses; as a result, analysis according to geographic location was not possible.
Additionally, while the study was cross-sectional and prospective in nature, it relied on participants to recall past events which could have been subject to recall bias; this is inherent to any study requiring recall of previous events.
Conclusion
STs in restorative dentistry, prosthodontics, periodontics and endodontics expressed multiple issues faced during the first and third waves of the COVID-19 pandemic. They reported a perceived reduction in clinical contact time, logbook training procedures and study day postponement. Trainees also reported high levels of stress during both waves of the pandemic but most indicated they were supported during key times of the pandemic. Trainees suggested that increased flexibility in timetabling and clinical exposure could help alleviate perceived impact on both clinical exposure and mental health.
Data availability
Data can be provided by the corresponding author upon reasonable request.
References
British Dental Association. Updates from week commencing 16 March 2020. 2020.
Office for National Statistics. Coronavirus (COVID-19) Infection Survey technical article: waves and lags of COVID-19 in England, June 2021. 2021. Available at https://www.ons.gov.uk/releases/coronaviruscovid19 infectionsurveytechnicalarticlewavesandlagsofcovid19 inenglandjune2021 (accessed July 2024).
British Medical Association. BMA Covid Review 4 - The public health response by UK governments to COVID-19. 2022. Available at https://www.bma.org.uk/media/5980/bma-covid-review-report-4-28-july-2022.pdf (accessed July 2024).
Kennelly B, Callaghan M O, Coughlan D et al. The COVID-19 pandemic in Ireland: An overview of the health service and economic policy response. Health Policy Technol 2020; 9: 419-429.
NHS. Redeploying the clinical dental workforce to support the NHS clinical delivery plan for COVID-19. Available at https://www.england.nhs.uk/coronavirus/documents/redeploying-the-clinical-dental-workforce-to-support-the-nhs-clinical-delivery-plan-for-covid-19/ (accessed July 2024).
UK Parliament. Effect of covid-19 on dental services. 2021. Available at https://commonslibrary.parliament.uk/research-briefings/cdp-2021-0001/ (accessed July 2024).
Kieran R, Moloney C, Alken S et al. Patient knowledge, personal experience, and impact of the first wave of the COVD-19 pandemic in an Irish oncology cohort. Ir J Med Sci 2023; 192: 533-540.
NHS England. Standard operating procedure. Transition to recovery A phased transition for dental practices towards the resumption of the full range of dental provision. 2020. Available at https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/06/C0575-dental-transition-to-recovery-SOP-4June.pdf (accessed July 2024).
UK Committee of Postgraduate Dental Deans and Directors. A Reference Guide for Postgraduate Dental Core and Specialty Training in the UK. 2021. Available at https://www.copdend.org/wp-content/uploads/2021/10/Dental-Gold-Guide-2021-FINAL.pdf (accessed July 2024).
Mylonas P, Barratt O, Chin J. The COVID-19 effect on training opportunities, mental health and wellbeing of postgraduate trainees in Wales. Faculty Dent J 2021; 13: 17-22.
Aulakh G, Wanis C, Wilson G, Moore R. The impact of COVID-19 on oral surgery training. Oral Surg 2021; 14: 313-320.
Pritchard E, Matthews P C, Stoesser N et al. Impact of vaccination on new SARS-CoV-2 infections in the United Kingdom. Nat Med 2021; 27: 1370-1378.
Collin V, O Selmo E, Whitehead P. Psychological distress and the perceived impact of the COVID-19 pandemic on UK dentists during a national lockdown. Br Dent J 2021; DOI: 10.1038/s41415-020-2592-5.
Owen C, Seddon C, Clarke K, Bysouth T, Johnson D. The impact of the COVID-19 pandemic on the mental health of dentists in Wales. Br Dent J 2022; 232: 44-54.
Funding
This study was jointly funded by Cardiff University and Health Education and Improvement Wales.
Author information
Authors and Affiliations
Contributions
Petros Mylonas led the ethical approval, study design, methodology, data collection, analysis of results and manuscript writing. Olivia Spicer assisted in ethical approval, study design, interpretation of results and review of the final manuscript. Jann Siew Chin assisted in study design, interpretation of results and review of the final manuscript.
Corresponding author
Ethics declarations
The authors declare no conflicts of interests.
This work was presented at the 2023 Spring Meeting of the British Society of Restorative Dentistry.
Ethical approval was sought and provided by Cardiff University Dental School Research Ethics Committee (DSREC no. 2033a) and was reviewed by the UK Committee of Postgraduate Dental Deans and Directors (COPDEND) Secretariat. Consent was obtained in a previously published two-step process requiring participants to read the required participant information and clicking ‘next' and to complete and submit all responses for the questionnaire.
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0.© The Author(s) 2024.
About this article
Cite this article
Mylonas, P., Spicer, O. & Chin, J. A national survey of the impact of the COVID-19 pandemic on training and wellbeing of restorative and mono-speciality specialist trainees in the UK and Ireland. Br Dent J (2024). https://doi.org/10.1038/s41415-024-7679-y
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41415-024-7679-y