Abstract
Background
Radiotherapy increases contralateral breast cancer risk, while hormone therapy reduces it; their combined effects are unclear.
Methods
Data from two US retrospective cohort studies of 5-year breast cancer survivors (stage I-III, ages 20–84), Kaiser Permanente (KP, 1990–2012) and SEER (1990–2013), were analysed. Contralateral breast radiation doses were estimated for the KP cohort. Multivariable Poisson regression estimated relative risks (RRs) and excess relative risks per Gray (ERR/Gy), stratified by hormone therapy use.
Results
KP cohort (n = 9053) included 353 contralateral breast cancer cases (73% ER+); SEER cohort (n = 244,834) included 10,470 cases (72% ER+). Among women with ER+ first breast cancer, radiotherapy increased the risk of ER+ contralateral breast cancer in non-users of hormone therapy (KP RR = 2.2, 95%CI:1.20–4.14; SEER RR = 1.12, 1.04–1.21), but not in users (KP RR = 0.88, 0.61–1.26; SEER RR = 1.03, 0.94–1.12). In KP, higher radiation dose increased risk of ER+ contralateral breast cancer among non-users (ERR/Gy=1.39, 95%CI:0.33,3.66), but not among users (ERR/Gy= –0.13, –0.36,0.23). Radiotherapy also increased risk of ER– contralateral breast cancer (KP RR = 1.85, 95%CI: 0.95–3.59; SEER RR = 1.12, 1.01–1.23), especially in younger exposed women (SEER RR = 1.31, 1.02-1.69 for age <40 vs 40+ years). Additionally, the risk increased linearly with radiation dose to the contralateral breast (ERR/Gy=0.87, 0.04,2.72).
Conclusions
Radiotherapy increased contralateral breast cancer risk, but hormone therapy appeared to mitigate this risk for ER+ cases. These findings have important implications for individuals exposed to chest radiation.
Similar content being viewed by others
Introduction
Radiotherapy is an effective breast cancer treatment that reduces the risk of recurrence and breast cancer mortality [1]. The incidental radiation dose from the radiation treatment can, however, increase the risk of contralateral breast cancer [1,2,3]. Changes in radiotherapy delivery have successfully reduced this incidental dose [4], but given the widespread use of adjuvant radiotherapy, it is estimated that 17% of contralateral breast cancers could be related to incidental radiation exposure [4]. Hormone therapy is a highly effective treatment for ER+ breast cancer that reduces the risk of recurrence, breast cancer mortality, and contralateral breast cancer [5,6,7]. However, the combined effect of radiotherapy and hormone therapy on contralateral breast cancer risk is uncertain.
Most previous studies of radiotherapy and contralateral breast cancer included populations treated before the widespread introduction of hormone therapy [1, 2, 8, 9]. The Kaiser Permanente (KP) Breast Cancer Survivors Study is a cohort of breast cancer survivors diagnosed between 1990 and 2016 in a general community setting [10]. We used detailed treatment data from electronic medical records (EMRs) for hormone therapy, chemotherapy, and radiotherapy to estimate the combined effect of radiotherapy and hormone therapy on contralateral breast cancer. In the KP cohort, we estimated radiation dose to the contralateral breast and its association with contralateral breast cancer risk. This in-depth analysis was complemented with a large-scale population-based analysis in the SEER-9 cancer registries.
Methods
Study design and participants
KP cohort
The study population included 9901 breast cancer survivors diagnosed with unilateral first primary invasive breast cancer between 1990 and 2012 in three KP centres: KP Colorado (01/01/1994–12/31/2010), KP Northwest (01/01/1990–12/31/2005) and KP Washington (01/01/1990–12/31/2012). To account for the minimum latency period for radiation-related solid cancers [11], our study population was restricted to individuals who had survived for at least five years and cancer-free after diagnosis. Eligible subjects were women treated with surgery, with known stage (I-III), diagnosed age 20–84 years, and known radiotherapy and hormone therapy receipt. We excluded women who received prophylactic removal of the contralateral breast at initial surgery (Fig. 1). Our analytical population included 9053 five-year breast cancer survivors. Follow-up started five years after breast cancer diagnosis and continued until the earliest occurrence of an outcome event or one of the following censoring events: death, diagnosis of a second primary cancer diagnosis, KP disenrollment, or end of study (12/31/2015 for KP Colorado; 12/31/2017 for KP Washington; 12/31/2010 for KP Northwest).
The KP cohort study was approved by the Institutional Review Boards of each participating institution and the National Institutes of Health. A waiver of written informed consent was granted for the cohort creation based on the minimal risk of this electronic linkage-based research.
SEER cohort
We identified a population-based cohort of 289,394 women diagnosed with a unilateral first primary invasive breast cancer who survived and were cancer-free at least 5 years after diagnosis using the SEER-9 cancer registries from 1990–2013 [12]. We similarly restricted the SEER cohort to women treated with surgery, had a known stage (I-III), diagnosed at age 20–84 years, and excluded those who had removal of the contralateral breast at initial surgery. We also excluded patients for whom radiotherapy or hormone therapy was recommended, but unknown if administered, as well as patients with unknown information on hormone therapy, leaving 244,834 five-year breast cancer survivors (Supplementary Fig. 1). Follow-up started 5 years after breast cancer diagnosis until the earliest occurrence of an outcome event, second primary cancer diagnosis, death, last follow-up, or end of study (12/31/2018).
Procedures
Data collection
For the KP cohort, we extracted data from EMRs, administrative billing and pharmacy dispensing records to ascertain patients’ demographic characteristics and initial breast cancer treatment (surgery type, radiotherapy, chemotherapy and hormone therapy). Patients were linked to local tumour registries or SEER Seattle-Puget-Sound (for KP Washington) to obtain tumour characteristics for the first primary breast cancer and all subsequent cancers. Vital status, date and cause of death were determined from the tumour registries and EMRs with additional linkage to the National Death Index for individuals with unknown cause of death (for KP Colorado).
Radiotherapy information in both the KP and SEER cohorts was ascertained from tumour registries and defined as any radiotherapy given as part of the initial breast cancer treatment. In SEER, hormone therapy was defined as any hormone therapy given as initial treatment or within one year of diagnosis. For KP, we included any hormone therapy prescription given from the date of diagnosis to the end of the study. Among ER+ patients who received hormone therapy, 94% started treatment within one year of diagnosis.
Radiation dosimetry in the KP cohort
We collected radiation summaries for all patients who received radiotherapy in the KP cohort. Digital copies were sent to the MD Anderson Late Effects Group, where a certified medical dosimetrist with expertise in late effects extracted treatment parameters for each radiotherapy field (e.g., machine, energy, treatment field types, wedge use and angles, delivered tumour dose and etc.). Individual contralateral breast dose reconstruction was performed for a subset of exposed subjects (N = 2442, 25%) as described elsewhere [13]. Briefly, contralateral breast doses were determined using a combination of radiation parameters and prior physical measurements [14] of absorbed dose in anthropomorphic phantoms. The average dose received by five subregions of the contralateral breast was estimated: nipple, upper inner quadrant (UIQ), lower inner quadrant (LIQ), upper outer quadrant (UOQ), and lower outer quadrant (LOQ).
For the current study, we estimated contralateral breast doses for all exposed subjects in the cohort by training a customised deep neural network using the previously reconstructed field-specific doses as ground truth and the corresponding abstracted radiotherapy parameters as input features. Based on prior research [15,16,17,18], our neural network consisted of 5 dense layers, each with a rectified linear unit activation function, and a dropout rate of 0.2. We used 60% of the data for training and 40% for held-out testing and a mean square dose error loss function. The model predicted dose to the five breast subregions from each radiotherapy field, enabling rapid dose estimation for the entire cohort without the need for manual, measurement-based reconstruction. On the held-out testing set, the coefficient of determination (R²) between the previously reconstructed doses and the predicted doses for each radiotherapy field was 0.98.
Total individual dose was obtained by summing contributions from all radiotherapy fields received by each patient. The mean dose to the whole contralateral breast was then calculated by averaging the doses to the five subregions. In 95% of patients with previously reconstructed doses, the predicted mean dose to the whole contralateral breast differed by less than 20 cGy. On average, the artificial intelligence method slightly overestimated the dose by 6 cGy (standard deviation 8 cGy) compared to the MD Anderson reconstruction, with a mean absolute difference of 8 cGy. Doses could not be estimated for 15% of the exposed patients (28 cases and 933 non-cases) due to either a missing radiation summary or incomplete information on radiation parameters.
Outcomes
The outcome of interest was a second primary cancer in the contralateral breast (including any invasive or in situ breast cancer) developed at least five years after the first breast cancer diagnosis until the end of follow-up.
Statistical analysis
KP and SEER cohort studies
We estimated relative risk (RR) and 95% confidence Intervals (CIs) for contralateral breast cancer according to patient characteristics and radiotherapy and hormone therapy receipt using multivariable Poisson regression analysis. We used the expected number of breast cancers as an offset to indirectly adjust for attained age and attained calendar year [19]. The expected number of cases was estimated by multiplying the SEER-9 incidence rates of first breast cancer in the female population by the corresponding age, race, and period-specific person-years.
For the KP cohort, multivariable models were adjusted for age (20–39, 40–54, 55–69, 70–84) and year of diagnosis (1990–1997, 1998–2005, 2006–2012), radiotherapy (no/yes), chemotherapy (no/yes), and hormone therapy (no/yes) receipt and KP study centre (KP Colorado, KP Northwest and KP Washington). The SEER models were adjusted for age (20–39, 40–54, 55–69, 70–84) and diagnosis year (1990–1997, 1998–2005, 2006–2013), radiotherapy (no/unknown vs yes), chemotherapy (no/unknown vs yes), and hormone therapy (no/unknown vs yes). We additionally adjusted the SEER models for grade (1, 2, 3, 4, unknown) and tumour size (<1 cm, 1-<2 cm, 2-<5 cm, 5+ cm, and unknown) of the first breast cancer since these factors were also associated with contralateral breast cancer risk in SEER and could be an indication of misclassification of metastases as contralateral breast cancer in SEER. Adjustment factors were selected based on clinical importance or association with contralateral breast cancer risk in the multivariable analysis (p < 0.05).
In both cohorts, we evaluated the relationship of hormone therapy with radiotherapy restricted to patients who had an ER+ first breast cancer, i.e., eligible to receive hormone therapy. We estimated the risk of contralateral breast cancer after radiotherapy, stratified by whether patients received and did not receive hormone therapy, and reported the p-value for the heterogeneity of RR between the two subgroups (p-difference).
For the KP cohort, we also used multivariable Poisson regression to estimate relative risk and 95% CIs for contralateral breast cancer in relation to categories of mean radiation dose to the contralateral breast. Using dose as a continuous variable, we fit a regression model to evaluate whether there was a statistically significant linear association (p-trend <0.05) between the radiation dose and the occurrence of contralateral breast cancer. We also evaluated the radiation dose-response by hormone therapy receipt for each outcome and reported the p-value for heterogeneity of the ERR/Gy. Specifically, we used a linear model where the excess RR (ERR) = βD, in which the ERR is the RR minus 1, D is the equal dose, and β is the regression coefficient. Likelihood ratio-based tests and CIs were reported to assess the statistical significance and precision of our estimates.
P-values for heterogeneity of relative risks were estimated using nested likelihood ratio tests. All tests were 2-sided with statistical significance set at p < 0.05. Data were analysed using SEER*Stat 8.4.3, and DATAB, AMFIT and PECAN modules of Epicure (Hirosoft Corporation).
Results
KP cohort
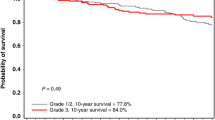
There were 9053 five-year breast cancer survivors in the KP cohort. After a mean follow-up of 6 years (range: 0.1–22 years), 353 women developed contralateral breast cancer (259 ER+, 73%) (Table 1). Overall, about 70% of the cohort received radiotherapy, 66% had breast-conserving surgery, 38% received chemotherapy, and 83% of the women with ER+ breast cancer received hormone therapy.
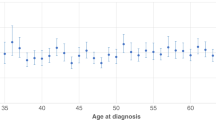
Age at first breast cancer diagnosis was inversely associated with contralateral breast cancer risk (RR = 0.24, 95%CI: 0.14–0.41 for age 70+ vs age <40, p-trend<0.001). Overall, there was no relationship between ER-status, stage, grade, or tumour size of the first breast cancer and risk of contralateral breast cancer (Supplementary Table 1). Similar patterns were observed for ER+ and ER- contralateral breast cancer. Receipt of radiotherapy increased with year of diagnosis and stage at diagnosis, was more common after breast-conserving surgery than mastectomy, and was slightly more common with chemotherapy (Supplementary Table 2).
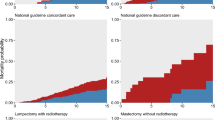
Overall, the relative risk of developing contralateral breast cancer was 1.07 (95%CI: 0.85–1.35) after radiotherapy; we observed a significantly decreased risk after hormone therapy (RR = 0.63, 95%CI:0.50–0.78) (Table 2). Radiotherapy receipt patterns were similar among those that did and did not receive hormone therapy (Supplementary Table 3). In those that did not receive hormone therapy, the risk of contralateral breast cancer after radiotherapy was 1.57 (95%CI:0.94–2.62), whereas there was no elevated risk of contralateral breast cancer after radiotherapy in those that also received hormone therapy (RR = 0.94, 95%CI: 0.69–1.29, p-difference = 0.09) (Table 2). For the risk of developing an ER+ contralateral breast cancer, these differences were even more marked and statistically significant; the RR for radiotherapy was 2.22 (95%CI:1.20–4.14) without hormone therapy and 0.88 (95%CI:0.61–1.26) with hormone therapy (p-difference = 0.01). The risk of ER- contralateral breast cancer was increased after radiotherapy (RR = 1.85, 95%CI:0.95–3.59).
Among patients treated with radiotherapy, most were treated with tangential fields with a prescribed dose of 45-50 Gy delivered in fractions of 1.8-2 Gy to the breast or chest wall (Supplementary Table 4). Approximately 16% received additional fields, including supraclavicular and internal mammary node irradiation. Very few patients received hypo-fractionated radiotherapy (6%) or partial breast radiotherapy (<1%). The estimated dose to the contralateral breast was highest for the UIQ (mean = 1.55 Gy, range: 0.02–3.11) and lowest for the LOQ (mean = 0.60 Gy, range: 0.008–1.23). The mean average dose to the whole contralateral breast was 1.02 Gy (range: 0.015–2.08 Gy). Patients who received higher radiation doses are more likely to have been diagnosed at a younger age and higher stage, undergone mastectomy, and been treated in earlier years, and no difference with respect to hormone therapy receipt (Supplementary Table 5).
Overall, there was a statistically significant increase in ER- contralateral breast cancer risk with increasing radiation dose to the contralateral breast (ERR/Gy = 0.87, 95%CI: 0.04,2.72, p-trend = 0.033) (Table 3). A significant radiation dose-response (ERR/Gy = 1.37, 95% CI: 0.05, 5.85, p-trend = 0.036) was also observed among ER+ first breast cancer patients who received hormone therapy. However, the number of ER- cases among ER+ first breast cancer patients who did not receive hormone therapy was too small to yield meaningful results (n = 7). Among ER+ first breast cancer patients that received hormone therapy, the relative risk of developing an ER+ contralateral breast cancer associated with 1+ Gy versus 0 Gy was 0.97 (95%CI: 0.65–1.44) with no significant dose-response (ERR/Gy = -0.13, 95%CI:−0.36, 0.23, p-trend = 0.42). In contrast, among those who did not receive hormone therapy, the relative risk was 2.74 (95%CI:1.39–5.40) and significantly associated with radiation dose (ERR/Gy of 1.39 (95%CI:0.33–3.66, p-trend = 0.003). There was a significant heterogeneity of the ERR/Gy between ER+ first breast cancer patients who received and did not receive hormone therapy (p-difference = 0.006).
SEER cohort
In the SEER cohort of 244,834 five-year breast cancer survivors, 10,470 developed a contralateral breast cancer (72% ER+) after a mean follow-up of 8 years (range 0.1–23 years) (Supplementary Table 6). A slightly lower proportion of patients underwent breast-conserving surgery (61%) than in the KP cohort (66%). Initial radiotherapy was 58% versus 70% in the KP cohort; a slightly lower proportion was classified as receiving initial chemotherapy (36% vs 38%), and a much lower proportion was classified as receiving hormone therapy (ER+ patients: 57% vs 83%).
The risk of contralateral breast cancer decreased with age and year of first breast cancer diagnosis (RR = 0.47, 95%CI:0.43–0.51 for 70+ vs <40 years, p < 0.001) (Supplementary Table 7). There was no association with stage of first breast cancer, but the risk was higher when the first breast cancer was ER- (compared to ER + ) (RR = 1.12, 95%CI:1.07–1.19). The risk for ER- contralateral breast cancer was increased after a first breast cancer of higher grade (p < 0.001) and larger tumour size (p < 0.029).
Overall, there was a small but statistically significantly increased risk of contralateral breast cancer after radiotherapy (yes vs no/unknown) (RR = 1.07, 95%CI: 1.03–1.12), and a decreased risk after hormone therapy (yes vs no/unknown) (RR = 0.92, 95%CI: 0.88–0.96) (Table 4). Among ER+ first breast cancer patients who did not receive hormone therapy, the risk of contralateral breast cancer after radiotherapy was 1.09 (95%CI:1.02–1.17) compared to 1.03 (95%CI:0.95–1.11) for those who received hormone therapy (p-difference=0.028). The risk of ER+ contralateral breast cancer after radiotherapy was 1.12 (95%CI:1.04–1.21) among those who did not receive hormone therapy vs 1.03 (95%CI:0.94–1.12) among those who did receive hormone therapy (p-difference = 0.16). For ER- contralateral breast cancer, the risk after radiotherapy was 1.12 (95%CI:1.01–1.23). The risk of contralateral breast cancer after radiotherapy was highest for the youngest women; among ER+ first breast cancer patients aged 20–39 years at diagnosis who did not receive hormone therapy the risk of ER+ contralateral breast cancer after radiotherapy was 1.37 (95%CI:0.97–1.95) and the overall risk of ER- contralateral breast cancer after radiotherapy was 1.31 (95% CI: 1.02–1.69) for the youngest women (Supplementary Table 8).
Patterns of receipt of radiotherapy by patient and tumour characteristics and among those who did and did not receive hormone therapy were broadly similar to the KP cohort (Supplementary Tables 9 and 10).
Discussion
We studied the risk of contralateral breast cancer after radiotherapy stratified by hormone therapy receipt in two US cohorts of breast cancer patients treated since the 1990s who survived at least 5 years. In the KP cohort, women with ER+ first breast cancer who did not receive hormone therapy had a significantly increased risk of ER+ contralateral breast cancer after radiotherapy (RR = 2.22), and the risk increased linearly with radiation dose to the contralateral breast. Nevertheless, there was no evidence of elevated risk associated with radiotherapy receipt and radiation dose among women who also received hormone therapy. The risk of ER- contralateral breast cancer was also increased after radiotherapy with a significant radiation dose-response. The patterns of risk estimates of radiotherapy stratified by hormone therapy were broadly consistent and statistically significant, although attenuated, in the larger general population analysis using the SEER cancer registries. The risk of radiation-related contralateral breast cancer was highest for women <age 40 at first breast cancer diagnosis.
Our study treatment period from 1990 to 2012 captured important changes, including the reduction of the incidental radiation dose to the contralateral breast [4], and the widespread introduction of hormone therapy. As far as we are aware, no other studies have reported findings for the risk of contralateral breast cancer associated with radiotherapy stratified by hormone therapy receipt. In the pooled analysis of randomised trials of radiotherapy and breast conserving-surgery the Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) reported a significantly increased risk of contralateral breast cancer in women treated with radiotherapy (RR = 1.18, p = 0.002) with an excess cumulative risk of 1.8% by 15 years [5]. The risk after radiotherapy on those not treated with systemic therapy (chemotherapy or tamoxifen) was still increased (RR = 1.21, p = 0.01), but results were not presented for tamoxifen only. These trials were predominantly conducted in the 1970s and early 1980s using old radiotherapy regimens. In a large Dutch cohort of women treated between 1989 and 2002 [20], radiotherapy was not associated with an increased risk of contralateral breast cancer (RR = 1.04, 95%CI: 0.88–1.24). The authors noted that this could be because a large proportion of patients aged <45 years received hormone therapy (56%), but they did not present any results stratified by hormone therapy receipt. In the Dutch cohort analysis of women diagnosed from 2003–2010 [21], there was also no overall contralateral breast cancer risk associated with radiotherapy (RR = 0.94, 95%CI: 0.86–1.02). Still, results were not presented according to receipt of hormone therapy. A recent pooled analysis of BRCA mutation carriers found an increased risk of contralateral breast cancer after radiotherapy (RR = 1.44, 95%CI:1.12–1.86) [22]. The authors stated that there was no evidence of statistically significant interaction with hormone therapy, but also did not present risk estimates stratified by hormone therapy receipt, so we could not compare our findings. Additionally, a higher percentage of their study population was ER- (35%), and there was no analysis by contralateral breast cancer subtype.
There have been a few studies of radiotherapy and contralateral breast cancer that had detailed dosimetry to evaluate dose-response, but these studies were primarily conducted in earlier treatment periods and in younger women [2, 8, 9, 23, 24]. The WECARE case-control study [2] included women diagnosed between 1985-1999 and treated before age 55. The estimated mean dose was 1.1 Gy (range: 0.02-6.2 Gy) to the contralateral breast tumour location, and the OR for contralateral breast cancer was 2.5 for women diagnosed before age 40 who received >1 Gy compared to the non-exposed women. Our estimated radiation dose-response of an ERR/Gy of 0.87 for ER- contralateral breast cancer and 1.39 for ER+ contralateral breast cancer (among ER+ first breast cancer without hormone therapy) was similar in magnitude to their estimate of ERR/Gy of 1.0 (95%CI: 0.1–3.0). As the WECARE study focused on younger women, they included a larger proportion of ER- breast cancers (23%), and only 34% of their population received hormone therapy; they did not evaluate the radiation dose-response in relation to receipt of hormone therapy. In a Dutch cohort of women treated from 1970 to 1986, radiation doses were estimated for women treated before age 45. The authors reported a larger estimated dose for women treated with internal mammary chain fields [9]. We also found that the risk of radiation-related breast cancer was highest in the youngest women (age <40 at diagnosis) in the SEER cohort. Due to the smaller sample size in the KP cohort, we were unpowered to evaluate the age effect on the radiation risk. Other previous studies by Boice et al. (1992) [8], Storm et al. (1992) [24] and Basco et al. (1985) [23] included women of all ages diagnosed between 1935 and 1982 who were mostly treated with mastectomy rather than breast-conserving surgery and conducted prior to the widespread introduction of hormone therapy.
The role of endogenous oestrogens in the risk of radiation-related breast cancer is supported by the finding in other studies that radiation-related breast cancer risk is reduced in childhood cancer [25] and Hodgkin lymphoma survivors [26] who also received ovarian irradiation. A Phase-II clinical trial evaluated low-dose tamoxifen after chest irradiation in childhood cancer survivors and demonstrated reductions in breast density, which is a biomarker for breast cancer risk [27]. Further work on the potential for prevention of radiation-related ER+ breast cancer by hormone therapies is warranted.
Current US guidelines [28, 29] advise using hormone therapy for prevention in women at high risk of breast cancer. However, they do not extend this recommendation to women who have undergone chest irradiation, due to a lack of sufficient evidence. Our findings provide the first direct evidence that hormone therapy could be used to prevent radiation-related breast cancer.
The strengths of our two cohorts are complementary with detailed treatment data in the KP cohort and the large sample size and general population in SEER. Both also have long-term follow-up, which is required for studying radiation-related breast cancers that are known to take 5-10 years to develop. Assessment of the contralateral breast cancer by subtype enabled us to test the specificity of the risk after hormone therapy, and we adjusted for underlying trends in subtype-specific breast cancer rates using the general population rates as an offset in the Poisson regression model. Detailed treatment data for the KP cohort included radiotherapy summaries, which enabled us to evaluate the treatment techniques and estimate radiation doses to the contralateral breast. The results of the two studies were qualitatively similar, but the risk estimates were lower in SEER. It is well known that there is under-reporting of treatment in SEER, particularly for hormone therapy [30], which likely partly explains the lower risk estimates in SEER compared to the KP cohort, as non-differential misclassification usually biases risk estimates toward the null. It is also possible that there was misclassification of metastases as contralateral breast cancer [31], which could differ according to treatment and could bias results toward or away from the null. This could explain the association between contralateral breast cancer risk and tumour size and grade in SEER, which we included as adjustment factors. Also, as our data only includes the initial breast cancer treatment, we did not account for prophylactic mastectomy during follow-up. While some women may opt for this procedure later, this likely represents a small proportion, as prophylactic mastectomy at the time of initial surgery is often preferred for its single surgical event and recovery period. These limitations in conjunction with the smaller sample size in KP and wide confidence intervals, leave uncertainty about the magnitude of the risks. Overlap existed between the KP and SEER cohorts: 3692 (1.5%) patients from the KPWA cohort are included in the SEER cohort (N = 244,834). This overlap will therefore have a negligible impact on our results. We restricted our analysis to five-year survivors, resulting in the inclusion of only patients diagnosed up until 2013. This meant we had relatively few patients who received hypo-fractionated or partial-breast irradiation. The impact of these more recent changes in radiotherapy practice as well as the effect of the type of hormone therapy on radiation risk,warrants further investigation.
In summary, we observed an increased risk of ER- contralateral breast cancer after radiotherapy as well as an increased risk of ER+ contralateral breast cancer after radiotherapy in women who did not receive hormone therapy, with a significant radiation dose-response and higher radiation-related risk at younger ages. However, there was no associated risk of ER+ contralateral breast cancer from the incidental radiation dose in women who also received hormone therapy. This novel finding of potential prevention of radiation-related ER+ breast cancer by hormone therapy could have important clinical and public health implications, especially for individuals exposed to chest radiation for medical purposes (such as childhood cancer or Hodgkin lymphoma survivors).
Data availability
Data from this study, including individual participant data, are not available for sharing. Summary statistical data will be available from the corresponding author upon reasonable request, with the permission of the contributing Kaiser centres.
References
Clarke M, Collins R, Darby S, Davies C, Elphinstone P, Evans V, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;366:2087–106.
Stovall M, Smith SA, Langholz BM, Boice JD Jr, Shore RE, Andersson M, et al. Dose to the contralateral breast from radiotherapy and risk of second primary breast cancer in the WECARE study. Int J Radiat Oncol Biol Phys. 2008;72:1021–30.
Giannakeas V, Lim DW, Narod SA. The risk of contralateral breast cancer: a SEER-based analysis. Br J Cancer. 2021;125:601–10.
Watt GP, Smith SA, Howell RM, Perez-Andujar A, Reiner AS, Cervino L, et al. Trends in radiation dose to the contralateral breast during breast cancer radiation therapy. Radiat Res. 2023;200:331–9.
Early Breast Cancer Trialists’ Collaborative G. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365:1687–717.
Gierach GL, Curtis RE, Pfeiffer RM, Mullooly M, Ntowe EA, Hoover RN, et al. Association of Adjuvant Tamoxifen and Aromatase inhibitor therapy with contralateral breast cancer risk among US women with breast cancer in a general community setting. JAMA Oncol. 2017;3:186–93.
Pan H, Gray R, Braybrooke J, Davies C, Taylor C, McGale P, et al. 20-year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years. N Engl J Med. 2017;377:1836–46.
Boice JD Jr., Harvey EB, Blettner M, Stovall M, Flannery JT. Cancer in the contralateral breast after radiotherapy for breast cancer. N Engl J Med. 1992;326:781–5.
Hooning MJ, Aleman BM, Hauptmann M, Baaijens MH, Klijn JG, Noyon R, et al. Roles of radiotherapy and chemotherapy in the development of contralateral breast cancer. J Clin Oncol. 2008;26:5561–8.
Ramin C, Veiga LHS, Vo JB, Curtis RE, Bodelon C, Aiello Bowles EJ, et al. Risk of second primary cancer among women in the Kaiser Permanente Breast Cancer Survivors Cohort. Breast Cancer Res. 2023;25:50.
United Nations Scientific Committee on the Effects of Atomic Radiation 2000 Report to the General Assembly, with Annexes Ionizing radiation: Sources and Biological Effects. New York: United Nations; 2000.
National Cancer Institute. SEER*Stat Database: Incidence - SEER Research Plus Data with Additional Fields and Case Listing, 9 Registries, Nov 2020 Sub (1975–2018) released April 2021, based on the November 2020 submission. Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) (accessed Nov 30, 2023).
Lee C, Borrego D, Veiga LHS, Smith SA, Howell RM, Curtis RE, et al. Trends in dose to the contralateral breast from breast cancer radiotherapy in the United States. Radiat Res. 2025. https://doi.org/10.1667/rade-25-00069.1. Online ahead of print.
Bernstein JL, Langholz B, Haile RW, Bernstein L, Thomas DC, Stovall M, et al. Study design: evaluating gene-environment interactions in the etiology of breast cancer - the WECARE study. Breast Cancer Res. 2004;6:R199–214.
Ahn SH, Kim E, Kim C, Cheon W, Kim M, Lee SB, et al. Deep learning method for prediction of patient-specific dose distribution in breast cancer. Radiat Oncol. 2021;16:154.
Hou Z, Qin L, Gu J, Liu Z, Liu J, Zhang Y, et al. Deep learning-powered radiotherapy dose prediction: clinical insights from 622 patients across multiple sites tumor at a single institution. Radiat Oncol. 2025;20:80.
Liu J, Zhang X, Cheng X, Sun L. A deep learning-based dose prediction method for evaluation of radiotherapy treatment planning. J Radiat Res Appl Sci. 2024;17:100757–66.
Kui X, Liu F, Yang M, Wang H, Liu C, Huang D, et al. A review of dose prediction methods for tumor radiation therapy. Meta-Radiol. 2024;2:100057–79.
Yasui Y, Liu Y, Neglia JP, Friedman DL, Bhatia S, Meadows AT, et al. A methodological issue in the analysis of second-primary cancer incidence in long-term survivors of childhood cancers. Am J Epidemiol. 2003;158:1108–13.
Schaapveld M, Visser O, Louwman WJ, Willemse PH, de Vries EG, van der Graaf WT, et al. The impact of adjuvant therapy on contralateral breast cancer risk and the prognostic significance of contralateral breast cancer: a population based study in the Netherlands. Breast Cancer Res Treat. 2008;110:189–97.
Kramer I, Schaapveld M, Oldenburg HSA, Sonke GS, McCool D, van Leeuwen FE, et al. The influence of adjuvant systemic regimens on contralateral breast cancer risk and receptor subtype. J Natl Cancer Inst. 2019;111:709–18.
van Barele M, Akdeniz D, Heemskerk-Gerritsen BAM, Genepso, Andrieu N, Nogues C, et al. Contralateral breast cancer risk in patients with breast cancer and a germline-BRCA1/2 pathogenic variant undergoing radiation. J Natl Cancer Inst. 2023;115:1318–28.
Basco VE, Coldman AJ, Elwood JM, Young ME. Radiation dose and second breast cancer. Br J Cancer. 1985;52:319–25.
Storm HH, Andersson M, Boice JD Jr, Blettner M, Stovall M, Mouridsen HT, et al. Adjuvant radiotherapy and risk of contralateral breast cancer. J Natl Cancer Inst. 1992;84:1245–50.
Veiga LH, Curtis RE, Morton LM, Withrow DR, Howell RM, Smith SA, et al. Association of breast cancer risk after childhood cancer with radiation dose to the breast and anthracycline use: a report from the childhood cancer survivor study. JAMA Pediatr. 2019;173:1171–9.
Krul IM, Opstal-van WindenAWJ, Aleman BMP, Janus CPM, van Eggermond AM, De Bruin ML, et al. Breast cancer risk after radiation therapy for Hodgkin lymphoma: influence of gonadal hormone exposure. Int J Radiat Oncol Biol Phys. 2017;99:843–53.
Bhatia S, Palomares MR, Hageman L, Chen Y, Landier W, Smith K, et al. A randomized Phase IIb study of Low-dose Tamoxifen in chest-irradiated cancer survivors at risk for breast cancer. Clin Cancer Res. 2021;27:967–74.
Force USPST, Owens DK, Davidson KW, Krist AH, Barry MJ, Cabana M, et al. Medication use to reduce risk of breast cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;322:857–67.
Visvanathan K, Fabian CJ, Bantug E, Brewster AM, Davidson NE, DeCensi A, et al. Use of endocrine therapy for breast cancer risk reduction: ASCO Clinical Practice Guideline Update. J Clin Oncol. 2019;37:3152–65.
Haas CB, Bowles EJA, Lee JM, Specht J, Buist DSM. Accuracy of tumor registry versus pharmacy dispensings for breast cancer adjuvant endocrine therapy. Cancer Causes Control. 2022;33:1145–53.
Begg CB, Ostrovnaya I, Geyer FC, Papanastasiou AD, Ng CKY, Sakr RA, et al. Contralateral breast cancers: Independent cancers or metastases? Int J Cancer. 2018;142:347–56.
Acknowledgements
The training and testing of the deep learning dosimetry method were performed using the computational resources of the NIH Biowulf high-performance computing cluster (https://hpc.nih.gov).
Funding
This work was supported by the Intramural Research Programme of the Division of Cancer Epidemiology and Genetics of the US National Cancer Institute (NCI), National Institute of Health. Authors employed by NIH include LHSV, JBV, REC, MMM, MS, CL, CR, CB, GLG, and ABG. Data collected at Kaiser Permanente Colorado was supported by contracts from NCI (HHSN 261201800469P, HHSN 261201700708P, HHSN 261201600711P) and a subcontract with RTI International (HHSN 26120090017C). Data collected at Kaiser Permanente Washington was supported by NCI grants (1R01CA1205621 and P01CA154292) and NCI contracts (HHSN 261201700564P, HHSN 75N91019P00076, HHSN 5N91020P00327). Data collected at Kaiser Permanente Northwest was supported by NCI subcontracts with RTI International (Nos. 20-312-0212208, 17-312-0212208). EJAB was also supported by an NCI grant (R50CA211115). Cancer incidence data used in this study were supported by the Cancer Surveillance System of the Fred Hutchinson Cancer Research Centre, which is funded by Contract No. N01-CN-67009 and N01-PC-35142 from the Surveillance, Epidemiology and End Results (SEER) Programme of the National Cancer Institute, with additional support from the Fred Hutchinson Cancer Research Centre and the State of Washington. The contributions of the NIH author(s) were made as part of their official duties as NIH federal employees, are in compliance with agency policy requirements, and are considered Works of the United States Government. However, the findings and conclusions presented in this paper are those of the author(s) and do not necessarily reflect the views of the NIH or the U.S. Department of Health and Human Services. Open access funding provided by the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
LHSV and ABDG conceived and designed the study. LHSV, GLG, SAS, RMH, MMM, MS, REC, CR, CB, HSF, EJAB, DSMB, SW, JBV, CL, and ABDG were involved in the acquisition, analysis, and interpretation of the data. LHSV and ABDG conducted the statistical analysis. SAS, RMH, MMM, MS and CL conducted the dosimetry. LHSV and ABDG drafted the manuscript. REC, LHSV, DSMB, EJAB, HSF, SW, JBV, ABDG and GLG gave administrative and technical support. LHSV and ABDG verified the data and take responsibility for the integrity and accuracy of the data analysis. All authors had access to all data reported in this study, revised the manuscript for intellectual content and approved the final version for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the National Institutes of Health Institutional Review Board (IRB) and the IRBs of KP Northwest, Colorado, and Washington. Informed consent was waived because KP health plan members had previously consented to the use of their data for linkage-based research through their enrolment. Additionally, the study posed minimal risk and could not have been conducted practicably without the waiver. All procedures adhered to the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Veiga, L.H.S., Gierach, G.L., Smith, S.A. et al. Contralateral breast cancer after radiotherapy and hormone therapy in two cohorts of US breast cancer survivors. Br J Cancer 134, 269–278 (2026). https://doi.org/10.1038/s41416-025-03240-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41416-025-03240-w