Abstract
Background
The prevalence of iron deficiency in the Lebanese pediatric population is unknown. The aim of this study is to estimate this prevalence in Lebanese schoolchildren and to assess the relation between iron status and related factors.
Subjects/methods
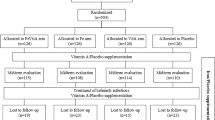
A total of 903 children aged 8–18 years (466 boys and 437 girls) were included in the study. Recruitment was done from ten schools with different SES levels and located in the Great Beirut and Mount Lebanon areas. Serum ferritin was measured in all participants and testosterone was measured only in boys using Immulite chemiluminescent assays.
Results
For the entire sample, the median serum ferritin concentration was 30.0 [19.8–44.8] ng/mL and the prevalence of iron deficiency (ferritin < 15 ng/mL) was 14.2%. Iron deficiency was higher in girls compared with boys (respectively, 20.8% and 7.9%). This prevalence varied with the SES (respectively, 11.6%, 11.9%, and 16.8% in high, middle, and low SES, p = 0.09). Iron deficiency increased with age (9.5%, 15.7%, and 17.5%, respectively, for the age groups 8–11, 12–14, and 15–18, p = 0.014) and did not differ between normal, overweight, and obese groups (p = 0.07). In boys, a significant positive correlation was observed between ferritin and total testosterone (rho = 0.150, p = 0.001).
Conclusion
The prevalence of iron deficiency is relatively low in Lebanon. Younger boys, menstruating girls, and children from low SES are more prone to iron deficiency, while BMI has no impact.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Arosio P, Levi S. Cytosolic and mitochondrial ferritins in the regulation of cellular iron homeostasis and oxidative damage. Biochim Biophys Acta. 2010;1800:783–92.
WHO. Serum ferritin concentrations for the assessment of iron status and iron deficiency in populations. Vitamin and Mineral Nutrition Information System; 2019. https://www.who.int/vmnis/indicators/serum_ferritin.pdf.
Pfeiffer CM, Looker AC. Laboratory methodologies for indicators of iron status: strengths, limitations, and analytical challenges. Am J Clin Nutr. 2017;106 Suppl 6 :1606S–14S.
Daru J, Colman K, Stanworth SJ, De La Salle B, Wood EM, Pasricha S-R. Serum ferritin as an indicator of iron status: what do we need to know? Am J Clin Nutr. 2017;106 Suppl 6 :1634S–9S.
Cullis JO, Fitzsimons EJ, Griffiths WJ, Tsochatzis E, Thomas DW. Investigation and management of a raised serum ferritin. Br J Haematol. 2018;181:331–40.
Halterman JS, Kaczorowski JM, Aligne CA, Auinger P, Szilagyi PG. Iron deficiency and cognitive achievement among school-aged children and adolescents in the United States. Pediatrics. 2001;107:1381–6.
Bruner AB, Joffe A, Duggan AK, Casella JF, Brandt J. Randomised study of cognitive effects of iron supplementation in non-anaemic iron-deficient adolescent girls. Lancet Lond Engl. 1996;348:992–6.
Rowland TW, Deisroth MB, Green GM, Kelleher JF. The effect of iron therapy on the exercise capacity of nonanemic iron-deficient adolescent runners. Am J Dis Child. 1988;142:165–9.
Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: a systematic analysis of population-representative data. Lancet Glob Health. 2013;1:e16–25.
Hartfield D. Iron deficiency is a public health problem in Canadian infants and children. Paediatr Child Health. 2010;15:347–50.
Oatley H, Borkhoff CM, Chen S, Macarthur C, Persaud N, Birken CS, et al. Screening for iron deficiency in early childhood using serum ferritin in the primary care setting. Pediatrics. 2018;142: pii: e20182095. https://doi.org/10.1542/peds.2018-2095.
van der Merwe LF, Eussen SR. Iron status of young children in Europe. Am J Clin Nutr. 2017;106 Suppl 6 :1663S–71S.
Dupont C. [Prevalence of iron deficiency]. Arch Pediatr. 2017;24:5S45–8.
Ferrari M, Mistura L, Patterson E, Sjöström M, Díaz LE, Stehle P, et al. Evaluation of iron status in European adolescents through biochemical iron indicators: the HELENA Study. Eur J Clin Nutr. 2011;65:340–9.
Hercberg S, Preziosi P, Galan P. Iron deficiency in Europe. Public Health Nutr. 2001;4:537–45.
Tawfik AA, Hanna ET, Abdel-Maksoud AM. Anemia and iron deficiency anemia in Egypt. IOSR J Pharm 2015;5:5.
Shattnawi KK, Alomari M, Al-Sheyab N, Salameh AB. The relationship between plasma ferritin levels and body mass index among adolescents. Sci Rep. 2018;8:15307.
Salami A, Bahmad HF, Ghssein G, Salloum L, Fakih H. Prevalence of anemia among Lebanese hospitalized children: risk and protective factors. PLoS ONE 2018;13:e0201806.
Lynch S, Pfeiffer CM, Georgieff MK, Brittenham G, Fairweather-Tait S, Hurrell RF, et al. Biomarkers of nutrition for development (BOND)-iron review. J Nutr 2018;148 Suppl 1 :1001S–67S.
Gibson RS. Principles of nutritional assessment. New York; Oxford: Oxford University Press; 2005. http://www.tandfonline.com/toc/rwhi20/.
Nead KG, Halterman JS, Kaczorowski JM, Auinger P, Weitzman M. Overweight children and adolescents: a risk group for iron deficiency. Pediatrics. 2004;114:104–8.
Pinhas-Hamiel O, Newfield RS, Koren I, Agmon A, Lilos P, Phillip M. Greater prevalence of iron deficiency in overweight and obese children and adolescents. Int J Obes Relat Metab Disord. 2003;27:416–8.
Eftekhari M, Mozaffari-Khosravi H, Shidfar F. The relationship between BMI and iron status in iron-deficient adolescent Iranian girls. Public Health Nutr. 2009;12:2377–81.
Liu Z, Ye F, Zhang H, Gao Y, Tan A, Zhang S, et al. The association between the levels of serum ferritin and sex hormones in a large scale of Chinese male population. PLoS ONE 2013;8:e75908.
Chao K-C, Chang C-C, Chiou H-Y, Chang J-S. Serum ferritin is inversely correlated with testosterone in boys and young male adolescents: a cross-sectional study in Taiwan. PLoS ONE 2015;10:e0144238.
WHO. Growth reference data for 5-19 years. WHO; 2019. https://www.who.int/growthref/en/.
Gannagé-Yared M-H, Farah V, Chahine E, Balech N, Ibrahim T, Asmar N, et al. Distribution and correlates of non-high-density lipoprotein cholesterol and triglycerides in Lebanese school children. J Clin Lipido. 2016;10:378–85.
Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power3: a flexible statistical power analysis program for the social, behavioral,and biomedical sciences. Behav Res Methods. 2007;39:175–91.
Hwalla N, Al Dhaheri AS, Radwan H, Alfawaz HA, Fouda MA, Al-Daghri NM, et al. The prevalence of micronutrient deficiencies and inadequacies in the middle east and approaches to interventions. Nutrients. 2017;9:229. https://doi.org/10.3390/nu9030229.
Abou-Zeid AH, Abdel-Fattah MM, Al-Shehri AA, Hifnawy TM, Al-Hassan, S-AA. Anemia and nutritional status of schoolchildren living at Saudi high altitude area. Saudi Med J. 2006;27:862–9.
Milman N, Backer V, Laursen EM, Graudal N, Ibsen KK, Jordal R. Serum ferritin in children and adolescents. Results from population surveys in 1979 and 1986 comprising 1312 individuals. Eur J Haematol. 1994;53:16–20.
Beard JL, Connor JR. Iron status and neural functioning. Annu Rev Nutr. 2003;23:41–58.
Dallman PR. Biochemical basis for the manifestations of iron deficiency. Annu Rev Nutr. 1986;6:13–40.
Looker AC, Dallman PR, Carroll MD, Gunter EW, Johnson CL. Prevalence of iron deficiency in the United States. J Am Med Assoc. 1997;277:973–6.
Sekhar DL, Murray-Kolb LE, Kunselman AR, Weisman CS, Paul IM. Association between menarche and iron deficiency in non-anemic young women. PLoS ONE. 2017;12:e0177183.
Oh HL, Lee JA, Kim DH, Lim JS. Reference values for serum ferritin and percentage of transferrin saturation in Korean children and adolescents. Blood Res. 2018;53:18–24.
Nasreddine L, Naja F, Chamieh MC, Adra N, Sibai A-M, Hwalla N. Trends in overweight and obesity in Lebanon: evidence from two national cross-sectional surveys (1997 and 2009). BMC Public Health. 2012;12:798.
Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999-2016. Pediatrics. 2018;141:e20173459.
Skalicky A, Meyers AF, Adams WG, Yang Z, Cook JT, Frank DA. Child food insecurity and iron deficiency anemia in low-income infants and toddlers in the United States. Matern Child Health J. 2006;10:177–85.
Grossmann M, Panagiotopolous S, Sharpe K, MacIsaac RJ, Clarke S, Zajac JD, et al. Low testosterone and anaemia in men with type 2 diabetes. Clin Endocrinol. 2009;70:547–53.
Dhindsa S, Ghanim H, Batra M, Kuhadiya ND, Abuaysheh S, Sandhu S, et al. Insulin resistance and inflammation in hypogonadotropic hypogonadism and their reduction after testosterone replacement in men with Type 2 diabetes. Diabetes Care 2016;39:82–91.
Dhindsa S, Ghanim H, Batra M, Kuhadiya ND, Abuaysheh S, Green K, et al. Effect of testosterone on hepcidin, ferroportin, ferritin and iron binding capacity in patients with hypogonadotropic hypogonadism and type 2 diabetes. Clin Endocrinol. 2016;85:772–80.
Funding
This work was supported by a grant of the “Conseil de recherche de l'Université Saint-Joseph” FM249, Beirut.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics
The study protocol was approved by the Ethics Committee at Hôtel-Dieu de France Hospital (CEHDF449).
Informed consent
A written informed consent was signed by the parents of the included children.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
El Khoury, R., Sleilaty, G. & Gannagé-Yared, MH. Prevalence of Iron deficiency in Lebanese schoolchildren. Eur J Clin Nutr 74, 1157–1163 (2020). https://doi.org/10.1038/s41430-020-0590-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41430-020-0590-y
This article is cited by
-
Prevalence and status of Lipoprotein (a) among Lebanese school children
Scientific Reports (2020)