Abstract
Background/objectives
To characterise the infraorbital artery (IOA) and its orbital branch, which are key structures encountered during inferior orbital explorations, with potential for orbital haemorrhage and vision loss if inappropriately handled.
Methods
Thirteen embalmed heads (26 orbits) were dissected. The following parameters were measured: orientation of the IOA in relation to the infraorbital nerve (ION); presence or absence of the orbital branch of the IOA; and the distance between the orbital branch of the IOA to the inferior orbital rim.
Results
In the pterygopalatine fossa, the orientation of the IOA relative to V2 was medial (n = 9, 34.6%), inferior (n = 4, 15.4%), lateral (n = 4, 15.4%), inferolateral (n = 3, 11.5%), superolateral (n = 3, 11.5%), inferomedial (n = 2, 7.7%) and superior (n = 1, 3.8%). In the infraorbital canal, the IOA in relation to the ION was as follows: superomedial (n = 12, 46.2%), medial (n = 9, 34.6%), superior (n = 2, 7.7%), inferomedial (n = 2, 7.7%) and superolateral (n = 1, 3.8%). An orbital branch of the IOA was identified in 21/26 orbits (80.8%). The mean distance of the orbital branch to the inferior orbital rim was 13.0 ± 4.8 mm (range 2.0-23.0 mm).
Conclusions
The IOA is an important vascular structure to recognise during inferior orbitotomies. The most common configuration is an IOA that runs medially to V2 in the pterygopalatine fossa, then superomedially to the ION within the infraorbital canal. The orbital branch of the IOA emerges 13 mm posterior to the inferior orbital rim. Recognition of these arterial branches and appropriate cauterization are paramount for avoiding significant operative complications.
Similar content being viewed by others
Introduction
The orbital floor is a surgical corridor with relevance across multiple surgical specialties. It provides a route of access for orbital floor fracture repair, orbital floor decompression, and exploration of the inferior orbit. It is therefore paramount that surgeons are knowledgeable of vascular structures and their variants within the inferior orbit. The infraorbital artery (IOA) travels within the inferior orbital fissure and infraorbital canal, and often emits an orbital branch along the latter segment. Inadvertent trauma could result in profuse bleeding, with risks of vision loss and impaired visualisation of the surgical field. The aim of this study was to describe the anatomy of the infraorbital artery and its orbital branch to inform inferior orbital surgical approaches.
Materials and methods
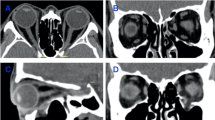
Ethics approval was obtained from the institutional review board prior to undertaking this study. This study adhered to the tenets of the Declaration of Helsinki. Thirteen formalin-fixed cadaver heads (26 orbits) were dissected. Red and blue coloured silicone was injected into the bilateral common carotid arteries and internal jugular veins respectively. A swinging eyelid approach was performed to reach the inferior orbit in the preseptal plane, followed by a subperiosteal dissection beyond the inferior orbital rim. The course of the IOA in relation to the infraorbital nerve (ION) within the infraorbital canal was recorded. The presence or absence of the orbital branch of the IOA was noted in each dissection. The distance between the orbital branch of the IOA and a point on the inferior orbital rim, above the infraorbital foramen, was measured. If there was more than 1 orbital branch of the IOA, the distance from the inferior orbital rim was taken from the more anterior branch. An example of the IOA and its orbital branch identified during dissection, is demonstrated in Fig. 1.
The infraorbital nerve (ION, solid arrow), infraorbital artery (IOA, asterisk) and orbital branches of the IOA (dashed arrows) are demonstrated. A anterior, L lateral, M medial, P posterior. A Orbital floor dissection in the subperiosteal plane demonstrates the ION within its canal, with the IOA running medially. B Once the roof of the infraorbital canal was removed, the IOA and its two orbital branches could be clearly identified travelling medial to the ION.
A two-tailed unpaired t-test was performed to compare the distance of the orbital branch from the inferior orbital rim between right and left sides, when present bilaterally. Statistical analysis was performed using GraphPad Prism Software. A p-value less than 0.05 was considered to be statistically significant.
Results
The results of this study are summarised in Tables 1–3. In the pterygopalatine fossa, the IOA was noted to traverse in the following positions relative to the second branch of the trigeminal nerve (V2): medial (n = 9, 34.6%), inferior (n = 4, 15.4%), lateral (n = 4, 15.4%), inferolateral (n = 3, 11.5%), superolateral (n = 3, 11.5%), inferomedial (n = 2, 7.7%) and superior (n = 1, 3.8%). The orientation of the IOA in relation to the ION in the infraorbital canal was recorded as follows: superomedial (n = 12, 46.2%), medial (n = 9, 34.6%), superior (n = 2, 7.7%), inferomedial (n = 2, 7.7%) and superolateral (n = 1, 3.8%).
The orbital branch of the IOA was identified in 21/26 orbits (80.8%). It was absent in both orbits in 2 specimens and unilaterally absent in 1 specimen. Its mean distance from the inferior orbital rim was 13.0 ± 4.8 mm (range 2.0–23.0 mm). There were 3 orbits that had two orbital branches of the IOA; this occurred bilaterally in 1 specimen and unilaterally in 1 specimen. In the bilateral case, the more anterior branch was located 7 mm and 6.5 mm, while the more posterior branch was 12.5 mm and 13.5 mm, posterior to the orbital rim. In the unilateral case, the orbital branches were encountered 11.5 mm and 16 mm from the orbital rim. In the 10 specimens (20 orbits) with orbital branches present bilaterally, a comparison of its distance from the inferior orbital rim between right and left sides demonstrated that there was no significant difference (p = 0.26).
Discussion
This cadaveric dissection study represents one of the largest to date to investigate the IOA and its orbital branch. The indications for an inferior orbital exploration are broad and encompass fracture repair, orbital floor reconstruction, decompressions and inferior orbital pathologies that may necessitate biopsy, debulking or en bloc excision. From an endonasal perspective, any associated vascular bundle is important to identify during approaches to the ION and maxillary roof. The IOA and its orbital branch are therefore key structures to recognise and avoid during any of these surgical explorations. The aim of this study was twofold: to determine the position of the IOA in relationship to the ION, and secondly to determine the presence and position of its orbital branch.
The IOA branches from the internal maxillary artery in the pterygopalatine fossa, where it ascends to reach the posteromedial aspect of the inferior orbital fissure, before emerging with the ION within the infraorbital canal [1]. The relationship between the IOA and ION has been investigated in several cadaveric dissection studies. At the transitional point between the pterygopalatine and orbitomaxillary segments of the ION, the IOA was often situated inferior or posterolateral to the nerve (75%), although other variants included an anteromedial position (15%) and a high loop anterior to the nerve (10%) [2]. In contrast, in this study, there were many variations of the IOA’s position relative to V2. The most common configuration was the IOA travelling medially to V2 in the pterygopalatine fossa upon branching from the internal maxillary artery, in 34.6% of cases. Li et al. reported that the IOA continued medial to the ION in 75% of cases when viewed within the roof of the maxillary sinus, from an endonasal prelacrimal approach [3]. Other variations of the IOA in relation to the ION were superior, inferior or intraneural positions where the artery traversed between ION fibres [3]. Kazkayasi et al. reported similar data in their cadaveric work, where the IOA was consistently found to be superomedial to the ION upon its exit at the infraorbital foramen [4]. This was consistent with our results, where the IOA was most commonly superomedial to the ION in the infraorbital canal.
The orbital branch of the IOA is an important orbital floor landmark and has been described in select orbital and ophthalmic anatomical texts [1, 5,6,7]. In this study, the orbital branch was present in 21 out of 26 orbits (80.8%), which reflects the experiences described in Patel et al.’s cadaveric study which demonstrated its presence in 8 of 9 orbits [8]. However, in a clinical study of orbital floor explorations, the orbital branch was present in 10 consecutive cases [9]. These disparate results likely represent sampling bias, though indicate that the orbital branch is found in the majority of cases. Histopathological studies have confirmed that the orbital branch traverses within a neurovascular bundle, accompanied by a small vein and peripheral nerve [8].
Much of the work regarding the orbital branch of the IOA has stemmed from experiences with significant orbital haemorrhage that were ultimately deemed preventable [9,10,11]. In these papers, the indications for accessing the orbital floor were for reconstructive purposes following a floor blowout fracture, medial wall fracture accessed via a subciliary approach, and maxillary atelectasis. The timing of haemorrhage was variable, occurring either immediately upon inadvertent intraoperative trauma, or 10 minutes to 15 hours postoperatively [9,10,11]. This demonstrates the importance of anticipation and planned cauterisation. Notably, the orbital branch of the IOA supplies multiple structures, including the inferior oblique, inferior rectus, orbital floor contents including orbital fat, and lacrimal sac from terminal branches [1, 6, 8, 12]. However, dividing the orbital branch is unlikely to compromise vascular supply of the relevant extraocular muscles and orbital fat, due to the abundance of internal and external carotid anastomoses with the inferior muscular branch of the ophthalmic artery [1]. Division of the orbital branch can be performed with bipolar electrocautery, which is preferable to monopolar cautery to minimise thermal damage to the ION [9].
In this study, the orbital branch of the IOA emerged at an average distance of 13.0 ± 4.8 mm (range 2.0-23.0 mm) posterior to the inferior orbital rim, which is consistent with data derived from prior cadaveric work. In two separate cadaveric dissections, the orbital branch emerged at a mean distance of 16.6 mm (range 10.0-23.0 mm) and 14.1 mm (range 3.0-20.0 mm) from the orbital rim [8, 13]. Similarly, clinical studies of inferior orbitotomies have reported that the orbital branch appears along the infraorbital canal at a mean distance of 14.4 mm (range 13.0-17.0 mm) posterior to the rim [9, 10]. In this study, there was no significant difference in the distance from the orbital branch to the inferior orbital rim between sides, when bilateral orbital branches were present. This would indicate some degree of anatomical symmetry in the arterial branching pattern. However, while most specimens were consistent with this observation, there was one cadaver with orbital branches that arose 2.0 mm and 12.5 mm from the inferior orbital rim (Table 3). The power of the statistical analysis would be improved with a larger sample size.
While the orbital branch usually emerges as a solitary vessel, there may also be multiple branches. We had 3 instances of two orbital branches arising from the IOA, with one specimen demonstrating this variant bilaterally. Similarly, Chien et al.’s cadaveric study found that 5 of 14 orbits had 1-2 additional branches of the IOA accompanying smaller branching nerves of the ION [13]. These measurements are supported by intraoperative clinical observations, where multiple branches may appear as 2-3 vessels appearing in 3-4 mm increments along the infraorbital canal [10]. Finally, the orbital branch can be variable in its configuration, and may emerge from the IOA as a thick band or a thin duplicate structure [8]. Either way, it can masquerade as a band of connective tissue and upwards retraction of the orbital contents should clearly present the arterial vessel for cauterisation.
We acknowledge that there are limitations inherent to a cadaveric dissection study. The IOA and its orbital branch were readily identified as being distinct from the adjacent ION, but red silicone was nevertheless injected to confirm the arterial structures. In 5 out of 26 orbits, no orbital branch was identified, which was a higher proportion than data reported from other cadaveric and clinical studies. This may have been a true reflection of significant anatomical variations. However, the integrity of a fragile orbital branch may have become compromised during the silicone injection or fixation process. In addition, further clinical data from inferior orbitotomies is necessary to validate our cadaveric measurements.
In conclusion, the IOA and its orbital branch are important arterial structures that should be properly anticipated and managed during any inferior orbitotomy. Cadaveric dissections in this study demonstrated that the IOA commonly traversed medially to V2 in the pterygopalatine fossa, then moved superomedially to the ION within the infraorbital canal. The orbital branch of the IOA emerged on average 13 mm from the inferior orbital rim, but multiple arterial branches was also occasionally observed. Careful dissection and handling of these structures is key to prevention of orbital haemorrhage and preservation of the surgical field.
Summary
What was known before
-
There is heterogeneous data on the position of the infraorbital artery in relation to V2 within the pterygopalatine fossa and orbital floor.
-
The orbital branch of the infraorbital artery is an important landmark in orbital floor explorations. There is heterogeneous data on its prevalence.
What this study adds
-
This is the one of the largest cadaveric studies to date to characterise the infraorbital artery’s orientation in relation to V2, and its arterial branching pattern.
-
The infraorbital artery is most commonly medial to V2 in the pterygopalatine fossa, followed by a superomedial position to the infraorbital nerve within the canal.
-
The orbital branch was present in 80.8% of orbits dissected, and its distance to the inferior orbital rim was 13.0 mm.
References
Dutton JJ. Atlas of Clinical and Surgical Orbital Anatomy : Expert Consult: Online and Print. Philadelphia, UNITED STATES: Elsevier - Health Sciences Division; 2011.
Herzallah IR, Elsheikh EM, Casiano RR. Endoscopic endonasal study of the maxillary nerve: a new orientation. Am J Rhinol. 2007;21:637–43.
Li L, London NR Jr, Prevedello DM, Carrau RL. Anatomical variants of the infraorbital canal: implications for the prelacrimal approach to the orbital floor. Am J Rhinol Allergy. 2020;34:176–82.
Kazkayasi M, Ergin A, Ersoy M, Tekdemir I, Elhan A. Microscopic anatomy of the infraorbital canal, nerve, and foramen. Otolaryngol Head Neck Surg. 2003;129:692–7.
Rootman J. Orbital Surgery: A Conceptual Approach. 2nd Ed. ed: Lippincott Williams & Wilkins (LWW); 2013.
Whitnall S. Anatomy of the human orbit and accessory organs of vision. New York: Oxford University Press; 1979.
Hayreh SS. Orbital vascular anatomy. Eye (Lond). 2006;20:1130–44.
Patel AV, Rashid A, Jakobiec FA, Lefebvre DR, Yoon MK. Orbital branch of the infraorbital artery: further characterization of an important surgical landmark. Orbit. 2015;34:212–5.
Rubin PA, Hatton MP, Bilyk JR. Orbital perforating branch of the infraorbital artery: an important landmark in orbital surgery. Ophthalmic Plast Reconstr Surg. 2005;21:447–9.
Coulter VL, Holds JB, Anderson RL. Avoiding complications of orbital surgery: the orbital branches of the infraorbital artery. Ophthalmic Surg. 1990;21:141–3.
Hwang K, Kim JH, Kang YH. Orbital hematoma caused by bleeding from orbital branch of the infraorbital artery after reconstruction of an orbital fracture. J Craniofac Surg. 2014;25:375–6.
Bergen MP. Microvessels in the human orbit in relation to the connective tissue system. Acta Morphol Neerl Scand. 1982;20:139–50.
Chien HF, Wu CH, Wen CY, Shieh JY. Cadaveric study of blood supply to the lower intraorbital fat: etiologic relevance to the complication of anaerobic cellulitis in orbital floor fracture. J Formos Med Assoc. 2001;100:192–7.
Acknowledgements
Dr Tong is supported by an Australian Government Research Training Program Scholarship.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
The authors confirm contribution as follows: Study conception: JYT, DS; study design: JYT, WC, AJP, DS; data collection: JYT, JS; data analysis: JYT, JS; manuscript composition and revision: JYT, JS, WC, AJP, DS.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tong, J.Y., Sung, J., Chan, W. et al. Anatomy of the infraorbital artery and its orbital branch. Eye 39, 1380–1383 (2025). https://doi.org/10.1038/s41433-025-03671-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03671-y