Abstract
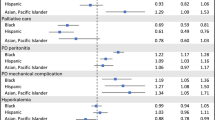
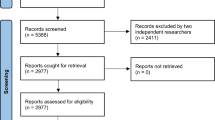
Peyronie’s Disease, which is known to have racial/ethnic disparities in the general population, has never been studied in the veteran population. We compared the diagnosis and treatment rates for Peyronie’s Disease among United States veterans of various racial-ethnic backgrounds at Veterans Affairs medical centers, which are equal-access systems. We queried the Veterans Affair Informatics and Computing Infrastructure to identify 17,647 Peyronie’s Disease patients in the United States by ICD-9 or ICD-10 code between 2015–2020. We assessed demographic characteristics, clinical characteristics, Veterans Affairs facility information, and treatment patterns. Racial-ethnic demographics of veterans with Peyronie’s Disease were 71.4% White, 15.4% Black, 5.8% Hispanic, 1.6% Native American, 0.3% Asian, and 5.4% unknown. Treatment rate was 13.6% overall, 13.6% of Whites (ref), 14.3% of Blacks (p = 0.2985), 13.5% of Hispanics (p = 0.9205), 9.1% of Asians (p = 0.3319), 16.7% of Native Americans (p = 0.1406), and 9.6% of unknown (p = 0.0041). White patients were more likely to receive injectional therapy and less likely to undergo surgery than Black patients. Peyronie’s Disease patients at Veterans Affairs facilities are treated at the same rate, indicating that equal-access healthcare systems may mitigate racial-ethnic disparities. Further research is necessary to account for differences in disease severity and Veterans Affairs surgeon availability.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All data are available from the corresponding author upon reasonable request.
References
Terrier JE, Nelson CJ. Psychological aspects of Peyronie’s disease. Transl Androl Urol. 2016;5:290–5. https://doi.org/10.21037/tau.2016.05.14.
Arafa M, Eid H, El-Badry A, Shamloul R. The prevalence of Peyronie’s disease in diabetic patients with erectile dysfunction. Int J Impot Res. 2007;19:213–7. https://doi.org/10.1038/sj.ijir.3901518.
Bjekic MD, Vlajinac HD, Sipetic SB, Marinkovic JM. Risk factors for Peyronie’s disease: a case-control study. BJU Int. 2006;97:570–4. https://doi.org/10.1111/j.1464-410X.2006.05969.x.
Pavone C, D’Amato F, Dispensa N, Torretta F, Magno C. Smoking, diabetes, blood hypertension: possible etiologic role for Peyronie’s disease? Analysis in 279 patients with a control group in Sicily. Arch Ital Urol Androl. 2015;87:20–24. https://doi.org/10.4081/aiua.2015.1.20.
Seal KH, Metzler TJ, Gima KS, Bertenthal D, Maguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs Health Care, 2002-2008. Am J Public Health. 2009;99:1651–8. https://doi.org/10.2105/AJPH.2008.150284.
Lindsay MB, Schain DM, Grambsch P, Benson RC, Beard CM, Kurland LT. The incidence of Peyronie’s disease in Rochester, Minnesota, 1950 through 1984. J Urol 1991;146:1007–9. https://doi.org/10.1016/s0022-5347(17)37988-0.
Sommer F, Schwarzer U, Wassmer G, Bloch W, Braun M, Klotz T, et al. Epidemiology of Peyronie’s disease. Int J Impot Res. 2002;14:379–83. https://doi.org/10.1038/sj.ijir.3900863.
Dibenedetti DB, Nguyen D, Zografos L, Ziemiecki R, Zhou X. A population-based study of Peyronie’s disease: prevalence and treatment patterns in the United States. Adv Urol. 2011;2011:282503 https://doi.org/10.1155/2011/282503.
Riviere P, Luterstein E, Kumar A, Vitzthum LK, Deka R, Sarkar RR, et al. Survival of African American and non-Hispanic white men with prostate cancer in an equal-access health care system. Cancer. 2020;126:1683–90. https://doi.org/10.1002/cncr.32666.
Planning O of P and. National Center for Veterans Analysis and Statistics. https://www.va.gov/vetdata/. Accessed 2 Aug 2021.
Liu Y, Sayam S, Shao X, Wang K, Zheng S, Li Y, et al. Prevalence of and trends in diabetes among veterans, United States, 2005–2014. Prev Chronic Dis. 2017;14:E135. https://doi.org/10.5888/pcd14.170230.
Hinojosa R. Veterans’ likelihood of reporting cardiovascular disease. J Am Board Fam Med. 2019;32:50–57. https://doi.org/10.3122/jabfm.2019.01.180148.
Fryar CD, Herrick K, Afful J, Ogden CL. Cardiovascular disease risk factors among male veterans, U.S., 2009-2012. Am J Prevent Med. 2016;50:101–5. https://doi.org/10.1016/j.amepre.2015.06.011.
Gould CE, Rideaux T, Spira AP, Beaudreau SA. Depression and anxiety symptoms in male veterans and non-veterans: the Health and Retirement Study. Int J Geriatr Psychiatry. 2015;30:623–30. https://doi.org/10.1002/gps.4193.
Stuntz M, Perlaky A, Vignes Fdes, Kyriakides T, Glass D. The prevalence of Peyronie’s disease in the United States: a population-based study. PLoS ONE. 2016;11:e0150157. https://doi.org/10.1371/journal.pone.0150157.
Billups KL. Erectile dysfunction as a marker for vascular disease. Curr Urol Rep. 2005;6:439–44. https://doi.org/10.1007/s11934-005-0039-9.
Blumentals WA, Gomez-Caminero A, Joo S, Vannappagari V. Is erectile dysfunction predictive of peripheral vascular disease. Aging Male. 2003;6:217–21. https://doi.org/10.1080/13685530312331309752.
Nelson CJ, Diblasio C, Kendirci M, Hellstrom W, Guhring P, Mulhall JP. The chronology of depression and distress in men with Peyronie’s disease. J Sex Med. 2008;5:1985–90. https://doi.org/10.1111/j.1743-6109.2008.00895.x.
Ginzburg K, Ein-Dor T, Solomon Z. Comorbidity of posttraumatic stress disorder, anxiety and depression: A 20-year longitudinal study of war veterans. J Affect Disord. 2010;123:249–57. https://doi.org/10.1016/j.jad.2009.08.006.
Zhang X, Lin D, Pforsich H, Lin VW. Physician workforce in the United States of America: forecasting nationwide shortages. Hum Resour Health. 2020;18:8 https://doi.org/10.1186/s12960-020-0448-3.
Zullig LL, Carpenter WR, Provenzale D, Weinberger M, Reeve BB, Jackson GL. Examining potential colorectal cancer care disparities in the Veterans Affairs health care system. J Clin Oncol. 2013;31:3579–84. https://doi.org/10.1200/JCO.2013.50.4753.
Trivedi AN, Grebla RC, Wright SM, Washington DL. Despite improved quality of care in the Veterans Affairs health system, racial disparity persists for important clinical outcomes. Health Aff. 2011;30:707–15. https://doi.org/10.1377/hlthaff.2011.0074.
Chakkera HA, O’Hare AM, Johansen KL, Hynes D, Stroupe K, Colin PM, et al. Influence of race on kidney transplant outcomes within and outside the department of Veterans Affairs. JASN. 2005;16:269–77. https://doi.org/10.1681/ASN.2004040333.
Yamoah K, Lee KM, Awasthi S, Alba PR, Perez C, Anglin-Foote TR, et al. Racial and ethnic disparities in prostate cancer outcomes in the Veterans Affairs health care system. JAMA Netw Open. 2022;5:e2144027. https://doi.org/10.1001/jamanetworkopen.2021.44027.
Bureau, U. S. C. Geographic levels. 2021. https://www.census.gov/programs-surveys/economic-census/guidance-geographies/levels.html#par_textimage_34.
Funding
This project was funded by the Copeland Foundation Grant awarded by the University of Miami, Department of Public Health Services.
Author information
Authors and Affiliations
Contributions
SN—Methodology, software, formal analysis, investigation, resources, data curation, writing – original draft, funding acquisition. IZ—Methodology, validation, data curation, writing – review & editing. IE—Methodology, investigation, data curation. SB—Methodology, writing – review & editing, supervision. RR—Conceptualization, writing – review & editing, supervision. TM—Conceptualization, methodology, investigation, resources, writing – review & editing, supervision, project administration.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Bruce W. Carter Veterans Affairs Medical Center Institutional Review Board.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nackeeran, S., Zucker, I., Efimenko, I. et al. Diagnosis and treatment patterns of Peyronie’s disease among different racial, ethnic, and regional groups in the Veterans Affairs healthcare system. Int J Impot Res 35, 706–711 (2023). https://doi.org/10.1038/s41443-022-00615-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41443-022-00615-y
This article is cited by
-
Commentary on diagnosis and treatment patterns of Peyronie’s disease among different racial, ethnic, and regional groups in the Veterans Affairs health care system
International Journal of Impotence Research (2023)