Abstract
Pelvic physical therapy is an evidence-based, first-line treatment for many pelvic floor disorders and sexual dysfunction. Studies have shown that pelvic physical therapy programs can both improve pelvic floor dysfunctions and sexual function. This article aims to provide an overview of the current state of the art regarding pelvic physical therapy for male sexual dysfunction to inform healthcare providers who treat men with sexual dysfunction better. A literature review was performed in Google Scholar, PubMed, and Science Direct to find review articles, research articles, and case studies about the effect of pelvic physical therapy treatments for male sexual dysfunction. Twenty-six articles were found about various pelvic physical therapy interventions. Besides this overview of the literature, an overview of interventions used in clinical practice is also provided. This narrative review supports the potential efficacy of pelvic physical therapy in addressing male sexual dysfunction. Pelvic physical therapy approaches that comprise exercise modalities, electrotherapy approaches, manipulative techniques, lifestyle changes, behavioral suggestions, and pain management strategies, should be suggested for potential benefits in improving erectile function, premature ejaculation, and sexual dysfunction-associated chronic pelvic pain. More research is needed to examine the effect of pelvic physical therapy on hypoactive sexual desire and delayed ejaculation.
Similar content being viewed by others
Introduction
Sexual dysfunction can be treated by various disciplines [1, 2] including pelvic physical therapists. In pelvic physical therapy (PPT) practice, pelvic floor muscle (PFM) function is a central focus point. Besides in-depth knowledge and skills to rehabilitate PFM function and reduce pain, pelvic physical therapists have profound knowledge of the biomechanics of the lower back, hip, pelvis, and pelvic organs. This knowledge is complemented by skills to treat affected joints, muscles, nerves, and connective tissues in this body region. Notwithstanding this specialized knowledge about the pelvic region, a biopsychosocial therapeutic approach is always required to fully understand the impact of presented symptoms of male sexual dysfunction [3].
Research supporting the effectiveness of PPT in men with sexual dysfunction shows improvements in erectile function, ejaculatory control, and overall sexual satisfaction following a course of pelvic floor rehabilitation [3]. This approach offers a promising alternative or complementary treatment to traditional medical interventions. Because a comprehensive overview of current PPT treatment options for male sexual dysfunction is lacking, this article aims to provide a narrative review of the current PPT approach for male sexual function problems.
Methods
A literature search for reviews addressing PPT for male sexual dysfunction was performed between January 1993 and December 2023 in Google Scholar, PubMed, and Science Direct using the search terms: male sexual disorders, erectile dysfunction (ED), male delayed orgasm, premature ejaculation (PE), delayed ejaculation (DE), anorgasmia, male orgasm, ejaculation, sexual dysfunction associated chronic pelvic pain syndrome (CPPS), physiotherapy, pelvic floor physiotherapy, pelvic exercise, pelvic physiotherapy, pelvic physical therapy, and exercise. This systematic search focused on sample size, intervention, outcome measures, and results concerning male sexual functioning. In addition, an overview is given of treatment methods based on clinical experience, supported by evidence where this was available.
Twenty-six articles were found specifically on PPT interventions for male sexual dysfunction, including 14 randomised clinical trials and 12 other articles (prospective cohorts and case reports). Questionnaire-based surveys and expert opinions types of articles were also included. Only studies published in English were considered.
Results
An overview of the literature review is listed in Table 1. Results are presented as well as treatment options and indications of how this option could be beneficial for sexual dysfunctions and CPPS. For interested non-pelvic physical therapist readers, a brief explanation of the working mechanisms is added to increase their level of insight and understanding.
Pelvic floor muscle exercises
The PFMs play a crucial role in sexual function, supporting erectile function and ejaculation control [4]. Dysfunctional PFMs can lead to difficulties in maintaining an erection or result in PE [5]. By engaging in targeted exercises and therapies, men can optimize PFM function, potentially alleviating symptoms of sexual dysfunction [6]. Therefore, in PPT practice, sexual function needs to be discussed addressing erectile function, ejaculation, and orgasm, including pain before, during, or after orgasm, sexual desire, arousal, and satisfaction.
During sexual activity, relaxation of PFMs is required for penile erection [5]. To sustain an erection when sexually aroused, a subtle coordinated interplay of muscle tension at the base of the penis shaft is needed [2]. Functionally, men need to be capable of contracting and relaxing the PFMs in a coordinated way for optimal sexual function. Any increase or decrease in muscle tension will affect coordination and muscle control. Treatment of any sexual dysfunction in PPT practice will, therefore, always include exercises to optimize muscle relaxation, strength, endurance, and coordination, aiming to regain adequate control over the PFMs and improve sexual functioning [7]. Studies demonstrated that PPT significantly improved erectile function in men with mild to moderate ED [5, 7]. The exercises focused on enhancing pelvic blood flow and muscle function, addressing the underlying causes of ED. PFM training including exercises that improve PFM control can increase intravaginal ejaculation latency time in men with PE [8]. Stronger superficial PFM may enhance orgasmic satisfaction during ejaculation [9]. A systematic review by Gbiri et al. highlighted the positive impact of PFM training on sexual function, concluding that PPT can be considered a valuable non-pharmacological intervention [7].
Biofeedback treatment
Biofeedback can be useful to provide better insight into PFM function when adequate muscle control is difficult. Visual and auditory feedback during the biofeedback treatment can help to gain insight into the ability to contract or relax the PFM. Biofeedback-assisted exercises may increase PFM control, enhance awareness, and generate faster results, increasing confidence to perform and apply the exercises functionally [10, 11]. Biofeedback measures before and after the treatment will provide the patient with more insight into the treatment results, which can help increase their self-confidence and sense of control over their PFMs and be helpful during the performance of home exercises and applied during sexual activities.
Biofeedback can be an effective non-pharmacological intervention for men with sexual dysfunction. It must be noted that individual responses can vary. Factors such as patient compliance, severity of PFM and sexual dysfunction, and underlying health conditions may influence the effectiveness of biofeedback-assisted interventions. A personalized approach, guided by healthcare professionals, is crucial for optimizing outcomes. Biofeedback-guided treatment can result in greater improvement than PFM exercises alone when treating ED [12].
Other studies demonstrated that biofeedback-assisted exercise interventions may contribute to improved penile blood flow, increased PFM function, and enhanced ejaculatory control in men experiencing ED [11,12,13]. Biofeedback holds promise as a non-pharmacological intervention for men with sexual dysfunction. However, comprehensive and personalized approaches, along with further research, are essential for establishing the role of biofeedback in the broader spectrum of sexual health interventions.
Electrostimulation
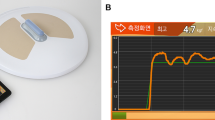
Electrostimulation methods, ranging from transcutaneous electrical nerve stimulation (TENS) to more advanced modalities, have shown promise in addressing underlying factors contributing to sexual dysfunction (see Fig. 1). During electrostimulation, different settings can be applied for different goals, such as improving strength or decreasing muscle tone, and reducing pain [7]. TENS, a non-invasive electrostimulation method, has been investigated for its potential to manage sexual dysfunction [14, 15]. Uribe et al. (2020) show that TENS of posterior tibial nerve when stimulated retrogradely through the stimulation of the posterior tibial nerve, decreases the parasympathetic pathway of the overactive response of the ejaculatory reflex arc thereby contributing to improve lifelong PE [16]. By modulating the ejaculatory reflex, these interventions aim to enhance ejaculatory control. However, research in this area is still in its early stages, necessitating further investigation [15].
The efficacy of electrostimulation methods may vary among individuals, influenced by factors such as the underlying cause of sexual dysfunction, patient compliance, and overall health [17]. A personalized approach, guided by healthcare professionals, is crucial for optimizing outcomes and ensuring patient safety. Nonetheless, electrostimulation presents a promising approach to the management of sexual dysfunction in men [18]. The literature suggests potential benefits in improving erectile function and ejaculatory control [15, 18]. However, further research and clinical trials are needed to establish the efficacy, safety, and optimal use of these methods in diverse patient populations.
Manipulative therapy techniques
Musculoskeletal complaints can be treated using joint mobilizations and mobilizing exercises to improve the range of motion in the affected joints. Better mechanical movement combined with massaging techniques including fascia and trigger point releases will help to decrease pain and increase the elasticity, contractability, condition, and recovery of affected tissues, improving muscle relaxation, strength, and coordination [19]. Reduced or increased mobility, inflammation, and pain in the lower back, hip, sacroiliac joints, coccyx, symphysis pubis, and surrounding muscles can contribute to pain and discomfort during sexual activity [20]. Sufficient joint mobility also creates more options for different sexual positions [21] (see Fig. 2).
Postural tips and tricks to be applied during sexual activity may help increase sexual pleasure if it leads to a situation in which sexual activities can be performed comfortably and painlessly [2]. When coccyx pain is present, a non-invasive mobilization of the coccyx (NIMOC), can be applied (see Fig. 2). Coccyx pain is often accompanied by increased PFM tone, and decreased coordination. This subtle treatment method has proved very effective in clinical practice [22] and may add to improving sexual dysfunction as a result of pain reduction and increased control over the PFMs.
In men with genital pain or CPPS, increased PFM tone is very common [6, 23]. Tender muscles in the pelvic floor, abdomen, and gluteal region can be detected in men with CPPS [24]. These musculoskeletal complaints are often treated in PPT practice using an integrated multidisciplinary approach including trigger point and myofascial release therapies. Individual responses to manipulative therapy methods can vary, and considerations, such as the underlying cause of sexual dysfunction, patient preferences, and overall health are important. A personalized approach, guided by healthcare professionals, is essential for optimizing outcomes. As research in manipulative therapy for sexual dysfunction evolves, future studies are needed to explore optimal treatment protocols, long-term efficacy, and the integration of manipulative therapies with other interventions to provide a comprehensive approach to sexual health.
Relaxation and breathing techniques
PFM contraction and relaxation should be coordinated and functional for optimal control over the bladder, the bowel, and sexual function [25]. Therefore, optimizing the PFM function can help to reduce all of these complaints. In the case of increased muscle tone, the first step to focus on is relaxation. PFM relaxation can be pursued by doing local and general relaxation exercises. Adequate local relaxation is easier in combination with deep abdominal breathing techniques, free diaphragmatic movement, and abdominal relaxation [26].
During inhalation, the diaphragm descends pushing the abdominal organs outward into the abdominal wall and down toward the pelvic floor, which ideally follows the downward direction of the moving diaphragm (see Fig. 3). This requires the relaxation of both the abdominal and PFMs. During exhalation, the movement direction is reversed and can be combined with contractions of the pelvic floor and abdominal muscles [26] (see Fig. 3). This procedure can be practiced repeatedly without altering the normal breathing pattern focusing on various levels of contraction and complete relaxation in the process. Better PFM relaxation can create opportunities for a better blood flow toward the penis which may improve erectile function. To allow painless sexual function, the PFMs should relax easily during deep breathing. Very often it is assumed that the PFMs need strengthening. However, it is impossible to adequately contract the PFMs when the muscle tone is increased. Further contraction of the already contracted and tight muscle will be very hard. Therefore, relaxation is very often the first requirement to create movement potential and to feel and coordinate muscle movement because increased PFM tone is common in men with sexual dysfunction, especially in men with CPPS [3, 27].
Lifestyle changes and physical activity interventions
Healthy living habits positively affect sexual health. Physical therapists encourage physical activity as part of a healthy lifestyle and to prevent illnesses [28, 29]. Physical activity interventions are an essential part of physical therapy to improve overall health and physical capability in ill and healthy people. Regular general exercise reduces fatigue and improves physical fitness, muscle strength, endurance, balance, and flexibility. Therefore, it can be assumed that leisure activities that include physical and systemic exercises and training improve men’s physical condition, which also improves their sexual health [30, 31].
Aerobic exercises, such as walking, swimming, and yoga can also assist PFM coordination as long as the activities are enjoyed and stimulate relaxation [7]. Men who exercise regularly, tend to have higher sexual desire as a result of increased testosterone secretion during the training, which also tends to reduce the occurrence of ED [21].
Mind-body approaches
Many individuals are unaware of the role their pelvic floor plays in sexual function. By educating men about the importance of these muscles and teaching them how to control and relax them, pelvic physical therapists empower patients to actively participate in their recovery. PPT programs promote awareness of the mind-body connection.
PPT extends beyond physical techniques to include mind-body approaches such as yoga and mindfulness. These practices may positively impact psychological factors contributing to sexual dysfunction, promoting relaxation, and reducing anxiety [32]. Mindfulness approaches, such as mindfulness-based cognitive therapy (MBCT), have shown promise in reducing psychological distress related to sexual dysfunction. Research by Brotto et al. (2008) suggests that mindfulness interventions can enhance sexual well-being by promoting present-moment awareness and reducing performance pressure [33]. Although the participants in this study were females, mindfullness might be considered in men, but further studies are needed.
Biopsychosocial approaches
Sexual dysfunction in men is a multifaceted issue influenced by biological, psychological, and social factors [34, 35]. Sexual dysfunction, encompassing conditions like ED and PE, demands a holistic understanding that goes beyond purely somatic and physiological aspects. Biopsychosocial approaches recognize the interplay between biological, psychological, and social factors in shaping sexual health [34,35,36].
Biopsychosocial approaches offer a holistic and patient-centered framework for addressing sexual dysfunction in men. From cognitive-behavioral therapy (CBT) to integrative sex therapy, the literature supports the effectiveness of interventions that consider biological, psychological, and social dimensions [37]. However, ongoing research and clinical exploration are essential to refine and expand these approaches for diverse patient populations.
CBT, a psychological intervention, has demonstrated efficacy in addressing psychological contributors to sexual dysfunction [38]. Studies, such as that by Althof et al. (2006), highlight the role of CBT in reducing performance anxiety and improving overall sexual satisfaction [39]. Integrative sex therapy combines psychological counseling with educational and behavioral interventions [40]. Research by Metz et al. (2017) underscores the effectiveness of this approach in addressing both psychological and relational aspects of sexual dysfunction [38].
Given the diverse nature of sexual dysfunction, a personalized approach that considers individual circumstances, preferences, and the severity of dysfunction is crucial. Physical therapists work closely with individuals to identify specific issues, and contributing factors, and design personalized exercise regimens. PPT should be tailored individually and consist of a biopsychosocial approach to treat effectively sexual dysfunctions that the approaches align with the unique needs of each patient [41].
Conclusion
This narrative review supports the potential efficacy of PPT in addressing male sexual dysfunction. The effectiveness of PPT for male sexual dysfunction is contingent on a variety of factors, such as the patient’s overall health, adherence to treatment, and the underlying causes of the sexual dysfunction. Therefore, a personalized treatment plan, developed in collaboration between the patient and the healthcare professional, ensures that the specific concerns of each patient are addressed effectively.
Further research and clinical trials can help to establish standardized protocols and to better understand the long-term effectiveness of PPT in this context. More research is needed to examine the effectiveness of PPT in the treatment of hyposexual desire disorder and delayed ejaculation.
References
Padoa A, McLean L, Morin M, Vandyken C. The overactive pelvic floor (OPF) and sexual dysfunction. Part 2: evaluation and treatment of sexual dysfunction in OPF patients. Sex Med Rev. 2021;9:76–92.
Rosenbaum TY. Pelvic floor involvement in male and female sexual dysfunction and the role of pelvic floor rehabilitation in treatment: a literature review. J Sex Med. 2007;4:4–13.
Yaacov D, Nelinger G, Kalichman L. The effect of pelvic floor rehabilitation on males with sexual dysfunction: a narrative review. Sex Med Rev. 2022;10:162–7.
Kim JK, Lee YJ, Kim H, Song SH, Jeong SJ, Byun SS. A prospectively collected observational study of pelvic floor muscle strength and erectile function using a novel personalized extracorporeal perineometer. Sci Rep. 2021;11:18389.
Lavoisier P, Roy P, Dantony E, Watrelot A, Ruggeri J, Dumoulin S. Pelvic-floor muscle rehabilitation in erectile dysfunction and premature ejaculation. Phys Ther. 2014;94:1731–43.
Cohen D, Gonzalez J, Goldstein I. The role of pelvic floor muscles in male sexual dysfunction and pelvic pain. Sex Med Rev. 2016;4:53–62.
Gbiri CAO, Akumabor JC. Effectiveness of physiotherapy interventions in the management male sexual dysfunction: a systematic review. Int J Sex Health. 2023;35:52–66.
Pastore AL, Palleschi G, Fuschi A, Maggioni C, Rago R, Zucchi A, et al. Pelvic floor muscle rehabilitation for patients with lifelong premature ejaculation: a novel therapeutic approach. Ther Adv Urol. 2014;6:83–8.
La Pera G. Awareness and timing of pelvic floor muscle contraction, pelvic exercises and rehabilitation of pelvic floor in lifelong premature ejaculation: 5 years experience. Arch Ital Urol Androl. 2014;86:123–5.
Hite M, Curran T. Biofeedback for pelvic floor disorders. Clin Colon Rectal Surg. 2020;34:056–61.
Prota C, Gomes CM, Ribeiro LH, de Bessa J Jr., Nakano E, Dall’Oglio M, et al. Early postoperative pelvic-floor biofeedback improves erectile function in men undergoing radical prostatectomy: a prospective, randomized, controlled trial. Int J Impot Res. 2012;24:174–8.
Van Kampen M, De Weerdt W, Claes H, Feys H, De Maeyer M, Van Poppel H. Treatment of erectile dysfunction by perineal exercise, electromyographic biofeedback, and electrical stimulation. Phys Ther. 2003;83:536–43.
Sighinolfi MC, Rivalta M, Mofferdin A, Micali S, De Stefani S, Bianchi G. Potential effectiveness of pelvic floor rehabilitation treatment for postradical prostatectomy incontinence, climacturia, and erectile dysfunction: a case series. J Sex Med. 2009;6:3496–9.
Shechter A, Mondaini N, Serefoglu EC, Gollan T, Deutsch F, Appel B, et al. A novel on-demand therapy for lifelong premature ejaculation using a miniature transperineal electrical stimulator-the vPatch: an as-treated analysis. J Sex Med. 2023;20:22–9.
Shechter A, Serefoglu EC, Gollan T, Springer S, Meiry G, Appel B, et al. Transcutaneous functional electrical stimulation-a novel therapy for premature ejaculation: results of a proof of concept study. Int J Impot Res. 2020;32:440–5.
Uribe OL, Sandoval-Salinas C, Corredor HA, Martínez JM, Saffon JP. Transcutaneous electric nerve stimulation to treat patients with premature ejaculation: phase II clinical trial. Int J Impot Res. 2020;32:434–9.
da Fonseca Pedroso IM, Siqueira MLS, de Sousa Santos T, de Paula Barbosa K, de Lima EAN, Sampaio A, et al. Conservative treatment of sexual dysfunction among men undergoing prostate cancer treatment: a systematic review. Sex Med Rev. 2024;12:710–9.
Rislanu A, Auwal H, Musa D, Auwal A. Comparative effectiveness of electrical stimulation and aerobic exercise in the management of erectile dysfunction: a randomized clinical trial. Ethiop J Health Sci. 2020;30:961–70.
Abner TDSS, Dantas MIO, Azevedo-Santos IF, DeSantana JM. Joint mobilization associated or not to other therapies reduces chronic musculoskeletal pain: a systematic review. BrJP. 2020;3:73–85.
Roberts A, Harris K, Outen B, Bukvic A, Smith B, Schultz A, et al. Osteopathic manipulative medicine: a brief review of the hands-on treatment approaches and their therapeutic uses. Medicines. 2022;9:33.
Areskoug-Josefsson K, Gard G. Physiotherapy as a promoter of sexual health. Physiother Theory Pract. 2015;31:390–5.
Slieker-ten Hove MP. Down under, top relevant: pelvic floor dysfunction problems in patients with coccygeal, hip and low back pain. J Pelvic, Obs and Gyn Physiotherapy. 2016;118:58–60.
Baranowski AP, Mandeville AL, Edwards S, Brook S, Cambitzi J, Cohen M. Male chronic pelvic pain syndrome and the role of interdisciplinary pain management. World J Urol. 2013;31:779–84.
Bradley MH, Rawlins A, Brinker CA. Physical therapy treatment of pelvic pain. Phys Med Rehabil Clin N Am. 2017;28:589–601.
Padoa A, McLean L, Morin M, Vandyken C. “The overactive pelvic floor (OPF) and sexual dysfunction” Part 1: Pathophysiology of OPF and its impact on the sexual response. Sex Med Rev. 2021;9:64–75.
Talasz H, Kremser C, Talasz HJ, Kofler M, Rudisch A. Breathing,(S) training and the pelvic floor—a basic concept. Healthcare. 2022;10:1035.
Hetrick DC, Ciol MA, Rothman I, Turner JA, Frest M, Berger RE. Musculoskeletal dysfunction in men with chronic pelvic pain syndrome type III: a case-control study. J Urol. 2003;170:828–31.
Bortz W 2nd, Wallace DH. Physical fitness, aging, and sexuality. West J Med. 1999;170:167.
Sharma R, Biedenharn KR, Fedor JM, Agarwal A. Lifestyle factors and reproductive health: taking control of your fertility. Reprod Biol Endocrinol. 2013;11:66.
Monga TN, Tan G, Ostermann HJ, Monga U, Grabois M. Sexuality and sexual adjustment of patients with chronic pain. Disabil Rehabil. 1998;20:317–29.
Esposito K, Ciotola M, Giugliano F, Maiorino MI, Autorino R, De Sio M, et al. Effects of intensive lifestyle changes on erectile dysfunction in men. J Sex Med. 2009;6:243–50.
Pascoe MC, Bauer IE. A systematic review of randomised control trials on the effects of yoga on stress measures and mood. J Psychiatr Res. 2015;68:270–82.
Brotto LA, Basson R, Luria M. A mindfulness-based group psychoeducational intervention targeting sexual arousal disorder in women. J Sex Med. 2008;5:1646–59.
Montorsi F, Adaikan G, Becher E, Giuliano F, Khoury S, Lue TF, et al. Summary of the recommendations on sexual dysfunctions in men. J Sex Med. 2010;7:3572–88.
Rosen RC. Prevalence and risk factors of sexual dysfunction in men and women. Curr Psychiatry Rep. 2000;2:189–95.
Colonnello E, Ciocca G, Limoncin E, Sansone A, Jannini EA. Redefining a sexual medicine paradigm: subclinical premature ejaculation as a new taxonomic entity. Nat Rev Urol. 2021;18:115–27.
Tripodi F, Reisman Y, Lowenstein L The biopsychosocial approach in sexual medicine disorders. Textbook of rare sexual medicine conditions. Springer; 2022. p. 7–18.
Metz M, Epstein N, Mccarthy B Cognitive-behavioral therapy for sexual dysfunction. Routledge; 2017.
Althof SE, Leiblum SR, Chevret-Measson M, Hartmann U, Levine SB, McCabe M, et al. Psychological and interpersonal dimensions of sexual function and dysfunction. J Sex Med. 2005;2:793–800.
Perelman MA. Combination therapy for sexual dysfunction: Integrating sex therapy and pharmacotherapy. Handbook of sexual dysfunction. 2005:13–41.
Sandler MD, Ledesma B, Thomas J, Ben-Ezra L, Lokeshwar SD, Paz LA, et al. Biopsychosocial approach to male chronic pelvic pain syndrome: recent treatments and trials. Sex Med Rev. 2023;12:59–66.
Claes H, Baert L. Pelvic floor exercise versus surgery in the treatment of impotence. Br J Urol. 1993;71:52–7.
Claes H, Van Kampen M, Baert L. Pelvic floor exercise in the treatment of impotence. Eur J Phys Rehabil Med. 1995;5:42–6.
Dorey G, Speakman M, Feneley R, Swinkels A, Dunn C, Ewings P. Randomised controlled trial of pelvic floor muscle exercises and manometric biofeedback for erectile dysfunction. Br J Gen Pract. 2004;54:819–25.
Mohammed AH, Zedan MA, Ban HM. Role of pelvic floor muscle exercises in management of erectile dysfunction in patients with chronic obstructive pulmonary disease. Egypt J Chest Dis Tuberc. 2015;64:47–50.
Kurkar A, Abulsorour SM, Gamal RM, Eltaher AM, Safwat AS, Gadelmoula MM, et al. Treatment of premature ejaculation: a new combined approach. Egypt Rheumatol Rehabil. 2015;42:39–44.
La Pera G, Nicastro A. A new treatment for premature ejaculation: the rehabilitation of the pelvic floor. J Sex Marital Ther. 1996;22:22–6.
Pastore AL, Palleschi G, Leto A, Pacini L, Iori F, Leonardo C, et al. A prospective randomized study to compare pelvic floor rehabilitation and dapoxetine for treatment of lifelong premature ejaculation. Int J Androl. 2012;35:528–33.
Altunan B, Gundogdu AA, Ozcaglayan TIK, Unal A, Turgut N. The effect of pelvic floor exercise program on incontinence and sexual dysfunction in multiple sclerosis patients. Int Urol Nephrol. 2021;53:1059–65.
Dorey G, Speakman MJ, Feneley RC, Swinkels A, Dunn CD. Pelvic floor exercises for erectile dysfunction. BJU Int. 2005;96:595–7.
Anderson RU, Wise D, Sawyer T, Chan CA. Sexual dysfunction in men with chronic prostatitis/chronic pelvic pain syndrome: improvement after trigger point release and paradoxical relaxation training. J Urol. 2006;176:1534–9.
Begot I, Peixoto TC, Gonzaga LR, Bolzan DW, Papa V, Carvalho AC, et al. A home-based walking program improves erectile dysfunction in men with an acute myocardial infarction. Am J Cardiol. 2015;115:571–5.
Carboni C, Fornari A, Bragante KC, Averbeck MA, Vianna da Rosa P, Mea Plentz RD. An initial study on the effect of functional electrical stimulation in erectile dysfunction: a randomized controlled trial. Int J Impot Res. 2018;30:97–101.
Geraerts I, Van Poppel H, Devoogdt N, De Groef A, Fieuws S, Van Kampen M. Pelvic floor muscle training for erectile dysfunction and climacturia 1 year after nerve sparing radical prostatectomy: a randomized controlled trial. Int J Impot Res. 2016;28:9–13.
Kałka D, Domagała Z, Dworak J, Womperski K, Rusiecki L, Marciniak W, et al. Association between physical exercise and quality of erection in men with ischaemic heart disease and erectile dysfunction subjected to physical training. Kardiol Pol. 2013;71:573–80.
Lamina S, Okoye CG, Dagogo TT. Therapeutic effect of an interval exercise training program in the management of erectile dysfunction in hypertensive patients. J Clin Hypertens. 2009;11:125–9.
Lin YH, Yu TJ, Lin VC, Wang HP, Lu K. Effects of early pelvic-floor muscle exercise for sexual dysfunction in radical prostatectomy recipients. Cancer Nurs. 2012;35:106–14.
Palm P, Zwisler AO, Svendsen JH, Thygesen LC, Giraldi A, Jensen KG, et al. Sexual rehabilitation for cardiac patients with erectile dysfunction: a randomised clinical trial. Heart. 2019;105:775–82.
Yüksel ÖH, Memetoğlu ÖG, Ürkmez A, Aktaş İ, Verit A. The role of physical activity in the treatment of erectile dysfunction. Rev Int Androl. 2015;13:115–9.
Dorey G, Feneley RC, Speakman MJ, Robinson JP, Paterson J. Pelvic floor muscle exercises and manometric biofeedback for erectile dysfunction and postmicturition dribble: three case studies. J Wound Ostomy Continence Nurs. 2003;30:44–51.
Acknowledgements
We are grateful to Ege Can Serefoglu for suggesting the idea of this narrative review.
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and Affiliations
Contributions
ES and ENC performed the literature search, selected the papers, and ES, AB, and ENC wrote the draft of the manuscript. The final version of the manuscript has been reviewed and edited by ES, AB, HBY, and BM. All the authors discussed the results and contributed to the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sahin, E., Brand, A., Cetindag, E.N. et al. Pelvic physical therapy for male sexual disorders: a narrative review. Int J Impot Res 37, 941–949 (2025). https://doi.org/10.1038/s41443-025-01034-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41443-025-01034-5