Abstract
Post-Orgasmic Illness Syndrome (POIS) is a rare medical condition characterized by a range of distressing physical and cognitive symptoms that occur following ejaculation in affected individuals. Little is known about the complex interaction between self-esteem and relationship factors that affect those living with POIS. This study investigated the impact of POIS on intimate relationships and feelings of isolation and stigmatization, including questions related to personal and partner control over symptoms. Furthermore, it aims to provide a clinical framework for addressing the psychosocial concerns of this patient population and their partners. Eighty-three patients (76.3% white, 37.5% with Bachelor’s degree, 73.8% middle income or higher) with POIS completed the Sexual Dysfunction Attribution Scale (SDAS) as part of the larger survey study. Surveys were distributed via social media, online groups, and forums including the subreddit: “POIS”, Twitter, and “POISCENTER” and were completed between 05/21/24–06/09/24. Descriptive, exploratory, and demographic data of the participants are provided from this survey. Patients with POIS were likely to report feeling no personal control over their symptoms (81.9%), feeling that their symptoms would “always be present” (96.4%), and feeling that they were personally to blame for their sexual dysfunction (60.2%). Overall, 80.7% reported that their symptoms negatively affected their relationships, and 37.3% reported not having sex within the past year. Our results can help providers to understand the experiences of patients with POIS and equip them to recommend the appropriate resources. Further research may use advanced analytical and qualitative techniques to better elucidate this population’s challenges.
Similar content being viewed by others
Introduction
Post-orgasmic illness syndrome (POIS) is a rare medical condition characterized by a range of distressing physical and cognitive symptoms that occur following ejaculation in affected individuals [1]. Historically, POIS was first described in a paired case study of two men experiencing similar symptoms after orgasm by Waldinger and Schweitzer [2]. Since then, several cases of POIS have been described in the literature with alternative theories for proposed etiologies [3,4,5].
As a foundation, Waldinger et al. [1] created five diagnostic criteria, the first being the presentation of at least one of the seven symptom clusters. These seven clusters include general, flu-like, head, eyes, nose, throat, or muscle symptoms. The other four criteria for POIS diagnosis are as follows: patients must experience symptoms that occur immediately after or within a few hours of ejaculation, symptoms must reoccur post-ejaculation nearly always, lasting two to seven days and then spontaneously disappearing [1]. The exact etiology of POIS has been unclear in the literature thus far. However, in addition to Waldinger’s diagnostic criteria, he proposed what is currently the most widely accepted etiology of POIS. He described POIS to likely be caused by an autologous immune response as he demonstrated through positive skin-prick tests of POIS patients to their own semen [1]. However, a recent case study on a POIS patient showed that they did not have an IGE-mediated immune response to their semen despite still meeting the diagnostic criteria laid out by Waldinger [3]. Another study completed by Xi et al. [6] in 2023 conducted a skin-prick test on POIS patients and controls and found positive immune responses with no major differences between the two groups. Other proposed etiologies have included a mu-opioid receptor disorder [3], association with Dhat syndrome [4], or progesterone deficiency [5].
Most recent investigations into POIS have focused on etiologies, physical effects, diagnostic criteria, and treatment of symptoms [7,8,9]. While it is not currently fully understood what causes POIS, there have been numerous case studies into different treatment options with a wide range of efficacy and little replication across studies [10,11,12]. Depending on the definition used, POIS may or may not also fall under the definition of a sexual functional disability as its effects begin post-coitus. Functional disabilities or impairments are broadly defined as those symptoms that limit one’s ability to complete everyday functions or activities in their daily lives [13].
In the broader literature on chronic illness and sexual dysfunction, there is a high degree of psychosocial burden for individuals with these conditions [14]. For example, erectile dysfunction (ED) is clearly associated with decreased health of relationships [14]. Sufferers of ED also have high rates of absenteeism and it has been shown that their chronic illness has an impact on their ability to complete their work satisfactorily [15].
From its original discovery, more has become known about POIS; however, information gaps still exist regarding the disease process. Much of the recent focus has leaned toward determining the etiology of POIS alongside potential disease treatments [16]. However, in this study, we aim to shed light on the psychosocial burden of this condition. While all aspects of POIS are essential, our objective is to add perspective on the complex interaction between self-esteem and relationship factors that affect those living with POIS.
Methods
Participants
The data for the current study was taken from a larger project focused on the psychosocial burden of POIS. The larger study aimed to gather information related to psychosocial burden, specific symptoms, and functional impacts of POIS symptomatology using a series of surveys related to each area of interest. Follow-up focus groups were conducted to additionally assess POIS symptomatology and functional impacts. Participants for the current study were English-speaking, 18 years or older, male-at-birth, and either (1) had been diagnosed with POIS by a physician (45.8%) or (2) reported symptoms consistent with a diagnosis of POIS. As a part of the larger study, participants completed several anonymous online self-report surveys during the summer of 2024 about their symptoms during the summer of 2024. Participants were required to indicate prior diagnosis of POIS and answer a selection of diagnostic questions related to their diagnosis. If participants had not previously been diagnosed, they had to meet all diagnostic criteria questions correctly or they were excluded from the rest of the surveys. Although the survey link was publicly shared, the need to correctly answer diagnostic questions in order to proceed made it harder for ‘bad actors’ or bots to answer the questions. Participants could theoretically have participated multiple times but timestamped answers and lack of grouping in survey completion times/dates makes this less likely. These surveys also collected demographic information. The UMass Chan institutional review board approved this study for survey distribution to POIS patients using online forums and groups. The surveys were distributed via the following websites: POIScenter.com, Facebook, Instagram, Twitter, and Reddit (r/POIS). Participants for the current study included 83 POIS patients. Participants were only included if they completed the entirety of the Sexual Dysfunction Attribution Scale (SDAS). Three individuals (3.6%) did not complete the demographic survey. Two individuals did not report ethnicity (2.5%; 2 of the 80 who completed demographic surveys).
Materials and procedures
Currently, no measure of sexual dysfunction has been created explicitly for use in POIS. Instead, this study utilized the Sexual Dysfunction Attribution Scale (SDAS), developed by Stephenson and Meston in 2016 [17] based off of the Relationship Attribution Measure (RAM), which has been validated in males and females [18]. The RAM is a commonly used measure to assess causal attributions in relationship conflict and distress (e.g., partner versus self-responsibility, blame, intent). Prior to the creation of the SDAS, there was no scale specific to causal attribution in those partners with sexual dysfunction. Stephenson and Meston [17] used the RAM to create the SDAS in an effort to directly assess relational attributions for sexual dysfunction [17]. In this effort, the SDAS questions largely parallel the wording of the RAM, with minor adjustments to make the content of the situation specific to sexual dysfunction as opposed to general relationship conflict or distress. For example, a question on the RAM that assesses self-blame (i.e., internal locus of control) states “My spouse’s behavior was due to something about me (e.g., the type of person I am, the mood I was in)” while a similar question on the SDAS states “Something about me personally causes my sexual difficulties (e.g., the type of person I am, the mood I am in)”. While the SDAS was initially designed to “measure a range of attributions including locus, control, and blame” regarding sexual dysfunction symptoms [19] in women, it was converted for use with the male POIS population for the current study with no significant variations in question design. The SDAS includes 13 items which assess causal attributions, sexual functioning, and subjective well-being related to symptoms [17]. SDAS items are rated on a 6-point Likert scale from Strongly Disagree to Strongly Agree with higher scores indicative of higher agreement for each item’s question. The only change for the SDAS in the current study was the use of a Likert-type slider with a number reference to indicate their answer to the question rather than radio buttons with numbers alone. Table 1 shows the survey questions in order of presentation and the survey response options. Questions 1 through 6 were presented to participants with 6 response options (Likert option 1 through 6). Questions 7 through 13 were presented with the aforementioned slider bar response options with anchors of 1 and 6 present (see Table 1). Descriptive statistics were utilized in an exploratory fashion to investigate the overall level of sexual dysfunction among this study’s POIS population.
Results
Participant characteristics
The demographic information for study participants is shown in Table 2. The sample consisted of 83 male-at-birth POIS patients (100% male-at-birth and 100% male gender identity). The participants were mostly White (76.3%), single (63.8%) men from urban communities (56.3%). They were in early to middle adulthood (63.8% were between the ages of 25 and 44), were highly educated (71.3% had at least a Bachelor’s degree or greater), and belonged to middle to upper middle-income socioeconomic classes (66.3%). Table 2 shows the work status and disability status of the participants. As can be seen in the table, the vast majority of the sample was employed (76.5%) with no disability status (85.0%). The most commonly reported disability status was having a physical disability (66.7% of those who reported having mental and/or physical disability statuses). Most participants had health insurance (73.4%). Fifty-two participants (65.0%) reported having sexual intercourse within the past year.
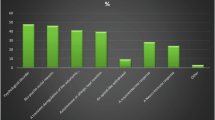
SDAS survey results
The SDAS survey results are shown in Fig. 1 for the first 6 SDAS questions and in Fig. 2 for the following 7 questions which focus on locus of control/fault. Notable results from the SDAS include: 78.3% at least slightly agreed to the statement “something about me physically causes my sexual dissatisfaction”, while less than half (48.2%) of respondents agreed to the statement “Something about me personally causes my sexual difficulties”. Roughly 66.3% of respondents agreed that the cause of their sexual difficulties is specific to sexual activity as opposed to being caused by something that their partner does (only 25.3% agreed to this statement) or caused by an outside circumstance (e.g., lack of privacy; only 24.1% agreed to this statement). The vast majority (80.7%) of respondents agreed that POIS affects their relationships.
N = 83. Slightly disagree, moderately disagree, and strongly disagree were combined into one dichotomous “disagree” option for the purposes of creating this chart. Similarly, slightly, moderately, and strongly agree were combined into a single “agree” option. See Table 1 for SDAS survey questions’ text and response option anchors.
N = 83. These questions were presented with slider bar options with the positive and negatively skewed anchors that are listed in Table 1. The slider bar represented a 6-point Likert Scale. For the purposes of creating this figure, the lowest 3 response options and the highest 3 response options were combined to form two dichotomous categories that are presented here.
Most respondents (96.4%) reported their symptoms were stable over time. Specifically, they were more likely to feel that the causes of their sexual dysfunction “will always be present”. Additionally, over 81–85% of respondents believed that both they (81.9%) and their partner (85.5%) had little to no control over the causes of their sexual difficulties. When asked who deserves to be blamed for their sexual difficulties, the majority of respondents were more likely to blame themselves for their sexual dysfunction (60.2% assigned personal blame) as compared to blaming their partner (only 7.2%).
Discussion
The results of the current study found that those with POIS tended to report little internal locus of control and high levels of hopelessness regarding their symptoms. Specifically, they were likely to report that the cause of their symptoms would “always be present” and that they were personally to blame for their sexual dysfunction. Understandably, over 80% (80.7%) reported that their symptoms negatively affected their relationships. The results of this study support previously assumed ideas about POIS and show that it affects numerous aspects of patients’ lives [20]. To our knowledge and following an in-depth search of current medical literature, there has not been a study focused on the psychosocial aspects of POIS to date, although there is previous literature that has mentioned some of the psychosocial impacts that POIS patients have described feeling [17]. It should be noted that the current study is descriptive in nature and that no control group was utilized for comparison.
While the etiology of POIS is not yet fully understood, treatment of the patients’ mental and physical ailments is of the utmost importance. In looking at the SDAS survey results of the study population it is clear that they do not feel that they have control over their symptoms or the syndrome that causes it. It is also causing distress in patient relationships. Additionally, based on the current study’s survey responses on frequency of sexual activity, the POIS patients in this sample are having less sex per year on average than most healthy males in the same age cohorts [21]. For example, in a national survey of men aged 18–44, only about 15–25% reported not having sex within the past year [21]. The current study’s results, however, found that 37.3% of POIS patients have not had sex within the past year.
Although this study was not intended to identify causal reasons for psychosocial burden in POIS, we hypothesize that the study results may be related to the consistency of POIS symptomatology, the possible severity of those symptoms, and/or to the psychological effects of having chronic sexual dysfunction. We believe that the psychological impacts of POIS may present similarly to those of other chronic illnesses and other forms of sexual dysfunction. For example, in a study of erectile dysfunction (ED) those with symptoms of ED reported significantly higher rates of depression than those without symptoms of ED as well as a lower quality of life, and decreased intimacy and sexual satisfaction [22, 23]. It is also understood that sexual dysfunction, such as ED, can create physical and emotional changes in their partners, ranging from increased sexual dissatisfaction, and orgasm difficulty [24]. Although female partners of POIS sufferers were not included in this study, the result showing 80.7% of respondents felt that POIS had an effect on their relationship clearly indicates that there must be some effect on their partnerships. Additionally, those with POIS show a high level of unemployment at a rate of 23.5% (see Table 3), which may correlate with chronic absenteeism or an inability to complete their work in a way that allows them to stay employed at the average rate.
One limitation of this study was the use of the SDAS scale as it has not been used for male sexual dysfunction previously. Future studies into the psychosocial effects of POIS should investigate the replicability of results and further expand on the topics that patients noted to better understand the causal effects of the psychosocial aspect of POIS. Future research should also investigate treatment and care for the mentally debilitating psychosocial and intimate relationship aspects of POIS. Additionally, the survey is subject to response bias, being shared online, with patients more bothered by their POIS symptoms being more likely to fill out the survey. Finally, the current study did not have access to a control group in order to compare those with POIS to those without other sexual dysfunctions. Future research should address these limitations.
Conclusion
The current descriptive study in men with POIS found that those individuals tend to have little internal locus of control over their symptoms and tend to blame themselves for these symptoms. They believe that their condition will be consistently present and tend to feel hopeless about their symptoms. Additionally, those with POIS have a high relationship burden with 80.9% reporting negative effects on their relationship, with over one third reporting abstaining from sex within the past year. Understanding the psychosocial burden of POIS is important so that an increased focus can be provided on possible treatment strategies (e.g., relationship counseling) for such psychosocial impacts.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Waldinger MD, Meinardi MMHM, Zwinderman AH, Schweitzer DH. Postorgasmic Illness Syndrome (POIS) in 45 Dutch caucasian males: clinical characteristics and evidence for an immunogenic pathogenesis (Part 1). J Sex Med. 2011;8:1164–70. https://doi.org/10.1111/j.1743-6109.2010.02166.x
Waldinger MD, Schweitzer DH. Postorgasmic illness syndrome: two cases. J Sex Marital Ther. 2002;28:251–5. https://doi.org/10.1080/009262302760328280
Jiang N, Xi G, Li H, Yin J. Postorgasmic Illness Syndrome (POIS) in a Chinese Man: no proof for IgE‐mediated allergy to semen. J Sex Med. 2015;12:840–5. https://doi.org/10.1111/jsm.12813
Ashby J, Goldmeier D. Postorgasm illness syndrome–a spectrum of illnesses. J Sex Med. 2010;7:1976–81. https://doi.org/10.1111/j.1743-6109.2010.01707.x
Dexter S. Benign coital headache relieved by partner’s pregnancies with implications for future treatment. BMJ Case Rep. 2010;2010:bcr10.2009.2359 https://doi.org/10.1136/bcr.10.2009.2359
Xi GP, Yang RX, Zhang J, Ma YM, Zhong XY. Clinical characteristics, allergic response to autologous semen, and desensitization in patients with postorgasmic illness syndrome. Sex Med. 2023;11:qfad068. https://doi.org/10.1093/sexmed/qfad068
Huang TB, Yu JJ, Du YJ, Liu ZY. Novel treatment for post-orgasmic illness syndrome: a case report and literature review. Asian J Androl. 2021;24:332–4. https://doi.org/10.4103/aja202170
Odusanya BO, Pearce I, Modgil V. Post orgasmic illness syndrome: a review. Int J Impot Res. 2024. https://doi.org/10.1038/s41443-024-00860-3
Abdessater M, Elias S, Mikhael E, Alhammadi A, Beley S. Post orgasmic illness syndrome: what do we know till now? Basic Clin Androl. 2019;29:13. https://doi.org/10.1186/s12610-019-0093-7
Bolanos J, Morgentaler A. Successful treatment of post-orgasmic illness syndrome with human chorionic gonadotropin. Urol Case Rep. 2019;29:101078. https://doi.org/10.1016/j.eucr.2019.101078
McLean-Tooke A, Klinken E. Post-orgasmic illness syndrome successfully treated with omalizumab: a case report. J Sex Marital Ther. 2024;50:342–5. https://doi.org/10.1080/0092623X.2023.2295256
Shanholtzer A, Stephens JR, Lauter C, Peters KM. Post orgasmic illness syndrome successfully managed with antihistamine: a case report. Urol Case Rep. 2022;45:102189. https://doi.org/10.1016/j.eucr.2022.102189
Üstün B, Kennedy C. What is “functional impairment”? disentangling disability from clinical significance. World Psychiatry. 2009;8:82–5.
Mulhall J, King R, Glina S, Hvidsten K. Importance of and satisfaction with sex among men and women worldwide: results of the global better sex survey. J Sex Med. 2008;5:788–95. https://doi.org/10.1111/j.1743-6109.2007.00765.x
Goldstein I, Goren A, Li VW, Maculaitis MC, Tang WY, Hassan TA. The association of erectile dysfunction with productivity and absenteeism in eight countries globally. Int J Clin Pract. 2019;73:e13384. https://doi.org/10.1111/ijcp.13384
Paulos MR, Avelliino GJ. Post-orgasmic illness syndrome: history and current perspectives. Fertil Steril. 2020;113:13–5. https://doi.org/10.1016/j.fertnstert.2019.11.021
Stephenson KR, Meston CM. Heterosexual Women’s causal attributions regarding impairment in sexual function: factor structure and associations with well-being. Arch Sex Behav. 2016;45:1989–2001. https://doi.org/10.1007/s10508-016-0741-3
Fincham FD, Bradbury TN Relationship Attribution Measure. 1992. https://doi.org/10.1037/t01182-000.
Shimazu L, Stephenson KR, Meston CM Sexual dysfunction attributions scale. In: Handbook of sexuality-related measures. 4th ed. Rutledge Tayler & Francis Group; 2020. pp. 627-34.
Reisman Y. Clinical experience with Post-Orgasmic Illness Syndrome (POIS) patients—characteristics and possible treatment modality. Int J Impot Res. 2021;33:556–62. https://doi.org/10.1038/s41443-020-0314-9
Ueda P, Mercer CH, Ghaznavi C, Herbenick D. Trends in frequency of sexual activity and number of sexual partners among adults aged 18–44 years in the US, 2000–2018. JAMA Netw Open. 2020;3:e203833. https://doi.org/10.1001/jamanetworkopen.2020.3833
Shiri R, Koskimäki J, Tammela TLJ, Häkkinen J, Auvinen A, Hakama M. Bidirectional relationship between depression and erectile dysfunction. J Urol. 2007;177:669–73. https://doi.org/10.1016/j.juro.2006.09.030
Elterman DS, Bhattacharyya SK, Mafilios M, Woodward E, Nitschelm K, Burnett AL. The quality of life and economic burden of erectile dysfunction. Res Rep Urol. 2021;13:79–86. https://doi.org/10.2147/RRU.S283097
Jiann B, Su C, Tsai J. Is female sexual function related to the male partners’ erectile function? J Sex Med. 2013;10:420–9. https://doi.org/10.1111/j.1743-6109.2012.03007.x
Acknowledgements
The research team would like to thank the POIS patients for their participation in this project. We would also like to thank Dr. Julia Maietta for her consultation on this study and Drs. K. Stephenson. & C. M. Meston for developing the SDAS.
Author information
Authors and Affiliations
Contributions
LNM: helped develop study, RedCap survey, statistical analysis, lead author of manuscript, corresponding author. IB: designed study, received IRB approval, statistical analyses, edited manuscript. MC: helped draft manuscript and RedCap survey. CS: Helped draft manuscript. KR: helped to design research study. OJ: helped to design research study. DB: Helped with study design and acted as on call Psychiatrist. AJR: Co-PI and edited manuscript. RSR: Co-PI and edited manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study and its methods were conducted in accordance with all relevant guidelines and regulations set forth by the UMass Chan School of Medicine IRB Board and were approved by the UMass Chan School of Medicine IRB Board under Study Code: STUDY00001641.
Informed consent
Informed consent was obtained from all participants. No images were taken during this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maietta, L.N., Bronson, I., Cabral, M. et al. Post-orgasmic illness syndrome and its effects on self esteem and relationships: a survey. Int J Impot Res (2025). https://doi.org/10.1038/s41443-025-01103-9
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41443-025-01103-9
This article is cited by
-
Comment on Post-orgasmic illness syndrome and its effects on self esteem and relationships: a survey
International Journal of Impotence Research (2025)