Abstract
Gastrointestinal dysfunction (GID) may play a key role in Parkinson’s disease (PD) but its relationship with disease progression remains unclear. We recruited 404 PD cases, 37 iRBD (isolated REM Sleep Behaviour Disorder) and 105 controls. Participants completed the Gastrointestinal Dysfunction Scale for PD (GIDS-PD) and standardised disease severity assessments. Whole gut transit time (WGTT) was measured by ingestion of blue dye and recorded time to blue stools appearance (‘Blue Poop Challenge’) in a subset of PD cases. Gastrointestinal symptoms were more common and prevalent in iRBD and PD versus controls, and WGTT was significantly higher in PD versus controls. After adjustment for confounding factors, disease stage was not a significant predictor of GIDS-PD Constipation or Bowel Irritability scores. Longitudinal assessment of GIDS-PD scores and WGTT confirmed stability over a 4 year period. Bowel dysfunction may be a phenotypic feature in a subset of Parkinson’s with implications for patient stratification and management.
Similar content being viewed by others
Introduction
Although it is widely accepted that gastrointestinal (GI) symptoms are common in Parkinson’s disease (PD), there is a lack of information on how GI dysfunction (GID) changes over the disease course. Given that constipation has been identified as a risk factor for faster PD progression1 and a feature of a proposed PD subtype2, and that dysphagia and weight loss are associated with accelerated mortality3,4, it is important to identify how early in the disease process these symptoms begin, how prevalent they are and whether they are aggravated or ameliorated by disease severity and other factors such as medication and lifestyle.
Classically, constipation is thought to increase with Parkinson’s severity and studies have previously reported an association between increasing disease severity/duration and constipation but showed only modest correlations or did not present the strength of the association5,6. Furthermore, longitudinal studies of GID in PD7,8,9,10 have reported an increase in symptoms over time but most exhibit important methodological limitations such as small and heterogeneous clinical samples, the use of limited questions or general non-motor instruments to assess GID, and typically fail to account for relevant clinical and lifestyle factors such as medication, diet, water intake and exercise.
Moreover, most psychometric tools used to assess GID in PD have null or modest correlations with objective measures of GID11,12,13. Currently available objective measures of gut motility include magnetic resonance imaging14, scintigraphy15, radio opaque markers16 and wireless motility capsules17. These techniques are expensive, invasive and warrant in-person attendance at a specialised centre, requiring specialised equipment and staff, which prevents their widespread use in studies. The ingestion of blue dye, colloquially named ‘Blue Poop Challenge’ (BPC), is a safe, an inexpensive and scalable technique to measure whole gut transit time (WGTT), has been validated in a large cohort of healthy individuals and found to be the strongest marker of transit time compared to traditional psychometric transit time measures18. However, the BPC has not previously been employed to characterise WGTT in PD.
In this study, we used a PD-specific validated self-report questionnaire, the Gastrointestinal Dysfunction for Parkinson’s Disease Scale (GIDS-PD)19 to characterise the profile of gastrointestinal symptoms across PD stages, from RBD to late-stage disease, in order to better understand its heterogeneity, and assessed longitudinal change in GIDS-PD scores over time, adjusting for relevant clinical confounders. We also employed the BPC in PD to objectively assess gut transit time over the disease course.
Results
Demographic and clinical description of PD sample
A total of 404 people with PD (H&Y = 1, n = 77; H&Y = 2, n = 234; H&Y = 3, n = 57; H&Y = 4, n = 34; H&Y5 = 2), 37 people with iRBD and 72 controls participated in the study. A summary of demographic and clinical sample characteristics is presented in Table 1. When comparing across PD stages, there were no statistical differences in prevalence of iRBD history, diet, water intake and smoking. There were no differences in age, MoCA scores, opioid-based drugs and anticholinergic drugs, diet, water intake and smoking between the PD, iRBD and control groups. There were also no differences in self-reported GI diagnoses between groups except for constipation, with higher prevalences in the iRBD and PD compared to the control group. One iRBD participant was on a dopamine agonist for Restless Legs Syndrome. There was a statistically significant increase in age, disease duration, MDS-UPDRS scores, LEDD, opioid-based drugs and anticholinergic drugs across disease stage, whilst MoCA scores decreased, denoting worse disease severity across the H&Y stages.
GID symptoms across disease stage
Table 2 summarises individual and composite GIDS-PD scores across the groups. Unadjusted comparisons of GIDS-PD domain scores across the PD groups, stratified by H&Y stage, demonstrated a main effect of PD stage on GIDS-PD Constipation scores (H(3) = 36.714, p < 0.001), Bowel Irritability (H(3) = 11.402, p = 0.010) and Upper GI scores (H(3) = 50.580, p < 0.001). This indicates a general increase in self-reported GI symptoms in all domains with advancing disease stage (Fig. 1). Accordingly, we found a correlation between motor disease severity (MDS-UPDRS-III) and both GIDS-PD Constipation score (rho = 0.19, p < 0.001) and GIDS-PD Upper GI score (rho = 0.25, p < 0.0001).
GIDS-PD Constipation, Bowel Irritability and Upper GI scores were higher in the iRBD group and PD compared to controls, but not between PD and iRBD, suggesting that the GIDS-PD is sensitive to early GI dysfunction in prodromal states. Interestingly, the iRBD group also had higher GIDS-PD Constipation than early PD (H&Y = 1), but this significance was lost after Bonferroni correction. In terms of frequency of individual symptoms, hard stools and incomplete sense of evacuation were the most reported symptoms across groups (Table 2). Interestingly, difficulty swallowing was also common across groups, with a higher prevalence in iRBD cases compared to early PD (H&Y = 1) (Table 2).
In the PD group, participants with a positive RBD history prior to PD diagnosis had significantly higher GIDS-PD Constipation scores (9.4 ± 8.0) compared to those with a negative RBD history (7.0 ± 6.4; Mann–Whitney: U = 8013.0, p = 0.016).
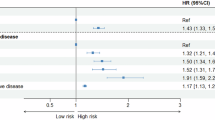
In the PD group, linear regression analysis was performed to further evaluate the effect of disease stage on gastrointestinal dysfunction with adjustment for relevant covariates. This showed that H&Y stage was predictive of GIDS-PD Upper GI scores but not GIDS-PD Constipation and Bowel irritability domain score (Table 3). Having a positive history of prodromal RBD was the strongest predictor of GIDS-PD Constipation scores. Exercising 3 times a week or more was also associated with decreased Constipation scores. Caffeine intake was associated with lower GIDS-PD Bowel Irritability scores and anticholinergic medication use was associated with higher Bowel Irritability scores. GIDS-PD Upper GI scores were associated with higher H&Y stage and use of anticholinergic medication. We also repeated regression analysis with MDS-UPDRS III instead of H&Y for all GIDS-PD subscores and confirmed our results, MDS-UPDRS scores were a significant predictor for GIDS-PD Upper GI scores but not Constipation or Bowel Irritability (Supplementary Table 1).
Because the prevalence of daily laxative use increased significantly across stages and including it as a covariate in the regression models would induce a bias (those with laxative use score higher in item GIDS-PD 1), we repeated the linear regression analysis for GIDS-PD constipation in participants who were not on regular laxatives (H&Y = 1, n = 67; H&Y = 2, n = 162; H&Y = 3, n = 27; H&Y = 4, n = 11) and observed similar results, with RBD prodromal history, but not H&Y and other variables, predicting GIDS-PD Constipation scores (F(6, 150) = 2.295, p = 0.038, R2 = 0.09).
Longitudinal characterisation of GI scores
A subset of participants completed the GIDS-PD longitudinally. 281 participants completed it twice, with an average interval of 1.6 (±0.7) years between timepoints. Of those, 144 participants completed it a third time, on average 2.8 (±0.9) years after visit 1 and 45 completed it a fourth time, on average 3.8 (±0.8) years after visit 1. Mixed-effects analysis showed a significant increase in PD motor severity (MDS-UPDRS-III) at each timepoint (score of 29.8, 33.8, 38.8 and 45.9 respectively; F(1.213, 132.6) = 39.32, p < 0.0001) as well as in Hoehn and Yahr stage (F(1.457, 192.3) = 27.43, p < 0.0001) and LEDD (328.3 mg, 550.0.mg, 631.8 mg and 777.9 mg respectively; (F(0.7315, 91.44) = 84.17, p < 0.0001). Mixed-effects models did not show significant differences in GIDS-PD scores between timepoints over an average of 4 years of follow-up (GIDS-PD Constipation, F(2.708, 412.6) = 2.142, p = 0.1009; GIDS-PD Bowel Irritability, F(2.668, 406.4) = 1.354, p = 0.2583; GIDS - PD Upper GI, F(2.864,433.4) = 0.3570, p = 0.7748, Mixed-effects models) (Fig. 2). Participants were then stratified according to PD duration (≤2.0 years from PD diagnosis at v1, n = 162; ≥2.01 years from PD diagnosis at v1, n = 119) to investigate whether longitudinal changes in GIDS-PD scores were more prominent in early or later disease. Mixed-effects models did not reveal significant differences in longitudinal GIDS-PD scores in either group (p > 0.2852).
No significant differences in GIDS-PD scores were observed over 4 visits spanning an average of 3-year follow-up in 245 PD participants (A–C) and over 2 year follow-up (D–F) in 25 RBD cases. GIDS-PD Gastrointestinal Dysfunction Scale–Parkinson’s disease, RBD REM Sleep Behaviour Disorder. Error bars represent SD.
A paired longitudinal analyses of 40 PD participants who were drug-naïve at baseline and started on dopaminergic medication at the subsequent follow-up visit (interval between visits 1.5 y ± 0.6), showed a significant decrease in bowel frequency scores (GIDS-PD item 1, W = 133, p = 0.0416), increase in straining (GIDS-PD item 2, W = 89.00, p = 0.0502) and no differences in dysphagia or gastric emptying scores (GIDS-PD item 9, p > 0.9999; GIDS-PD item 7, p = 0.07267, respectively) between the first and second visit.
25 iRBD cases completed the GIDS-PD longitudinally, after an average time interval of 1.1 (±0.1) years and 20 completed it a third time at 2.2 (±0.4) years follow-up. At the third time-point, 3 RBD participants had converted to PD and 1 to Lewy Body dementia. Mixed effects models did not show differences in GIDS-PD scores of iRBD participants between visits 1, 2 and 3 (0.4244 > F < 1.712, 0.5417 < p < 0.2026).
Objective measurement of GID
Ninety-six participants with PD and 54 paired household controls ingested a blue food dye to measure whole gut transit time (WGTT). Ten PD cases, but no controls, took laxatives in the days following the blue dye ingestion and were excluded from the analysis. Eighty-six participants were included in the analysis (H&Y = 1, n = 27; H&Y = 2, n = 42; H&Y = 3, n = 12; H&Y = 4, n = 5). None reported discomfort following dye ingestion. There were no differences in the interval between the last normal stool and food dye ingestion between PD (0.4 ± 0.4 h) and controls (0.3 ± 0.4 h) (W = −300 p = 0.9788, Wilcoxon). WGTT was significantly higher in PD cases (62.9 ± 43.4 h) compared to household controls (36.6 ± 26.4 h) (W = −993.0, p < 0.001, Wilcoxon) (Fig. 3A). Thirty-eight PD cases (44.1%) and 8 controls (14.8%) were above normative cut-off for slow transit time (≥59 h)20, with the longest transit time recorded at 240 h in the PD group, despite the participant reporting daily emptying of bowels. There were no differences in WGTT across H&Y stages (Kruskal–Wallis test, H(4) = 2.932, p = 0.4022) (Fig. 3B).
WGTT was significantly higher in PD cases compared to household controls (A). Within the PD cohort, there were no differences in WGTT across H&Y stages (B). Grid line depicts cut-off for delayed transit time (59 h). H&Y Hoehn and Yahr, PD Parkinson’s Disease, WGTT whole gut transit time. ****p ≤ 0.0001. Error bars represent SD.
Slower transit time was significantly correlated with higher GIDS-PD Constipation score (rho = 0.53, p < 0.001) and MDS-UPDRS constipation (item 1.1, rho = 0.32, p = 0.003), providing objective validation of the GIDS-PD as a tool to assess gut function in PD (Supplementary Fig. 1). WGTT correlated with age at visit (rho = 0.30, p = 0.005), LEDD (rho = 0.21, p = 0.049) and motor fluctuations (MDS-UPDRS Part IV, rho = 0.23, p = 0.036) but not with other MDS-UPDRS scores or other GIDS-PD scores. GIDS-PD constipation scores also were significantly associated with motor fluctuations (rho = 0.18, p = 0.036). There were no significant associations between WGTT and disease duration or cognitive scores. Partial correlations between WGTT and GIDS-PD Constipation scores withstood adjustment for age and LEDD (r = 0.31, p = 0.005). Between group comparison (Mann–Whitney U test) showed that PD patients with a high WGTT (≥59 h) had higher GIDS-PD Constipation scores compared to those with lower WGTT (p < 0.001), but no such differences were found for Upper GI subscores or abdominal fullness (GIDS-PD item 7), suggesting that the WGTT is more reflective of intestinal transit time rather than gastric emptying.
Discussion
In this study, we formally characterised self-reported gastrointestinal dysfunction across disease stages, using the GIDS-PD. Our findings indicate that GID is common even in the prodromal phase of the disease (in patients with RBD), and although the prevalence of most GI symptoms increases with disease stage, a subset of participants with advanced disease did not report symptoms, suggesting that GI dysfunction is not a universal feature of the disease. Following adjustment for covariates, upper GI dysfunction was significantly associated with disease stage. However, our data indicate that constipation is not driven by disease stage or motor severity but is better explained by other factors such as a positive history of RBD and lack of exercise. The concept that constipation is not associated with PD severity is supported by previous studies. Rodriguez-Blazquez21 did not find significant correlations with the gastrointestinal score and motor scores of the SCOPA-AUT or H&Y in a sample of 387 people with PD. Using the Parkinson’s Progression Markers Initiative database, Pagano et al.6, found a significant but weak correlation between constipation and MDS-UPDRS-III score after adjusting for age (r = 0.10, p = 0.037). In the same study, dopamine transporter imaging did not show significant correlations between constipation score and dopaminergic pathology, leading the authors to suggest that constipation may be due to an impairment of non-dopaminergic pathways. Accordingly, Dai et al.22 also found that constipation was associated with axial symptoms (r = 0.19, p = 0.012), which are considered to be non-dopaminergic. One current theory in the aetiology and progression of PD is the ‘Body-first versus Brain-first’ hypothesis, which associates iRBD with a peripheral nervous system involvement subtype, characterised by autonomic damage and gut symptomatology before involvement of the CNS dopaminergic system2. Our adjusted analysis of GIDS-PD Constipation scores supports this hypothesis as it suggests that constipation is not associated with disease severity but with prodromal RBD history.
Congruently, a high prevalence of GI symptoms in the iRBD cohort was also observed, equivalent to PD stages H&Y 1 and 2. In a multi-centre study, Ferini-Strambi et al.23 found high prevalence of GID in 318 iRBD cases with significant differences in constipation, straining and sialorrhoea compared to controls23. Aguirre-Mardones et al. also found high prevalence of constipation (52%) and straining (73%) in a sample of 44 iRBD cases24. These prevalence figures are in keeping with those found in this study. The higher prevalence of several GIDS-PD symptoms in the iRBD cohort compared to early PD cohort supports the hypothesis given that the iRBD group is likely composed of ‘body-first’ prodromal PD whereas the other PD groups are likely to include a combination of cases with ‘brain-first’ PD and ‘body-first’ PD. Moreover, when we stratified all PD participants together by RBD symptoms prior to PD diagnosis, those who were RBD positive had significantly higher GIDS-PD constipation scores and prodromal RBD was a strong predictor of GIDS-PD scores.
It is unlikely that the lower GIDS-PD Constipation scores in the early PD group compared to the iRBD group are explained by the introduction of dopaminergic medication. Dopaminergic medication has been consistently associated with an increase in constipation (e.g., decreased bowel frequency and increased gastrointestinal transit time)5,25,26,27,28,29, and our subanalysis of drug naïve PD cases showed a deterioration of constipation symptoms after PD medication introduction, confirming previous findings. Thus introduction of dopaminergic medication is unlikely to fully explain the drop in prevalence in early PD when compared to the iRBD. Of note, we also found an association between with motor fluctuations and both higher GIDS-PD constipation scores and higher WGTT, indicating that constipation may impact on symptom management, most likely through the inhibitive effect on levodopa absorption.
In keeping with the adjusted regression analysis for GIDS-PD Constipation, longitudinal analysis of GIDS-PD Constipation scores suggested minimal change over time. We also did not observe a significant increase in Bowel Irritability and Upper GI subscores over 4 years of follow-up. Constipation is typically thought to worsen with disease duration due to progression of PD pathology, but our data (cross-sectional regression analysis and longitudinal analysis of self-reported GI symptoms and WGTT) suggests that constipation is a feature of a subset of people with Parkinson’s. Our findings have important implications for patient stratification in clinical studies and clinical trials, as well as for the clinical management of gut symptoms in PD through allowing health teams to identify those at risk of constipation and promoting better understanding of protective factors.
It is possible that the lack of an observed association between constipation severity and disease stage is attributable to the increased prevalence of daily laxative intake in higher disease stages, however, the WGTT substudy only included participants that did not take laxatives and did not show increase in transit time across stages. Furthermore, linear regression analysis in the subset of people who did not take laxatives confirmed the main regression analysis findings, with prodromal RBD, but not H&Y, being the only significant predictor of GIDS-PD constipation score.
Only one other longitudinal study has found similar results to ours. Edwards et al.7 followed a small heterogenous sample of 56 PD cases (H&Y = 1–5) over 18 months and found an increase in frequency and severity of constipation, but not in sialorrhoea, dysphagia, heartburn, bloating or nausea as measured by their custom-made (unvalidated) GID survey. They also did not see a difference in total GI scores or the development of new GI symptoms over the follow-up period, which they attributed to a lack of significant change in PD severity and short follow-up period. Conversely, Stanković et al.10 followed 86 de novo PD cases and found that all SCOPA-AUT items regarding gastrointestinal dysfunction significantly increased over 3 years, except for dysphagia. Erro et al.9 followed 61 de-novo untreated PD cases and found that sialorrhoea, swallowing difficulties, nausea, weight loss and constipation, as measured by the Non-Motor Symptom Scale, increased significantly at a 4-year follow-up. However, no PD staging was available, and the follow-up included the introduction of dopaminergic medication which is known to worsen constipation5,25,26,27,28,29. It is thus possible that the discrepancies between previous studies and ours may be attributable to the fact that 211 of our 245 participants were already on dopaminergic medication at visit 1 thus minimising the dopaminergic effect seen in other studies, other sample characteristics (e.g. over-representation of a given subtype such as body-first PD), as well as the lack of adjustment for covariates in other studies. A key aspect of this study is that it highlights the importance of confounding factors on influencing the relationship between GID and disease stage. In addition to prodromal RBD, caffeine intake, and exercise were identified as factors associated with GIDS-PD scores. Exercise has previously been associated with improvement of constipation in PD30, a finding reinforced by our results, with important implications for self-management. Coffee intake was associated with less bowel irritability scores in keeping with studies which attribute a protective effect of caffeine to motor and non-motor symptoms of PD29,31 but which could also be attributable to avoidance behaviour, as people with bowel irritability tend to avoid caffeinated drinks. In our study, anticholinergic drug use was also associated with increased GIDS-PD Bowel Irritability and Upper GI scores, likely due to side-effects such as gastroesophageal reflux, nausea, vomiting, constipation, bloating, abdominal pain, and weight loss32,33,34.
In keeping with the findings of the GIDS-PD analyses, we did not find differences in transit time across H&Y stages, which supports the premise that constipation is a relatively stable feature in PD. Similarly, studies using radio opaque markers (ROMs) have reported differences between controls and PD cases but have not shown significant correlations with PD severity16,35,36. The average transit time in our study also corroborated previous literature using ROMs (89–108 h for PD cases)16,35,36. Importantly, the GIDS-PD Total and Constipation scores correlated significantly with WGTT, providing objective validation of the GIDS-PD as a tool to assess gut function in PD and outperforming correlation strength between other psychometric measures of constipation and ROMs11,12,13.
The presentation of difficulty in swallowing in iRBD is another interesting finding of this study. Dysphagia is classically considered to be a complication of advanced PD and there are few studies investigating its prevalence in early stages when it may be an indicator of an alternate diagnosis37. One study has reported dysphagia being present 2 years before PD diagnosis38. Similar to our results, Verbaan et al.39 noted a difficulty swallowing frequency of 34% in H&Y = 1 & 2 whilst Erro et al.9 observed a prevalence of 11.1% in early untreated PD cases. A study by Konings et al., which identified GI predictors of PD onset in a large US based nationwide medical record network, showed strong association between dysphagia and PD onset (RR 2.27, 95% CI 2.10–2.45)40. However, difficulty swallowing and/or dysphagia can be present in older populations without neurological disorders and partly attributed to factors such as age, medication and heartburn41,42.
Limitations of this study must be noted. In spite of its comprehensive nature, the GIDS-PD relies on self-report and it is therefore possible that GI symptom frequency and severity were under reported. However, the GID-PD Constipation subscore and WGTT showed a strong significant correlation suggesting that the GIDS-PD is a reliable instrument. Group characteristics were also an important limitation. The iRBD group was predominantly male (only 5% women) which might contribute to a lower observed frequency of GI symptoms as females are known to have higher prevalence of GID in the general population43,44. In the PD cohort, history of RBD was self-reported and not confirmed by PSG, as such iRBD history might be underreported as patients with mild severity of symptoms and/or who do not have a sleep partner are less likely to report it45. Lastly, the longitudinal follow-up of only 4 years provides limited information on how GI symptoms evolve over the disease course, however, we found a significant increase in UPDRS-III scores, H&Y as well as LEDD over this period thus the lack of progression in GID scores cannot not be attributed to lack of PD motor progression within this time frame. Future studies with larger sample sizes and longer follow-up period that adjust for relevant confounders will add to our understanding of GID across PD stages and its relationship with disease progression.
In conclusion, this study shows that gut dysfunction is common in PD and occurs from the earliest stages of the disease process (before the onset of motor symptoms) but is heterogeneous. GID is not a universal feature of PD, even in very late-stage disease, but rather occurs in a subset of cases. Cross-sectional and longitudinal analysis of both objective and self-reported measures of gut function suggest that constipation is not associated with disease severity and could thus represent a PD phenotype, whereas upper GI symptoms increase incrementally with disease stage. Moreover, our findings have important implications for patient stratification in clinical studies and clinical trials, as well as for the clinical management of gut symptoms in PD by allowing healthcare teams to identify those at risk of constipation and promoting engagement with protective factors (e.g., physical exercise).
Methods
Participants
This study was approved by the Cambridgeshire 3 Research Ethics Committee (08/H0306/26). PD and iRBD participants were recruited from the Cambridge Parkinson’s Disease Research Clinic and the Discovery Cohort study (Targeting the early pathological pathways in Parkinson’s Disease)46, respectively. All participants were approached when they came to their regular research appointment. PD cases met UK Parkinson’s Disease Society Brain Bank diagnostic criteria for idiopathic PD, and exclusion criteria included a diagnosis of dementia according to MDS criteria47 and the presence of other neurodegenerative disorders. iRBD cases were diagnosed by a sleep physician and confirmed by polysomnography. All iRBD patients had been reviewed by a neurologist to exclude phenoconversion to PD or related synucleinopathies using diagnostic criteria at the time of study48. Controls were spouses of iRBD and PD participants and the only exclusion criterion was the presence of neurodegenerative disorder. Written informed consent was obtained from all participants. Participants with gastrointestinal conditions were not excluded as the aim was to capture a comprehensive overview of GI symptoms in PD.
Data collection
Clinical assessments coincided with participant’s regular research appointments and were performed between December 2019 and April 2024 at the research clinic or as home visits for those with accessibility issues. Longitudinal assessments were conducted at 12 to 24 months intervals, according to the scheduling of their research clinic appointments. A trained clinician (neurologist/neuropsychologist) conducted clinical assessments. Participants were assessed using the MDS-UPDRS (during ‘on’ state if medicated for PD) and the Hoehn and Yahr (H&Y) scale. In people with PD, history of RBD symptoms prior to PD diagnosis was recorded via clinical assessment. Levodopa equivalent daily dose (LEDD) was calculated according to an adapted version of the Tomlinson formula49. Anticholinergic medication and opiate-based drug use was recorded. Anticholinergic burden was calculated using an online calculator adapted from Scottish Intercollegiate Guidelines Network (available at: https://www.acbcalc.com/). Montreal Cognitive Assessment (MoCA)50 was administered to assess cognitive function. Gastrointestinal symptoms were assessed with the GIDS-PD19, a Likert self-report scale composed of 12 items pertaining to 3 domains: Constipation (frequency of bowel movements, straining, hardness of stools, and incomplete evacuation), Bowel Irritability (abdominal pain, abnormal increase in stool passing, distension/bloating, and weight loss), and Upper GI symptoms (dysphagia, sialorrhea, heartburn, and nausea). Supplementary items 1a (measures taken to increase bowel movement frequency), 1b (duration of constipation), A (diet), B (water intake), C (caffeinated drinks intake), D (exercise), E (smoking), and F (medical diagnosis of GID) are not used for scoring but provide important additional information.
Gut transit time was measured as the length of time, in hours, between ingestion of a blue food dye (PME© sky blue) and first appearance of blue stool18 (Blue Poop Challenge). Participants were asked to ingest 20 drops of dye (approximately 1 mL), mixed with a liquid of their choice, within 2 h of their last defecation. Its ingredients are considered safe for human consumption51,52. Participants were asked to avoid laxatives after ingesting the blue food dye and when this was not possible due to discomfort, laxative use was annotated and the participant excluded from analysis. The BPC was performed only once per participant.
Data analysis
Data analyses were performed using SPSS version 29.0 and Graphpad Prism version 9. Results are presented as mean ± standard deviation (SD). All analyses were two-tailed, with significance considered at p < 0.05 for unadjusted comparisons. Any missing item on the GIDS-PD invalidated its total score and domain scores. Shapiro–Wilk’s test did not confirm distribution normality for continuous variables therefore Kruskal–Wallis or Wilcoxon signed-rank tests were used for between-group comparisons of continuous variables, as appropriate, and Chi-square (χ2) analysis were used for comparisons of dichotomous variables. Bonferroni correction for multiple tests were used for pairwise comparisons. Spearman’s correlation coefficient was used to correlate GIDS-PD scores with other clinical measures and WGTT. A base linear regression model was created to assess the predictive role of age, sex and H&Y stage on GIDS-PD domain scores (model 1). Then, a backward stepwise approach was used until best model fit was achieved. Covariates included age at visit, sex, medication use (LEDD, opioids, anticholinergics), history of prodromal RBD and relevant lifestyle variables (diet, water intake, smoking and exercise level).
Data availability
Anonymized data are available upon reasonable request by any qualified investigator.
References
Camacho, M. et al. Early constipation predicts faster dementia onset in Parkinson’s disease. NPJ Parkinsons Dis. 7, https://doi.org/10.1038/s41531-021-00191-w (2021).
Borghammer, P. & Van Den Berge, N. Brain-first versus gut-first Parkinson’s disease: a hypothesis. J. Parkinsons Dis. 9, S281–S295 (2019).
Cersosimo, M. G. et al. Weight loss in Parkinson’s disease: the relationship with motor symptoms and disease progression. Biomed. Res. Int. 2018, 1–7 (2018).
Dilmaghani, S. et al. Severity of dysphagia is associated with hospitalizations and mortality in patients with Parkinson’s disease. Neurogastroenterol. Motil. 34, https://doi.org/10.1111/nmo.14280 (2022).
Krogh, K., Ostergaard, K., Sabroe, S. & Laurberg, S. Clinical aspects of bowel symptoms in Parkinson’s disease. Acta Neurol. Scand. 117, 60–64 (2008).
Pagano, G. et al. Constipation is not associated with dopamine transporter pathology in early drug-naïve patients with Parkinson’s disease. Eur. J. Neurol. 25, 307–312 (2018).
Edwards, L., Quigley, E. M. M., Hofman, R. & Pfeiffer, R. F. Gastrointestinal symptoms in Parkinson disease: 18-month follow-up study. Mov. Disord. 8, 83–86 (1993).
Yong, V. W. et al. Progressive and accelerated weight and body fat loss in Parkinson’s disease: a three-year prospective longitudinal study. Parkinsonism Relat. Disord. 77, 28–35 (2020).
Erro, R. et al. The non-motor side of the honeymoon period of Parkinson’s disease and its relationship with quality of life: a 4-year longitudinal study. Eur. J. Neurol. 23, 1673–1679 (2016).
Stanković, I. et al. Longitudinal assessment of autonomic dysfunction in early Parkinson’s disease. Parkinsonism Relat. Disord. 66, 74–79 (2019).
Knudsen, K. et al. Objective colonic dysfunction is far more prevalent than subjective constipation in Parkinson’s disease: a colon transit and volume study. J. Parkinsons Dis. 7, 359–367 (2017).
Grønlund, D. et al. Comparison of subjective and objective measures of constipation—employing a new method for categorizing gastrointestinal symptoms. J. Pharm. Toxicol. Methods 94, 23–28 (2018).
De Pablo-Fernández, E., Passananti, V., Zárate-López, N., Emmanuel, A. & Warner, T. Colonic transit, high-resolution anorectal manometry and MRI defecography study of constipation in Parkinson’s disease. Parkinsonism Relat. Disord. 66, 195–201 (2019).
Willis, D. et al. A novel method for measuring bowel motility and velocity with dynamic magnetic resonance imaging in two and three dimensions. NMR Biomed. 35, 1–13 (2022).
Borghammer, P., Knudsen, K., Fedorova, T. D. & Brooks, D. J. Imaging Parkinson’s disease below the neck. NPJ Parkinsons Dis. 3, https://doi.org/10.1038/s41531-017-0017-1 (2017).
Knudsen, K., Krogh, K., Østergaard, K. & Borghammer, P. Constipation in parkinson’s disease: subjective symptoms, objective markers, and new perspectives. Mov. Disord. 32, 94–105 (2017).
Su, A., Gandhy, R., Barlow, C. & Triadafilopoulos, G. Utility of the wireless motility capsule and lactulose breath testing in the evaluation of patients with Parkinson’s disease who present with functional gastrointestinal symptoms. BMJ Open Gastroenterol. 4, https://doi.org/10.1136/bmjgast-2017-000132 (2017).
Asnicar, F. et al. Blue poo: impact of gut transit time on the gut microbiome using a novel marker. Gut 70, 1665–1674 (2021).
Camacho, M., Greenland, J. C. & Williams-Gray, C. H. The Gastrointestinal Dysfunction Scale for Parkinsonas disease. Mov. Disord. 36, 2358–2366 (2021).
Nandhra, G. K. et al. Normative values for region-specific colonic and gastrointestinal transit times in 111 healthy volunteers using the 3D-Transit electromagnet tracking system: influence of age, gender, and body mass index. Neurogastroenterol. Motil. 32, https://doi.org/10.1111/nmo.13734 (2020).
Rodriguez-Blazquez, C., Forjaz, M. J., Frades-Payo, B., De Pedro-Cuesta, J. & Martinez-Martin, P. Independent validation of the scales for outcomes in Parkinson’s disease-autonomic (SCOPA-AUT). Eur. J. Neurol. 17, 194–201 (2010).
Dai, Y. et al. Correlations between constipation and the axial symptoms, related motor symptoms in Parkinson’s disease. Zhonghua Yi Xue Za Zhi 96, 324–328 (2016).
Ferini-Strambi, L. et al. Autonomic symptoms in idiopathic REM behavior disorder: a multicentre case-control study. J. Neurol. 261, 1112–1118 (2014).
Aguirre-Mardones, C. et al. Prevalence and timeline of nonmotor symptoms in idiopathic rapid eye movement sleep behavior disorder. J. Neurol. 262, 1568–1578 (2015).
Müller, B. et al. Autonomic symptoms and dopaminergic treatment in de novo Parkinson’s disease. Acta Neurol. Scand. 127, 290–294 (2013).
Pagano, G., Tan, E. E., Haider, J. M., Bautista, A. & Tagliati, M. Constipation is reduced by beta-blockers and increased by dopaminergic medications in Parkinson’s disease. Parkinsonism Relat. Disord. 21, 120–125 (2015).
Hauser, R. A. et al. Randomized double-blind multicenter evaluation of pramipexole extended release once. Mov. Disord. 25, 2542–2549 (2010).
Liu, C. Z. et al. Rasagiline, an inhibitor of MAO-B, decreases colonic motility through elevating colonic dopamine content. Neurogastroenterol. Motil. 30, https://doi.org/10.1111/nmo.13390 (2018).
Kenna, J. E. et al. Characterization of gastrointestinal symptom type and severity in Parkinson’s disease: a case–control study in an Australian cohort. Mov. Disord. Clin. Pract. 1–9, https://doi.org/10.1002/mds.28675 (2020).
Gan, J. et al. A survey of subjective constipation in Parkinson’s disease patients in shanghai and literature review. BMC Neurol. 18, https://doi.org/10.1186/s12883-018-1034-3 (2018).
Prediger, R. D. S. Effects of caffeine in Parkinson’s disease: from neuroprotection to the management of motor and non-motor symptoms. J. Alzheimers Dis. 20, https://doi.org/10.3233/JAD-2010-091459 (2010).
Collamati, A. et al. Anticholinergic drugs and negative outcomes in the older population: from biological plausibility to clinical evidence. Aging Clin. Exp. Res. 28, 25–35 (2016).
Mungan, Z. & Şimşek, B. P. Which drugs are risk factors for the development of gastroesophageal reflux disease? Turk. J. Gastroenterol. 28, S38–S43 (2017).
Rodríguez-Ramallo, H. et al. Association between anticholinergic burden and constipation: a systematic review. Healthcare 9, https://doi.org/10.3390/healthcare9050581 (2021).
Jost, W. H. & Schimrigk, K. Constipation in Parkinson’s disease. Wien. Klin. Wochenschr. 69, 906–909 (1991).
Jost, W. H. & S. B. Defecatory disorders in de novo Parkinsonians-colonic transit and electromyogram of the external anal sphincter. Wien. Klin. Wochenschr. 110, 535–537 (1998).
Postuma, R. B. et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov. Disord. 30, 1591–1601 (2015).
Noyce, A. J. et al. Severe dysphagia as a presentation of Parkinson’s disease. Mov. Disord. 27, 457–458 (2012).
Verbaan, D. et al. Patient-reported autonomic symptoms in Parkinson disease. Neurology. 69, 333–341(2007).
Konings, B. et al. Gastrointestinal syndromes preceding a diagnosis of Parkinson’s disease: testing Braak’s hypothesis using a nationwide database for comparison with Alzheimer’s disease and cerebrovascular diseases. Gut 72, 2103–2111 (2023).
Wolf, U. et al. Prevalence of oropharyngeal dysphagia in geriatric patients and real-life associations with diseases and drugs. Sci. Rep. 11, https://doi.org/10.1038/s41598-021-99858-w (2021).
Cho, S. Y. et al. Prevalence and risk factors for dysphagia: a USA community study. Neurogastroenterol. Motil. 27, 212–219 (2015).
Freire, A. C., Basit, A. W., Choudhary, R., Piong, C. W. & Merchant, H. A. Does sex matter? the influence of gender on gastrointestinal physiology and drug delivery. Int. J. Pharm. 415, 15–28 (2011).
Gonenne, J. et al. Effect of female sex hormone supplementation and withdrawal on gastrointestinal and colonic transit in postmenopausal women. Neurogastroenterol. Motil. 18, 911–918 (2006).
Eisensehr, I., Lindeiner, H. V., Jager, M. & Noachtar, S. N. REM sleep behavior disorder in sleep-disordered patients with versus without Parkinson’s disease: is there a need for polysomnography?. J. Neurol. Sci. 186, 7–11 (2001).
Szewczyk-Krolikowski, K. et al. The influence of age and gender on motor and non-motor features of early Parkinson’s disease: initial findings from the Oxford Parkinson Disease Center (OPDC) discovery cohort. Parkinsonism Relat. Disord. 20, 99–105 (2014).
Dubois, B. et al. Diagnostic procedures for Parkinson’s disease dementia: recommendations from the Movement Disorder Society Task Force. Mov. Disord. 22, 2314–2324 (2007).
Barber, T. R. et al. Prodromal parkinsonism and neurodegenerative risk stratification in rem sleep behavior disorder. Sleep 40, https://doi.org/10.1093/sleep/zsx071 (2017).
Tomlinson, C. L. et al. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov. Disord. 25, 2649–2653 (2010).
Nasreddine, Z. S. et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 53, 695–699 (2005).
Bensoltane, S., Bouzbid, S. D. & Adjabi, S. Food additive evidence in food supplements most commonly consumed by cancer patients. J. Bioresour. Manag. 10, http://corescholar.libraries.wright.edu/jbm (2023).
Younes, M. et al. Follow-up of the re-evaluation of glycerol (E 422) as a food additive. EFSA J. 20, https://doi.org/10.2903/j.efsa.2022.7353 (2022).
Acknowledgements
The authors thank all the participants for their involvement in this study. M.C. and J.C.G. are supported by Cambridge Centre for Parkinson-Plus, and M.C. received funding for this work from the Evelyn Trust. C.H.W.G. is supported by the Medical Research Council (MR/W029235/1) and the NIHR Cambridge Biomedical Research Centre (NIHR203312). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. K.M.S. was supported by a PhD fellowship from the Wellcome trust (106565/Z/14/Z) and a postdoctoral fellowship from the Guarantors of Brain, and is currently an employee of AstraZeneca. C.D. received funding from the National Institute for Health and Care Research, Addenbrooke’s Charitable Trust, Association of British Neurologists, and Patrick Berthoud Charitable Trust. M.H. received funding from Parkinson’s UK, National Institute for Health Research Oxford Biomedical Research Centre (BRC) and Cure Parkinson’s Trust. For the purpose of Open Access, the author has applied a Creative Commons Attribution (CC BY) licence to any Author Accepted Manuscript version arising from this submission.
Author information
Authors and Affiliations
Contributions
M.C. conceived the study, collected data and performed the statistical analysis. C.H.W.G. assisted with study conception and establishing and supervising the study. J.C.G., C.D., K.M.S., B.P., D.A., J.R., M.O. and M.T.H. assisted with data collection and execution of the project. M.C. wrote the first draft of the manuscript that was critically read, revised, and approved by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Camacho, M., Greenland, J.C., Daruwalla, C. et al. The profile of gastrointestinal dysfunction in prodromal to late-stage Parkinson’s disease. npj Parkinsons Dis. 11, 123 (2025). https://doi.org/10.1038/s41531-025-00900-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41531-025-00900-9
This article is cited by
-
Influence of autonomic dysfunction on sleep disturbance in drug-naïve patients with Parkinson’s disease
Neurological Sciences (2026)