Abstract
There is increasing evidence that sex hormones may impact the development of obstructive lung disease (OLD). Therefore, we studied the effect of bilateral oophorectomy (oophorectomy) on the development of OLD. Women were identified from the Mayo Clinic Cohort Study of Oophorectomy and Aging-2. Data were collected using the Rochester Epidemiology Project records-linkage system. A total of 1653 women who underwent oophorectomy and 1653 referent women of similar age were assessed for OLD using diagnostic codes and medical record abstraction. Women who underwent oophorectomy had an overall higher risk of all OLD, all chronic obstructive pulmonary disease (COPD), emphysema, and chronic bronchitis but not of all asthma, confirmed asthma, or confirmed COPD. The association with all OLD was stronger in women who were age ≤45 years at oophorectomy, never smokers, non-obese, and in women with benign indications; however, the interactions were not statistically significant. There was an increased risk of all asthma in women age ≤45 years at oophorectomy who took estrogen therapy. Never smokers of all ages had a stronger association of oophorectomy with all asthma and all COPD, whereas smokers had a stronger association of oophorectomy with emphysema and chronic bronchitis. Non-obese women of all ages had a stronger association of oophorectomy with all COPD, emphysema, and chronic bronchitis. The results of this study combined with the increased risk of several chronic diseases reported in previous studies suggest that oophorectomy in premenopausal women should be avoided unless there is clear evidence of a high genetic risk of ovarian cancer.
Similar content being viewed by others
Introduction
It is now apparent that some diseases affect women disproportionately more than men. Although behavioral and environmental factors play important roles in the development of obstructive lung disease (OLD), the potential role of sex-specific factors is only partially understood1,2,3,4,5.
There is abundant evidence implicating sex hormones in the pathophysiology of asthma in women. Asthma has a bimodal age distribution, affecting males predominately in childhood and women predominately after puberty. Prevalence of severe asthma and healthcare utilization rises in women as age increases until reaching menopause6. Among women with asthma, the forced expiratory volume at 1 s (FEV1) and diffusing capacity for carbon monoxide vary during the menstrual cycle. Lung function dips in the luteal phase when there is a peak in both estrogen and progesterone7,8. In this premenstrual phase, one-third of women with asthma also experience worsening of their respiratory symptoms that appear to be partially reversed by contraceptive use9,10. Furthermore, early menarche has been associated with increased risk of asthma11.
In addition, there are sex differences in chronic obstructive pulmonary disease (COPD). The National Health Interview Survey described a higher self-reported prevalence of COPD in women than in men12. In addition, the National Health and Nutrition Examination Survey (NHANES) I and III studies further demonstrated that the mortality associated with COPD is higher in men but is declining over time more rapidly in men, narrowing the mortality gap between sexes13. Changes in smoking trends may influence these differences, but the NHANES III study also demonstrated that 80% of non-smokers with COPD were women14. Among smokers, women have increased susceptibility with more rapid FEV1 and computed tomography (CT) density decline than their male counterparts15,16,17. In addition, women have higher reported disease burden, depression, and worse quality of life18.
Female reproductive hormones, namely estrogen and progesterone, influence lung function as women advance in their reproductive lifespan. Estradiol is the major active estrogen form in humans, and binds to estrogen receptors that are broadly distributed in many cell types in the lung5. Activation of these receptors can modulate immune cells and airway structural functions in complex ways.
Progesterone modulates airway function as well. Progesterone receptors are present on cilia of airway epithelial cells, and their activation decreases cilia beat frequency. Progesterone level is the highest in the luteal phase, when lung function has been found to be the lowest in menstruating women with asthma7.
Menopause marks the end of reproduction due to ovarian follicular depletion. Bilateral oophorectomy (oophorectomy) with or without concurrent hysterectomy may cause premature or early menopause which may lead to symptoms necessitating the use of hormonal replacement therapy, primarily estrogen therapy19. The effects of menopause on lung function and on predisposition to asthma and COPD are not well defined. Some studies have suggested that there is a decreased risk of asthma after spontaneous menopause, and reversal with hormone replacement therapy20,21,22,23. Furthermore, although some studies found that menopause was associated with higher FEV1, forced vital capacity (FVC), and FEV1/FVC24, other studies suggested that menopause was associated with worsened symptoms and worsened FEV1 and FVC25,26.
To further investigate the effects of sex hormones on lung pathology, we studied the effect of bilateral oophorectomy on the development of OLD using a population-based cohort study design.
Methods
Study population
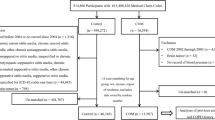
Women were identified as part of the Mayo Clinic Cohort Study of Oophorectomy and Aging-2 (MOA-2)27,28,29, and data were collected using the Rochester Epidemiology Project medical records-linkage system. The system links outpatient and inpatient medical records from all medical care providers in Olmsted County, Minnesota30,31,32,33. The study included all premenopausal women who underwent bilateral oophorectomy or second unilateral oophorectomy for a nonmalignant indication before age 50 years (n = 1653), between 1 January 1988 and 31 December 2007 in Olmsted County, Minnesota. Simple random sampling was used to match each woman to a referent woman born in the same year (±1) who had not undergone bilateral oophorectomy or second unilateral oophorectomy before index date. For each pair, index date was the date of oophorectomy.
Ethics
Women were not contacted directly as part of the study; therefore, written informed consent was not required. However, women were excluded if they did not authorize the use of their medical record for research (only 2.5% of women in the overall population)33. Research activities were approved by both the Mayo Clinic and the Olmsted Medical Center Review Boards.
Assessment of characteristics at index date
Chronic conditions present at index date were electronically abstracted using the International Classification of Diseases diagnostic codes assigned to each woman before index date. We used the diagnostic codes recommended by the U.S. Department of Health and Human Services to define the following 15 chronic conditions: depression, substance abuse disorders, dementia, schizophrenia or psychosis, hyperlipidemia, hypertension, diabetes (both type 1 and type 2), cardiac arrhythmias, coronary artery disease, stroke, congestive heart failure, arthritis, cancer, osteoporosis, and chronic kidney disease34,35. Anxiety was added to the list because it was common in our population and was considered related to the aging process. By contrast, three additional chronic conditions were excluded from the list because they were uncommon in the study population (autism spectrum disorder, human immunodeficiency virus, and hepatitis). Finally, two additional chronic conditions were excluded because they were the outcomes of this study (asthma and COPD). In total, the study considered 16 chronic conditions. Each condition required two or more corresponding diagnostic codes separated by >30 days. Demographic information, clinical characteristics, surgical indication, and use of estrogen therapy were manually abstracted from the medical records in the Rochester Epidemiology Project by a nurse or by a physician (L.G.R.). Income at the census block group level was derived from U.S. Census data.
Assessment of OLD and diagnostic criteria
The outcome of interest in this cohort study was OLD and included asthma and COPD. All diagnostic codes defined by the U.S. Department of Health and Human Services for asthma and COPD assigned at any time before or after index date through December 31, 2018 were obtained from the electronic indexes of the Rochester Epidemiology Project (Supplementary Table 1). To avoid false positives, subjects were required to meet specific screening criteria. We required one or more codes for asthma, COPD, or emphysema, and two or more codes separated by >90 days and <1 year for chronic bronchitis. Women who met the screening criteria before index date were considered as prevalent OLD and were excluded from all analyses. The medical records for all remaining women who met the screening criteria on or after index date were abstracted by a physician (T.T.N.) to confirm the presence of OLD and to determine specific type, date of onset, and other characteristics. We excluded women for whom medical record abstraction revealed that the date of onset was before index date (prevalent OLD).
All available pulmonary function tests (PFT) were independently reviewed by a physician (T.T.N.) and interpreted based on current guidelines. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2019 guideline was used to define fixed obstruction for the diagnosis of confirmed COPD. The Global Initiative for Asthma (GINA) 2019 guideline was used to define variable obstruction for the diagnosis of confirmed asthma. Chest CT reports interpreted by a radiologist were additionally used to determine parenchymal abnormalities, including emphysema. We used these criteria to categorize the type of OLD (Table 1). Women could have more than one type of OLD to account for potential disease overlap36.
We considered all types of OLD combined, including confirmed asthma, probable asthma, possible asthma, confirmed COPD, probable COPD, emphysema without airflow limitation, emphysema without PFT, undifferentiated OLD, chronic bronchitis, and other OLD. We also considered specific types for all asthma (confirmed, probable, and possible), confirmed asthma, all COPD (confirmed, probable, and emphysema), confirmed COPD, emphysema (without airflow limitation and without PFT), and chronic bronchitis (Table 1).
Statistical analysis
Women were followed from their index date until the date of OLD (combined or specific type), death, last visit with a care provider in the Rochester Epidemiology Project, or the end of the study (December 31, 2018). The oophorectomy and referent cohorts were balanced at baseline using inverse probability weights derived from a logistic regression model including several characteristics at baseline: 16 chronic conditions (list provided above), years of education (≤12, 13–16, and >16), household income quartiles (<$42,000, $42,000–56,999, $57,000–71,999, ≥$72,000), race (white vs. nonwhite), body mass index (BMI; ≥ 30 kg/m2 vs. <30), cigarette smoking (current or former vs. never), age at index date (continuous), and calendar year (continuous). The inverse probability weights were calculated separately within each stratum to maximize the balance of the characteristics. After balancing using inverse probability weights, the standardized differences for all of the characteristics considered were below the recommended threshold of 0.10 (i.e., negligible imbalance between the two cohorts; data not shown).
Cox proportional hazards models were used to estimate hazard ratios (HRs) and 95% CIs with age as the time scale, and with each woman entering the risk set at her respective age at index date. The Cox models used robust sandwich covariance estimates to account for the inclusion of women in both cohorts (referent women who underwent subsequent bilateral oophorectomy) and for the use of estimated weights. The proportional hazards assumption was tested using graphical methods and adding time-dependent covariates to the models, and was met for all models. Cumulative incidence curves were estimated using the Kaplan-Meier method and included inverse probability weighting. Differences between the oophorectomy and referent cohorts were also measured using absolute risk increase (ARI) or reduction, calculated by subtracting the two absolute risks at 25 years after index date.
Analyses were performed for all women overall and separately within strata by age at oophorectomy (≤45 and 46–49 y), by estrogen therapy within each age group, by surgical indication, by smoking status (current or former vs. never), and by obesity (BMI ≥ 30 vs. <30 kg/m2). Stratification by age at oophorectomy, estrogen therapy, and surgical indication was based on the status of the woman who underwent oophorectomy in each pair. By contrast, stratification by smoking and obesity was based on the status for each woman separately (e.g., never smokers who underwent oophorectomy were compared with never smoker referent women). We also performed two sets of sensitivity analyses to (1) censor referent women at the time of bilateral oophorectomy if it was performed after index date, and (2) exclude women with any of the 16 chronic conditions at index date. Tests of statistical significance were conducted at the two-tailed alpha level of 0.05. Analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, NC).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Results
Characteristics at index date
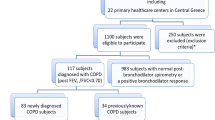
A total of 1653 women who underwent oophorectomy and 1653 referent women of similar age were assessed for OLD using diagnostic codes and medical record abstraction (Supplementary Fig. 1). A total of 317 (19.2%) women who underwent oophorectomy and 218 (13.2%) referent women had prevalent OLD before index date and were excluded from all analyses. In a case-control analysis at baseline, oophorectomy was associated with OLD before index date (odds ratio, 1.41; 95% CI, 1.15–1.73; P = 0.001; adjusted for the variables included in the inverse probability weights).
Table 2 shows the baseline characteristics for the 1336 women who underwent oophorectomy and 1435 referent women included in analyses for OLD outcomes. Women in the oophorectomy group were more frequently white, had higher BMI, and had more chronic conditions at index date. Most women (89.8%) underwent hysterectomy concurrent with oophorectomy.
Follow-up and menopause characteristics
Supplementary Table 2 shows the follow-up characteristics and details about menopause in the oophorectomy and referent cohorts. The median length of follow-up was similar in the two cohorts. The median age at menopause was 44.0 years (interquartile range [IQR], 40.0–47.0) in women with oophorectomy and 50.0 years (IQR, 46.5–52.0) in referent women. Only 36% of the referent women who reached menopause received estrogen therapy.
Over a median of 18.6 years of follow-up (IQR 14.2–23.5), 214 women who underwent oophorectomy and 164 referent women developed de novo OLD (Supplementary Fig. 1). Supplementary Table 3 shows the clinical characteristics of women who developed any type of asthma (confirmed, probable, or possible) and any type of COPD (confirmed, probable, or emphysema). The age at asthma onset was similar between women who underwent oophorectomy (median, 51 y; IQR, 45–56) and referent women (median, 50 y; IQR, 45–56). However, women who underwent oophorectomy developed COPD at a younger age (median, 54 y; IQR, 52–59) compared with referent women (median, 60 y; IQR, 53–63). FEV1 and FVC from the earliest PFT with variable obstruction were similar for both groups of women with de novo asthma. Among women with de novo COPD, the FEV1 and FVC measurements were lower for referent women, possibly due to their older age at onset of COPD (Supplementary Table 3).
Cohort study analyses
The results for all OLD outcomes and for specific types of OLD after oophorectomy or index date are shown in Tables 3 and 4 and Supplementary Table 4. Women who underwent oophorectomy had an overall higher risk of all OLD (HR, 1.31; 95% CI, 1.07–1.61; ARI, 5.7%), all COPD (HR, 1.57; 95% CI, 1.04–2.36; ARI, 2.6%), emphysema (HR, 2.13; 95% CI, 1.18–3.85; ARI, 2.4%), and chronic bronchitis (HR, 1.77; 95% CI, 1.18–2.67; ARI, 2.8%) compared to referent women; but no significant difference in risk for all asthma, confirmed asthma, or confirmed COPD (Fig. 1). There was a stronger association of oophorectomy with all OLD among women aged ≤45 years at oophorectomy (overall and in those with estrogen therapy), women with benign ovarian indications, never smokers, and non-obese women. However, the interactions by age at oophorectomy, estrogen therapy, surgical indication, smoking status, and obesity were not statistically significant (Table 3 and Supplementary Fig. 2).
a All OLD; b, all asthma; c, all COPD; d, chronic bronchitis. The curves were weighted using inverse probability weights derived from a logistic regression model including 16 chronic conditions present at index, years of education, quartiles of household income, race, body mass index, cigarette smoking, and age and calendar year at index date (details provided in text). COPD chronic obstructive pulmonary disease, HR hazard ratio, OLD obstructive lung disease.
The results for all asthma and all COPD outcomes after oophorectomy are shown in Table 3 and in Figs. 2 and 3. Although there was a stronger association of oophorectomy with all asthma for women who took estrogen therapy after oophorectomy in the ≤45 years age group, the interaction by age at oophorectomy was not significant. However, the interaction by smoking status was significant (P = 0.03), with an increased risk observed in never smokers who underwent oophorectomy compared to never smokers in the referent cohort (HR, 1.47; 95% CI, 1.01–2.12; ARI, 6.0%). There was no significant association in the smoking stratum (Fig. 2). The association of oophorectomy with all COPD was stronger for women aged ≤45 years at oophorectomy (HR, 1.88; 95% CI, 1.09–3.25; 95% CI, ARI, 4.4%), for never smokers (HR, 10.4; 95% CI, 1.28–84.6; ARI, 1.9%), and for non-obese women (HR, 1.94; 95% CI, 1.16–3.24; ARI, 3.6%); however, there were no significant interactions for any of the stratified analyses (Fig. 3).
a, b Strata by age at oophorectomy; c, d strata by surgical indication; e, f strata by smoking status; g, h strata by body mass index at index date. The curves were weighted using inverse probability weights derived from a logistic regression model including 16 chronic conditions present at index, years of education, quartiles of household income, race, body mass index, cigarette smoking, and age and calendar year at index date (details provided in text). The interaction was significant by smoking status (P = 0.03), but not by age at oophorectomy, surgical indication, or by body mass index. BMI body mass index, HR hazard ratio.
a, b Strata by age at oophorectomy; c, d strata by surgical indication; e, f strata by smoking status; g, h strata by body mass index at index date. The curves were weighted using inverse probability weights derived from a logistic regression model including 16 chronic conditions present at index, years of education, quartiles of household income, race, body mass index, cigarette smoking, and age and calendar year at index date (details provided in text). The interactions were not significant by age at oophorectomy, surgical indication, smoking status, or by body mass index. BMI body mass index, HR hazard ratio.
The results for confirmed asthma and confirmed COPD outcomes after oophorectomy are shown in Supplementary Table 4. There was no association of oophorectomy with confirmed asthma, but there was an association with confirmed COPD among never smokers (HR, 9.45, 95% CI, 1.14–78.2, ARI, 1.7%), and the interaction by smoking status was significant (P = 0.04).
The results for emphysema and chronic bronchitis outcomes after oophorectomy are shown in Table 4. Within the smoking stratum there was a stronger association of oophorectomy with emphysema (HR, 2.17, 95% CI, 1.21–3.92, ARI, 5.4%) and with chronic bronchitis (HR, 2.09, 95% CI, 1.23–3.54, ARI, 5.3%). Non-obese women had a stronger association of oophorectomy with emphysema (HR, 2.19; 95% CI, 1.04–4.64; ARI, 3.0%) and with chronic bronchitis (HR, 2.21; 95% CI, 1.23–3.98; ARI, 2.5%). However, the interactions by smoking or obesity were not significant (Table 4).
Sensitivity analyses
In the first set of sensitivity analyses, referent women who underwent bilateral oophorectomy after index date were censored at the date of oophorectomy. In the second set of sensitivity analyses, we considered the risk of de novo OLD within the subset of women with none of the 16 chronic conditions at index date (702 women who underwent oophorectomy and 925 referent women). The results from both sets of sensitivity analyses were virtually the same as the results from the primary analyses (data not shown).
Discussion
In this population-based cohort study, we evaluated the impact of bilateral oophorectomy on the risk of OLD. We found an overall higher risk of all OLD, all COPD, emphysema, and chronic bronchitis. The increased risk of all OLD was not explained by smoking status or by obesity. Indeed, there was a stronger association of oophorectomy with all OLD in never smokers and in non-obese women. We suggest that smoking and obesity may be stronger risk factors for OLD than oophorectomy. Therefore, the effect of oophorectomy becomes detectable only in women without these stronger risk factors. An increased risk for asthma was observed only in women ≤45 years who took estrogen therapy after oophorectomy and in never smokers. This study highlights that patients with oophorectomy do have increased respiratory symptoms associated with a clinical diagnosis of OLD. Figure 4 shows a general causal diagram including the possible effects of smoking, obesity, and other confounders or modifiers considered in our analyses.
A previous study using the same MOA-2 cohorts used in this study showed an increased rate of accumulation of several chronic conditions after oophorectomy, including asthma and COPD. However, asthma and COPD were defined only using diagnostic codes27. In the current study, we did not observe an increased risk of asthma or COPD when the diagnosis required confirmation by PFT. In clinical practice, patients are frequently diagnosed with COPD or asthma without PFT data. The diagnosis of asthma is primarily based on clinical history, and pulmonary function testing can be normal in asthmatics who have mild disease or are well treated at the time of testing. Based on GOLD guidelines, COPD should be diagnosed based on persistent post-bronchodilator obstruction. In our study, we did not find an association with COPD confirmed by PFT data; however, we did observe an increase in chronic bronchitis and emphysema which do not require PFT data for diagnosis.
Several prior studies investigated the effects of sex on respiratory disease by studying the relationship between menopause and lung function or COPD. Using the UK Biobank, Amaral et al. reported that women who underwent spontaneous menopause, especially at early ages, experienced a lower FVC, FEV1, but not FEV1/FVC ratio – suggesting a more restrictive than obstructive process in menopause. This association was stronger in women with earlier spontaneous menopause and in women who underwent surgical menopause26. Tang et al. also used the UK biobank data with similar results and noted that early menopause was associated with higher risk of COPD-related hospitalization and death. They also noted that contraceptive use was associated with lower risk of COPD-related hospitalization and death, and with higher FEV1 and FVC37. In our study, we found an increased risk of overall OLD which included COPD, chronic bronchitis, and emphysema in women who underwent bilateral oophorectomy. However, we did not see a clear association with COPD when applying stringent GOLD criteria, probably because many of the patients did not have pulmonary function data. COPD, chronic bronchitis, and emphysema are frequently diagnosed without PFT in medical practice, particularly in primary care and community settings. Our study highlights real world associations between oophorectomy and OLD.
There is less evidence in the literature relating asthma to menopause, especially to menopause induced by oophorectomy. The risk of severe asthma decreases in women after the age of 45 years, but not in men38; this decrease has been explained by the change in hormones associated with menopause. The Nurses’ Health Study and other studies suggested that spontaneous menopause is protective against asthma, but the protection is reversed by estrogen therapy20,24,39. Troisi et al. reported that the risk of asthma was associated with duration of estrogen therapy in both current and past users20. Jarvis et al. reported an association of estrogen therapy with asthma, particularly in non-obese women. They suggested that lean women have less circulating endogenous estrogen and are more responsive to exogenous estrogen21. However, in these studies, information about menopause, estrogen therapy, and asthma was collected via interview and may be incomplete or biased. By contrast, our study used medical records information to confirm the association of estrogen therapy with increased risk of asthma in women who underwent oophorectomy.
In the current study, the risk of asthma after oophorectomy was increased among never smokers and in women less than 46 years of age who received estrogen therapy. However, our findings may not be directly comparable with findings from previous studies because spontaneous menopause and oophorectomy are not equivalent processes. In spontaneous menopause, the reduction of hormonal levels is slow and progressive, whereas in oophorectomy there is an abrupt reduction that may affect airway and lung biology differently. Matulonga-Diakiese et al. suggested that the increased risk of asthma after surgical menopause may be due to the loss of testosterone that has an immunomodulatory effect against asthma23.
Obesity may modify the association between oophorectomy and different types of OLD. In our study, the association was stronger in non-obese women for all OLD, all COPD, and chronic bronchitis, but was similar for emphysema and asthma (non-significant differences). By contrast, Matulonga-Diakiese et al. reported an association of spontaneous menopause with increased risk of asthma restricted to obese women and explained the association with the higher levels of circulating estrogen in obese women23.
There are several strengths to our study. First, to the best of our knowledge, this is the first large, population-based cohort study to compare the effects of oophorectomy on the development of OLD to a referent group. Second, we had direct access to medical record documentation of the oophorectomies. Third, we validated OLD diagnoses using spirometric measurements including post-bronchodilator and bronchoprovocation data, and we applied current GOLD and GINA guidelines. Finally, we balanced our cohorts for possible confounders including age at index date, BMI, race, education, smoking history, 16 chronic conditions, and others.
There are also several limitations to our study. First, our study involved a single geographical location in the United States, and the observed findings may differ in other populations. Second, using the strict GOLD and GINA criteria to confirm COPD and asthma may have caused some misclassification. For instance, using an FEV1/FVC ratio of <70% may misclassify obstruction in older patients40. In addition, the devices used for spirometry were not standardized, and may have varied across care providers and over time.
Third, a large proportion of women in both cohorts developed “possible asthma”. These women were clinically diagnosed with asthma without documented PFT. However, when we applied the stringent GINA criteria, there was no increased risk of asthma in women with oophorectomy. The discrepancies in diagnosis of OLD are not surprising. Discordance of asthma and COPD diagnosis has been well described41,42,43,44. One study reported that only 55% of doctor-diagnosed asthma and 56% of doctor-diagnosed COPD had spirometry performed. Among patients with spirometry, 70% of asthma patients and 10% of COPD patients had concordant spirometry patterns41. Other studies suggested that ~70% of COPD worldwide may be underdiagnosed, whereas up to 60% may be overdiagnosed. Approximately 46% of these overdiagnosed patients are receiving respiratory medications42,43. Moreover, women are more likely to be underdiagnosed for OLD than men45,46,47.
There is mounting evidence that sex hormones play a role in the development and disease severity of OLD. Women who underwent bilateral oophorectomy in a population-based cohort study had a higher risk of asthma primarily if they underwent oophorectomy at a younger age and received estrogen therapy after the oophorectomy. Therefore, our findings suggest that the age of onset of menopause and estrogen therapy may influence the risk of asthma. They also suggest that the timing of hormone cessation and hormone replacement may play a role in lung pathology. We also found an association of oophorectomy with the development of COPD, chronic bronchitis, and emphysema. Although a clear sexual dimorphism in airway pathology exists, further investigation comparing spontaneous and surgical menopause is warranted to better understand the impact of hormonal changes on the lung throughout the lifespan of women.
The results of this study, combined with the increased risk of several chronic diseases and of multimorbidity reported from previous studies, suggest that bilateral oophorectomy for benign indications in premenopausal women should be avoided unless there is clear evidence of a high genetic risk of ovarian cancer27. The harmful effect of bilateral oophorectomy on the lung, heart, brain, bone, and other organs and systems outweigh the prevention of ovarian cancer in women at average risk.
Data availability
The tables of results from the sensitivity analyses are available from the corresponding author upon request. By contrast, to obtain the data that support the findings of this study, the user must submit a brief outline of the intended use of the data (no longer than a page). In addition, the user will be required to sign a data-sharing agreement, and provide payment to the Mayo Clinic for administrative costs in the preparation of the shared file of de-identified data. The application for data can be submitted with a brief outline of the data need to the corresponding author Megan Dulohery Scrodin.
References
Raghavan, D. & Jain, R. Increasing awareness of sex differences in airway diseases. Respirology 21, 449–459 (2016).
Townsend, E. A., Miller, V. M. & Prakash, Y. S. Sex differences and sex steroids in lung health and disease. Endocr. Rev. 33, 1–47 (2012).
Fuentes, N. & Silveyra, P. Endocrine regulation of lung disease and inflammation. Exp. Biol. Med. 243, 1313–1322 (2018).
Haggerty, C. L., Ness, R. B., Kelsey, S. & Waterer, G. W. The impact of estrogen and progesterone on asthma. Ann. Allergy Asthma Immunol. 90, 284–291 (2003).
Sathish, V., Martin, Y. N. & Prakash, Y. S. Sex steroid signaling: implications for lung diseases. Pharm. Ther. 150, 94–108 (2015).
Zein, J. G. et al. Impact of age and sex on outcomes and hospital cost of acute asthma in the United States, 2011–2012. PLoS One 11, e0157301 (2016).
Farha, S. et al. Effects of the menstrual cycle on lung function variables in women with asthma. Am. J. Respir. Crit. Care Med. 180, 304–310 (2009).
Rubio Ravelo, L., Gago Rodríguez, B., Almirall Collazo, J. J., Bell Heredia, L. & Fernández Fernández, L. Comparative study of progesterone, estradiol and cortisol concentrations in asthmatic and non-asthmatic women. Allergol. Immunopathol. 16, 263–266 (1988).
Rao, C. K. et al. Characteristics of perimenstrual asthma and its relation to asthma severity and control: data from the Severe Asthma Research Program. Chest 143, 984–992 (2013).
Jenkins, M. A. et al. Parity and decreased use of oral contraceptives as predictors of asthma in young women. Clin. Exp. Allergy 36, 609–613 (2006).
Al-Sahab, B., Hamadeh, M. J., Ardern, C. I. & Tamim, H. Early menarche predicts incidence of asthma in early adulthood. Am. J. Epidemiol. 173, 64–70 (2011).
Akinbami, L. J. & Liu, X. Chronic obstructive pulmonary disease among adults aged 18 and over in the United States, 1998–2009. NCHS Data Brief, 1–8 (2011).
Ford, E. S., Mannino, D. M., Zhao, G., Li, C. & Croft, J. B. Changes in mortality among us adults with COPD in two national cohorts recruited from 1971–1975 and 1988–1994. Chest 141, 101–110 (2012).
Celli, B. R., Halbert, R. J., Nordyke, R. J. & Schau, B. Airway obstruction in never smokers: results from the Third National Health and Nutrition Examination survey. Am. J. Med. 118, 1364–1372 (2005).
Sørheim, I. C. et al. Gender differences in copd: are women more susceptible to smoking effects than men? Thorax 65, 480–485 (2010).
Amaral, A. F. S., Strachan, D. P., Burney, P. G. J. & Jarvis, D. L. Female smokers are at greater risk of airflow obstruction than male smokers. UK Biobank. Am. J. Respir. Crit. Care Med. 195, 1226–1235 (2017).
Coxson, H. O. et al. The presence and progression of emphysema in COPD as determined by ct scanning and biomarker expression: a prospective analysis from the ECLIPSE study. Lancet Respir. Med. 1, 129–136 (2013).
Martinez, F. J. et al. Sex differences in severe pulmonary emphysema. Am. J. Respir. Crit. Care Med. 176, 243–252 (2007).
Morabia, A. & Costanza, M. C. International variability in ages at menarche, first livebirth, and menopause. World Health Organization collaborative study of Neoplasia and Steroid Contraceptives. Am. J. Epidemiol. 148, 1195–1205 (1998).
Troisi, R. J., Speizer, F. E., Willett, W. C., Trichopoulos, D. & Rosner, B. Menopause, postmenopausal estrogen preparations, and the risk of adult-onset asthma. A prospective cohort study. Am. J. Respir. Crit. Care Med. 152, 1183–1188 (1995).
Jarvis, D. & Leynaert, B. The association of asthma, atopy and lung function with hormone replacement therapy and surgical cessation of menstruation in a population-based sample of English women. Allergy 63, 95–102 (2008).
Barr, R. G. et al. Prospective study of postmenopausal hormone use and newly diagnosed asthma and chronic obstructive pulmonary disease. Arch. Intern. Med. 164, 379–386 (2004).
Matulonga-Diakiese, B. et al. Risk of asthma onset after natural and surgical menopause: results from the french E3N cohort. Maturitas 118, 44–50 (2018).
Carlson, C. L., Cushman, M., Enright, P. L., Cauley, J. A. & Newman, A. B. Hormone replacement therapy is associated with higher FEV1 in elderly women. Am. J. Respir. Crit. Care Med. 163, 423–428 (2001).
Real, F. G. et al. Lung function, respiratory symptoms, and the menopausal transition. J. Allergy Clin. Immunol. 121, 72–80.e73 (2008).
Amaral, A. F., Strachan, D. P., Gómez Real, F., Burney, P. G. & Jarvis, D. L. Lower lung function associates with cessation of menstruation: UK Biobank data. Eur. Respir. J. 48, 1288–1297 (2016).
Rocca, W. A. et al. Accelerated accumulation of multimorbidity after bilateral oophorectomy: a population-based cohort study. Mayo Clin. Proc. 91, 1577–1589 (2016).
Rocca, W. A. et al. Bilateral oophorectomy and accelerated aging: cause or effect. J. Gerontol. A Biol. Sci. Med. Sci. 72, 1213–1217 (2017).
Rocca, W. A. et al. Cohort profile: the Mayo Clinic Cohort Study of Oophorectomy and Aging-2 (MOA-2) in Olmsted County, Minnesota (USA). BMJ Open 7, e018861 (2017).
St Sauver, J. L., Grossardt, B. R., Yawn, B. P., Melton, L. J. 3rd & Rocca, W. A. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester Epidemiology Project. Am. J. Epidemiol. 173, 1059–1068 (2011).
St Sauver, J. L. et al. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin. Proc. 87, 151–160 (2012).
Rocca, W. A., Yawn, B. P., St Sauver, J. L., Grossardt, B. R. & Melton, L. J. 3rd History of the Rochester Epidemiology Project: Half a century of medical records linkage in a US population. Mayo Clin. Proc. 87, 1202–1213 (2012).
St Sauver, J. L. et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int. J. Epidemiol. 41, 1614–1624 (2012).
Cohen, J. W., Cohen, S. B. & Banthin, J. S. The Medical Expenditure Panel Survey: a national information resource to support healthcare cost research and inform policy and practice. Med. Care 47, S44–50 (2009).
Goodman, R. A., Posner, S. F., Huang, E. S., Parekh, A. K. & Koh, H. K. Defining and measuring chronic conditions: Imperatives for research, policy, program, and practice. Prev. Chronic Dis. 10, E66 (2013).
Snider, G. L. Chronic obstructive pulmonary disease: a definition and implications of structural determinants of airflow obstruction for epidemiology. Am. Rev. Respir. Dis. 140, S3–8 (1989).
Tang, R., Fraser, A. & Magnus, M. C. Female reproductive history in relation to chronic obstructive pulmonary disease and lung function in UK Biobank: a prospective population-based cohort study. BMJ Open 9, e030318 (2019).
Zein, J. G. et al. Asthma is more severe in older adults. PLoS One 10, e0133490 (2015).
Romieu, I. et al. Postmenopausal hormone therapy and asthma onset in the E3N cohort. Thorax 65, 292–297 (2010).
Roberts, S. D. et al. FEV1/FVC ratio of 70% misclassifies patients with obstruction at the extremes of age. Chest 130, 200–206 (2006).
Heffler, E. et al. Misdiagnosis of asthma and COPD and underuse of spirometry in primary care unselected patients. Respir. Med. 142, 48–52 (2018).
Diab, N. et al. Underdiagnosis and overdiagnosis of chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 198, 1130–1139 (2018).
Sator, L. et al. Overdiagnosis of COPD in subjects with unobstructed spirometry: a bold analysis. Chest 156, 277–288 (2019).
Ng, B., Sadatsafavi, M., Safari, A., FitzGerald, J. M. & Johnson, K. M. Direct costs of overdiagnosed asthma: a longitudinal, population-based cohort study in British Columbia, Canada. BMJ Open 9, e031306 (2019).
Ancochea, J. et al. Underdiagnosis of chronic obstructive pulmonary disease in women: quantification of the problem, determinants and proposed actions. Arch. Bronconeumol. 49, 223–229 (2013).
Delgado, A., Saletti-Cuesta, L., López-Fernández, L. A., Gil-Garrido, N. & Luna Del Castillo Jde, D. Gender inequalities in COPD decision-making in primary care. Respir. Med. 114, 91–96 (2016).
Martinez, C. H. et al. Gender differences in symptoms and care delivery for chronic obstructive pulmonary disease. J. Women’s Health (Larchmt.) 21, 1267–1274 (2012).
Acknowledgements
The Mayo Clinic Cohort Study of Oophorectomy and Aging (MOA-2) used the resources of the Rochester Epidemiology Project (REP) medical records-linkage system, which is supported by the National Institute on Aging (NIA; R33 AG058738), by the Mayo Clinic Research Committee, and by fees paid annually by REP users. However, the content of this article is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health (NIH) or the Mayo Clinic. W.A.R. was partly funded by the grants U54 AG044170 and RF1 AG055151 from the National Institute on Aging, National Institutes of Health, and by the Ralph S. and Beverley E. Caulkins Professorship of Neurodegenerative Diseases Research of the Mayo Clinic.
Author information
Authors and Affiliations
Contributions
Study conception and design: T.T.N., W.A.R., R.V., and M.M.D.S.; acquisition, analysis, or interpretation of data: T.T.N., C.Y.S., L.G.R., and W.A.R.; drafting of the manuscript: T.T.N. and M.M.D.S.; critical revisions of the manuscript: all authors. Final approval of the manuscript: all authors. All authors take responsibility for the integrity and accuracy of the work.
Corresponding author
Ethics declarations
Competing interests
W.A.R. has received research support from the National Institutes of Health (R01 AG052425, RF1 AG055151, U54 AG044170, U01 AG006786, and R33 AG058738). R.V. has received research support from the NIH (HL140486, HL142061, and AI147394) as well as research grant funding from Pfizer, Bristol Myers Squibb, and Sun Pharmaceuticals for research unrelated to this study. For the remaining authors, no conflicts were declared. No author had conflicts of interest directly related to the subject of this manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nguyen, T.T., Smith, C.Y., Gazzuola Rocca, L. et al. A population-based cohort study on the risk of obstructive lung disease after bilateral oophorectomy. npj Prim. Care Respir. Med. 32, 52 (2022). https://doi.org/10.1038/s41533-022-00317-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41533-022-00317-4
This article is cited by
-
Sexually dimorphic response to tobacco exposure in COPD: a systematic review and meta-analysis
BMC Pulmonary Medicine (2026)
-
Soft mist, dry powder, and smart inhalers: comparative technologies and clinical impact on asthma and COPD management
The Egyptian Journal of Bronchology (2025)