Abstract
Effective vaccination strategies adaptable to emerging viruses like SARS-CoV-2 and capable of inducing robust protective immunity are needed. We evaluated the immunogenicity and protective efficacy of homologous and heterologous prime/boost regimens against SARS-CoV-2 in K18-hACE2 mice and Syrian hamsters using Newcastle disease virus (NDV-HXP-S, intranasal) and modified vaccinia virus Ankara (MVA-S(3P), intramuscular) vectors encoding a prefusion-stabilized SARS-CoV-2 spike (S) protein. All regimens protected against weight loss and markedly reduced viral replication and lung pathology. Vaccination induced serum anti-S and anti-receptor binding domain IgGs and neutralizing antibodies against ancestral virus and variants. In mice, mucosal anti-S IgA and IgG were detected after NDV-HXP-S immunization. Homologous MVA-S(3P)/MVA-S(3P) and heterologous NDV-HXP-S/MVA-S(3P) elicited higher polyfunctional systemic T-cell responses, while homologous NDV-HXP-S/NDV-HXP-S induced stronger pulmonary CD8+ T cells. Hamsters vaccinated with NDV-HXP-S exhibited protection of the upper respiratory tract, with the NDV-HXP-S/MVA-S(3P) regimen showing a trend toward reduced direct contact transmission of SARS-CoV-2. These findings demonstrate the capacity of NDV and MVA vector platforms to induce robust systemic and mucosal antigen-specific humoral and T-cell responses against SARS-CoV-2, contributing to protection against both disease and transmission, and support further exploration of these vector platforms for vaccination against SARS-CoV-2 and potentially other pathogens.
Similar content being viewed by others
Introduction
The swift development and distribution of vaccines in response to the emergence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is estimated to have saved millions of lives1,2. Despite this significant achievement, there remains a pressing need for safe, efficient, durable, and low-cost vaccines to prevent coronavirus disease 2019 (COVID-19) and address future emerging threats such as SARS-CoV-2 variants or other viruses with epidemic and pandemic potential. In this context, various heterologous prime/boost vaccination strategies combining mRNA vaccines, recombinant protein vaccines, inactivated vaccines or viral vector vaccines (particularly adenovirus-based vaccines) have been tested, demonstrating longer and better protection against COVID-193. Additionally, data collected from COVID-19 clinical trials performed in Thailand and Brazil revealed greater effectiveness of heterologous prime/boost vaccinations versus homologous vaccinations4,5. However, relatively few studies have assessed heterologous combinations of distinct viral vectors for COVID-19 vaccination. Moreover, vaccines that can prevent not only severe disease but also virus infection at the mucosal entry site and viral transmission are needed.
Viral vectors serve as low-cost, powerful and rapid vaccine platforms against emerging viruses, capable of inducing robust and durable antigen-specific protective immune responses. They have been employed in both preclinical and clinical trials as vaccines against a variety of infectious disease pathogens, including human immunodeficiency virus (HIV), Ebola virus, and more recently, SARS-CoV-26. Among viral vector-based vaccines, adenovirus-based platforms played a pivotal role during the COVID-19 pandemic, with notable examples such as Oxford–AstraZeneca, Janssen, Sputnik V, Sputnik Light, Convidecia, and iNCOVACC vaccines, all of which utilize different adenovirus vectors and have demonstrated favorable immunogenicity and efficacy profiles7. In particular, we have developed COVID-19 vaccine candidates based on two different viral vectors: i) a Newcastle disease virus (NDV) vector encoding a prefusion SARS-CoV-2 spike (S) protein stabilized by introducing six proline substitutions (Hexa Pro, HXP) (termed NDV-HXP-S)8,9,10,11, and ii) a modified vaccinia virus Ankara (MVA) vector also encoding a prefusion SARS-CoV-2 S protein stabilized by three proline substitutions, termed MVA-S(3P)12,13,14,15,16. Both vaccine candidates have been successfully tested in several preclinical studies in animal models, showing them to be safe, highly efficacious and inducing robust, polyfunctional and broad antigen-specific immune responses8,9,10,11,12,13,14,15,16. Moreover, NDV-HXP-S has been demonstrated in several phase 1/2 clinical trials to be safe and highly immunogenic when given intramuscularly or intranasally17,18,19,20, and has been approved as a booster COVID-19 vaccine in Thailand and Mexico after phase 3 clinical trials. While a single dose of these vaccines can provide protective immunity after SARS-CoV-2 challenge8,9,10,11,12,13,14,15,16, booster doses can enhance immune responses, resulting in stronger, longer-lasting, and broader protection that may be necessary to achieve sterilizing immunity and block viral transmission. One of the concerns of homologous prime/boost regimens using viral vector vaccines is the potential for the vector-specific immune response generated by the first dose to partially neutralize the second dose21,22. However, using a different viral vector for the second dose in a heterologous prime/boost regimen circumvents this issue and often results in improved immune responses21,22. Particularly, MVA has proved in several preclinical and clinical trials to serve as a safe and excellent booster in heterologous prime/boost regimens23,24,25.
The objective of the experiments described here was to assess the potential of previously developed NDV-HXP-S and MVA-S(3P) vaccine candidates, when used in various prime/boost immunization regimens. NDV-HXP-S was delivered intranasally to facilitate the induction of mucosal responses, while intramuscular administration of MVA-S(3P) was performed to activate a systemic response. This approach was intended to enhance the magnitude of antigen-specific immune responses and improve protection against SARS-CoV-2 in two animal models, mice and hamsters. Thus, we tested, the immunogenicity and protective efficacy of four different prime/boost vaccination regimens in transgenic K18-hACE2 mice and Golden Syrian hamsters challenged with SARS-CoV-2: homologous MVA-S(3P)/MVA-S(3P) and NDV-HXP-S/NDV-HXP-S, or heterologous MVA-S(3P)/NDV-HXP-S and NDV-HXP-S/MVA-S(3P). One potential advantage of combining NDV and MVA is the capacity to engage both mucosal and systemic immune responses, depending on the route of administration and vaccine platform. The results demonstrated that, in general, all homologous and heterologous prime/boost vaccination regimens were highly immunogenic, inducing systemic and mucosal SARS-CoV-2-specific immune responses, and providing strong protection against SARS-CoV-2 infection in both animal models. However, slightly differences were observed among the regimens. Specifically, the heterologous NDV-HXP-S/MVA-S(3P) vaccine strategy exhibited distinct immunological advantages, inducing robust systemic antigen-specific CD4+ and CD8+ T-cell responses, as well as pulmonary CD8+ T-cell responses in mice, along with strong systemic and mucosal humoral immunity in both animal models. Moreover, in hamsters, intranasal vaccination with NDV-HXP-S conferred protection of the upper respiratory tract, and the NDV-HXP-S/MVA-S(3P) regimen showed a trend toward reduced direct contact transmission of SARS-CoV-2, although the limited sample size precludes definitive conclusions. These findings support further evaluation of NDV and MVA vectors in prime/boost strategies to elicit systemic and mucosal immunity against SARS-CoV-2 and other viruses with epidemic and pandemic potential.
Results
Immunization with NDV and MVA viral vectors encoding SARS-CoV-2 S protein provides protection of K18-hACE2 transgenic mice challenged with SARS-CoV-2
To assess the protective efficacy of different homologous (MVA-S(3P)/MVA-S(3P) or NDV-HXP-S/NDV-HXP-S) or heterologous (MVA-S(3P)/NDV-HXP-S or NDV-HXP-S/MVA-S(3P)) prime/boost immunization regimens, ten female K18-hACE2 mice per group were immunized intramuscularly with 1 × 107 plaque-forming units (PFUs) of MVA-S(3P) or intranasally with 1 × 106 embryo infectious dose 50 (EID50) of NDV-HXP-S. Four weeks later the corresponding second dose was administered, as indicated in Fig. 1A. Mice inoculated with PBS were used as control group. After four weeks all mice were challenged intranasally with 1 x 105 PFUs of SARS-CoV-2 (Wuhan MAD6 isolate, containing D614G mutation). Mouse body weight and mortality were monitored during 17 days after the challenge. Immunized K18-hACE2 mice experienced low (5%) body weight loss during the first 3 days post-challenge, but then regained body weight (Fig. 1B) and all of them survived (Fig. 1C). There were no statistically significant differences among vaccination groups in weight loss or survival. In contrast, PBS control mice lost more than 20% of their body weight (Fig. 1B) and all reached humane endpoints by 7 days post-challenge, at which point they were euthanized in accordance with institutional ethical guidelines (Fig. 1C). To evaluate the effect of vaccination on SARS-CoV-2 replication, on day 5 post-challenge five mice per group were sacrificed, and the lungs and nasal washes (NW) were collected and processed to measure SARS-CoV-2 subgenomic E or genomic RdRp RNA (Fig. 1D, E), as well as live infectious virus (Fig. 1F, G). Compared with the control group, all four immunization regimens demonstrated a significant reduction in SARS-CoV-2 subgenomic and genomic RNA levels both in lungs (Fig. 1D) and NW (Fig. 1E). SARS-CoV-2 subgenomic and genomic RNA levels in mouse lungs from all four vaccination groups were comparable to those of uninfected mice, suggesting that viral replication was below the detection limit at this time point (Fig. 1D). However, in NW from all four vaccination groups, SARS-CoV-2 subgenomic and genomic RNA levels were observed above the limit of detection (LOD), indicating that there was some viral replication in this site (Fig. 1E). In line with these results, no live infectious virus was detected in the lungs from all four vaccination groups, whereas significantly higher viral yields were detected in the lungs of the control group (Fig. 1F). On the other hand, no live infectious virus was detected in NW samples obtained from all mice, except in one mouse from the control group (Fig. 1G). This may reflect natural clearance of virus at this time point rather than a vaccine effect, as live virus was also mostly undetectable in control mice.
A Mouse efficacy schedule. Female K18-hACE2 transgenic mice (n = 10 mice/group) were immunized with homologous (MVA-S(3P)/MVA-S(3P) and NDV-HXP-S/NDV-HXP-S) or heterologous (MVA-S(3P)/NDV-HXP-S and NDV-HXP-S/MVA-S(3P)) prime/boost immunization regimens, as indicated. Mice received two doses with a 4-week interval (days 0 and 28), of 1 × 107 PFUs of MVA-S(3P) by the intramuscular (IM) route in 100 μL of PBS (50 μL/leg) or of 1 × 106 EID50 of NDV-HXP-S by the intranasal (IN) route in 50 μL of PBS. Mice inoculated with PBS were used as a control group. On days 14 post-prime and 26 post-boost (day 54; 2 days pre-challenge), serum samples were obtained from each mouse, as indicated. At day 56 (4 weeks post-boost) all mice were challenged intranasally with 1 × 105 PFUs of SARS-CoV-2 MAD6 isolate (ancestral Wuhan strain). At day 5 post-challenge, five mice per group were sacrificed and lungs, nasal washes (NW) and serum samples collected as indicated. Vaccinated mice were left until day 17 post-challenge, when spleens, lungs, NW and serum samples were collected. B, C The challenged mice were monitored for change of body weight (B) and mortality (C) for 17 days. †: mice were euthanized due to loss of more than 20% of initial body weight. D, E Virus replication in lung samples (D) and NW (E). SARS-CoV-2 subgenomic E and genomic RdRp mRNA detected by RT-qPCR at 5 days after SARS-CoV-2 virus infection. The geometric mean with geometric standard deviation (SD) of mRNA levels (in relative units normalized to uninfected mice) from duplicates of each lung sample and nasal wash for each group are represented. Limit of detection (LOD) = 100. F, G SARS-CoV-2 infectious virus in lung samples (F) and NW (G) at 5 days post-challenge. The geometric mean with geometric SD of live virus (PFUs/g of lung tissue or PFUs/mL of nasal wash) from triplicates of each sample for each group are represented. The dotted line represents the LOD. Ordinary one-way ANOVA of transformed data followed by Tukey’s multiple comparison test: **p < 0.002; ***p < 0.0002; ****p < 0.0001.
Lung histopathological evaluations at day 5 post-challenge showed that all vaccinated mice had only occasional mild lesions, with lung inflammation scores (Fig. 2A) and percentages of lung areas with lesions (Fig. 2B) being significantly lower than those of control mice. Mice vaccinated with any of the four vaccination regimens showed only focal thickening of alveolar septa, occasional mild perivascular and peribronchiolar mononuclear infiltrates and the sporadic appearance of mild inflammatory infiltrates within the alveoli. In contrast, mice inoculated with PBS exhibited diffuse moderate to severe thickening of the alveolar septa, diffuse severe mononuclear cell infiltrates within the alveolar spaces, and disseminated severe perivascular and peribronchiolar mononuclear infiltrates (Fig. 2C).
A Mean and SD of cumulative histopathological lesion scores in lung samples taken from immunized K18-hACE2 mice euthanized at day 5 post-challenge. Unpaired nonparametric Kruskal-Wallis test: *p < 0.033; **p < 0.002; ***p < 0.0002. B Mean and SD of lung area percentage affected by inflammatory lesions in lung samples taken from immunized K18-hACE2 mice euthanized at day 5 post-challenge. Ordinary one-way ANOVA followed by Tukey’s multiple comparisons test: **p < 0.002; ***p < 0.0002. C Representative lung histopathological sections (H&E staining) observed in immunized K18-hACE2 transgenic mice euthanized at day 5 post-challenge. A general view of the lung area (magnification: 4x) along with histopathological details from selected lung areas (red boxes) have been displayed (magnification: 10x). In vaccinated mice, alveolar spaces were larger and more evident, while inflammatory changes were less severe than those observed in unvaccinated mice (unprotected control group). Vaccinated mice showed mild lung lesions characterized by the presence of mild to moderate septal thickening, multifocal mild perivascular and peribronchiolar mononuclear infiltrates consisting mainly of lymphocytes (red arrows), as well as occasional alveoli with mild cellular infiltrates. In contrast, in unvaccinated mice inflammatory lesions were more severe and diffuse. Such lesions were characterized by diffuse moderate to severe septal thickening, disseminated severe perivascular and peribronchiolar mononuclear infiltrates (black arrows), alveolar spaces densely populated by inflammatory cells, mainly monocytes (red arrowheads), and bronchi or bronchioles with detached epithelium or inflammatory cells in the lumen, changes characteristic of bronchitis or bronchiolitis (black arrowheads). The analysis was performed by a pathologist who was blinded to the group information. D mRNA levels of several cytokines/chemokines detected by RT-qPCR in lungs obtained at 5 days post-challenge. The geometric mean with geometric SD of RNA levels (in relative units normalized to uninfected mice) from duplicates of each sample for each group are represented. Ordinary one-way ANOVA of transformed data followed by Tukey’s multiple comparisons test: *p < 0.033; **p < 0.002; ***p < 0.0002; ****p < 0.0001.
Moreover, the impact of vaccination on the pro-inflammatory cytokine profile induced in infected mice was analysed at day 5 post-challenge by measuring by RT-qPCR in lung samples the mRNA levels of key cytokines (Fig. 2D). The results showed that all vaccination regimens significantly downregulated mRNA levels of CXCL10, CCL2, TNF-α, and IFNγ compared to the control group. IL-10 was significantly reduced in all groups except MVA-S(3P)/NDV-HXP-S. IL-6 was significantly reduced only in NDV-HXP-S/NDV-HXP-S and NDV-HXP-S/MVA-S(3P) (Fig. 2D). These results confirm that vaccination limited the pro-inflammatory response, although no consistent pattern of superiority was observed among regimens.
Immunization with NDV and MVA viral vectors induces potent systemic and mucosal SARS-CoV-2-specific antibody responses in K18-hACE2 transgenic mice
We next evaluated SARS-CoV-2-specific systemic and mucosal humoral responses in serum samples and NW from transgenic K18-hACE2 mice vaccinated with all four regimens of MVA-S(3P) and NDV-HXP-S combinations (Fig. 3). To evaluate systemic humoral responses, we measured serum anti-S Wuhan IgG titers by ELISA at days 14 post-prime and 26 post-boost (2 days pre-challenge), as well as at days 5 and 17 post-challenge. The results revealed that after the first dose, on day 14 post-prime, mice vaccinated with MVA-S(3P) (administered intramuscularly) elicited higher serum anti-S Wuhan IgG titers (mean around 105) than mice vaccinated with NDV-HXP-S (administered intranasally), which exhibited greater variability (mean of approximately 103). Notably, two mice in each NDV-HXP-S vaccinated group failed to develop detectable anti-S binding IgG antibodies (Fig. 3A), indicating inter-individual variability in the vaccine response following a single dose of NDV-HXP-S, which may be due to intrinsic biological differences among animals, variations in vaccine uptake or immune competence, or technical factors related to sample processing. After the second dose, on day 26 post-boost, serum anti-S Wuhan IgG titers increased in all four vaccination groups, reaching similar levels (between 105 and 106). At this time point, the NDV-HXP-S/MVA-S(3P) vaccination regimen showed a trend toward higher titers compared to other regimens, although differences were not statistically significant, except when compared to MVA-S(3P)/MVA-S(3P), for which a significant difference was observed (Fig. 3A). By day 5 post-challenge, serum anti-S Wuhan IgG titers barely changed in any of the four vaccination groups, with the NDV-HXP-S/MVA-S(3P) vaccination regimen maintained the highest titers, which were significantly higher only when compared to the MVA-S(3P)/MVA-S(3P) regimen (Fig. 3A). By day 17 post-challenge, serum anti-S Wuhan IgG titers increased in all groups except the NDV-HXP-S/MVA-S(3P) vaccination group (Fig. 3A). Notably, NDV-HXP-S/NDV-HXP-S and MVA-S(3P)/NDV-HXP-S vaccination regimens induced significantly higher titers than the NDV-HXP-S/MVA-S(3P) regimen at this time point (Fig. 3A).
A Systemic anti-S IgG titers against Wuhan determined by ELISA in individual mouse serum samples collected from K18-hACE2 mice at day 14 post-prime, day 26 post-boost, day 5 post-challenge and day 17 post-challenge. The geometric mean with geometric SD of endpoint titers from duplicates of each sample for each group are represented. The dotted line represents the LOD. Unpaired ordinary one-way ANOVA followed by Tukey’s multiple comparisons test of transformed data: *p < 0.033; **p < 0.002; ***p < 0.0002; ****p < 0.0001. B Isotype anti-S IgG1, IgG2c and IgG3 titers against Wuhan determined by ELISA in pooled mouse serum samples (n = 5) collected from K18-hACE2 mice at day 26 post-boost. The geometric mean with geometric SD of endpoint titers from duplicates of each sample for each group are represented. The dotted line represents the LOD. Two-way ANOVA followed by Tukey’s multiple comparisons test: *p < 0.033; ***p < 0.0002; ****p < 0.0001. C Systemic anti-S IgG titers against Wuhan, Beta, Omicron BA.1, BA.5 and XBB.1.5 determined by ELISA in pooled mouse serum samples (n = 5) collected from K18-hACE2 mice at day 14 post-prime and day 26 post-boost. The geometric mean with geometric SD of endpoint titers from duplicates of each sample for each group are represented. The dotted line represents the LOD. Two-way ANOVA followed by Tukey’s multiple comparisons test: *p < 0.033; ****p < 0.0001. D Neutralizing antibody titers against SARS-CoV-2 Wuhan (MAD6 isolate). NT50 titers were evaluated in individual mouse serum samples collected at day 26 post-boost, day 5 post-challenge and day 17 post-challenge using a live virus MNT assay. The geometric mean with geometric SD of NT50 values from triplicates of each sample for each group are represented. The dotted line represented the LOD. Unpaired ordinary one-way ANOVA followed by Tukey’s multiple comparisons test of transformed data: *p < 0.033; **p < 0.002; ***p < 0.0002. E SARS-CoV-2 neutralizing antibody titers against several SARS-CoV-2 variants of concern. NT50 titers against Wuhan (MAD6 isolate), Beta, Omicron BA.1, BA.5 and XBB.1.5 were evaluated in pooled mouse serum samples (n = 5) collected at day 26 post-boost, using a live virus MNT assay. The geometric mean with geometric SD of NT50 values from triplicates of each pooled group sample are represented. The dotted line represents the LOD. Unpaired ordinary one-way ANOVA followed by Tukey’s multiple comparisons test of transformed data: *p < 0.033; ****p < 0.0001. F, G Mucosal anti-S IgA (F) and anti-S IgG (G) levels against Wuhan determined by ELISA in pooled NW (n = 5) collected from K18-hACE2 mice on day 17 post-challenge. For the PBS/PBS group, pooled NW were collected on day 5 post-challenge. Data are presented as mean optical density (OD) at 450 nm from serial dilutions, with SD calculated from duplicate measurements.
Isotype analysis of anti-S Wuhan IgG antibodies in pooled sera obtained on day 26 post-boost (2 days pre-challenge) revealed that all vaccine regimens induced levels of IgG2c > IgG1 > IgG3, and a IgG2c/IgG1 ratio above 1, indicating a Th1-like protective immune response, with significantly higher anti-S binding IgG2c, IgG1 and IgG3 antibodies for the NDV-HXP-S/MVA-S(3P) group (Fig. 3B).
We next analysed IgG titers against the S protein of different SARS-CoV-2 variants, including Beta, and Omicron subvariants BA.1, BA.5, and XBB.1.5, in pooled sera obtained on days 14 post-prime and 26 post-boost (2 days pre-challenge) (Fig. 3C). On day 14 post-prime, mice vaccinated with one dose of MVA-S(3P) elicited similarly high serum IgG titers against S protein from Beta and Omicron BA.5 as against S protein from Wuhan, whereas serum IgG titers against S protein from Omicron BA.1 and XBB.1.5 subvariants were slightly lower (Fig. 3C, left). On the other hand, mice vaccinated with one dose of NDV-HXP-S elicited similar serum IgG titers against S protein from Wuhan and Beta, lower IgG titers against S protein from Omicron BA.1 and BA.5 subvariants, and undetectable IgG titers against S protein from XBB.1.5 subvariant, all of which were significantly lower than those induced by one dose of MVA-S(3P) (Fig. 3C, left). On day 26 post-boost, serum anti-S IgG titers increased in all four vaccination groups, with high IgG titers against the S protein from Beta and Omicron BA.1, comparable to those against the S protein from Wuhan (Fig. 3C, right). However, serum IgG titers against the S protein from Omicron BA.5 and XBB.1.5 subvariants were lower across all vaccination regimens, with MVA-S(3P)/MVA-S(3P) and MVA-S(3P)/NDV-HXP-S inducing the highest IgG titers, followed by NDV-HXP-S/MVA-S(3P), which induced significant higher titers than NDV-HXP-S/NDV-HXP-S (Fig. 3C, right).
The neutralization capacity against live SARS-CoV-2 Wuhan strain (MAD6 isolate, D614G), was measured on serum samples collected at day 26 post-boost (2 days pre-challenge) and at days 5 and 17 post-challenge using microneutralization (MNT) assays (Fig. 3D). At day 26 post-boost, serum NT50 titers against the ancestral Wuhan D614G SARS-CoV-2 strain were comparable among the NDV-HXP-S/NDV-HXP-S, MVA-S(3P)/NDV-HXP-S, and NDV-HXP-S/MVA-S(3P) vaccination regimens (Fig. 3D). The NDV-HXP-S/MVA-S(3P) regimen showed again a trend toward higher NT50 titers compared to the other two regimens, with all three groups inducing significantly higher NT50 titers than the MVA-S(3P)/MVA-S(3P) regimen (Fig. 3D). Interestingly, by day 5 post-challenge, serum NT50 titers against the ancestral Wuhan D614G SARS-CoV-2 increased in the MVA-S(3P)/NDV-HXP-S and NDV-HXP-S/MVA-S(3P) heterologous vaccination regimens compared to day 26 post-boost. These titers were slightly higher than those induced by the NDV-HXP-S/NDV-HXP-S homologous regimen, with all three groups showing significantly higher NT50 titers than the MVA-S(3P)/MVA-S(3P) homologous regimen at this time point (Fig. 3D). By day 17 post-challenge, the MVA-S(3P)/MVA-S(3P) and NDV-HXP-S/NDV-HXP-S homologous regimens further increased serum NT50 titers against the ancestral Wuhan D614G SARS-CoV-2 compared to day 5 post-challenge. In contrast, the MVA-S(3P)/NDV-HXP-S and NDV-HXP-S/MVA-S(3P) heterologous regimens showed a modest decline in serum NT50 titers compared to day 5 post-challenge (Fig. 3D), possibly reflecting reduced antigenic stimulation due to early viral clearance. At this time point, the NDV-HXP-S/NDV-HXP-S regimen induced significantly higher serum NT50 titers than the MVA-S(3P)/MVA-S(3P) and MVA-S(3P)/NDV-HXP-S regimens (Fig. 3D).
Next, we analysed the NT50 titers against other live SARS-CoV-2 variants in pooled sera collected on day 26 post-boost (2 days pre-challenge). Serum NT50 titers against the Beta variant were high but consistently lower than those against the ancestral Wuhan D614G SARS-CoV-2 across all vaccination groups, following a similar pattern among groups (Fig. 3E). Against the Omicron BA.1 and BA.5 subvariants, only the MVA-S(3P)/NDV-HXP-S and NDV-HXP-S/MVA-S(3P) heterologous vaccination regimens elicited detectable and comparable serum NT50 titers. Notably, only the MVA-S(3P)/NDV-HXP-S heterologous vaccination regimen elicited detectable serum NT50 titers against the Omicron XBB.1.5 subvariant (Fig. 3E), although results were based on pooled samples and should be interpreted with caution.
Finally, to evaluate mucosal humoral responses, we measured anti-S Wuhan IgA and IgG levels by ELISA in pooled NW collected at day 17 post-challenge. The results showed that mice vaccinated intranasally with NDV-HXP-S exhibited higher anti-S Wuhan IgA levels than those in the MVA-S(3P)/MVA-S(3P) group, with the NDV-HXP-S/MVA-S(3P) regimen inducing the highest levels among the tested regimens, although differences were not statistically significant (Fig. 3F). Regarding mucosal anti-S Wuhan IgG levels, both the NDV-HXP-S/NDV-HXP-S and NDV-HXP-S/MVA-S(3P) vaccination groups induced higher levels compared to the MVA-S(3P)/NDV-HXP-S and MVA-S(3P)/MVA-S(3P) groups, with the NDV-HXP-S/NDV-HXP-S regimen showing a trend toward even higher levels, although differences were not statistically significant (Fig. 3G).
Immunization with NDV and MVA viral vectors elicits SARS-CoV-2 S-specific CD4+ and CD8+ T-cell responses after virus challenge in K18-hACE2 transgenic mice
While all four immunizations regimens with NDV-HXP-S and MVA-S(3P) elicited systemic and mucosal SARS-CoV-2-specific humoral responses, it was of interest to assess the degree of activation of T cells. First, to evaluate systemic T-cell responses, we analysed SARS-CoV-2 S-specific CD4+ and CD8+ T cells in splenocytes from K18-hACE2 mice vaccinated with the four different MVA-S(3P) and NDV-HXP-S prime/boost regimens, collected on day 17 post-challenge (Fig. 4). Splenocytes were stimulated ex vivo with a mixture of Wuhan S peptide pools (spanning the entire S protein) and an intracellular cytokine staining (ICS) assay was performed to measure the induction of SARS-CoV-2 Wuhan S-specific CD4+ and CD8+ T cells expressing CD107a, and/or secreting IFNγ, and/or TNFα, and/or IL-2. The results showed that all vaccinated mice elicited systemic S-specific CD4+ and CD8+ T-cell responses, which were mainly mediated by CD8+ T lymphocytes (Fig. 4). Mice vaccinated with MVA-S(3P)/MVA-S(3P) and NDV-HXP-S/MVA-S(3P) elicited significantly higher S-specific CD4+ and CD8+ T-cell responses than the other vaccination groups (Fig. 4A), which also exhibited the greatest polyfunctional response, with the majority of S-specific CD4+ and CD8+ T cells displaying two or more functions (Fig. 4B). The analysis of the memory phenotype of systemic S-specific CD4+ and CD8+ T cells (measuring in S-specific T cells the expression of CD127 and CD62L surface markers, which defined different memory subpopulations: T central memory (Tcm; CD127+/CD62L+), T effector memory (Tem; CD127+/CD62L−), and T effector (Te; CD127−/CD62L−) cells) showed that in all vaccination groups, S-specific CD4+ and CD8+ T cells were mainly of the Te and Tem phenotypes, with the combination of MVA-S(3P)/MVA-S(3P) and NDV-HXP-S/MVA-S(3P) triggering the highest Te and Tem responses (Fig. 4C).
Systemic SARS-CoV-2 S-specific T-cell responses, directed against S peptide pools, were analysed in splenocytes obtained at day 17 post-challenge, and evaluated by ICS, as described in Materials and Methods. A Magnitude of systemic S-specific CD4+ (left panel) and CD8+ (right panel) T-cell responses in spleens. Percentages of CD4+ or CD8+ T cells expressing CD107a and/or producing IFNγ and/or TNFα and/or IL-2. P values were determined as described in Materials and Methods using an approach that corrects measurements for the medium response, calculating confidence intervals (***p < 0.001). B Polyfunctional profile (based on expression of selected markers CD107a, IFNγ, TNFα, and IL-2) of total systemic S-specific CD4+ (left panel) and CD8+ (right panel) T-cell responses in spleens. The response profiles are shown on the x axis, and the percentages of T cells for each of the vaccination groups are shown on the y axis. The pie charts summarize the percentage of S-specific T cells exhibiting one, two, three, or four markers, which are shown color coded. C Memory phenotypic profiles of the systemic S-specific CD4+ and CD8+ T cells. Percentages of naive (CD127−/CD62L+), T central memory (Tcm) (CD127+/CD62L+), T effector memory (Tem) (CD127+/CD62L−), and T effector (Te) (CD127−/CD62L−) CD4+ (left panel) or CD8+ (right panel) T cells expressing CD107a, and/or secreting IFN-γ, TNF-α, and IL-2 in response to stimulation with S peptide pools.
Next, we assessed local SARS-CoV-2 S-specific T-cell responses in lung cells from K18-hACE2 mice vaccinated with the four MVA-S(3P) and NDV-HXP-S prime/boost regimens, collected on day 17 post-challenge (Fig. 5). Lung cells were stimulated ex vivo with the same Wuhan S peptide pools used for splenocyte analysis. The results showed that all vaccinated mice elicited mucosal S-specific CD8+ T-cell responses, whereas CD4+ T cells were not detected (Fig. 5). Notably, mice vaccinated with NDV-HXP-S/NDV-HXP-S elicited significantly higher S-specific CD8+ T-cell responses than the other groups (Fig. 5A). These responses were polyfunctional (Fig. 5B) and predominantly of a Te phenotype (Fig. 5C).
Pulmonary SARS-CoV-2 S-specific T-cell responses, directed against S peptide pools, were analysed in lung cells obtained at day 17 post-challenge, and evaluated by ICS, as described in Materials and Methods. A Magnitude of mucosal S-specific CD8+ T-cell responses in lung cells. Percentages of CD8+ T cells expressing CD107a and/or producing IFNγ and/or TNFα and/or IL-2. P values were determined as described in Materials and Methods using an approach that corrects measurements for the medium response, calculating confidence intervals (**p < 0.002; ***p < 0.001). B Polyfunctional profile (based on expression of selected markers CD107a, IFNγ, TNFα, and IL-2) of total mucosal S-specific CD8+ T-cell responses in lung cells. The response profiles are shown on the x axis, and the percentages of CD8+ T cells for each of the vaccination groups are shown on the y axis. The pie charts summarize the percentage of S-specific CD8+ T cells exhibiting one, two, three, or four markers, which are shown color coded. C Memory phenotypic profiles of the mucosal S-specific CD8+ T cells. Percentages of naive (CD127−/CD62L+), T central memory (Tcm; CD127+/CD62L+), T effector memory (Tem; CD127+/CD62L−), and T effector (Te; CD127−/CD62L−) CD8+ T cells expressing CD107a, and/or secreting IFN-γ, TNF-α, and IL-2 in response to stimulation with S peptide pools.
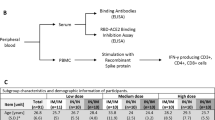
Immunization with NDV and MVA viral vectors encoding SARS-CoV-2 S protein protects hamsters challenged with SARS-CoV-2
Golden Syrian hamsters are considered the gold standard for immunogenicity and vaccine protection against SARS-CoV-2 infection. Hence, we next employed this animal model to study the protective efficacy against direct exposure to SARS-CoV-2 and SARS-CoV-2 transmission of homologous and heterologous prime/boost immunization regimens with MVA-S(3P) and NDV-HXP-S vaccines. Eight female Golden Syrian hamsters per group were first immunized intramuscularly with 1 x 108 PFUs of MVA-S(3P) or intranasally with 1 x 106 EID50 of NDV-HXP-S, and a second dose was administered four weeks after the first dose, as indicated in Fig. 6A. Hamsters inoculated with PBS, empty MVA or NDV viral vectors were included as control groups. Four weeks after the booster dose, hamsters were challenged intranasally with 1 x 105 PFUs of SARS-CoV-2 (Wuhan New York (NY) isolate, containing D614G mutation). Body weight was monitored for 5 days post-challenge. All vaccination groups were protected against body weight loss, whereas viral vector control groups lost over 10% of body weight by 5 days post-challenge (Fig. 6B). To assess the effect of vaccination on viral replication in all vaccination groups, throat swab samples were collected at days 1, 3 and 5 post-challenge and processed for the presence of SARS-CoV-2 genomic RNA copies. Compared with the control groups, all intranasally vaccination groups with NDV-HXP-S (NDV-HXP-S/NDV-HXP-S, MVA-S(3P)/NDV-HXP-S and NDV-HXP-S/MVA-S(3P)) showed a reduction in genomic RNA copies on days 3 and 5 post-challenge, while MVA-S(3P)/MVA-S(3P) displayed higher genomic RNA levels than the NDV-HXP-S-based groups but still lower levels than the control groups, which remained consistent on both days (Fig. 6C). Infectious SARS-CoV-2 was measured in nasal turbinates and right lung lobes (upper and lower) at days 2 and 5 post-challenge. Compared with the control groups, the intranasally vaccination groups with NDV-HXP-S exhibited a similarly significant reduction in viral titers in the upper respiratory tract, as measured in the nasal turbinates on day 2 post-challenge; all vaccination groups showed no detectable infectious virus on day 5 post-challenge (Fig. 6D). In the lower respiratory tract (upper and lower right lung lobes), no infectious SARS-CoV-2 was detected in the four vaccination groups at any of the two time points analysed, compared to the control groups (Fig. 6E). Further histopathology analyses on the left lung lobes collected on day 5 post-challenge confirmed protection, showing significantly lower or undetectable levels of necrosis and inflammation in all vaccination groups compared to control groups (Fig. 6F, Supplementary Fig. 1).
A Design of the study. Six- to eight-week-old female Golden Syrian hamsters were used. Groups 1-4 (n = 8/group) were vaccinated with either homologous or heterologous prime/boost regimens with NDV-HXP-S and MVA-S(3P). Groups 5 and 6 were vaccinated with empty MVA and NDV viral vectors as negative control. Group 7 was inoculated with PBS as healthy control. NDV viral vector vaccine was administrated via intranasal (IN) route and MVA viral vector vaccine was administrated via intramuscular (IM) route at days 0 and 28. Serum was collected at day 55 (1 day pre-challenge). Vaccination groups 1-6 were challenged with 1 ×105 PFUs of SARS-CoV-2 New York strain at day 56, while group 7 was mock challenged with PBS. Throat swabs were collected at days 1, 3 and 5 post-challenge. A subset of hamsters (n = 4/group) were euthanized at days 2 and 5 post-challenge to harvest lungs lobes (upper right lung lobe and lower right lung lobe) and nasal turbinates. B Body weight change of hamsters. Body weight was monitored for 5 days post-challenge. C Genomic viral RNA copies in throat swabs. Throat swabs were collected in 200 μL of PBS at days 1, 3 and 5 post-challenge and SARS-CoV-2 N genomic copies detected by RT-qPCR. The geometric mean with geometric SD of values from triplicates of each sample for each group are represented. The dotted line represents the LOD, and the dashed line represents the limit of quantification (LOQ). Two-way ANOVA followed by Tukey’s multiple comparisons test: *p < 0.033; **p < 0.002. (D) Viral load in the nasal turbinates. Nasal turbinates were collected from vaccination groups 1-6 and the healthy control group at days 2 and 5 post-challenge and homogenized in 0.5 mL of PBS. Viral titers were measured by plaque assay on Vero-E6 cells. The geometric mean with geometric SD of values (PFUs/mL) of each sample for each group are represented. The dotted line represents the LOD. Two-way ANOVA followed by Tukey’s multiple comparisons test: ****p < 0.0001. E Viral load in the lungs. The upper and lower right lung lobes were collected at days 2 and 5 post-challenge and homogenized in 1 mL of PBS. Viral titers were measured by plaque assay on Vero-E6 cells. The geometric mean with geometric SD of values (PFUs/mL) of each sample for each group are represented. The dotted line represents the LOD. Two-way ANOVA followed by Tukey’s multiple comparisons test: ****p < 0.0001. F Pathology analyses of the left lung lobes. Left lung lobes from vaccination groups collected at day 5 post-challenge were fixed in 4% paraformaldehyde, cut into 5 µm sections and stained with H&E. The slides were evaluated by a pathologist who was blinded to the group information. The scoring system is shown in Supplementary Table 1. The geometric mean with geometric SD of cumulative histopathological lesion scores are represented. The dotted line represents the LOD. Unpaired nonparametric Kruskal-Wallis test: ****p < 0.0001.
Immunization with NDV and MVA viral vectors induces potent SARS-CoV-2-specific antibody responses in hamsters
We next evaluated SARS-CoV-2-specific systemic humoral responses in serum samples from hamsters vaccinated with the four different vaccination regimens indicated in Fig. 6. Anti-S and anti-receptor-binding domain (RBD) (both from Wuhan) IgG titers were measured by ELISA at four weeks post-boost in individual serum samples. Serum anti-RBD IgG titers in all four vaccination groups ranged between 104 and 106, with the NDV-HXP-S/MVA-S(3P) vaccination regimen eliciting the highest titers. In contrast, the MVA-S(3P)/MVA-S(3P) group induced significantly lower titers compared to the other three regimens (Fig. 7A). However, serum anti-S IgG titers were comparable across all four vaccination groups, ranging between 105 and 106 (Fig. 7B). The neutralization capacity of pooled serum samples obtained four weeks post-boost was measured using a neutralization assay against pseudo-typed SARS-CoV-2 ancestral, Delta, Omicron BA.1, or Omicron XBB.1.5 viruses. Serum fifty percent inhibitory dilution (ID50) titers were lower in the MVA-S(3P)/MVA-S(3P) group compared to the other three regimens (Fig. 7C). All vaccination groups induced in serum samples higher titers of neutralizing antibodies against the ancestral and Delta variant, followed by the Omicron BA.1. Of note none of the vaccination groups exhibited neutralization against Omicron XBB.1.5 variant (Fig. 7C).
A, B Anti-RBD (A) and anti-S (B) IgG titers against Wuhan determined by ELISA in individual serum samples collected from hamsters at day 27 post-boost (day 55; 1 day pre-challenge). The geometric mean with geometric SD of endpoint titers from duplicates of each sample for each group are represented. The dotted line represents the LOD. Ordinary one-way ANOVA of transformed data followed by Tukey’s multiple comparison test: *p < 0.033; **p < 0.002; ***p < 0.0002; ****p < 0.0001. C SARS-CoV-2 neutralizing antibody titers against ancestral SARS-CoV-2 and variants of concern. ID50 titers against Wuhan, Delta, Omicron BA.1, and XBB.1.5 were evaluated in pooled hamster serum samples collected at day 27 post-boost (day 55; 1 day pre-challenge), using a pseudo-virus neutralization assay. The geometric mean with geometric SD of ID50 titers of each pooled group sample are represented. The dotted line represents the LOD. Two-way ANOVA followed by Tukey’s multiple comparisons test: *p < 0.033; **p < 0.002; ****p < 0.0001.
Immunization with NDV and MVA viral vectors encoding SARS-CoV-2 S protein reduces direct contact transmission of SARS-CoV-2 in a hamster model
To further assess the protective efficacy of homologous and heterologous prime/boost immunization regimens on direct contact transmission, four index hamsters from each immunization group (Fig. 6) were cohoused on day 1 post-challenge with four naïve hamsters, forming the recipient groups (RGs) (Fig. 8A). Specifically, each naïve hamster was cohoused individually with one infected index hamster, with two hamsters per cage, allowing precise monitoring of transmission dynamics under controlled conditions. Body weight remained stable in all RGs cohoused with vaccinated hamsters after 4 days of cohouse, indicating protection against weight loss compared to control groups (Fig. 8B). In trend with the significantly lower viral shedding observed in animals vaccinated intranasally with NDV-HXP-S (Fig. 6C), a significantly lower viral shedding was observed in throat swabs from their corresponding recipient hamsters at days 3 and 5 post-challenge (days 2 and 4 post-cohouse), compared to homologous MVA-S(3 P)/MVA-S(3P) vaccination and the control groups (Fig. 8C). In line with these findings, infectious SARS-CoV-2 was undetectable in nasal turbinates and lung tissues (upper and lower lobes) in at least three out of four RG hamsters cohoused with NDV-HXP-S-vaccinated animals (Fig. 8D, E). In contrast, RGs exposed to MVA-S(3P)/MVA-S(3P) or control donors showed higher levels of infectious virus in all tissues analysed. Lung histopathology on day 5 post-challenge (day 4 post-cohouse) revealed significantly reduced inflammation and necrosis in RGs cohoused with NDV-HXP-S-vaccinated animals compared to controls (Fig. 8F, Supplementary Fig. 1). Notably, the heterologous NDV-HXP-S/MVA-S(3P) regimen resulted in undetectable infectious virus and minimal lung pathology in all four recipient animals, while the NDV-HXP-S/NDV-HXP-S and MVA-S(3P)/NDV-HXP-S regimens also conferred partial protection, with at least three out of four RG animals showing no detectable infectious virus and minimal lesions (Fig. 8D–F). However, these differences were not statistically significant, likely due to the limited number of animals per group, which represents a limitation of the study.
A Design of the study. Six- to eight-week-old female Golden Syrian hamsters were used. Four naïve hamsters per group were cohoused with challenged hamsters from vaccination groups 1-6 groups at day 1 post-challenge, forming the recipient groups (RGs). Throat swabs were collected at days 3 and 5 post-challenge. Hamsters from each RG were euthanized at day 5 post-challenge to harvest lungs lobes (upper right lung lobe and lower right lung lobe) and nasal turbinates. B Body weight change of recipient hamsters. Body weight was monitored for 5 days post-challenge. C Genomic viral RNA copies in throat swabs of recipient hamsters. Throat swabs of RGs were collected in 200 μL of PBS at days 3 and 5 post-challenge and SARS-CoV-2 N genomic copies detected by RT-qPCR. The geometric mean with geometric SD of values from triplicates of each sample for each group are represented. The dotted line represents the LOD, and the dashed line represents the LOQ. Two-way ANOVA followed by Tukey’s multiple comparisons test: ***p < 0.0002; ****p < 0.0001. D Viral load in the nasal turbinates of recipient hamsters. Nasal turbinates were collected from RG 1-6 and the healthy control group at day 5 post-challenge and homogenized in 0.5 ml of PBS. Viral titers were measured by plaque assay on Vero-E6 cells. The geometric mean with geometric SD of values (PFUs/mL) of each sample for each group are represented. The dotted line represents the LOD. Ordinary one-way ANOVA of transformed data followed by Tukey’s multiple comparison test: **p < 0.002; ***p < 0.0002; ****p < 0.0001. E Viral load in the lungs of recipient hamsters. The upper and lower right lung lobes were collected at day 5 post-challenge and homogenized in 1 mL of PBS. Viral titers were measured by plaque assay on Vero-E6 cells. The geometric mean with geometric SD of values (PFUs/mL) of each sample for each group are represented. The dotted line represents the LOD. Ordinary one-way ANOVA of transformed data followed by Tukey’s multiple comparison test: *p < 0.033; **p < 0.002; ***p < 0.0002; ****p < 0.0001. F Pathology analyses of the left lung lobes of recipient hamsters. Left lung lobes from RGs collected at day 5 post-challenge were fixed in 4% paraformaldehyde, cut into 5 µm sections and stained with H&E. The slides were evaluated by a pathologist who was blinded to the group information. The scoring system is shown in Supplementary Table 1. Mean and SD of cumulative histopathological lesion scores are represented. The dotted line represents the LOD. Unpaired nonparametric Kruskal-Wallis test: *p < 0.033; **p < 0.002; ***p < 0.0002.
Discussion
The emergence of SARS-CoV-2 variants capable of evading immunity from prior infection or vaccination has posed significant challenges for ongoing vaccination strategies, particularly in terms of booster coverage and vaccine supply. In this context, heterologous prime/boost vaccination represents a promising approach to enhance immune responses and broaden protection. This strategy involves the sequential administration of different vaccine platforms or vectors encoding the same or different antigens. Compared to homologous regimens, heterologous combinations have been reported to elicit stronger and more durable immune responses, and in certain settings, improved protective efficacy in preclinical and clinical studies3,26,27. These benefits are especially evident when heterologous boosters are used following vector-based priming, as reviewed elsewhere3,26,27. Early studies in HIV and malaria models demonstrated improved protection when combining distinct vaccine platforms, with efficacy depending on the order of administration28,29. More recently, heterologous vector combinations, such as chimpanzee adenovirus followed by MVA, have proven safe and immunogenic in clinical trials for Ebola23. Similar strategies have shown enhanced T-cell responses in malaria vaccine studies25. Moreover, heterologous prime/boost immunization regimens using different vaccine platforms (e.g., mRNA, protein, inactivated, and viral vectors) have generally induced stronger humoral and T-cell responses against SARS-CoV-2 than homologous regimens, as shown in preclinical and clinical studies30,31,32,33,34,35. These findings highlight the potential advantage of heterologous prime/boost vaccination against SARS-CoV-2. To our knowledge, our study is the first one that evaluate the combination of two distinct viral-vector COVID-19 vaccines (NDV and MVA-based) in a heterologous prime/boost strategy against SARS-CoV-2. Heterologous prime/boost regimens using NDV- and MVA-based vaccines have been previously tested against different pathogens, such as H5N1 avian influenza virus36 and avian bornaviruses37,38,39, yielding promising results.
Here, we studied the immunogenicity and efficacy against SARS-CoV-2 infection in virus susceptible transgenic K18-hACE2 mice and Golden Syrian hamsters immunized with different homologous and heterologous prime/boost vaccine combinations that include two viral vector-based vaccine candidates encoding a prefusion-stabilized SARS-CoV-2 S protein (NDV-HXP-S and MVA-S(3P)). Both vaccine candidates have previously demonstrated to be highly efficacious in protecting against SARS-CoV-2 infection in different animal models and against different SARS-CoV-2 variants8,9,10,11,12,13,14,15,16. Moreover, NDV-HXP-S has entered several phase 1/2 clinical trials, proving to be safe and immunogenic17,18,19,20. All four prime/boost vaccine regimens provided comparable protection against SARS-CoV-2 in both animal models, significantly reducing, compared to controls groups, viral RNA in NW (in mice), throat swabs (in hamsters), and lungs (in mice and hamsters), as well as viral loads in the lungs (in mice and hamsters) and nasal turbinates (in hamsters), and levels of lung pro-inflammatory cytokines (in mice), with only mild and occasional lung histopathological lesions. Notably, hamsters vaccinated intranasally with NDV-HXP-S exhibited a trend toward a more rapid reduction in viral RNA levels in throat swabs, along with a significantly lower viral load in nasal turbinates, highlighting the importance of the route of administration in controlling infection at the mucosal entry site. As infection controls, we used PBS-inoculated mice to establish a disease baseline and empty vector–inoculated hamsters to assess innate responses in transmission studies. We acknowledge the need for consistency and plan to include both control types in future studies to better dissect innate immunity.
Beyond the protective effect observed in both mice and hamsters, all vaccination regimens elicited robust SARS-CoV-2-specific humoral and T-cell responses at both systemic and mucosal levels, responses that have been associated with protective immunity40. All vaccination groups elicited comparable high titers of binding anti-S (or anti-RBD) IgG and neutralizing antibodies in the serum of mice and hamsters, similar to those induced in mice immunized with the authorized Pfizer-BioNTech mRNA vaccine, BNT162b241,42. Furthermore, we have previously compared the SARS-CoV-2 neutralizing and S protein-binding activity of postvaccination sera from individuals receiving the NDV-HXP-S vaccine to those vaccinated with the mRNA vaccine BNT162b2 (Pfizer-BioNTech). The results from a phase I clinical trial in Thailand demonstrated that NDV-HXP-S vaccinees generated a higher proportion of neutralizing antibodies and higher absolute neutralizing antibody titers against SARS-CoV-2 than individuals vaccinated with BNT162b2, with a response more focused on the RBD43. In addition, studies in hamsters have shown that, similar to our findings (where intranasal administration of NDV-HXP-S, either in homologous or heterologous prime/boost regimens, prevented direct contact transmission of SARS-CoV-2) mucosal (intranasal) immunization with a chimpanzee adenoviral-vectored SARS-CoV-2 vaccine (ChAd-SARS-CoV-2-S) effectively prevents sequential transmission of SARS-CoV-2 to unvaccinated hamsters. In contrast, intramuscular (systemic) immunization with a mRNA COVID-19 vaccine did not block virus replication in the lungs or sequential SARS-CoV-2 transmission in hamsters44. All these results suggest that the immune responses and protective efficacy induced by the NDV-HXP-S and MVA-S(3P) vaccine candidates appear comparable to those reported for established mRNA and adenovirus-vectored vaccines in similar models, suggesting their potential as complementary options in vaccination strategies. However, future investigations involving direct comparisons of NDV-HXP-S and MVA-S(3P) vaccine candidates with standard approved COVID-19 vaccines, such as mRNA-based and adenovirus-vectored vaccines, are needed and will offer a broader perspective. This will help further define the role of the NDV-HXP-S and MVA-S(3P) vaccine candidates in the control of SARS-CoV-2 infection and highlight the potential advantages of heterologous prime/boost NDV/MVA strategies in achieving durable and broad-spectrum immunity.
In addition, the analysis of serum neutralizing capacity against different variants in both animal models revealed that, although all vaccination groups induced high neutralizing antibody titers against ancestral SARS-CoV-2 and earlier variants such as Beta or Delta, the heterologous combinations tended to elicit modest but detectable neutralizing antibodies against more recent Omicron subvariants, such as BA.1 or BA.5 in the mouse model, and BA.1 in the hamster model. Additionally, in mice, we observed the induction of S-specific CD4+ and CD8+ T-cell responses in the spleen, with the MVA-S(3P)/MVA-S(3P) and the NDV-HXP-S/MVA-S(3P) regimens generating a higher magnitude of CD4+ and CD8+ T cells compared to the NDV-HXP-S/NDV-HXP-S and MVA-S(3P)/NDV-HXP-S groups.
Mucosal SARS-CoV-2-specific humoral and T-cell responses were also effectively induced in our study. Mucosal antibodies, such as secretory IgAs, play a crucial role in neutralizing pathogens at the entry site and preventing viral dissemination45, while lung tissue-resident memory T cells provide long-lasting protection against respiratory viruses46. Consistent with this, higher levels of anti-S IgA and IgG antibodies were detected in NW of mice intranasally immunized with NDV-HXP-S, along with S-specific CD8+ T-cell responses in lung cells, compared to the homologous MVA-S(3P)/MVA-S(3P) regimen, in which MVA-S(3P) was administered intramuscularly. Specifically, NDV-HXP-S/MVA-S(3P) induced higher levels of anti-S IgA antibodies in NW, whereas NDV-HXP-S/NDV-HXP-S elicited a higher magnitude of S-specific CD8+ T-cells in lung cells. These findings align with numerous preclinical and clinical studies, demonstrating that intranasal immunization elicits strong neutralizing antibody production, as well as mucosal IgA and T-cell responses, which help prevent SARS-CoV-2 infection in both the upper and lower respiratory tracts (reviewed in ref. 47). Consistent with our results, previous studies in multiple animal models have also demonstrated that intranasal administration of NDV-vectored vaccines encoding the SARS-CoV-2 S protein induces strong mucosal IgA responses and tissue-resident memory T cells in the respiratory tract, significantly reducing viral loads in both the nasal cavity and lungs10,11,48,49,50. Our results highlight the importance of mucosal vaccine delivery in eliciting robust local immunity to protect against respiratory viruses. Since NDV- and MVA-based vaccines can be administered intranasally, they have the potential to elicit strong mucosal and pulmonary immune responses at the respiratory epithelium, the primary site of SARS-CoV-2 infection, effectively blocking viral entry. This leads to enhanced protection throughout the respiratory tract, limiting viral spread, and potentially preventing transmission. Future investigations should further evaluate vaccine efficacy at mucosal surfaces to fully understand the protective capacity of these vaccination strategies. Such investigations will provide deeper insights into the immune mechanisms triggered by NDV-HXP-S and MVA-S(3 P), reinforcing their potential as intranasal vaccine candidates.
Regarding the viral transmission study in hamsters, recipient groups RG5 and RG6 (cohoused with NDV-WT/NDV-WT and MVA-WT/MVA-WT donor hamsters, respectively) exhibited weight loss and viral loads in respiratory tissues comparable to those observed in animals vaccinated with NDV-WT/NDV-WT or MVA-WT/MVA-WT and directly challenged with SARS-CoV-2, indicating efficient transmission of the virus. These results reflect robust viral transmission in the hamster model, consistent with previous studies employing similar experimental designs that reported comparable findings regarding SARS-CoV-2 transmission dynamics and viral loads in cohoused hamsters51,52,53. Notably, all vaccination regimens that included intranasal NDV-HXP-S immunization reduced SARS-CoV-2 replication in cohoused unvaccinated animals, as evidenced by decreased viral RNA in throat swabs and lower or undetectable infectious virus in nasal turbinates and lungs, compared to MVA-S(3P)/MVA-S(3P) and control groups. Only the NDV-HXP-S/MVA-S(3P) group showed a complete absence of live virus in all tested respiratory tissues in all animals tested, suggesting an enhanced capacity to control infection and prevent effective transmission in this model, although the limited sample size precludes definitive conclusions. Our definition of transmission is based on the detection of viable virus in tissues rather than on transient viral RNA detection in throat swabs. Nonetheless, additional studies with larger sample sizes and the quantification of subgenomic viral RNA will be required to confirm this finding and to assess potential differences in transmission-blocking efficacy between regimens. Several studies have demonstrated the capacity of intranasally administered COVID-19 vaccines to reduce transmission in hamster models44,54,55, reinforcing the importance of using mucosal administration to better prevent transmission. These data underscore the potential of mucosal vaccination strategies to limit virus spread, but should be interpreted with caution given the exploratory nature of the transmission model used. The mechanism of protection against transmission is not fully understood, but some studies suggest that mucosal IgA and lung T-cell responses could be responsible for this transmission protection44.
Another important factor to take into consideration is the order of vaccine administration. A prime-pull strategy, which involves a systemic prime immunization to induce a strong immune response followed by a mucosal boost to “pull” immune effectors into mucosal tissues, has been shown to enhance local immunity at mucosal surfaces and can provide enhanced protection against respiratory pathogens56,57,58. Interestingly, in our study, the heterologous regimen with intranasal priming using NDV-HXP-S followed by intramuscular boosting with MVA-S(3P) was at least as immunogenic and effective, and in some parameters, more immunogenic and effective than the reverse regimen with intramuscular NDV-HXP-S priming and intranasal MVA-S(3P) boosting. Specifically, the NDV-HXP-S/MVA-S(3P) prime/boost regimen induced broader neutralization potency, as well as higher systemic CD4+ and CD8+ T-cell responses and mucosal anti-S IgA and IgG antibodies, than the MVA-S(3P)/NDV-HXP-S vaccination regimen. Furthermore, among all regimens evaluated in the hamster transmission study, only the NDV-HXP-S/MVA-S(3P) prime/boost strategy completely eliminated live virus loads in the lungs and nasal turbinates of all cohoused hamsters; however, the limited sample size precludes definitive conclusions. These results indicate that the sequence of the vaccination impacts the magnitude of immune response induction and the level of protection. This phenomenon was observed for malaria in 1993, where a prime injection with recombinant vaccinia virus followed by a booster injection with recombinant influenza virus, failed to induce protection, while the reverse combination was highly effective in protection against the parasite29. Moreover, these results also suggests that intranasal priming with NDV-HXP-S may play a unique role in shaping both systemic and mucosal (or local respiratory) immune responses, potentially through the early induction of mucosal antibodies and pulmonary tissue-resident memory T cells59. Several studies have shown that intranasal priming can establish robust mucosal immunity that is further enhanced by a subsequent systemic boost, resulting in strong cross-talk between both compartments60. NDV-based vectors are particularly well-suited for intranasal administration, as they efficiently target respiratory epithelial cells and elicit both secretory IgA and T-cell responses in the respiratory tract9,61. Additionally, it is well established that MVA-based vaccines serve as potent systemic boosters62,63. These factors likely explain the superior or comparable protection observed with the intranasal NDV-HXP-S prime/intramuscular MVA-S(3P) boost regimen compared to the intramuscular MVA-S(3P) prime/intranasal NDV-HXP-S pull strategy. Together with other findings64,65,66, these results support the concept that heterologous prime/boost regimens with live viral vectors encoding the appropriate proteins or epitopes represent a promising vaccination strategy.
Although anti-vector immunity is a known concern with repeated use of the same viral vector, the homologous NDV-HXP-S/NDV-HXP-S and MVA-S(3P)/MVA-S(3P) regimens elicited strong humoral and T-cell responses and conferred robust protection. This suggests that anti-NDV and anti-MVA immunity did not significantly impair the SARS-CoV-2-specific immunogenicity or efficacy induced by NDV-HXP-S and MVA-S(3P) vaccine candidates in either animal model, consistent with our previous findings9,67. Consequently, employing different viral vector vaccines to circumvent anti-vector immunity remains a potential advantage.
Finally, we acknowledge several limitations of our study. The relatively small sample sizes, especially in the hamster transmission experiments, limit the statistical power to compare vaccination regimens. Future animal studies with larger sample sizes will help to validate these findings and establish optimal vaccination strategies for long-term protection against respiratory viruses. Moreover, future studies should include NDV and MVA vector vaccines adapted to new emerging SARS-CoV-2 variants and longer follow-up periods to assess the durability and breadth of protection, increasing the translational relevance of vaccine studies. Direct head-to-head comparisons with approved mRNA or adenovirus-vectored vaccines, along with other relevant platforms, will be important to define the translational potential of NDV/MVA heterologous strategies and to contextualize safety, immunogenicity, protective efficacy, ease of administration, and manufacturing scalability/costs. Moreover, given the known neuroinvasion of SARS-CoV-2 in the K18-hACE2 mouse model, and that a single intramuscular dose of an MVA-based vaccine expressing the ancestral SARS-CoV-2 Wuhan S protein (MVA-S) was sufficient to prevent viral replication and brain damage in the brain68, future studies assessing NDV-based or heterologous NDV/MVA combinations should include systematic analysis of viral replication and pathology in central nervous system tissues to confirm the extent of neuroprotection. Despite these limitations, our findings support the feasibility of combining mucosal and systemic vaccination with NDV and MVA vaccine platforms to enhance protection against disease, with potential to also limit transmission.
In summary, our study provides a comprehensive comparative evaluation of the immunogenicity and protective efficacy against SARS-CoV-2 of two clinically relevant viral vectors (NDV and MVA) administered via different routes, in both homologous and heterologous prime/boost regimens, across two complementary animal models (K18-hACE2 mice and Golden Syrian hamsters). The simultaneous assessment of immunogenicity, protection from disease, and transmission-blocking potential in these models enhances the translational relevance of our findings. We believe this integrated approach contributes valuable insights into the development of heterologous vaccination strategies, supporting future outbreak preparedness and the advancement of viral vector platforms.
Methods
Animals and ethics statement
Female transgenic K18-hACE2 mice [034860-B6. Cg-Tg(K18-ACE2)2Prlmn/J, genetic background C57BL/6 J x SJL/J F2] (9 weeks-old at the beginning of the study), which express the human angiotensin converting enzyme-2 (ACE2) receptor and are susceptible to SARS-CoV-2 infection, were acquired from the Jackson Laboratory (through Charles River). Mouse immunizations were carried out in the biosafety level 2 (BSL-2) animal facility of the Centro Nacional de Biotecnología (CNB-CSIC) (Madrid, Spain), and then animals were transferred to the BSL-3 facilities at the Centro de Investigación en Sanidad Animal (CISA)-Instituto Nacional de Investigaciones Agrarias (INIA)-Consejo Superior de Investigaciones Científicas (CSIC) (Valdeolmos, Madrid, Spain), where SARS-CoV-2 challenge was performed. The Ethical Committees of Animal Experimentation (CEEA) of CSIC, CNB-CSIC and CISA-INIA-CSIC approved the mouse studies, which were authorized by the Division of Animal Protection of the Comunidad de Madrid (PROEX 169.4/20 and 161.5/20). Animal procedures followed the international guidelines and Spanish law under the Royal Decree (RD) 53/2013.
Female Golden Syrian hamsters (HsdHan®: AURA) were purchased from Inotiv and experiments were performed in accordance with protocols (PROTO202000098 and CEIRR program, 13-0386 PRYR II-IACUC-2013-1408) approved by the Institutional Animal Care and Use Committee (IACUC) at the Icahn School of Medicine at Mount Sinai (ISMMS). All hamster experiments with live SARS-CoV-2 were performed in the Centers for Disease Control and Prevention (CDC)/US Department of Agriculture (USDA)-approved BSL-3 biocontainment facility of the Global Health and Emerging Pathogens Institute at the ISMMS, in accordance with institutional biosafety requirements.
Cells
Vero-E6 cells (from African green monkey kidney, ATCC catalog number CRL-1586) were grown in Dulbecco’s modified Eagle’s medium (DMEM) (Gibco-Life Technologies) supplemented with HEPES (10 mM; Gibco-Life Technologies), non-essential amino acids (0.1 mM; Sigma-Aldrich), penicillin (100 U/mL; Sigma-Aldrich), streptomycin (100 mg/mL; Sigma-Aldrich), and 10% heat inactivated fetal bovine serum (FBS). Vero/TMPRSS2 (Vero-E6 cell line modified to constitutively express TMPRSS2 serine protease, under geneticin selection, in order to be highly susceptible to SARS-CoV-2 infection) were maintained in DMEM (Gibco-Life Technologies) supplemented with HEPES (10 mM; Gibco-Life Technologies), nonessential amino acids (0.1 mM; Sigma-Aldrich), penicillin (100 U/mL; Sigma-Aldrich), streptomycin (100 µg/mL; Sigma-Aldrich), Geneticin (G418, 1 mg/mL, Merck-Life Sciences), and 10% heat inactivated FBS. Baby hamster kidney cells stably expressing human ACE2 (BHK-ACE2) and BHK-derived cell line stably expressing T7 RNA polymerase (BSRT7) were also used in this study. BHK-ACE2 were maintained in DMEM (Gibco-Life Technologies) containing 10% (vol/vol) heat inactivated FBS, 100 U/mL of penicillin and 100 µg/mL of streptomycin (Gibco-Life Technologies). Cell cultures were maintained in a humidified incubator at 37 °C with 5% CO2.
Vaccine candidates
We have used in this study two vaccine candidates against COVID-19 based on poxvirus MVA and NDV as viral vectors. Regarding poxviruses, we have used the attenuated MVA wild-type (MVA-WT) poxvirus strain, derived from the Chorioallantois vaccinia virus Ankara strain69, and the recombinant MVA-S(3P) vaccine candidate13,14,15,16. MVA-S(3P) expresses a Wuhan derived human codon optimized full-length prefusion-stabilized SARS-CoV-2 S protein, containing 3 mutations in the furin cleavage site (R682G, R683S, and R685S) to prevent cleavage of the S protein in S1 and S2 domains, and 3 proline (3P) substitutions in the S2 region that stabilize the S protein in a prefusion conformation (A942P, K986P, and V987P), as previously described13,14,15,16. All MVA viruses were grown in permissive culture chicken cells (DF-1), purified by centrifugation through two 36% (wt/vol) sucrose cushions in 10 mM Tris-HCl (pH 9), and titrated in DF-1 cells using a plaque immunostaining assay, as previously described in ref. 70. All viral stocks were free of contamination with mycoplasma (checked by Mycoplasma Gel Detection kit; Biotools), bacteria (checked by growth on LB plates without ampicillin), or fungi (checked by growth on Columbia blood agar plates; Oxoid).
NDV-HXP-S vaccine encoding the prefusion-stabilized ancestral Wuhan SARS-CoV-2 S protein was produced as previously described in ref. 10. Briefly, 10- or 11-day old specific pathogen-free (SPF) embryonated chicken eggs (AvsBio, Norwich, CT, USA) were infected to produce the NDV-HXP-S vaccine candidate. After virus infection in the allantoic cavity, eggs were incubated at 37 °C for 3–4 days and cooled at 4 °C overnight10. To concentrate the viruses, allantoic fluids were clarified by centrifugation at 4000 rpm at 4 °C for 30 min using a Sorvall Legend RT Plus Refrigerated Benchtop Centrifuge (Thermo Fisher Scientific). Clarified allantoic fluids were laid on top of a 20% sucrose cushion in PBS (pH 7.4, Gibco-Life Technologies). Ultracentrifugation in a Beckman L7-65 ultracentrifuge at 25,000 rpm for 2 h at 4 °C using a Beckman SW28 rotor (Beckman Coulter, CA, USA) was performed to pellet the viruses through the sucrose cushion while soluble egg proteins were removed. The virus pellets were re-suspended in PBS (pH 7.4) and stored at −80 °C until use. Infectious virus titer was determined by EID5010.
SARS-CoV-2 viruses
The SARS-CoV-2 isolate MAD6, similar to the Wuhan strain but containing the D614G mutation in the S protein71, was kindly provided by Dr. José M. Honrubia and Prof. Luis Enjuanes (CNB-CSIC, Madrid, Spain), and was used to challenge K18-hACE2 mice. The stock virus was prepared as previously described in refs. 13,14,15,16. The SARS-CoV-2 isolate New York, similar to the Wuhan strain but containing the D614G mutation in the S protein, was used to challenge hamsters. The virus isolate was grown on Vero/TMPRSS2 cells and validated by whole genome sequencing using the next-generation sequencing platform MinION (Oxford Nanopore Technologies), following the manufacturer’s instructions.
The SARS-CoV-2 beta (B.1.351) variant (hCoV-19/France/PDL-IPP01065i/2021), was supplied through the European Virus Archive-Global (Evag) platform, a project funded by the European Union’s Horizon 2020 research and innovation programme under grant agreement No. 653316. The virus was sent by the National Reference Centre for Respiratory Viruses hosted by Institut Pasteur (Paris, France) headed by Pr. Sylvie van der Werf, and the human sample from which the virus was isolated by Dr. Besson J., Bioliance Laboratory, Saint-Herblain; France. The SARS-CoV-2 B.1.1.529 Omicron variant (hCoV-19/Belgium/rega-20174/2021, EPI_ISL_6794907) (also termed BA.1) was supplied by Prof. Piet Maes from KU Leuven (Belgium) through Dr. Robbert Boudewijns and Dr. Kai Dallmeier (KU Leuven, Belgium). The SARS-CoV-2 Omicron BA.5 (EPI_ISL_13424827) and XBB.1.5 (EPI_ISL_16939528) subvariants were kindly provided by Prof. Rafael Delgado (Hospital Universitario 12 de Octubre, Madrid, Spain). SARS-CoV-2 viral stocks were amplified by propagation in Vero/TMPRSS2 cells by inoculation at a multiplicity of infection of 0.001 PFUs/cell. Cell supernatants were harvested at 72 h post-infection (hpi), cleared by centrifugation, aliquoted, and stored at −80 °C. Virus infectivity titers were determined by a standard plaque assay or by a median tissue culture infectious dose (TCID50) assay in Vero-E6 cells, as previously described in refs. 13,14,15,16.
Efficacy study schedule in K18-hACE2 transgenic mice
Groups of female K18-hACE2 mice (n = 10 mice/group; 9 weeks-old at the beginning of the study) were immunized with homologous (MVA/MVA and NDV/NDV) or heterologous (MVA/NDV and NDV/MVA) prime/boost immunization regimens using NDV-HXP-S and MVA-S(3P) vaccine candidates, to evaluate the efficacy of the vaccination regimens. Mice received two doses, with a four-week interval (days 0 and 28), of 1 × 107 PFUs of MVA-S(3P) by the intramuscular route in 100 μL of PBS (50 μL/leg) or of 1 × 106 EID50 of NDV-HXP-S by the intranasal route in 50 μL of PBS. Mice inoculated with PBS were used as a control group. On days 14 post-prime and 26 post-boost (day 54; 2 days pre-challenge), blood was collected from each mouse by submandibular bleeding. The blood was incubated at 37 °C for 1 h, maintained at 4 °C overnight, and centrifuged at 3600 rpm for 20 min at 4 °C to obtain serum samples. The obtained serum samples were then inactivated at 56 °C for 30 min and stored at −20 °C until analysis of humoral immune responses. Four weeks after the second immunization (day 56), all mice were anesthetized in an isoflurane chamber and challenged with a lethal dose (1 × 105 PFUs) of SARS-CoV-2 MAD6 (Wuhan derived strain) by the intranasal route in 50 μL of PBS. Mice were then monitored for body weight changes, signs and symptoms of disease, and mortality for 17 days post-challenge. Animals with more than a 20% of weight loss or presenting severe signs and symptoms of disease (lack of movement, breathing difficulties, etc.) were euthanized by cervical dislocation. At day 5 post-challenge (day 61), five mice per group were euthanized, and lungs, NW, spleens, and serum samples were collected. The entire left lung lobe was removed from each mouse and immersion-fixed in zinc formalin (Sigma-Aldrich) for 48 h. After the fixation period, samples were routinely processed and embedded in paraffin for subsequent histopathological evaluation. The right lung lobes were divided longitudinally into two, with one part placed in RNALater stabilization reagent (Sigma-Aldrich) and stored at −80 °C until RNA extraction, and the other lung part was weighed and stored at −80 °C until analysis of virus yields. NW samples from each mouse were collected by flushing into the nasal cavity 400 μL of PBS; then, the samples were spun down to separate cellular pellet and supernatant and stored at −80 °C until use for RNA extraction and detection of infectious virus, respectively. Moreover, on day 17 post-challenge (day 73), surviving vaccinated mice (n = 5/group) were euthanized, and spleens, lung cells, NW, and serum samples were collected for analysis. At this time point, lungs were processed to obtain single-cell suspension using a gentleMACS™ Dissociator and GentleMACS C tubes (Miltenyi Biotec), following manufacturer’s protocols. Briefly, lungs were placed in PBS with a protease inhibitor cocktail and kept on ice until processing. It is then transferred to a GentleMACS C tube, where Liberase TL and DNase I were added. Tissue dissociation is performed using the m_lung_01 and m_lung_02 programs on the GentleMACS dissociator, with an enzyme incubation step in between. The cell homogenate was filtered through 70 µm cell strainers and red blood cells lysed using lysis buffer before resuspending in maintenance medium.
Analysis of SARS-CoV-2 viral yields by plaque assay in mouse samples
Lung and NW samples from K18-hACE2 mice, harvested at day 5 post-challenge, were analysed for the presence of SARS-CoV-2 infectious virus using a plaque assay, as previously described in refs. 13,14,15,16. Lungs were harvested, weighed, and stored directly at −80 °C until homogenization with a gentleMACS dissociator (Miltenyi Biotec) in 2 mL of PBS. Undiluted and serial ten-fold dilutions of homogenized lung tissue or NW samples were added in triplicate to Vero-E6 cell monolayers seeded in 12-well plates at 5 x 105 cells/well. After 1 h of adsorption, the inoculum was removed and plates were incubated at 37 °C, 5% CO2 in 2:1 DMEM 2X-4% FBS:Avicel® RC-591 (microcrystalline cellulose and carboxymethylcellulose sodium, DuPont Nutrition Biosciences ApS). After three days, cells were fixed for 1 h with 10% formaldehyde (Sigma-Aldrich), the supernatant was removed, and plaques were visualized by adding 0.5% crystal violet (Sigma-Aldrich). SARS-CoV-2 titers were determined in PFUs per gram of lung tissue or in PFUs per mL of NW.
Quantification of SARS-CoV-2 and cytokine mRNA by reverse transcription-quantitative polymerase chain reaction (RT-qPCR) in mouse samples
At day 5 post-challenge, lung and NW samples from K18-hACE2 mice were harvested and mRNA from these samples was extracted, as previously described in refs. 13,14,15,16. Lungs, stored in RNALater (Sigma-Aldrich) at −80 °C, were homogenized using a gentleMACS dissociator (Miltenyi Biotec) in 2 mL of RLT buffer (Qiagen) containing β-mercaptoethanol (Sigma-Aldrich). A total of 600 μL of homogenized lung tissue was utilized to isolate total RNA using the RNeasy Mini Kit (Qiagen), according to the manufacturer’s specifications. On the other hand, cellular pellets of NW samples were resuspended in 50 μL of RLT buffer (Qiagen) containing β-mercaptoethanol (Sigma-Aldrich) and used to extract RNA using the RNeasy Mini Kit (Qiagen), according to the manufacturer’s specifications.
RNA from lung and NW samples were subjected to analysis for quantifying SARS-CoV-2 mRNA using RT-qPCR, following a previously described method13,14,15,16. SARS-CoV-2 viral mRNA content was determined using previously validated sets of primers and probes specific for the SARS-CoV-2 subgenomic RNA for protein E and the genomic RNA-dependent RNA polymerase (RdRp), and gene expression was normalized to the expression of the cellular 28S ribosomal RNA gene72. Additionally, the mRNA expression levels of key proinflammatory cytokines (IL-6, CXCL10, CCL2, IL-10, TNFα and IFNγ) were also measured in lung samples using specific TaqMan probes (Thermo Fisher Scientific; the sequence will be provided upon request). The specific cytokine gene expression was also calculated relative to the expression of the cellular 28S ribosomal RNA gene, as previously described in refs. 13,14,15,16. mRNA arbitrary units (A.U.) were quantified relative to negative RNA samples (from uninfected mice) using the 2-ΔΔCt method. All samples were tested in duplicates.
Lung histopathology of mice
Lung histopathology in K18-hACE2 mice was analysed using lung samples collected on day 5 post-challenge, as previously described in refs. 13,14,15,16. To assess the character and severity of lung histopathological lesions, lung inflammation scoring parameters based on previous reports on SARS-CoV-2 infection in mouse models were used73. These histopathological parameters were graded following a semi-quantitative scoring system as follows: (0) no lesion; (1) minimal lesion; (2) mild lesion; (3) moderate lesion; (4) severe lesion. The cumulative scores of the histopathological lesions provided the total score for each animal. In each experimental group, individual scores were used to calculate the group average. In addition, haematoxylin & eosin-stained sections were visually scored 0–6 based on the percentage of lung area affected by inflammatory lesions as follows: 0% lung injury (score 0); < 5% (score 1); 6–10% (score 2); 11–20% (score 3); 21–30% (score 4); 31–40% (score 5); > 40% (score 6). In each experimental group, individual scores were used to calculate the group average.
Enzyme-linked immunosorbent assay (ELISA) in serum samples and NW from mice
The titers of binding anti-S IgG, IgG1, IgG2c and IgG3 antibodies in individual or pooled sera from immunized mice were measured by ELISA, as previously described in refs. 13,14,15,16. Endpoint IgG titers were measured as the last serum dilution that gave an absorbance value at 450 nm at least 3 times higher than that of a naive serum. Additionally, the levels of binding anti-S IgA and IgG antibodies in pooled NW from immunized mice were also measured by ELISA, using serial dilutions and assessing the absorbance at 450 nm, as previously described in refs. 13,14,15,16. The soluble SARS-CoV-2 S proteins used to coat the plates were derived from the Wuhan strain (GenBank accession number MN908947.3), Beta variant (EPI_ISL_712096) and the Omicron BA.1 (OL672836.1), BA.5 (ON249995.1) and XBB.1.5 (OP790748.1) subvariants. The recombinant expression vectors for protein production were prepared as previously described in refs. 13,14,15,16,74, and the soluble S proteins were expressed in mammalian cells and purified from cell supernatants as previously reported74.
Neutralization of live SARS-CoV-2 in serum samples from mice
The capacity of individual or pooled sera obtained from immunized mice to neutralize live SARS-CoV-2 virus was measured using a microneutralization test (MNT) assay in a BSL-3 laboratory at the CNB-CSIC, as previously described in refs. 13,14,15,16. Serially diluted serum samples in DMEM-2% FBS medium were incubated at a 1:1 ratio with 100 TCID50 of SARS-CoV-2 parental Wuhan strain virus (MAD6 isolate, containing the D614G mutation in the S protein), Beta variant, or Omicron BA.1, BA.5 or XBB.1.5 subvariants in 96-well tissue culture plates for 1 h at 37 °C. Then, mixtures of serum samples and SARS-CoV-2 were added in triplicate to Vero-E6 cell monolayers seeded in 96-well plates at 1.5 x 104 cells/well. Cells were allowed to be infected for 72 h, after which they were fixed and subsequently stained with 5% Crystal Violet (Sigma-Aldrich). Once the plates were dry, cell monolayers were solubilized with 1% SDS (Sigma-Aldrich) and absorbance was measured at 570 nm to determine the neutralization percentage. To obtain the 50% neutralization titers (NT50), half maximal effective concentration (EC50) and 95% confidence intervals (95% CI) were calculated using a nonlinear regression model fit with settings for agonist concentration versus normalized response curve using GraphPad Prism version 10.2.1 Software.
Intracellular cytokine staining (ICS) assay in splenocytes and lung cells from mice
Spleens or lungs extracted at day 17 post-challenge from each mouse were pooled per group, processed mechanically, blood-cell depleted, and filtered through 40-µm cell strainers until single-cell samples were obtained. Then, splenocytes or lung cells were stimulated with SARS-CoV-2 S peptide pools (1 µg/mL; JPT Peptide Technologies), spanning the entire S protein from the Wuhan strain as consecutive 15-mers overlapping by 11 amino acids, and the magnitude, polyfunctionality and memory phenotype of SARS-CoV-2 S-specific CD4+ and CD8+ T cells expressing CD107a, and/or secreting IFNγ, and/or TNFα, and/or IL-2 were analysed by an ICS assay, as previously described in ref. 74. Cells were acquired with a Gallios flow cytometer (Beckman Coulter), and analyses of the data were performed with the FlowJo software version 10.4.2 (Tree Star), as previously described in ref. 74.
Vaccine efficacy and direct-contact transmission study in hamsters
Six- to eight-week-old female Golden Syrian hamsters (HsdHan®: AURA, Inotiv) (n = 8/group) were vaccinated intranasally with 1 x 106 EID50 of NDV-HXP-S or wildtype LaSota NDV (NDV-WT) strains or intramuscularly with 1 x 108 PFUs of MVA-S(3P) or MVA-WT in a four-week interval between doses. Vaccines were diluted in PBS (Gibco-Life Technologies) in a total volume of 50 µL or 100 µL per dose for its intranasal or intramuscular administration, respectively. For intranasal administration, hamsters were anesthetized with ketamine/xylazine cocktail. Four weeks post-boost vaccinated hamsters were bled and serum samples were collected for further analyses. Then, hamsters from all vaccination groups were anesthetized and challenged with 1 × 105 PFUs of SARS-CoV-2 New York strain by the intranasal route, except that the healthy control group that was mock-challenged with the same amount of PBS (50 µL). Four naïve hamsters per group were cohoused with challenged hamsters from vaccination groups 1–6 at day 1 post-challenge, forming the recipient groups (RGs). Specifically, each naïve recipient hamster (recipient group) was cohoused individually with one infected donor hamster (challenged with SARS-CoV-2 24 h prior). Two animals were housed per cage, with a cage surface area of approximately 1000 cm². The cohousing period lasted for 4 days, after which donor hamsters and recipient hamsters were sacrificed for assessment of viral load and pathology to evaluate protection. Body weight changes were monitored for 5 days post-challenge and throat swabs were collected at days 1, 3 and 5 post-challenge of donors and at days 3 and 5 post- challenge of recipients in 200 µL of PBS. Four vaccinated hamsters from each group were euthanized at days 2 and 5 post-challenge to harvest lungs lobes (upper and lower right lung lobes), and nasal turbinates. Four hamsters from each recipient group were euthanized at day 5 post-challenge to harvest lungs lobes (upper and lower right lung lobes), and nasal turbinates. Each right lung lobe was homogenized in 1 mL of PBS, and the nasal turbinates were homogenized in 0.5 mL of PBS. Viral titers in the nasal turbinates and lung homogenates were measured by a plaque assay on Vero-E6 cells. Genomic viral RNA copies were measured by qPCR. The left lung lobes were collected at day 5 post-challenge and fixed/perfused with neutral buffered formalin for histopathology.
SARS-CoV-2 RT-qPCR in hamster samples
RNA was extracted from throat swab samples from hamsters using the QIAamp Viral RNA Mini Kit (QIAGEN, Germantown, MD) according to the manufacturer’s instructions. Genomic copies of SARS-CoV-2 were measured through Nucleocapsid (N) gene, as previously described in ref. 75. Briefly, Forward Primer (5’-GACCCCAAAATCAGCGAAAT-3’) and Reverse Primer (5’-TCTGGTTACTGCCAGTTGAATCTG-3’) were used, yielding a 72 bp amplicon. RT-qPCR was performed using the iTaq™ Universal SYBR Green One-Step Kit (Bio-Rad, Hercules, CA) and the CFX Opus 96 Real-Time PCR System (Bio-Rad, Hercules, CA), following the manufacturer recommended thermal cycling conditions. Standard curves were generated using the 2019-nCoV_N_Positive Control plasmid (IDT, Cat No.10006625), which encodes the N gene of SARS-CoV-2 isolate Wuhan-Hu-1 (GenBank: NC_045512.2). A no-template control and a condition with 2 x 105 copies of the positive control plasmid were added in triplicate as internal negative and positive controls, respectively. Melt curve analysis was also performed to confirm amplification specificity, following the manufacturer recommended thermal cycling conditions. Copies per sample were afterwards calculated (obtained copies/5 µL of RNA extracted per reaction x 60 µL of total RNA extracted per sample).
Plaque assay with hamster tissues
Vero-E6 cells (ATCC, CRL-1586) were seeded in 12-well plates and the next day, confluent monolayers were infected with serial 10-fold dilutions of viral stock or supernatants of hamster tissue homogenates at 37 °C and 5% CO2 using an inoculum of 200 μL per well. Plates were rocked every 10–15 min, and after 1 h, inoculum was removed and an overlay consisting of MEM (Lonza) with penicillin/streptomycin (Corning), L-Glutamine (Gibco-Life Technologies), HEPES (Gibco-Life Technologies), BSA (MP Biomedicals), and NaHCO3 supplemented with 0.7% purified agar (Oxoid) and 2% FBS (Peak Serum) was added to each well. Cells were then incubated at 37 °C and 5% CO2 for 72 hpi. Plaque assays were then fixed with 10% formaldehyde overnight. Immunostaining was performed using anti-SARS-CoV-2 NP (1C7C7, Creative Biolabs) for the primary antibody at a 1:1000 dilution for 2 h at room temperature on a shaker. Anti-mouse IgG (Abcam ab6823) was used for the secondary antibody at a 1:5000 dilution for 45 min at room temperature on a shaker. Plaques were developed using TrueBlue substrate (KPL Seracare) for 10 min at room temperature on a shaker. All samples were frozen at −80 °C once before evaluation of viral titers.
Histopathology of lungs from hamsters
Formalin-fixed, paraffin-embedded left lung tissues obtained from hamsters were cut into 5 μm sections and stained with hematoxylin and eosin (H&E) by the Biorepository and Pathology Core at ISMMS. All sections were evaluated by a veterinary pathologist who was blinded to the vaccination groups in the Comparative Pathology Laboratory (CPL) at ISMMS. The scoring system used is shown in Supplementary Table 1, and was previously described10. The slides were scanned using OptraSCAN Scanner.
ELISA in serum samples from hamsters
ELISA was performed to measure RBD- and S-specific IgGs in the serum of vaccinated hamsters. In brief, Immulon 4 HBX 96-well ELISA plates (Thermo Fisher Scientific) were coated with 2 μg/mL of recombinant trimeric S protein or RBD protein (50 μL per well) in PBS overnight at 4 °C. The plates were then washed three times with 220 μL of PBS containing 0.1% (v/v) Tween-20 (PBST). The plates were subsequently blocked with 220 μL of blocking solution (3% goat serum, 0.5% dry milk, 96.5% PBST) per well for 1 h at room temperature. The blocking buffer was decanted, and hamster sera were 3-fold serially diluted in blocking solution starting at 1:30 dilution followed by a 2 h incubation at room temperature. The plates were washed three times with 220 μL of PBST and 50 μL of horseradish peroxidase (HRP)-conjugated goat anti-hamster IgG (H + L) cross-adsorbed secondary antibody (Invitrogen, HA6007) was added at 1:3000 dilution. The plates were incubated for 1 h at room temperature and washed three times with 220 μL of PBST. Then, 100 μL of o-phenylenediamine dihydrochloride (SigmaFast OPD, Sigma) substrate was added per well, and the plates were developed for 10 min and then 50 μL of 3 M hydrochloric acid (HCl) was added to each well to quench the reactions. The optical density (OD) was measured at 492 nm on a Synergy 4 plate reader (BioTek). An average of OD values for blank wells plus 3 standard deviations was used to set a cutoff value for each plate. The endpoint titers were calculated and graphed using GraphPad Prism 10.2.1.
Pseudo-virus neutralization assay in serum samples from hamsters
Pseudo-virus neutralization assay was performed in serum samples from vaccinated hamsters, as previously described9. Replication-competent vesicular stomatitis viruses (VSVs) carrying an enhanced green fluorescent protein (eGFP) reporter and expressing ancestral Wuhan, Delta, BA.1, or XBB.1.5 SARS-CoV-2 S (rcVSV-eGFP-CoV2-S) in place of VSV-G were used. One day prior to use in the neutralization assay, 2 x 104 BHK-ACE2 cells were seeded in flat bottom 96 well plates (Corning Falcon). Pooled serum samples were heat inactivated at 56 °C for 30 min before usage. Virus stocks were pre-mixed with 4-fold serially diluted serum, starting at 1:10 dilution, in DMEM-10% FBS-1% penicillin/streptomycin and incubated for 15 min at room temperature. The virus plus serum mixture was subsequently transferred onto the BHK-ACE2 target cells. At 12 hpi, GFP counts were measured using the Celigo imaging cytometer (Nexcelom Biosciences, version 4.1.3.0). Each assay was done in duplicates. For calculation of the inhibitory dilution at which 50% neutralization is achieved (ID50), GFP counts from “no serum” conditions were set to 100%; GFP counts of each condition (serum treated) were normalized to no serum control wells. Inhibition curves were generated using GraphPad Prism 10.2.1 with “log (inhibitor) vs normalized response-variable slope” settings.
Statistical procedures
All graphs, calculations, and statistical analyses were performed using GraphPad Prism software. To determine differences between groups, ordinary one-way ANOVA of transformed data followed by Tukey’s multiple comparisons test was used for the statistical analysis of SARS-CoV-2 and cytokine mRNA levels in mouse samples and SARS-CoV-2 viral yields in mouse and hamster samples. An unpaired nonparametric Kruskal-Wallis test was employed for the statistical evaluation of lung histopathological scores in mouse and hamster samples and an unpaired ordinary one-way ANOVA followed by Tukey’s multiple comparisons test for the percentage of lung area with lesions in mouse samples. An unpaired ordinary one-way ANOVA followed by Tukey’s multiple comparisons test of transformed data was used for the statistical analysis of IgG titers from individual mouse and hamster serum samples and live virus neutralizing (NT50) antibody titers from individual or pooled mouse serum samples, whereas an ordinary two-way ANOVA followed by Tukey’s multiple comparisons test was used for the statistical analysis of IgG titers against S from SARS-CoV-2 variants and isotype IgG titers from pooled mouse serum samples and NT50 antibody titers from pooled hamster samples. Statistical analysis of the ICS assay data was performed using an approach that corrects measurements for background response calculating confidence intervals and p-values, as previously described in ref. 76. In the hamster study, statistical differences in SARS-CoV-2 genomic copies/sample were determined using a two-way ANOVA followed by Tukey’s multiple comparisons test of transformed data. Statistical significance is indicated as follows: *p < 0.033; **p < 0.002; ***p < 0.0002; ****p < 0.0001.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding authors on reasonable request.
References
Barouch, D. H. Covid-19 Vaccines - Immunity, Variants, Boosters. N. Engl. J. Med 387, 1011–1020, https://doi.org/10.1056/NEJMra2206573 (2022).
Ioannidis, J. P. A., Pezzullo, A. M., Cristiano, A. & Boccia, S. Global Estimates of Lives and Life-Years Saved by COVID-19 Vaccination During 2020-2024. JAMA Health Forum 6, e252223, https://doi.org/10.1001/jamahealthforum.2025.2223 (2025).
He, Q. et al. Heterologous prime-boost: breaking the protective immune response bottleneck of COVID-19 vaccine candidates. Emerg. Microbes Infect. 10, 629–637, https://doi.org/10.1080/22221751.2021.1902245 (2021).
Costa Clemens, S. A. et al. Heterologous versus homologous COVID-19 booster vaccination in previous recipients of two doses of CoronaVac COVID-19 vaccine in Brazil (RHH-001): a phase 4, non-inferiority, single blind, randomised study. Lancet 399, 521–529, https://doi.org/10.1016/S0140-6736(22)00094-0 (2022).
Markewitz, R. D. H. et al. Differences in Immunogenicity of Three Different Homo- and Heterologous Vaccination Regimens against SARS-CoV-2. Vaccines (Basel) 10, 649, https://doi.org/10.3390/vaccines10050649 (2022).
Travieso, T., Li, J., Mahesh, S., Mello, J. & Blasi, M. The use of viral vectors in vaccine development. NPJ Vaccines 7, 75. https://doi.org/10.1038/s41541-022-00503-y (2022).
Sallard, E., Zhang, W., Aydin, M., Schroer, K. & Ehrhardt, A. The Adenovirus Vector Platform: Novel Insights into Rational Vector Design and Lessons Learned from the COVID-19 Vaccine. Viruses 15, 204, https://doi.org/10.3390/v15010204 (2023).
Gonzalez-Dominguez, I. et al. Trivalent NDV-HXP-S Vaccine Protects against Phylogenetically Distant SARS-CoV-2 Variants of Concern in Mice. Microbiol Spectr. 10, e0153822. https://doi.org/10.1128/spectrum.01538-22 (2022).
Slamanig, S. et al. Intranasal SARS-CoV-2 Omicron variant vaccines elicit humoral and cellular mucosal immunity in female mice. EBioMedicine 105, 105185. https://doi.org/10.1016/j.ebiom.2024.105185 (2024).
Sun, W. et al. A Newcastle disease virus expressing a stabilized spike protein of SARS-CoV-2 induces protective immune responses. Nat. Commun. 12, 6197. https://doi.org/10.1038/s41467-021-26499-y (2021).
Tcheou, J. et al. Safety and Immunogenicity Analysis of a Newcastle Disease Virus (NDV-HXP-S) Expressing the Spike Protein of SARS-CoV-2 in Sprague Dawley Rats. Front Immunol. 12, 791764. https://doi.org/10.3389/fimmu.2021.791764 (2021).
Abdelnabi, R. et al. Optimized vaccine candidate MVA-S(3P) fully protects against SARS-CoV-2 infection in hamsters. Front Immunol. 14, 1163159. https://doi.org/10.3389/fimmu.2023.1163159 (2023).
Perez, P. et al. Preclinical immune efficacy against SARS-CoV-2 beta B.1.351 variant by MVA-based vaccine candidates. Front Immunol. 14, 1264323. https://doi.org/10.3389/fimmu.2023.1264323 (2023).
Perez, P. et al. Intranasal administration of a single dose of MVA-based vaccine candidates against COVID-19 induced local and systemic immune responses and protects mice from a lethal SARS-CoV-2 infection. Front Immunol. 13, 995235. https://doi.org/10.3389/fimmu.2022.995235 (2022).
Perez, P. et al. MVA-based vaccine candidates expressing SARS-CoV-2 prefusion-stabilized spike proteins of the Wuhan, Beta or Omicron BA.1 variants protect transgenic K18-hACE2 mice against Omicron infection and elicit robust and broad specific humoral and cellular immune responses. Front Immunol. 15, 1420304. https://doi.org/10.3389/fimmu.2024.1420304 (2024).
Perez, P. et al. A Single Dose of an MVA Vaccine Expressing a Prefusion-Stabilized SARS-CoV-2 Spike Protein Neutralizes Variants of Concern and Protects Mice From a Lethal SARS-CoV-2 Infection. Front Immunol. 12, 824728. https://doi.org/10.3389/fimmu.2021.824728 (2022).
Duc Dang, A. et al. Safety and immunogenicity of an egg-based inactivated Newcastle disease virus vaccine expressing SARS-CoV-2 spike: Interim results of a randomized, placebo-controlled, phase 1/2 trial in Vietnam. Vaccine 40, 3621–3632, https://doi.org/10.1016/j.vaccine.2022.04.078 (2022).
López-Macías, C. et al. Phase II study on the safety and immunogenicity of single-dose intramuscular or intranasal administration of the AVX/COVID-12 “Patria” recombinant Newcastle disease virus vaccine as a heterologous booster against COVID-19 in Mexico. Vaccine 43, 126511 (2025).
Pitisuttithum, P. et al. Safety and immunogenicity of an inactivated recombinant Newcastle disease virus vaccine expressing SARS-CoV-2 spike: Interim results of a randomised, placebo-controlled, phase 1 trial. EClinicalMedicine 45, 101323. https://doi.org/10.1016/j.eclinm.2022.101323 (2022).
Ponce-de-Leon, S. et al. Interim safety and immunogenicity results from an NDV-based COVID-19 vaccine phase I trial in Mexico. NPJ Vaccines 8, 67. https://doi.org/10.1038/s41541-023-00662-6 (2023).
Bliss, C. M. et al. Assessment of novel vaccination regimens using viral vectored liver stage malaria vaccines encoding ME-TRAP. Sci. Rep. 8, 3390. https://doi.org/10.1038/s41598-018-21630-4 (2018).
Tang, J., Amin, M. A. & Campian, J. L. Past, Present, and Future of Viral Vector Vaccine Platforms: A Comprehensive Review. Vaccines (Basel) 13, https://doi.org/10.3390/vaccines13050524 (2025).
Happe, M. et al. Heterologous cAd3-Ebola and MVA-EbolaZ vaccines are safe and immunogenic in US and Uganda phase 1/1b trials. NPJ Vaccines 9, 67. https://doi.org/10.1038/s41541-024-00833-z (2024).
Venkatraman, N. et al. Safety and Immunogenicity of a Heterologous Prime-Boost Ebola Virus Vaccine Regimen in Healthy Adults in the United Kingdom and Senegal. J. Infect. Dis. 219, 1187–1197, https://doi.org/10.1093/infdis/jiy639 (2019).
Vuola, J. M. et al. Differential immunogenicity of various heterologous prime-boost vaccine regimens using DNA and viral vectors in healthy volunteers. J. Immunol. 174, 449–455, https://doi.org/10.4049/jimmunol.174.1.449 (2005).
Launay, O. & Thill, P. Heterologous prime boost COVID 19 vaccination. Infect. Dis. Now. 52, S7–S8, https://doi.org/10.1016/j.idnow.2022.09.011 (2022).
Lu, S. Heterologous prime-boost vaccination. Curr. Opin. Immunol. 21, 346–351, https://doi.org/10.1016/j.coi.2009.05.016 (2009).
Hu, S. L. et al. Protection of macaques against SIV infection by subunit vaccines of SIV envelope glycoprotein gp160. Science 255, 456–459, https://doi.org/10.1126/science.1531159 (1992).
Li, S. et al. Priming with recombinant influenza virus followed by administration of recombinant vaccinia virus induces CD8+ T-cell-mediated protective immunity against malaria. Proc. Natl Acad. Sci. USA 90, 5214–5218, https://doi.org/10.1073/pnas.90.11.5214 (1993).
Cheng, H. et al. Immunogenicity and Safety of Homologous and Heterologous Prime-Boost Immunization with COVID-19 Vaccine: Systematic Review and Meta-Analysis. Vaccines (Basel) 10, 798, https://doi.org/10.3390/vaccines10050798 (2022).
Garg, I., Sheikh, A. B., Pal, S. & Shekhar, R. Mix-and-Match COVID-19 Vaccinations (Heterologous Boost): A Review. Infect. Dis. Rep. 14, 537–546, https://doi.org/10.3390/idr14040057 (2022).
Heinen, N. et al. In-depth analysis of T cell immunity and antibody responses in heterologous prime-boost-boost vaccine regimens against SARS-CoV-2 and Omicron variant. Front Immunol. 13, 1062210. https://doi.org/10.3389/fimmu.2022.1062210 (2022).
Garrett, N. et al. Safety, effectiveness and immunogenicity of heterologous mRNA-1273 boost after prime with Ad26.COV2.S among healthcare workers in South Africa: The single-arm, open-label, phase 3 SHERPA study. PLOS Glob. Public Health 4, e0003260, https://doi.org/10.1371/journal.pgph.0003260 (2024).
Laghlali, G. et al. Enhanced mucosal SARS-CoV-2 immunity after heterologous intramuscular mRNA prime/intranasal protein boost vaccination with a combination adjuvant. Mol. Ther. 32, 4448–4466, https://doi.org/10.1016/j.ymthe.2024.10.016 (2024).
Liu, J. et al. Heterologous prime-boost immunizations with chimpanzee adenoviral vectors elicit potent and protective immunity against SARS-CoV-2 infection. Cell Discov. 7, 123, https://doi.org/10.1038/s41421-021-00360-4 (2021).
Veits, J. et al. Protective efficacy of several vaccines against highly pathogenic H5N1 avian influenza virus under experimental conditions. Vaccine 26, 1688–1696, https://doi.org/10.1016/j.vaccine.2008.01.016 (2008).
Olbert, M. et al. Viral vector vaccines expressing nucleoprotein and phosphoprotein genes of avian bornaviruses ameliorate homologous challenge infections in cockatiels and common canaries. Sci. Rep. 6, 36840. https://doi.org/10.1038/srep36840 (2016).
Runge, S. et al. Viral vector vaccines protect cockatiels from inflammatory lesions after heterologous parrot bornavirus 2 challenge infection. Vaccine 35, 557–563, https://doi.org/10.1016/j.vaccine.2016.12.022 (2017).
Rall, I., Amann, R., Malberg, S., Herden, C. & Rubbenstroth, D. Recombinant Modified Vaccinia Virus Ankara (MVA) Vaccines Efficiently Protect Cockatiels Against Parrot Bornavirus Infection and Proventricular Dilatation Disease. Viruses 11, 1130, https://doi.org/10.3390/v11121130 (2019).
Koch, T., Mellinghoff, S. C., Shamsrizi, P., Addo, M. M. & Dahlke, C. Correlates of Vaccine-Induced Protection against SARS-CoV-2. Vaccines (Basel) 9, https://doi.org/10.3390/vaccines9030238 (2021).
Marcos-Villar, L. et al. Heterologous mRNA/MVA delivering trimeric-RBD as effective vaccination regimen against SARS-CoV-2: COVARNA Consortium. Emerg. Microbes Infect. 13, 2387906. https://doi.org/10.1080/22221751.2024.2387906 (2024).
Marcos-Villar, L. et al. Modulating the immune response to SARS-CoV-2 by different nanocarriers delivering an mRNA expressing trimeric RBD of the spike protein: COVARNA Consortium. NPJ Vaccines 9, 53. https://doi.org/10.1038/s41541-024-00838-8 (2024).
Carreno, J. M. et al. An inactivated NDV-HXP-S COVID-19 vaccine elicits a higher proportion of neutralizing antibodies in humans than mRNA vaccination. Sci. Transl. Med 15, eabo2847. https://doi.org/10.1126/scitranslmed.abo2847 (2023).
Darling, T. L. et al. Mucosal immunization with ChAd-SARS-CoV-2-S prevents sequential transmission of SARS-CoV-2 to unvaccinated hamsters. Sci. Adv. 10, eadp1290. https://doi.org/10.1126/sciadv.adp1290 (2024).
Brandtzaeg, P. Secretory IgA: Designed for Anti-Microbial Defense. Front Immunol. 4, 222, https://doi.org/10.3389/fimmu.2013.00222 (2013).
Sallusto, F., Geginat, J. & Lanzavecchia, A. Central memory and effector memory T cell subsets: function, generation, and maintenance. Annu Rev. Immunol. 22, 745–763, https://doi.org/10.1146/annurev.immunol.22.012703.104702 (2004).
Chavda, V. P., Vora, L. K., Pandya, A. K. & Patravale, V. B. Intranasal vaccines for SARS-CoV-2: From challenges to potential in COVID-19 management. Drug Discov. Today 26, 2619–2636, https://doi.org/10.1016/j.drudis.2021.07.021 (2021).
de Swart, R. L. & Belov, G. A. Advantages and challenges of Newcastle disease virus as a vector for respiratory mucosal vaccines. Curr. Opin. Virol. 62, 101348. https://doi.org/10.1016/j.coviro.2023.101348 (2023).
de Swart, R. L. et al. Intranasal administration of a live-attenuated recombinant newcastle disease virus expressing the SARS-CoV-2 Spike protein induces high neutralizing antibody levels and protects from experimental challenge infection in hamsters. Vaccine 40, 4676–4681, https://doi.org/10.1016/j.vaccine.2022.07.005 (2022).
Warner, B. M. et al. Mucosal Vaccination with a Newcastle Disease Virus-Vectored Vaccine Reduces Viral Loads in SARS-CoV-2-Infected Cynomolgus Macaques. Vaccines (Basel) 12, 404, https://doi.org/10.3390/vaccines12040404 (2024).
Gonzalez-Dominguez, I. et al. Mucosal multivalent NDV-based vaccine provides cross-reactive immune responses against SARS-CoV-2 variants in animal models. Front Immunol. 16, 1524477. https://doi.org/10.3389/fimmu.2025.1524477 (2025).
Port, J. R. et al. SARS-CoV-2 disease severity and transmission efficiency is increased for airborne compared to fomite exposure in Syrian hamsters. Nat. Commun. 12, 4985. https://doi.org/10.1038/s41467-021-25156-8 (2021).
Sia, S. F. et al. Pathogenesis and transmission of SARS-CoV-2 in golden hamsters. Nature 583, 834–838, https://doi.org/10.1038/s41586-020-2342-5 (2020).
Christensen, D. et al. Protection against SARS-CoV-2 transmission by a parenteral prime-Intranasal boost vaccine strategy. EBioMedicine 84, 104248. https://doi.org/10.1016/j.ebiom.2022.104248 (2022).
Port, J. R. et al. Infection- or AZD1222 vaccine-mediated immunity reduces SARS-CoV-2 transmission but increases Omicron competitiveness in hamsters. Nat. Commun. 14, 6592. https://doi.org/10.1038/s41467-023-42346-8 (2023).
Russell, M. W., Moldoveanu, Z., Ogra, P. L. & Mestecky, J. Mucosal Immunity in COVID-19: A Neglected but Critical Aspect of SARS-CoV-2 Infection. Front Immunol. 11, 611337. https://doi.org/10.3389/fimmu.2020.611337 (2020).
Lycke, N. Recent progress in mucosal vaccine development: potential and limitations. Nat. Rev. Immunol. 12, 592–605, https://doi.org/10.1038/nri3251 (2012).
Belyakov, I. M. & Ahlers, J. D. What role does the route of immunization play in the generation of protective immunity against mucosal pathogens?. J. Immunol. 183, 6883–6892, https://doi.org/10.4049/jimmunol.0901466 (2009).
Woodland, D. L. & Kohlmeier, J. E. Migration, maintenance and recall of memory T cells in peripheral tissues. Nat. Rev. Immunol. 9, 153–161, https://doi.org/10.1038/nri2496 (2009).
Song, Y., Mehl, F. & Zeichner, S. L. Vaccine Strategies to Elicit Mucosal Immunity. Vaccines (Basel) 12, 191, https://doi.org/10.3390/vaccines12020191 (2024).
Zhang, Q. Y. et al. Newcastle Disease Virus (NDV)-based vaccine candidate against SARS-CoV-2 Omicron by intranasal immunization. Antivir. Res 220, 105757. https://doi.org/10.1016/j.antiviral.2023.105757 (2023).
Volz, A., Fux, R., Langenmayer, M. C. & Sutter, G. Modified vaccinia virus ankara (MVA)–development as recombinant vaccine and prospects for use in veterinary medicine]. Berl. Munch. Tierarzt. Wochenschr. 128, 464–472 (2015).
Altenburg, A. F. et al. Modified vaccinia virus ankara (MVA) as production platform for vaccines against influenza and other viral respiratory diseases. Viruses 6, 2735–2761, https://doi.org/10.3390/v6072735 (2014).
Miyahira, Y. et al. Recombinant viruses expressing a human malaria antigen can elicit potentially protective immune CD8+ responses in mice. Proc. Natl Acad. Sci. USA 95, 3954–3959, https://doi.org/10.1073/pnas.95.7.3954 (1998).
Murata, K. et al. Characterization of in vivo primary and secondary CD8+ T cell responses induced by recombinant influenza and vaccinia viruses. Cell Immunol. 173, 96–107, https://doi.org/10.1006/cimm.1996.0255 (1996).
Rodrigues, M. et al. Influenza and vaccinia viruses expressing malaria CD8+ T and B cell epitopes. Comparison of their immunogenicity and capacity to induce protective immunity. J. Immunol. 153, 4636–4648 (1994).
Perdiguero, B. et al. Highly Attenuated Poxvirus-Based Vaccines Against Emerging Viral Diseases. J. Mol. Biol. 435, 168173. https://doi.org/10.1016/j.jmb.2023.168173 (2023).
Villadiego, J. et al. Full protection from SARS-CoV-2 brain infection and damage in susceptible transgenic mice conferred by MVA-CoV2-S vaccine candidate. Nat. Neurosci. 26, 226–238, https://doi.org/10.1038/s41593-022-01242-y (2023).
Mayr, A., Stickl, H., Muller, H. K., Danner, K. & Singer, H. The smallpox vaccination strain MVA: marker, genetic structure, experience gained with the parenteral vaccination and behavior in organisms with a debilitated defence mechanism (author’s transl)]. Zentralbl Bakteriol. B 167, 375–390 (1978).
Ramirez, J. C., Gherardi, M. M. & Esteban, M. Biology of attenuated modified vaccinia virus Ankara recombinant vector in mice: virus fate and activation of B- and T-cell immune responses in comparison with the Western Reserve strain and advantages as a vaccine. J. Virol. 74, 923–933, https://doi.org/10.1128/jvi.74.2.923-933.2000 (2000).
Diez, J. M. et al. Cross-neutralization activity against SARS-CoV-2 is present in currently available intravenous immunoglobulins. Immunotherapy 12, 1247–1255, https://doi.org/10.2217/imt-2020-0220 (2020).
Corman, V. M. et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Eur. Surveill. 25, 2000045, https://doi.org/10.2807/1560-7917.ES.2020.25.3.2000045 (2020).
Sun, S. H. et al. A Mouse Model of SARS-CoV-2 Infection and Pathogenesis. Cell Host Microbe 28, 124–133.e124, https://doi.org/10.1016/j.chom.2020.05.020 (2020).
Garcia-Arriaza, J. et al. COVID-19 vaccine candidates based on modified vaccinia virus Ankara expressing the SARS-CoV-2 spike induce robust T- and B-cell immune responses and full efficacy in mice. J. Virol. 95, e02260–02220, https://doi.org/10.1128/JVI.02260-20 (2021).
Dagotto, G. et al. Comparison of Subgenomic and Total RNA in SARS-CoV-2 Challenged Rhesus Macaques. J. Virol. 95, e02370–02320, https://doi.org/10.1128/JVI.02370-20 (2021).
Garcia-Arriaza, J., Najera, J. L., Gomez, C. E., Sorzano, C. O. & Esteban, M. Immunogenic profiling in mice of a HIV/AIDS vaccine candidate (MVA-B) expressing four HIV-1 antigens and potentiation by specific gene deletions. PLoS One 5, e12395, https://doi.org/10.1371/journal.pone.0012395 (2010).
Acknowledgements
We thank CSIC and MCIU for continuous support. We thank CISA-INIA-CSIC (Valdeolmos, Madrid, Spain) for the BSL-3 facilities to perform the mouse study. SARS-CoV-2 MAD6 virus isolate was kindly provided by Dr. José M. Honrubia and Prof. Luis Enjuanes (CNB-CSIC, Madrid, Spain). SARS-CoV-2 Omicron BA.1 (B.1.1.529) variant was kindly provided by Prof. Piet Maes from KU Leuven (Belgium) through Dr. Robbert Boudewijns and Dr. Kai Dallmeier (KU Leuven, Belgium). SARS-CoV-2 Omicron BA.5 (EPI_ISL_13424827) and XBB.1.5 (EPI_ISL_16939528) subvariants were kindly provided by Prof. Rafael Delgado (Hospital Universitario 12 de Octubre, Madrid, Spain). SARS-CoV-2 Beta (B.1.351) variant was obtained through the European Virus Archive goes Global (Evag) platform by an MTA agreement. We thank the Histology Facility at CNB-CSIC for histological preparation of mouse lung samples. We thank Carlos Óscar Sánchez Sorzano from the CNB Bioinformatic Unit for help with the statistical analysis, José María Casasnovas (CNB-CSIC) for providing the S protein used in ELISAs of mouse serum samples, and Jorge Esteban (CNB-CSIC) for laboratory manager help. We thank Dr. Peter Palese (ISMMS) for providing support and help during the whole study. We appreciate the work of Randy Albrecht, Carlos Franco and the Center for Comparative Medicine and Surgery (CCMS) team overseeing the CBSL-3 and ABSL-3 facilities at ISMMS. The Conventional Biocontainment Facility (CBF) is a NIH BSL3/BSL-3 facility that is part of the BSL-3 Biocontainment CoRE. This core is supported by subsidies from the ISMMS Dean’s Office and by investigator support through a cost recovery mechanism. We also thank Dr. Benhur Lee (ISMMS) for providing the rcVSV reverse genetics system to generate rcVSVs expressing the S protein of SARS-CoV-2 variants. This research was supported by CSIC grant 202120E079, grant CNS2022-135511 funded by the Spanish Ministry of Science, Innovation and Universities (MCIU)/Spanish Research Agency (AEI)/10.13039/501100011033 and by the European Union NextGenerationEU/PRTR to promote the consolidation of research, and funds from Centro de Investigación Biomédica en Red de Enfermedades Infecciosas (CIBERINFEC) co-financed with FEDER funds (to J.G.-A.); CSIC grant 2020E84 (to M.E.); Spanish MCIU/AEI/10.13039/501100011033 grant PID2020-114481RB-I00 (to J.G.-A. and M.E.). This work was also partly supported by CRIPT (Center for Research on Influenza Pathogenesis and Transmission), an NIAID-funded Center of Excellence for Influenza Research and Response (CEIRR, contract # 75N93021C00014) (to A.G.-S.). This works is also supported by seed funding awarded by ISMMS Department of Microbiology (to W.S.). This research work was also funded by the European Commission-NextGenerationEU, through CSIC’s Global Health Platform (PTI Salud Global) (to J.G.-A. and M.E.). J.G.-A. also received grants from the European Commission HORIZON-HLTH-2023-DISEASE-03-18 (Project MARVAX: 101137183 and Project FLAVIVACCINE: 101137006). J.G.-A. and M.E. also acknowledges financial support from the Spanish AEI/10.13039/501100011033, through the “Severo Ochoa” Programme for Centres of Excellence in R&D (SEV-2017-0712, CEX2023-001386-S). The funders were not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization: J.G.-A., M.E., A.G.-S., W.S.; Formal analysis: P.P., K.J., J.G.-A.; Funding acquisition: J.G.-A., M.E., A.G.-S., W.S.; Investigation: P.P., K.J., I.G.-D., D.R.-M., A.A., A.C., S.S., S.F., M.A.N., P.J.S.-C., N.L., T.Y.L., J.G.-A.; Methodology: P.P., K.J., I.G.-D., D.R.-M., A.A., A.C., S.S., S.F., M.A.N., P.J.S.-C., N.L., T.Y.L., J.G.-A.; Supervision: J.G.-A., M.E., A.G.-S., W.S.; Validation: P.P., K.J., A.G.-S., J.G.-A.; Visualization: P.P., K.J., J.G.-A.; Writing—original draft: P.P., K.J., J.G.-A.; Writing—review and editing: all authors. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The A.G.-S. laboratory has received research support from GSK, Pfizer, Senhwa Biosciences, Kenall Manufacturing, Blade Therapeutics, Avimex, Johnson & Johnson, Dynavax, 7Hills Pharma, Pharmamar, ImmunityBio, Accurius, Nanocomposix, Hexamer, N-fold LLC, Model Medicines, Atea Pharma, Applied Biological Laboratories and Merck. A.G.-S. has consulting agreements for the following companies involving cash and/or stock: Castlevax, Amovir, Vivaldi Biosciences, Contrafect, 7Hills Pharma, Avimex, Pagoda, Accurius, Esperovax, Applied Biological Laboratories, Pharmamar, CureLab Oncology, CureLab Veterinary, Synairgen, Paratus, Pfizer, Virofend and Prosetta. A.G.-S. has been an invited speaker in meeting events organized by Seqirus, Janssen, Abbott, Astrazeneca and Novavax. A.G.-S. is inventor on patents and patent applications on the use of antivirals and vaccines for the treatment and prevention of virus infections and cancer, owned by the ISMMS, New York. ISMMS has filed patent application entitled “Recombinant Newcastle disease virus expressing SARS-COV-2 spike protein and uses thereof” which names A.G.-S. and W.S. as co-inventors. A.G.-S. and W.S. serve on the scientific advisory board of CastleVax and are listed as co-founders of the company. The rest of the authors declare that they have no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pérez, P., Jiang, K., González-Domínguez, I. et al. Immunogenicity and efficacy of homologous and heterologous NDV and MVA SARS-CoV-2 vaccines in mice and hamsters. npj Vaccines 10, 246 (2025). https://doi.org/10.1038/s41541-025-01299-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41541-025-01299-3