Abstract
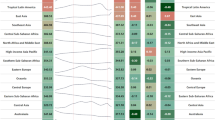
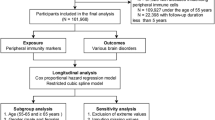
Growing evidence suggests that peripheral diseases serve as risk factors for dementia, but the population-level burden of dementia associated with various peripheral diseases has remained unknown. Here, by conducting a systematic review and Bayesian meta-analyses to estimate the relative risks of 26 peripheral diseases across 9 systems with dementia, including 202 articles searched from the PubMed until 6 September 2024, we identified 16 peripheral diseases as associated with increased risk of dementia. With the relative risks estimated from meta-analyses, prevalences extracted from the Global Burden of Disease Study, and communalities among these 16 peripheral diseases derived from the UK Biobank, we analysed the population attributable fractions (PAFs) of these 16 peripheral diseases for dementia, stratified by sex, age, sociodemographic index level, world region and country, and trends from 1990 to 2021. Globally, these peripheral diseases collectively were related to a combined PAF of 33.18% (95% confidence interval (CI) 16.80–48.43) of dementia burden, corresponding to 18.8 million prevalent cases. The leading ten PAF contributors were periodontal diseases (6.10%, 95% CI 0.95–10.28), cirrhosis and other chronic liver diseases (5.51%, 95% CI 1.77–8.86), age-related and other hearing loss (4.70%, 95% CI 3.51–6.06), blindness and vision loss (4.30%, 95% CI 3.43–5.05), type 2 diabetes mellitus (3.80%, 95% CI 3.06–4.53), chronic kidney disease (2.74%, 95% CI 1.53–4.02), osteoarthritis (2.26%, 95% CI 0.41–4.12), stroke (1.01%, 95% CI 0.86–1.17), ischaemic heart disease (0.97%, 95% CI 0.69–1.29) and chronic obstructive pulmonary disease (0.92%, 95% CI 0.34–1.54). This study revealed that a series of peripheral diseases were associated with increased risk of dementia and collectively were related to about one-third of the global dementia burden, highlighting the need for targeted public health strategies.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The GBD 2021 is publicly available via Global Health Data Exchange at https://vizhub.healthdata.org/gbd-results/. The UK Biobank resources can be accessed through applications on their website (https://www.ukbiobank.ac.uk/enable-your-research/apply-for-access). All included literature in the meta-analysis is available via PubMed at https://pubmed.ncbi.nlm.nih.gov/. The data extracted from studies included in the meta-analysis and the GBD dataset used in the study are available via Figshare at https://doi.org/10.6084/m9.figshare.30634574 (ref. 293). The UK Biobank data were used under licence and are thus not publicly available.
Code availability
The analytical methods in the study do not involve developing new computer code or algorithm that have not been previously reported. The analytical methods in the study had been described in detail in the article, with citations to the sources containing the relevant methodology and code. Accordingly, the original code required to reanalyse the data in this article is available from the corresponding author upon request.
References
Arthurton, L. et al. Dementia is a neglected noncommunicable disease and leading cause of death. Nat. Rev. Neurol. 21, 63–64 (2025).
Global Action Plan on the Public Health Response to Dementia 2017–2025 (World Health Organization, 2017).
GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health 7, e105–e125 (2022).
Livingston, G. et al. Dementia prevention, intervention, and care: 2024 report of the Lancet standing Commission. Lancet 404, 572–628 (2024).
Walsh, S. et al. Population-level interventions for the primary prevention of dementia: a complex evidence review. Lancet 402, S13 (2023).
Mansournia, M. A. & Altman, D. G. Population attributable fraction. Br. Med. J. 360, k757 (2018).
Stephan, B. C. M. et al. Population attributable fractions of modifiable risk factors for dementia: a systematic review and meta-analysis. Lancet Healthy Longev. 5, e406–e421 (2024).
Shang, X. et al. Association of a wide range of chronic diseases and apolipoprotein E4 genotype with subsequent risk of dementia in community-dwelling adults: a retrospective cohort study. EClinicalMedicine 45, 101335 (2022).
Huang, L. Y. et al. Identifying modifiable factors and their joint effect on brain health: an exposome-wide association study. Geroscience 46, 6257–6268 (2024).
Ren, Y. et al. Multimorbidity, cognitive phenotypes, and Alzheimer’s disease plasma biomarkers in older adults: a population-based study. Alzheimers Dement. 20, 1550–1561 (2024).
Ben Hassen, C. et al. Association between age at onset of multimorbidity and incidence of dementia: 30 year follow-up in Whitehall II prospective cohort study. Br. Med. J. 376, e068005 (2022).
Calvin, C. M., Conroy, M. C., Moore, S. F., Kuzma, E. & Littlejohns, T. J. Association of multimorbidity, disease clusters, and modification by genetic factors with risk of dementia. JAMA Netw. Open 5, e2232124 (2022).
Smith, E. E. et al. Systemic determinants of brain health in ageing. Nat. Rev. Neurol. 20, 647–659 (2024).
Zhao, B. et al. Heart-brain connections: phenotypic and genetic insights from magnetic resonance images. Science 380, abn6598 (2023).
Testai, F. D. et al. Cardiac contributions to brain health: a scientific statement from the American Heart Association. Stroke 55, e425–e438 (2024).
Dodd, J. W. Lung disease as a determinant of cognitive decline and dementia. Alzheimers Res. Ther. 7, 32 (2015).
Lutsey, P. L. et al. Impaired lung function, lung disease, and risk of incident dementia. Am. J. Respir. Crit. Care Med. 199, 1385–1396 (2019).
Smith, M. L., Wade, J. B., Wolstenholme, J. & Bajaj, J. S. Gut microbiome–brain–cirrhosis axis. Hepatology 80, 465–485 (2024).
Cheng, Y. et al. Physiological β-amyloid clearance by the liver and its therapeutic potential for Alzheimer’s disease. Acta Neuropathol. 145, 717–731 (2023).
Viggiano, D. et al. Mechanisms of cognitive dysfunction in CKD. Nat. Rev. Nephrol. 16, 452–469 (2020).
Bello-Corral, L. et al. Implications of gut and oral microbiota in neuroinflammatory responses in Alzheimer’s disease. Life Sci. 333, 122132 (2023).
Ma, X., Shin, Y. J., Yoo, J. W., Park, H. S. & Kim, D. H. Extracellular vesicles derived from Porphyromonas gingivalis induce trigeminal nerve-mediated cognitive impairment. J. Adv. Res. 54, 293–303 (2023).
Beydoun, H. A. et al. Mediating and moderating effects of plasma proteomic biomarkers on the association between poor oral health problems and incident dementia: the UK Biobank study. Geroscience 46, 5343–5363 (2024).
Dominy, S. S. et al. Porphyromonas gingivalis in Alzheimer’s disease brains: evidence for disease causation and treatment with small-molecule inhibitors. Sci. Adv. 5, eaau3333 (2019).
GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403, 2133–2161 (2024).
GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 402, 203–234 (2023).
GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob. Health 9, e144–e160 (2021).
GBD 2019 IMID Collaborators. Global, regional, and national incidence of six major immune-mediated inflammatory diseases: findings from the Global Burden of Disease Study 2019. EClinicalMedicine 64, 102193 (2023).
Walsh, S. et al. Considering challenges for the new Alzheimer’s drugs: clinical, population, and health system perspectives. Alzheimers Dement. 20, 6639–6646 (2024).
Ferguson, E. L. et al. Visual Impairment, Eye Conditions, And Diagnoses Of Neurodegeneration And Dementia. JAMA Netw. Open 7, e2424539 (2024).
Rutherford, B. R., Brewster, K., Golub, J. S., Kim, A. H. & Roose, S. P. Sensation and psychiatry: linking age-related hearing loss to late-life depression and cognitive decline. Am. J. Psychiatry 175, 215–224 (2018).
Burton, M. J. et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob. Health 9, e489–e551 (2021).
Liu, Z. T., Liu, M. H., Xiong, Y., Wang, Y. J. & Bu, X. L. Crosstalk between bone and brain in Alzheimer’s disease: mechanisms, applications, and perspectives. Alzheimers Dement. 20, 5720–5739 (2024).
Shi, T. et al. Osteocyte-derived sclerostin impairs cognitive function during ageing and Alzheimer’s disease progression. Nat. Metab. 6, 531–549 (2024).
Bajinka, O., Simbilyabo, L., Tan, Y., Jabang, J. & Saleem, S. A. Lung–brain axis. Crit. Rev. Microbiol. 48, 257–269 (2022).
Hoogendijk, E. O. et al. Frailty: implications for clinical practice and public health. Lancet 394, 1365–1375 (2019).
Skou, S. T. et al. Multimorbidity. Nat. Rev. Dis. Primers 8, 48 (2022).
Valletta, M. et al. Association of mild and complex multimorbidity with structural brain changes in older adults: a population-based study. Alzheimers Dement. 20, 1958–1965 (2024).
Hoffmann, J. P., Liu, J. A., Seddu, K. & Klein, S. L. Sex hormone signaling and regulation of immune function. Immunity 56, 2472–2491 (2023).
Yu, B. et al. B cell-specific XIST complex enforces X-inactivation and restrains atypical B cells. Cell 184, 1790–1803 (2021).
Gulati, M., Dursun, E., Vincent, K. & Watt, F. E. The influence of sex hormones on musculoskeletal pain and osteoarthritis. Lancet Rheumatol. 5, e225–e238 (2023).
Vosters, T. G. et al. The association and contribution of gender-related characteristics to prevalent chronic kidney disease in women and men in a multi-ethnic population—the HELIUS study. BMC Public Health 25, 853 (2025).
García, G. G. et al. Sex and gender differences in chronic kidney disease and access to care around the globe. Semin. Nephrol. 42, 101–113 (2022).
Kautzky-Willer, A., Leutner, M. & Harreiter, J. Sex differences in type 2 diabetes. Diabetologia 66, 986–1002 (2023).
Tramunt, B. et al. Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia 63, 453–461 (2020).
Reue, K. & Wiese, C. B. Illuminating the mechanisms underlying sex differences in cardiovascular disease. Circ. Res. 130, 1747–1762 (2022).
Hu, F. B. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care 34, 1249–1257 (2011).
Stein, M. M. et al. Innate immunity and asthma risk in Amish and Hutterite farm children. New Engl. J. Med. 375, 411–421 (2016).
Feng, M. et al. Associations of early life exposures and environmental factors with asthma among children in rural and urban areas of Guangdong, China. Chest 149, 1030–1041 (2016).
Zuo, T., Kamm, M. A., Colombel, J.-F. & Ng, S. C. Urbanization and the gut microbiota in health and inflammatory bowel disease. Nat. Rev. Gastroenterol. Hepatol. 15, 440–452 (2018).
Hunter, D. J. & Bierma-Zeinstra, S. Osteoarthritis. Lancet 393, 1745–1759 (2019).
GBD 2021 Osteoarthritis Collaborators. Global, regional, and national burden of osteoarthritis, 1990–2020 and projections to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Rheumatol. 5, e508–e522 (2023).
Momtazmanesh, S. et al. Global burden of chronic respiratory diseases and risk factors, 1990–2019: an update from the Global Burden of Disease Study 2019. EClinicalMedicine 59, 101936 (2023).
Xie, W. et al. Association of electronic cigarette use with incident respiratory conditions among US adults from 2013 to 2018. JAMA Netw. Open 3, e2020816 (2020).
GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 395, 709–733 (2020).
Ramke, J., Zwi, A. B., Palagyi, A., Blignault, I. & Gilbert, C. E. Equity and blindness: closing evidence gaps to support universal eye health. Ophthalmic Epidemiol. 22, 297–307 (2015).
Jiang, C. Y. et al. Global, regional, and national prevalence of hearing loss from 1990 to 2019: a trend and health inequality analyses based on the Global Burden of Disease Study 2019. Ageing Res. Rev. 92, 102124 (2023).
GBD 2019 Hearing Loss Collaborators. Hearing loss prevalence and years lived with disability, 1990–2019: findings from the Global Burden of Disease Study 2019. Lancet 397, 996–1009 (2021).
Peres, M. A. et al. Oral diseases: a global public health challenge. Lancet 394, 249–260 (2019).
Luan, Y. et al. Universal coverage for oral health care in 27 low-income countries: a scoping review. Glob. Health Res. Policy 9, 34 (2024).
Wang, R., Li, Z., Liu, S. & Zhang, D. Global, regional, and national burden of 10 digestive diseases in 204 countries and territories from 1990 to 2019. Front. Public Health 11, 1061453 (2023).
GBD 2017 Cirrhosis Collaborators. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 5, 245–266 (2020).
Kinane, D. F., Stathopoulou, P. G. & Papapanou, P. N. Periodontal diseases. Nat. Rev. Dis. Primers 3, 17038 (2017).
Howell, J. et al. A global investment framework for the elimination of hepatitis B. J. Hepatol. 74, 535–549 (2021).
Paraje, G. R., Jha, P., Savedoff, W. & Fuchs, A. Taxation of tobacco, alcohol, and sugar-sweetened beverages: reviewing the evidence and dispelling the myths. BMJ Glob. Health 8, e011866 (2023).
Chen, S. et al. Temporal trends in population attributable fractions of modifiable risk factors for dementia: a time-series study of the English Longitudinal Study of Ageing (2004–2019). BMC Med. 22, 268 (2024).
Welberry, H. J., Tisdell, C. C., Huque, M. H. & Jorm, L. R. Have we been underestimating modifiable dementia risk? An alternative approach for calculating the combined population attributable fraction for modifiable dementia risk factors. Am. J. Epidemiol. 192, 1763–1771 (2023).
GBD 2021 Demographics Collaborators. Global age-sex-specific mortality, life expectancy, and population estimates in 204 countries and territories and 811 subnational locations, 1950-2021, and the impact of the COVID-19 pandemic: a comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet 403, 1989–2056 (2024).
GBD 2021 Nervous System Disorders Collaborators. Global, regional, and national burden of disorders affecting the nervous system, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. 23, 344–381 (2024).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br. Med. J. 372, n71 (2021).
Guyatt, G. H. et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Br. Med. J. 336, 924–926 (2008).
Wells, G. et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (2013).
Aromataris, E. et al. JBI Manual for Evidence Synthesis. JBI https://synthesismanual.jbi.global (2024).
Klaver, C. C. et al. Is age-related maculopathy associated with Alzheimer’s disease? The Rotterdam Study. Am. J. Epidemiol. 150, 963–968 (1999).
Kessing, L. V., Lopez, A. G., Andersen, P. K. & Kessing, S. V. No increased risk of developing Alzheimer disease in patients with glaucoma. J. Glaucoma 16, 47–51 (2007).
Ou, Y., Grossman, D. S., Lee, P. P. & Sloan, F. A. Glaucoma, Alzheimer disease and other dementia: a longitudinal analysis. Ophthalmic Epidemiol. 19, 285–292 (2012).
Helmer, C. et al. Is there a link between open-angle glaucoma and dementia? The Three-City-Alienor cohort. Ann. Neurol. 74, 171–179 (2013).
Ekström, C. & Kilander, L. Pseudoexfoliation and Alzheimer’s disease: a population-based 30-year follow-up study. Acta Ophthalmol. 92, 355–358 (2014).
Exalto, L. G. et al. Severe diabetic retinal disease and dementia risk in type 2 diabetes. J. Alzheimers Dis. 42, S109–S117 (2014).
Lai, S. W., Lin, C. L. & Liao, K. F. Cataract may be a non-memory feature of Alzheimer’s disease in older people. Eur. J. Epidemiol. 29, 405–409 (2014).
Keenan, T. D., Goldacre, R. & Goldacre, M. J. Associations between primary open angle glaucoma, Alzheimer’s disease and vascular dementia: record linkage study. Br. J. Ophthalmol. 99, 524–527 (2015).
Su, C. W., Lin, C. C., Kao, C. H. & Chen, H. Y. Association between glaucoma and the risk of dementia. Medicine 95, e2833 (2016).
Davies-Kershaw, H. R. et al. Vision impairment and risk of dementia: findings from the English Longitudinal Study of Ageing. J. Am. Geriatr. Soc. 66, 1823–1829 (2018).
Brenowitz, W. D., Kaup, A. R., Lin, F. R. & Yaffe, K. Multiple sensory impairment is associated with increased risk of dementia among black and white older adults. J. Gerontol. A 74, 890–896 (2019).
Lee, C. S. et al. Associations between recent and established ophthalmic conditions and risk of Alzheimer’s disease. Alzheimers Dement. 15, 34–41 (2019).
Naël, V. et al. Vision loss and 12-year risk of dementia in older adults: the 3C cohort study. Eur. J. Epidemiol. 34, 141–152 (2019).
Choi, S., Jahng, W. J., Park, S. M. & Jee, D. Association of age-related macular degeneration on Alzheimer or Parkinson disease: a retrospective cohort study. Am. J. Ophthalmol. 210, 41–47 (2020).
Hwang, P. H. et al. Dual sensory impairment in older adults and risk of dementia from the GEM Study. Alzheimers Dement. 12, e12054 (2020).
Lee, A. T. C. et al. Higher dementia incidence in older adults with poor visual acuity. J. Gerontol. A 75, 2162–2168 (2020).
Tran, E. M. et al. Association of visual impairment with risk of incident dementia in a Women’s Health Initiative population. JAMA Ophthalmol. 138, 624–633 (2020).
Xiao, Z. et al. Association of glaucoma and cataract with incident dementia: a 5-year follow-up in the Shanghai Aging Study. J. Alzheimers Dis. 76, 529–537 (2020).
Ehrlich, J. R., Swenor, B. K., Zhou, Y. & Langa, K. M. The longitudinal association of vision impairment with transitions to cognitive impairment and dementia: findings from the Aging, Demographics and Memory Study. J. Gerontol. A 76, 2187–2193 (2021).
Hwang, P. H. et al. Ophthalmic conditions associated with dementia risk: The Cardiovascular Health Study. Alzheimers Dement. 17, 1442–1451 (2021).
Chang, P. Y. et al. Vascular complications of diabetes: natural history and corresponding risks of dementia in a national cohort of adults with diabetes. Acta Diabetol. 58, 859–867 (2021).
Killeen, O. J., Zhou, Y. & Ehrlich, J. R. Objectively measured visual impairment and dementia prevalence in older adults in the US. JAMA Ophthalmol. 141, 786–790 (2023).
Park, D. Y., Kim, M., Bae, Y., Jang, H. & Lim, D. H. Risk of dementia in newly diagnosed glaucoma: a nationwide cohort study in Korea. Ophthalmology 130, 684–691 (2023).
Shang, X. et al. Associations of ophthalmic and systemic conditions with incident dementia in the UK Biobank. Br. J. Ophthalmol. 107, 275–282 (2023).
Gates, G. A., Anderson, M. L., McCurry, S. M., Feeney, M. P. & Larson, E. B. Central auditory dysfunction as a harbinger of Alzheimer dementia. Arch. Otolaryngol. Head Neck Surg. 137, 390–395 (2011).
Lin, F. R. et al. Hearing loss and incident dementia. Arch. Neurol. 68, 214–220 (2011).
Gurgel, R. K. et al. Relationship of hearing loss and dementia: a prospective, population-based study. Otol. Neurotol. 35, 775–781 (2014).
Davies, H. R., Cadar, D., Herbert, A., Orrell, M. & Steptoe, A. Hearing impairment and incident dementia: findings from the English Longitudinal Study of Ageing. J. Am. Geriatr. Soc. 65, 2074–2081 (2017).
Golub, J. S. et al. Observed hearing loss and incident dementia in a multiethnic cohort. J. Am. Geriatr. Soc. 65, 1691–1697 (2017).
Heywood, R. et al. Hearing loss and risk of mild cognitive impairment and dementia: findings from the Singapore Longitudinal Ageing Study. Dement. Geriatr. Cogn. Disord. 43, 259–268 (2017).
Su, P. et al. Age-related hearing loss and dementia: a 10-year national population-based study. Eur. Arch. Otorhinolaryngol. 274, 2327–2334 (2017).
Amieva, H., Ouvrard, C., Meillon, C., Rullier, L. & Dartigues, J. F. Death, depression, disability, and dementia associated with self-reported hearing problems: a 25-year study. J. Gerontol. A 73, 1383–1389 (2018).
Vassilaki, M. et al. Informant-based hearing difficulties and the risk for mild cognitive impairment and dementia. Age Ageing 48, 888–894 (2019).
Osler, M. et al. Hearing loss, cognitive ability, and dementia in men age 19–78 years. Eur. J. Epidemiol. 34, 125–130 (2019).
Kuo, P. L. et al. Prevalence of concurrent functional vision and hearing impairment and association with dementia in community-dwelling medicare beneficiaries. JAMA Netw. Open 4, e211558 (2021).
Brewster, K. K. et al. Age-related hearing loss, late-life depression, and risk for incident dementia in older adults. J. Gerontol. A 76, 827–834 (2021).
Chern, A., Sharma, R. K. & Golub, J. S. Hearing loss and incident dementia: claims data from the New York SPARCS database. Otol. Neurotol. 43, 36–41 (2022).
Myrstad, C. et al. Hearing impairment and risk of dementia in The HUNT Study (HUNT4 70+): a Norwegian cohort study. EClinicalMedicine 66, 102319 (2023).
Tonelli, M. et al. Associations between hearing loss and clinical outcomes: population-based cohort study. EClinicalMedicine 61, 102068 (2023).
Hendriks, S. et al. Risk factors for young-onset dementia in the UK Biobank. JAMA Neurol. 81, 134–142 (2024).
Cantuaria, M. L. et al. Hearing loss, hearing aid use, and risk of dementia in older adults. JAMA Otolaryngol. Head Neck Surg. 150, 157–164 (2024).
Chen, T. B. et al. Comorbidity and dementia: a nationwide survey in Taiwan. PLoS ONE 12, e0175475 (2017).
Labenz, C., Kostev, K., Kaps, L., Galle, P. R. & Schattenberg, J. M. Incident dementia in elderly patients with nonalcoholic fatty liver disease in Germany. Dig. Dis. Sci. 66, 3179–3185 (2021).
Lampignano, L. et al. Liver health and dementia in an Italian older population: findings from the Salus in Apulia Study. Front. Aging Neurosci. 13, 748888 (2021).
Parikh, N. S. et al. Association between liver fibrosis and incident dementia in the UK Biobank study. Eur. J. Neurol. 29, 2622–2630 (2022).
Xiao, T., van Kleef, L. A., Ikram, M. K., de Knegt, R. J. & Ikram, M. A. Association of nonalcoholic fatty liver disease and fibrosis with incident dementia and cognition: The Rotterdam Study. Neurology 99, e565–e573 (2022).
Shang, Y., Widman, L. & Hagström, H. Nonalcoholic fatty liver disease and risk of dementia: a population-based cohort study. Neurology 99, e574–e582 (2022).
Wang, Y. et al. Nonalcoholic fatty liver disease, serum cytokines, and dementia among rural-dwelling older adults in China: a population-based study. Eur. J. Neurol. 29, 2612–2621 (2022).
Jeong, S. et al. Association of non-alcoholic fatty liver disease with incident dementia later in life among elder adults. Clin. Mol. Hepatol. 28, 510–521 (2022).
Lu, Y. et al. Liver integrity and the risk of Alzheimer’s disease and related dementias. Alzheimers Dement. 20, 1913–1922 (2024).
Solfrizzi, V. et al. Liver fibrosis score, physical frailty, and the risk of dementia in older adults: The Italian Longitudinal Study on Aging. Alzheimers Dement. 6, e12065 (2020).
Yuan, S. et al. Digestive system diseases, genetic risk, and incident dementia: a prospective cohort study. Am. J. Prev. Med. 66, 516–525 (2024).
Paik, W. H. et al. Acute pancreatitis and the risk of dementia in diabetes: a nationwide cohort study using Korean Healthcare Claims Database. J. Alzheimers Dis. 94, 205–216 (2023).
Liang, C. S. et al. The risk of Alzheimer’s disease after acute appendicitis with or without appendectomy. J. Am. Med. Dir. Assoc. 23, 601–607.e602 (2022).
Silber, J. H. et al. Alzheimer’s dementia after exposure to anesthesia and surgery in the elderly: a matched natural experiment using appendicitis. Ann. Surg. 276, e377–e385 (2022).
Hung, K. C., Sun, C. K., Chen, J. Y., Wang, H. C. & Kao, C. H. Association between abdominal hernia and the risk of subsequent dementia. Brain Behav. 9, e01434 (2019).
Chen, C. K., Wu, Y. T. & Chang, Y. C. Association between chronic periodontitis and the risk of Alzheimer’s disease: a retrospective, population-based, matched-cohort study. Alzheimers Res. Ther. 9, 56 (2017).
Holmer, J., Eriksdotter, M., Schultzberg, M., Pussinen, P. J. & Buhlin, K. Association between periodontitis and risk of Alzheimer’s disease, mild cognitive impairment and subjective cognitive decline: a case–control study. J. Clin. Periodontol. 45, 1287–1298 (2018).
Tiisanoja, A. et al. Oral diseases and inflammatory burden and Alzheimer’s disease among subjects aged 75 years or older. Spec. Care Dentist 39, 158–165 (2019).
de Oliveira Araújo, R. et al. Association between periodontitis and Alzheimer’s disease and its impact on the self-perceived oral health status: a case–control study. Clin. Oral Investig. 25, 555–562 (2021).
Holmer, J. et al. Periodontal conditions and incident dementia: a nationwide Swedish cohort study. J. Periodontol. 93, 1378–1386 (2022).
Kulkarni, M. S. et al. Poor oral health linked with higher risk of Alzheimer’s disease. Brain Sci. 13, 1555 (2023).
Yoo, J. E. et al. Association between dental diseases and oral hygiene care and the risk of dementia: a retrospective cohort study. J. Am. Med. Dir. Assoc. 24, 1924–1930.e1923 (2023).
Stein, P. S., Desrosiers, M., Donegan, S. J., Yepes, J. F. & Kryscio, R. J. Tooth loss, dementia and neuropathology in the Nun study. J. Am. Dent. Assoc. 138, 1314–1322 (2007).
Batty, G. D. et al. Oral disease in relation to future risk of dementia and cognitive decline: prospective cohort study based on the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified-Release Controlled Evaluation (ADVANCE) trial. Eur. Psychiatry 28, 49–52 (2013).
Takeuchi, K. et al. Tooth loss and risk of dementia in the community: the Hisayama study. J. Am. Geriatr. Soc. 65, e95–e100 (2017).
Kusama, T., Takeuchi, K., Kiuchi, S., Aida, J. & Osaka, K. Poor oral health and dementia risk under time-varying confounding: a cohort study based on marginal structural models. J. Am. Geriatr. Soc. 72, 729–741 (2024).
Ott, A. et al. Diabetes mellitus and the risk of dementia: The Rotterdam Study. Neurology 53, 1937–1942 (1999).
Peila, R., Rodriguez, B. L. & Launer, L. J. Type 2 diabetes, APOE gene, and the risk for dementia and related pathologies: The Honolulu-Asia Aging Study. Diabetes 51, 1256–1262 (2002).
Schnaider Beeri, M. et al. Diabetes mellitus in midlife and the risk of dementia three decades later. Neurology 63, 1902–1907 (2004).
Yaffe, K. et al. Diabetes, impaired fasting glucose, and development of cognitive impairment in older women. Neurology 63, 658–663 (2004).
Irie, F. et al. Enhanced risk for Alzheimer disease in persons with type 2 diabetes and APOE epsilon4: the Cardiovascular Health Study Cognition Study. Arch. Neurol. 65, 89–93 (2008).
Raffaitin, C. et al. Metabolic syndrome and risk for incident Alzheimer’s disease or vascular dementia: the Three-City Study. Diabetes Care 32, 169–174 (2009).
Xu, W. et al. Accelerated progression from mild cognitive impairment to dementia in people with diabetes. Diabetes 59, 2928–2935 (2010).
Ahtiluoto, S. et al. Diabetes, Alzheimer disease, and vascular dementia: a population-based neuropathologic study. Neurology 75, 1195–1202 (2010).
Cheng, D. et al. Type 2 diabetes and late-onset Alzheimer’s disease. Dement. Geriatr. Cogn. Disord. 31, 424–430 (2011).
Cheng, C. et al. Type 2 diabetes and antidiabetic medications in relation to dementia diagnosis. J. Gerontol. A 69, 1299–1305 (2014).
Mehlig, K. et al. Physical activity, weight status, diabetes and dementia: a 34-year follow-up of the population study of women in Gothenburg. Neuroepidemiology 42, 252–259 (2014).
Davis, W. A., Zilkens, R. R., Starkstein, S. E., Davis, T. M. & Bruce, D. G. Dementia onset, incidence and risk in type 2 diabetes: a matched cohort study with the Fremantle Diabetes Study Phase I. Diabetologia 60, 89–97 (2017).
Salinas, R. M., Hiriart, M., Acosta, I., Sosa, A. L. & Prince, M. J. Type 2 diabetes mellitus as a risk factor for dementia in a Mexican population. J. Diabetes Complications 30, 1234–1239 (2016).
Wennberg, A. M. V. et al. Longitudinal association between diabetes and cognitive decline: The National Health and Aging Trends Study. Arch. Gerontol. Geriatr. 72, 39–44 (2017).
Rawlings, A. M. et al. The association of late-life diabetes status and hyperglycemia with incident mild cognitive impairment and dementia: The ARIC Study. Diabetes Care 42, 1248–1254 (2019).
Frison, E. et al. Diabetes-associated dementia risk and competing risk of death in the Three-City Study. J. Alzheimers Dis. 71, 1339–1350 (2019).
Barbiellini Amidei, C. et al. Association between age at diabetes onset and subsequent risk of dementia. JAMA 325, 1640–1649 (2021).
Li, F. R. et al. Influence of diabetes duration and glycemic control on dementia: a cohort study. J. Gerontol. A 76, 2062–2070 (2021).
Yen, F. S., Wei, J. C., Yip, H. T., Hwu, C. M. & Hsu, C. C. Diabetes, hypertension, and the risk of dementia. J. Alzheimers Dis. 89, 323–333 (2022).
Nagar, S. D. et al. Investigation of hypertension and type 2 diabetes as risk factors for dementia in the All of Us cohort. Sci Rep. 12, 19797 (2022).
Wang, K. & Liu, H. Early-onset subgroup of type 2 diabetes and risk of dementia, Alzheimer’s disease and stroke: a cohort study. J. Prev. Alzheimers Dis. 8, 442–447 (2021).
Sasaki, Y. et al. Chronic kidney disease: a risk factor for dementia onset: a population-based study. The Osaki-Tajiri Project. J Am Geriatr Soc 59, 1175–1181 (2011).
O’Hare, A. M. et al. Relationship between longitudinal measures of renal function and onset of dementia in a community cohort of older adults. J. Am. Geriatr. Soc. 60, 2215–2222 (2012).
Miwa, K. et al. Chronic kidney disease is associated with dementia independent of cerebral small-vessel disease. Neurology 82, 1051–1057 (2014).
Kuo, Y. T. et al. Risk of dementia in patients with end-stage renal disease under maintenance dialysis-a nationwide population-based study with consideration of competing risk of mortality. Alzheimers Res. Ther. 11, 31 (2019).
Tseng, T. J., Yen, Y. T., Yang, Y. H., Chen, Y. H. & Chan, T. C. Association between the occurrence of albuminuria and the risk of early dementia among older people upon health examination: a community-based cohort study in Taiwan. BMJ Open 10, e041664 (2020).
Hiramatsu, R., Iwagami, M. & Nitsch, D. Association between chronic kidney disease and incident diagnosis of dementia in England: a cohort study in Clinical Practice Research Datalink. BMJ Open 10, e033811 (2020).
Wang, M. et al. Kidney function and dementia risk in community-dwelling older adults: the Shanghai Aging Study. Alzheimers Res. Ther. 13, 21 (2021).
Kjaergaard, A. D., Johannesen, B. R., Sørensen, H. T., Henderson, V. W. & Christiansen, C. F. Kidney disease and risk of dementia: a Danish nationwide cohort study. BMJ Open 11, e052652 (2021).
Månsson, T. & Elmståhl, S. Processing speed is affected by early impairment in kidney function in the general elder population. BMC Nephrol. 22, 314 (2021).
Lee, S. I. et al. Decreased renal function is associated with incident dementia: an IMRD-THIN retrospective cohort study in the UK. Alzheimers Dement. 18, 1943–1956 (2022).
Singh-Manoux, A. et al. Association between kidney function and incidence of dementia: 10-year follow-up of the Whitehall II cohort study. Age Ageing 51, afab259 (2022).
Yeh, T. S. et al. Kidney function, albuminuria, and their modification by genetic factors and risk of incident dementia in UK Biobank. Alzheimers Res. Ther. 15, 138 (2023).
Kwon, M. J. et al. Exploring the link between chronic kidney disease and Alzheimer’s disease: a longitudinal follow-up study using the Korean National Health Screening Cohort. Biomedicines 11, 1606 (2023).
Kelly, D. M. et al. Impaired kidney function, cerebral small vessel disease and cognitive disorders: the Framingham Heart Study. Nephrol. Dial Transplant. 39, 1911–1922 (2024).
Desmond, D. W., Moroney, J. T., Sano, M. & Stern, Y. Incidence of dementia after ischemic stroke: results of a longitudinal study. Stroke 33, 2254–2260 (2002).
Kuller, L. H. et al. Risk factors for dementia in the cardiovascular health cognition study. Neuroepidemiology 22, 13–22 (2003).
Srikanth, V. K. et al. Progressive dementia after first-ever stroke: a community-based follow-up study. Neurology 63, 785–792 (2004).
Ivan, C. S. et al. Dementia after stroke: the Framingham Study. Stroke 35, 1264–1268 (2004).
Simons, L. A., Simons, J., McCallum, J. & Friedlander, Y. Lifestyle factors and risk of dementia: Dubbo Study of the elderly. Med J Aust 184, 68–70 (2006).
Yip, A. G., Brayne, C. & Matthews, F. E. Risk factors for incident dementia in England and Wales: The Medical Research Council Cognitive Function and Ageing Study. A population-based nested case–control study. Age Ageing 35, 154–160 (2006).
Hayden, K. M. et al. Vascular risk factors for incident Alzheimer disease and vascular dementia: the Cache County study. Alzheimer Dis. Assoc. Disord. 20, 93–100 (2006).
Qiu, C., Xu, W., Winblad, B. & Fratiglioni, L. Vascular risk profiles for dementia and Alzheimer’s disease in very old people: a population-based longitudinal study. J. Alzheimers Dis. 20, 293–300 (2010).
de Bruijn, R. F. et al. The potential for prevention of dementia across two decades: the prospective, population-based Rotterdam Study. BMC Med. 13, 132 (2015).
Ganguli, M. et al. Rates and risk factors for progression to incident dementia vary by age in a population cohort. Neurology 84, 72–80 (2015).
Hendrie, H. C. et al. Statin use, incident dementia and Alzheimer disease in elderly African Americans. Ethn. Dis. 25, 345–354 (2015).
Corraini, P. et al. Long-term risk of dementia among survivors of ischemic or hemorrhagic stroke. Stroke 48, 180–186 (2017).
Hsu, P. F. et al. C-reactive protein predicts incidence of dementia in an elderly Asian community cohort. J. Am. Med. Dir. Assoc. 18, 277.e277–277.e211 (2017).
Li, C. H. et al. Factors of post-stroke dementia: a nationwide cohort study in Taiwan. Geriatr. Gerontol. Int. 19, 815–822 (2019).
Guo, X., Östling, S., Kern, S., Johansson, L. & Skoog, I. Increased risk for dementia both before and after stroke: a population-based study in women followed over 44 years. Alzheimers Dement. 14, 1253–1260 (2018).
Clair, L., Anderson, H., Anderson, C., Ekuma, O. & Prior, H. J. Cardiovascular disease and the risk of dementia: a survival analysis using administrative data from Manitoba. Can. J. Public Health 113, 455–464 (2022).
Lu, Y. et al. Cardiometabolic and vascular disease factors and mild cognitive impairment and dementia. Gerontology 68, 1061–1069 (2022).
Zhong, W. et al. Prevalent stroke, age of its onset, and post-stroke lifestyle in relation to dementia: a prospective cohort study. Alzheimers Dement. 19, 3998–4007 (2023).
Koton, S. et al. Association of ischemic stroke incidence, severity, and recurrence with dementia in the atherosclerosis risk in communities cohort study. JAMA Neurol. 79, 271–280 (2022).
Dove, A. et al. Cardiometabolic multimorbidity accelerates cognitive decline and dementia progression. Alzheimers Dement. 19, 821–830 (2023).
Kauko, A., Engler, D., Niiranen, T., Ortega-Alonso, A. & Schnabel, R. B. Increased risk of dementia differs across cardiovascular diseases and types of dementia—data from a nationwide study. J. Intern. Med. 295, 196–205 (2024).
Hwangbo, S. et al. Dementia incidence and population-attributable fraction for dementia risk factors in Republic of Korea: a 12-year longitudinal follow-up study of a national cohort. Front. Aging Neurosci. 15, 1126587 (2023).
Veronese, N. et al. Multimorbidity increases the risk of dementia: a 15 year follow-up of the SHARE study. Age Ageing 52, afad052 (2023).
Aronson, M. K. et al. Women, myocardial infarction, and dementia in the very old. Neurology 40, 1102–1106 (1990).
Kivipelto, M. et al. Apolipoprotein E epsilon4 allele, elevated midlife total cholesterol level, and high midlife systolic blood pressure are independent risk factors for late-life Alzheimer disease. Ann. Intern. Med. 137, 149–155 (2002).
Newman, A. B. et al. Dementia and Alzheimer’s disease incidence in relationship to cardiovascular disease in the Cardiovascular Health Study cohort. J. Am. Geriatr. Soc. 53, 1101–1107 (2005).
Bursi, F. et al. Heart disease and dementia: a population-based study. Am. J. Epidemiol. 163, 135–141 (2006).
Ikram, M. A. et al. Unrecognized myocardial infarction in relation to risk of dementia and cerebral small vessel disease. Stroke 39, 1421–1426 (2008).
Chen, R. et al. Incident dementia in a defined older Chinese population. PLoS ONE 6, e24817 (2011).
Takahashi, P. Y., Caldwell, C. R. & Targonski, P. V. Effect of vascular burden as measured by vascular indexes upon vascular dementia: a matched case–control study. Clin. Interv. Aging 7, 27–33 (2012).
Haring, B. et al. Cardiovascular disease and cognitive decline in postmenopausal women: results from the Women’s Health Initiative Memory Study. J. Am. Heart Assoc. 2, e000369 (2013).
Rusanen, M. et al. Heart diseases and long-term risk of dementia and Alzheimer’s disease: a population-based CAIDE study. J. Alzheimers Dis. 42, 183–191 (2014).
Kuo, S. C. et al. Association between comorbidities and dementia in diabetes mellitus patients: population-based retrospective cohort study. J. Diabetes Complications 29, 1071–1076 (2015).
Heath, C. A., Mercer, S. W. & Guthrie, B. Vascular comorbidities in younger people with dementia: a cross-sectional population-based study of 616 245 middle-aged people in Scotland. J. Neurol. Neurosurg. Psychiatry 86, 959–964 (2015).
Booker, A., Jacob, L. E., Rapp, M., Bohlken, J. & Kostev, K. Risk factors for dementia diagnosis in German primary care practices. Int. Psychogeriatr. 28, 1059–1065 (2016).
Deng, J. et al. Prevalence and effect factors of dementia among the community elderly in Chongqing, China. Psychogeriatrics 18, 412–420 (2018).
Imahori, Y. et al. Association of ischemic heart disease with long-term risk of cognitive decline and dementia: a cohort study. Alzheimers Dement. 19, 5541–5549 (2023).
Liang, J. et al. Association between onset age of coronary heart disease and incident dementia: a prospective cohort study. J. Am. Heart Assoc. 12, e031407 (2023).
Olesen, K. K. W. et al. Diabetes and coronary artery disease as risk factors for dementia. Eur. J. Prev. Cardiol. 32, 477–484 (2025).
Forti, P. et al. Atrial fibrillation and risk of dementia in non-demented elderly subjects with and without mild cognitive impairment (MCI). Arch. Gerontol. Geriatr. 44, 155–165 (2007).
Marengoni, A., Qiu, C., Winblad, B. & Fratiglioni, L. Atrial fibrillation, stroke and dementia in the very old: a population-based study. Neurobiol. Aging 32, 1336–1337 (2011).
Dublin, S. et al. Atrial fibrillation and risk of dementia: a prospective cohort study. J. Am. Geriatr. Soc. 59, 1369–1375 (2011).
de Bruijn, R. F. et al. Association between atrial fibrillation and dementia in the general population. JAMA Neurol. 72, 1288–1294 (2015).
Liao, J. N. et al. Risk and prediction of dementia in patients with atrial fibrillation—a nationwide population-based cohort study. Int. J. Cardiol. 199, 25–30 (2015).
Marzona, I. et al. Risk of dementia and death in patients with atrial fibrillation: a competing risk analysis of a population-based cohort. Int. J. Cardiol. 220, 440–444 (2016).
Walters, K. et al. Predicting dementia risk in primary care: development and validation of the Dementia Risk Score using routinely collected data. BMC Med. 14, 6 (2016).
Singh-Manoux, A. et al. Atrial fibrillation as a risk factor for cognitive decline and dementia. Eur. Heart J. 38, 2612–2618 (2017).
Ding, M. et al. Atrial fibrillation, antithrombotic treatment, and cognitive aging: a population-based study. Neurology 91, e1732–e1740 (2018).
Chen, L. Y. et al. Association of atrial fibrillation with cognitive decline and dementia over 20 years: The ARIC-NCS (Atherosclerosis Risk in Communities Neurocognitive Study). J. Am. Heart Assoc. 7, e007301 (2018).
Kim, D. et al. Risk of dementia in stroke-free patients diagnosed with atrial fibrillation: data from a population-based cohort. Eur. Heart J. 40, 2313–2323 (2019).
Rydén, L. et al. Atrial fibrillation increases the risk of dementia amongst older adults even in the absence of stroke. J. Intern. Med. 286, 101–110 (2019).
Bansal, N. et al. Incident atrial fibrillation and risk of dementia in a diverse, community-based population. J. Am. Heart Assoc. 12, e028290 (2023).
van Oijen, M. et al. Atherosclerosis and risk for dementia. Ann. Neurol. 61, 403–410 (2007).
Guerchet, M. et al. Association between a low ankle-brachial index and dementia in a general elderly population in Central Africa (Epidemiology of Dementia in Central Africa Study). J. Am. Geriatr. Soc. 61, 1135–1140 (2013).
Huang, S. W. et al. Osteoarthritis increases the risk of dementia: a nationwide cohort study in Taiwan. Sci Rep. 5, 10145 (2015).
Chen, K. T. et al. Rheumatic diseases are associated with a higher risk of dementia: a nation-wide, population-based, case–control study. Int. J. Rheum. Dis. 21, 373–380 (2018).
Innes, K. E. & Sambamoorthi, U. The Association of osteoarthritis and related pain burden to incident Alzheimer’s disease and related dementias: a retrospective cohort study of U.S. Medicare beneficiaries. J. Alzheimers Dis. 75, 789–805 (2020).
Swain, S. et al. Temporal relationship between osteoarthritis and comorbidities: a combined case control and cohort study in the UK primary care setting. Rheumatology 60, 4327–4339 (2021).
Kiadaliri, A., Dell’Isola, A., Turkiewicz, A. & Englund, M. Rheumatic and musculoskeletal diseases and risk of dementia: a nested case–control study. ACR Open Rheumatol. 6, 504–510 (2024).
Guo, R. et al. Osteoarthritis, osteoarthritis treatment and risk of incident dementia: a prospective cohort study based on UK Biobank. Age Ageing 53, afae167 (2024).
Endo, Y. et al. Radiographic knee osteoarthritis is a risk factor for the development of dementia: locomotive syndrome and health outcomes in the Aizu Cohort Study. J. Clin. Med. 13, 4956 (2024).
Liao, W. C., Lin, C. L., Chang, S. N., Tu, C. Y. & Kao, C. H. The association between chronic obstructive pulmonary disease and dementia: a population-based retrospective cohort study. Eur. J. Neurol. 22, 334–340 (2015).
Xie, F. & Xie, L. COPD and the risk of mild cognitive impairment and dementia: a cohort study based on the Chinese Longitudinal Health Longevity Survey. Int. J. Chron. Obstruct. Pulmon. Dis. 14, 403–408 (2019).
Xiao, T. et al. Lung function impairment and the risk of incident dementia: The Rotterdam Study. J. Alzheimers Dis. 82, 621–630 (2021).
Wotton, C. J. & Goldacre, M. J. Associations between specific autoimmune diseases and subsequent dementia: retrospective record-linkage cohort study, UK. J. Epidemiol. Commun. Health 71, 576–583 (2017).
Mahmoudi, E. et al. Diagnosis of Alzheimer’s disease and related dementia among people with multiple sclerosis: large cohort study, USA. Mult. Scler. Relat. Disord. 57, 103351 (2022).
Cho, E. B. et al. The risk of dementia in multiple sclerosis and neuromyelitis optica spectrum disorder. Front. Neurosci. 17, 1214652 (2023).
Huang, J. et al. Inflammatory diseases, inflammatory biomarkers, and Alzheimer disease: an observational analysis and Mendelian randomization. Neurology 100, e568–e581 (2023).
Fleming, N. H., Bahorik, A., Xia, F. & Yaffe, K. Risk of dementia in older veterans with multiple sclerosis. Mult. Scler. Relat. Disord. 82, 105372 (2024).
Zhang, B. et al. Inflammatory bowel disease is associated with higher dementia risk: a nationwide longitudinal study. Gut 70, 85–91 (2021).
Zingel, R., Bohlken, J. & Kostev, K. Association between inflammatory bowel disease and dementia: a retrospective cohort study. J. Alzheimers Dis. 80, 1471–1478 (2021).
Kim, G. H. et al. Risk of neurodegenerative diseases in patients with inflammatory bowel disease: a nationwide population-based cohort study. J. Crohns Colitis 16, 436–443 (2022).
Rønnow Sand, J. et al. Risk of dementia in patients with inflammatory bowel disease: a Danish population-based study. Aliment. Pharmacol. Ther. 56, 831–843 (2022).
Sun, Y. et al. Association between inflammatory bowel disease and dementia: a longitudinal cohort study. Inflamm. Bowel Dis. 28, 1520–1526 (2022).
Aggarwal, M. et al. Alzheimer disease occurs more frequently in patients with inflammatory bowel disease: insight from a nationwide study. J. Clin. Gastroenterol. 57, 501–507 (2023).
Garcia-Argibay, M., Hiyoshi, A. & Montgomery, S. Association between dementia risk and ulcerative colitis, with and without colectomy: a Swedish population-based register study. BMJ Open 13, e074110 (2023).
Abuabara, K. et al. Cause-specific mortality in patients with severe psoriasis: a population-based cohort study in the U.K. Br. J. Dermatol. 163, 586–592 (2010).
Pezzolo, E. et al. Psoriasis is not associated with cognition, brain imaging markers, and risk for dementia: The Rotterdam Study. J. Am. Acad. Dermatol. 85, 671–680 (2021).
Kim, M., Park, H. E., Lee, S. H., Han, K. & Lee, J. H. Increased risk of Alzheimer’s disease in patients with psoriasis: a nationwide population-based cohort study. Sci. Rep. 10, 6454 (2020).
Leisner, M. Z. et al. Psoriasis and risk of mental disorders in Denmark. JAMA Dermatol. 155, 745–747 (2019).
Lin, C. C., Lin, H. C. & Chiu, H. W. Association between psoriasis and dementia: a population-based case–control study. Am. J. Clin. Dermatol. 20, 457–463 (2019).
Wu, C. Y., Hu, H. Y., Chou, Y. J., Li, C. P. & Chang, Y. T. Psoriasis is not a risk factor for dementia: a 12-year nationwide population-based cohort study. Arch. Dermatol. Res. 312, 657–664 (2020).
Kridin, K. et al. Psoriasis and dementia: a cross-sectional study of 121,801 patients. Acta Derm. Venereol. 100, adv00250 (2020).
Zhang, Y. R. et al. Immune-mediated diseases are associated with a higher incidence of dementia: a prospective cohort study of 375,894 individuals. Alzheimers Res. Ther. 14, 130 (2022).
Eriksson, U. K., Gatz, M., Dickman, P. W., Fratiglioni, L. & Pedersen, N. L. Asthma, eczema, rhinitis and the risk for dementia. Dement. Geriatr. Cogn. Disord. 25, 148–156 (2008).
Pan, T. L. et al. Atopic dermatitis and dementia risk: a nationwide longitudinal study. Ann. Allergy Asthma Immunol. 127, 200–205 (2021).
Magyari, A. et al. Adult atopic eczema and the risk of dementia: a population-based cohort study. J. Am. Acad. Dermatol. 87, 314–322 (2022).
Joh, H. K. et al. Allergic diseases and risk of incident dementia and Alzheimer’s disease. Ann. Neurol. 93, 384–397 (2023).
Ng, T. P., Chiam, P. C. & Kua, E. H. Mental disorders and asthma in the elderly: a population-based study. Int. J. Geriatr. Psychiatry 22, 668–674 (2007).
Chen, M. H. et al. Risk of dementia among patients with asthma: a nationwide longitudinal study. J. Am. Med. Dir. Assoc. 15, 763–767 (2014).
Peng, Y. H. et al. Adult asthma increases dementia risk: a nationwide cohort study. J. Epidemiol. Commun. Health 69, 123–128 (2015).
Bartels, C. M. et al. Alzheimer incidence and prevalence with and without asthma: a Medicare cohort study. J. Allergy Clin. Immunol. 154, 498–502 (2024).
Lu, K. et al. Association between autoimmune rheumatic diseases and the risk of dementia. BioMed Res. Int. 2014, 861812 (2014).
Wallin, K. et al. Midlife rheumatoid arthritis increases the risk of cognitive impairment two decades later: a population-based study. J. Alzheimers Dis. 31, 669–676 (2012).
Lin, T. M. et al. Autoimmune rheumatic diseases increase dementia risk in middle-aged patients: a nationwide cohort study. PLoS ONE 13, e0186475 (2018).
Min, C., Bang, W. J., Kim, M., Oh, D. J. & Choi, H. G. Rheumatoid arthritis and neurodegenerative dementia: a nested case–control study and a follow-up study using a national sample cohort. Clin. Rheumatol. 39, 159–166 (2020).
Kronzer, V. L. et al. Trends in incidence of dementia among patients with rheumatoid arthritis: a population-based cohort study. Semin. Arthritis Rheum. 51, 853–857 (2021).
Xue, M. et al. Diabetes mellitus and risks of cognitive impairment and dementia: a systematic review and meta-analysis of 144 prospective studies. Ageing Res. Rev. 55, 100944 (2019).
Ronksley, P. E., Brien, S. E., Turner, B. J., Mukamal, K. J. & Ghali, W. A. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 342, d671 (2011).
Zhang, J. & Yu, K. F. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 280, 1690–1691 (1998).
Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 36, 1–48 (2010).
Röver, C. Bayesian random-effects meta-analysis using the bayesmeta R package. J. Stat. Softw. 93, 1–51 (2020).
Röver, C. & Friede, T. Using the bayesmeta R package for Bayesian random-effects meta-regression. Comput. Methods Programs Biomed. 229, 107303 (2023).
Ambati, J. et al. Repurposing anti-inflammasome NRTIs for improving insulin sensitivity and reducing type 2 diabetes development. Nat. Commun. 11, 4737 (2020).
Seide, S. E., Röver, C. & Friede, T. Likelihood-based random-effects meta-analysis with few studies: empirical and simulation studies. BMC Med. Res. Method. 19, 16 (2019).
Spiegelhalter, D. J., Abrams, K. R. & Myles, J. P. Bayesian Approaches to Clinical Trials and Health-Care Evaluation (John Wiley & Sons, 2004).
Harrer, M., Cuijpers, P., Furukawa, T. & Ebert D. Doing Meta-analysis with R: A Hands-On Guide (Chapman and Hall/CRC, 2021).
Jakobsen, J. C., Wetterslev, J., Winkel, P., Lange, T. & Gluud, C. Thresholds for statistical and clinical significance in systematic reviews with meta-analytic methods. BMC Med. Res. Methodol. 14, 120 (2014).
Morey, R. D. & Rouder, J. N. Bayes factor approaches for testing interval null hypotheses. Psychol. Methods 16, 406–419 (2011).
Villamor, E. et al. Patent ductus arteriosus and bronchopulmonary dysplasia-associated pulmonary hypertension: a Bayesian meta-analysis. JAMA Netw. Open 6, e2345299 (2023).
Albuquerque, A. M., Tramujas, L., Sewanan, L. R., Williams, D. R. & Brophy, J. M. Mortality rates among hospitalized patients with COVID-19 infection treated with tocilizumab and corticosteroids: a bayesian reanalysis of a previous meta-analysis. JAMA Netw. Open 5, e220548 (2022).
Levin, M. L. The occurrence of lung cancer in man. Acta Unio Int. Contra Cancrum 9, 531–541 (1953).
Barnes, D. E. & Yaffe, K. The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol. 10, 819–828 (2011).
Livingston, G. et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396, 413–446 (2020).
Sudlow, C. et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12, e1001779 (2015).
Bycroft, C. et al. The UK Biobank resource with deep phenotyping and genomic data. Nature 562, 203–209 (2018).
Lee, M. et al. Variation in population attributable fraction of dementia associated with potentially modifiable risk factors by race and ethnicity in the US. JAMA Netw. Open 5, e2219672 (2022).
Deng, Z. & Yang, Y. Population attributable fractions of a wide range of peripheral diseases for the burden of dementia. figshare https://doi.org/10.6084/m9.figshare.30634574 (2025).
Acknowledgements
The data acquired from the UK Biobank in this study were under application number 70109. The UK Biobank received ethical approval from the North West Multi-Centre Research Ethics Committee (REC reference 11/NW/0382), and all participants provided written informed consent. The GBD is funded by the Bill & Melinda Gates Foundation. This work was supported by the STI 2030 Major Projects (2022ZD0211603), the National Natural Science Foundation of China (82330099, 82530100), the Key-Area Research and Development Program of Guangdong Province (2023B0303040003) and Science and Technology Program of Guangzhou (2023A03J0708) to Y.T.; the National Natural Science Foundation of China (82473563) and Guangzhou Science and Technology Programme (2024A03J0911) to Y.X.; Guangzhou Science and Technology Plan Project (2025A04J4443) and Sun Yat-sen Clinical Research Cultivating Program (SYS-Q-202208) to H.L.; and the National Natural Science Foundation of China (81872261) to S.X. The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the paper.
Author information
Authors and Affiliations
Contributions
Z.D., Y.Y., Q.L. and S.X. are co-first authors. Z.D., Y.Y., Q.L. and Y.T. designed the study. Z.D., Y.Y., Q.L., S.X., Y.Z. and Y.T. accessed the data, performed the statistical analysis and verified the underlying data reported in the paper. Z.D., Y.Y., Q.L. and Y.T. drafted the initial paper. All authors critically revised the paper for important intellectual content. Y.T. supervised the study. All authors have full access to all of the data in the study and take responsibility to submit for publication. All authors have read and approved the final paper. Y.T. has the final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Human Behaviour thanks Nooshin Abbasi, Christian Razo and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Tables 1–25 and Figs. 1–71.
Supplementary Data 1
The detailed spatial distribution of dementia prevalence and DALYs, as well as the PAF, prevalence rates and case numbers of dementia related to overall and nine classes of peripheral diseases, across GBD regions and countries.
Supplementary Data 2
Details of the characteristics and quality assessment of all the included articles.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Deng, Z., Yang, Y., Lin, Q. et al. Population attributable fractions of a wide range of peripheral diseases for the burden of dementia. Nat Hum Behav (2026). https://doi.org/10.1038/s41562-025-02392-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41562-025-02392-2