Abstract
Anaplastic lymphoma kinase (ALK) is a receptor tyrosine kinase (RTK) that acts as an oncogenic driver in solid and haematological malignancies in both children and adults. Although ALK-expressing (ALK+) tumours show strong initial responses to the series of ALK inhibitors currently available, many patients will develop resistance. In this Review, we discuss recent advances in ALK oncogenic signalling, together with existing and promising new modalities to treat ALK-driven tumours, including currently approved ALK-directed therapies, namely tyrosine kinase inhibitors, and novel approaches such as ALK-specific immune therapies. Although ALK inhibitors have changed the management and clinical history of ALK+ tumours, they are still insufficient to cure most of the patients. Therefore, more effort is needed to further improve outcomes and prevent the tumour resistance, recurrence and metastatic spread that many patients with ALK+ tumours experience. Here, we outline how a multipronged approach directed against ALK and other essential pathways that sustain the persistence of ALK+ tumours, together with potent or specific immunotherapies, could achieve this goal. We envision that the lessons learned from treating ALK+ tumours in the clinic could ultimately accelerate the implementation of innovative combination therapies to treat tumours driven by other tyrosine kinases or oncogenes with similar properties.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
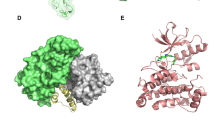
The crystal structures used for Fig. 4 were downloaded from PDB with the following accessions: 3L9P for WT human ALK and neuroblastoma, 2XP2 for crizotinib; 3AOX for alectinib; 6MX8 for brigatinib; 4MKC of ceritinib, 4CLJ for lorlatinib; 9GBE for NVL-655. PyMol session files of the above structures with the in silico mutated residues reported in Fig. 4 are available in the public figshare repository (https://figshare.com/projects/ALK/234473).
References
Hallberg, B. & Palmer, R. H. Mechanistic insight into ALK receptor tyrosine kinase in human cancer biology. Nat. Rev. Cancer 13, 685–700 (2013).
De Munck, S. et al. Structural basis of cytokine-mediated activation of ALK family receptors. Nature 600, 143–147 (2021). With Reshetnyak et al. (ref. 3), this article describes the structure and mechanisms of activation of the ALK receptor.
Reshetnyak, A. V. et al. Mechanism for the activation of the anaplastic lymphoma kinase receptor. Nature 600, 153–157 (2021). With DeMunck et al. (ref. 2), this article describes the structure and mechanism of activation of the ALK receptor.
Blandin, A. F. et al. ALK amplification and rearrangements are recurrent targetable events in congenital and adult glioblastoma. Clin. Cancer Res. 29, 2651–2667 (2023).
Bergaggio, E. et al. ALK inhibitors increase ALK expression and sensitize neuroblastoma cells to ALK.CAR-T cells. Cancer Cell 41, 2100–2116.e2110 (2023). This paper demonstrates the efficacy of the combination of ALK.CAR T cells with lorlatinib in pre-clinical mouse models of neuroblastoma.
Morris, S. W. et al. Fusion of a kinase gene, ALK, to a nucleolar protein gene, NPM, in non-Hodgkin’s lymphoma. Science 263, 1281–1284 (1994). This is the seminal paper that descibes the discovery of the ALK gene as an oncogene in lymphoma.
Soda, M. et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature 448, 561–566 (2007). This paper was the first to demonstrate that ALK fusions can occur outside ALCL and that they can be oncogenic drivers in NSCLC.
Rikova, K. et al. Global survey of phosphotyrosine signaling identifies oncogenic kinases in lung cancer. Cell 131, 1190–1203 (2007).
Chiarle, R., Voena, C., Ambrogio, C., Piva, R. & Inghirami, G. The anaplastic lymphoma kinase in the pathogenesis of cancer. Nat. Rev. Cancer 8, 11–23 (2008).
Mano, H. ALKoma: a cancer subtype with a shared target. Cancer Discov. 2, 495–502 (2012).
Schneider, J. L., Lin, J. J. & Shaw, A. T. ALK-positive lung cancer: a moving target. Nat. Cancer 4, 330–343 (2023).
Kwak, E. L. et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N. Engl. J. Med. 363, 1693–1703 (2010). This seminal paper describes, for the first time, the efficacy of the ALK inhibitor crizotinib in patients with ALK+ NSCLC, opening the path to the development of several generations of ALK TKIs.
Shaw, A. T. et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N. Engl. J. Med. 368, 2385–2394 (2013). This study led to FDA approval of crizotinib as the first ALK TKI for lung cancer treatment.
Gambacorti Passerini, C. et al. Crizotinib in advanced, chemoresistant anaplastic lymphoma kinase-positive lymphoma patients. J. Natl Cancer Inst. 106, djt378 (2014).
Gambacorti-Passerini, C. et al. Long-term effects of crizotinib in ALK-positive tumors (excluding NSCLC): a phase 1b open-label study. Am. J. Hematol. 93, 607–614 (2018).
Gambacorti-Passerini, C., Mussolin, L. & Brugieres, L. Abrupt relapse of ALK-positive lymphoma after discontinuation of crizotinib. N. Engl. J. Med. 374, 95–96 (2016). This works shows that ALK+ lymphoma persister cells survive for many years in patients who are otherwise in complete remission.
Lin, J. J., Riely, G. J. & Shaw, A. T. Targeting ALK: precision medicine takes on drug resistance. Cancer Discov. 7, 137–155 (2017).
Borenas, M. et al. ALK ligand ALKAL2 potentiates MYCN-driven neuroblastoma in the absence of ALK mutation. EMBO J. 40, e105784 (2021).
Cheong, T. C. et al. Mechanistic patterns and clinical implications of oncogenic tyrosine kinase fusions in human cancers. Nat. Commun. 15, 5110 (2024). This work provides experimental evidence and mechanistic insights on the formation and selection of ALK fusions in cancer.
Mathas, S. et al. Gene deregulation and spatial genome reorganization near breakpoints prior to formation of translocations in anaplastic large cell lymphoma. Proc. Natl Acad. Sci. USA 106, 5831–5836 (2009).
Ou, S. I., Zhu, V. W. & Nagasaka, M. Catalog of 5’ fusion partners in ALK-positive NSCLC circa 2020. JTO Clin. Res. Rep. 1, 100015 (2020).
Childress, M. A. et al. ALK fusion partners impact response to ALK inhibition: differential effects on sensitivity, cellular phenotypes, and biochemical properties. Mol. Cancer Res. 16, 1724–1736 (2018).
Armstrong, F. et al. Differential effects of X-ALK fusion proteins on proliferation, transformation, and invasion properties of NIH3T3 cells. Oncogene 23, 6071–6082 (2004).
Lasota, J. et al. Colorectal adenocarcinomas harboring ALK fusion genes: a clinicopathologic and molecular genetic study of 12 cases and review of the literature. Am. J. Surg. Pathol. 44, 1224–1234 (2020).
Yoshida, T. et al. Differential crizotinib response duration among ALK fusion variants in ALK-positive non-small-cell lung cancer. J. Clin. Oncol. 34, 3383–3389 (2016).
Woo, C. G. et al. Differential protein stability and clinical responses of EML4-ALK fusion variants to various ALK inhibitors in advanced ALK-rearranged non-small cell lung cancer. Ann. Oncol. 28, 791–797 (2017).
Lin, J. J. et al. Impact of EML4-ALK variant on resistance mechanisms and clinical outcomes in ALK-positive lung cancer. J. Clin. Oncol. 36, 1199–1206 (2018).
Richards, M. W. et al. Crystal structure of EML1 reveals the basis for Hsp90 dependence of oncogenic EML4-ALK by disruption of an atypical beta-propeller domain. Proc. Natl Acad. Sci. USA 111, 5195–5200 (2014).
Christopoulos, P. et al. EML4-ALK fusion variant V3 is a high-risk feature conferring accelerated metastatic spread, early treatment failure and worse overall survival in ALK+ non-small cell lung cancer. Int. J. Cancer 142, 2589–2598 (2018).
Christopoulos, P. et al. Identification of a highly lethal V3+ TP53+ subset in ALK+ lung adenocarcinoma. Int. J. Cancer 144, 190–199 (2019).
Camidge, D. R. et al. Brigatinib versus crizotinib in ALK inhibitor-naive advanced ALK-positive NSCLC: final results of phase 3 ALTA-1L trial. J. Thorac. Oncol. 16, 2091–2108 (2021).
Penzel, R., Schirmacher, P. & Warth, A. A novel EML4-ALK variant: exon 6 of EML4 fused to exon 19 of ALK. J. Thorac. Oncol. 7, 1198–1199 (2012).
Anai, S. et al. A case of lung adenocarcinoma resistant to crizotinib harboring a novel EML4-ALK variant, exon 6 of EML4 fused to exon 18 of ALK. J. Thorac. Oncol. 11, e126–e128 (2016).
Le, A. T., Varella-Garcia, M. & Doebele, R. C. Oncogenic fusions involving exon 19 of ALK. J. Thorac. Oncol. 7, e44 (2012).
Delsol, G. et al. A new subtype of large B-cell lymphoma expressing the ALK kinase and lacking the 2; 5 translocation. Blood 89, 1483–1490 (1997).
Kemps, P. G. et al. ALK-positive histiocytosis: a new clinicopathologic spectrum highlighting neurologic involvement and responses to ALK inhibition. Blood 139, 256–280 (2022).
Guerreiro Stucklin, A. S. et al. Alterations in ALK/ROS1/NTRK/MET drive a group of infantile hemispheric gliomas. Nat. Commun. 10, 4343 (2019).
Hiwatari, M. et al. Novel TENM3-ALK fusion is an alternate mechanism for ALK activation in neuroblastoma. Oncogene 41, 2789–2797 (2022).
Chiarle, R. et al. NPM-ALK transgenic mice spontaneously develop T-cell lymphomas and plasma cell tumors. Blood 101, 1919–1927 (2003). This is the first paper to demonstarte that the NPM–ALK fusion acts as an oncogenic driver of lymphoma in mouse models.
Kreutmair, S. et al. Existence of reprogrammed lymphoma stem cells in a murine ALCL-like model. Leukemia 34, 3242–3255 (2020).
Soda, M. et al. A mouse model for EML4-ALK-positive lung cancer. Proc. Natl Acad. Sci. USA 105, 19893–19897 (2008).
Voena, C. et al. Efficacy of a cancer vaccine against ALK-rearranged lung tumors. Cancer Immunol. Res. 3, 1333–1343 (2015).
Maddalo, D. et al. In vivo engineering of oncogenic chromosomal rearrangements with the CRISPR/Cas9 system. Nature 516, 423–427 (2014).
Blasco, R. B. et al. Simple and rapid in vivo generation of chromosomal rearrangements using CRISPR/Cas9 technology. Cell Rep. 9, 1219–1227 (2014).
Hallberg, B. & Palmer, R. H. ALK and NSCLC: targeted therapy with ALK inhibitors. F1000 Med. Rep. 3, 21 (2011).
Mosse, Y. P. et al. Identification of ALK as a major familial neuroblastoma predisposition gene. Nature 455, 930–935 (2008). With George et al. (ref. 47), this article demonstrates that ALK mutations are found in familiar and sporadic neuroblastomas and cause a constitutive activation of the ALK receptor.
George, R. E. et al. Activating mutations in ALK provide a therapeutic target in neuroblastoma. Nature 455, 975–978 (2008). With Mosse et al. (ref. 46), this article demonstrates that ALK mutations are found in familiar and sporadic neuroblastomas and cause a constitutive activation of the ALK receptor.
Janoueix-Lerosey, I. et al. Somatic and germline activating mutations of the ALK kinase receptor in neuroblastoma. Nature 455, 967–970 (2008).
Chen, Y. et al. Oncogenic mutations of ALK kinase in neuroblastoma. Nature 455, 971–974 (2008).
Bresler, S. C. et al. ALK mutations confer differential oncogenic activation and sensitivity to ALK inhibition therapy in neuroblastoma. Cancer Cell 26, 682–694 (2014).
Bresler, S. C. et al. Differential inhibitor sensitivity of anaplastic lymphoma kinase variants found in neuroblastoma. Sci. Transl. Med. 3, 108ra114 (2011).
Berry, T. et al. The ALK(F1174L) mutation potentiates the oncogenic activity of MYCN in neuroblastoma. Cancer Cell 22, 117–130 (2012).
Heukamp, L. C. et al. Targeted expression of mutated ALK induces neuroblastoma in transgenic mice. Sci. Transl. Med. 4, 141ra191 (2012).
Zhu, S. et al. Activated ALK collaborates with MYCN in neuroblastoma pathogenesis. Cancer Cell 21, 362–373 (2012).
Javanmardi, N. et al. Analysis of ALK, MYCN, and the ALK ligand ALKAL2 (FAM150B/AUGalpha) in neuroblastoma patient samples with chromosome arm 2p rearrangements. Genes Chromosomes Cancer 59, 50–57 (2020).
Schleiermacher, G. et al. Emergence of new ALK mutations at relapse of neuroblastoma. J. Clin. Oncol. 32, 2727–2734 (2014).
Murugan, A. K. & Xing, M. Anaplastic thyroid cancers harbor novel oncogenic mutations of the ALK gene. Cancer Res. 71, 4403–4411 (2011).
Ohshima, K. et al. Integrated analysis of gene expression and copy number identified potential cancer driver genes with amplification-dependent overexpression in 1,454 solid tumors. Sci. Rep. 7, 641 (2017).
Caren, H., Abel, F., Kogner, P. & Martinsson, T. High incidence of DNA mutations and gene amplifications of the ALK gene in advanced sporadic neuroblastoma tumours. Biochem. J. 416, 153–159 (2008).
Pillay, K., Govender, D. & Chetty, R. ALK protein expression in rhabdomyosarcomas. Histopathology 41, 461–467 (2002).
van Gaal, J. C. et al. Anaplastic lymphoma kinase aberrations in rhabdomyosarcoma: clinical and prognostic implications. J. Clin. Oncol. 30, 308–315 (2012).
Wiesner, T. et al. Alternative transcription initiation leads to expression of a novel ALK isoform in cancer. Nature 526, 453–457 (2015).
Inam, H. et al. Genomic and experimental evidence that ALK(ATI) does not predict single agent sensitivity to ALK inhibitors. iScience 24, 103343 (2021).
Couts, K. L. et al. ALK inhibitor response in melanomas expressing EML4-ALK fusions and alternate ALK isoforms. Mol. Cancer Ther. 17, 222–231 (2018).
Hrustanovic, G. et al. RAS-MAPK dependence underlies a rational polytherapy strategy in EML4-ALK-positive lung cancer. Nat. Med. 21, 1038–1047 (2015).
Tulpule, A. et al. Kinase-mediated RAS signaling via membraneless cytoplasmic protein granules. Cell 184, 2649–2664.e2618 (2021). This work shows new modalities by which EML4–ALK fusion can activate downstrean signalling including the MAPK pathway in NSCLC.
Menotti, M. et al. Wiskott-Aldrich syndrome protein (WASP) is a tumor suppressor in T cell lymphoma. Nat. Med. 25, 130–140 (2019).
Umapathy, G. et al. The kinase ALK stimulates the kinase ERK5 to promote the expression of the oncogene MYCN in neuroblastoma. Sci. Signal. 7, ra102 (2014).
Eleveld, T. F. et al. Relapsed neuroblastomas show frequent RAS-MAPK pathway mutations. Nat. Genet. 47, 864–871 (2015).
Zamo, A. et al. Anaplastic lymphoma kinase (ALK) activates Stat3 and protects hematopoietic cells from cell death. Oncogene 21, 1038–1047 (2002).
Chiarle, R. et al. Stat3 is required for ALK-mediated lymphomagenesis and provides a possible therapeutic target. Nat. Med. 11, 623–629 (2005). This work reaveals the crucial importance of the JAK–STAT3 pathway in ALK+ ALCL.
Werner, M. T., Zhao, C., Zhang, Q. & Wasik, M. A. Nucleophosmin-anaplastic lymphoma kinase: the ultimate oncogene and therapeutic target. Blood 129, 823–831 (2017).
Ambrogio, C. et al. NPM-ALK oncogenic tyrosine kinase controls T-cell identity by transcriptional regulation and epigenetic silencing in lymphoma cells. Cancer Res. 69, 8611–8619 (2009).
Piva, R. et al. Gene expression profiling uncovers molecular classifiers for the recognition of anaplastic large-cell lymphoma within peripheral T-cell neoplasms. J. Clin. Oncol. 28, 1583–1590 (2010).
Amin, H. M. et al. Selective inhibition of STAT3 induces apoptosis and G(1) cell cycle arrest in ALK-positive anaplastic large cell lymphoma. Oncogene 23, 5426–5434 (2004).
Bai, L. et al. A potent and selective small-molecule degrader of STAT3 achieves complete tumor regression in vivo. Cancer Cell 36, 498–511.e417 (2019).
Garces de Los Fayos Alonso, I. et al. PDGFRbeta promotes oncogenic progression via STAT3/STAT5 hyperactivation in anaplastic large cell lymphoma. Mol. Cancer 21, 172 (2022).
Zhang, J. P. et al. A novel model of controlling PD-L1 expression in ALK+ anaplastic large cell lymphoma revealed by CRISPR screening. Blood 134, 171–185 (2019).
Liang, H. C. et al. Super-enhancer-based identification of a BATF3/IL-2R-module reveals vulnerabilities in anaplastic large cell lymphoma. Nat. Commun. 12, 5577 (2021).
Wu, C. et al. STAT1 is phosphorylated and downregulated by the oncogenic tyrosine kinase NPM-ALK in ALK-positive anaplastic large-cell lymphoma. Blood 126, 336–345 (2015).
Rajan, S. S. et al. The mechanism of cancer drug addiction in ALK-positive T-cell lymphoma. Oncogene 39, 2103–2117 (2020).
Takezawa, K., Okamoto, I., Nishio, K., Janne, P. A. & Nakagawa, K. Role of ERK-BIM and STAT3-survivin signaling pathways in ALK inhibitor-induced apoptosis in EML4-ALK-positive lung cancer. Clin. Cancer Res. 17, 2140–2148 (2011).
Slupianek, A. et al. Role of phosphatidylinositol 3-kinase-Akt pathway in nucleophosmin/anaplastic lymphoma kinase-mediated lymphomagenesis. Cancer Res. 61, 2194–2199 (2001).
Mastini, C. et al. Targeting CCR7-PI3Kgamma overcomes resistance to tyrosine kinase inhibitors in ALK-rearranged lymphoma. Sci. Transl. Med. 15, eabo3826 (2023).
Sampson, J., Richards, M. W., Choi, J., Fry, A. M. & Bayliss, R. Phase-separated foci of EML4-ALK facilitate signalling and depend upon an active kinase conformation. EMBO Rep. 22, e53693 (2021).
Dardaei, L. et al. SHP2 inhibition restores sensitivity in ALK-rearranged non-small-cell lung cancer resistant to ALK inhibitors. Nat. Med. 24, 512–517 (2018).
Ota, K. et al. Induction of PD-L1 expression by the EML4-ALK oncoprotein and downstream signaling pathways in non-small cell lung cancer. Clin. Cancer Res. 21, 4014–4021 (2015).
Li, J. et al. Tumour-derived substrate-adherent cells promote neuroblastoma survival through secreted trophic factors. Mol. Oncol. 15, 2011–2025 (2021).
Claeys, S. et al. ALK positively regulates MYCN activity through repression of HBP1 expression. Oncogene 38, 2690–2705 (2019).
Hassler, M. R. et al. Insights into the pathogenesis of anaplastic large-cell lymphoma through genome-wide DNA methylation profiling. Cell Rep. 17, 596–608 (2016).
Pawlicki, J. M. et al. NPM-ALK-induced reprogramming of mature TCR-stimulated T cells results in dedifferentiation and malignant transformation. Cancer Res. 81, 3241–3254 (2021).
Turner, S. D., Yeung, D., Hadfield, K., Cook, S. J. & Alexander, D. R. The NPM-ALK tyrosine kinase mimics TCR signalling pathways, inducing NFAT and AP-1 by RAS-dependent mechanisms. Cell Signal. 19, 740–747 (2007).
Ambrogio, C. et al. The anaplastic lymphoma kinase controls cell shape and growth of anaplastic large cell lymphoma through Cdc42 activation. Cancer Res. 68, 8899–8907 (2008).
Choudhari, R. et al. Redundant and nonredundant roles for Cdc42 and Rac1 in lymphomas developed in NPM-ALK transgenic mice. Blood 127, 1297–1306 (2016).
Colomba, A. et al. Activation of Rac1 and the exchange factor Vav3 are involved in NPM-ALK signaling in anaplastic large cell lymphomas. Oncogene 27, 2728–2736 (2008).
Younes, A. et al. Brentuximab vedotin (SGN-35) for relapsed CD30-positive lymphomas. N. Engl. J. Med. 363, 1812–1821 (2010).
Garcia-Bermudez, J. et al. Squalene accumulation in cholesterol auxotrophic lymphomas prevents oxidative cell death. Nature 567, 118–122 (2019).
Zhang, Q. et al. Chimeric kinase ALK induces expression of NAMPT and selectively depends on this metabolic enzyme to sustain its own oncogenic function. Leukemia 37, 2436–2447 (2023).
Prutsch, N. et al. STAT3 couples activated tyrosine kinase signaling to the oncogenic core transcriptional regulatory circuitry of anaplastic large cell lymphoma. Cell Rep. Med. 5, 101472 (2024).
Schiefer, A. I., Vesely, P., Hassler, M. R., Egger, G. & Kenner, L. The role of AP-1 and epigenetics in ALCL. Front. Biosci. 7, 226–235 (2015).
Atsaves, V. et al. Constitutive control of AKT1 gene expression by JUNB/CJUN in ALK+ anaplastic large-cell lymphoma: a novel crosstalk mechanism. Leukemia 29, 2162–2172 (2015).
Borenas, M. et al. ALK signaling primes the DNA damage response sensitizing ALK-driven neuroblastoma to therapeutic ATR inhibition. Proc. Natl Acad. Sci. USA 121, e2315242121 (2024).
Martinengo, C. et al. ALK-dependent control of hypoxia inducible factors mediates tumor growth and metastasis. Cancer Res 74, 6094–6106 (2014).
Voena, C. et al. Oncogenic ALK regulates EMT in non-small cell lung carcinoma through repression of the epithelial splicing regulatory protein 1. Oncotarget 7, 33316–33330 (2016).
Pashley, S. L. et al. The mesenchymal morphology of cells expressing the EML4-ALK V3 oncogene is dependent on phosphorylation of Eg5 by NEK7. J. Biol. Chem. 300, 107144 (2024).
Moog-Lutz, C. et al. Activation and inhibition of anaplastic lymphoma kinase receptor tyrosine kinase by monoclonal antibodies and absence of agonist activity of pleiotrophin. J. Biol. Chem. 280, 26039–26048 (2005).
Riera, L. et al. Involvement of Grb2 adaptor protein in nucleophosmin-anaplastic lymphoma kinase (NPM-ALK)-mediated signaling and anaplastic large cell lymphoma growth. J. Biol. Chem. 285, 26441–26450 (2010).
Ceccon, M. et al. Excess of NPM-ALK oncogenic signaling promotes cellular apoptosis and drug dependency. Oncogene 35, 3854–3865 (2016). With Amin et al. (ref. 109), this article demonstrates that NPM–ALK fusion signalling in lymphoma causes oncogene addiction and oncogenic stress.
Amin, A. D. et al. Evidence suggesting that discontinuous dosing of ALK kinase inhibitors may prolong control of ALK+ tumors. Cancer Res 75, 2916–2927 (2015). With Ceccon et al. (ref. 108), this article demonstrates that NPM–ALK fusion signalling in lymphoma causes oncogene addiction and oncogenic stress.
Karaca Atabay, E. et al. Tyrosine phosphatases regulate resistance to ALK inhibitors in ALK+ anaplastic large cell lymphoma. Blood 139, 717–731 (2022).
Honorat, J. F., Ragab, A., Lamant, L., Delsol, G. & Ragab-Thomas, J. SHP1 tyrosine phosphatase negatively regulates NPM-ALK tyrosine kinase signaling. Blood 107, 4130–4138 (2006).
Han, Y. et al. Loss of SHP1 enhances JAK3/STAT3 signaling and decreases proteosome degradation of JAK3 and NPM-ALK in ALK+ anaplastic large-cell lymphoma. Blood 108, 2796–2803 (2006).
Han, Y. et al. Restoration of shp1 expression by 5-AZA-2′-deoxycytidine is associated with downregulation of JAK3/STAT3 signaling in ALK-positive anaplastic large cell lymphoma. Leukemia 20, 1602–1609 (2006).
Ng, S. Y. et al. Targetable vulnerabilities in T- and NK-cell lymphomas identified through preclinical models. Nat. Commun. 9, 2024 (2018).
Baumgartner, C. K. et al. The PTPN2/PTPN1 inhibitor ABBV-CLS-484 unleashes potent anti-tumour immunity. Nature 622, 850–862 (2023).
Sodir, N. M. et al. SHP2: a pleiotropic target at the interface of cancer and its microenvironment. Cancer Discov. 13, 2339–2355 (2023).
Boutterin, M. C. et al. Control of ALK (wild type and mutated forms) phosphorylation: specific role of the phosphatase PTP1B. Cell Signal. 25, 1505–1513 (2013).
Voena, C. et al. The tyrosine phosphatase Shp2 interacts with NPM-ALK and regulates anaplastic lymphoma cell growth and migration. Cancer Res. 67, 4278–4286 (2007).
Valencia-Sama, I. et al. SHP2 inhibition with TNO155 increases efficacy and overcomes resistance of ALK inhibitors in neuroblastoma. Cancer Res. Commun. 3, 2608–2622 (2023).
Mura, G. et al. Regulation of CD45 phosphatase by oncogenic ALK in anaplastic large cell lymphoma. Front. Oncol. 12, 1085672 (2022).
Malcolm, T. I. et al. Anaplastic large cell lymphoma arises in thymocytes and requires transient TCR expression for thymic egress. Nat. Commun. 7, 10087 (2016).
Kielbowski, K., Zychowska, J. & Becht, R. Anaplastic lymphoma kinase inhibitors—a review of anticancer properties, clinical efficacy, and resistance mechanisms. Front. Pharmacol. 14, 1285374 (2023).
Zou, H. Y. et al. An orally available small-molecule inhibitor of c-Met, PF-2341066, exhibits cytoreductive antitumor efficacy through antiproliferative and antiangiogenic mechanisms. Cancer Res. 67, 4408–4417 (2007).
Mosse, Y. P. et al. Targeting ALK with crizotinib in pediatric anaplastic large cell lymphoma and inflammatory myofibroblastic tumor: a Children’s Oncology Group Study. J. Clin. Oncol. 35, 3215–3221 (2017).
Mosse, Y. P. et al. Safety and activity of crizotinib for paediatric patients with refractory solid tumours or anaplastic large-cell lymphoma: a Children’s Oncology Group phase 1 consortium study. Lancet Oncol. 14, 472–480 (2013).
Pearson, A. D. J. et al. Second Paediatric Strategy Forum for anaplastic lymphoma kinase (ALK) inhibition in paediatric malignancies: ACCELERATE in collaboration with the European Medicines Agency with the participation of the Food and Drug Administration. Eur. J. Cancer 157, 198–213 (2021).
Butrynski, J. E. et al. Crizotinib in ALK-rearranged inflammatory myofibroblastic tumor. N. Engl. J. Med. 363, 1727–1733 (2010). With Bossi et al. (ref. 129), this article shows the potent antitumour activity of the ALK TKI crisotinib in other tumours such as ALK+ IMT and in ALK+ ALCL.
Gambacorti-Passerini, C., Messa, C. & Pogliani, E. M. Crizotinib in anaplastic large-cell lymphoma. N. Engl. J. Med. 364, 775–776 (2011).
Bossi, E. et al. Phase two study of crizotinib in patients with anaplastic lymphoma kinase (ALK)-positive anaplastic large cell lymphoma relapsed/refractory to chemotherapy. Am. J. Hematol. 95, E319–E321 (2020). With Butrynski et al. (ref. 127), this article shows the potent antitumour activity of the ALK TKI crisotinib in other tumours such as ALK+ IMT and in ALK+ ALCL.
Rindone, G. et al. A monocentric analysis of the long-term safety and efficacy of crizotinib in relapsed/refractory ALK+ lymphomas. Blood Adv. 7, 314–316 (2023).
Brugieres, L. et al. Efficacy and safety of crizotinib in ALK-positive systemic anaplastic large-cell lymphoma in children, adolescents, and adult patients: results of the French AcSe-crizotinib trial. Eur. J. Cancer 191, 112984 (2023).
Foster, J. H. et al. Activity of crizotinib in patients with ALK-aberrant relapsed/refractory neuroblastoma: a Children’s Oncology Group Study (ADVL0912). Clin. Cancer Res. 27, 3543–3548 (2021).
Doebele, R. C. et al. Mechanisms of resistance to crizotinib in patients with ALK gene rearranged non-small cell lung cancer. Clin. Cancer Res. 18, 1472–1482 (2012).
Chun, S. G., Choe, K. S., Iyengar, P., Yordy, J. S. & Timmerman, R. D. Isolated central nervous system progression on crizotinib: an Achilles heel of non-small cell lung cancer with EML4-ALK translocation? Cancer Biol. Ther. 13, 1376–1383 (2012).
Peters, S. et al. Alectinib versus crizotinib in untreated ALK-positive non-small-cell lung cancer. N. Engl. J. Med. 377, 829–838 (2017). This work led to the approval of alectinib as a a first-line treatment for ALK+ NSCLC.
Camidge, D. R. et al. Brigatinib versus crizotinib in ALK-positive non-small-cell lung cancer. N. Engl. J. Med. 379, 2027–2039 (2018).
Shaw, A. T. et al. Ceritinib in ALK-rearranged non-small-cell lung cancer. N. Engl. J. Med. 370, 1189–1197 (2014).
Shaw, A. T. et al. Ceritinib versus chemotherapy in patients with ALK-rearranged non-small-cell lung cancer previously given chemotherapy and crizotinib (ASCEND-5): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 18, 874–886 (2017).
Gadgeel, S. et al. Alectinib versus crizotinib in treatment-naive anaplastic lymphoma kinase-positive (ALK+) non-small-cell lung cancer: CNS efficacy results from the ALEX study. Ann. Oncol. 29, 2214–2222 (2018).
Sakamoto, H. et al. CH5424802, a selective ALK inhibitor capable of blocking the resistant gatekeeper mutant. Cancer Cell 19, 679–690 (2011).
Horn, L. et al. Ensartinib vs crizotinib for patients with anaplastic lymphoma kinase-positive non-small cell lung cancer: a randomized clinical trial. JAMA Oncol. 7, 1617–1625 (2021).
Gadgeel, S. M. et al. Safety and activity of alectinib against systemic disease and brain metastases in patients with crizotinib-resistant ALK-rearranged non-small-cell lung cancer (AF-002JG): results from the dose-finding portion of a phase 1/2 study. Lancet Oncol. 15, 1119–1128 (2014).
Fischer, M. et al. Ceritinib in paediatric patients with anaplastic lymphoma kinase-positive malignancies: an open-label, multicentre, phase 1, dose-escalation and dose-expansion study. Lancet Oncol. 22, 1764–1776 (2021).
Veleanu, L., Lamant, L. & Sibon, D. Brigatinib in ALK-positive ALCL after failure of brentuximab vedotin. N. Engl. J. Med. 390, 2129–2130 (2024).
Johnson, T. W. et al. Discovery of (10R)-7-amino-12-fluoro-2,10,16-trimethyl-15-oxo-10,15,16,17-tetrahydro-2H-8,4-(metheno)pyrazolo[4,3-h][2,5,11]-benzoxadiazacyclotetradecine-3-carbonitrile (PF-06463922), a macrocyclic inhibitor of anaplastic lymphoma kinase (ALK) and c-ros oncogene 1 (ROS1) with preclinical brain exposure and broad-spectrum potency against ALK-resistant mutations. J. Med. Chem. 57, 4720–4744 (2014).
Gainor, J. F. et al. Molecular mechanisms of resistance to first- and second-generation ALK inhibitors in ALK-rearranged lung cancer. Cancer Discov. 6, 1118–1133 (2016).
Shaw, A. T. et al. First-line lorlatinib or crizotinib in advanced ALK-positive lung cancer. N. Engl. J. Med. 383, 2018–2029 (2020).
Camidge, D. R. Lorlatinib should not be considered as the preferred first-line option in patients with advanced ALK rearranged NSCLC. J. Thorac. Oncol. 16, 528–531 (2021).
Fukano, R. et al. Alectinib for relapsed or refractory anaplastic lymphoma kinase-positive anaplastic large cell lymphoma: an open-label phase II trial. Cancer Sci. 111, 4540–4547 (2020).
Wang, Q. A., Chen, H. W., Wu, R. C. & Wu, C. E. Update of diagnosis and targeted therapy for ALK+ inflammation myofibroblastic tumor. Curr. Treat. Options Oncol. 24, 1683–1702 (2023).
Infarinato, N. R. et al. The ALK/ROS1 inhibitor PF-06463922 overcomes primary resistance to crizotinib in ALK-driven neuroblastoma. Cancer Discov. 6, 96–107 (2016).
Goldsmith, K. C. et al. Lorlatinib with or without chemotherapy in ALK-driven refractory/relapsed neuroblastoma: phase 1 trial results. Nat. Med. 29, 1092–1102 (2023). This study shows the efficacy of the ALK TKI lorlatinib in patients with neuroblastoma carrying ALK genetic alterations.
Shiba-Ishii, A. et al. Analysis of lorlatinib analogs reveals a roadmap for targeting diverse compound resistance mutations in ALK-positive lung cancer. Nat. Cancer 3, 710–722 (2022).
Soumerai, J. D. et al. Next-generation ALK inhibitors are highly active in ALK-positive large B-cell lymphoma. Blood 140, 1822–1826 (2022).
Zhu, L., Ma, S. & Xia, B. Remarkable response to alectinib for metastatic papillary thyroid cancer with STRN-ALK fusion: a case report. Front. Oncol. 12, 1009076 (2022).
Bagchi, A. et al. Lorlatinib in a child with ALK-fusion-positive high-grade glioma. N. Engl. J. Med. 385, 761–763 (2021).
Ou, S. I., Nagasaka, M., Brazel, D., Hou, Y. & Zhu, V. W. Will the clinical development of 4th-generation “double mutant active” ALK TKIs (TPX-0131 and NVL-655) change the future treatment paradigm of ALK+ NSCLC? Transl. Oncol. 14, 101191 (2021).
Murray, B. W. et al. TPX-0131, a potent CNS-penetrant, next-generation inhibitor of wild-type ALK and ALK-resistant mutations. Mol. Cancer Ther. 20, 1499–1507 (2021).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT04849273 (2023).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT05384626 (2024).
Lin, J. J. et al. NVL-655 is a selective and brain-penetrant inhibitor of diverse ALK-mutant oncoproteins, including lorlatinib-resistant compound mutations. Cancer Discov. 14, 2367–2386 (2024). This work shows the efficacy of the fourth-generation ALK TKI NVL-655 in patients that failed previous ALK TKIs.
Mizuta, H. et al. Gilteritinib overcomes lorlatinib resistance in ALK-rearranged cancer. Nat. Commun. 12, 1261 (2021).
Ando, C. et al. Efficacy of gilteritinib in comparison with alectinib for the treatment of ALK-rearranged non-small cell lung cancer. Cancer Sci. 114, 4343–4354 (2023).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT06225427 (2024).
Drilon, A. et al. Safety and antitumor activity of the multitargeted Pan-TRK, ROS1, and ALK inhibitor entrectinib: combined results from two phase I trials (ALKA-372-001 and STARTRK-1). Cancer Discov. 7, 400–409 (2017).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT02568267 (2025).
Treis, D. et al. Sustained response to entrectinib in an infant with a germline ALKAL2 variant and refractory metastatic neuroblastoma with chromosomal 2p gain and anaplastic lymphoma kinase and tropomyosin receptor kinase activation. JCO Precis. Oncol. 6, e2100271 (2022).
Keam, S. J. Iruplinalkib: first approval. Drugs 83, 1717–1721 (2023).
Yang, Y. et al. Envonalkib versus crizotinib for treatment-naive ALK-positive non-small cell lung cancer: a randomized, multicenter, open-label, phase III trial. Signal Transduct. Target. Ther. 8, 301 (2023).
Boike, L., Henning, N. J. & Nomura, D. K. Advances in covalent drug discovery. Nat. Rev. Drug Discov. 21, 881–898 (2022).
Schneider, M. et al. The PROTACtable genome. Nat. Rev. Drug Discov. 20, 789–797 (2021).
Bekes, M., Langley, D. R. & Crews, C. M. PROTAC targeted protein degraders: the past is prologue. Nat. Rev. Drug Discov. 21, 181–200 (2022).
Yan, G. et al. Targeting cysteine located outside the active site: an effective strategy for covalent ALKi design. J. Med. Chem. 64, 1558–1569 (2021).
Powell, C. E. et al. Chemically induced degradation of anaplastic lymphoma kinase (ALK). J. Med. Chem. 61, 4249–4255 (2018).
Sun, N. et al. Development of a Brigatinib degrader (SIAIS117) as a potential treatment for ALK positive cancer resistance. Eur. J. Med. Chem. 193, 112190 (2020).
Gao, Y. et al. Catalytic degraders effectively address kinase site mutations in EML4-ALK oncogenic fusions. J. Med. Chem. 66, 5524–5535 (2023).
Chang, L. et al. Systematic profiling of conditional pathway activation identifies context-dependent synthetic lethalities. Nat. Genet. 55, 1709–1720 (2023).
Ceccon, M. et al. Mitochondrial hyperactivation and enhanced ROS production are involved in toxicity induced by oncogenic kinases over-signaling. Cancers 10, 509 (2018).
Lin, J. J., Gainor, J. F., Lam, V. K. & Lovly, C. M. Unlocking the next frontier in precision oncology: addressing drug-tolerant residual disease. Cancer Discov. 14, 915–919 (2024).
Waliany, S. et al. P1.12B.02 Mechanisms of resistance to first-line vs later-line alectinib in ALK fusion-positive non-small cell lung cancer. J. Thorac. Oncol. 19 (Suppl. 10), S199–S200 (2024).
Yoda, S. et al. Sequential ALK inhibitors can select for lorlatinib-resistant compound ALK mutations in ALK-positive lung cancer. Cancer Discov. 8, 714–729 (2018).
Solomon, B. J. et al. Lorlatinib versus crizotinib in patients with advanced ALK-positive non-small cell lung cancer: 5-year outcomes from the phase III CROWN study. J. Clin. Oncol. 42, 3400–3409 (2024).
Dagogo-Jack, I. et al. Treatment with next-generation ALK inhibitors fuels plasma ALK mutation diversity. Clin. Cancer Res. 25, 6662–6670 (2019).
Choi, Y. L. et al. EML4-ALK mutations in lung cancer that confer resistance to ALK inhibitors. N. Engl. J. Med. 363, 1734–1739 (2010). This seminal paper shows that mutations affecting the ALK kinase domain are frequent mechanisms of resistance to ALK TKIs.
Berko, E. R. et al. Circulating tumor DNA reveals mechanisms of lorlatinib resistance in patients with relapsed/refractory ALK-driven neuroblastoma. Nat. Commun. 14, 2601 (2023).
Desai, A. & Lovly, C. M. Strategies to overcome resistance to ALK inhibitors in non-small cell lung cancer: a narrative review. Transl. Lung Cancer Res. 12, 615–628 (2023).
Dagogo-Jack, I. et al. MET alterations are a recurring and actionable resistance mechanism in ALK-positive lung cancer. Clin. Cancer Res. 26, 2535–2545 (2020).
Katayama, R. et al. Mechanisms of acquired crizotinib resistance in ALK-rearranged lung cancers. Sci. Transl. Med. 4, 120ra117 (2012).
Lovly, C. M. et al. Rationale for co-targeting IGF-1R and ALK in ALK fusion-positive lung cancer. Nat. Med. 20, 1027–1034 (2014).
Tanizaki, J. et al. Activation of HER family signaling as a mechanism of acquired resistance to ALK inhibitors in EML4-ALK-positive non-small cell lung cancer. Clin. Cancer Res. 18, 6219–6226 (2012).
Voena, C. et al. The EGFR family members sustain the neoplastic phenotype of ALK+ lung adenocarcinoma via EGR1. Oncogenesis 2, e43 (2013).
Lee, H. J. et al. Drug resistance via feedback activation of Stat3 in oncogene-addicted cancer cells. Cancer Cell 26, 207–221 (2014).
Cooper, A. J., Sequist, L. V. & Lin, J. J. Third-generation EGFR and ALK inhibitors: mechanisms of resistance and management. Nat. Rev. Clin. Oncol. 19, 499–514 (2022).
Isozaki, H. et al. Non-small cell lung cancer cells acquire resistance to the ALK inhibitor alectinib by activating alternative receptor tyrosine kinases. Cancer Res. 76, 1506–1516 (2016).
Crystal, A. S. et al. Patient-derived models of acquired resistance can identify effective drug combinations for cancer. Science 346, 1480–1486 (2014).
Horn, L. et al. Monitoring therapeutic response and resistance: analysis of circulating tumor DNA in patients with ALK+ lung cancer. J. Thorac. Oncol. 14, 1901–1911 (2019).
Recondo, G. et al. Diverse resistance mechanisms to the third-generation ALK inhibitor lorlatinib in ALK-rearranged lung cancer. Clin. Cancer Res. 26, 242–255 (2020).
Yun, M. R. et al. Targeting YAP to overcome acquired resistance to ALK inhibitors in ALK-rearranged lung cancer. EMBO Mol. Med. 11, e10581 (2019).
Haderk, F. et al. Focal adhesion kinase-YAP signaling axis drives drug-tolerant persister cells and residual disease in lung cancer. Nat. Commun. 15, 3741 (2024).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT04292119 (2021).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT03202940 (2024).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT04005144 (2022).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT04800822 (2024).
Drilon, A. et al. SHP2 inhibition sensitizes diverse oncogene-addicted solid tumors to re-treatment with targeted therapy. Cancer Discov. 13, 1789–1801 (2023).
Ek, T. et al. Long-lasting response to lorlatinib in patients with ALK-driven relapsed or refractory neuroblastoma monitored with circulating tumor DNA analysis. Cancer Res. Commun. 4, 2553–2564 (2024).
Prokoph, N. et al. IL10RA modulates crizotinib sensitivity in NPM1-ALK+ anaplastic large cell lymphoma. Blood 136, 1657–1669 (2020).
Laimer, D. et al. PDGFR blockade is a rational and effective therapy for NPM-ALK-driven lymphomas. Nat. Med. 18, 1699–1704 (2012).
Levacq, D., D’Haene, N., de Wind, R., Remmelink, M. & Berghmans, T. Histological transformation of ALK rearranged adenocarcinoma into small cell lung cancer: a new mechanism of resistance to ALK inhibitors. Lung Cancer 102, 38–41 (2016).
Takegawa, N. et al. Transformation of ALK rearrangement-positive adenocarcinoma to small-cell lung cancer in association with acquired resistance to alectinib. Ann. Oncol. 27, 953–955 (2016).
Kaiho, T., Nakajima, T., Iwasawa, S., Yonemori, Y. & Yoshino, I. ALK rearrangement adenocarcinoma with histological transformation to squamous cell carcinoma resistant to alectinib and ceritinib. Onco Targets Ther. 13, 1557–1560 (2020).
Koyama, K. et al. Overexpression of CD 133 and BCL-2 in non-small cell lung cancer with neuroendocrine differentiation after transformation in ALK rearrangement-positive adenocarcinoma. Pathol. Int. 69, 294–299 (2019).
Siaw, J. T. et al. 11q Deletion or ALK activity curbs DLG2 expression to maintain an undifferentiated state in neuroblastoma. Cell Rep. 32, 108171 (2020).
Fukuda, K. et al. Epithelial-to-mesenchymal transition is a mechanism of ALK inhibitor resistance in lung cancer independent of ALK mutation status. Cancer Res. 79, 1658–1670 (2019).
Meads, M. B., Gatenby, R. A. & Dalton, W. S. Environment-mediated drug resistance: a major contributor to minimal residual disease. Nat. Rev. Cancer 9, 665–674 (2009).
Yamada, T. et al. Paracrine receptor activation by microenvironment triggers bypass survival signals and ALK inhibitor resistance in EML4-ALK lung cancer cells. Clin. Cancer Res. 18, 3592–3602 (2012).
Hu, H. et al. Three subtypes of lung cancer fibroblasts define distinct therapeutic paradigms. Cancer Cell 39, 1531–1547.e1510 (2021).
Desai, B. et al. Peristromal niches protect lung cancers from targeted therapies through a combined effect of multiple molecular mediators. Preprint at bioRxiv https://doi.org/10.1101/2024.04.24.590626 (2024).
Chuang, T. P. et al. ALK fusion NSCLC oncogenes promote survival and inhibit NK cell responses via SERPINB4 expression. Proc. Natl Acad. Sci. USA 120, e2216479120 (2023).
Gainor, J. F. et al. ALK rearrangements are mutually exclusive with mutations in EGFR or KRAS: an analysis of 1,683 patients with non-small cell lung cancer. Clin. Cancer Res. 19, 4273–4281 (2013).
Awad, M. M. et al. Acquired resistance to KRAS(G12C) inhibition in cancer. N. Engl. J. Med. 384, 2382–2393 (2021).
Offin, M. et al. Acquired ALK and RET gene fusions as mechanisms of resistance to osimertinib in EGFR-mutant lung cancers. JCO Precis. Oncol. 2, PO.18.00126 (2018).
Hebart, H., Lang, P. & Woessmann, W. Nivolumab for refractory anaplastic large cell lymphoma: a case report. Ann. Intern. Med. 165, 607–608 (2016).
Rigaud, C. et al. Efficacy of nivolumab in a patient with systemic refractory ALK+ anaplastic large cell lymphoma. Pediatr. blood Cancer 65, e26902 (2018).
Gainor, J. F. et al. EGFR mutations and ALK rearrangements are associated with low response rates to PD-1 pathway blockade in non-small cell lung cancer: a retrospective analysis. Clin. Cancer Res. 22, 4585–4593 (2016).
Spigel, D. R. et al. Phase 1/2 study of the safety and tolerability of nivolumab plus crizotinib for the first-line treatment of anaplastic lymphoma kinase translocation—positive advanced non-small cell lung cancer (CheckMate 370). J. Thorac. Oncol. 13, 682–688 (2018).
Mastini, C., Martinengo, C., Inghirami, G. & Chiarle, R. Anaplastic lymphoma kinase: an oncogene for tumor vaccination. J. Mol. Med. 87, 669–677 (2009).
Ait-Tahar, K. et al. Correlation of the autoantibody response to the ALK oncoantigen in pediatric anaplastic lymphoma kinase-positive anaplastic large cell lymphoma with tumor dissemination and relapse risk. Blood 115, 3314–3319 (2010). This paper shows the prognostic impact of spontaneous immune responses to the ALK antigen in patients with ALK+ ALCL.
Passoni, L. et al. In vivo T-cell immune response against anaplastic lymphoma kinase in patients with anaplastic large cell lymphomas. Haematologica 91, 48–55 (2006).
Mota, I. et al. ALK peptide vaccination restores the immunogenicity of ALK-rearranged non-small cell lung cancer. Nat. Cancer 4, 1016–1035 (2023). This paper identifies ALK peptides that are immunogenic in mice and humans.
Awad, M. M. et al. Epitope mapping of spontaneous autoantibodies to anaplastic lymphoma kinase (ALK) in non-small cell lung cancer. Oncotarget 8, 92265–92274 (2017).
Cheever, M. A. et al. The prioritization of cancer antigens: a national cancer institute pilot project for the acceleration of translational research. Clin. Cancer Res. 15, 5323–5337 (2009).
Chiarle, R. et al. The anaplastic lymphoma kinase is an effective oncoantigen for lymphoma vaccination. Nat. Med. 14, 676–680 (2008).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT05950139 (2024).
Carpenter, E. L. et al. Antibody targeting of anaplastic lymphoma kinase induces cytotoxicity of human neuroblastoma. Oncogene 31, 4859–4867 (2012).
Sano, R. et al. An antibody-drug conjugate directed to the ALK receptor demonstrates efficacy in preclinical models of neuroblastoma. Sci. Transl. Med. 11, eaau9732 (2019).
Li, T. et al. Structural basis for ligand reception by anaplastic lymphoma kinase. Nature 600, 148–152 (2021).
Walker, A. J. et al. Tumor antigen and receptor densities regulate efficacy of a chimeric antigen receptor targeting anaplastic lymphoma kinase. Mol. Ther. 25, 2189–2201 (2017).
Mazot, P. et al. The constitutive activity of the ALK mutated at positions F1174 or R1275 impairs receptor trafficking. Oncogene 30, 2017–2025 (2011).
US National Library of Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/study/NCT06803875 (2025).
Mecca, C. et al. Discovery of ALK-specific TCR clonotypes for the development of TCR-T cell therapies against ALK-positive cancers. Cancer Res. 84, 21 (2024).
Stadler, S. et al. Endogenous CD4 T cells that recognize ALK and the NPM1::ALK fusion protein can be expanded from human peripheral blood. Cancer Immunologist. Res. https://doi.org/10.1158/2326-6066.CIR-24-0445 (2025).
Solomon, B. J. et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N. Engl. J. Med. 371, 2167–2177 (2014).
Awad, M. M. & Shaw, A. T. ALK inhibitors in non-small cell lung cancer: crizotinib and beyond. Clin. Adv. Hematol. Oncol. 12, 429–439 (2014).
Schoffski, P. et al. Long-term efficacy update of crizotinib in patients with advanced, inoperable inflammatory myofibroblastic tumour from EORTC trial 90101 CREATE. Eur. J. Cancer 156, 12–23 (2021).
Soria, J. C. et al. First-line ceritinib versus platinum-based chemotherapy in advanced ALK-rearranged non-small-cell lung cancer (ASCEND-4): a randomised, open-label, phase 3 study. Lancet 389, 917–929 (2017).
Camidge, D. R. et al. Updated efficacy and safety data and impact of the EML4-ALK fusion variant on the efficacy of alectinib in untreated ALK-positive advanced non-small cell lung cancer in the global phase III ALEX study. J. Thorac. Oncol. 14, 1233–1243 (2019).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT02767804 (2024).
Shaw, A. T. et al. Lorlatinib in non-small-cell lung cancer with ALK or ROS1 rearrangement: an international, multicentre, open-label, single-arm first-in-man phase 1 trial. Lancet Oncol. 18, 1590–1599 (2017).
Solomon, B. J. et al. Lorlatinib in patients with ALK-positive non-small-cell lung cancer: results from a global phase 2 study. Lancet Oncol. 19, 1654–1667 (2018).
Solomon, B. J. et al. Efficacy and safety of first-line lorlatinib versus crizotinib in patients with advanced, ALK-positive non-small-cell lung cancer: updated analysis of data from the phase 3, randomised, open-label CROWN study. Lancet Respir. Med. 11, 354–366 (2023).
Lin, J. J. et al. Safety and preliminary activity of the selective ALK inhibitor NVL-655 in patients with ALK fusion-positive solid tumors. Mol. Cancer Ther. 22, B154 (2023).
Ardini, E. et al. Entrectinib, a Pan-TRK, ROS1, and ALK inhibitor with activity in multiple molecularly defined cancer indications. Mol. Cancer Ther. 15, 628–639 (2016).
Parker, A. R. et al. Novel covalent modification of human anaplastic lymphoma kinase (ALK) and potentiation of crizotinib-mediated inhibition of ALK activity by BNP7787. Onco Targets Ther. 8, 375–383 (2015).
Zhang, C. et al. Proteolysis targeting chimeras (PROTACs) of anaplastic lymphoma kinase (ALK). Eur. J. Med. Chem. 151, 304–314 (2018).
Kang, C. H. et al. Induced protein degradation of anaplastic lymphoma kinase (ALK) by proteolysis targeting chimera (PROTAC). Biochem. Biophys. Res. Commun. 505, 542–547 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT02729961 (2019).
Guan, J. et al. Anaplastic lymphoma kinase L1198F and G1201E mutations identified in anaplastic thyroid cancer patients are not ligand-independent. Oncotarget 8, 11566–11578 (2017).
Wu, W., Haderk, F. & Bivona, T. G. Non-canonical thinking for targeting ALK-fusion onco-proteins in lung cancer. Cancers 9, 164 (2017).
Katic, L. & Priscan, A. Multifaceted roles of ALK family receptors and augmentor ligands in health and disease: a comprehensive review. Biomolecules 13, 1490 (2023).
Inoue, T. & Thomas, J. H. Suppressors of transforming growth factor-beta pathway mutants in the Caenorhabditis elegans dauer formation pathway. Genetics 156, 1035–1046 (2000).
Englund, C. et al. Jeb signals through the Alk receptor tyrosine kinase to drive visceral muscle fusion. Nature 425, 512–516 (2003). With Lee et al. (ref. 262), this article provides preliminary evidence about the roles for the ALK receptor in normal development in Drosophila.
Lee, H. H., Norris, A., Weiss, J. B. & Frasch, M. Jelly belly protein activates the receptor tyrosine kinase Alk to specify visceral muscle pioneers. Nature 425, 507–512 (2003). With Englund et al. (ref. 261), this article provides preliminary evidence about the roles for the ALK receptor in normal development in Drosophila.
Yao, S. et al. Anaplastic lymphoma kinase is required for neurogenesis in the developing central nervous system of zebrafish. PLoS ONE 8, e63757 (2013).
Fadeev, A., Krauss, J., Singh, A. P. & Nusslein-Volhard, C. Zebrafish Leucocyte tyrosine kinase controls iridophore establishment, proliferation and survival. Pigment. Cell Melanoma Res. 29, 284–296 (2016).
Bilsland, J. G. et al. Behavioral and neurochemical alterations in mice deficient in anaplastic lymphoma kinase suggest therapeutic potential for psychiatric indications. Neuropsychopharmacology 33, 685–700 (2008).
Witek, B. et al. Targeted disruption of ALK reveals a potential role in hypogonadotropic hypogonadism. PLoS ONE 10, e0123542 (2015).
Guan, J. et al. FAM150A and FAM150B are activating ligands for anaplastic lymphoma kinase. eLife 4, e09811 (2015). With Reshetnyak et al. (ref. 268), this article demonstates the physiological ligands of the ALK receptor.
Reshetnyak, A. V. et al. Augmentor alpha and beta (FAM150) are ligands of the receptor tyrosine kinases ALK and LTK: hierarchy and specificity of ligand-receptor interactions. Proc. Natl Acad. Sci. USA 112, 15862–15867 (2015). With Guan et al. (ref. 267), this article demonstates the physiological ligands of the ALK receptor.
Zhang, H. et al. Deorphanization of the human leukocyte tyrosine kinase (LTK) receptor by a signaling screen of the extracellular proteome. Proc. Natl Acad. Sci. USA 111, 15741–15745 (2014).
Orthofer, M. et al. Identification of ALK in thinness. Cell 181, 1246–1262.e1222 (2020).
Defaye, M. et al. The neuronal tyrosine kinase receptor ligand ALKAL2 mediates persistent pain. J. Clin. Invest. 132, e154317 (2022).
Acknowledgements
The authors thank N. Chamberlin for her critical reading of the text. The work has been supported by grants from the NIH/NCI R01 CA196703-01, the NIH/NCI P50 CA265826-01A1_LUNG SPORE, the LUNGevity ALK-positive Lung Cancer Research Award, the PoweRD 2 CureALK+ Lung Cancer TeamLab support, the AIRC IG 2021 — ID. 26011 project to R.C.; AIRC under IG 2019 — ID. 23146 to C.V.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article. R.C., C.A. and C.V. contributed substantially to discussion of the content. R.C., C.A. and C.V. wrote the article. All authors reviewed and/or edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
R.C. is the founder and consultant of ALKEMIST Bio. C.V., F.I. and C.A. declare no conflict of interest.
Peer review
Peer review information
Nature Reviews Cancer thanks Keith Ligon, Aaron Hata and Bengt Hallberg for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Antibody–drug conjugates
-
(ADC). Targeted therapies that link an antibody to a cytotoxic drug, delivering the drug specifically to cancer cells by binding to the antigen expressed on their surface.
- Basket trials
-
Clinical trials that test the effectiveness of a single drug or treatment on multiple types of cancer that share a common genetic mutation, regardless of the cancer cell of origin or cancer type.
- Breakpoint variants
-
Different, yet specific, locations within the same gene in which chromosomal breaks occur, leading to structural rearrangements such as translocations or fusions.
- Circulating tumour DNA
-
(ctDNA). Fragments of DNA released into the bloodstream from cancer cells, which can be analysed to detect and monitor presence, progression and response to treatment.
- Complete remission
-
The absence of all detectable signs of disease following cancer treatment.
- Compound ALK mutants
-
The presence of two or more mutations within the same gene, occurring either on the same allele (cis) or different alleles (trans). They usually arise as a mechanism of resistance to targeted therapy.
- Drug-tolerant persister cells
-
A small subpopulation of cancer cells that enter a dormant state, allowing them to survive harsh conditions or treatments, such as chemotherapy or tyrosine kinase inhibitor, and potentially cause recurrence or treatment failure.
- First-line therapy
-
The initial treatment recommended for a particular disease or condition, typically based on its effectiveness and safety.
- Oncogenic stress
-
A detrimental effect on tumour cell fitness that results from the overexpression or excessive activation of an oncogene, which can cause cellular stress, senescence or death, which can be exploited for cancer therapy.
- Partner gene
-
One of the two genes involved in a fusion event, often due to chromosomal rearrangements, that can lead to abnormal gene function.
- Patient-derived xenograft models
-
(PDX models). Models in which tumour tissue from a patient is implanted into immunodeficient mice, allowing researchers to study the tumour’s growth, drug response and biology in vivo while maintaining its original characteristics.
- Steric hindrance
-
The prevention of chemical reactions or interactions owing to physical obstruction caused by the spatial arrangement of atoms or groups within a molecule.
- Tyrosine kinase inhibitors
-
(TKIs). Small drugs capable of binding to the catalytic domain of a tyrosine kinase and disrupting the kinase activity and downstream signal transduction pathways.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Voena, C., Ambrogio, C., Iannelli, F. et al. ALK in cancer: from function to therapeutic targeting. Nat Rev Cancer 25, 359–378 (2025). https://doi.org/10.1038/s41568-025-00797-9
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41568-025-00797-9
This article is cited by
-
Engineering bi-directional chemically-modulated synthetic condensates for cellular control
Nature Communications (2025)