Abstract
Use of signal transduction inhibitors as single agents to treat cancer leads to resistance because of the plasticity of intracellular signaling, and combination therapy can overcome this. We describe the first-in-human trial of avutometinib (RAF–MEK clamp) and defactinib (focal adhesion kinase inhibitor) in patients with solid tumors. The trial met its primary endpoint and recommended a phase 2 dose and schedule. The recommended phase 2 dose and schedule for a 28-day cycle was determined to be avutometinib 3.2 mg once a day, twice weekly (Monday and Thursday or Tuesday and Friday), and defactinib 200 mg twice a day, seven days a week. Both drugs were administered orally on a 3 weeks ‘on’ and 1 week ‘off’ basis. The pharmacokinetics and pharmacodynamics were consistent with previous reports of avutometinib and defactinib used as single agents. Key findings include an objective response rate of 42.3% (11 of 26; 95% confidence interval 23.4–63.1) and a median progression-free survival of 20.1 months (95% confidence interval 11.2–43.9) in patients with low-grade serous ovarian cancer. This study demonstrates the importance of intermittent dosing schedules in combined targeting of the mitogen-activated protein kinase and focal adhesion kinase pathways to improve tolerability, and has acquired proof of concept of anti-tumor activity against low-grade serous ovarian cancer, a tumor relatively resistant to chemotherapy. ClinicalTrials.gov identifier NCT03875820.
Similar content being viewed by others
Main
The mitogen-activated protein kinase (MAPK) pathway is a crucial cellular signaling cascade contributing to proliferation and apoptosis, and is often activated as a key driver of oncogenesis. Observed clinical efficacy with MEK-only inhibitors has shown MEK to be a crucial and targetable signaling node in the MAPK pathway, downstream of oncogenic mutations in genes such as BRAF, KRAS and EGFR driving cellular proliferation. MEK-only inhibitors have been licensed for use in combination in a number of diseases such as melanoma1,2, colon cancer3, thyroid cancer4 and neurofibromatosis5, a nonmalignant hyperproliferative condition. Focal adhesion kinase (FAK) is a nonreceptor tyrosine kinase that mediates integrin signaling, is key to signaling through avian sarcoma virus gene product p60, phosphoinoside-3-kinase and rat sarcoma virus oncogene homolog family (RAS), and is involved in biological processes such as driving epithelial to mesenchymal transition, cell proliferation and immune escape6. Combinations of MEK and FAK inhibitors have been shown to be beneficial in preclinical models of melanoma7, uveal melanoma8 and more recently in low-grade serous ovarian cancer (LGSOC)9. There have been attempts to test the clinical combination of a MEK-only inhibitor and a FAK inhibitor before; however, overlapping toxicity, drug interactions and a lack of efficacy were reasons why further development of this combination was abandoned10.
We hypothesized that inhibiting the MAPK pathway (with the RAF–MEK clamp avutometinib) and FAK pathway (with the FAK inhibitor defactinib) would cause meaningful clinical responses in MAPK pathway-driven solid tumors, including LGSOC.
Avutometinib is a RAF–MEK clamp that, in addition to inhibiting MEK, induces the formation of dominant negative RAF–MEK complexes preventing phosphorylation of MEK by ARAF, BRAF and CRAF11,12. In a phase 1 trial with avutometinib used as a single agent, we modeled pharmacokinetic and pharmacodynamic data to develop a highly effective intermittent twice-a-week dosing schedule of avutometinib with single-agent activity in KRAS-mutated tumors13. Further, the FAK inhibitor defactinib has been characterized in phase 1–3 trials and has shown limited anticancer activity14,15,16.
We aimed to explore the combination of the RAF–MEK clamp avutometinib with the FAK inhibitor defactinib in a phase 1 clinical trial evaluating tolerability, pharmacokinetics, pharmacodynamics and efficacy across a range of MAPK pathway-driven solid tumors, including LGSOC (FRAME; NCT03875820).
Results
Demographics
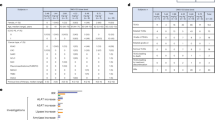
Ninety-one patients were recruited to the trial between 18 December 2017 and 8 June 2023, 90 of whom received at least one dose and were evaluable for toxicity (safety population). Median follow-up was 12.2 months (95% confidence interval (CI) 9.0–15.5). Safety-evaluable patients were recruited across the dose escalation (n = 12) and dose expansion cohorts, including LGSOC (n = 19), KRAS-mutated nonsmall cell lung cancer (NSCLC; n = 20), KRAS-mutated colorectal cancer (CRC; n = 10), pancreatic cancer (PC; n = 10), NSCLC with KRAS G12V mutations (n = 10), solid tumors with RAS or RAF mutations who consented to biopsy (n = 7) and endometrial or ovarian cancers with RAS or RAF mutations (n = 2). The median age was 61 years (range 21–78), 38% were men and 62% were women, and the median number of previous lines of treatment was 3 (range 1–10) (Table 1).
Dose escalation
The FRAME study followed a modified 3 + 3 dose escalation pattern and had four planned dose escalation cohorts (Fig. 1). Three patients were treated at dose level 1 (28-day cycle with avutometinib 3.2 mg once a day, twice weekly (Monday and Thursday or Tuesday and Friday) + defactinib 200 mg twice a day, seven days a week, both drugs given on a 3 weeks ‘on’ and 1 week ‘off’ (for 3 in every 4 weeks) basis. No dose-limiting toxicities (DLTs) were recorded and two parallel dose escalation cohorts were opened for recruitment: cohort 2a (28-day cycle with avutometinib 4 mg once a day, twice weekly + defactinib 200 mg twice a day, seven days a week, both drugs given for 3 in every 4 weeks) and cohort 2b (28-day cycle with avutometinib 3.2 mg once a day, twice weekly + defactinib 400 mg twice a day, seven days a week, both drugs given for 3 in every 4 weeks). Dose level 2b was not tolerated with DLTs in two of three patients, which were grade 2 rash resulting in an inability to receive the minimum planned dose of drug in the first cycle (defined at least 5 doses of avutometinib and 32 doses of defactinib), and no further patients were treated on this cohort. Dose level 2a was considered tolerable with 0 of 6 patients experiencing DLTs. Dose level 3 was not explored because dose level 2b was not tolerated. Following treatment at dose level 2a of ten patients with KRASM NSCLC and seven patients in the RAS–RAF mutation-enriched solid tumor (ST) biopsy cohort, it was noted that multiple patients experienced chronic grade 2 skin rash requiring dose interruptions. It was also noted that two patients on dose level 1 had responded to treatment and had an ongoing partial response to treatment at the time of decision-making, suggesting that it was an active dose and was tolerable at 12 months of treatment. A further factor taken into consideration was the pharmacokinetic profiles of both drugs, which suggested that drug concentrations achieved in dose level 1 were in a pharmacodynamically active range. Because this combination would likely be used as chronic treatment over months or years of treatment, the safety review committee decided to declare dose level 1 the recommended phase 2 dose (RP2D). All subsequent patients were treated at dose level 1 (Fig. 1).
Dose levels 2a and 2b were explored in parallel after dose level 1 had been deemed safe by the safety review committee. Dashed lines indicate that dose level 3 was not explored in the dose escalation part of the trial because stopping criteria were met for dose level 2b. Dose level 2a was selected for the dose expansion part of the trial. After ten patients in the KRASM NSCLC cohort and seven in the ST biopsy cohort had been treated with dose level 2b, the decision was made to update the RP2D to dose level 1 (the detailed rationale is provided in the main text). Other expansion cohorts include LGSOC, RAS-mutant CRC, PC, RAS–RAF mutant endometrioid subtype of gynecological cancers (ovarian, endometrial, endometriosis-related) (EOC); G12V-specific KRAS mutant nonsmall cell lung cancer (KRASG12V NSCLC). ST biopsy cohort, solid tumors (enriched for those with RAS mutations who were eligible for one pretreatment and two post treatment biopsies).
Tolerability
Twelve patients were treated in the dose escalation cohorts. There were two protocol defined DLTs in the dose escalation cohorts (0 of 3) in cohort 1, 0 of 6 in cohort 2a and 2 of 3 in cohort 2b (described previously). Seventy-eight patients were treated in the dose expansion cohorts.
Additional Bayesian analysis of the DLT rate at RP2D17 (3 DLTs and 64 patients), using a beta-binomial conjugate model with a Beta (1,1) prior, estimates the posterior mean DLT rate to be 6.1% (95% highest posterior density interval: 1.1% to 11.7%) (Extended Data Table 1).
The five most common adverse events (AEs) in the trial were rash (90%), creatine phosphokinase (CPK) elevation (56%), aspartate aminotransferase (AST) elevation (43%), hyperbilirubinemia (38%) and diarrhea (38%). The percentages of these common toxicity criteria for adverse events that were grade 3–4 were 8%, 9%, 1%, 2% and 1%, respectively. Table 2 documents AEs that were present in 10% or more of patients.
Pharmacokinetics and pharmacodynamics
The pharmacokinetics of both drugs were assessed in cycle 1 day 8 or day 15 for 48 h on days when patients received avutometinib (Fig. 2). At the RP2D, the geometric mean of the area under the plasma concentration versus time curve (AUC) to 48 h and the maximum plasma concentration (Cmax) of avutometinib were 11,463 h ng−1 ml−1 coefficient of variation (CV) (CV 37) and 342 ng ml−1 (CV 34), respectively. The geometric mean of the AUC to 12 h and the Cmax of defactinib at the RP2D were 2,099 h ng−1 ml−1 (CV 102) and 273 ng ml−1 (CV 80), respectively (Tables 3 and 4). These parameters were similar to the profiles of both drugs used as single agents in clinical trials13,14. Although not formally tested, these findings do not suggest an obvious drug–drug interaction between avutometinib and defactinib.
Biopsies were done in nine patients with a biopsy pretreatment, biopsy 4–24 h after a single dose of avutometinib (run-in dose) taken within 3–7 days of the first dose of combination therapy and a third biopsy during combination therapy 4–24 h of avutometinib dose taken within 2 weeks of the start of cycle 2. Levels of p-MEK and p-ERK were quantified in antibody bead-based assays in flash-frozen tissue and levels of p-FAK were quantified using immunohistochemistry. a, Samples from eight of nine patients passed quality control checks for p-MEK assessment in all three samples. The fold change in median fluorescence intensity (MFI) units is shown on the y axis. Horizontal dashed line represents baseline. b, Samples from four of nine patients passed the quality control checks for p-ERK assessment in all three samples. The fold change in MFI units is shown on the y axis. Open circles represent a patient with screening p-ERK levels below the lower limit of detection of the assay. Horizontal dashed line represents baseline. c, It was possible to detect cytoplasmic p-FAK in all three samples from seven patients. Absolute histochemical (H) score is shown on the x axis.
Phosphorylated mitogen activated protein kinase kinase (p-MEK), phosphorylated extracellular signal regulated kinase (p-ERK) and phosphorylated focal adhesion kinase (p-FAK) were evaluated in three biopsies: pretreatment, post single-dose avutometinib (run-in dose) and post combination therapy dose that showed target engagement (Fig. 2a–c).
Efficacy
Eighty-two patients were considered evaluable for response in the study. The findings for patients with KRAS-mutated NSCLC, and CRC and PC are described in Extended Data Fig. 1a,b.
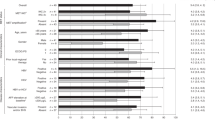
The most important finding of the study was the outcome for patients with LGSOC. Because patients with LGSOC from the dose escalation cohort benefited from the treatment, patients with LGSOC in the dose escalation and expansion cohorts were analyzed together (n = 26). The objective response rate (ORR) and median progression-free survival (mPFS) of patients in this study were 42.3% (11 of 26; 95% CI 23.4–63.1%) and 20.1 months (95% CI 11.2–43.9), respectively. Of note in the 24 patients for whom it was possible to sequence samples for KRAS mutations, the ORR and mPFS in patients with and without KRAS mutations were 58.3% (7 of 12; 95% CI 27.7–84.8) and 30.8 months (95% CI 17.4 to not reached) versus 33.3% (4 of 12; 95% CI 9.9–65.1) and 8.9 months (95% CI 5.3 to not reached), respectively (Fig. 3, Extended Data Table 2 and Extended Data Fig. 2). Eleven patients with LGSOC had previously received a MEK inhibitor and the ORR in this patient cohort was 27.3% (3 of 11; 95% CI 6–61). Of 27 patients with LGSOC who were evaluable for toxicity, only 4% (1 of 27) discontinued or withdrew because of toxicity (in this case grade 3 skin toxicity). A further interesting finding in this study was that two patients with LGSOC had brain metastasis before enrolling on the study and in both the metastatic lesions in the brain shrank (Extended Data Fig. 3). Detailed outcomes of patients in different individual cohorts are present in Supplementary Figs. 1–5 and Supplementary Tables 1–3.
a, Best overall response in patients with LGSOC in the dose escalation and dose expansion parts of the study. Dashed horizontal line represents −30%, which is considered a partial response as per response evaluation criteria for solid tumours (RECIST 1.1). b, Progression free survival (PFS) of all patients with LGSOC in the study. Histograms in gray indicate previous treatment with prior MEK inhibitors.
Discussion
The combination of MEK-only inhibitors and a FAK inhibitor has been attempted before and was abandoned because of drug–drug interaction leading to associated toxicity with those agents, and limited efficacy10. This FRAME study built upon a pharmacokinetically-pharmacodynamically (PK–PD)-driven unique intermittent dosing schedule of the RAF–MEK clamp avutometinib as a single agent13 to design a combination trial with the FAK inhibitor defactinib. Single-agent phase 1, 2 and 3 studies of FAK inhibitors have shown limited success15,16,18. This clinical study shows encouraging clinical activity for a combination of the RAF–MEK clamp avutometinib with the FAK inhibitor defactinib, and led to the breakthrough designation by the Food and Drug Administration (FDA) for the combination of avutometinib and defactinib in patients with LGSOC, and launch of the ongoing registration-enabling study (RAMP301; NCT06072781). The FDA granted accelerated approval for the combination of avutometinib and defactinib for KRAS mutated recurrent LGSOC on 8 May 2025.
The results of this study utilize the Pharmacological Audit Trail, which uses tolerability, pharmacokinetics and pharmacodynamics to recommend a phase 2 dose and schedule19. The study was also expanded to different cohorts to further fine-tune the dose decision and opened several cohorts to evaluate signals of efficacy in multiple MAPK pathway-driven tumor types. At the RP2D of the combination of avutometinib and defactinib, the pharmacological profile was in the range of that detected in previous phase 1 studies13,14,20,21 and although no formal pharmacokinetic interaction studies were done, drug levels did not suggest an obvious drug–drug interaction between avutometinib and defactinib. In keeping with the mechanism of action of the RAF–MEK clamp avutometinib, reduction in phosphorylation of p-MEK and p-ERK was observed after treatment with avutometinib and the combination of avutometinib and defactinib. Interestingly, a reduction in the phosphorylation of p-FAK was observed following treatment with defactinib when compared with the increase in p-FAK following single-dose avutometinib treatment, providing an insight into possible reasons for the synergy of the combination.
There were no confirmed partial responses in the PC and CRC cohorts; however, because PK, PD and tolerability were established in these cohorts of patients, this combination has been added to and is being evaluated in combination with standard of care treatment in PC (in combination with gemcitabine and nab-paclitaxel; NCT5669482) and colon cancer (in combination with cetuximab; NCT06369259). In the setting of KRAS-mutated NSCLC, the ORR and mPFS of these patients are 11.1% and 3.5 months, respectively, with confirmed responses in patients with KRAS G12V and G12C mutations. Currently, this dose and schedule of avutometinib and defactinib are being evaluated in combination with standard of care treatment in patients with KRAS G12C NSCLC (in combination with sotorasib; NCT05074810).
The most significant finding from this study is the high response in patients with LGSOC. LGSOC is a subtype of ovarian cancer with 30% of patients harboring a KRAS mutation22 and have poor response rates to standard chemotherapy, ORR 13% (ref. 23). The tolerability of avutometinib and defactinib was documented. Of patients with LGSOC, 27 were evaluable for toxicity and only 4% (1 on 27) discontinued or withdrew because of toxicity (in this case grade 3 skin toxicity). In previously published MEK inhibitor studies in LGSOC, dose reductions and discontinuation because of toxicity were not provided in the phase 2 clinical trial of selumetinib24, but discontinuation rates because of AEs were 36% with trametinib25 and 31% with binimetinib23. The higher toxicity observed in the trametinib and binimetinib studies may be because of the need for continuous dosing with these MEK inhibitors. The PK and PD profiles of avutometinib enabled the current effective and highly intermittent dose–schedule proposed by the authors in a previous trial and is likely to represent an improved tolerability13. Twenty-six patients with LGSOC were evaluable for efficacy in the escalation and expansion cohorts. The ORR and m-PFS in patients with LGSOC in this study were 42.3% and 20.1 months, respectively. Several phase 2 and phase 3 trials have evaluated MEK inhibitors in LGSOC with response rates and progression-free intervals ranging from 15% to 26% and from 9 to 13 months, respectively: selumetinib 15% and 11 months24, trametinib 26% and 13 months25 and binimetinib 16% and 9.1 months23. Of note, it was possible to sequence KRAS in 24 of 26 response-evaluable patients with LGSOC in this study. The ORR and m-PFS of patients with KRAS-mutated LGSOC treated in this study were 58.3% (7 of 12) and 30.8 months, respectively. These results are favorable when put into context with other MEK inhibitor studies in which reported response rates and mPFS in RAS- or RAF-mutated LGSOC are: 14% and mPFS not calculated for selumetinib24, 50% and 13.2 months for trametinib25 and 44% and 17.6 months for binimetinib23. Given that the tolerability of the combination of avutometinib and defactinib is better than that previously published with MEK-only inhibitors in LGSOC, the promising ORR and mPFS in this study including patients treated with prior MEK inhibitors, and the minimal benefit from chemotherapy seen previously, a phase 2 study (RAMP201; NCT04625270) was opened randomizing patients between single-agent avutometinib versus the combination of avutometinib and defactinib. Further, a phase 3 study (RAMP301; NCT06072781) was launched evaluating the combination in LGSOC compared with investigators’ choice of therapy.
A shortcoming of this trial is that not all patients in all cohorts were genotyped; for example, not all patients in the dose escalation, PC and endometroid ovarian cancer cohorts were sequenced. As with complex treatment schedules of signal transduction inhibitors, the initial R2PD dose level 2a had to be modified to dose level 1. The ORR and mPFS in the LGSOC cohort are encouraging but the trial was not statistically powered to study ORR or PFS. Further studies will require more randomized trials to ascertain the activity of avutometinib versus the combination of avutometinib and defactinib (RAMP201; NCT04625270) and the combination versus the standard of care in LGSOC (RAMP301; NCT06072781).
To conclude, we report a phase 1 clinical trial with signal searching basket expansion cohorts in multiple tumor types with multiple novel aspects including a highly intermittent dosing regimen of a nonchemotherapy combination of the RAF–MEK clamp avutometinib with the FAK inhibitor defactinib that showed improved tolerability. This study demonstrated encouraging ORR and mPFS compared with historical trials with chemotherapy, hormonal therapy and MEK-only inhibitors in patients with LGSOC who are now being further evaluated in randomized phase 3 studies.
Methods
Compliance with reporting guidelines
The CONSORT-DEFINE checklist for early phase dose-finding trials, alongside the study protocol are provided in the Supplementary data to enhance transparency and ensure accurate reporting of the study’s findings26.
Trial objectives
The primary objective of this study was to recommend a phase 2 dose and to characterize the safety profile for the combination of avutometinib and defactinib. The secondary endpoint included establishing the pharmacokinetic profile of avutometinib and defactinib administered together. The tertiary endpoints included characterizing the clinical efficacy of the combination in patients with solid tumors, studying the pharmacodynamic profile of both drugs and assessing biomarkers of sensitivity and resistance to the combination.
Determination of starting dose
A clinical trial of avutometinib administered as a single agent determined the maximal tolerated dose of avutometinib as 4 mg twice a week (Monday and Thursday or Tuesday and Friday) on a 3 weeks ‘on’, 1 week ‘off’, 28-day schedule13. The starting dose for this combination phase 1 study was 3.2 mg delivered at the same schedule and was lower than the single-agent dose. Phase 1 trials of defactinib evaluated doses between 12 and 750 mg twice daily14 and single-agent phase 2 trials were conducted at a dose of 400 mg twice daily15,16. The starting dose of defactinib in this combination study was at a lower dose; that is, 200 mg twice daily.
Trial design
This study followed a modified 3 + 3 dose escalation design (Fig. 1). If dose level 1 was tolerated, dose levels 2a and 2b were opened simultaneously. Patients were not randomized to dose levels 2a and 2b and were allocated to each cohort alternatively in an pragmatic way to ensure efficient recruitment in the trial. If either dose level 2a or dose level 2b was not tolerated, dose level 3 was not explored. Following RP2D, multiple expansion cohorts were opened. Following establishment of a recommended dose, tumor expansion cohorts were studied. Dose level 2a was selected as the initial RP2D (‘Results’). Version 1.0 of the protocol, dated 7 September 2017, featured two initial expansion cohorts (KRAS-mutated NSCLC and RAS–RAF-enriched ST biopsy cohort). After ten patients in the NSCLC cohort and seven in the solid tumour cohort had been treated with dose level 2b, the decision was made to update the RP2D to dose level 1. Additional expansion cohorts were introduced by amendments to the protocol in version 2.6 dated 4 April 2019 (LGSOC and CRC) and version 4.0 dated 30 June 2020 (PC, RAS–RAF mutant endometrioid subtype of gynecological cancers (ovarian, endometrial, endometriosis-related) and G12V-specific KRAS mutant nonsmall cell lung cancer).
Tumor types are described in Fig. 1. The planned cohort sizes of 10–20 patients were not based on formal calculations. However, it was estimated that with 80 patients in total in the expansion cohorts, the probability of seeing no responses was <0.1% if the true response rate was 20%, and the probability of seeing two or more responses was 99.9%. The 80% CI if the response rate was 10% was [6.4%; 16.0%], the 80% CI if the response rate was 20% was [14.3%; 26.4%] and the 80% CI if the response rate was 30% was [23.7%; 37.5%].
Statistical methods
Analysis populations
-
(1)
Safety population: includes any patient who received at least one administration of the investigational medicinal products, VS-6766 [avutometinib] and/or defactinib.
-
(2)
Intention-to-treat population: contains all patients enrolled in the study (regardless of whether they were later found to be ineligible, a protocol violator, given the wrong treatment or dose allocation, never treated and so on).
-
(3)
Response-evaluable patient population: must have received at least one cycle of the trial medication, have had a baseline Response Evaluation Criteria in Solid Tumors (RECIST) assessment and at least one post baseline RECIST assessment to be evaluable for response. Patients who progressed before the first scheduled post baseline RECIST assessment were still evaluable for response.
-
(4)
DLT evaluable population: all eligible dose escalation patients who received the combination of VS-6766 [avutometinib] and defactinib and either:
-
(a)
completed minimum safety evaluation requirements and received at least 5 of 6 doses of VS-6766 [avutometinib] (or 5 of 7 doses in patients requiring the run-in dose) and 32 out of 42 doses of defactinib during the first cycle at a specified new dose level
or
-
(b)
experienced a DLT during the first cycle at a specified new dose level.
-
(a)
Baseline characteristics are presented descriptively. Median follow-up was calculated using the reverse Kaplan–Meier approach. ORRs are presented with their 95% CIs. The mPFS, defined as the time from the first combination dose to progression or death, was estimated using the Kaplan–Meier method and shown together with a 95% CI. Waterfall plots were used to graphically present best percentage change from baseline of the sum of lesion diameters according to RECIST v.1.1. A swimmer plot was utilized to display PFS by patient and previous MEK inhibitor treatment for all LGSOC patients.
Participants
Patients aged 18 years or older were eligible for the study. Inclusion criteria were hemoglobin ≥9 g d−1, absolute neutrophil count of ≥1.5 × 109 per liter, platelet count of >100 × 109 per liter, bilirubin ≤1.5 upper limit of normal, AST and alanine aminotransferase (ALT) of ≤2.5 upper limit of normal if no liver metastasis was present or ≤5 upper limit of normal if liver metastasis was present. A calculated creatinine clearance of ≥50 ml min−1 or a serum creatinine of ≤1.5 upper limit of normal was permissible. Patients had to have a corrected QT interval of <470 ms. Exclusion criteria were chemotherapy, endocrine therapy, biological therapy, immunotherapy or radiotherapy (except for palliative radiotherapy) in the past 4 weeks. Major surgery in the past 4 weeks was an exclusion criterion as was a known history of Gilbert’s syndrome and history of acute or chronic pancreatitis. Specific exclusion criteria for ocular disease included history of glaucoma, history of retinal vein occlusion and features predisposing to retinal vein occlusion such as uncontrolled hypertension and uncontrolled diabetes. Patients administered a strong CYP3A4 and strong CYP2C9 inhibitor for the past 7 days before the first dose of trial medication were excluded.
Toxicity assessment
Toxicity was assessed using CTC AE V4. Patients were seen on every week for the first 8 weeks on treatment and every 4 weeks following that. DLT was any event that was deemed highly probably or probably related to avutometinib or defactinib in the first cycle of treatment and included grade 4 neutropenia, grade 3 or higher thrombocytopenia associated with clinically significant bleeding, febrile neutropenia, infection associated with grade 3 or 4 neutropenia, and grade 3 or higher increase in bilirubin associated with grade 3 or grade 4 elevation of AST and ALT. Grade 3 skin toxicity occurring after dose reduction or if grade 3 skin toxicity persists for 2 weeks after appropriate supportive measures and grade 3 ophthalmological toxicity were deemed as DLTs. Inability to receive at least 5 doses of avutometinib and at least 32 doses of defactinib in cycle 1 and delay in starting cycle 2 by ≥2 weeks because of treatment-related toxicity, which have not resolved to baseline or grade 1 or lower, were considered DLTs. Drug-related grade 5 toxicity or any other toxicity that the investigator deemed dose limiting was considered a DLT. Alopecia of any grade and isolated laboratory changes of any grade without clinical significance or clinical sequela were not considered DLTs. Grade 3 or grade 4 toxicity of any other organ was deemed a DLT with the following exceptions: grade 3 or 4 nausea or vomiting unless patients had received optimal antiemetics; grade 3 or 4 diarrhea unless patents had received optimal anti-diarrheal treatment; grade 3 or 4 AST or ALT unless it increased by two or more grades since baseline; grade 3 bilirubin; and grade 3 CPK elevation.
Pharmacokinetics
Pharmacokinetic sampling was conducted on the day of avutometinib dosing in the second or third week of dosing; that is, in cycle 1 between day 8 and day 21. Samples were collected at pre-dose, 30 min and 1, 2, 4, 8, 12, 24 and 48 h. The plasma concentrations of avutometinib and defactinib were obtained by liquid chromatography–mass spectrometry. Pharmacokinetic parameters such as Cmax, terminal half-life and AUC were calculated using noncompartmental analysis (Phoenix v8.1, Certara).
Pharmacodynamics
In patients who consented to biopsies, three biopsies were conducted. Patients had a pretreatment biopsy, then had a run-in dose of avutometinib between −7 and −3 days of starting combination therapy. The second biopsy was conducted within 4–24 h of the run-in dose. The third biopsy was conducted at 4–24 h after a dose of avutometinib within 2 weeks of starting cycle 2. Phosphorylation of MEK (Ser222) and ERK (Thr185–Try187) was assessed using an antibody bead-based Luminex platform27. Phosphorylation of cytoplasmic FAK was assessed by immunohistochemistry. Primary antibody used was p-FAK (Tyr397) antibody clone D20B1 (cat. no. 8556, Cell Signaling Technologies, 1:50 dilution for 1 h). Detection was undertaken with an EnVision Flex High pH Kit Rabbit Kit (cat. no. K800021-2, Dako). Graphs were generated using GraphPad Prism v.10.4.1.
Response evaluation
Response evaluation was conducted with computed tomography or magnetic resonance imaging using RECIST 1.1. Scans were conducted at baseline and every 8 weeks up to cycle 6, following which scans were done at 8–12 weeks at the investigators’ discretion.
Progression was defined as either radiological progression or clinical progression. In the case of clinical progression, the date at which the patient was considered to have progressed clinically was recorded. Examples of clinical progression include patients with LGSOC with no change in their target lesions as per RECIST 1.1 but showing clinical signs of bowel obstruction.
Ethical considerations
The trial was conducted as per the principles of the Declaration of Helsinki. The protocol was reviewed and allowed to proceed by the Medicines and Healthcare products Regulatory Agency (MHRA) UK. The protocol was also reviewed by the National Research and Ethics Committee REC/LO/1473. The trial was registered with EudraCT: EudraCT number 2017-001035-39.
Trial administration
The trial was conducted across four units: the Drug Development Unit at the Royal Marsden NHS Foundation Trust, London, UK; the Gynecological Unit at The Royal Marsden NHS Foundation Trust, London, UK; The Christie Hospital, Manchester, UK; and Newcastle Upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, UK. The academic sponsor of the trial was the Institute of Cancer Research and The Royal Marsden Hospital NHS Foundation Trust. Trial funding was provided by Verastem Oncology and Chugai pharmaceutical company. Two weekly safety review committee meetings were held to evaluate toxicity with the chief investigator or chief investigator delegate and principal investigator or principal investigator delegate for every site with a patient on study. Dose escalation decisions were made by the safety review committee with the addition of an external independent clinician from the Experimental Cancer Medicine Centre who was not taking part in the study and who had time to review the toxicity and efficacy presented at the dose escalation meeting.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The anonymized derived data from this study that underly the results will be made available upon consideration of a reasonable scientific proposal by the sponsoring institutions. Requests are to be sent to the corresponding author.
Code availability
No relevant code to be made available.
References
Robert, C. et al. Improved overall survival in melanoma with combined dabrafenib and trametinib. N. Engl. J. Med. 372, 30–39 (2015).
Larkin, J. et al. Combined vemurafenib and cobimetinib in BRAF-mutated melanoma. N. Engl. J. Med. 371, 1867–1876 (2014).
Kopetz, S. et al. Encorafenib, binimetinib, and cetuximab in BRAF V600E-mutated colorectal cancer. N. Engl. J. Med. 381, 1632–1643 (2019).
Ho, A. L. et al. Selumetinib plus adjuvant radioactive iodine in patients with high-risk differentiated thyroid cancer: a phase III, randomized, placebo-controlled trial (ASTRA). J. Clin. Oncol. 40, 1870–1878 (2022).
Weiss, B. D. et al. NF106: a Neurofibromatosis Clinical Trials Consortium phase II Trial of the MEK inhibitor mirdametinib (PD-0325901) in adolescents and adults with NF1-related plexiform neurofibromas. J. Clin. Oncol. 39, 797–806 (2021).
Dawson, J. C., Serrels, A., Stupack, D. G., Schlaepfer, D. D. & Frame, M. C. Targeting FAK in anticancer combination therapies. Nat. Rev. Cancer 21, 313–324 (2021).
Rozanc, J. et al. Phosphoprotein patterns predict trametinib responsiveness and optimal trametinib sensitisation strategies in melanoma. Cell Death Differ. 26, 1365–1378 (2019).
Paradis, J. S. et al. Synthetic lethal screens reveal cotargeting FAK and MEK as a multimodal precision therapy for GNAQ-driven uveal melanoma. Clin. Cancer Res. 27, 3190–3200 (2021).
McNamara, B. et al. Preclinical efficacy of RAF/MEK clamp avutometinib in combination with FAK inhibition in low grade serous ovarian cancer. Gynecol. Oncol. 183, 133–140 (2024).
Mak, G. et al. A phase Ib dose-finding, pharmacokinetic study of the focal adhesion kinase inhibitor GSK2256098 and trametinib in patients with advanced solid tumours. Br. J. Cancer 120, 975–981 (2019).
Ishii, N. et al. Enhanced inhibition of ERK signaling by a novel allosteric MEK inhibitor, CH5126766, that suppresses feedback reactivation of RAF activity. Cancer Res. 73, 4050–4060 (2013).
Lito, P. et al. Disruption of CRAF-mediated MEK activation is required for effective MEK inhibition in KRAS mutant tumors. Cancer Cell 25, 697–710 (2014).
Guo, C. et al. Intermittent schedules of the oral RAF-MEK inhibitor CH5126766/VS-6766 in patients with RAS/RAF-mutant solid tumours and multiple myeloma: a single-centre, open-label, phase 1 dose-escalation and basket dose-expansion study. Lancet Oncol. 21, 1478–1488 (2020).
Jones, S. F. et al. A phase I study of VS-6063, a second-generation focal adhesion kinase inhibitor, in patients with advanced solid tumors. Invest. New Drugs 33, 1100–1107 (2015).
Gerber, D. E. et al. Phase 2 study of the focal adhesion kinase inhibitor defactinib (VS-6063) in previously treated advanced KRAS mutant non-small cell lung cancer. Lung Cancer 139, 60–67 (2020).
Fennell, D. A. et al. Maintenance defactinib versus placebo after first-line chemotherapy in patients with merlin-stratified pleural mesothelioma: COMMAND-a double-blind, randomized, phase II study. J. Clin. Oncol. 37, 790–798 (2019).
Gonen, M. A Bayesian evaluation of enrolling additional patients at the maximum tolerated dose in Phase I trials. Contemp. Clin. Trials 26, 131–140 (2005).
Brastianos, P. K. et al. Alliance A071401: phase II trial of focal adhesion kinase inhibition in meningiomas with somatic NF2 mutations. J. Clin. Oncol. 41, 618–628 (2023).
Banerji, U. & Workman, P. Critical parameters in targeted drug development: the pharmacological audit trail. Semin. Oncol. 43, 436–445 (2016).
Martinez-Garcia, M. et al. First-in-human, phase I dose-escalation study of the safety, pharmacokinetics, and pharmacodynamics of RO5126766, a first-in-class dual MEK/RAF inhibitor in patients with solid tumors. Clin. Cancer Res. 18, 4806–4819 (2012).
Shimizu, T. et al. A first-in-Asian phase 1 study to evaluate safety, pharmacokinetics and clinical activity of VS-6063, a focal adhesion kinase (FAK) inhibitor in Japanese patients with advanced solid tumors. Cancer Chemother. Pharmacol. 77, 997–1003 (2016).
Manning-Geist, B. et al. MAPK pathway genetic alterations are associated with prolonged overall survival in low-grade serous ovarian carcinoma. Clin. Cancer Res. 28, 4456–4465 (2022).
Monk, B. J. et al. MILO/ENGOT-ov11: binimetinib versus physician’s choice chemotherapy in recurrent or persistent low-grade serous carcinomas of the ovary, fallopian tube, or primary peritoneum. J. Clin. Oncol. 38, 3753–3762 (2020).
Farley, J. et al. Selumetinib in women with recurrent low-grade serous carcinoma of the ovary or peritoneum: an open-label, single-arm, phase 2 study. Lancet Oncol. 14, 134–140 (2013).
Gershenson, D. M. et al. Trametinib versus standard of care in patients with recurrent low-grade serous ovarian cancer (GOG 281/LOGS): an international, randomised, open-label, multicentre, phase 2/3 trial. Lancet 399, 541–553 (2022).
Yap, C. et al. Enhancing reporting quality and impact of early phase dose-defining clinical trial: CONSORT dose-finding extension (CONSORT-DEFINE) guidance. Br. Med. J. 383, e076387 (2023).
Stewart, A. et al. Differences in signaling patterns on PI3K inhibition reveal context specificity in KRAS-mutant cancers. Mol. Cancer Ther. 18, 1396–1404 (2019).
Acknowledgements
We acknowledge funding from Chugai Pharmaceuticals and Verastem Oncology towards running this study. The funders did not participate in the conceptualization, design, data collection, analysis or preparation of the manuscript. We also acknowledge infrastructural funding from the Experimental Cancer Medicine Initiative and the National Institute of Health Sciences (NIHR) Biomedical Research Centre, to participating Centers. The authors from the Institute of Cancer Research acknowledge funding from the Cancer Research UK Convergence Science Centre grant (CTRQQR-2021\100009) and Cancer Research UK grant to the The Institute of Cancer Research, Clinical Trials and Statistics Unit (C1491/A25351). U.B. was a recipient of NIHR grant RP-2016-07-028.
Author information
Authors and Affiliations
Contributions
U.B., J.S.d.B., S.B., C.Y., K.S., R.R., M.P. and T.P. were responsible for the study concept and design. S.B., M.G.K., A.G., A.I.G., V.S.P., A.T., R.S., R.C., R.G., N.T., A.S., A.P., J.L., A.M., J.S.d.B. and U.B. were responsible for data acquisition. M.R., R.R., B.G., K.S., N.T., T.P., M.P., J.R., C.Y. and U.B. analyzed the data. S.S. undertook medical supervision of the study. All authors were involved in data interpretation and in the writing, revision and critical review of the manuscript. All authors have approved the submitted version and are accountable for their contributions and the integrity of the work.
Corresponding author
Ethics declarations
Competing interests
S.B. has received honoraria for consulting and/or advisory board work from AbbVie, AstraZeneca, BioNTech, Eisai, Gilead, GlaxoSmithKline, Grey Wolf Therapeutics, Immunogen, Incyte, ITM Oncologics, Lilly, Merck Sharpe Dohme, Mersana, Myriad, Oncxerna, Pharmaand, Seagen, TORL BioTherapeutics, Verastem, Zymeworks; honoraria and/or expenses from AbbVie, AstraZeneca, GlaxoSmithKline, Immunogen, Merck Sharpe Dohme, Mersana, Takeda, Verastem and Zymeworks; research funding from AstraZeneca, GlaxoSmithKline; and PI for Global/ENGOT lead RAMP201 and ENGOT lead RAMP301 (Verastem-sponsored). M.G.K. has a consulting or advisory role with Bayer, Guardant Health, Janssen, Roche, Seattle Genetics and Zai Lab; has received speaker fees from BMS, Eisai, Janssen, Roche and Servier; travel, accommodation or expenses from BerGenBio, BMS, Janssen, Roche, Servier and Zai Lab; and research grants from Novartis and Roche. A.G. declares no competing interests. A.I.G. declares no competing interests. V.S.P. declares no competing interests. A.T. declares no competing interests. R.S. has received travel expenses from Bayer and for educational symposia from AstraZeneca. R.C. declares no competing interests. R.G. declares no competing interests. M.R. is an Institute for Cancer Research (ICR) employee. R.R. is an ICR employee. R.G. is an ICR employee. K.S. is an ICR employee. N.T. declares no competing interests. T.P. is an ICR employee. M.P. is an ICR employee. S.S. has received research grants from Verastem Oncology, Merck Sharpe Dohme; advisory board honoraria from Ellipses Pharma and Exscientia/Recursion; and is on the nonremunerated advisory board of Duke Street Bio, Ellipsis, Grey Wolf Therapeutics, Merck Sharp and Dohme and Roche. J.R. has received an advisory board honorarium from Novartis and is an ICR employee. C.Y. is an ICR employee and has received honoraria Faron Pharon Pharmaceuticals, Bayer, Trogenix and Merck. A.S. is an ICR employee; has received travel support from Sanofi, Roche-Genentech and Nurix; honoraria as a speaker from Astellas Pharma and Merck Sharp Dohme; and is on the advisory board of DE Shaw Research, CHARM therapeutics, Ellipses Pharma and Droia Ventures. A.P. declares no competing interests. J.L. has received research grants from Roche-Genentech, Astex, Merck Sharp Dohme, Janssen and Verastem Oncology; and is on the advisory boards of Basilia, Roche, GlaxoSmithKline and Servier. A.M. has received research grants Astex, Merck and Merck Sharp Dohme; honoraria from Chugai, Faron, Merck, GlaxoSmithKline, Seagen, Takeda and Janssen; travel support from Amgen and Janssen; and is on the advisory boards of Imugene, Jansson, Merck, Takeda, Merck Sharp Dohme, Genmab, Pfizer, AstraZeneca and Immutep. J.S.d.B. is an ICR employee, named as an inventor, with no financial interest for patent 8,822,438, submitted by Janssen that covers the use of abiraterone acetate with corticosteroids; has received research support from AstraZeneca, Cellcentric, Crescendo, Daiichi, Immunic Therapeutics, MetaCurUm, Myricx, Nurix, Oncternal, Orion and Sanofi Aventis; honoraria from advisory boards of AbbVie, Acai Therapeutics, Amgen, Amunix, Astellas, Bayer, Bioxcel Therapeutics, Celcuity, Crescendo, Daiichi, Dark Blue Therapeutics, Duke Street Bio, Dunad Therapeutics, Endeavor Biomedicines INC, Genentech-Roche, GSK, Macrogenics, Merck Serono, MetaCurUm, Moma Therapeutics, Myricx, Novartis, Nurix, Nuvation Bio, One-Carbon Therapeutics, Oncternal, Orion, Page Therapeutics, Peptone, Pfizer, Takeda, Tango Therapeutics, Tubulis, GmbH and VIR Biotechnology. U.B. is an ICR employee, named as an inventor on patents arising from this trial, ICR has has entered into a license agreement with Verastem Oncology and UB is due to receive a proportion of income arising from this license in accordance with the institute's rewards to discoverers policy; has received research grants from Verastem Oncology, Chugai and Avacta; and honoraria for advisory board work from Carrick Therapeutics, Pharmenable, Ellipses, Amalus Therapeutics, Dania Therapeutics and Pegascy. The Institute of Cancer Research has commercial interests in CYP17, AKT, CHK1, RAF, MPS1, FLT3/Aurora Kinase inhibitors, GCN2 activators, molecular glues and folate targeted thymidylate synthetase inhibitors.
Peer review
Peer review information
Nature Medicine thanks Claire Friedman, Mithat Gonen, R. Wendel Naumann and Robert Wenham for their contribution to the peer review of this work. Primary Handling Editor: Ulrike Harjes, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Best overall response in colorectal, pancreatic cancer and NSCLC patients of patients on study.
A. Reduction in size in tumors in the patients with KRAS mutated colorectal cancer and pancreatic cancer expansions. B. Reduction size in tumors in patients with KRAS mutated NSCLC in the escalation, KRAS mutated NSCLC expansion and KRAS G12V mutation cohort. NSCLC: Non-small cell lung cancer.
Extended Data Fig. 2 Progression free survival of LGSOC patients by KRAS mutation status.
Kaplan-Meier curves of progression free survival (PFS) for LGSOC patients by KRAS mutation status, from the first combination dose in the REP population. LGSOC: low-grade serous ovarian cancer. REP: Response evaluable patients.
Extended Data Fig. 3 Response in brain metastasis.
Patient with a diagnosis of LGOSC with brain metastasis was treated in the dose escalation in dose level 1 which is the recommended phase 2 dose. The patient had radiotherapy to brain metastases 6 months prior to trial entry. The patient, further had neurosurgery 2 months prior to trial entry. A. Pretreatment scans showing MRI bilateral brain metastasis. B. Representative sections form MRI scans showing reduction in flair and size of brain metastasis. MRI = magnetic resonance imaging. T1 = T1 weighted longitudinal relaxation time.
Supplementary information
Supplementary Information
Supplementary Tables 1–4, Figs. 1–5, FRAME protocol and FRAME statistical analysis plan.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Banerjee, S., Krebs, M.G., Greystoke, A. et al. Defactinib with avutometinib in patients with solid tumors: the phase 1 FRAME trial. Nat Med 31, 3074–3080 (2025). https://doi.org/10.1038/s41591-025-03763-y
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41591-025-03763-y
This article is cited by
-
Small-molecule drug discovery in malignant melanoma: current status and prospective developments
Medicinal Chemistry Research (2026)
-
Avutometinib and Defactinib: First Approval
Drugs (2025)