Abstract
α2-Macroglobulin is a highly abundant serum protein involved in the development of atherosclerosis and cardiac hypertrophy. However, its circulating molecular form and exact concentrations in human health/diseases are not known. Blue native-polyacrylamide gel electrophoresis of human serum was used to confirm the native conformation of α2-macroglobulin. We created an enzyme-linked immunosorbent assay suitable for quantifying its circulating molecular form and undertook a cross-sectional study to measure its serum levels in 248 patients with diabetes mellitus and 59 healthy volunteers. The predominant circulating molecular form of α2-macroglobulin was the tetramer, whereas its dimer was detectable in patients with high serum levels of α2-macroglobulin. The serum α2-macroglobulin concentration was not associated with glycated hemoglobin or any other glycemic variable as evaluated from 48-h continuous glucose monitoring, but showed close correlation with left ventricular posterior wall thickness, carotid artery intima-media thickness, urinary albumin:creatinine ratio (ACR) and brachial–ankle pulse wave velocity (baPWV). Multivariate analysis revealed only the ACR and baPWV to be independent variables influencing serum levels of α2-macroglobulin. Thus, an increased ACR and baPWV are associated with higher serum concentrations of α2-macroglobulin, and the latter may contribute to the mechanism by which albuminuria increases the risk of developing cardiovascular diseases.
Similar content being viewed by others
Introduction
In humans, α2-macroglobulin is the largest non-immunoglobulin molecule among the highly abundant proteins in the peripheral blood circulation. α2-macroglobulin is synthesized mainly in the liver as a result of coordination between endothelial cells and hepatocytes1. α2-macroglobulin can inhibit a broad spectrum of serine, threonine, and metalloproteases as well as pro-inflammatory cytokines2. It can also induce transcriptional activation of various genes essential for the proliferation/hypertrophy of cells, oncogenesis and atherosclerosis3.
Studies using stored pooled human plasma have suggested that two identical α2-macroglobulin subunits of size 182 kDa are disulfide-bonded to form dimers, which interact non-covalently to yield a tetrameric structure4,5. In biologic fluids, α2-macroglobulin tetramers appear to be predominant, but may undergo structural changes during manipulation and preservation6. Thus, the exact circulating molecular forms of α2-macroglobulin associated with health and diseases have yet to be elucidated.
A 182-kDa protein termed “cardiac isoform of α2-macroglobulin” was shown to induce expression of muscle-specific genes associated with the pressure-overloaded heart and to cause cardiac hypertrophy directly7,8,9,10. This putative “isoform” was claimed to be a key molecule inducing myocardial infarction and cardiac hypertrophy, especially in people with diabetes mellitus (DM) on the basis of serum level measurements11,12,13. Recently, we and others demonstrated using mass spectrometry that the corresponding proteins in rats and humans were indistinguishable from α2-macroglobulin molecule9,14.
Serum levels of α2-macroglobulin were determined first by Ganrot and Scherstén in 196715 and have been shown to be increased in some DM populations, females and certain age groups15,16. Increased levels in DM patients were later ascribed mostly to associated conditions, such as microvascular complications17, or worsened glycemic control18,19,20,21. However, those classical studies employed several assay methods using limited numbers of samples, whereas recent studies using commercial enzyme-linked immunosorbent assay (ELISA) kits have reported serum levels of α2-macroglobulin to be low8,11,12,22,23,24,25. The concentrations reported thus far have been very inconsistent, ranging widely over six orders of magnitude15,16,17,18,19,20,21,22,23,25,26,27. Also, the pathophysiologic role of this factor in human diseases remains unknown.
Microalbuminuria has been measured to assess renal risk in early diabetic nephropathy, but is also a strong predictor of cardiovascular diseases28,29,30. People with type-1 diabetes mellitus (T1DM) and nephropathy carry a tenfold greater risk of adverse cardiovascular outcome compared with those without these disorders31. A slightly increased urinary albumin:creatinine ratio (ACR) carries an increased atherosclerotic risk32, which is reduced by the regression of albuminuria28,33. The latter is also associated with premature death34,35,36,37 which, in those with T1DM, is due mainly to cardiovascular factors37. However, the mechanisms relating albuminuria with an increased cardiovascular risk are not known.
We established a new ELISA to quantify circulating levels of the molecular form of human α2-macroglobulin using an antibody that can recognize its monomers, dimers and tetramers in human serum. We designed a cross-sectional study to ascertain if this important molecule is related to diabetic microvascular complications and the risk factors of cardiac/atherosclerotic diseases.
Results
To study the native conformation of circulating α2-macroglobulin molecules, we incubated purified α2-macroglobulin protein and fresh human serum treated with and without dithiothreitol (DTT) and subjected them to sodium dodecyl sulfate (SDS)-PAGE and western blotting. A single band representing α2-macroglobulin-like immunoreactivity corresponding to the size of standard α2-macroglobulin protein was detected on western blots from healthy human serum. Treatment of serum and an α2-macroglobulin standard with increasing concentrations of DTT (1, 10 and 25 mM) reduced the standard α2-macroglobulin protein to form monomers of size 182 kDa (Fig. 1a). Blue native (BN)-PAGE of serum and standard α2-macroglobulin protein and subsequent immunoblotting revealed a single band corresponding to an α2-macroglobulin tetramer of size 725 kDa in untreated samples, whereas treatment of serum and standard α2-macroglobulin with DTT reduced the protein into monomers of size 182 kDa (Fig. 1b). A band corresponding to an α2-macroglobulin dimer was very faint or barely visible in the lane for a sample of healthy serum or in the lane for standard tetrameric α2-macroglobulin. However, in some untreated sera of patients with DM who showed increased serum levels of α2-macroglobulin, dimers of α2-macroglobulin were visible (Fig. 1c). These results suggested that circulating α2-macroglobulin molecules in healthy humans consisted of tetramers that could be monomerized completely by reducing intermolecular disulfide bonds, and that dimers could be present in some patients with DM.
Molecular form of circulating α2-macroglobulin molecules in humans. (a) Representative SDS-PAGE under reducing and non-reducing conditions of purified human α2-macroglobulin protein and human serum. Ten-microliters of fresh human serum diluted to 1:80 and pretreated with 25 mM (lane 1), 10 mM (lane 2), 1 mM (lane 3), 0.1 mM (lane 4), or 0.01 mM of DTT (lane 5), 0.5 µg of purified α2-macroglobulin protein pretreated with 25 mM (lane 6) or 0.1 mM of DTT (lane 7), and 10 µL of fresh human serum diluted to 1:80 and pretreated with (lane 8) or without 0.5% SDS (lane 9) were subjected to 4–20% gradient gel electrophoresis and immunoblotted using human α2-macroglobulin antibody. (b) BN-PAGE of human serum and purified α2-macroglobulin protein pretreated with and without DTT. Purified α2-macroglobulin protein (0.1 µg) pretreated without (lane 1) or with 25 mM of DTT (lane 2) and 10 μL of fresh human serum diluted to 1:400 pretreated without (lane 3) or with 25 mM of DTT (lane 4) were subjected to BN-PAGE and subsequent immunoblotting using human α2-macroglobulin antibody. (c) BN-PAGE of purified α2-macroglobulin protein and diluted sera and subsequent immunoblotting using human α2-macroglobulin antibody. Purified α2-macroglobulin (0.05 μg) protein pretreated without (lane 1) or with 25 mM of DTT (lane 2), and 10 µL of diluted sera (1:400) obtained from 3 healthy volunteers (lane 3–5) and 4 patients with diabetes (lane 6–9) showing increased α2-macroglobulin concentrations were subjected to BN-PAGE and subsequent immunoblotting. The figure shows the cropped blots and the full-length blots are presented in Supplementary Fig. 1a–c.
We established an ELISA using anti-human monoclonal mouse α2-macroglobulin IgG, which has been confirmed to recognize monomeric, dimeric and tetrameric α2-macroglobulin molecules. A curve prepared with tetrameric α2-macroglobulin standards (0.0–0.2 µg/mL) showed parallelism with those of serially diluted serum samples in the ELISA of α2-macroglobulin (Fig. 2a). When serial dilutions of serum were applied to the standard curve, a very good correlation was obtained (R2 = 0.9646). The concentration of unknown samples was determined by interpolation, which is reliant on a standard curve being generated appropriately. The intra-assay coefficient of variation (CV) of serum samples was 2.3% (n = 8) and inter-assay CV was 13.8% (n = 14). These results suggested that our ELISA was suitable for quantifying serum concentrations of α2-macroglobulin in humans. Using serum samples from 40 DM patients, we compared the results obtained with the current ELISA and those determined using quantitative western blotting14 (in which α2-macroglobulin molecules in serum should undergo reduction/monomerization during SDS-PAGE). Data for the ELISA of α2-macroglobulin showed close correlation with the total concentration of monomerized α2-macroglobulin (R2 = 0.575, p < 0.0001) (Fig. 2b).
α2-macroglobulin ELISA. (a) Parallelism of the dilution curve generated by normal human serum serially diluted to 1:40000, 1:80000, 1:120000, 1:160000, 1:200000, 1:240000, and 1:320000 (open circles) with the human α2-macroglobulin standard regression curve (closed circles). (b) Serum α2-macroglobulin levels of 40 DM patients were determined using quantitative western blotting and by ELISA, and the two values were plotted to observe potential correlations.
We measured serum concentrations of α2-macroglobulin in 59 healthy volunteers and 248 patients with DM (Table 1). Patients with DM showed significantly higher serum levels of α2-macroglobulin (310.4 ± 114.2 mg/dL) than healthy volunteers (272.9 ± 76.5 mg/dL) (p = 0.0169) (Fig. 3). When the data of all 307 subjects were analyzed together, serum levels of α2-macroglobulin did not correlate with HbA1c level. To confirm no association between serum α2-macroglobulin with glycaemic control or glycaemic fluctuation in DM, we analyzed the results of 57 individuals who underwent 48-h CGM at the time of measuring serum levels of α2-macroglobulin. Neither the mean glucose level nor data on glycemic fluctuation (standard deviation, CV, mean amplitude of glycemic excursions) showed a correlation with serum levels of α2-macroglobulin. These results negate the current belief that serum concentrations of α2-macroglobulin reflect glycemic control.
Comparison of serum α2-macroglobulin levels in healthy volunteers and in patients with diabetes mellitus. Serum samples obtained from 59 healthy volunteers (Controls) and 248 patients with diabetes were subjected to ELISA of α2-macroglobulin. Wide horizontal bars indicate the mean and the shorter horizontal bars indicate the SD. The unpaired t-test was used to compare serum levels for the two groups.*p < 0.05 vs. controls.
Pearson’s univariate correlation analysis revealed a positive correlation of serum levels of α2-macroglobulin with the ACR, baPWV, maximum intima media thickness (maxIMT), left ventricular posterior wall thickness (LVPWth) and interventricular septum thickness (IVSth), but not with HbA1c levels (Table 2). Serum levels of α2-macroglobulin in DM patients with retinopathy were higher than those without (Table 2). Of 248 patients with diabetes, 51 had cardiovascular disease as evidenced by coronary angiography, CT of coronary arteries and/or cardiac ultrasonography. Least square multivariate analyses revealed that only the ACR and baPWV were associated independently with higher serum levels of α2-macroglobulin, and that age, sex, eGFR or the presence of retinopathy or cardiovascular disease were not independent variables influencing serum levels of α2-macroglobulin (Table 3). Also, serum levels of α2-macroglobulin in DM patients with normoalbuminuria (281.0 ± 95.1 mg/dL, n = 131) were not significantly higher than those of healthy volunteers (272.9 ± 76.5 mg/dL, n = 59). Taken together, these results suggested that the ACR and baPWV had an impact on higher serum concentrations of α2-macroglobulin.
Discussion
We developed a highly sensitive ELISA to recognize human α2-macroglobulin molecules in serum specifically. The limit of detection was 0.5 ng/mL, and the standard curves obtained by diluting the serum from 1:40,000 to 1:320,000 showed parallelism with the standard purified tetramer protein of α2-macroglobulin. Inter-assay and intra-assay CVs were small, and the results were stably reproducible. α2-macroglobulin levels in human serum have ranged by six orders of magnitude, and reported to be 0.5–2.5 µg/dL when measured using commercial ELISA kits22,23,25. Albumin and Ig molecules make up the greatest proportion of plasma proteins, but α2-macroglobulin is regarded to be one of top-12 abundant proteins. In the present study, the serum concentration of α2-macroglobulin in healthy volunteers was 272.9 ± 76.5 mg/dL, which was quite reasonable.
Considering the well-described potent biologic activities of α2-macroglobulin10,38,39,40,41 and its predominance over other bioactive substances in plasma, significant fluctuations of this important molecule in the peripheral blood circulation could affect the onset and/or progression of human diseases. Our system is the first ELISA suitable for quantifying α2-macroglobulin levels in human serum accurately.
BN-PAGE revealed that the α2-macroglobulin-like immunoreactivity in human serum migrated to a position corresponding to that of the purified tetramer protein of α2-macroglobulin of size 725 kDa. Reduction of the disulfide bonds of purified α2-macroglobulin protein and α2-macroglobulin molecules in human serum by DTT treatment followed by BN-PAGE and western blotting revealed that α2-macroglobulin molecules in serum were separated completely into monomers of size 182 kDa even in the absence of SDS. Furthermore, neither serum nor purified α2-macroglobulin protein were monomerized following SDS-PAGE due to non-covalent bonding, whereas both were monomerized completely with reduction of disulfide bonds after DTT treatment. These data argue against the current belief based on studies using stored human plasma that two disulfide-bonded α2-macroglobulin dimers are non-covalently bonded to form tetramers in the peripheral blood circulation2,4,5,42.
In some patients with DM whose serum α2-macroglobulin levels were increased markedly, dimeric components were observed in addition to tetramers according to BN-PAGE. Thus, dimers of α2-macroglobulin may be formed in human blood if α2-macroglobulin synthesis is enhanced. Our results demonstrate that the α2-macroglobulin antibody that we used had cross-reactivity with monomers, dimers and tetramers, which could be present in human serum. We compared the results of semiquantitative measurement of serum α2-macroglobulin monomerized after DTT treatment and SDS-PAGE with measurements by ELISA using 40 samples of human serum, and found that both were highly correlated (Fig. 2b). We concluded that our ELISA reflected the circulating components of human α2-macroglobulin molecules.
We also found significantly high serum levels of α2-macroglobulin in DM patients compared with healthy volunteers. Several studies have reported a positive correlation between the HbA1c level and α2-macroglobulin level in serum20,21,22, but we did not. To negate the possibility that blood glucose levels in DM affect serum concentrations of α2-macroglobulin, we obtained the exact glycemic profiles of 57 individuals through 48-h CGM. Neither the mean blood glucose levels of the entire 48-h recordings nor variables of glycemic fluctuation (standard deviation, CV) correlated with serum levels of α2-macroglobulin. Univariate regression analysis of 248 DM patients revealed that the α2-macroglobulin level correlated with the ACR, baPWV, maxIMT, LVPWth, IVSth, but not with the HbA1c level. Serum levels of α2-macroglobulin were significantly higher in DM patients with retinopathy than those without retinopathy. Among these variables, however, multiple regression analysis with the α2-macroglobulin level as the objective variable revealed only the ACR and baPWV to be significant independent variables affecting the serum level of α2-macroglobulin. The association of the urinary albumin concentration with an increased level of this important molecule may be linked to the mechanism by which albuminuria increases the risk of developing cardiac and atherosclerotic diseases.
Albuminuria was originally identified as an incipient marker of diabetic nephropathy43,44, but is now well documented as an independent predictor of cardiovascular morbidity and mortality not only in T1DM and T2DM28,37,45,46, but across varied non-DM populations29,36,47,48. Accumulating evidence suggests that proteinuria is a stronger predictor of cardiovascular disease than traditional risk factors such as cholesterol and blood pressure30,49, whereas albuminuria is associated with an increased risk starting well below the cutoff for microalbuminuria29,48,49. However, the exact pathophysiologic conditions responsible for the overwhelming cardiovascular consequences induced specifically by trace albuminuria, but not in patients without albuminuria, have remained unknown to date.
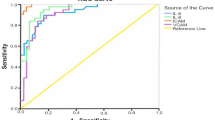
Several mechanisms have been proposed to contribute to the cardiovascular consequences of albuminuria, including inflammation, endothelial dysfunction, thrombogenic factors, and insulin resistance50,51,52,53. In nephrotic syndrome, hepatic synthesis of the high-molecular-weight protein α2-macroglobulin has been shown to be enhanced significantly to replace lost liver-derived proteins in experimental animals54 and humans55, resulting in a net increase in its serum levels54. The present study demonstrated a close correlation between serum levels of α2-macroglobulin and the ACR, and that the former start to rise when a trace amount of albumin is excreted. Considering the magnitude of increased post-transcriptional α2-macroglobulin synthesis in the liver in response to urinary protein excretion54,55,56, it is reasonable to assume that circulating α2-macroglobulin levels may be increased far more profoundly by urinary albumin than by other factors such as sex, age, glycemic control or diabetic retinopathy. A proposed mechanistic link relating albuminuria to increased serum level of α2-macroglobulin and cardiovascular disease in diabetes is depicted in Fig. 4.
Considering the limited number of individuals employed in this cross-sectional study, whether an increased serum level of α2-macroglobulin in diabetes mellitus could serve as a mediator of albuminuria that, ultimately, results in cardiovascular diseases, is not known. Also, whether preventive therapy can reverse albuminuria and reduce the serum level of α2-macroglobulin is not known. Further studies to ascertain if measurement of the serum level of α2-macroglobulin could help to identify patients at a high risk of cardiovascular disease should be carried out.
In conclusion, using a sensitive and specific ELISA, we identified, among other laboratory parameters, a close association between serum levels of α2-macroglobulin with ACR and baPWV. Measurement of serum levels of α2-macroglobulin could help to identify patients at high risk of cardiovascular diseases.
Methods
Study participants
We enrolled 248 patients with DM (39 with T1DM, 204 with T2DM, and 5 with gestational DM) and 59 healthy volunteers at Kitasato University Medical Center or Kitasato University Hospital. Excluded from the analyses were patients with infectious diseases, malignancy, end-stage renal failure, autoimmune thyroid diseases and those receiving corticosteroids. We obtained information on the medical and life histories of all participants.
Patients underwent routine evaluation of systemic diseases covered by the universal health coverage system in Japan57,58. These included electrocardiography (ECG), radiography (chest and abdomen), ultrasonography (neck and/or abdomen), urinalysis, complete blood count, biochemical analyses of serum, as well as tests for levels of free thyroxine, free triiodothyronine, thyroid-stimulating hormone (TSH) and thyroid antibodies. DM patients underwent ophthalmologic and neurologic tests, the anti-glutamic acid decarboxylase antibody test as well as measurements of glycated albumin and/or glycated hemoglobin (HbA1c), fasting serum insulin, and urinary ACR.
Glycemic control/fluctuation was assessed in 54 DM patients without macroalbuminuria (18 males and 36 females; 41.3 ± 13.5 years; HbA1c, 8.0 ± 1.8%) and 3 people without DM (3 females; 40.0 ± 2.6 years; 5.7 ± 0.2%) using 48-h continuous glucose monitoring (CGM) recording (CGMS® GOLD, Medtronic Minimed, Northridge, CA, USA)59,60.
Cardiovascular diseases were diagnosed by ECG, exercise electrocardiography, ankle–brachial pressure index, brachial–ankle pulse wave velocity (baPWV), cardiac catheterization/angiography, and/or coronary computed tomography. For healthy volunteers, the blood-test data at the most recent medical checkup were used to confirm the absence of other systemic diseases and as analytical data.
Collection of serum samples
Blood samples from study participants were collected into vacutainers. Serum was separated immediately in a refrigerated centrifuge and stored in aliquots at −30 °C until processing.
Materials
Purified human α2-macroglobulin protein (725 kDa) was obtained from Enzo Life Science (New York, USA), anti-human monoclonal mouse α2-macroglobulin (immunoglobulin (Ig)G1 clone) from R&D Systems (Minneapolis, MN, USA), and goat anti-mouse IgG (H + L)-horseradish peroxidase (HRP) conjugate from Bio-Rad Laboratories (Hercules, CA, USA). Native PAGE™ Sample Buffer, Native PAGE Running Buffer, Dark Blue Cathode Buffer, Native Mark™ Unstained Protein Standard, and Light Blue Cathode Buffer were obtained from Thermo Fisher Scientific (Waltham, MA, USA). DTT, Blocking One and Peroxidase Stain 3,3′-Diaminobenzidine kit (Brown Stain) were purchased from Nacalai Tesque (Kyoto, Japan). Immune-Blot® polyvinylidene difluoride membrane, Sequi-Blot™ membrane, Precision Plus Protein™ Dual Color Standards and Mini-PROTEAN® TGX™ were obtained from Bio-Rad Laboratories. Perfect NT Gel, Perfect NT Gel System and SDS-PAGE Running Buffer were obtained from DRC (Tokyo, Japan), and ECL Prime Western Blotting Detection Reagent from GE Healthcare (Buckinghamshire, UK).
ELISA of α2-macroglobulin
All measurements were carried out in triplicate. One-hundred microliters of human α2-macroglobulin protein diluted to 0.5–80 ng/mL and serum samples diluted to 1:160,000 with phosphate-buffered saline (PBS) were incubated overnight at 4 °C in a 96-well microplate. Plates were washed thrice and blocked with 200 µL/well of PBS containing 0.05% Tween®20 (PBS-T) and 5% (w/v) skimmed milk/Tris-buffered saline (TBS) for 2 h at room temperature. After washing thrice with PBS-T (200 µL/well), plates were incubated overnight with 100 µL of anti-human monoclonal mouse α2-macroglobulin at 1:5,000 dilution. Then, plates were washed thrice with PBS-T (200 µL/well) and reacted with 1:10,000 goat anti-mouse IgG (H + L)-HRP conjugate (100 µL/well) and allowed to stand at room temperature for 1 h under light-shielding. After washing four times with PBS-T (200 µL/well), o-phenylenediamine/0.05 M phosphate-citrate buffer (100 µL/well) was added for 30 min at room temperature under light-shielding, then overlaid with 3 N HCl (100 µL/well) to terminate the reaction. Absorbance of the plate was measured at 490 nm using a microplate reader (iMark™; Bio-Rad Laboratories).
Polyacrylamide gel electrophoresis (PAGE) followed by western blotting
SDS-PAGE was performed using purified human α2-macroglobulin protein and human serum essentially as described61,62 except for the following modifications. Ten-microliters of fresh human serum diluted to 1:80 and 0.5 µg of purified α2-macroglobulin protein pretreated with or without DTT were subjected to 4–20% gradient gel electrophoresis using Mini-PROTEAN® TGX™ and subsequent immunoblotting using human α2-macroglobulin antibody.
Blue native PAGE was performed as described63 except for the following modifications. Native PAGE™ Sample Buffer was used to dissolve 0.1 µg of standard α2-macroglobulin and to dilute 0.025 µL of serum. After pretreatment with or without 25 mM of DTT, 10 µL of diluted samples was loaded on a 5–20% gradient Perfect NT Gel using Native PAGE Running Buffer as a positive electrode and Dark Blue Cathode Buffer as a negative electrode according to manufacturer instructions. Native Mark™ Unstained Protein Standard was used as a marker of molecular size. After migrating samples at 150 V to one-third of the entire gel, Dark Blue Cathode Buffer in the negative electrode was replaced with Light Blue Cathode Buffer to complete the remaining electrophoresis.
After electrophoresis, the gel was photographed, transferred to a PVDF membrane (Immune-Blot®) at 75 V for 120 min, incubated with 8% acetic acid for 15 min, then with sterilized water for 5 min, and air-dried to fix the protein. The PVDF membrane was then immersed in MeOH to remove Coomassie brilliant blue G-250 dye. Then, it was washed with sterilized water, blocked at 4 °C overnight with Blocking One and, after washing thrice with TBS-T, incubated overnight with human α2-macroglobulin antibody (1:5000 dilution) at 4 °C. After incubation with goat anti-mouse IgG (H + L)-HRP Conjugate (1:10000 dilution) for 1 h, protein bands were detected using ECL and photographed and analyzed with ImageQuant LAS 4000 (GE Healthcare).
Quantitative western blotting to measure levels of monomerized α2-macroglobulin
Serum samples from 40 consecutive DM patients were diluted 40-fold with binding buffer (50 mM DTT, 0.5% SDS, 10% glycerol/1 M Tris-HCl) and subjected to SDS-PAGE with a protein marker (Precision Plus Protein™ Dual Color Standards) using a 5% Perfect NT Gel and a Perfect NT Gel System SDS-PAGE Running Buffer at 120 V for 60–90 min. Proteins in the gels were then transferred to a PVDF membrane (Sequi-Blot™) at 60 mA for 60 min and incubated overnight at 4 °C with Blocking One. After washing thrice with TBS-T, the PVDF membrane was incubated with human α2-macroglobulin antibody (1:3000 dilution) for 90 min, and then with goat anti-mouse IgG(H + L)-HRP Conjugate (1:5000 dilution) for 1 h at room temperature. The PVDF membrane was visualized using Brown Stain. The intensity of each band was quantified using the ImageQuant TL program (GE Healthcare). All densitometric data were converted to relative monomer concentrations using twofold serially diluted samples of control protein.
Statistical analyses
Data are the mean ± SD unless indicated otherwise. Statistical analyses were carried out using JMP v5 (SAS institute, Cary, NC, USA) and Prism 5 (GraphPad Software, La Jolla, CA, USA). Differences between groups were examined for significance using the unpaired t-test. Correlation analysis was undertaken on the relationship between the α2-macroglobulin level and each parameter. Multiple regression analyses were done employing age, sex, diabetic retinopathy, the ACR, estimated glomerular filtration rate (eGFR), baPWV and cardiovascular disease as an explanatory variable and serum level of α2-macroglobulin as an objective variable. P < 0.05 was considered significant.
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committees of Kitasato University Medical Center (Saitama, Japan; 29–27) and Kitasato University Hospital (Kanagawa, Japan; B17-119). All study methods were undertaken in accordance with the relevant guidelines and regulations of these two organizations as well as the Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan. Written informed consent was obtained from all participants.
Data Availability
All data generated or analyzed during this study are included in this article.
References
Talamini, M. A., McCluskey, M. P., Buchman, T. G. & De Maio, A. Expression of alpha2-macroglobulin by the interaction between hepatocytes and endothelial cells in coculture. Am J Physiol 275, R203–211 (1998).
Rehman, A. A., Ahsan, H. & Khan, F. H. Alpha-2-macroglobulin: a physiological guardian. J Cell Physiol 228, 1665–1675 (2013).
Gopal, U., Gonzalez-Gronow, M. & Pizzo, S. V. Activated alpha2-macroglobulin regulates transcriptional activation of c-myc target genes through cell surface GRP78 protein. J Biol Chem 291, 10904–10915 (2016).
Jensen, P. E. & Sottrup-Jensen, L. Primary structure of human alpha 2-macroglobulin. Complete disulfide bridge assignment and localization of two interchain bridges in the dimeric proteinase binding unit. J Biol Chem 261, 15863–15869 (1986).
Sottrup-Jensen, L. et al. The primary structure of alpha 2-macroglobulin and localization of a Factor XIIIa cross-linking site. Ann N Y Acad Sci 421, 41–60 (1983).
Wyatt, A. R., Kumita, J. R., Farrawell, N. E., Dobson, C. M. & Wilson, M. R. Alpha-2-macroglobulin is acutely sensitive to freezing and lyophilization: Implications for structural and functional studies. PLoS One 10, e0130036 (2015).
Mariappan, M., Selvamurugan, N. & Rajamanickam, C. Purification and characterization of a high-molecular-weight protein induced in rat serum during the development of cardiac hypertrophy. Arch Biochem Biophys 281, 287–297 (1990).
Prabhakar, R. & Rajamanickam, C. Serum protein of 135-kDa molecular weight-a molecular signal for cardiac hypertrophy. Arch Biochem Biophys 302, 425–430 (1993).
Rajamanickam, C., Sakthivel, S., Babu, G. J., Lottspeich, F. & Kadenbach, B. Cardiac isoform of alpha-2 macroglobin, a novel serum protein, may induce cardiac hypertrophy in rats. Basic Res Cardiol 96, 23–33 (2001).
Rajan, S., Radhakrishnan, J. & Rajamanickam, C. Direct injection and expression in vivo of full-length cDNA of the cardiac isoform of alpha-2 macroglobulin induces cardiac hypertrophy in the rat heart. Basic Res Cardiol 98, 39–49 (2003).
Annapoorani, P. et al. Cardiac isoform of alpha-2 macroglobulin-a new biomarker for myocardial infarcted diabetic patients. Atherosclerosis 186, 173–176 (2006).
Rajamanickam, C., Sakthivel, S., Kurian Joseph, P. & Athimoolam Janarthanan, R. A novel serum protein of molecular weight 182 kDa: a molecular marker for an early detection of increased left ventricular mass in patients with cardiac hypertrophy. J Cardiovasc Risk 5, 335–338 (1998).
Soman, S., Manju, C. S., Rauf, A. A., Indira, M. & Rajamanickam, C. Role of cardiac isoform of alpha-2 macroglobulin in diabetic myocardium. Mol Cell Biochem 350, 229–235 (2011).
Takada, T. et al. Serum monomeric alpha2-macroglobulin as a clinical biomarker in diabetes. Atherosclerosis 228, 270–276 (2013).
Ganrot, P. O. & Scherstén, B. Serum α2-macroglobulin concentration and its variation with age and sex. Clin Chim Acta 15, 113–120 (1967).
Tunstall, A. M., Merriman, J. M., Milne, I. & James, K. Normal and pathological serum levels of alpha2-macroglobulins in men and mice. J Clin Pathol 28, 133–139 (1975).
Ahmad, J., Singh, M. & Saleemuddin, M. A study of plasma alpha-2-macroglobulin levels in type 2 diabetic subjects with microalbuminuria. J Assoc Physicians India 49, 1062–1065 (2001).
Ceriello, A. et al. Increased alpha 2-macroglobulin in diabetes: a hyperglycemia related phenomenon associated with reduced antithrombin III activity. Acta Diabetol Lat 26, 147–154 (1989).
Gray, R. S. et al. Alpha 2-macroglobulin and proliferative retinopathy in type 1 diabetes. Horm Metab Res 14, 389–392 (1982).
James, K., Merriman, J., Gray, R. S., Duncan, L. J. & Herd, R. Serum alpha 2-macroglobulin levels in diabetes. J Clin Pathol 33, 163–166 (1980).
Lisowska-Myjak, B., Pachecka, J., Kaczynska, B., Miszkurka, G. & Kadziela, K. Serum protease inhibitor concentrations and total antitrypsin activity in diabetic and non-diabetic children during adolescence. Acta Diabetol 43, 88–92 (2006).
Chung, T. J. et al. Association of salivary alpha 2-macroglobulin levels and clinical characteristics in type 2 diabetes. J Diabetes Investig 7, 190–196 (2016).
Dursun, E. et al. The interleukin 1 alpha, interleukin 1 beta, interleukin 6 and alpha-2-macroglobulin serum levels in patients with early or late onset Alzheimer’s disease, mild cognitive impairment or Parkinson’s disease. J Neuroimmunol 283, 50–57 (2015).
Meenakshisundaram, R., Sweni, S. & Thirumalaikolundusubramanian, P. Cardiac isoform of alpha 2 macroglobulin: a marker of cardiac involvement in pediatric HIV and AIDS. Pediatr Cardiol 31, 203–207 (2010).
Zabel, M. et al. Assessing candidate serum biomarkers for Alzheimer’s disease: a longitudinal study. J Alzheimers Dis 30, 311–321 (2012).
Thieme, R. et al. Analysis of alpha-2 macroglobulin from the long-lived and cancer-resistant naked mole-rat and human plasma. PLoS One 10, e0130470 (2015).
Varma, V. R. et al. Alpha-2 macroglobulin in Alzheimer’s disease: a marker of neuronal injury through the RCAN1 pathway. Mol Psychiatry 22, 13–23 (2017).
de Zeeuw, D. et al. Albuminuria, a therapeutic target for cardiovascular protection in type 2 diabetic patients with nephropathy. Circulation 110, 921–927 (2004).
Gerstein, H. C. et al. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA 286, 421–426 (2001).
Ljungman, S., Wikstrand, J., Hartford, M. & Berglund, G. Urinary albumin excretion-a predictor of risk of cardiovascular disease. A prospective 10-year follow-up of middle-aged nondiabetic normal and hypertensive men. Am J Hypertens 9, 770–778 (1996).
Tuomilehto, J. et al. Incidence of cardiovascular disease in Type 1 (insulin-dependent) diabetic subjects with and without diabetic nephropathy in Finland. Diabetologia 41, 784–790 (1998).
Deckert, T. et al. Cohort study of predictive value of urinary albumin excretion for atherosclerotic vascular disease in patients with insulin dependent diabetes. BMJ 312, 871–874 (1996).
Jansson, F. J. et al. Regression of albuminuria and its association with incident cardiovascular outcomes and mortality in type 1 diabetes: the FinnDiane Study. Diabetologia 61, 1203–1211 (2018).
Borch-Johnsen, K. & Kreiner, S. Proteinuria: value as predictor of cardiovascular mortality in insulin dependent diabetes mellitus. BMJ 294, 1651–1654 (1987).
Groop, P. H. et al. The presence and severity of chronic kidney disease predicts all-cause mortality in type 1 diabetes. Diabetes 58, 1651–1658 (2009).
Hillege, H. L. et al. Urinary albumin excretion predicts cardiovascular and noncardiovascular mortality in general population. Circulation 106, 1777–1782 (2002).
Rossing, P., Hougaard, P., Borch-Johnsen, K. & Parving, H. H. Predictors of mortality in insulin dependent diabetes: 10 year observational follow up study. BMJ 313, 779–784 (1996).
Brownlee, M. α2- macroglobulin and reduced basement -membrane degradation inn diabetes. Lancet 307, 779–780 (1976).
Hubbard, W. J. Alpha-2 macroglobulin-enzyme complexes as suppressors of cellular activity. Cell Immunol 39, 388–394 (1978).
Koo, P. H. Human alpha 2-macroglobulin: a major serum factor cytotoxic for tumor cells. Cancer Lett 18, 169–177 (1983).
Tiggelman, A. M., Linthorst, C., Boers, W., Brand, H. S. & Chamuleau, R. A. Transforming growth factor-beta-induced collagen synthesis by human liver myofibroblasts is inhibited by alpha2-macroglobulin. J Hepatol 26, 1220–1228 (1997).
Marrero, A. et al. The crystal structure of human alpha2-macroglobulin reveals a unique molecular cage. Angew Chem Int Ed Engl 51, 3340–3344 (2012).
Mogensen, C. E. Microalbuminuria predicts clinical proteinuria and early mortality in maturity-onset diabetes. N Engl J Med 310, 356–360 (1984).
Viberti, G. C. et al. Microalbuminuria as a predictor of clinical nephropathy in insulin-dependent diabetes mellitus. Lancet 1, 1430–1432 (1982).
Dinneen, S. F. & Gerstein, H. C. The association of microalbuminuria and mortality in non-insulin-dependent diabetes mellitus. A systematic overview of the literature. Arch Intern Med 157, 1413–1418 (1997).
Morrish, N. J., Stevens, L. K., Fuller, J. H., Jarrett, R. J. & Keen, H. Risk factors for macrovascular disease in diabetes mellitus: the London follow-up to the WHO Multinational Study of Vascular Disease in Diabetics. Diabetologia 34, 590–594 (1991).
Damsgaard, E. M., Froland, A., Jorgensen, O. D. & Mogensen, C. E. Microalbuminuria as predictor of increased mortality in elderly people. BMJ 300, 297–300 (1990).
Wachtell, K. et al. Albuminuria and cardiovascular risk in hypertensive patients with left ventricular hypertrophy: the LIFE study. Ann Intern Med 139, 901–906 (2003).
Perkovic, V. et al. The relationship between proteinuria and coronary risk: a systematic review and meta-analysis. PLoS Med 5, e207 (2008).
Deckert, T., Feldt-Rasmussen, B., Borch-Johnsen, K., Jensen, T. & Kofoed-Enevoldsen, A. Albuminuria reflects widespread vascular damage. The Steno hypothesis. Diabetologia 32, 219–226 (1989).
Mykkanen, L. et al. Microalbuminuria is associated with insulin resistance in nondiabetic subjects: the insulin resistance atherosclerosis study. Diabetes 47, 793–800 (1998).
Pedrinelli, R. et al. Microalbuminuria and endothelial dysfunction in essential hypertension. Lancet 344, 14–18 (1994).
Stehouwer, C. D. et al. Increased urinary albumin excretion, endothelial dysfunction, and chronic low-grade inflammation in type 2 diabetes: progressive, interrelated, and independently associated with risk of death. Diabetes 51, 1157–1165 (2002).
Stevenson, F. T., Greene, S. & Kaysen, G. A. Serum alpha 2-macroglobulin and alpha 1-inhibitor 3 concentrations are increased in hypoalbuminemia by post-transcriptional mechanisms. Kidney Int 53, 67–75 (1998).
de Sain-van der Velden, M. G. et al. Plasma alpha 2 macroglobulin is increased in nephrotic patients as a result of increased synthesis alone. Kidney Int 54, 530–535 (1998).
de Sain-van der Velden, M. G. et al. Nephrotic proteinuria has No net effect on total body protein synthesis: measurements with (13)C valine. Am J Kidney Dis 35, 1149–1154 (2000).
Chida, S. et al. Levels of albuminuria and risk of developing macroalbuminuria in type 2 diabetes: historical cohort study. Sci Rep 6, 26380 (2016).
Kamata, Y. et al. Distinct clinical characteristics and therapeutic modalities for diabetic ketoacidosis in type 1 and type 2 diabetes mellitus. J Diabetes Compl 31, 468–472 (2017).
Ogawa, A. et al. New indices for predicting glycaemic variability. PLoS One 7, e46517 (2012).
Hayashi, A. et al. Distinct biomarker roles for HbA1c and glycated albumin in patients with type 2 diabetes on hemodialysis. J Diabetes Compl 30, 1494–1499 (2016).
Shichiri, M., Nonaka, D., Lee, L. J. & Tanaka, K. Identification of the salusin-beta receptor using proteoliposomes embedded with endogenous membrane proteins. Sci Rep 8, 17865 (2018).
Tani, Y., Yamada, S., Inoshita, N., Hirata, Y. & Shichiri, M. Regulation of growth hormone secretion by (pro)renin receptor. Sci Rep 5, 10878 (2015).
Hoshiyama, A. et al. Identification of plasma binding proteins for glucose-dependent insulinotropic polypeptide. Endocrine J, in press (2019).
Acknowledgements
The authors thank Yukiko Kato for her assistance with quantification of α2-macroglobulin using western blotting. This work was supported in part by Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan to M.S. (18H05383), Y.Ko. (17K19926) and K.F. (18K15431), by the Parents’ Association Grant of Kitasato University School of Medicine to S.Y. and by Kitasato University ‘Shogaku-Kifu’ research support to M.S. The latter’s support arose originally from Sanofi K.K., Shionogi & Co. Ltd., Pfizer Academic Contributions, Astellas Academic Support, Taisho Toyama Pharmaceutical Co. Ltd. Japan Boehringer Ingelheim Life Science Research Support and Ono Pharmaceuticals. The funders had no role in the study design, data collection or analysis, decision to publish, or preparation of the manuscript. No additional external funding was received for this study. We thank Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
S.Y. and K.F. processed serum samples, established the ELISA and measured α2-macroglobulin levels in serum. T.T. and J.O. collected serum samples and clinical information on DM patients. Y. Ka. and M.S. collected serum samples from patients with DM, evaluated their clinical course and confirmed the final diagnoses. S.Y., K.F., S.K. and Y. Ko. undertook native gel electrophoresis and confirmed circulating levels of α2-macroglobulin. S.Y., J.O. and T.T. undertook statistical analyses and M.S. confirmed the results. M.S. conceived experiments, analyzed data and secured funding. M.S. wrote, reviewed and edited the manuscript. All authors discussed the results and commented on the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yoshino, S., Fujimoto, K., Takada, T. et al. Molecular form and concentration of serum α2-macroglobulin in diabetes. Sci Rep 9, 12927 (2019). https://doi.org/10.1038/s41598-019-49144-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-019-49144-7
This article is cited by
-
Matrix metalloproteinases in arthritis: towards precision medicine
Nature Reviews Rheumatology (2023)
-
Plasma markers of COVID-19 severity: a pilot study
Respiratory Research (2022)
-
Major trace elements and their binding proteins in the early phase of Covid-19 infection
JBIC Journal of Biological Inorganic Chemistry (2022)
-
Suprabasin-derived bioactive peptides identified by plasma peptidomics
Scientific Reports (2021)
-
Circulating prorenin: its molecular forms and plasma concentrations
Hypertension Research (2021)