Abstract
In Japan, the governmental recommnendation of HPV vaccine has been suspended since June 2013, due to media reports of alleged adverse vaccination events. Although evidence of effectiveness and safety of the HPV vaccine has been universally demonstrated, and the medical and academic organizations across Japan have requested the resumption of the government’s recommendation, the Japanese government has not changed their official stance towards the HPV vaccine. Under the current suspension of the national government’s recommendation, one local government Isumi City started sending a leaflet containing information of cervical cancer and HPV vaccine, but not recommendation for the vaccine, to the tagted girls born in the fiscal year (FY) 2003. The cumulative vaccination rate of them reached 10.07% (14/139), which was significantly higher than that (0.00%) for girls born in FY 2002 who did not receive such a leaflet (p < 0.001). We sincerely ask the national government to change their stance towards the HPV vaccine. We also strongly suggest that, in the meantime, local governments immediately begin to provide an appropriate information of cervical cancer and HPV vaccine to the targeted girls and their parents in a way similar to what Isumi City has now shown to be effective.
Similar content being viewed by others
Introduction
The majority of cervical cancer cases can be easily preventable by a combination of HPV vaccination and routine cervical cancer screening. Despite this fact, we have previously shown that the age-adjusted incidence of cervical cancer in Japan has been steadily increasing since 20001. The cervical cancer screening rate in Japan has become extremely low, as compared to other developed countries over the same period. The screening rate for young women at the age of 20–24 is currently only around 10%, and even in females aged 25–29 and 30–39, the screening rate is only around 10–20% and around 10–30%, respectively2. Low inoculation rate of HPV vaccine is another issue to overcome to reduce cervical cancer incidence.
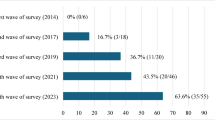
Financial support from the Japanese government for HPV vaccination for girls aged 13–16 began in the fiscal year (FY: April–March) 20103. Females born between FY 1994 and FY 1999 have enjoyed rates of vaccination protection approaching 70%, although the vaccination was not free4,5,6. In April 2013, HPV vaccination became a part of the routine immunization program, meaning that thereafter females aged 12–16 could receive the vaccination for free. News stories related to cervical cancer prevention such as risk of developing cervical cancer, its etiology, and the effects of vaccination frequently appeared in the media until 2012, however, after March 2013 they were replaced with anti-vaccination contents7. Due to repeated media reports of alleged adverse vaccination events, the Ministry of Health, Labour and Welfare (MHLW) suspended its recommendation for the HPV vaccine in June 2013. For girls born in or after 2000 in Japan, who reached the age for vaccination after suspension of the governmental recommendation, their HPV vaccination rates have been declined, despite the vaccination was still free3. The cumulative vaccination rates for girls born in FY2000, FY2001, FY 2002 and FY2003 were reported to be 14.3%, 1.6%, 0.4% and 0.2%, respectively8. In Japan, parental consent is required for their daughter’s HPV vaccination, and our previous internet survey suggested that acceptance or refusal of the HPV vaccine was determined predominantly by the mother's perceptions of risk versus benefits, rather than the daughter's wishes in Japan9.
Protective effect of HPV vaccine against cervical cancer or its precancerous lesion of the cervix has been shown not only from overseas10 but also in Japan11,12, and safety of HPV vaccine has been also internationally and domestically demonstrated13,14. The medical and academic organizations across Japan have requested the resumption of the government’s recommendation;15 nevertheless the MHLW has not changed their official stance towards the HPV vaccine. Although the HPV vaccine is still regarded as a ‘routine vaccination’ in Japan, the national government still does not ‘officially recommend’ it. In addition, neither more potent 9-valent HPV vaccine nor immunization for boys have been approved yet in a national routine immunization program3,16. Moreover, seven years have now passed since the announcement of the governmental suspension of the HPV vaccine recommendation. We have already reported that Japanese mothers’ intentions to have their daughters vaccinated have been further eroded over this period17.
Under these dire circumstances, we must find a way to re-disseminate HPV vaccination nationwide as a countermeasure against the recent increase of cervical cancer among young women1. A recent survey conducted by the MHLW found that only 5.6% of all local governments across the nation (97/1741), under the current suspension of the government’s recommendation, sent leaflets containing only information of HPV vaccine, but not recommendation for the vaccine, individually to the girls and their parents18. In the present study, we have analyzed the effectiveness of one type of leaflet that one local government, not on a national basis, has been sending to individuals of HPV vaccination age or to their parents under the governmental suspension of the HPV vaccine recommendation.
Methods
Isumi City is a small municipality, with a population of 38,000 (Table 1)19. On July 29, 2019, the Isumi City government started sending an informational/educational leaflet (Table 2 and Supplementary Figure), which addressed the risks of cervical cancer and the role of the HPV vaccine in its prevention, to all 139 girls who were born in FY 2003 and reached 16 years old at that time. The present study was a population-based analysis to compare the first vaccination rates before and after this project, and necessary data on monthly vaccination numbers of girls in the targeted age group was provided by the Division of Health Promotion and Senior Services, Isumi City.
Written informed consent was obtained to use their personal data regarding HPV vaccination for the girls who got immunized in FY 2019. There was only one person whose informed consent was not obtained and excluded from the analysis. In contrast, for the girls who got immunized by FY 2018, informed consent was obtained through opt-out methods. It was shown as < 10 if the number of girls who was vaccinated is less than 10 before and in FY 2018, in view of not revealing personal information based on the ethical regulation for epidemiological research in Japan. Likewise, the total number of targeted girls in each FY was also withheld, so that each girl is not to be identified personally.
Statistics
The rates of HPV vaccination were compared by Fisher’s exact test. The level of statistical significance was set at p = 0.05.
Ethical statement
This study was approved by the Institutional Review Board and Ethics Committee of the Osaka University Medical Hospital (#13261-9). We conducted the present study in accordance with relevant guidelines and regulations.
Statement of significance
Under the current suspension of the national government’s recommendation of HPV vaccine, providing an appropriate information of cervical cancer and HPV vaccine to the targeted girls and their parents from a local government was shown to be effective.
Results
When the Japanese government was actively promoting the vaccine, the cumulative rates of the first (of three) vaccination shots in the targeted girls born between FY 1994 and FY 1999 substantially increased from 58.60 to 94.67% (Table 3). However, beginning in 2013, when the government withdrew its recommenadtion, the vaccination rates in Isumi City dropped dramatically, and none of the girls born in FY 2001 or 2002 received vaccination by the beginning of FY 2019, although the HPV vaccine was still regarded in Japan as a ‘routine vaccination’ and people can be immunized in medical facilities on request at any time.
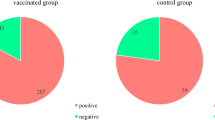
In response, the Isumi City government started on July 29, 2019 sending an informational/educational leaflet which explained the risks of cervical cancer and role the HPV vaccine in its prevention, to all 139 girls who were born in FY 2003 and reached 16 years old at that time. FY 2019 was the last one when those girls could get HPV vaccination. Only 2 girls born in FY 2003 in the city had been vaccinated prior to the individual leaflet/notification. After receiving the leaflet, 12 girls got immunized (Fig. 1). The cumulative vaccination rate significantly increased from 1.44 (2/139) to 10.07% (14/139) (p = 0.003). Subsequently, the cumulative vaccination rate for girls born in FY 2003 in Isumi City reached 10.07% (14/139) by December 31, 2019, which was significantly higher than that (0.00%) for girls born in FY 2002 who did not receive such a leaflet (p < 0.001) (Table 3).
On the other hand, out of 489 girls born later in FY 2004–2007, who were also the targets of HPV vaccine but did not receive the individual notification/leaflet, only 6 girls had been vaccinated by December 31, 2019. This proportion 1.23% (6/489) for those born in FY 2004–2007 was significantly smaller than the rate 10.07% for the girls born in FY 2003 who received the leaflet (14/139) (p < 0.001), while it did not show significant difference from the rate 0.00% (0/148) for the girls born in FY 2002 (p = 0.34). Moreover, in 2019, 3 girls born in FY 2004–2007 received the HPV vaccine between April and July without information leaflet, and another 3 girls received it between August and December, however the cumulative vaccination rate did not increase significantly throughout the year (3/489 to 6/489, p = 0.51).
These results indicated that increase in the HPV vaccination rate among the targeted girls born in FY 2003 was strongly influenced by the leaflet sent individually by the local government, as long as no other factors, such as mothers’ change in awareness for vaccination for their daughters, seemed to make impact in our analysis.
Discussion
The World Health Organization (WHO) regarded vaccine hesitancy, the reluctance or refusal to vaccinate despite the availability of vaccines, as one of the 10 threats to global health in 201920. Mechanisms of HPV vaccine hesitancy after the suspension of the governmental recommendation at first were explained from the viewpoints of behavioral economics21. Lack of information on HPV vaccine in the targeted girls and their parents has become an additional barrier because only 5.6% of all the local governments across the nation sent certain types of leaflets containing information on HPV vaccine individually to the girls and their parents inside the municipality under the suspension of the governmental recommendation18. Any promotional activities of HPV vaccine have not been conducted to increase HPV vaccination rates by local governments, doctors, and school teachers, because of suspension.
Sending individually an information leaflet about cervical cancer and HPV vaccination from a local government to the targeted girls and their parents appeared to be effective for promoting HPV vaccination. By the first of FY2020, females born in FYs 2000, 2001, 2002 and 2003 were already over 12–16, the targeted ages for the vaccine. Future risk of cervical cancer for girls born in FY 2004 will significantly increase in FY 2020 when they become 16 years old, which is the last year for routine HPV vaccination22,23, unless the government's recommendations for HPV vaccination are reinstated. We sincerely ask the national government to change their stance towards the HPV vaccine. We also strongly suggest that, in the meantime, local governments could immediately begin, even if it is still under the current circumstances of the suspension of the governmental recommendation, to provide an appropriate information of cervical cancer and HPV vaccine to the targeted girls and their parents in such a way that Isumi City has now proven it useful. Up until now, there have not been any other reports to demonstrate the effectiveness of sending an information leaflet by local governments in Japan.
A previous internet survey conducted by the MHLW found that 38.8% of the tagted girls had not heard of significance and safety of HPV vaccine at all, and that 33.8% of the mothers of the targeted girls wanted to get appropreate information at the consultation counter of a local government17. Moreover, 45.0% of the targeted girls and 38.4% of thier mothers replied that they could not decide whether to receive the HPV vaccine because they did not have adequate knowledge about HPV vaccine well. In Japan, mothers play more important roles for decision of their daughters’ vaccination9. Fathers' participation in the mothers' decision-making did not increase the likelihood of HPV vaccination for their daughters, however, an educational leaflet was proved to be effective to enhance fathers’ enrollment for decision of their daughters’ vaccination24.
We believe that providing an appropriate information of cervical cancer and HPV vaccine to the targeted girls and their parents, which can be conducted under the current circumstances, is a potentially effective tool to support decision-making of HPV vaccination for the targetted girls and their mothers, and it is educational as well for their knowledge and attitudes toward cervical cancer. It was demonstrated that effectiveness was enhanced when doctors explained about HPV vaccine using with informational leaflet, probably due to proper opportunities to understand the content well and ask questions25. Improvement of the contents of leaflets by taking viewpoints of behavioral economics might further increase HPV vaccination rates21. There was a report that secondary acceptance of HPV vaccination by the parents of adolescents is more common than we might suppose26. We could improve vaccination rate more if we consider this possibility and repeat providing the leaflets. We suppose that this is the last strategy for re-dissemination of HPV vaccination in Japan while still under the suspension of the governmental recommendation We will no longer overlook this situation.
Abbreviations
- FY:
-
Fiscal year
- HPV:
-
Human papillomavirus
- MHLW:
-
Ministry of Health, Labour and Welfare
- WHO:
-
World Health Organization
References
Yagi, A. et al. Epidemiologic and clinical analysis of cervical cancer using data from the population-based Osaka Cancer Registry. Cancer Res. 79, 1252–1259 (2019).
Comprehensive Survey of Living Conditions. The Ministry of Health, Labor and Welfare, Japan (Accessed 5 April 2020); https://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa18/index.html
Ikeda, S. et al. HPV vaccination in Japan: what is happening in Japan?. Expert Rev. Vaccines 18, 323–325 (2019).
Ueda, Y. et al. Japan’s failure to vaccinate girls against human papillomavirus. Am. J. Obstet. Gynecol. 212, 405–406 (2015).
Hanley, S. J. et al. HPV vaccination crisis in Japan. Lancet 385, 2571 (2015).
Sekine, M. et al. Japanese crisis of HPV vaccination. Int. J. Pathol. Clin. Res. 2, 039 (2016).
Okuhara, T., Ishikawa, H., Okada, M., Kato, M. & Kiuchi, T. Newspaper coverage before and after the HPV vaccination crisis began in Japan: a text mining analysis. BMC Public Health 19, 770 (2019).
Nakagawa, S. et al. Corrected human papillomavirus vaccination rates for each birth fiscal year in Japan. Cancer Sci. 111, 2156–2162 (2020).
Egawa-Takata, T. et al. Survey of Japanese mothers of daughters eligible for human papillomavirus vaccination on attitudes about media reports of adverse events and the suspension of governmental recommendation for vaccination. J. Obstet. Gynaecol. Res. 41, 1965–1971 (2015).
Luostarinen, T. et al. Vaccination protects against invasive HPV-associated cancers. Int. J. Cancer 142, 2186–2187 (2018).
Ueda, Y. et al. Dynamic changes in Japan’s prevalence of abnormal findings in cervical cytology depending on birth year. Sci. Rep. 8, 5612 (2018).
Yagi, A. et al. Evaluation of future cervical cancer risk in Japan, based on birth year. Vaccine 37, 2889–2891 (2019).
Suzuki, S. & Hosono, A. No association between HPV vaccine and reported post-vaccination symptoms in Japanese young women: results of the Nagoya study. Papillomavirus Res. 5, 96–103 (2018).
Arbyn, M. & Xu, L. Efficacy and safety of prophylactic HPV vaccines: a cochrane review of randomized trials. Expert Rev. Vaccines 17, 1085–1091 (2018).
Iwata, S., Okada, K., Kawana, K. & Expert Council on Promotion of Vaccination. Consensus statement from 17 relevant Japanese academic societies on the promotion of the human papillomavirus vaccine. Vaccine 35, 2291–2292 (2017).
Ueda, Y., Yagi, A., Ikeda, S., Enomoto, T. & Kimura, T. Beyond resumption of the Japanese Government’s recommendation of the HPV vaccine. Lancet Oncol. 19, 1563–1564 (2018).
Yagi, A. et al. Time-dependent changes of the intention of mothers in Japan to inoculate their daughters with the HPV vaccine after suspension of governmental recommendation. Hum. Vaccines Immunother. 14, 2497–2502 (2018).
The Council of the MHLW (Accessed 5 April 2020); https://www.mhlw.go.jp/stf/newpage_06462.html
Ministry of Internal Affairs and Communications (Accessed 1 Aug 2020); https://www.soumu.go.jp/main_content/000633314.pdf#search=%27%E7%94%9F%E7%94%A3%E5%B9%B4%E9%BD%A2%E4%BA%BA%E4%BD%8F%E6%B0%91+%E4%BA%BA%E5%8F%A3+%E4%B8%96%E5%B8%AF%E6%95%B0%27
WHO: Ten threats to global health in 2019 (Accessed 1 Aug 2020); https://www.who.int/news-room/feature-stories/ten-threats-to-global-health-in-2019
Yagi, A., Ueda, Y. & Kimura, T. A behavioral economics approach to the failed HPV vaccination program in Japan. Vaccine 35, 6931–6933 (2017).
Tanaka, Y. et al. Outcomes for girls without HPV vaccination in Japan. Lancet Oncol. 17, 868–869 (2016).
Yagi, A. et al. Realistic fear of cervical cancer risk in Japan depending on birth year. Hum. Vaccines Immunother. 13, 1700–1704 (2017).
Egawa-Takata, T. et al. Fathers’ participation in the HPV vaccination decision-making process doesn’t increase parents’ intention to make daughters get the vaccine. Hum. Vaccines Immunother. https://doi.org/10.1080/21645515.2019.1697107 (2020).
Shiomi, M. et al. A survey of Japanese mothers on the effectiveness of the Ministry of Health, Labor and Welfare’s revised HPV vaccine leaflet. Hum. Vaccines Immunother. https://doi.org/10.1080/21645515.2020.1723362 (2020).
Kornides, M. L., McRee, A. L. & Gilkey, M. B. Parents who decline HPV vaccination: who later accepts and why?. Acad. Pediatr. 18(2S), S37–S43 (2018).
Acknowledgements
We would like to thank Dr. G. S. Buzard for his constructive critique and editing of our manuscript, and equally, the officials of the Division of Health Promotion and Senior Services, Isumi City Hall, Chiba, Japan for their support.
Funding
This study was supported by a Grant from the Japanese Agency for Medical Research and Development (AMED 20ck0106562h0001).
Author information
Authors and Affiliations
Contributions
Y.U., A.Y., A.M. and H.K. created the research plan and collected the data. Y.U. analyzed the raw data. All the authors analyzed the final data. Y.U. wrote the manuscript. Y.U. and R.M. revised the manuscript. All the authors approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
AY and YU received a lecture fee, and YU received a research Grant (J550703673), from Merck Sharp & Dohme (MSD). TK received a research fund (VT#55166) from Merck Sharp & Dohme (MSD). The other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ueda, Y., Yagi, A., Abe, H. et al. The last strategy for re-dissemination of HPV vaccination in Japan while still under the suspension of the governmental recommendation. Sci Rep 10, 16091 (2020). https://doi.org/10.1038/s41598-020-73120-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-020-73120-1
This article is cited by
-
The impact of medical expert-led sex education on sexual health knowledge among Japanese junior high school students: a quantitative study
BMC Public Health (2025)
-
Change of HPV vaccination rates in Japan: the effect of individual notifications implemented by local governments
International Journal of Clinical Oncology (2022)
-
Attitudes and behaviors of obstetricians and gynecologists toward HPV vaccination: a 7-year follow-up survey in Japan
International Journal of Clinical Oncology (2022)