Abstract
Many bariatric procedures are more effective for improving type-2 diabetes mellitus (T2DM) than conventional pharmacotherapy. The current research evaluated factors linked to complete and partial remission or improvement of T2DM after laparoscopic sleeve gastrectomy (LSG). The current prospective study included all diabetic patients who were submitted LSG between January 2015 and June 2018 and completed a 2-year follow-up period. Patients were assessed at baseline and 2 years after LSG. This work comprised of 226 diabetic cases. Two years after LSG, 86 patients (38.1%) achieved complete remission of DM, and 24 (10.6%) reached partial remission. Only 14 patients (6.2%) showed no change in their diabetic status. On univariate analysis, age ≤ 45 years, duration of diabetes ≤ 5 years, use of a single oral antidiabetic, HbA1c ≤ 6.5%, HOMA-IR ≤ 4.6, C-peptide > 2.72 ng/mL, and BMI ≤ 40 kg/m2 predicted complete remission. The independent predictors of complete remission were age ≤ 45 years, duration of diabetes ≤ 5 years, use of a single oral antidiabetic, HOMA-IR ≤ 4.6, and C-peptide > 2.72 ng/mL. A combined marker of young age, short duration of DM, and low HOMA-IR predicted complete remission with sensitivity 93% and specificity 82%. Independent predictors of complete remission of T2DM after LSG were younger age, shorter duration, single oral antidiabetic, lower HOMA-IR, and higher C-peptide.
Similar content being viewed by others
Introduction
In 1997, obesity was declared an epidemic by the World Health Organization1; however, its prevalence is increasing worldwide. It is estimated that over 2 billion adults, i.e., about 39% of human beings, were overweight or obese in 20162. The burden of obesity is aggravated by its associated comorbidities as type 2-diabetes mellitus (T2DM) and cardiovascular diseases (CVD), among others3. The increase in obesity rates seems to be the main factor for the recent surge in the prevalence of T2DM4. About 44% of the burden of T2DM is attributable to overweight and obesity5, and 9.5% of all body mass index-related deaths were due to diabetes in obese patients4.
Despite efforts through lifestyle interventions to treat obesity and T2DM, only a minority of patients achieved long-term weight loss and glycemic targets6. There is a reasonable body of evidence to confirm that many bariatric procedures are more effective than conventional pharmacotherapy for improvement or even inducing complete remission of T2DM7,8,9,10. These procedures include Roux-en-Y gastric bypass11, sleeve gastrectomy12, and duodenal switch/biliopancreatic diversion13.
Recently, laparoscopic sleeve gastrectomy (LSG) turned into the most popular bariatric operation in many parts of the world14. The current analysis aimed to assess the possible factors linked to complete and partial remission or improvement of T2DM after laparoscopic sleeve gastrectomy (LSG).
Patients and methods
This prospective work included patients who were submitted LSG between January 2015 and June 2018. The ethics committee approved the study at the Cairo University Hospitals. All methods were performed in accordance with the relevant guidelines and regulations. Besides, written informed consent was obtained from all subjects.
Inclusion criteria were subjects with T2DM, aged 18–65 years, with BMI ≥ 35. Exclusion criteria were subjects who had revisional LSG and those with type-1 diabetes mellitus.
Patients were reviewed at baseline and 2 years after LSG. Data registered were demographic and anthropometric (age, sex, weight), laboratory (fasting blood glucose, HbA1c, C-peptide, insulin level), and clinical (insulin and/or oral medications, diabetes duration, the existence of elevated blood pressure, hyperlipidemia) characteristics. Percent weight loss and BMI change were obtained using the previously reported methods15. Insulin resistance was calculated by the homeostasis model assessment of insulin resistance (HOMA-IR)16.
The current analysis adopted the standardized American Society of Bariatric and Metabolic Surgery definitions of evolution of T2D post-bariatric procedures17 (Table 1).
The operation began with the division of gastrosplenic ligament along the greater curvature 4 cm from the pylorus up to the left diaphragmatic crus with ultrasonic shears18. The stomach was then mobilized and divided along the lesser curvature from antrum (4 cm from pylorus) till reaching the angle of His using buttressed (SeamGuard, Gore, Inc., Flagstaff, Arizona, USA) linear 60-mm stapler (Covidien Tristapler, Medtronic, Minneapolis, Minnesota, USA) over the calibration tube (Midsleeve 36 Fr) introduced into the gastric lumen18. The specimen was extracted through the umbilical port. The operation was ended with a methylene blue leak testing.
Statistical analysis was performed using IBM SPSS Statistics version 22 (IBM Corp., Armonk, NY, USA). The power of the test used for primary outcome measure was estimated using the G Power software (Institutfür Experimentelle Psychologie, Heinrich Heine Universität, Düsseldorf, Germany) version 3.1.9.2. Numerical variables were calculated as mean and standard deviation or median and range as appropriate. Qualitative variables were calculated as frequency and percentage. Chi-square test (Fisher’s exact test) was used to examine the relation between qualitative variables. For quantitative variables, comparison between two arms was made using independent sample t-test or Mann–Whitney test. Multivariate analysis was performed using logistic regression method for the significant factors found on univariate analysis. Odds ratio (OR) with its 95% confidence interval (CI) were used for risk estimation. A p-value < 0.05 was considered significant.
Consent to participate
Consents were done for all enrolled cases.
Results
At the start of the study, 254 patients were included, however, only 226 completed the follow-up. Only those who completed the follow-up were included in the analysis.
Table 2 shows the baseline data of the 226 patients of the studied group. Hypertension and dyslipidemia were common comorbidities. Near 40% of the studied group received insulin for glycemic control.
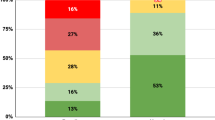
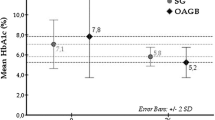
Two years after LSG, 86 patients (38.1%) achieved complete remission of DM, and 24 (10.6%) reached partial remission. Besides, improvement of diabetes occurred in 102 patients (45.1%). Only 14 patients (6.2%) showed no change in their diabetic status. More than half of those with hypertension and dyslipidemia got resolution of the disease (Table 3).
Table 4 shows a significant difference between patients who developed complete remission of T2DM and those who did not, in all pre-and postoperative characteristics except sex, hypertension, dyslipidemia, insulin therapy, and preoperative weight.
On univariate analysis, predictive factors for complete remission were age ≤ 45 years, duration of diabetes ≤ 5 years, use of a single oral antidiabetic, HbA1c ≤ 6.5%, HOMA-IR ≤ 4.6, C-peptide > 2.72 ng/mL, and BMI ≤ 40 kg/m2 (Table 5). Using logistic regression, the independent predictors of complete remission were age ≤ 45 years, duration of diabetes ≤ 5 years, use of a single oral antidiabetic, HOMA-IR ≤ 4.6, and C-peptide > 2.72 ng/mL (Table 6). A combined marker of young age, short duration of DM, and low HOMA-IR provide a very good prediction of complete remission with sensitivity 93% and specificity 82%.
Discussion
Several reports have confirmed bariatric surgery’s effectiveness in resolving type-2 diabetes with a diverse remission rate and/or improvement rate. Many studies have proposed predictors of remission of diabetes after weight-loss operations19,20,21,22,23,24,25,26,27. Others introduced scores for such predictors28,29,30,31,32,33. The majority of these studies included different types of bariatric procedures, particularly RYGB. Previous studies investigating SG cases involved a small sample size21,34,35 or omitted many important factors like age, HbA1c, and C-peptide22,24,36. Almost all studies followed up their patients for 1 year. The current research probably presents the largest series of patients treated with LSG who were followed up for 2 years.
The study demonstrated that predictive factors for T2DM complete remission at 2 years were age ≤ 45 years, duration of diabetes ≤ 5 years, use of a single oral antidiabetic, HbA1c ≤ 6.5%, HOMA-IR ≤ 4.6, C-peptide > 2.72 ng/mL, and BMI ≤ 40 kg/m2. On multivariate analysis, independent predictors of complete remission were younger age, shorter duration, single oral antidiabetic, lower HOMA-IR, and higher C-peptide. A combined marker of young age, short duration of DM, and low HOMA-IR provide a very good prediction of complete remission with 93% sensitivity and 82% specificity.
In the current study, complete remission occurred in 38% of patients in addition to 10.6% partial remission. Metabolic failure is observed in only 6.2% of cases. A recent meta-analysis in the United Kingdom reported a rate of diabetes remissions of 94.5 per 1,000 person-years, an 18-fold increased chance for remission than matched controls37. The authors found a larger effect size in patients undergoing gastric bypass compared to SG. Malabsorptive procedures tend to have a better antidiabetic impact compared to restrictive procedures as SG38. It has been reported that RYGB results in 50–80% remission rate of T2DM39,40,41.
The explanation for resolution or improvement remains unclear, but decreased energy intake and weight loss probably significantly contribute to this process. However, early resolution of diabetes within 1 week of surgery indicates that weight loss per se cannot explain the entire mechanism33,42. The effect of restrictive procedures as SG may be attributed to the immediate and severe caloric restriction that forces the human body to use internal energy sources43. Thus, ectopic fat from the hepatic tissue and other stores are mobilized and utilized44. A reduction in liver fat content normalizes hepatic insulin sensitivity by improving fasting plasma glucose43. These findings are supported by observing liver volume and liver fat content reduction after a low-calorie diet before bariatric surgery45,46,47. Moreover, after 1 week of restricted energy intake, normalization of β-cell function has been demonstrated48. Therefore, food restriction can sensibly explain the rapid postoperative metabolic improvement.
However, SG can be viewed as more than a restrictive procedure. It has been followed by decreased ghrelin secretion and increased GLP-1 synthesis, changes similar to those reported after in RYGB49. It was suggested that the balance between ghrelin and GLP-1 might be the key to improved glucose homeostasis50. Numerous studies have verified increased levels of bile acids after SG that could lead to ameliorations in insulin sensitivity, incretin secretion, and postprandial glycemia51,52.
The predictive factors found in the current study go in accordance with the shared denominators of diabetes remission in previous studies. Many studies proposed younger age19,25,26,27,53, shorter duration of DM20,23,26,27,54,55, lower HbA1c19,20,23,25,33, no preoperative insulin use26,55,56. Like the present study, others found a higher rate of complete remission with lower insulin resistance expressed as lower levels of HOMA-IR57,58. In some studies, poor control of DM with lower preoperative C-peptide levels was linked to poor control of diabetes after bariatric surgery25,59,60.
In obesity-associated T2DM, decreased insulin sensitivity is the first lesion, ensued by elevated insulin levels. Hyperglycemia arises because of β-cell failure to synthesize sufficient insulin. T2DM develops when pancreatic β-cell dysfunction follows in the face of decreased insulin sensitivity61. Hepatic insulin resistance is mainly implicated in elevated blood glucose levels and overt diabetes20. Insulin resistance with caloric overload leads to hepatic steatosis causing hepatic insulin resistance. Consequently, insulin fails to suppress liver glucose production leading to hyperglycemia43, and the process is self-exacerbating. Higher HOMA-IR levels indicating greater insulin resistance can be markers of less chance of diabetic remission after bariatric surgery.
It sounds logical that less preoperative β-cell dysfunction is a determinant of diabetes remission following surgery. This is because the steady deterioration of β-cell function is an aspect of the natural history of diabetes25. The current study found that a C-peptide level < 2.7 ng/mL is an independent factor predicting complete remission of DM. C-peptide is considered a more accurate evaluation of pancreatic β-cell function than insulin. A large percentage of insulin synthesized by the pancreas is degraded during the first pass hepatic metabolism compared to a negligible C-peptide amount62. Older age and longer duration of diabetes are consequently associated with lower residual β cell mass63,64.
Prediction models of diabetes remission were previously suggested for more practical implementation in clinical practice. For example, the DiaRem score included four variables for accurate remission prediction, namely the use of insulin, age, HbA1c, and type of antidiabetic medication65. The need for insulin therapy was the strongest indicator in this scoring system. Later studies ensured external validation of this score in independent populations66,67. ABCD score determined four factors; age at surgery (A), baseline BMI (B), C-peptide level (C), and diabetes duration (D) to construct a 0 to 10 scoring system31.
Almost all studies and predicting scores share common factors that can be categorized into two groups, disease status and preoperative management characteristics. Collectively, a longer duration and more progressive disease requiring more aggressive treatment allocate the patient fewer odds of diabetic remission. Careful preoperative assessment of these factors may guide a better selection of bariatric surgery candidates who will benefit from resolving the serious comorbidity T2DM alongside weight reduction.
Although the literature reported much data regarding the improvement of T2DM after LSG, to our knowledge, only a few studies addressed the factors linked to complete and partial remission, improvement, or unchanged status of T2DM after LSG. Besides, the reasonable number of cases with an acceptable follow-up period is a strength point of this study. The limitations of our study are mainly its nature as a single-center study. This raises the possibility of selection bias and difficulty of generalization to the entire bariatric population.
It should be noted that patient who did respond to sleeve may proceed malabsorptive procedures such as single anastomosis gastric bypass or Roux en-Y gastric bypass. Duodenal switch as well as (Single anastomosis duodeno–ileal bypass) SADI are not commonly practiced in our center.
In conclusion, we found that independent predictors of complete remission of T2DM after LSG were younger age, shorter duration, single oral antidiabetic, lower HOMA-IR, and higher C-peptide. A combined marker of young age, short duration of DM, and low HOMA-IR provide a perfect prediction of complete remission with 93% sensitivity and 82% specificity. It is sensible to say that this work can help recognize cases that are most likely to avail from SG regarding the extent of T2DM remission.
References:
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–xii, 1–253.
Obesity and overweight [Internet]. [cited 2020 Dec 21]. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
Apovian, C. M. Obesity: definition, comorbidities, causes, and burden. Am J Manag Care. 22, s176-185 (2016).
Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 377, 13–27 (2017).
Tino, S. et al. Prevalence and factors associated with overweight and obesity among patients with type 2 diabetes mellitus in Uganda-a descriptive retrospective study. BMJ Open. 10(11), e039258 (2020).
Cătoi, A. F., Pârvu, A., Mureşan, A. & Busetto, L. Metabolic mechanisms in obesity and type 2 diabetes: insights from bariatric/metabolic surgery. Obes. Facts. 8, 350–363 (2015).
Müller-Stich, B. P. et al. Surgical versus medical treatment of type 2 diabetes mellitus in nonseverely obese patients: a systematic review and meta-analysis. Ann. Surg. 261, 421–429 (2015).
Yan, Y. et al. Roux-en-Y Gastric bypass versus medical treatment for type 2 diabetes mellitus in obese patients: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 95, e3462 (2016).
Hsu, C.-C. et al. Effect of bariatric surgery vs medical treatment on type 2 diabetes in patients with body mass index lower than 35: five-year outcomes. JAMA Surg. 150, 1117–1124 (2015).
Ribaric, G., Buchwald, J. N. & McGlennon, T. W. Diabetes and weight in comparative studies of bariatric surgery vs conventional medical therapy: a systematic review and meta-analysis. Obes. Surg. 24, 437–455 (2014).
Ikramuddin, S. et al. Lifestyle intervention and medical management with vs without Roux-en-Y gastric bypass and control of hemoglobin A1c, LDL cholesterol, and systolic blood pressure at 5 years in the diabetes surgery study. JAMA 319, 266–278 (2018).
Gill, R. S., Birch, D. W., Shi, X., Sharma, A. M. & Karmali, S. Sleeve gastrectomy and type 2 diabetes mellitus: a systematic review. Surg. Obes. Relat. Dis. 6, 707–713 (2010).
Cho, E.-Y., Kemmet, O. & Frenken, M. Biliopancreatic diversion with duodenal switch in patients with type 2 diabetes mellitus: is the chance of complete remission dependent on therapy and duration of insulin treatment?. Obes. Facts. 4, 18–23 (2011).
Ozsoy, Z. & Demir, E. Which bariatric procedure is the most popular in the world? A bibliometric comparison. Obes Surg. 28, 2339–2352 (2018).
Hatoum, I. J. & Kaplan, L. M. Advantages of percent weight loss as a method of reporting weight loss after Roux-en-Y gastric bypass. Obesity (Silver Spring). 21, 1519–1525 (2013).
Matthews, D. R. et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985).
Elgenaied, I. et al. Factors associated with complete and partial remission, improvement, or unchanged diabetes status of obese adults 1 year after sleeve gastrectomy. Surg. Obes. Relat. Dis. 16(10), 1521–1530 (2020).
Brethauer, S. A. et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg. Obes. Relat. Dis. 11, 489–506 (2015).
Park, J. Y. & Kim, Y. J. Prediction of diabetes remission in morbidly obese patients after Roux-en-Y gastric bypass. Obes. Surg. 26, 749–756 (2016).
Hall, T. C., Pellen, M. G. C., Sedman, P. C. & Jain, P. K. Preoperative factors predicting remission of type 2 diabetes mellitus after Roux-en-Y gastric bypass surgery for obesity. Obes. Surg. 20, 1245–1250 (2010).
Rosenthal, R., Li, X., Samuel, S., Martinez, P. & Zheng, C. Effect of sleeve gastrectomy on patients with diabetes mellitus. Surg. Obes. Relat. Dis. 5, 429–434 (2009).
Praveen Raj, P. et al. Do bariatric surgery-related type 2 diabetes remission predictors add clinical value? A study on Asian Indian obese diabetics. Obes. Surg. 27, 2113–2119 (2017).
Robert, M. et al. Predictive factors of type 2 diabetes remission 1 year after bariatric surgery: impact of surgical techniques. Obes. Surg. 23, 770–775 (2013).
Jurowich, C. et al. Improvement of type 2 diabetes mellitus (T2DM) after bariatric surgery—who fails in the early postoperative course?. Obes. Surg. 22, 1521–1526 (2012).
Souteiro, P. et al. Preoperative beta cell function is predictive of diabetes remission after bariatric surgery. Obes Surg. 27, 288–294 (2017).
Lee, W.-J. et al. Predictors of diabetes remission after bariatric surgery in Asia. Asian J. Surg. 35, 67–73 (2012).
Ramos-Levi, A. et al. Diagnosis of diabetes remission after bariatic surgery may be jeopardized by remission criteria and previous hypoglycemic treatment. Obes. Surg. 23, 1520–1526 (2013).
Aminian, A. et al. Individualized metabolic surgery score: procedure selection based on diabetes severity. Ann. Surg. 266, 650–657 (2017).
Ugale, S. et al. Prediction of remission after metabolic surgery using a novel scoring system in type 2 diabetes – a retrospective cohort study. J. Diabetes Metab. Disord. 13, 89 (2014).
Still, C. D. et al. Preoperative prediction of type 2 diabetes remission after Roux-en-Y gastric bypass surgery: a retrospective cohort study. Lancet Diabetes Endocrinol. 2, 38–45 (2014).
Lee, W.-J. et al. Predicting success of metabolic surgery: age, body mass index, C-peptide, and duration score. Surg. Obes. Relat. Dis. 9, 379–384 (2013).
Ramos-Levi, A. M. et al. Statistical models to predict type 2 diabetes remission after bariatric surgery. J. Diabetes. 6(5), 472–477 (2014).
Hayes, M. T., Hunt, L. A., Foo, J., Tychinskaya, Y. & Stubbs, R. S. A model for predicting the resolution of type 2 diabetes in severely obese subjects following Roux-en Y gastric bypass surgery. Obes Surg. 21, 910–916 (2011).
Ramos-Leví, A. M. et al. C-peptide levels predict type 2 diabetes remission after bariatric surgery. Nutr. Hosp. 28, 1599–1603 (2013).
Jiménez, A. et al. Long-term effects of sleeve gastrectomy and Roux-en-Y gastric bypass surgery on type 2 diabetes mellitus in morbidly obese subjects. Ann. Surg. 256, 1023–1029 (2012).
Heshmati, K., Harris, D. A., Aliakbarian, H., Tavakkoli, A. & Sheu, E. G. Comparison of early type 2 diabetes improvement after gastric bypass and sleeve gastrectomy: medication cessation at discharge predicts 1-year outcomes. Surg. Obes. Relat. Dis. 15(12), 2025–2032 (2019).
Yska, J. P. et al. Remission of type 2 diabetes mellitus in patients after different types of bariatric surgery: a population-based cohort study in the United Kingdom. JAMA Surg. 150, 1126–1133 (2015).
Park, J. Y. Prediction of type 2 diabetes remission after bariatric or metabolic surgery. J. Obes. Metab. Syndr. 27, 213–222 (2018).
Schauer, P. R. et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 366, 1567–1576 (2012).
Mingrone, G. et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N. Engl. J. Med. 366, 1577–1585 (2012).
Buchwald, H. et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am. J. Med. 122(248–256), e5 (2009).
Kashyap, S. R. et al. Acute effects of gastric bypass versus gastric restrictive surgery on β-cell function and insulinotropic hormones in severely obese patients with type 2 diabetes. Int. J. Obes. 34, 462–471 (2010).
Taylor, R. Type 2 diabetes. Diabetes Care 36, 1047–1055 (2013).
Knop, F. K. & Taylor, R. Mechanism of metabolic advantages after bariatric surgery. Diabetes Care 36, S287–S291 (2013).
Edholm, D. et al. Preoperative 4-week low-calorie diet reduces liver volume and intrahepatic fat, and facilitates laparoscopic gastric bypass in morbidly obese. Obes. Surg. 21, 345–350 (2011).
Lewis, M. C. et al. Change in liver size and fat content after treatment with Optifast very low calorie diet. Obes.Surg. 16, 697–701 (2006).
Colles, S. L., Dixon, J. B., Marks, P., Strauss, B. J. & O’Brien, P. E. Preoperative weight loss with a very-low-energy diet: quantitation of changes in liver and abdominal fat by serial imaging. Am. J. Clin. Nutr. 84, 304–311 (2006).
Lim, E. L. et al. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 54, 2506–2514 (2011).
Benaiges, D. et al. Laparoscopic sleeve gastrectomy: More than a restrictive bariatric surgery procedure?. World J. Gastroenterol. 21, 11804–11814 (2015).
Peterli, R. et al. Metabolic and hormonal changes after laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy: a randomized. Prospect. Trial Obes. Surg. 22, 740–748 (2012).
Steinert, R. E. et al. Bile acids and gut peptide secretion after bariatric surgery: a 1-year prospective randomized pilot trial. Obesity (Silver Spring). 21, E660-668 (2013).
Penney, N. C., Kinross, J., Newton, R. C. & Purkayastha, S. The role of bile acids in reducing the metabolic complications of obesity after bariatric surgery: a systematic review. Int. J. Obes. (Lond). 39, 1565–1574 (2015).
Hamza, N. et al. Predictors of remission of type 2 diabetes mellitus after laparoscopic gastric banding and bypass. Surg. Obes. Relat. Dis. 7, 691–696 (2011).
Schauer, P. R. et al. Bariatric surgery versus intensive medical therapy for diabetes–3-year outcomes. N. Engl. J. Med. 370, 2002–2013 (2014).
Yu, H. et al. Visceral fat area as a new predictor of short-term diabetes remission after Roux-en-Y gastric bypass surgery in Chinese patients with a body mass index less than 35 kg/m2. Surg. Obes. Relat. Dis. 11, 6–11 (2015).
Scopinaro, N., Adami, G. F., Bruzzi, P. & Cordera, R. Prediction of diabetes remission at long term following biliopancreatic diversion. Obes. Surg. 27, 1705–1708 (2017).
Bhasker, A. G. et al. Predictors of remission of T2DM and metabolic effects after laparoscopic Roux-en-y gastric bypass in obese Indian diabetics-a 5-year study. Obes. Surg. 25, 1191–1197 (2015).
Yan, H. et al. Defining and predicting complete remission of type 2 diabetes: a short-term efficacy study of open gastric bypass. OFA 6, 176–184 (2013).
Aarts, E. O. et al. Preoperative fasting plasma C-peptide level may help to predict diabetes outcome after gastric bypass surgery. Obes. Surg. 23, 867–873 (2013).
Lee, W.-J. et al. C-peptide predicts the remission of type 2 diabetes after bariatric surgery. Obes. Surg. 22, 293–298 (2012).
Mezza, T. et al. β-cell fate in human insulin resistance and type 2 diabetes: a perspective on islet plasticity. Diabetes 68, 1121–1129 (2019).
Najjar, S. M. & Perdomo, G. Hepatic insulin clearance: mechanism and physiology. Physiology 34, 198–215 (2019).
Saisho, Y. β-cell dysfunction: Its critical role in prevention and management of type 2 diabetes. World J. Diabetes. 6, 109–124 (2015).
Khanna, V. et al. Adults with long-duration type 2 diabetes have blunted glycemic and β-cell function improvements after bariatric surgery. Obesity (Silver Spring). 23, 523–526 (2015).
Still, C. D. et al. A probability score for preoperative prediction of type 2 diabetes remission following RYGB surgery. Lancet Diabetes Endocrinol. 2, 38–45 (2014).
Mehaffey, J. H. et al. Type 2 diabetes remission following gastric bypass: does diarem stand the test of time?. Surg. Endosc. 31, 538–542 (2017).
Aron-Wisnewsky, J. et al. The advanced-DiaRem score improves prediction of diabetes remission 1 year post-Roux-en-Y gastric bypass. Diabetologia 60, 1892–1902 (2017).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Salman, A.A., Salman, M.A., Marie, M.A. et al. Factors associated with resolution of type-2 diabetes mellitus after sleeve gastrectomy in obese adults. Sci Rep 11, 6002 (2021). https://doi.org/10.1038/s41598-021-85450-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-021-85450-9
This article is cited by
-
Diabetes Remission After Bariatric Surgery: A 10-Year Follow-Up Study
Obesity Surgery (2025)
-
Comparison of SADI-S Versus SG in Chinese with Diabetes and BMI < 35 kg/m2:a Retrospective Study with Medium-Term Outcomes
Obesity Surgery (2025)
-
Identification of circulating apolipoprotein M as a new determinant of insulin sensitivity and relationship with adiponectin
International Journal of Obesity (2024)
-
Association of Baseline Triglyceride-Glucose Index with Poor Glycemic Control and Diabetes Remission After Metabolic Surgery
Obesity Surgery (2023)