Abstract
With wide socioeconomic mortality differential among older adults in India, a constant question of death clustering across high-risk families and communities arises. The present study uses a follow-up survey from India to investigate the socioeconomic, demographic and health predictors of old-age mortality clustering. Data of 16,964 older adults nested within 12,981 households from 2352 communities were used from India Human Development Survey (IHDS) round-I (2005) who were further tracked down in round-II (2012). Bivariate association between the determinants of old-age mortality was investigated using the log-rank test. The multivariate analysis involved estimating the random-intercept Weibull proportional hazard model with three levels—individual (level 1), family (level 2) and community (level 3). We analyzed the sensitivity of multivariate results to unobservable variable and selection biases using the e-value method. The empirical analysis confirms that the risk of mortality is significantly heterogeneous between the families. The health status of older adults and the family’s socioeconomic status in the early years emerged as prominent predictors of a longer lifespan. With a strong association between household income and mortality hazard risk, the present study urges early life interventions as those started in late-life might have negligible impact on keeping the older adults alive and healthy.
Similar content being viewed by others
Introduction
The famous phrase of Thomas Hobbes denotes human lives as “nasty, brutish and short”1. Historically, people used to survive merely 25 years from birth; however, with the evolution in living conditions of human society and a vast reduction in the mortality rates, average life expectancy at birth has grown nearly 45 years today2. Though initially, developed countries experienced such mortality reductions in a non-uniform manner, the mortality reduction in younger ages was comparably much higher than the others due to a decline in the fatality figure of infectious diseases3. Such progress was combined with the falling fertility rates and increasing life expectancy, leading to an increase in the share of the aged in the total population4.
As per the United Nations report, the aged population would increase from 0.7 billion (9% of the global population) in 2019 to 1.5 billion (16%) in 20505. Developed countries that have already experienced the demographic transition try to break the stereotypes of the aged population being dependent, frail, and burdened for society. Policies are working towards promoting the wellbeing of older adults and promoting healthy aging among individuals6. However, such policy reforms are rare in developing nations where the focus is on fulfilling the development needs of children and youth. Notably, even if the pace of population aging started in the high-income countries, by 2050, 80% of the older population is expected to live in low-and-middle-income countries, which brings the old-age mortality issue to the central stage6.
A systematic review from developed and developing countries indicate that social determinants like socioeconomic, cultural and environmental conditions, living and working conditions, social and community networks, the lifestyle of individuals are prominent predictors of old-age mortality7. Two longitudinal studies from UK and USA found a long term impact (i.e. nearly 2 and 6 years respectively) of socioeconomic and health status of individuals with survival in old ages8,9. A follow-up study from Taiwan found that individuals with higher ages, poor schooling, consistent unemployment and poor life satisfaction in wave 1 have a higher probability of mortality in later periods10. However, the health status of individuals (in the form of activities of daily living conditions and self-reported chronic diseases) emerged as the primary predictor among all the other factors. Though marriage had a significant protective impact on the lives of individuals, males were less likely to be alive in follow-up surveys10. A study from Bangladesh provided evidence that being head of the household and residing with a spouse or son helped reduce mortality among older adults11. Studies from Ethiopia, New Zealand, Israel and the United States found that living in a rural area, having different ethnic groups and continents of origin, and experiencing financial hardship or stress can easily trigger mortality at older ages12,13,14,15. Such differences in mortality risks across socioeconomic, cultural and environmental conditions suggest unequal distribution of mortality risks among older adults. These deaths may be clustered among certain families and communities, putting them under the higher-risk categories.
In India, 60 years and above population is projected to rise 13.2% in 203116. Lesser consideration towards the older adults can create a more significant loss in the future in the form of old-age mortality or repercussions like catastrophic health spending, social and financial insecurity and physical, social and emotional distress17,18. Few existing literatures from India have shown the effect of age, gender, caste and living standard on old-age mortality19,20. Studies have shown that prior co-morbidities among older adults have further worsened the old-age mortality risks. Thus, maintaining a healthy lifestyle that involves eating a balanced diet, physical activity, and avoiding substance abuse has contributed to fewer diseases, further reducing the mortality risk in older ages6. Despite knowledge of such determinants, the quality and quantity of life of older adults in India vary across families and communities. This brings the need to understand the risk factors for such unequal distribution of mortality risks among older adults by considering heterogeneity at the household and community levels. The present study improves upon the limitations of extant studies and aims to examine the risk factors of old-age mortality in India using a multilevel survival approach based on a nationally representative survey. Present study also uses the follow up survey data to indicate the predictors of old-age mortality and contributes to the recent literature in this area through robust evidence.
Methods
Data
This research article utilized the India Human Development Survey (IHDS) wave-I and wave-II, jointly administered by the National Council of Applied Economic Research (NCAER) and the University of Maryland. IHDS is a nationally-representative, multi-topic, large-scale survey that provides essential information on health and morbidity, education, employment and economic status, fertility and marital relations, and social capital of the Indian population. IHDS wave-I and wave-II were conducted during 2005 and 2012, respectively, across all India’s states and union territories except for Andaman & Nicobar Islands and Lakshadweep. Both waves of IHDS adopted a multistage stratified random sampling design, and further details on sampling design, data collection and informed consent are available elsewhere21,22. Notably, IHDS wave-II was a panel survey, which re-interviewed 83% of the original IHDS wave-I households. Further details regarding the IHDS wave-II panel component are available in the user guide22.
This study refers to persons aged 60 years and above as older adults. Intending to examine old-age mortality, this study utilized the tracking sheet data of IHDS wave-II from 2005 to 2012. Further, to explore the determinants of mortality in older adults, we merged the individual-, household- and community-level information from wave-I with the tracking sheet information in wave-II. The analytical sample of this study is 16,964 older adults residing in 12,891 families and nested within 2,352 communities in India.
Mortality statement
The information regarding the mortality status of older adults was obtained from the IHDS wave-II tracking sheet data. With the aim of re-interviewing wave-I households during wave-II, the IHDS collected data on the status of all wave-I respondents during wave-II (this information comprised the tracking sheet data). Notably, during wave-II, IHDS gathered information of the survival status of respondents and the year of death prior to wave-II if respondents were not alive. Therefore, this information on survival status and survival time was used to analyze the mortality of older adults in India. All older adults who died during this period were coded as “Yes”; otherwise, they were coded as “No”.
Statistical methods
At the outset, we examined the sample distribution of older adults. Next, we estimated the incidence rate of old-age mortality between 2005 and 2012 and grouped it by gender and age group. Further, we performed bivariate and multivariable analyses to achieve the study objectives. Note that the mortality data described in “Mortality statement” contain censored observations (those older adults who did not experience mortality between wave-I and wave-II and older adults who were lost to follow-up). Therefore, in the bivariate analysis, we calculated the mean survival duration of older adults across the categories of risk factors by accounting for censoring in the data23. Further, log-rank tests were performed to examine the association between the risk factors and older adults’ mortality status by adjusting for censored cases. Statistical details of the log-rank test are available elsewhere23.
The multivariable analysis involved estimating random-intercept parametric survival regression models. Survival regression models help utilize the information from censored records in the retrospective life-course data, thereby curtailing the loss of crucial information23. Notably, parametric survival regression models have the advantage of more efficiently utilizing the information from censored cases compared to semi-parametric regression models23. In the survival models, our event of interest is the binary survival status of the older adults between IHDS 2005 and 2012.
Additionally, parametric survival regression models allow us to choose the underlying statistical distribution of time-to-old-age mortality23. Based on theoretical knowledge and statistical evidence, we use the Weibull proportional hazard model in our study. The Weibull regression model is appropriate when the hazard of the failure event (here, risk of mortality) is either monotonically increasing or decreasing23. Based on existing knowledge of human mortality, we know that the risk of mortality rises steadily among older adults with progressing age24,25. A similar trend is observed in our data (see Fig. 2) of Indian older adults. Therefore, using the Weibull regression hazard model to estimate mortality risk among Indian older adults is theoretically justified25. The statistical fit of the models was examined by comparing the Akaike information criterion (AIC) and Bayesian information criterion (BIC) scores of the five prominent random-intercept survival regression models (Exponential, Weibull, Lognormal, Loglogistic and Gamma). We aim to use the model with the lowest AIC and BIC scores, as that would best fit the data.
In the random-intercept Weibull hazard model, we included individual (level 1), family (level 2) and community (level 3) as the three levels. 16,964 older adults from 12,981 families were nested within 2352 communities, forming a hierarchical structure in our study sample. In India, older adults from the same families of the same communities are likely to share the same socioeconomic characteristics and household environment, which means the mortality risk might also be shared. Estimating mortality hazard using standard survival regression would overestimate the risk in this scenario, and using a multilevel framework becomes necessary26,27. The statistical description of the three-level random-intercept survival regression model is given below:
Here, \({s}_{k}\) is the level 3 residual (group effect at community-level), \({c}_{jk}\) is the level 2 residual (group effect at family-level) and \({e}_{ijk}\) is the level 1 residual (individual level). \(h\left({t}_{ijk}\right) \mathrm{and} {h}_{0}\left({t}_{ijk}\right)\) are overall and baseline hazard of old-age mortality for ith persons belonging to the jth family of kth community. \({\beta }_{1}\),\({\beta }_{2}\) and \({\beta }_{3}\) gives the hazard coefficient of old-age mortality for the person-level, family-level and community-level independent variables, respectively, given the effect of all other independent variables and the group-level effects remains constant.
The random-intercept regression models provide the Intraclass Correlation Coefficient (ICC) and Median Hazard Ratio (MHR), which measures the mortality clustering of older adults within the families and the communities, respectively. The family-level ICC measures the correlation in mortality risk among older adults belonging to the same family of the same community27,28. It is calculated as29:
where, \({\sigma }_{i}^{2}\), \({\sigma }_{f}^{2}\), and \({\sigma }_{c}^{2}\) are the individual-, family- and community-level random-effect variance.
Equivalently, the community-level ICC denotes the correlation in mortality risk among older adults of the same community27,29. It is calculated as:
where the notations have the usual meaning. The ICC value lies between 0 and 1. The higher the value of ICC, the greater is the extent of mortality clustering at the respective levels.
Equivalently, the family-level (or community-level) MHR gives the median relative change in the hazard of the old-age mortality among all possible identical older adults pairs from two separate randomly selected families (or communities) that are ordered by mortality risk30. The family-level and community MHR is calculated as:
where the notations have the usual meaning. The value of MHR is always greater than or equal to one such that the higher the value, the more is the heterogeneity in the old-age mortality risk across clusters. Further statistical details regarding the ICC and MHR are available from the cited references.
Further, the multivariable association between the independent variables and old-age mortality risk was shown using hazard ratios (HR). The HR gives the hazard of old-age mortality compared to the baseline mortality risk among older adults belonging to a particular category of an explanatory variable when the effect of other explanatory variables and the community- and family-level variability remain constant23.
Moreover, sensitivity analysis was performed by inspecting the presence of unobservable variable bias in the adjusted hazard ratios using the e-value method31,32. The e-value method gives the e-value statistic, which is defined as the minimum strength of association (on the hazard ratio scale) that an unmeasured confounder would need to have with both the treatment and the outcome variables after adjusting for the effect of other independent variables, such that the treatment-outcome variable association is nullified31. Therefore, the higher the e-value, the more robust is the corresponding hazard ratio to unobserved variable bias. The statistical significance of the e-value was determined from the CI limit (nearest limit to the null value of 1.00)32. The CI limit was 1.00 if the e-value was not statistically significant at the 5% level32.
We checked and found that none of the multivariable models violated the multicollinearity assumption33. Unfortunately, IHDS does not provide sample weight in the tracking sheet data, and the study results are unweighted. Statistical significance was determined at the 5% level unless mentioned otherwise. Statistical estimations were performed using the STATA 14 software34.
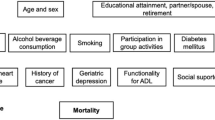
Explanatory variables
Existing studies have shown several factors which explain the mortality among older adults7,9,19,20. We included these variables, conditional to their availability in the IHDS dataset. All the below-mentioned characteristics were measured for the older adults during wave-I. The individual-level variables related to the older adults include:
-
(a)
Age-group (in years) (60–69, 70–79, 80 and above).
-
(b)
Gender (female, male).
-
(c)
Cardiovascular diseases (no, yes).
-
(d)
Hypertension (no, yes).
-
(e)
Diabetes (no, yes).
-
(f)
Respiratory illnesses (no, yes).
-
(g)
Other chronic illnesses (no, yes).
-
(h)
Activities of daily living (no disability, has disability).
-
(i)
Smokes tobacco (no, yes).
-
(j)
Drinks alcohol (no, yes).
-
(k)
Marital status (currently married, widowed, currently not married).
-
(l)
Level of education (more than 10 years of schooling, 6–10 years of schooling, less than 5 years of schooling, No formal schooling).
-
(m)
Working status (working, not working).
-
(n)
Participates in social groups (yes, no).
-
(o)
Headship status (household head, not household head).
The household-level variables considered in our study are:
-
(a)
Family structure (single generation, nuclear, joint/extended). It was prepared from the information on household members and their relationship with the household head.
-
(b)
Number of children in the household (three and more, two, one, none).
-
(c)
Household wealth quintile (richest, rich, middle, poor, poorest). The household wealth quintile for wave-I was calculated using principal component analysis using the available information on household asset ownership. We used standard procedures documented elsewhere35.
-
(d)
Household poverty (not below poverty line, below poverty line).
-
(e)
Caste of household head (others, other backward classes, scheduled castes, scheduled tribes). The caste system is a form of social hierarchy exclusive to India. Constitutionally, three distinct social groups are recognized in India—scheduled tribes (ST), scheduled castes (SC) and other backward classes (OBC). The ST (predominantly tribal) and SC categories comprise the most socially backward. They traditionally belonged to the lowest rung of India’s now-defunct caste system. People of the OBC category, as the name implies, are members of a socially and economically backward community. However, their circumstances are better than those of the SC/ST population. The “Others” category consists of all people who do not belong to the three caste groups.
-
(f)
Religion of household head (Hinduism, Islam, Others).
Taking a cue from extant research, we included three community contextual variables36,37,38:
-
(a)
Education level of community (low, medium, high).
-
(b)
Poverty status of community (low, medium, high).
-
(c)
Social standard of community (low, medium, high).
We constructed these three community contextual characteristics by aggregating the information on the education level of individuals, BPL status of household and caste of the household to the community level, respectively. Prior to aggregation, we constructed binary variables of each of the three characteristics. Community education level was defined as the proportion of individuals with more than 10 years of schooling among all individuals in the community. The higher the proportion of educated individuals, the greater the community's education standard. The community poverty status was defined as the proportion of BPL households among all households in the community. A higher proportion of below poverty line households means a greater prevalence of poverty in the community. Further, community social standard was constructed as the proportion of Non-SC/ST households among all households in the community. Therefore, the higher the proportion of Non-SC/ST households, the greater is the community’s social standard. For ease of interpretation, we categorized the proportions into three categories—“low” (lowest 33rd percentile), “medium” (middle 33rd percentile), and “high” (highest 33rd percentile).
Additionally, we included the following community-level characteristics:
-
(d)
Type of community (urban, rural).
-
(e)
Geographical region (southern, western, eastern, central, north eastern, northern). The geographical regions divided India’s erstwhile 33 states and union territories into six areas based on administrative divisions39.
Ethics approval and consent to participate
The present study utilized a publicly available secondary dataset with no information that would lead to the identification of the respondents. IHDS obtained the informed consent of respondents before the data collection. Therefore, no ethical approval was necessary for using these datasets. All survey methods were performed following the relevant guidelines and regulations.
Results
Sample description
Table 1 shows the characteristics of 16,964 older adults aged 60 years and above during IHDS 2005. Nearly 61% of older adults were aged between 60 and 69 years, and 50% were male. Nearly 6% and 4% of older adults had hypertension and diabetes, respectively. Moreover, one in ten older adults faced difficulty performing activities of daily living, one-fifth of older adults smoked tobacco, and 7% consumed alcohol. Further, six in ten older adults had no formal schooling, and 36% were widowed. While one-tenth of older adults lived in single generation households, 32% belonged to the lowest 40% wealth quintile households. Coming to the community context, we observed that 70% of older adults resided in rural areas, three in ten older adults belonged to communities with a high level of education and social standard. Further, 35% and 33% of children were from communities with low socioeconomic status and had a low maternal education level, respectively. In terms of population distribution, most older adults (33%) were from the Northern region, followed by the Southern (24%) region.
Figure 1 shows the Mortality Incidence Rate (per 1000 person-years lived (PYL)) among subgroups of older adults for 2005–2012. The overall old-age mortality rate was 39 per 1000 PYL. The mortality rate was higher in male older adults (42 deaths per 1000 PYL) and those aged 80 years and beyond (98 deaths per 1000 PYL) compared to their counterparts from other sub-groups.
Bivariate analysis
Table 2 shows the average survival duration and the bivariate association of old-age mortality with the individual-, family- and community-level determinants. Most of the individual and household level factors in 2005 were associated with old-age mortality between 2005 and 2012. The community’s education level, poverty status, and social standard were significantly associated with old-age mortality. Moreover, the mortality hazard was also significantly associated with the type and geographical region of the community.
Model specification
Table 3 shows the goodness-of-fit statistics for the Exponential, Weibull, Lognormal, Loglogistic and Gamma random-intercept survival regression models for old-age mortality. The Weibull regression models are the best fit as they have the lowest AIC and BIC scores among all the models. Further, Fig. 2 shows that the hazard of old-age mortality increases with the duration of observation. Therefore, the choice of the Weibull model is conceptually and statistically justified.
Extent of old-age mortality clustering among families and communities
Table 4 shows the family- and community-level effects from the random-intercept Weibull hazard models of old-age mortality, respectively. We calculated two regression models—the null model is an empty model without any covariates, and the full model includes all covariates (see “Statistical methods”). In both models, the variation in mortality risk at both family- and community-level was statistically significant. However, the family-level variation was at least twenty times higher than the community-level variation in both models. The family-level ICC for the full model shows a 61% correlation in the risk of mortality among older adults belonging to the same family of the same community (after adjusting for the individual-level, family-level and community-level characteristics). Moreover, the median hazard of mortality is 2.12 times higher (family-level MHR) between all pairs of high-risk and low-risk families. Additionally, the statistically significant Weibull regression parameter implies that the assumption of monotonically increasing mortality hazard with time is not violated.
Multivariable association and Sensitivity analysis
Table 5 (Columns 2 and 3) gives hazard ratios of association of old-age mortality risk with the explanatory variables after adjusting for the effect of other variables and accounting for the community- and family-level unobserved heterogeneity. We found that male older adults have 1.91 times [95% CI: (1.74, 2.11)] higher chance of mortality between 2005 and 2012 than their female counterparts. Older adults with cardiovascular diseases [HR: 1.37, CI: (1.11, 1.70)], diabetes [HR: 1.48, CI: (1.24, 1.77)], respiratory illnesses [HR: 1.60, CI: (1.38, 1.87)] and any other chronic illnesses [HR: 1.64, CI: (1.38, 1.87)] were more likely to die compared to those without the morbidity. Moreover, older adults who faced difficulty in activities of daily living and were not working had 1.26 [CI: (1.14, 1.39] and 1.63 [CI: (1.50, 1.76)] times greater hazard of experiencing mortality than those who had no disability and were working. The mortality hazard also increased with a decrease in education level among older adults. Interestingly, older adults who were not household heads faced an elevated risk of mortality [HR: 1.24, CI: (1.13, 1.36)] versus those who had headship.
Coming to family-level characteristics, we observed that older adults residing in nuclear [HR: 1.28, CI: (1.09, 1.51)] and joint/extended [HR: 1.50, CI: (1.29, 1.74)] families faced higher mortality risk than those residing in single generation households. The results also show an economic gradient in the mortality hazard among older adults. The risk of old-age mortality was 1.25 [CI: (1.09, 1.43)] and 1.30 [CI: (1.12, 1.51)] times more among individuals residing in poor and poorest wealth quintile households compared to the richest wealth quintile counterparts. Similarly, older adults from BPL households faced an elevated risk of old-age mortality at 1.13 times [CI: (1.03, 1.25)].
Contrary to the bivariate analysis, we find that the educational level, poverty status and social standard of community was not associated with mortality risk among older adults after adjusting for the effect of other independent variables and the community-level and family-level effects. However, older adults residing in communities from Northern [HR: 1.19, CI: (1.07, 1.32)] and Eastern [HR: 1.29, CI: (1.12, 1.48)] regions of India had higher mortality hazards compared to individuals residing in the Southern region.
Table 5 (columns 4 and 5) shows the sensitivity of the association between the occurrence of old-age mortality and its determinants to unobserved variable bias. Among the individual-level characteristics, we observed that the relationship of old-age mortality with—gender, cardiovascular diseases, diabetes, respiratory illnesses and other chronic morbidities, activities of daily living, smoking tobacco, work status and household headship status did not suffer from unobserved variable bias. Upon observing family-level characteristics, it was evident that the association of family, household wealth quintile and poverty status with old-age mortality was not sensitive to omitted variable bias.
After estimating the Weibull survival regression models, we obtained the adjusted cumulative hazard curve of old-age mortality grouped by lifestyle, social and economic characteristics (Fig. 3). Notably, the cumulative hazard curve in terms of smoking tobacco, drinking alcohol, level of education, family structure, the caste of household head and household wealth quintile were adjusted for the effect of other independent variables and the family- and community-level effects. We find that the graphs' results were in a similar direction to those obtained from the multivariable regression model.
Discussion
Today, with substantial health advancements worldwide, people can expect to live into their sixties and beyond. Longer life has provided opportunities for older people (such as pursuing their passion, education, new career) and opened their chance of contributing towards families and communities. However, the growing mortality and health risks during old age hinder such opportunities and contributions40. The present study reveals a significant loss in the old-age population between 2005 and 2012 with an unequal distribution of mortality risks across families and communities.
Using a follow-up survey from India, the present study shows that many high-risk families (mortality clustering in families) in India lose multiple members in 60 years and above ages. Although older adults share common characteristics among communities, the present study does not find any significant clustering of mortality at the community level. Even after adjusting the unobserved heterogeneity at family and community levels, mortality risk was higher among older male adults than female counterparts. Consistent with the previous literature, older adults with poor education and those residing in unemployed condition experiences higher mortality risk13,41. Long term consequence of widowhood status was prominent in the study as being widow brings higher mortality risks among older adults. Such misfortunate widowhood condition is also visible from extant Indian literature42. The possible explanation for such association includes the protective effect of marriages in social, psychological, economic and environmental support43. Household headship provides constant involvement and control on the household’s social, financial affairs and a sense of security and authority. This might be the reason that household headship in older adults prevents long term mortality risk in the present study.
Ample evidence reveals an essential role of the social participation of older adults on long term survival as it may protect them from loneliness, depression, stress, or sadness of being away from loved ones44. However, in contrast to past evidence, the present study found an insignificant association between social participation in the first wave and mortality risk until the follow-up period. Such association might be possible due to the long-term window of observation. Since the older adults actively indulged in social activities might not continue due to poor health, leaving them in distress which can turn to a shorter lifespan. The health status of older adults is the prominent predictor among all the individual factors10,45. For instance, if an individual had poor health status in the first wave (i.e., chronic diseases or difficulty doing daily activities) then, better education, working status, marital status, or social participation will not be much helpful in reducing the long-term mortality risk until and unless they take early preventive measures.
Extended or joint families experience higher mortality risks among older adults. Such association is possible as the joint or extended families will have more older adults than a single or nuclear generation, making them vulnerable to mortality risks. Moreover, having no children can also be responsible for higher old-age mortality risks due to financial insecurity and loneliness46. Past evidence from India shows a socioeconomic disparity in older-age mortality which is also evident in this study; however, they were unable to show long term impact20. Consistent with a longitudinal study from Taiwan, the present study found that the most prosperous older adults and those living above the poverty line in the first wave enjoy a longer lifespan in the future10. Despite a higher proportion of older adults in southern regions of India, mortality risks were higher in central, northern and eastern areas of India. This might be possible due to individuals’ better health care-seeking behavior in southern regions of India47. However, despite having a poor health care system in the north-eastern regions, the mortality risk remains lower in the present study. Surprisingly, this may be due to the family level factors acting as a protective shield for the older adults or a higher female population in older ages48,49. For instance, the solid biological advantage of females and satisfaction of being closer to family and community might help in lowering the mortality risk of north-eastern older adults.
Despite providing robust evidence of heterogeneity in older-age mortality risk at the family level and revealing the long-term effect of individual, household and community factors on older-age mortality risks, the present study has its limitations. Ample evidence shows that depression and life satisfaction are emerging as prominent indicators of a longer lifespan; however, we could not capture their effect due to the unavailability of information in the data used for this study50. Self-reported chronic conditions may create multiple problems in the form of biases like the accuracy of responses, so biological or clinical markers of chronic diseases should be considered while understanding the mortality dynamics of the individual51. The present study uses self-reported information of chronic diseases as the biological measures of older adults were unavailable. Additionally, the study results are unweighted and need to be interpreted accordingly.
Conclusion
In India, families are the prime source of caregivers for older adults. With significantly higher mortality risk heterogeneity across Indian families, the present study confirms that the familial-level factors (i.e., having children, income-level, poverty status and ethnicity) in early years of life may have a noticeable impact on the longer lifespan of older adults. Along with the individual-level factors (i.e., education, employment, support of a partner, social participation, and health behavior), health status in the form of chronic diseases and daily living activities remains to have a significant impact on the survival of older adults.
Past literature from developed countries shows no health gradient among rich and poor before the enlightenment of science and advanced technologies2. However, with the growing development of treatments and drugs, a wealthier population pays quickly to cure diseases and ensure a longer life. This trend continues in developing countries, too, combined with the lesser knowledge of health behavior among the uneducated population, increasing the disparities across socioeconomic statuses. Such past evidence and the detrimental effect of poverty and lower income in the present study confirms the unequal share of mortality distribution in old-age across families. The present study will help the policymakers understand the development of such a mortality gradient in the old-age population of India and provide efficient evidence of policy interventions across high-risk families. The long-term consequences of socioeconomic status and health conditions on old-age mortality risk further urge early life interventions as those started in late-life might have negligible impact on keeping the older adults alive and healthy.
Traditionally, joint or extended families were one of the characteristics of Indian life where older adults enjoy authority along with care from younger generations. However, changes in living arrangements and lifestyle in past years bring a shift towards the caregiver role in families. The emergence of new health conditions like life satisfaction, stress, and depression among wealthy and low-income families, further, urges future research on the old-age mortality risks in India.
References
Hobbes, T. Solitary, poor, nasty, brutish, and short. In: Yale University Press London Blog [Internet]. 5 Apr 2013 [cited 17 Dec 2021]. Available: https://yalebooksblog.co.uk/2013/04/05/thomas-hobbes-solitary-poor-nasty-brutish-and-short/.
Deaton, A., Cutler, D. & Lleras-Muney, A. The determinants of mortality. J. Econ. Perspect. 20, 97–120 (2006).
Wrigley, E.A., & Schofield, R.S. The population history of England 1541–1871. Cambridge University Press (1989).
Eggleston, K. N. & Fuchs, V. R. The new demographic transition: Most gains in life expectancy now realized late in life. J. Econ. Perspect. 26, 137–156 (2012).
UN Population Division. World Population Prospects 2019; Department of Economic and Social Affairs (ST/ESA/SER.A/424) (2019).
WHO. Ageing and health. In: 2018 [Internet]. [cited 15 May 2021]. Available: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health.
de Silva, V. L., Cesse, E. Â. P. & de Albuquerque, M. Social determinants of death among the elderly: A systematic literature review. Rev. Bras. Epidemiol. 17, 178–193 (2014).
Attanasio, O., & Emmerson, C. Differential mortality in the UK (2001).
Hurd, M.D., McFadden, D., & Merrill, A. 5. Predictors of mortality among the elderly. University of Chicago Press (2007).
Mete, C. Predictors of elderly mortality: Health status, socioeconomic characteristics and social determinants of health. Health Econ. 14, 135–148 (2005).
Rahman, M. O. Age and gender variation in the impact of household structure on elderly mortality. Int. J. Epidemiol. 28, 485–491 (1999).
Szanton, S. L. et al. Effect of financial strain on mortality in community-dwelling older women. J. Gerontol. B Psychol. Sci. Soc. Sci. 63, S369–S374 (2008).
Fantahun, M., Berhane, Y., Högberg, U., Wall, S. & Byass, P. Ageing of a rural Ethiopian population: Who are the survivors?. Public Health 123, 326–330 (2009).
Jatrana, S. & Blakely, T. Ethnic inequalities in mortality among the elderly in New Zealand. Aust. N. Z. J. Public Health 32, 437–443 (2008).
Jaffe, D. H., Neumark, Y. D., Eisenbach, Z. & Manor, O. Parity-related mortality: Shape of association among middle-aged and elderly men and women. Eur. J. Epidemiol. 24, 9–16 (2009).
Elderly in India 2021.pdf. Available: http://www.indiaenvironmentportal.org.in/files/file/Elderly%20in%20India%202021.pdf.
Brinda, E. M. et al. Health, social, and economic variables associated with depression among older people in low and middle income countries: World health organization study on global AGEing and adult health. Am. J. Geriatr. Psychiatry 24, 1196–1208 (2016).
Yang, W., & Hu, B. Catastrophic health expenditure and mental health in the older Chinese population: The moderating role of social health insurance. J. Gerontol. Ser. B. (2021).
Subramanian, S. V. et al. The mortality divide in India: the differential contributions of gender, caste, and standard of living across the life course. Am. J. Public Health 96, 818–825 (2006).
Po, J. Y. & Subramanian, S. Mortality burden and socioeconomic status in India. PLoS ONE 6, e16844 (2011).
Desai, S., Dubey, A., Joshi, B.L., Sen, M., Sharif, A., & Vanneman, R. India Human Development Survey Users’ Guide Release 03. University of Maryland and National Council of Applied Economic Research, New Delhi; 2010. Available: https://www.icpsr.umich.edu/icpsrweb/content/DSDR/idhs-data-guide.html.
Desai, S., Dubey, A., & Vanneman, R. India Human Development Survey-II Users’ Guide Release 01. University of Maryland and National Council of Applied Economic Research, New Delhi; 2015. Available: https://www.icpsr.umich.edu/icpsrweb/content/DSDR/idhs-II-data-guide.html.
Cleves, M., Gould, W., Gould, W. W., Gutierrez, R. & Marchenko, Y. An introduction to survival analysis using Stata 3rd edn. (Stata press, USA, 2013).
Bebbington, M., Lai, C.-D. & Zitikis, R. Modeling human mortality using mixtures of bathtub shaped failure distributions. J. Theor. Biol. 245, 528–538. https://doi.org/10.1016/j.jtbi.2006.11.011 (2007).
Juckett, D. A. & Rosenberg, B. Comparison of the Gompertz and Weibull functions as descriptors for human mortality distributions and their intersections. Mech. Ageing Dev. 69, 1–31. https://doi.org/10.1016/0047-6374(93)90068-3 (1993).
Snijders, T.A., & Bosker, R.J. Multilevel analysis: An introduction to basic and advanced multilevel modeling. Sage (2011).
Leckie, G. Three-level multilevel models-concepts. LEMMA VLE Module 11, 1–47 (2013).
Rabe-Hesketh, S. & Skrondal, A. Multilevel and longitudinal modeling using stata (Stata press, 2012).
Canette, I. In the spotlight: Intraclass correlations after multilevel survival models. 2016. Available: https://www.stata.com/stata-news/news31-2/intraclass-correlations/.
Austin, P. C., Wagner, P. & Merlo, J. The median hazard ratio: A useful measure of variance and general contextual effects in multilevel survival analysis. Stat. Med. 36, 928–938. https://doi.org/10.1002/sim.7188 (2017).
Linden, A., Mathur, M.B., & VanderWeele, T.J. EVALUE: Stata module for conducting sensitivity analyses for unmeasured confounding in observational studies. Statistical Software Components. Boston College Department of Economics; 2019. Available: https://ideas.repec.org/c/boc/bocode/s458592.html.
Linden, A., Mathur, M. B. & VanderWeele, T. J. Conducting sensitivity analysis for unmeasured confounding in observational studies using E-values: The evalue package. Stata J. 20, 162–175 (2020).
Collin, E.P. Stata command to compute collinearity diagnostics. UCLA: Academic Technology Services, Statistical Consulting Group (2010).
StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP (2015).
Filmer, D., & Scott, K. Assessing asset indices. The World Bank (2008).
Paul, R., Rashmi, R. & Srivastava, S. Association of mass media exposure with combustible and smokeless tobacco use among Indian population: findings from a panel survey. BMC Public Health 22, 125. https://doi.org/10.1186/s12889-021-12459-0 (2022).
Singh, P. K., Singh, L., Dubey, R., Singh, S. & Mehrotra, R. Socioeconomic determinants of chronic health diseases among older Indian adults: A nationally representative cross-sectional multilevel study. BMJ Open 9, e028426. https://doi.org/10.1136/bmjopen-2018-028426 (2019).
Ntenda, P. A. M. & Chuang, Y.-C. Analysis of individual-level and community-level effects on childhood undernutrition in Malawi. Pediatr. Neonatol. 59, 380–389. https://doi.org/10.1016/j.pedneo.2017.11.019 (2018).
MHA M of HA. Zonal Council. 2017. Available: https://web.archive.org/web/20170512022826/http://mha.nic.in/zonal_council.
Sibai, A. M. Mortality certification and cause-of-death reporting in developing countries. Bull. World Health Organ. 82, 83 (2004).
Hult, C., Stattin, M., Janlert, U. & Järvholm, B. Timing of retirement and mortality-A cohort study of Swedish construction workers. Soc. Sci. Med. 70, 1480–1486 (2010).
Bhat, M. Widows and Widowhood Mortality in India’ (1994).
Lillard, L. A. & Panis, C. W. Marital status and mortality: The role of health. Demography 33, 313–327 (1996).
Wu, J. & Li, J. The impact of social participation on older people’s death risk: an analysis from CLHLS. China Popul. Dev. Stud. 2, 173–185 (2018).
Falk, H. et al. Self-rated health and its association with mortality in older adults in China, India and Latin America—a 10/66 Dementia Research Group study. Age Ageing 46, 932–939 (2017).
de Jong, G. J., Dykstra, P. A. & Schenk, N. Living arrangements, intergenerational support types and older adult loneliness in Eastern and Western Europe. Demogr. Res. 27, 167–200 (2012).
Chatterjee, C., Nayak, N. C., Mahakud, J. & Chatterjee, S. C. Factors affecting the choice of health care utilisation between private and public services among the elderly population in India. Int. J. Health Plann. Manage. 34, e736–e751 (2019).
Brara, V. Culture and indigeneity: Women in Northeast India. Explor. E J. Indian Sociol. Soc. 72–90 (2017).
Devi, S.D., & Bagga, A. Ageing in women: A study in North-East India. Mittal Publications (2006).
Anstey, K. J., Luszcz, M. A. & Andrews, G. Psychosocial factors, gender and late-life mortality. Ageing Int. 27, 73–89 (2002).
Turra, C. M. et al. Determinants of mortality at older ages: The role of biological markers of chronic disease. Popul. Dev. Rev. 31, 675–698 (2005).
Desai, S., & Vanneman, R, National Council of Applied Economic Research NDelhi. India Human Development Survey (IHDS), 2005: Version 12. In: Inter-University Consortium for Political and Social Research (2008).
Desai, S., & Vanneman, R. India Human Development Survey-II (IHDS-II), 2011–12: Version 6 . In: Inter-University Consortium for Political and Social Research (2015).
Funding
This research received no specific grant from any funding agency, commercial entity or not-for-profit organization.
Author information
Authors and Affiliations
Contributions
Conceived and designed the research paper: R.P. and R.R.; analyzed the data: R.P.; wrote the manuscript: R.R.; refined the manuscript: R.P., R.R. All authors read and approved the final manuscript to be submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Paul, R., Rashmi Risk factors and clustering of mortality among older adults in the India Human Development Survey. Sci Rep 12, 6644 (2022). https://doi.org/10.1038/s41598-022-10583-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-022-10583-4
This article is cited by
-
Socioeconomic and geographic variations of disabilities in India: evidence from the National Family Health Survey, 2019–21
International Journal of Health Geographics (2024)
-
Insights on Poverty-based Inequality in Old-age Mortality in India
Discover Public Health (2024)
-
Migration status, physical limitations and associated self-rated health: a study of older Indian adults
BMC Geriatrics (2023)