Abstract
Fine-needle aspiration biopsy (FNAB) is a routine diagnostic test for thyroid nodules. The use of local anesthesia (LA) before the procedure is still controversial. This prospective study aimed to evaluate the degree of pain and specimen adequacy in liquid-based cytology (LBC) for FNAB of thyroid nodules with and without LA. A total of 100 consecutive patients with thyroid nodules who underwent FNAB with and without LA between January and December 2020 were included. Patients who received LA had a significantly lower immediate pain scale score (P = 0.01). Multivariate analysis demonstrated that no use of LA (odds ratio [OR] = 3.48, 95% confidence interval [CI] = 1.50–8.10, P = 0.004) and lesion abutting the trachea (OR = 6.14, 95% CI = 1.56–24.12, P = 0.009) were independently and significantly associated with pain degree immediately after FNAB. A higher proportion of patients who previously underwent FNAB thought that LA was helpful and should be performed prior to FNAB. However, the use of LA did not improve the specimen adequacy (P = 0.075). The results showed that administration of LA with a proper technique before ultrasound-guided FNAB might reduce immediate pain after the procedure, and patients may experience more pain when the aspirated nodules abut the trachea.
Similar content being viewed by others
Introduction
Aspiration biopsy is a well-established technique that has been implemented in clinical practice over the past 150 years and is the recommended first line investigation for evaluation of masses, especially those in the head and neck area. Owing to its safety, accuracy, and simplicity, fine-needle aspiration biopsy (FNAB) of the thyroid gland remains the most cost-effective, accurate, and routinely used diagnostic tool in the initial evaluation of thyroid nodules1,2,3,4,5,6.
The factors that influence specimen adequacy during FNAB remain unclear. An ideal FNAB procedure should provide adequate specimens for cytological diagnosis, with minimal patient discomfort. The benefits and necessity for administering local anesthesia (LA) before FNAB are controversial and highly debated.
Compared to conventional smear (CS), liquid-based cytology (LBC) employs advanced concentration techniques to reduce the number of unsatisfactory and false positive results and has significantly improved cytodiagnostic accuracy7,8. Over time, LBC may replace the CS technique when performing thyroid FNAB, since LBC is useful for the cytological analysis of blood-contaminated aspirates; blood contamination of aspirates can occur due to the high vascularity of a thyroid nodule or the use of a large-caliber needle7,8,9.
The purpose of our study was to evaluate pain intensity levels in ultrasound-guided FNAB with or without LA in patients with thyroid nodules. Additionally, the influence of LA on the specimen adequacy of LBC was assessed.
Results
Patient characteristics
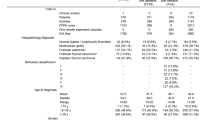
Between January and December 2020, 100 consecutive patients with thyroid nodules who underwent FNAB were enrolled. These patients had a median age of 53.0 (interquartile range, 42.0–62.0) years, and 67 (67.0%) were female. FNAB was performed with LA in 48 (48.0%) patients, and without LA in 52 (52.0%) patients. Patients with LA had a significantly greater proportion of previous FNAB experiences (70.8% vs. 34.6%, P < 0.001) than those without LA. There was no significant difference between the groups regarding demographics, procedural time, and nodule characteristics (Table 1).
Results of pain assessment
As presented in Table 2, the distribution of pain scores immediately after FNAB was significantly different between patients with and without LA (P = 0.010). The group with LA use had a significantly lower level of pain intensity immediately after the procedure. At 5 min after the procedures, the difference in the degree of pain became insignificant between the two groups. Regarding the subjective experience of pain, the patients with LA reported more pain at the superficial site (54.8% vs. 29.4%, P = 0.03) and less stabbing pain (58.1% vs. 67.7%, P = 0.42) than those without LA. Among patients with prior FNAB experience, significantly more patients in the LA group considered this FNAB experience to be less painful (79.4% vs. 16.7%, P < 0.001) compared to those without LA. Meanwhile, patients with a previous experience in the LA group were significantly more likely to report that LA is necessary prior to FNAB compared to those without LA (79.4% vs. 5.6%, P < 0.001).
Cytological results
The non-diagnostic sample rate was 13% in our study (n = 100). Although the rate of specimen adequacy was higher in FNAB performed under LA, the result was not statistically significant (93.8% vs. 80.8%, P = 0.075) (Table 3). There was no significant difference in the Bethesda System for Reporting Thyroid Cytopathology between the two groups (P = 0.462).
Association of local anesthesia with pain
Ordinal logistic regression was used to evaluate factors associated with immediate post-procedure pain intensity (Table 4). For the univariate analysis, no LA (odds ratio [OR] = 2.94, 95% confidence interval [CI] = 1.33–6.51, P = 0.008) or lesion against trachea (OR = 6.48, 95% CI = 1.83–23.01, P = 0.004) were significantly related to immediate pain scale. The Wong-Baker FACES Pain Rating Scale immediately after the procedure was not associated with needle size (the average scores and standard deviations for 18 gauge needle and 21–23 gauge needles were 2.41 ± 1.24 vs. 2.73 ± 1.73), number of needle passes, depth of the nodule and American Thyroid Association (ATA) sonographic risk stratification. Six variables with P < 0.2 in the univariate analysis were included in the multivariate analysis, including procedural time, administration of LA, nodule size, lesion against the trachea, and specimen adequacy. The results of multivariate analysis revealed that no LA (OR = 3.48, 95% CI = 1.50–8.10, P = 0.004) and lesion against the trachea (OR = 6.14, 95% CI = 1.56–24.12, P = 0.009) were independently and significantly associated with the degree of pain immediately after FNAB (Table 4).
Discussion
FNAB is regarded as a simple, safe, and cost-effective tool for evaluating thyroid nodules7. One of the main reasons for patient dissatisfaction with service quality is pain during the procedure10. To this end, LA has been used in FNAB of thyroid nodules to reduce pain and improve patient satisfaction with the quality of services11,12. Administration of LA may facilitate multiple and more accurate aspirates without more pain. However, the requirement and indications for LA remain controversial. Several researchers13,14,15 suggested that FNAB should be performed without LA when only one needle puncture is used. However, Gursoy et al.16 confirmed that a topical anesthetic cream could provide effective and non-invasive analgesia during FNAB of thyroid nodules. In addition, Liao et al.17 reported that the use of LA was associated with not only lower immediate pain scales but also higher specimen adequacy.
To our best knowledge, the present study is the first prospective trial to compare the pain scale and specimen adequacy between groups receiving FNAB of thyroid nodules with or without LA using LBC. We found no significant differences in age; sex; size, depth, and composition of thyroid nodules; needle size; number of needle passes; procedures; ATA nodule sonographic patterns; and risk of malignancy between the subjects receiving FNAB with or without LA. However, patients with LA had a higher rate of experience with FNAB (70.8% vs. 34.6%, P < 0.001). Administration of LA before FNAB was related to a significantly lower immediate pain scale score (P = 0.010), but this was not sustained at 5 min after the procedure (P = 0.356).
Several factors, including the use of LA16,17,18, characteristics of thyroid nodules17,19, and number of biopsied thyroid nodules20, have been reported to be associated with pain score after FNAB. However, the degree of pain after FNAB was not related to needle size21,22,23. In our study, we found that the absence of LA and the presence of a thyroid nodule against the trachea were independently and significantly associated with greater pain intensity after adjusting for multiple factors. Furthermore, among the patients with previous experience of FNAB, a higher proportion of the subjects who received LA felt less pain during this procedure and thought LA use is necessary compared with those without LA.
There are some differences between the results obtained in our study and those of previous reports and therefore our results should be interpreted cautiously. In our study, smaller caliber needles (27-gauge) were used for LA. A well-designed randomized controlled trial24 showed an inverse relationship between needle diameter and pain. In addition, we used 1% lidocaine instead of 2% lidocaine because 1% lidocaine or buffered lidocaine with bicarbonate may cause less discomfort than 2% lidocaine25. Finally, we waited for 10 s after subdermal injection of LA, and did not proceed with further administration of LA until the patient reported that the needle-puncture pain had disappeared. This pause allowed the local anesthetic to alleviate the pain caused by the needle piercing into the skin. If properly performed, this technique allows the subject to not feel any pain after the first puncture26.
It is worth noting that the subjects in our study had more intense pain when their thyroid nodules abutted the trachea. This phenomenon has not been previously discussed. The majority (~ 75%) of afferent activities from sensory terminals located in the airway, including the larynx and trachea, are mediated by non-myelinated C-fibers27. This may account for the pain sensation when the needle approached the trachea during FNAB. However, further studies should be conducted to clarify whether LA should be recommended in patients with lesions touching the trachea given that they are more likely to experience more pain during the procedure.
LBC has been used increasingly for thyroid FNAB because of its advantages over CS, including tolerance of bloody aspirates, less operator dependency on FNA, and the applicability of immunohistochemistry and molecular biology7,8. However, thyroid cytomorphology is more clearly seen on CS than in LBC28, and both of them are helpful, depending on the situation. In FNAB of thyroid nodules, the relationship between needle size and specimen adequacy in LBC is different from that in CS. No significant difference was found in the cytological adequacy between the different needle gauges using LBC22,23. To the best of our knowledge, no previous studies have assessed the effect of administration of LA on the specimen adequacy in LBC. Liao et al.17 reported that the use of LA was related to higher specimen adequacy in CS. However, our results demonstrated that regardless of whether the patients received LA or not, the rate of harvested cytological adequacy was not significantly different in LBC. The reason for this discrepancy is unclear, especially as LBC overcomes the drawback of bloody aspirate contamination that hinders visual analysis in CSs29. Further studies are required to clarify this matter.
The present study has several limitations. First, the patients with and without LA were not assigned randomly, and administration of LA was not performed in a blind method. No LA may affect the patient’s psychological expectation of pain, which has an influence on the pain scores. Second, our study included a relatively small number of participants, and there were far fewer male participants than female participants. Finally, the US-FNAB technique included only one sample with a single puncture. Accordingly, this study result should not be applied to FNAB with two or more samplings.
In conclusion, this study demonstrated that LA administration before FNAB using a proper technique reduced immediate pain after the procedure, and patients with thyroid nodules abutting the trachea may experience more pain during FNAB. Among the patients with previous experience of FNAB, a higher proportion of the subjects who received LA felt less pain during the procedure and thought LA use was necessary compared with those without LA.
Material and methods
Patient selection
This prospective study was conducted at Taipei Veterans General Hospital, a tertiary referral medical center, from January 2020 to December 2020. The study protocol was approved by the Institutional Review Board of the Taipei Veterans General Hospital (No. 2019-02-023A). All methods were performed in accordance with the relevant guidelines and regulations. Adult patients (aged > 20 years) who underwent ultrasound-guided FNAB for thyroid nodules were enrolled. Patients who underwent FNAB for assessment of cervical lymph nodes or other head and neck masses, had painful thyroid lesions, or had a history of allergy to LA were excluded. Written informed consent was obtained before the FNAB procedure from individual participants included in the study. All patient-identifiable data were anonymized.
Ultrasound-guided FNAB
Ultrasound-guided FNAB was performed by an experienced head and neck surgeon (L.-T.L.; has more than 5 years’ experience performing ultrasound-guided FNAB in over 1000 cases) using an Aloca Arietta 70 with a specialty transducer L55 high-resolution 13.0-MHz to 5.0-MHz 50 mm width real-time linear-array transducer. Patients were examined in the supine position with an extended neck for better exposure. The aspirated nodule was determined according to the most suspicious nodule on US visualization. The overlying skin area was sterilized with 75% alcohol solution.
Ultrasound-guided FNAB was performed using a freehand long-axis approach and positioning the linear array probe parallel to the needle for guidance. The needle was placed in the thyroid nodule under ultrasound guidance. A 21-gauge or 23-gauge needle attached to a 3-mL syringe was used for puncture, and an 18-gauge needle was applied for cystic or predominantly cystic (fluid component > 50%) thyroid nodules to drain the liquid content as much as possible. Only one needle puncture site was performed despite multiple needle passes, and the number of needle passes depended on the clinical suspicion.
Procedural data including needle size, number of needle passes during the procedure, and procedure time were collected. The characteristics of the nodules were also evaluated including the largest diameter of the thyroid nodule, depth of the nodule, whether the lesion abuts the trachea, presence of cystic lesions, and ATA nodule sonographic patterns and risk of malignancy30. The measures for the depth of the nodule included the distances between the skin and the superficial surface of the thyroid nodule (depth 1) and between the skin and the deepest surface of the thyroid nodule (depth 2).
FNAB with or without LA was performed alternatively in consecutive patients. Briefly, the first patient underwent FNAB without LA and the second patient underwent FNAB with LA. However, if the patient refused the arrangement, the next subject still followed the sequence. Therefore, less than half of the study patients received LA. First, approximately 0.2 mL of 1% lidocaine hydrochloride solution was injected subdermally. Following a 10 s pause, additional LA was injected after the patient reported that the needle-puncture pain had disappeared. The residual LA (a total of 1 mL) was injected into the soft tissue between the thyroid capsule and the skin overlying the target nodule with a 27-gauge needle attached to a 3-mL syringe.
Liquid-based cytology and cytological analysis
After centrifugation of the CytoLyt™ solution containing the aspirates, the obtained pellet was transferred to PreservCyt™ (Hologic-Cytyc Co.) solution and allowed to sit for 15 min. A single Papanicolaou-stained slide was prepared for each case using ThinPrep 5000 (Hologic-Cytyc Co.).
All ThinPrep slides were reviewed by two cytopathologists who specialized in cytological analysis of thyroid FNAB specimens and were blinded to the clinical data. Specimen adequacy was assessed using the Bethesda System for Reporting Thyroid31. The criteria for specimen adequacy consisted of at least six groups of follicular cells, and each group contained at least 10 cells and adequate cells for cytological analysis. Specimens that contained only abundant colloid or numerous inflammatory cells were considered inadequate. Specimens that consisted only of cystic contents were considered inadequate.
Pain assessment
The Wong-Baker FACES Pain Rating Scale29,32 was used to rate the degree of pain at two time points: immediately and 5 min after the completion of ultrasound-guided FNAB. The scale provides a six-item ordinal face scale. An incremental value of 2 is added for each face as the scale moves from to 0–10, ranging from a happy face at a pain score of 0 to a crying face at 10 (0 = no pain, 10 = worst pain). The patients were also interviewed after the procedure regarding the subjective experience of pain location (e.g., superficial, deep) and types of pain (e.g., stabbing, blunt, dull, pressure pain). Subjects who had previously undergone FNAB were also requested to compare the degree of pain between the two experiences (greater, similar, or less pain) and provide their opinion on the need for LA.
Statistical analysis
Categorical or ordinal variables were presented as counts (percentages) and continuous variables as medians (interquartile ranges). Comparisons between patients with and without LA were performed using Fisher’s exact test for categorical or ordinal variables, and the Mann–Whitney U test for continuous variables. Ordinal logistic regression was used to evaluate factors associated with pain degree immediately after FNAB. Variables with P < 0.2 in the univariate analysis were included in the multivariate model. Results of ordinal logistic regression analysis were presented as odds ratios (ORs) with 95% confidence intervals (CIs). Statistical significance was set at P < 0.05. All analyses were conducted using IBM SPSS Statistics for Windows version 26.0 (IBM Corp., Armonk, NY, USA).
References
Hegedüs, L. Clinical practice. The thyroid nodule. N. Engl. J. Med. 351, 1764–1771. https://doi.org/10.1056/NEJMcp031436 (2004).
Gharib, H. et al. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules: Executive summary of recommendations. J. Endocrinol. Investig. 33(Supplement), 51–56. https://doi.org/10.1007/BF03346587 (2010).
Castro, M. R. & Gharib, H. Continuing controversies in the management of thyroid nodules. Ann. Intern. Med. 142, 926–931. https://doi.org/10.7326/0003-4819-142-11-200506070-00011 (2005).
Gharib, H. Fine-needle aspiration biopsy of thyroid nodules: Advantages, limitations, and effect. Mayo Clin. Proc. 69, 44–49. https://doi.org/10.1016/s0025-6196(12)61611-5 (1994).
Mazzaferri, E. L. Management of a solitary thyroid nodule. N. Engl. J. Med. 328, 553–559. https://doi.org/10.1056/NEJM199302253280807 (1993).
Gharib, H. & Papini, E. Thyroid nodules: Clinical importance, assessment, and treatment. Endocrinol. Metab. Clin. North Am. 36, 707–735. https://doi.org/10.1016/j.ecl.2007.04.009 (2007).
Fadda, G. & Rossi, E. D. Liquid-based cytology in fine-needle aspiration biopsies of the thyroid gland. Acta Cytol. 55, 389–400. https://doi.org/10.1159/000329029 (2011).
Chang, H. et al. Comparison of diagnostic values of thyroid aspiration samples using liquid-based preparation and conventional smear: One-year experience in a single institution. APMIS 121, 139–145. https://doi.org/10.1111/j.1600-0463.2012.02944.x (2013).
Geers, C., Colin, I. M. & Gérard, A. C. Delta-like 4/Notch pathway is differentially regulated in benign and malignant thyroid tissues. Thyroid 21, 1323–1330. https://doi.org/10.1089/thy.2010.0444 (2011).
Rizvi, Z. et al. Service quality of diagnostic fine needle aspiration cytology in A tertiary care hospital of Lahore (process measure as Patient’s perspective). J. Ayub Med. Coll. Abbottabad 29, 93–97 (2017).
Rausch, P., Nowels, K. & Jeffrey, R. B. Jr. Ultrasonographically guided thyroid biopsy: A review with emphasis on technique. J. Ultrasound Med. 20, 79–85. https://doi.org/10.7863/jum.2001.20.1.79 (2001).
O’Malley, M. E. et al. US-guided fine-needle aspiration biopsy of thyroid nodules: Adequacy of cytologic material and procedure time with and without immediate cytologic analysis. Radiology 222, 383–387. https://doi.org/10.1148/radiol.2222010201 (2002).
Kim, D. W., Rho, M. H. & Kim, K. N. Ultrasound-guided fine-needle aspiration biopsy of thyroid nodules: is it necessary to use local anesthesia for the application of one needle puncture?. Korean J. Radiol. 10, 441–446. https://doi.org/10.3348/kjr.2009.10.5.441 (2009).
Yokozawa, T., Miyauchi, A., Kuma, K. & Sugawara, M. Accurate and simple method of diagnosing thyroid nodules the modified technique of ultrasound-guided fine needle aspiration biopsy. Thyroid 5, 141–145. https://doi.org/10.1089/thy.1995.5.141 (1995).
Danese, D., Sciacchitano, S., Farsetti, A., Andreoli, M. & Pontecorvi, A. Diagnostic accuracy of conventional versus sonography-guided fine-needle aspiration biopsy of thyroid nodules. Thyroid 8, 15–21. https://doi.org/10.1089/thy.1998.8.15 (1998).
Gursoy, A. et al. The analgesic efficacy of lidocaine/prilocaine (EMLA) cream during fine-needle aspiration biopsy of thyroid nodules. Clin. Endocrinol. 66, 691–694. https://doi.org/10.1111/j.1365-2265.2007.02802.x (2007).
Liao, L. J., Lo, W. C., Hsu, W. L., Cheng, P. W. & Wang, C. P. Assessment of pain score and specimen adequacy for ultrasound-guided fine-needle aspiration biopsy of thyroid nodules. J. Pain Res. 11, 61–66. https://doi.org/10.2147/JPR.S148088 (2018).
Gursoy, A. et al. Needle-free delivery of lidocaine for reducing the pain associated with the fine-needle aspiration biopsy of thyroid nodules: Time-saving and efficacious procedure. Thyroid 17, 317–321. https://doi.org/10.1089/thy.2006.0326 (2007).
Toman, H. et al. Effects of fine-needle aspiration biopsy (FNAB) nodule depth on pain score. Ir. J. Med. Sci. 185, 673–676. https://doi.org/10.1007/s11845-015-1337-y (2016).
Leboulleux, S. et al. Frequency and intensity of pain related to thyroid nodule fine-needle aspiration cytology. Thyroid 23, 1113–1118. https://doi.org/10.1089/thy.2012.0461 (2013).
Carpi, A. et al. Does large needle aspiration biopsy add pain to the thyroid nodule evaluation?. PLoS ONE 8, e58016. https://doi.org/10.1371/journal.pone.0058016 (2013).
Lee, Y. J. et al. Comparison of cytological adequacy and pain scale score in ultrasound-guided fine-needle aspiration of solid thyroid nodules for liquid-based cytology with with 23- and 25-gauge needles: A single-center prospective study. Sci. Rep. 9, 7027. https://doi.org/10.1038/s41598-019-43615-7 (2019).
Jung, S. J., Kim, D. W. & Baek, H. J. Comparison study of the adequacy and pain scale of ultrasound-guided fine-needle aspiration of solid thyroid nodules with a 21- or 23-gauge needle for liquid-based cytology: A single-center study. Endocr. Pathol. 29, 30–34. https://doi.org/10.1007/s12022-017-9508-1 (2018).
Arendt-Nielsen, L., Egekvist, H. & Bjerring, P. Pain following controlled cutaneous insertion of needles with different diameters. Somatosens. Mot. Res. 23, 37–43. https://doi.org/10.1080/08990220600700925 (2006).
Xia, Y., Chen, E., Tibbits, D. L., Reilley, T. E. & McSweeney, T. D. Comparison of effects of lidocaine hydrochloride, buffered lidocaine, diphenhydramine, and normal saline after intradermal injection. J. Clin. Anesth. 14, 339–343. https://doi.org/10.1016/s0952-8180(02)00369-0 (2002).
Lalonde, D. H. “Hole-in-one” local anesthesia for wide-awake carpal tunnel surgery. Plast. Reconstr. Surg. 126, 1642–1644. https://doi.org/10.1097/PRS.0b013e3181f1c0ef (2010).
Jammes, Y., Fornaris, E., Mei, N. & Barrat, E. Afferent and efferent components of the bronchial vagal branches in cats. J. Auton. Nerv. Syst. 5, 165–176. https://doi.org/10.1016/0165-1838(82)90037-6 (1982).
Mahajan, S., Rajwanshi, A., Srinivasan, R., Radotra, B. D. & Panda, N. Should liquid based cytology (LBC) be applied to thyroid fine needle aspiration cytology samples?: Comparative analysis of conventional and LBC smears. J. Cytol. 38, 198–202. https://doi.org/10.4103/JOC.JOC_6_17 (2021).
Abraham, T. M., de las Morenas, A., Lee, S. L. & Safer, J. D. In thyroid fine-needle aspiration, use of bedside-prepared slides significantly increased diagnostic adequacy and specimen cellularity relative to solution-based samples. Thyroid 21, 237–242. https://doi.org/10.1089/thy.2010.0211 (2011).
Haugen, B. R. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: What is new and what has changed?. Cancer 123, 372–381. https://doi.org/10.1002/cncr.30360 (2017).
Cibas, E. S. & Ali, S. Z. The 2017 Bethesda system for reporting thyroid cytopathology. Thyroid 27, 1341–1346. https://doi.org/10.1089/thy.2017.0500 (2017).
Wong, D. L. & Baker, C. M. Pain in children: Comparison of assessment scales. Okla. Nurse 33, 8 (1988).
Acknowledgements
This study was supported by the Taipei Veterans General Hospital (grant number V109C-184).
Author information
Authors and Affiliations
Contributions
Conception and design: T.L.L. and S.K.T. Development of methodology: T.L.L. Technical or material support: T.L.L and P.Y.W. Data collection, statistical review and manuscript drafting: T.L.L. Data verification, statistical review and manuscript revision: S.K.T. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
All authors declare that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, TL., Wei, PY. & Tai, SK. Effect of local anesthesia on pain scale and specimen adequacy in fine-needle aspiration biopsy of thyroid nodules for liquid-based cytology. Sci Rep 12, 18498 (2022). https://doi.org/10.1038/s41598-022-23031-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-022-23031-0