Abstract
Disordered eating behaviors (DEB) are more common in adolescents with type 1 diabetes (T1D) than in peers without diabetes. Emotional eating is a risk factor for binge eating in children and adolescents in the general population and is associated with increased intake of high energy-dense foods rich in sugars and fats. The primary objective is to evaluate whether emotional eating is associated with the metabolic control (glycated hemoglobin, plasma lipids and uric acid) in children and adolescents with type 1 diabetes and whether subjects with DEB (DEPS-R ≥ 20) have higher emotional eating than those without DEB. The secondary objective is to evaluate whether emotional eating is associated with the different symptoms of DEB. Emotional eating is positively correlated with HbA1c, total and LDL cholesterol values in children and adolescents with T1D. Subjects with DEB have a higher emotional eating score than subjects without DEB. Disinhibition is the most common disordered eating behavior in children and adolescents with T1D and is associated with a higher emotional eating score. Early identification and treatment of emotional eating could be tools for preventing DEB in people with type 1 diabetes. A total of 212 adolescents with T1D completed two self-administered questionnaires: the Diabetes Eating Problem Survey-Revised (DEPS-R) and the Emotional Eating Scale for Children and Adolescents (EES-C). Demographic (age, sex, duration of the disease), anthropometric (weight, height, BMI, BMI-SDS), therapeutic (type of insulin therapy, daily insulin dose) and metabolic (HbA1c, total cholesterol, HDL, LDL, triglycerides, uric acid) data were taken from the patients' medical records. The presence of other autoimmune diseases was also recorded.
Similar content being viewed by others
Introduction
Type 1 diabetes mellitus (T1D) is a chronic disease that requires lifelong insulin replacement therapy. This can be performed with multiple daily injections or with the use of an insulin pump and must be combined with blood glucose monitoring and quantification of carbohydrate intake at meals to establish the correct doses of insulin. This has a major impact on the quality of life of children with diabetes and their families and can lead to diabetes-related stress1. A recent national study in Sweden found that children and young people with T1D have more than twice the risk of psychiatric illness than their peers and siblings without diabetes2. Eating disorders (ED), after substance abuse, are the most frequent psychiatric disorders in adolescents with T1D and, as in the general population, predominantly affect females2,3.
Disordered eating behaviors (DEB) is a term that encompasses the whole spectrum of pathological behaviors related to eating, i.e., food restriction, excessive exercise to control body weight, binge eating, self-induced vomiting, and use of diuretics and laxatives. In DEB, these pathological behaviors often occur with reduced frequency and intensity that do not allow a diagnosis of ED4. Young people with diabetes also have another unique way of controlling body weight, which is the voluntary reduction/omission of insulin therapy, to induce hyperglycemia, glycosuria, ketonuria and weight loss5,6,7. DEB is also more common in young people with T1D than in peers without diabetes4,8,9. A recent Italian study performed in 690 adolescents with T1D aged 11–19 found a prevalence of DEB of 28.1% (21% in boys and 35% in girls). Teens with DEB were associated with higher HbA1c, BMI, and emotional and behavioral problems compared to adolescents without DEB. Furthermore, 39% of patients reduced/omitted insulin therapy and had higher glycated hemoglobin values than subjects who did not manipulate the therapy10. In some studies, the presence of DEB was also associated with alterations in plasma lipids11. These data are consistent with those of several other studies12,13,14. Binge eating is one of the most frequent DEB in screenings performed in adolescents with T1D (30%)15. A study performed in 506 Danish adolescents showed that 8.4% had overeating, 18% subclinical binge eating and 7.9% clinical binge eating. Patients with clinical binge eating (defined as ≥ 4 binge eating episodes over the past 28 days) had significantly higher HbA1c values than subjects without overeating16.
It is therefore very important to identify individuals at risk of developing DEB at an early stage. In 2010 Markovitz et al. proposed a screening questionnaire for DEB specific for people with diabetes, the Diabetes Eating Problem Survey—Revised (DEPS-R)17. This test, consisting of 16 items, allows the identification of individuals at higher risk of developing DEB who should be referred for psychiatric evaluation. The psychometric properties of the DEPS-R were subsequently confirmed by Wisting et al.18. Recently Calcaterra et al., starting from a clinimetric evaluation, proposed a division of the 16 items of the DEPS-R into four factors: restriction and body dissatisfaction, disinhibition, compensatory behaviors, and diabetes management, which are better suited than the original factors to the symptoms of DEB19,20.
Emotional eating is an eating pattern that consists of using food in response to negative emotions such as anxiety, sadness, loneliness, anger, and depression. It is frequent in children and adolescents of the general population and is considered a risk factor for binge eating21. It is associated with a dietary pattern characterized by the intake of hyperpalatable foods rich in sugars and fats22,23,24. In 2007 Tanofsky-Kraff modified the Emotional Eating Scale for adults (EES)25 adapting it to use in children (Emotional Eating Scale adapted for use in children and adolescents, EES-C). This scale has good convergent and discriminating validity and adequate reliability in the test retest and is considered a suitable tool for assessing emotional eating in children and adolescents between 8 and 18 years26.
Currently, the role of emotional eating as a risk factor for DEB in children and adolescents with T1D has not been thoroughly investigated. A survey of a small number of patients showed that adolescents with T1D have a higher frequency of emotional eating than their peers and that this correlates positively with HbA1c values27. The identification and treatment of emotional eating in adolescents with T1D could be the subject of intervention for the prevention of DEB.
The primary objectives of this work are (a) to assess whether in children and adolescents with T1D the presence of emotional eating is associated with metabolic control (glycated hemoglobin, plasma lipids, uric acid), with demographic (age, sex, duration of diabetes), anthropometric (BMI-SDS), therapeutic (insulin delivery method, with pump or multiple daily injections, and total daily dose), and clinical variables (association with other autoimmune diseases) and (b) whether subjects with DEB have a higher emotional eating score than subjects who do not have DEB. The secondary objective is to evaluate whether emotional eating is associated with the different symptoms (factors) of DEB: disinhibition, compensatory behaviors, restriction and body dissatisfaction, as defined in the clinimetric evaluation of the work by Calcaterra et al. and the impact of each of these symptoms on metabolic control (glycated hemoglobin, plasma lipids, uric acid). Disinhibition is the main symptom of binge eating disorder and bulimia nervosa, compensatory behaviors of bulimia nervosa and anorexia nervosa binge/purge subtype. Finally, restriction and body dissatisfaction is the main symptom of anorexia nervosa.
Since the EES-C is validated in several languages but not in Italian, we have validated the Italian version of the scale28,29,30.
Results
Characteristics of participants
In this cross-sectional study, 216 patients with T1D were recruited, representing 70% of the subjects aged between 10 and 17 years followed in our centre. Four patients (2 males and 2 females) were excluded because their questionnaires were incomplete. The final sample consisted of 212 patients (59% males) with a mean age of 14.4 ± 2.1 years. Twenty-nine percent of patients were receiving insulin therapy using a pump and the remainder received multiple daily injections. The mean BMI-SDS was −0.26 (SD 0.99), and the median HbA1c value was 7% (IQR 6.6–7.9%). According to the literature data, females have higher HbA1c values than males31. Total cholesterol, LDL, and HDL were also higher, while uric values were lower. Patient characteristics are shown in Table 1.
Psychometric properties of the Italian version of the EES-C questionnaire
The internal consistency of the Italian version of the EES-C questionnaire was excellent: the Cronbach's alpha coefficient was 0.934 in the whole sample, 0.944 in males and 0.925 in females. The convergent validity is confirmed by the positive and significant correlation between the EES-C score and that of the DEPS-R (r = 0.325, p < 0.001).
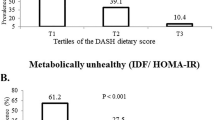
For the factor analysis, only components with an eigenvalue > 1 were extracted and after evaluation with Cattel's Scree test. The KMO value was 0.920 and the Bartlett test was significant. Three factors were extracted, which together explained 55% of the total variance of the items. Only items with a correlation > 0.40 were considered. The first factor was loaded by 12 items and explained 41% of the variance (eigenvalue 10.4). It represented food intake in response to unsettled and anxiety (unsettled and anxiety subscale, EES-C/UA). The second factor was loaded by 8 items, explained 8% of the variance (eigenvalue 1.9) and was related to symptoms of depression and frustration (depression and frustration subscale, EES-C/DF). Finally, the third factor was loaded by 5 items and accounted for 6% of the total variance (eigenvalue 1.4) and was correlated with symptoms of anger (anger subscale, EES-C/ANGER). Cronbach's coefficients for the three subscales were 0.848 for the EES-C/UA, 0.814 for the EES-C/DF and 0.925 for the EES-C/ANGER subscale. The three subscales were different from those in the original version of the EES-C questionnaire. Supplementary Table S1.
Results of the EES-C questionnaire
The median score on the EES-C questionnaire was 31 (IQR 11, 44) in the whole sample, 28.5 (IQR 7, 44) in boys and 33.5 (IQR 17, 42) in girls, without differences. By dividing patients into age groups (10–12 years, 13–15 years, 16–17 years), 16–17 years old had a higher EES-C score than 10–12 years old (33 ± 18 vs 24 ± 18, p = 0.015).
Results of the DEPS-R questionnaire
The mean score of the DEPS-R questionnaire score was 16 ± 11 and was higher in girls than in boys (18 ± 12 vs 14 ± 10, p = 0.007). There were no significant differences in the three age groups. In this study the internal consistency (Cronbach's alpha) of the DEPS-R questionnaire was good (0.84).
Relationship between EES-C score and study variables
Subjects in the higher quartile of EES-C score compared to those in the lower quartile had higher HbA1c values: 6.9% (IQR 6.7–8.1%) vs 6.7% (IQR 6.2–7.0%), p = 0.007. Total cholesterol, LDL and age were also significantly higher (Table 2). In the higher quartile of EES-C scores the prevalence of subjects with DEB was 39% compared to 11% in the lower quartile (p = 0.001) (Table 2).
Relationship between DEB and study variables
In the total sample 61 subjects had DEB (DEPS-R ≥ 20) (28.8%). The prevalence was significantly higher in girls than in males (41.9% vs 19.8% p < 0.001). Subjects with DEB had a higher EES-C test score than those without DEB: 35 (IQR 24, 46) vs 27 (IQR 6, 42) p = 0.001. This difference also persists when considering the two sexes separately: boys 37 (IQR 22, 44) vs 21 (IQR 5, 42) p = 0.041; girls 37 (IQR 24, 49) vs 32 (IQR 11, 38) p = 0.036. DEB subjects also had higher HbA1c, BMI-SDS and total cholesterol (Table 3). Dividing patients with DEB by age groups and comparing the EES-C score there were no significant differences (p = 0.38).
Multiple linear regression showed a significant correlation between DEPS-R score and HbA1c, BMI-SDS and EES-C score in the whole group and in boys and girls separately. Supplementary Table S2.
Relationship between DEB symptoms, emotional eating and metabolic control
In the total sample there were 49 (23.1%) patients with disinhibition. The EES-C score was higher than in subjects without disinhibition. BMI-SDS, HbA1c, total cholesterol and LDL-cholesterol were also higher. The number of patients with restriction and body dissatisfaction was 29 (13.4%). The EES-C score was not different from those of patients without the symptom. The HbA1c and BMI-SDS values were higher. Finally, compensatory behaviors were present in ten patients (4.7%). The EES-C score and the BMI-SDS were not different compared to subjects without the symptom. Glycated haemoglobin was higher. Comparisons between subjects with or without symptoms of DEB are presented in Table 4.
A total of 64 patients (30.2%) had symptoms of DEB: 41 had only one symptom (19.3%), 22 had two symptoms (10.4%) and only one patient had three symptoms (0.5%).
Discussion
Our study shows that emotional eating is related to metabolic control (HbA1c, plasma lipids) in patients with T1D aged 10–17 years and that subjects with DEB have a higher emotional eating score than those without DEB.
To our knowledge this is the first work to specifically study emotional eating in pediatric T1D and correlate it with DEB. Wheleer et al., investigating the relationship between intuitive eating and metabolic control in a group of 38 adolescents with T1D, found a higher frequency of emotional eating than in a control group and a positive relationship with HbA1c values. However, the study, which was carried out on a small number of patients, did not analyse the relationship between emotional eating and DEB27.
Recent studies in adults with T1D have shown that binge episodes and voluntary reduction of insulin therapy are preceded by an intensification of negative emotional states in the periods immediately preceding them. Guilt, frustration, and stress related to the burden of diabetes are the main negative emotions reported by patients32,33.
In this study, emotional eating, i.e. the use of food to cope with negative emotions, was greater in older adolescents (16–17 years), but there were no significant gender differences. Subjects with higher EES-C scores had higher HbA1c, total and LDL cholesterol values. These alterations in plasma lipids could be linked to an increased intake of energy-dense foods rich in sugars and fats, as described in adolescents with emotional eating in the general population22,23,24.
Emotional eating was unrelated to the type of insulin therapy (with pump or multiple daily injections) and to associations with other autoimmune diseases.
In our sample of children and adolescents, the prevalence of DEB was 28%, the same as found in a large national Italian sample of adolescents with T1D10 and in agreement with literature data, the prevalence was higher in girls than in boys. Subjects with DEB had higher HbA1c, BMI-SDS, total and LDL cholesterol values than those without DEB10,11,12,13,14.
Subjects with DEB had a significantly higher EES-C score than subjects without DEB, and this finding persisted even when considering boys and girls separately. When divided by groups age, there were no significant differences in subjects with DEB comparing the EES-C scores, which may mean that the emotional eating plays the same role in early, middle, and late adolescence.
Our choice to consider positive to the items of the DEPS-R only patients who respond very often/always allowed us to select those who have clinically relevant symptoms. Nevertheless, 30% of the T1D adolescents in our sample had at least one symptom of DEB.
Disinhibition (overeating and binge eating) was the most frequent symptom of DEB in our patients with T1D (22.7%). Patients with disinhibition have a significantly higher EES-C score than those without the symptom. HbA1c and BMI-SDS were also higher. Binge eating, is the main symptom of binge eating disorder and bulimia nervosa and in both pathologies it is strongly associated with emotional eating34,35. Our study shows that even in children and adolescents with T1D, overeating and binge eating are associated with emotional eating. In youth with T1D, binge eating is associated with psychosocial and physiological factors related to the disease36,37. It can be triggered by the inability to cope with negative emotions that are neutralized by the use of food32. In this, a potential role can be played by diabetes-specific distress, which refers to the negative emotions arising from living with diabetes and the burden of self-management and was reported in one in three adolescents with T1D38,39. Dealing with emotion is one of the diabetes-specific stressors found by Chao et al. in a sample of 205 early adolescents with T1D. The others were just having diabetes and managing diabetes40. Dealing with emotions included uncertainty about the future and the lifelong responsibility of diabetes. This agreed with the result of the Exploratory Factor Analysis of the EES-C questionnaire that highlights the high importance of the unsettled and anxiety factor. In addition, binge episodes can be a consequence of food restriction with a violation of abstinence resulting in loss of control eating41. Finally, large glycemic fluctuations due to insulin therapy can lead to hypothalamic dysregulation of hunger and satiety cues. During hypoglycemic episodes, patients experience intense hunger with loss of control eating and overeating37.
Restriction and body dissatisfaction (diet, omission of meals, and internalization of thinness), was present in 13.4% of our children and adolescents with T1D. These patients have an EES-C score similar to those of subjects without the symptom. The values of HbA1c are instead significantly higher. Food restriction and internalization of thinness are the main symptoms of anorexia nervosa (AN). In adolescents most forms of anorexia nervosa are of the restrictive type42,43 without bingeing and purging, which could justify the lack of high value for emotional eating. Unexpectedly, subjects with restriction and body dissatisfaction had a higher BMI-SDS than subjects without the symptom. It can be hypothesized that in patients with T1D, subjected to dietary rules associated with insulin therapy, the dietary restriction may be only cognitive and not also associated with a calorie restriction. However, this aspect was not addressed in our study. Also, patients who restrict may be more likely to experience hypoglycemic episodes that require intake of high-calorie sugary foods. Restriction can be also strongly associated with episodes of overeating.
Finally, compensatory behaviors (insulin reduction/omission and self-induced vomiting), the main symptom of bulimia nervosa and anorexia nervosa subtype binging/purging, was the least frequent symptom in our sample of T1D patients (4.6%). The EES-C scores were higher than in subjects without the symptom but the difference was not significant (p = 0.06). HbA1c values are higher. In our case series, compensatory behaviors consisted almost exclusively of subjects who reduced/omitted insulin therapy while only one patient had self-induced vomiting (0.5%). Literature data agree that the omission of therapy is responsible for the worsening of metabolic control5,6,7. The reduction/omission of insulin therapy is likely to be linked to psychological processes other than emotional eating, such as denial of the disease, self-destructive and suicidal ideation, and fear of severe hypoglycemia as observed in the study of Schober44.
Our study shows that the Italian version of the EES-C questionnaire presented excellent internal consistency and acceptable convergent validity. The factors are different from those of the original questionnaire but this probably reflects the emotional situation of young people with type 1 diabetes. The original EES-C questionnaire was validated in 159 normal weight or overweight subjects aged 8–18 years.
The high importance of the unsettled and anxiety component, compared to the original EES-C questionnaire, probably reflects the difficulties faced in the daily management of diabetes. Metabolic control depends on a large number of components, including insulin therapy, ingested carbohydrates, physical activity, emotional state, and stress, which often frustrate the patient's work and commitment, causing persistent uncertainty in achieving optimal blood sugar levels45.
Our study has several limitations. First, it is a cross-sectional study and does not allow us to draw causal relationships between emotional eating and DEB. Second, it is monocentric so the data cannot be extended to all subjects with T1D. However, they can be considered representative of children and adolescents with diabetes in Sardinia because our centre follows more than 50% of patients in the region from all areas of the island. Finally, the questionnaire Emotional Eating Scale for Children and Adolescents, in its original version, does not have a cut-off value so it is not possible to classify subjects as suffering from emotional eating and this should be the subject of another study.
In conclusion, our study shows that emotional eating is positively correlated with HbA1c and plasma lipids in patients with T1D and that subjects with disordered eating behaviors have a higher emotional eating score than those without DEB. All symptoms of DEB (disinhibition, compensatory behaviors, restriction and body dissatisfaction) were associated with a higher emotional eating score, but only for disinhibition the effect was significant. All symptoms were also associated with higher HbA1c values. Patients with T1D and disinhibition, have also higher BMI and plasma lipids values than those without food dyscontrol. In these youth, emotional eating could be the subject of psychotherapeutic intervention with a preventive effect on DEB. Compensatory behavior and restriction and body dissatisfaction seem to be less related to emotional eating and are probably associated with different psychological processes.
Methods
Characteristics of participants
We studied patients with T1D aged 10–17 years followed in the Pediatric Diabetology Unit of ASL Cagliari, Italy. The subjects had been diagnosed with diabetes for at least 12 months and were autonomous in the administration of insulin therapy. Patients with a diagnosis of eating disorder already being treated or other psychiatric disorders (depression, autism, ADHD, etc.) were excluded from the study. Subjects with other chronic diseases (neurological, genetic, hematological, etc.) or an inability to understand the meaning of the questionnaires were also excluded.
Procedure
This cross-sectional study was conducted in the period January-December 2019 with the approval of the AOU Cagliari Ethics Committee. Patients were asked, at the end of a routine visit, to complete two questionnaires: the Diabetes Eating Problems Survey-Revised (DEPS-R) and the Emotional Eating Scale for Children and Adolescents (EES-C). The questionnaires were completed after written consent was obtained from both the parents and the recruited subjects.
Demographic and clinical data
Demographic (age, sex, duration of the disease), anthropometric (weight, height, BMI, BMI-SDS), therapeutic (type of insulin therapy, i.e., pump or multiple daily injections, daily insulin dose) and metabolic (HbA1c, total cholesterol, HDL, LDL, triglycerides, uric acid) data were taken from the patients' medical records. The presence of other autoimmune diseases associated with type 1 diabetes was also recorded: chronic thyroiditis, coeliac disease and chronic autoimmune gastritis (positivity for anti-parietal cell antibodies, APCA).
Glycated hemoglobin (HbA1c) was determined by the immunoturbidimetric method, using the Siemens DCA Vantage Analyser.
Questionnaires
DEPS-R
The DEPS-R is a self-administered questionnaire with 16 items, a Likert scale never/rarely/sometimes/often/very often/always, and a score from 0 to 5. A higher value indicates greater pathology. The questionnaire was validated in Italian46. In accordance with the previous studies subjects with a score of ≥ 20 were considered to have DEB10,47.
Furthermore, independent of the total score and in accordance with Calcaterra's work, the DEPS-R items were used to define subjects with disinhibition, compensatory behaviors, restriction and body dissatisfaction, which represent the main phenotypes of disordered eating behaviors. Patients who responded often/very often to at least one of the 4 items were considered positive for the symptom. Each subject can have more than one symptom (Table 5).
EES-C
The EES-C is a self-administered 25-item questionnaire with a Likert scale I have no desire to eat/I have a small desire to eat/I have a moderate desire to eat/I have a strong desire to eat/I have a very strong desire to eat and a score from 0 to 4. The questionnaire examines the desire to eat in response to 25 different emotions26. Higher values indicate greater emotional eating. The EES-C questionnaire has three subscales: Anxiety/anger/frustration subscale, Depression subscale, and Unsettled subscale. The questionnaire was not validated in Italian so the original version was translated into Italian by a team with a diabetologist, a pediatrician and a psychologist with experience in diabetes and eating disorders. The draft of the Italian instrument was then retranslated into English by a native speaker interpreter and finally revised by the research team to evaluate any corrections. The translated items were then pretested to evaluate their comprehensibility on a small sample of 10 adolescents with type 1 diabetes followed in our center.
Statistical analysis
The internal consistency of the EES-C questionnaire was assessed using Cronbach's alpha. Values > 0.90 indicate an excellent consistency, values between 0.70 and 0.90 indicate good consistency, values between 0.60 and 0.70 indicate acceptable consistency, values between 0.50 and 0.60 indicate poor consistency, and values < 0.50 indicate unacceptable consistency48. For convergent validity, the correlation with the score of the DEPS-R questionnaire was assessed using Person's correlation coefficient (r) because binge eating, the most frequent symptom of DEB in adolescents with type 1 diabetes, is correlated with emotional eating21.
Then, we performed an Exploratory Factor Analysis (EFA) using the principal axis factoring method with varimax rotation, the same as those used by Tanofsky in his work validating the EES-C questionnaire in children and adolescents26. To assess the appropriateness of the data for factor analysis, the Kaiser–Meyer–Olkin (KMO) test for measuring sample adequacy and Bartlett’s test for sphericity were used. KMO should be > 0.50 and the chi-square value of Bartlett's test should be significant49.
Continuous distributed variables are expressed as the mean and standard deviation, otherwise they are expressed as the median and interquartile range (IQR). Categorical variables are presented as absolute numbers and percentages. The EES-C and DEPS-R questionnaires were analysed as a total score, and then divided by gender and age groups (10–12, 13–15, 16–17 years).
Since the EES-C scale does not have a cut-off value, to evaluate the association of emotional eating with the study variables, the total sample of diabetic patients was divided into quartiles based on the EES-C score values. The first and fourth quartiles were compared to evaluate the differences between demographic (age, sex, duration of diabetic disease), anthropometric (BMI-SDS), therapeutic (type of insulin therapy, daily insulin dose), metabolic (HbA1c, total cholesterol, HDL, triglycerides, uric acid) and clinical variables (association with other autoimmune diseases).
Subsequently, subjects with DEB (DEPS-R score ≥ 20) were compared with subjects without DEB for all study variables.
To evaluate the effects of the study variables on the DEPS-R score, a linear regression analysis was performed using the DEPS-R score as a dependent variable and the EES-C score, demographic, anthropometric, therapeutic, metabolic and clinical variables as independent variables. Tolerance values > 0.1 were considered acceptable to rule out multicollinearity. Variables with skewness and/or kurtosis >| 1 | (HbA1C and EES-C score) were transformed (square root) to perform linear regression analysis and Pearson's correlation.
Finally, to evaluate the association of the three symptoms of DEB with the EES-C score and with the metabolic variables (HbA1c, total cholesterol, HDL, triglycerides, uric acid) we created three groups: the first group included all patients with disinhibition, the second group included those with restriction and body dissatisfaction, and the third group included those with compensatory behaviors. Each nonexclusive group was compared with all subjects without the corresponding symptoms for the values of the variables indicated above.
For comparisons between groups, the two-tailed t test or the Mann–Whitney test was used when indicated. For the comparison between categorical variables the chi-square test was used. One-way analysis of variance with Tukey's post hoc test was used for comparisons between age groups. Values of p < 0.05 were considered significant. Statistical analysis was performed with the SPSS 28.0 package.
Ethical approval
The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards and was approved by the AOU Cagliari Ethics Committee.
Informed consent
Informed consent was obtained from all study participants.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Hilliard, M. E. et al. Screening and support for emotional burdens of youth with type 1 diabetes: Strategies for diabetes care providers. Pediatr. Diabetes. 19, 534–543 (2018).
Butwicka, A., Frisén, L., Almqvist, C., Zethelius, B. & Lichtenstein, P. Risks of psychiatric disorders and suicide attempts in children and adolescents with type 1 diabetes: a population-based cohort study. Diabetes Care 38, 453–459 (2015).
Mannucci, E. et al. Eating disorders in patients with type 1 diabetes: A meta-analysis. J. Endocrinol. Invest. 28, 417–419 (2005).
Young, V. et al. Eating problems in adolescents with type 1 diabetes: A systematic review with meta-analysis. Diabet. Med. https://doi.org/10.1111/j.1464-5491.2012.03771.x (2013).
Wisting, L., Froisland, D. H., Skrivarhaug, T., Dahl-Jorgensen, K. & Ro, O. Disturbed eating behavior and omission of insulin in adolescents receiving intensified insulin treatment. A nationwide population-based study. Diabetes Care 36, 3382–3387 (2013).
Bachle, C., Stahl-Pehe, A. & Joachim Rosenbauer, J. Disordered eating and insulin restriction in youths receiving intensified insulin treatment: Results from a nationwide population-based study. Int. J. Eat. Disord. https://doi.org/10.1002/eat.22463 (2016).
Pinhas-Hamiel, O. et al. Detecting intentional insulin omission for weight loss in girls with type 1 diabetes mellitus. Int. J. Eat. Disord. https://doi.org/10.1002/eat.22138 (2013).
Colton, P., Olmsted, M., Daneman, D., Rydall, A. & Rodin, G. Disturbed eating behavior and eating disorders in preteen and early teenage girls with type 1 diabetes. Diabetes Care 27, 1654–1659 (2004).
Broadley, M. M. et al. 25 Years of psychological research investigating disordered eating in people with diabetes: What have we learnt?. Diabet. Med. 37, 401–408 (2020).
Troncone, A. et al. Prevalence of disordered eating behaviors in adolescents with type 1 diabetes: Results of multicenter Italian Nationwide study. Int. J. Eat. Disord. https://doi.org/10.1002/eat.23764 (2022).
Cherubini, V. et al. Disordered eating behaviors in adolescents with type 1 diabetes: A cross-sectional population-based study in Italy. Int. J. Eat. Disord. https://doi.org/10.1002/eat.22889 (2018).
Nilsson, F., Broby Madsen, J. O., Kryger Jensen, A., Olsen, B. S. & Johannesen, J. High prevalence of disordered eating behavior in Danish children and adolescents with type 1 diabetes. Pediatr. Diabetes. https://doi.org/10.1111/pedi.13043 (2020).
Araia, E. et al. Gender differences in disordered eating behaviors and body dissatisfaction among adolescents with type 1 diabetes: Results from diabetes MILES youth—Australia. Int. J. Eat. Disord. 50, 1183–1193 (2017).
Altınok, Y. A. et al. Reliability and validity of the diabetes eating problem survey in Turkish children and adolescents with type 1 diabetes mellitus. J. Clin. Res. Pediatr. Endocrinol. 9, 323–328 (2017).
Jones, J. M., Lawson, M. L., Daneman, D., Olmsted, M. P. & Rodin, G. Eating disorders in adolescent females with and without type 1 diabetes: Cross sectional study. BMJ 320, 1563–1566 (2020).
Marks, K. P. et al. Overeating, binge eating, quality of life, emotional difficulties, and HbA1c in adolescents with type 1 diabetes: A Danish national survey. Diabetes Res. Clin. Pract. https://doi.org/10.1016/j.diabres.2021.109150 (2021).
Markowitz, J. T. et al. Brief screening tool for disordered eating in diabetes. Diabetes Care 33, 495–500 (2010).
Wisting, L., Dahl-Jorgensen, K., Froisland, D. H., Ro, O. & Skrivarhaug, T. Psychometric properties, norms, and factor-structure of the diabetes eating problem survey-revised in a large sample of children and adolescents with type 1 diabetes. Diabetes Care 36, 2198–2202 (2013).
Calcaterra, V. et al. Disturbed eating behaviors in youth with type 1 diabetes: An exploratory study about challenges in diagnosis. Diagnostics. https://doi.org/10.3390/diagnostics10121044 (2020).
Fava, G. A., Rafanelli, C. & Tomba, E. The clinical process in psychiatry: A clinimetric approach. J. Clin. Psychiatry. https://doi.org/10.4088/jcp.10r06444 (2012).
Allen, K. A., Byrne, S. M., La Puma, M., McLean, N. & Davis, E. A. The onset and course of binge eating in 8 to 13 year-old healthy weight, overweight and obese children. Eat. Behav. 9, 438–446 (2008).
Nguyen-Michel, S. T., Unger, J. B. & Spruijt-Metz, D. Dietary correlates of emotional eating in adolescence. Appetite 49, 494–499 (2007).
Bui, C., Lin, L. Y., Wu, C. Y., Chiu, Y. W. & Chiou, H. Y. Association between emotional eating and frequency of unhealthy food consumption among Taiwanese adolescents. Nutrients https://doi.org/10.3390/nu13082739 (2021).
Konttinen, E. J. K. et al. Emotional eating, health behaviours, and obesity in children: A 12-country cross-sectional study. Nutrients https://doi.org/10.3390/nu11020351 (2019).
Arnow, B., Kenardy, J. & Agras, W. S. The emotional eating scale: The development of a measure to assess coping with negative affect by eating. Int. J. Eat. Disord. 18, 79–90 (1995).
Tanofsky-Kraff, M. et al. Validation of the emotional eating scale adapted for use in children and adolescents (EES-C). Int. J. Eat. Disord. 40, 232–240 (2007).
Wheeler, B. J. et al. Intuitive eating is associated with glycaemic control in adolescents with type 1 diabetes mellitus. Appetite 96, 160–165 (2016).
Perpinà, C., Cebolla, A., Botella, C., Lurbe, E. & Torrò, M. I. Emotional eating scale for children and adolescents: Psychometric characteristics in a Spanish sample. J. Clin. Child. Adolesc. Psychol. 40, 424–433 (2011).
Kalogiratou, D. S. et al. Greek validation of emotional eating scale for children and adolescents. J. Mol. Biochem. 8, 26–32 (2019).
Bektas, M. et al. Psychometric properties of the Turkish version of the Emotional Eating Scale for children and adolescents. Eat. Behav. 22, 217–221 (2016).
Prigge, R., McKnight, J. A. & Wild, S. H. The Scottish Diabetes Research Network Epidemiology Group. International comparison of glycaemic control in people with type 1 diabetes: An update and extension. Diabetic. Med. https://doi.org/10.1111/dme.14766 (2021).
Moskovich, A. A. et al. Real-time predictors and consequences of binge eating among adults with type 1 diabetes. J. Eat. Disord. https://doi.org/10.1186/s40337-019-0237-3 (2019).
Merwin, R. M. et al. Momentary predictors of insulin restriction among adults with type 1 diabetes and eating disorder symptomatology. Diabetes Care https://doi.org/10.2337/dc15-0753 (2015).
Schaefer, L. M. et al. The role of affect in the maintenance of binge-eating disorder: Evidence from an ecological momentary assessment study. J. Abnorm. Psychol. https://doi.org/10.1037/abn0000517 (2020).
Reichenberger, J. et al. Emotional eating across different eating disorders and the role of body mass, restriction, and binge eating. Int. J. Eat. Disord. 54, 773–784 (2021).
Peterson, C. M., Fischer, S. & Young-Hyman, D. Topical review: A comprehensive risk model for disordered eating in youth with type 1 diabetes. J. Pediatr. Psychol. 40, 385–390 (2015).
Peterson, C. M. et al. Examination of psychosocial and physiological risk for bulimic symptoms in youth with type 1 diabetes transitioning to an insulin pump: A pilot study. J. Pediatr. Psychol. 43, 83–93 (2018).
Rechenberg, K., Whittemore, R., Holland, M. & Grey, M. General and diabetes-specific stress in adolescents with type 1 diabetes. Diabetes Res. Clin. Pract. https://doi.org/10.1016/j.diabres (2017).
Hagger, V., Hendieckx, C., Sturt, J., Skinner, T. C. & Speight, J. Diabetes distress among adolescents with type 1 diabetes: A systematic review. Curr. Diab. Rep. https://doi.org/10.1007/s11892-015-0694-2 (2016).
Chao, A. et al. General life and diabetes-related stressors in early adolescents with type 1 diabetes. J. Pediatr. Health Care https://doi.org/10.1016/j.pedhc (2015).
Elran-Barak, R. et al. Eating patterns in youth with restricting and binge eating/purging type anorexia nervosa. Int. J. Eat. Disord. https://doi.org/10.1002/eat.22289 (2014).
Herbrich, L., Kappel, V., van Noort, B. M. & Winter, S. Differences in set-shifting and central coherence across anorexia nervosa subtypes in children and adolescents. Eur. Eat. Disorders Rev. https://doi.org/10.1002/erv.2605 (2018).
Bat-Pitault, F., Da Silva, C., Charvin, I. & Da Fonseca, D. Sleep disturbances in anorexia nervosa subtypes in adolescence. Eat. Weight Disord. Stud. Anorexia Bulimia Obes. https://doi.org/10.1007/s40519-020-01033z (2020).
Schober, E. et al. Prevalence of intentional under- and overdosing of insulin in children and adolescents with type 1 diabetes. Pediatr. Diabetes. 12, 627–631 (2011).
Hoff, A. L., Mullins, L. L., Chaney, J. M., Hartman, V. L. & Domek, D. Illness uncertainty, perceived control, and psychological distress among adolescents with type 1 diabetes. Int. J. 16, 223–236 (2002).
Pinna, F. et al. Assessment of eating disorders with the diabetes eating problems survey—Revised (DEPS-R) in a representative sample of insulin-treated diabetic patients: A validation study in Italy. BMC Psychiatry https://doi.org/10.1186/s12888-017-1434-8 (2017).
Nip, A. S. Y. et al. Disordered eating behaviors in youth and young adults with type 1 or type 2 diabetes receiving insulin therapy: The SEARCH for diabetes in youth study. Diabetes Care https://doi.org/10.2337/dc18-2420 (2019).
Kline, P. The Handbook of Psychological Testing (Psychology Press, 2000).
Tabachnick, B. G. & Fidell, L. S. Using Multivariate Statistics (Allyn & Bacon/Pearson, 2007).
Author information
Authors and Affiliations
Contributions
C.R. and M.R.R. contributed to the conception, design, enrollment, clinical management of patients, acquisition of data and their analysis, drafted the manuscript, and provided final approval of the version to be published. E.Z., M.R.A., A.P.P., and D.R. contributed to the acquisition of data and their analysis, and provided final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
Carlo Ripoli has received a speaker honorarium from Eli-Lilly. Maria Rossella Ricciardi, Ester Zuncheddu, Maria Rosaria Angelo, Anna Paola Pinna, Daniela Ripoli have no conflicts of interest to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ripoli, C., Ricciardi, M.R., Zuncheddu, E. et al. Emotional eating and disordered eating behaviors in children and adolescents with type 1 diabetes. Sci Rep 12, 21854 (2022). https://doi.org/10.1038/s41598-022-26271-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-022-26271-2
This article is cited by
-
Efficacy of interventions to prevent eating disorders in people with type 1 diabetes: a systematic review
Journal of Eating Disorders (2026)
-
Uncovering distinct predictors of diabetes distress and depressive symptoms in a longitudinal survival analysis of incidence and remission: indication for diverging aetiological paths
Diabetologia (2026)