Abstract
To assess the effectiveness and safety of combining Saccharomyces boulardii powder with triple therapy as a primary approach for eradicating H. pylori infection, a total of 144 patients who tested positive for H. pylori and diagnosed with non-ulcer dyspepsia underwent endoscopy at two national centers between June 2017 and March 2019 were included. The patients were categorized into three groups using a subsection randomization method and received initial H. pylori eradication treatments. Microbial composition, eradication rates, symptom alleviation, and adverse reactions were monitored on the 14th and 44th days post-treatment. According to PP analysis showed the eradication rates for the SRAC group was 75%, BRAC was 93.18% and RAC was 65.2%. Group BRAC exhibited a marginally higher eradication rate compared to other groups. However, patients receiving Saccharomyces boulardii treatment exhibited an overall reduction in initial dyspepsia symptoms by the end of the treatment period. When employed as a primary strategy, the combination of Saccharomyces boulardii powder with triple therapy displayed notable efficacy and smaller gastrointestinal side effects in eradicating initial H. pylori infections among non-ulcer dyspepsia patients. Moreover, this approach demonstrated advantages in alleviating symptoms, exhibited favorable tolerance, and maintained a high level of clinical safety.
Similar content being viewed by others
Introduction
Helicobacter pylori (HP) stands as one of the most prevalent chronic infections in humans, bearing a close association with various upper gastrointestinal and extragastrointestinal disorders1. Comprehensive epidemiological studies in China underscore the potential of HP eradication in preventing gastric cancer and reversing precancerous lesions like gastric mucosal atrophy and intestinal metaplasia2. In 1994, the World Health Organization/International Agency for Cancer Research (WHO/IARC) designated Helicobacter pylori as a Class I carcinogen. The latest meta-analysis and epidemiological survey show that in recent years, the personal infection rate of Helicobacter pylori in Chinese Mainland is about 44.2%, but the domestic infection rate in China is as high as 71.21%3,4. Helicobacter pylori is closely related to gastric cancer, so eradication is vital importance. The expanding landscape of HP treatment has brought the challenge of drug resistance to the forefront, compromising the efficacy of eradication efforts. Presently, China recommends a 14-day, four-drug regimen featuring two antibiotics as the primary treatment, aimed at elongating the treatment duration and intensifying drug combinations to bolster eradication rates. However, this approach correlates with elevated adverse reactions5. In response, incorporating micro-ecological agents, mucosal protectors, and traditional Chinese medicine has emerged as a novel strategy to combat drug resistance and optimize eradication efficacy. Notably, the concept of “fighting bacteria with bacteria” has heightened interest in the role of probiotics in eradication treatment6.
Upon revisiting the role of probiotics in Helicobacter pylori eradication, in vitro experiments demonstrate the potential of lactobacillus (Lactobacillus acidophilus) or its byproducts to inhibit or eliminate Helicobacter pylori. Animal studies (involving Lactobacillus acidophilus) and clinical trials corroborate the efficacy of probiotics (including bifidobacterium, Lactobacillus acidophilus, and Enterococcus triple live bacteria) in bolstering the success of PPI triple therapy for Helicobacter pylori eradication. These probiotics also exhibit a capability to mitigate overall adverse reactions and specific symptoms, such as diarrhea, upper abdominal pain, nausea, and taste disruptions7,8. Nevertheless, the effectiveness of individual probiotic preparations varies, emphasizing the need for a targeted evaluation of single probiotics against Helicobacter pylori infection.
Among probiotic preparations, Saccharomyces boulardii (S. boulardii) reigns as a widely utilized contender. Homeyoung Zojaji et al. randomly enrolled 160 adult patients with biopsy confirmed Helicobacter pylori infection and divided them into a standard triple therapy combined with Saccharomyces boulardii group and a standard triple therapy group. The results showed no significant difference in eradication rates between the experimental group and the control group (87.5% vs. 81.2%)9. Similar results also appeared in another clinical study targeting children (71.4% vs. 61.9%, p > 0.05). The research results suggest that Saccharomyces boulardii can improve the eradication rate of Helicobacter pylori and reduce treatment-related side effects, especially diarrhea10. Nevertheless, another randomized controlled study compared standard triple therapy, Saccharomyces boulardii + standard triple therapy, and sequential therapy (89.1% vs. 77.1% vs. 95.5%, p < 0.05), and the results indicated that probiotic therapy was not superior to sequential therapy11. Research highlights the potential of Saccharomyces boulardii in enhancing eradication efficacy and reducing adverse reactions during Helicobacter pylori eradication. Nonetheless, the combined use of Saccharomyces boulardii with standard PPI triple therapy remains a subject of debate concerning both efficacy and safety. Moreover, the impact of this treatment on intestinal micro-ecology remains inadequately explored9,10. Therefore, this study aims to assess the effectiveness and safety of Saccharomyces boulardii powder when combined with triple therapy for Helicobacter pylori eradication. It also seeks to elucidate the influence of Helicobacter pylori treatment on intestinal micro-ecology and the predictive role of intestinal flora in treatment outcomes.
Material and methods
Patient enrollment
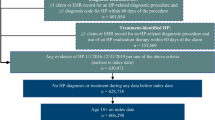
This clinical trial has been registered with the China Clinical Trial Registration Center (ChiCTR-IOR-16008610, 07/06/2016) and was approved by the Ethical Committee of Nanjing First Hospital, Nanjing Medical University (KY20160721-01). All methods were performed in accordance with the relevant guidelines and regulations. Between June 2017 and March 2019 from 2 medical centers in China, 144 patients between the ages of 18 and 65 years were enrolled in this study after receiving endoscopic evaluations for various GI symptoms. Each of these patients had rapid urease test proof of H. pylori infection, diagnosed as NUD and underwent initial HP eradication treatment. The inclusion criteria included (1) The diagnosis must be obtained through gastroscopy (within 1 month); (2) Positive for rapid urease test, positive for urea breath test within 2 weeks before or 1 month after gastroscopy; (3) Age 18 ~ 65 years old, gender unlimited; (4) Has not received formal eradication treatment of Helicobacter pylori in the past; (5) Have not taken any probiotics recently; (6) Sign informed consent. The exclusion criteria included (1) Those who have used antibiotics, bismuth agents or H2 receptor antagonist (H2RA) or proton pump inhibitor (PPI) within 4 weeks before treatment; (2) Pregnant or lactating women; (3) The patient also has other serious diseases that affect the evaluation of this study, such as severe liver disease, heart disease, cerebrovascular disease, kidney disease, malignant tumor and alcoholism; (4) Those who are allergic to the drugs used in this study; (5) Those who have participated in other drug research within 3 months; (6) Patient unable to correctly express their symptoms and wishes, unable to cooperate with the experimenter. Termination test criteria (1) Those who have serious adverse reactions during the test and cannot tolerate them; (2) Other diseases that interfere with the test during treatment; (3) Lost visit; (4) Pregnancy during treatment. We obtained informed consent from all subjects and their legal guardians.
Study design
This was a randomized, parallel-group study. 144 H. pylori-infected patients were recruited in the study and randomly assigned by a computer program into three groups: Group SRAC was treated with Saccharomyces boulardii powder + triple therapy (S. boulardii powder + rabeprazole + amoxicillin + clarithromycin. After 10 days, only Saccharomyces boulardii was given for 14 days). Group BRAC was treated with bismuth quadruple therapy (Rabeprazole + amoxicillin + clarithromycin + bismuth potassium citrate, 10 days). Group RAC was treated with triple therapy (Rabeprazole + amoxicillin + clarithromycin, 10 days). Patients assigned to Group SRAC received rabeprazole (Jichuan Pharmaceutical, Co. Ltd.,
Shanghai, China) 20 mg two times a day (bid); amoxicillin (Zhuhai United Laboratories Co, Ltd, Zhuhai,China) 1.0 g bid; clarithromycin (Abbott Laboratories Ltd, Shanghai, China) 500 mg bid; and S. boulardii powder (Laboratories Biocodex, Inc., France) 500 mg bid for 10 days. Additionally, S. boulardii powder was given for 4 days extend. Patients assigned to Group BRAC received bismuth quadruple therapy for 10 days. Bismuth potassium Citrate (Livzon Pharmaceutical Group, Inc., Zhuhai, China) 220 mg bid, the dosage frequency of other drugs is consistent with Group SRAC. Patients assigned to Group RAC received rabeprazole + amoxicillin + clarithromycin for 10 days, the drug dosage frequency is the same as Group SRAC. Considering the high resistance rate of metronidazole in the Center China population, we took amoxicillin and clarithromycin as our antibiotic choice. For patients who have failed their initial eradication, we provide a quadruple regimen of furazolidone 0.1 g bid + amoxicillin1.0 g bid + S. boulardii powder 500 mg bid + rabeprazole 20 mg bid for 10 days as remedial treatment. Continuing with the administration of S. boulardii powder only for an additional 14 days.
Study evaluations
Patients were evaluated at three visits: screening (0 day), end of treatment (14 days after the treatment initiation), follow-up the 13C-urea breath test 4 weeks after the therapy completion (44 day). A negative result is judged as Helicobacter pylori eradication. The patients were provided with stool for detection at each follow-up. Select patients who have successfully eradicated and provided three times stools for fecal microbiota analysis. After dividing and labeling fecal samples, the researchers immediately placed them in a − 80 ℃ refrigerator for freezing storage. The collected fecal samples were transported via cold chain to Tianjin Nuohe Zhiyuan Co., Ltd. for 16 s rRNA sequencing detection. Short term changes in gut microbiota before and after the eradication of Helicobacter pylori with the assistance of Saccharomyces boulardii powder combined with triple therapy. Record the patient's symptoms, improvement, medication, adverse reactions (such as nausea, abdominal pain, abdominal distension, diarrhea, and increased symptoms.) and other information in detail. Eradication rates were determined by both ITT- and PP-based analyses. All enrolled patients were included in the ITT analysis, but the PP analysis excluded those patients who dropped out due to side effects, loss to follow-up, or poor compliance.
16S rRNA gene amplicon pyrosequencing
According to the manufacturer protocols, we use the Stool DNA Kit (Omega Bio-tek, Norcross, GA, U.S) to extract DNA from the collected fecal samples. To measure the purity and concentration of microbial DNA, we use spectrophotometer and 2% agarose gel electrophoresis. Next step was the V3–V4 region of the bacteria 16S rRNA gene amplicon, inwhere two universal primers 338F(ACTCCTACGGGAGGCAGCAG) and 806R (GGACTACHVGGGTWTCTAAT) was used by PCR. The first step of PCR was 94 °C for 5 min, then did 28 cycles of 94 °C for 30 s, 55 °C for 30 s and 72 °C for 60 s, the final step was 72 °C for 7 min. Each PCR reaction system was consisted of 2X Taq Plus Master Mix (12.5 μL), BSA(3 μL with 2 ng/ul desity), 1.0 μL of each primer (5 μM), ddH2O and 30 ng of template DNA in a 25 μl volume. PCR products were collected and purified with QIAquick Gel Extraction Kit (QIAGEN, Germany).
Pooled purified amplicons at equimolar ratios, then paired-end sequenced (2 × 250) on an Illumina HiSeq2500 platform. The raw data were stored in the NCBI Sequence Read Archive (SRA) database. Using Trimmomatic to demultiplex and qualityfilter the raw fast files, and using silva to cluster Operational Taxonomic Units (OTUs) with 97% similarity cutoff. Then UCHIME was used to identify and remove chimeric sequences. The silva (SSU115) 16S rRNA database was analysed by RDP Classifier (http://rdp.cme.msu.edu/) with a confidence threshold of 70%. At each taxonomical level (Phylum, Class, Order, Family, and Genus), one analysis was performed respectively. The diversity of alpha (within samples) and beta (among samples) were analyzed by using Inhouse Perl scripts. The α diversity index was calculated by using Mothur software (version 1.31.2). The R (v3.1.1) software package is used for clustering analysis. UniFrac algorithm uses the information of system evolution to compare the differences of bacteria groups among samples, and makes further statistical analysis of the results12.
Statistical analysis
Data collected from all three groups were represented as the mean ± standard error of the mean (SEM). More than two groups’ datasets were evaulated by one-way ANOVA followed by Newman–Keuls post hoc tests. Among all three groups, statistical significance of nonparametric variables’differences was assessed by the nonparametric Turkey test followed by the Mann–Whitney U test when P < 0.05. The statistical analysis was performed by SPSS 25.0 software (Chicago, IL, USA).
Results
Baseline characteristics and eradication rates of the study population
A total of 144 individuals with H. pylori-positive non-ulcerative dyspepsia were enrolled in this study. These participants were randomly allocated to three treatment groups: SRAC (n = 48), BRAC (n = 48), and RAC (n = 48). Clinical parameters including age, gender, smoking status, BMI, endoscopic diagnosis, history of antibiotic exposure, past medical history and adverse event were consistent across all three groups. Eradication rates, assessed through both ITT and PP analyses, revealed a 75% eradication rate for group SRAC in both analyses. In group BRAC, ITT and PP analyses demonstrated eradication rates of 85.42% and 93.18%, respectively, while group RAC displayed rates of 62.5% (ITT) and 65.2% (PP). Two-group comparison tests established significant disparities in eradication rates across the groups (ITT analysis: SRAC vs. BRAC, p = 0.012; BRAC vs. RAC, p = 0.042) (PP analysis: SRAC vs. BRAC, p = 0.009; BRAC vs. RAC, p = 0.021). Particularly, group BRAC exhibited a marginally higher eradication rate compared to the other groups. Common adverse events included nausea, abdominal pain, abdominal distension, and diarrhea. The overall incidence of adverse events differed significantly among the three groups (p = 0.018), with a lower frequency of diarrhea observed in group SRAC compared to group BRAC (p = 0.01). Remarkably, patients receiving S. boulardii treatment exhibited an overall reduction in initial dyspepsia symptoms by the end of the treatment period (Table 1).
Comparison of fecal microbiome composition in Saccharomyces boulardii powder combined with triple therapy between treatment groups
For all three groups, fecal samples were subjected to sequencing of variable regions V4–V5 of the 16S rRNA gene using Illumina HiSeq/MiSeq platforms. This approach aimed to assess alterations in the gut microbial community. Operational taxonomic units (OTUs) were utilized to represent results with a 97% homology cutoff value (Fig. 1). Principal coordinates analysis (PCoA) exhibited distinct clustering of microbiota composition for each group (Fig. 2). A comparison of bacterial diversity before and after treatment revealed a significant diversity shift among the BRAC group (Fig. 2B, p < 0.05), whereas no significant diversity difference was observed for the SRAC and RAC groups around treatment (Fig. 2A, C). Following 14 days of treatment, the BRAC group displayed a more pronounced alteration in gut microbiota compared to the SRAC and RAC groups (p < 0.05), signifying a heightened impact of bismuth quadruple therapy on intestinal microecology. Diversity trends were reflected in Shannon and chao1 index analysis (Fig. 3), with all treatment groups demonstrating reduced diversity on the 14th day, followed by increased diversity on the 44th day. Lower community richness was observed in the RAC group compared to the other two groups (p < 0.05).
At the phylum level, the relative abundance of dominant taxa identified from sequencing across all three groups is illustrated in Fig. 4A, capturing specific gut microbiota changes. Prior to treatment, no significant variation in phylum levels was observed among the three groups, with Bacteroidota, Firmicutes, Proteobacteria, and Fusobacteria accounting for over 95% (p < 0.05). In the SRAC group, other prevalent bacteria included Actinobacteria, Acidobacteria, Tenericutes, Chloroflexi, Cyanobacteria, and Gemmatimonadetes. In the BRAC group, other notable bacteria encompassed Actinobacteria, Acidobacteria, Chloroflexi, Verrucomicrobia, Synergistetes, and Cyanobacteria. The RAC group exhibited additional dominant bacteria like Actinobacteria, Chloroflexi, Acidobacteria, Verrucomicrobia, Cyanobacteria, and Nitrospirae. Post-treatment, the relative abundance of Firmicutes decreased in the SRAC and BRAC groups, with subsequent recovery trends before treatment by the 44th day. In contrast, the RAC group displayed continuous Firmicutes abundance escalation following the 14th and 44th days of treatment. Changes in Bacteroidota, Proteobacteria, and Fusobacteria before and after treatment followed a similar pattern within each group. In the SRAC and RAC groups, relative abundance of Bacteroidota, Proteobacteria, and Fusobacteria declined after 14 days of treatment, rebounding after 44 days and reverting to pre-treatment trends. The converse was observed for the BRAC group, where these bacteria increased post-14-day treatment and decreased after 44 days.
At the genus level, variations in relative bacterial community abundance before and after treatment were evident, marked by distinct changes in bacterial genus composition with notable inter-individual differences. Bacteroides emerged as the most prevalent bacterium (Fig. 4B), and further details of intestinal bacteria composition are provided in Fig. 5. The SRAC group featured beneficial bacteria such as Bacteroides, Faecalibacterium, Prevotella_9, Lachnospiraceae_NK4A136_group, Roseburia, Lachnospira, Lachnoclostridium, and Parabacteroides. After 14 days of treatment, the SRAC group witnessed significant elevation in beneficial bacteria like Proteiniphilum and Anaerofustis (Fig. 5B, p < 0.05), along with a marked decrease in pathogenic bacteria including Helicobacter, Mycobacterium, Dialist, and Sanguibacteroides (Fig. 5B, p < 0.05). By the 44th treatment day, bacterial community abundance experienced a general increase. In the BRAC group, advantageous bacteria encompassed Bacteroides, Faecalibacterium, Prevotella_9, Escherichia-Shigella, Parabacteroides, Lachnoclostridium, and Roseburia. After 14 days of treatment, the BRAC group displayed notable increases in Faecalibacterium and Subdoligranulum (Fig. 5A, p < 0.05). On the 44th treatment day, Bifidobacterium, Collinsella, and Actinomyces showed higher abundances (Fig. 5A, p < 0.01), whereas Roseburia, Lachnospira, and Fusicatenibacters decreased significantly compared to pre-treatment levels (Fig. 5A, p < 0.05). In the RAC group, advantageous bacteria included Bacteroides, Prevotella_9, Fusobacterium, Faecalibacterium, Escherichia-Shigella, Parabacteroides, Roseburia and Sutterella. Following 14 days of treatment, the RAC group exhibited an increase in beneficial bacteria like Phascolarctobacterium (Fig. 5C, p < 0.05), coupled with a decrease in pathogenic bacteria such as Campylobacter, Streptococcus, Scardovia, Neisseria and Morganella (Fig. 5C, p < 0.05). By the 44th day of treatment, bacterial community abundance had risen compared to baseline. In summary, diverse treatment regimens yielded distinct impacts on intestinal microecology, with bismuth quadruple therapy displaying a more pronounced short-term interference on gut microbiota.
Disscusion
Helicobacter pylori, a prevalent Gram-negative microaerobic bacterium, has been a subject of continuous research since Warren and Marshall successfully cultured it from gastric mucosa in 1982. The widely employed standard PPI triple therapy since 1996, involving a proton pump inhibitor along with two antibiotics, has emerged as a prominent anti-Helicobacter pylori treatment globally, with treatment durations spanning 7–10 or even 14 days13,14,15. However, in recent years, escalating Helicobacter pylori drug resistance has led to the endorsement of bismuth quadruple therapy as the primary treatment approach in regions confronting high clarithromycin resistance, as recommended by the Maastricht and Toronto consensus16,17,18. Although bismuth quadruple therapy boasts a high eradication rate, it is accompanied by a significant incidence of associated side effects, including nephrotoxicity and potentially severe conditions like bismuth encephalopathy19. So it is crucial to urgently discover a new type of drug with high safety and effectiveness that can replace bismuth agents for the treatment of Helicobacter pylori. The integration of authoritative guidelines on Helicobacter pylori resistance also highlights the necessity of adding probiotics20.In light of emerging trends, microbiota research has gained prominence, prompting increased scholarly interest in harnessing probiotics as novel therapeutic regimens or supplementary agents for anti-Helicobacter pylori treatment8,21. In this context, our study endeavors to assess and compare the efficacy and safety of Saccharomyces boulardii in eradicating Helicobacter pylori combined with standard PPI triple therapy. Furthermore, our investigation committed to observing the changes in gut microbiota during the treatment, in order to find the potential correlations between gut microbiota and clinical efficacy.
Our randomized controlled trial stands as the sole recent experiment comparing the clinical efficacy of Saccharomyces boulardii combined with standard PPI triple therapy, simply standard PPI triple therapy, and a 10-day bismuth quadruple therapy. In a recent clinical meta ananlysis involving 15 RCT in children total 2156 patients, it was found that, Saccharomyces boulardii in combination with standard triple therapy was more effective than standard triple therapy alone and has a significantly lower incidence of total adverse events22. Another meta-analysis included 11 RCT with a total of 2200 patients, it was also mentioned that the addition of S. boulardii significantly increased the eradication rate and decreased some therapy-related side effects23. The novel and unique aspect of our research lies in exploring whether Saccharomyces boulardii can replace bismuth agents or can increase the eradication rate in the treatment of Helicobacter pylori. It is a worth noting that the eradication rate of the Saccharomyces boulardii combined with standard PPI triple therapy group is much higher than the standard PPI triple therapy group, but still significantly lower than that of the bismuth quadruple group. In a comprehensive clinical study incorporated 1620 participants, rigorously compare the clinical efficacy of bismuth quadruple therapy, standard triple therapy, and concomitant therapy. The results showed that the eradication rates were 90%, 84%, and 86%respectively. Bismuth quadruple therapy is the preferred first-line treatment option24. Similarly, for the regimen of omeprazole + clarithromycin + amoxicillin + bismuth potassium citrate, the eradication rate was as high as 93.7%. Even the eradication rate of drug-resistant strains far exceeded the expected 40%, reaching 84.6%25. In line with these findings, our study reports a bismuth quadruple therapy eradication rate of 93.94%, basically the same as them. Furthermore, our assessment of adverse reaction occurrences unveiled a substantially lower overall incidence in the Saccharomyces boulardii and standard PPI triple therapy group compared to the bismuth quadruple therapy cohort.
Probiotics, as active microorganisms, contribute to intestinal microbiota stability via anti-inflammatory and antioxidant mechanisms, thereby maintaining gut microbiota balance and inhibiting the proliferation of antibiotic resistant gut microbiota26,27. A recent meta-analysis found that probiotics as adjunctive drugs are effective in improving Helicobacter pylori eradication rates and reducing side effects. Analysis found no difference in efficacy between the use of a single probiotic or the combination use. Ranking the effectiveness of probiotics, it was found that the triple therapy with 10 days of adjunctive treatment using Saccharomyces boulardii or Lactobacillus was the most effective28. Furthmore, for Helicobacter pylori positive patients who have failed initial treatment, the natural clearance rate of exogenous administration of Saccharomyces boulardii alone is as high as 28%29. Saccharomyces boulardii, a resilient tropical fungus resistant to antibiotics, retains its potency when administered alongside antibiotics without genetic material transfer, thus ensuring safety. Our study capitalizes on Saccharomyces boulardii's capacity for stable colonization in the host intestinal tract after a two-week regimen30.
At present, the most important indicator for evaluating treatment plans is eradication rate, but there are still many other issues worth our attention, including antibiotic resistance and the impact of gastrointestinal microbiota. The use of antibiotics is actually a game process between short-term benefits and long-term risks for human health. Studies have also reported the long-term effects of antibiotics on gut microbiota, but individual differences and even intra individual differences are quite significant in the response to the same antibiotic31. In the triple therapy for H. pylori eradication, the addition of S. boulardii CNCM I-745 to the conventional antibiotic eradication therapy for H. pylori reduced the abundance of antimicrobial resistance genes, particularly those genes that confer resistance to lincosamides, tetracyclines, MLS-B, and a few genes in the beta-lactams class32.
At the phyla level, the composition and proportion of each sample varies at different phyla levels. Bacteroidetes and Firmicutes have the highest proportion, while the other top ranked phyla are Proteobacteria, Clostridium, Actinobacteria, Cyanobacteria and Acidobacteria. However, the result is not consistent with metagenomics. In 2022, Masoud et al. reported on the metagenomic changes in the microbiota before and after the addition of Saccharomyces boulardii in Helicobacter pylori eradication treatment, with Bacteroides, Clostridium, Ruinoccoccus, Dorea, Faecalibacterium, Vibrio, Thermotalia, and Lactobacillus being the dominant phylum33. However, there is still controversy over the differences in results due to different testing methods. In our study, Differential post-treatment changes in flora were observed across the three groups. After 14 days of treatment, the relative abundance of Bacteroidetes increased while the abundance of Firmicutes decreased in the Saccharomyces boulardii group and the standard triple group, while the changes in the bismuth quadruple treatment group were opposite. A recent microbiota analysis using lansoprazole, amoxicillin, and clarithromycin for the treatment of Helicobacter pylori. Although the drugs and doses are different, but the results are similar to ours. There is no significant difference in bacterial diversity before and after treatment34.
At the genus level, changes in the microbial community are more complex, but Bacteroides is the most common genus of bacteria both before and after treatment. After treatments, the relative abundance of the opportunistic pathogenic bacteria Escherichia and Shigella increased, with the bismuth quadruple group showing a more significant increase in abundance, ranking second in the bacterial changes after treatment and exhibiting statistical differences. Shigella is only present in humans and gorillas and is one of the main bacteria causing diarrhea35. This may explain why the bismuth quadruple group has a higher incidence of diarrhea compared to the other two groups. The abundance of Bacteroidetes in the Saccharomyces boulardii quadruple therapy group increased significantly after treatment. Bacteroidetes is a very important bacterium in the human gut and has a complex relationship with the host. Currently, most studies suggest that the genus Bacteroides can exert beneficial effects through mechanisms such as immune regulation, metabolism, and nutrition, and may play a protective role in the occurrence of side effects during the quadruple therapy with Saccharomyces boulardii36,37. The diversity of gut microbiota in the bismuth quadruple treatment group showed significant changes, indicating that bismuth may have a greater interfering effect on gut microbiota during the treatment process.
Our investigation further underscores the significantly reduced overall adverse reaction incidence and diarrhea rates in the Saccharomyces boulardii quadruple therapy group in comparison to the standard PPI triple therapy and bismuth quadruple therapy groups. Furthermore, the Saccharomyces boulardii and standard triple therapy group demonstrated superior clinical symptom relief and patient tolerance. Notably, the discernible distinctions in gut microbiota structure and function between the probiotic group and other cohorts highlight the regulatory impact of probiotic adjunct therapy on gut microbiota38. Consequently, the combined administration of Saccharomyces boulardii and standard triple therapy exhibits potential in minimizing post-treatment intestinal flora disturbances. Due to study duration limitations, the combination of Saccharomyces boulardii with standard PPI triple therapy fails to enhance the eradication rate achieved by standard PPI triple therapy, nor does Saccharomyces boulardii prove a viable replacement for bismuth in clinical treatment. Within the confines of the current sample size, we cautiously refrain from endorsing Saccharomyces boulardii as a complete substitute for bismuth or an unequivocal adjuvant in Helicobacter pylori treatment. Larger-scale clinical investigations are poised to provide more precise determinations in this regard. In addition, our analysis does not encompass the long-term effects on gut microbiota. Furthemore, for individual patients who failed eradication in each group, we have all provided remedial treatment. Unfortunately, there are still 6 patients who have failed. We all recommend them culturing with susceptibility testing or molecular determination of genotype resistance. There is no specific bacterial genera were found to potentially serve as predictive indicators for evaluating or predicting the eradication effect of Helicobacter pylori. In the future, future large-scale, high-quality, and multicenter RCTs need to carrry out to explor the potential microbial impact of Saccharomyces boulardii on Helicobacter pylori eradication.
Data availability
Data will be made available through publication and SRA database (PRJNA992363).
References
Goh, K. L. et al. Epidemiology of Helicobacter pylori infection and public health implications. Helicobacter 16(16 Suppl 1(0 1)), 1–9 (2011).
Li, Z. et al. Epidemiology of peptic ulcer disease: Endoscopic results of the systematic investigation of gastrointestinal disease in China. Am. J. Gastroenterol. 105(12), 2570–2577 (2010).
Ren, S. et al. Prevalence of Helicobacter pylori infection in China: A systematic review and meta-analysis. J. Gastroenterol. Hepatol. 37(3), 464–470 (2021).
Zhou, X. Z. et al. Large-scale, national, family-based epidemiological study on Helicobacter pylori infection in China: The time to change practice for related disease prevention. Gut 72(5), 855–869 (2023).
Liu, W. Z. et al. Fifth Chinese National Consensus Report on the management of Helicobacter pylori infection. Helicobacter 23(2), e12475 (2018).
Lesbros-Pantoflickova, D., Corthesy-Theulaz, I. & Blum, A. L. Helicobacter pylori and probiotics. J. Nutr. 137(3 Suppl 2), 812S-S818 (2007).
Zou, J., Dong, J. & Yu, X. Meta-analysis: Lactobacillus containing quadruple therapy versus standard triple first-line therapy for Helicobacter pylori eradication. Helicobacter 14(5), 97–107 (2009).
Myllyluoma, E. et al. Probiotic supplementation improves tolerance to Helicobacter pylori eradication therapy–A placebo-controlled, double-blind randomized pilot study. Aliment Pharmacol. Ther. 21(10), 1263–1272 (2005).
Zojaji, H. et al. The efficacy and safety of adding the probiotic Saccharomyces boulardiito standard triple therapy for eradication of H. pylori: A randomized controlled trial. Gastroenterol. Hepatol. Bed Bench 6(Suppl 1), S99–S104 (2013).
Bin, Z. et al. The efficacy of Saccharomyces boulardii CNCM I-745 in addition to standard Helicobacter pylori eradication treatment in children. Pediatr. Gastroenterol. Hepatol. Nutr. 18(1), 17–22 (2015).
Ozdil, K. et al. Levofloxacin based sequential and triple therapy compared with standard plus probiotic combination for Helicobacter pylori eradication. Hepato Gastroenterol. 58(109), 1148 (2011).
Zhang, Y. et al. Sulforaphane alter the microbiota and mitigate colitis severity on mice ulcerative colitis induced by DSS. AMB Express 10(1), 119 (2020).
Chey, W. D. et al. ACG clinical guideline: Treatment of Helicobacter pylori Infection. Am. J. Gastroenterol. 112(2), 212–239 (2017).
Liang, B. et al. Current and future perspectives for Helicobacter pylori treatment and management: From antibiotics to probiotics. Front. Cell. Infect. Microbiol. 12, 1042070 (2022).
Abadi, A. T. B. & Yamaoka, Y. Helicobacter pylori therapy and clinical perspective. J. Glob. Antimicrob. Res. 14, 111–117 (2018).
Fallone, C. A. et al. The Toronto consensus for the treatment of Helicobacter pylori infection in adults. Gastroenterology 151(1), 51-69 e14 (2016).
Malfertheiner, P. et al. Management of Helicobacter pylori infection-the Maastricht V/Florence consensus report. Gut 66(1), 6–30 (2017).
Malfertheiner, P. et al. Management of Helicobacter pylori infection: The Maastricht VI/Florence consensus report. Gut 71, 1724–1762 (2022).
Dore, M. P., Lu, H. & Graham, D. Y. Role of bismuth in improving Helicobacter pylori eradication with triple therapy. Gut 65(5), 870–878 (2016).
Fallone, C. A., Moss, S. F. & Malfertheiner, P. Reconciliation of recent Helicobacter pylori treatment guidelines in a time of increasing resistance to antibiotics. Gastroenterology 157(1), 44–53 (2019).
Madden, J. A. et al. Effect of probiotics on preventing disruption of the intestinal microflora following antibiotic therapy: A double-blind, placebo-controlled pilot study. Int. Immunopharmacol. 5(6), 1091–1097 (2005).
He, X. J. et al. The efficacy and safety of Saccharomyces boulardii in addition to antofloxacin-based bismuth quadruple therapy for Helicobacter pylori eradication: A single-center, prospective randomized-control study. Therap. Adv. Gastroenterol. 16, 17562848221147764 (2023).
Szajewska, H., Horvath, A. & Kolodziej, M. Systematic review with meta-analysis: Saccharomyces boulardii supplementation and eradication of Helicobacter pylori infection. Aliment Pharmacol. Ther. 41(12), 1237–1245 (2015).
Liou, J. M. et al. Concomitant, bismuth quadruple, and 14-day triple therapy in the first-line treatment of Helicobacter pylori: a multicentre, open-label, randomised trial. Lancet 388(10058), 2355–2365 (2016).
Sun, Q. et al. High efficacy of 14-day triple therapy-based, bismuth-containing quadruple therapy for initial Helicobacter pylori eradication. Helicobacter 15(3), 233–238 (2010).
Lv, Z. et al. Efficacy and safety of probiotics as adjuvant agents for Helicobacter pylori infection: A meta-analysis. Exp. Ther. Med. 9(3), 707–716 (2015).
Oh, B. et al. The effect of probiotics on gut microbiota during the Helicobacter pylori eradication: Randomized controlled trial. Helicobacter 21(3), 165–174 (2016).
Wang, F. et al. Probiotics in Helicobacter pylori eradication therapy: Systematic review and network meta-analysis. Clin. Res. Hepatol. Gastroenterol. 41(4), 466–475 (2017).
Qu, P. et al. Saccharomyces boulardii allows partial patients to avoid reusing bismuth quadruple for Helicobacter pylori rescue therapy: A single-center randomized controlled study. Front. Cell. Infect. Microbiol. 12, 903002 (2022).
Palma, M. L. et al. Probiotic Saccharomyces cerevisiae strains as biotherapeutic tools: Is there room for improvement?. Appl. Microbiol. Biotechnol. 99(16), 6563–6570 (2015).
Zaura, E. et al. Same exposure but two radically different responses to antibiotics: Resilience of the salivary microbiome versus long-term microbial shifts in feces. Mbio 6(6), 10–1128 (2015).
Cifuentes, S. G. et al. Saccharomyces boulardii CNCM I-745 supplementation modifies the fecal resistome during Helicobacter pylori eradication therapy. Helicobacter 27(2), e12870 (2022).
Keikha, M. & Kamali, H. The impact of Saccharomyces boulardii adjuvant supplementation on alternation of gut microbiota after H. pylori eradication; a metagenomics analysis. Gene Rep. 26, 101499 (2022).
Yanagi, H. et al. Changes in the gut microbiota composition and the plasma ghrelin level in patients with Helicobacter pylori-infected patients with eradication therapy. BMJ Open Gastroenterol. 4(1), e000182 (2017).
Kluge, E. W. Health Information Professionals in a Global eHealth World: Ethical and legal arguments for the international certification and accreditation of health information professionals. Int. J. Med. Inform. 97, 261–265 (2017).
Wexler, H. M. Bacteroides: The good, the bad, and the nitty-gritty. Clin. Microbiol. Rev. 20(4), 593–621 (2007).
Hooper, L. V. et al. Molecular analysis of commensal host-microbial relationships in the intestine. Science 291(5505), 881–884 (2001).
Cardenas, P. A. et al. Effect of Saccharomyces boulardii CNCM I-745 as complementary treatment of Helicobacter pylori infection on gut microbiome. Eur. J. Clin. Microbiol. Infect. Dis. 39(7), 1365–1372 (2020).
Funding
This work was supported by Shenzhen Science and Technology Planning Project (Grant Number KCXFZ20211020163558024).
Author information
Authors and Affiliations
Contributions
Y.C. and Z.Y.Z. designed the study. Y.Z. and B.Y.L. were responsible for the patient enrollment, follow-up and data analyses. Y.D. and Y.F.Z. obtained the gastroscopic examination and fecal collection. Y.Z. and Z.Y.Z. wrote the manuscript. QMD polished the article. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, Y., Lu, B., Dong, Y. et al. Saccharomyces boulardii combined with triple therapy alter the microbiota in the eradication of Helicobacter pylori infection. Sci Rep 14, 13152 (2024). https://doi.org/10.1038/s41598-024-63894-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-63894-z
Keywords
This article is cited by
-
Probiotics and prebiotics: new treatment strategies for oral potentially malignant disorders and gastrointestinal precancerous lesions
npj Biofilms and Microbiomes (2025)
-
Probiotic Saccharomyces boulardii Against Cronobacter sakazakii Infection: In Vitro and In Vivo Studies
Probiotics and Antimicrobial Proteins (2025)
-
Lactiplantibacillus plantarum ZJ316 Alleviates Helicobacter pylori-Induced Intestinal Inflammation by Sustaining Intestinal Homeostasis
Probiotics and Antimicrobial Proteins (2025)