Abstract
Double-lumen tubes (DLTs) are commonly used for one-lung ventilation (OLV) in thoracic surgery and the selection of an optimal size of DLTs is still a humongous task. The purpose of this study was to assess the feasibility and accuracy of the method for selecting an optimal size of DLTs in thoracic surgery. Sixty adult patients requiring a left side double-lumen tube (LDLT) for elective thoracoscopic surgery were included in this study. All patients were randomly allocated to the following two groups: Cuffs Collapsed group (CC group, n = 30) and Cuffs Inflated group (CI group, n = 30). In the Cuffs Collapsed group, the outer diameter of LDLT (the outer diameter of the tracheal and bronchial cuffs when they were collapsed as the outer diameter of the LDLT) matched with the inner diameter of the trachea and bronchus measured by the anesthesiologist on the chest CT slice; In the Cuffs Inflated group, the outer diameter of LDLT (the outer diameter of the tracheal and bronchial cuffs when they were inflated as the outer diameter of the LDLT) matched with the inner diameter of the trachea and bronchus measured by the anesthesiologist on the chest CT slice. The primary outcomes were the incidences of airway complications postoperative such as hoarseness and sore throat. The time of intubation and alignment, the incidences of LDLT displacement and adjustment, the peak airway pressure, the plateau airway pressure and the end-tidal carbon dioxide were also recorded. The incidences of airway complications postoperative such as sore throat and hoarseness were lower in the CI group than the CC group (P < 0.05), the intubation times was shorter in the CI group than the CC group (P < 0.05), while the peak airway pressure, the plateau airway pressure and the end-tidal carbon dioxide during two-lung ventilation and one-lung ventilation were no significant difference between two groups (P > 0.05). The method which matched the inner diameter of the trachea and bronchus measured on chest CT slice with the outer diameter of the tracheal and bronchial cuffs when they were inflated to select an appropriate size of LDLT can reduce the incidence of airway complications.
Trials registration: Clinical Trials: gov. no. NCT05739318. Registered at https://classic.clinicaltrials.gov 22/02/2023.
Similar content being viewed by others
Introduction
Trauma to the airway is the common complication after intubating of double-lumen tubes (DLTs) and the main reasons is excessive diameter of DLTs1. Oversize DLTs are difficult to intubate, which lead to forceful insertions or multiple intubations causing the injury of airway and teeth2, however, undersize DLTs can cause air leakage around the tracheal and bronchial cuffs affects the lung isolation3,4, besides, undersize DLTs may increase the pressure of airway during mechanical ventilation5.
Traditionally method recommended to select the size of DLTs is based on the gender and height of patients, however this method is not always accurate, especially in the asian females and persons with smaller statures6,7,8, and this approach can generate airway complications postoperative and affect the rapid recovery of patients9,10,11. So, how to reduce the injury of airway caused by the intubation of DLTs and reduce the discomfort of patients after thoracic surgery are the focus of anesthesiologists12. Therefore, the objective of this study was to investigate the feasibility and accuracy of the method for selecting an optimal size of double-lumen tube in thoracic surgery.
Results
General information
Sixty adult patients were enrolled in this study and one patient in the CI group was excluded for the LDLT was too short to reach the optimal position, ultimately, fifty-nine patients were completed the study. There was no significant difference between two groups in terms of demographic characteristics and intraoperative variables (P > 0.05) (Table 1).
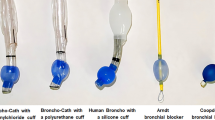
The outer diameter of the tracheal and the bronchial cuffs was measured when the cuffs were inflated or collapsed (Fig. 1) and their diameters were shown in Table 2. The size of the LDLT was chosen according to the inner diameter of the trachea and bronchus measured by chest CT scan.
Primary outcomes
The incidence of airway complications postoperative such as the hoarseness and sore throat scores after extubating in the postoperative anesthesia care unit (PACU) and the hoarseness scores twenty-four hours postoperatively in the CI group was significantly lower than the CC group (P < 0.05). There was no significant difference in sore throat scores 24 h after surgery (P > 0.05). (Table 3).
Secondary outcomes
The size choice of LDLT was significant difference between two groups (P < 0.05). The intubation time and alignment time in the CI group were significantly shorter than that in the CC group (P < 0.05). While the degree of lung collapse and the time of lung collapse was no significant difference between two groups (P > 0.05). In addition, there was no significant difference in the variable of pulmonary ventilation, the incidence of LDLT adjustment and displacement intraoperative between two groups(P > 0.05) (Table 4). There was no significant difference in the peak airway pressure, the plateau airway pressure and PetCO2 at TTLV, TOLV_immediately and TOLV_30mins (P > 0.05) (Table 5).
Discussion
DLTs are commonly used for OLV in most thoracic surgeries. Improperly sized of DLTs may lead to airway trauma and rupture. The results of this study showed that the size of LDLT was selected according to the method which matched the outer diameter of the tracheal and bronchial cuffs when they were inflated with the inner diameter of the trachea and bronchus measured on chest CT scan can reduce the incidence of airway complications such as hoarseness and sore throat, shorten the time of intubation. The main possible reasons may be as follows: (1) Smaller size of LDLT is softer than larger size of LDLT which may help to reduce the physical damage to the mucosa of trachea and bronchus caused by intubating or extubating; (2) The smaller size of LDLT is easier to pass through the narrow point such as glottis and annular cartilage to reduce the incidence of reintubation. (3) The smaller size of LDLT with thinner diameter had less frictional resistance when entering into the left main bronchus.
Slinger P et al. selected DLT for adults based on the patient’s height and sex: women < 1.6 m, 35 Fr, women > 1.6 m, 37 Fr, men < 1.7 m, 39 Fr, men > 1.7 m, 41 Fr13, recent, there is a tendency among anesthesiologists to use smaller size of DLTs, such as 35 Fr for females and 37 Fr for males to avoid airway trauma7. However, these choices were based on clinical experience alone and has no theoretical basis. In Shiqing L’s study the correct rate of selecting the size of DLT according to height and sex was 94.3% for male patients and only 51.1% for female patients14, even according to the diameter of cricoid ring and left main bronchus, the rate of agreement were 94.7% for male patients and 63.8% for female patients. In this study, the smaller size of LDLT was used in the CI group, therefore, the accuracy of size selection of LDLT was higher compared with other studies. Chengchao et al. measured the transverse diameter (TD-C) of the patient's annular cartilage by ultrasound and CT15 and conclusion that the accuracy of intubation was 90.2% in the ultrasound and 94.1% in the CT group, however, the size of DLT used in their study was range from 35 to 39, while in our study the size of LDLT was range from 28 to 35 in the CI group, so the incidence of airway complications such as hoarseness and sore throat was lower in our study.
Although the smaller size of LDLT was chosen in this study, there was no significant differences in the peak airway pressure, the plateau airway pressure and PetCO2 during TLV and OLV between the two groups; the degree of lung collapse and lung collapse time was also no statistical difference between the two groups, so it can be speculated that smaller size of LDLT had little effect on lung ventilation during TLV and OLV. In addition, there was no leakage of air around the tracheal and bronchial cuffs when the air pressure set at 20–25 cmH2O during the operation. So, we can select smaller size of LDLT according to this experimental method, which can reduce the intubation time, airway complications and had little impact on the lung ventilation intraoperative.
There were some limitations to this study. First, we measured the diameter of the tracheal and bronchial cuffs for this brand of DLT, so the data of cuffs’ diameter not be applicable with all brands of DLTs. Second, the overall sample size was small.
The method which matched the inner diameter of the trachea and bronchus measured on chest CT with the outer diameter of the tracheal and bronchial cuffs when they were inflated to select an appropriate size of LDLT can reduce the incidence of airway complications.
Methods
This study was approved by the medical ethics committee of the local Hospital (201805A160) and registered at the Clinical Trials.gov. (NCT05739318). This research was performed in accordance with relevant guidelines/regulations. Written informed consent was obtained from all subjects participating in the trial. Sixty adult patients, aged > 18 years and < 70 years, with American Society of Anesthesiologists (ASA) physical status I to II, requiring a left side double-lumen tube (LDLT) for elective thoracoscopic surgery were included in this study. The exclusion criteria as following: (1) have undergone lung operation or vocal cord surgery (2) hoarseness or sore throat was present previously, (3) The transverse and longitudinal diameters of the trachea or bronchus cannot be measured on chest CT images, (4) patients with visible anatomic abnormalities, (5) lung impairment, such as severe chronic obstructive pulmonary disease, (6) refusal to participate in the study.
An independent anesthesiologist trained by a senior radiologist screened all the patients the day before surgery and measured the inner diameter of the trachea and bronchus of the patients enrolled in this study on the chest CT slice where the trachea and bronchus were narrowest among all the tracheal and bronchus slice using the Picture Archiving and Communication System on computer (Fig. 2). All patients were randomly allocated to the Cuffs Collapsed group (CC group, n = 30) and Cuffs Inflated group (CI group, n = 30). In the Cuffs Collapsed group, selected the appropriate size of LDLT for patients by matching the outer diameter of LDLT (the outer diameter of the tracheal and bronchial cuffs when they were collapsed as the outer diameter of the LDLT) (Fig. 1, Table. 2) with the inner diameter of the trachea and bronchus measured by the anesthesiologist on the chest CT slice; In the Cuffs Inflated group, selected the appropriate size of LDLT for patients by matching the outer diameter of LDLT (the outer diameter of the tracheal and bronchial cuffs when they were inflated as the outer diameter of the LDLT) (Fig. 1, Table. 2) with the inner diameter of the trachea and bronchus measured by the anesthesiologist on the chest CT slice.
Randomization (1:1) was based on the code generated using SAS 9.2 software by a statistician who did not participate in this study. These codes were kept in sequentially numbered opaque envelopes and stored at the site of investigation until the end of the study.
All the patients were monitored with electrocardiography, noninvasive arterial blood pressure or invasive arterial blood pressure and oxygen saturation by pulse oximetry (SpO2) after entering into the operating room. General anesthesia was induced with intravenous 0.05 mg kg−1 Midazolam, 0.3 mg kg−1 Esketamine, 0.2 mg kg−1 Cis-atracurium and 0.3 µg kg−1 Sufentanil. All the patients were intubated with a LDLT (Tuoren Medical Technology Company, Xinxiang, China) by the same anesthesiologist via a video laryngoscope exactly 3 mins after receiving Cis-atracurium and confirmed the position of LDLT under direct vision of fiberoptic bronchoscope (FOB) (the bronchial cuff located below the carina without a hernia16). The trachea and bronchial cuffs were inflated with air and maintained the air pressure in the cuffs at 20–25 cmH2O by a barometer. The LDLT was fixed firmly at the patient’s mouth with cloth tape. After changing the patient position to the lateral decubitus position, the position of the LDLT was reassessed using FOB. Another independent anesthesiologist followed the patients postoperative and recorded the airway complications such as hoarseness, sore throat 30 mins after extubating and 24 h postoperatively.
Observed indicators
Primary outcomes were the incidences of the airway complications such as hoarseness, sore throat 30 mins after extubating and 24 h postoperatively. Secondary outcomes included the time of intubation, the time of adjusting the LDLT to the optimal position, the incidence of air leakage around the cuffs during surgery, the incidence of LDLT displaced, the peak airway pressure (Peak), the plateau airway pressure (Plateau) and end-tidal carbon dioxide (PetCO2) were recorded at two lungs ventilation (TTLV), immediately after OLV (TOLV_immediately) and 30 mins after OLV (TOLV_30mins). The tidal volume was calculated at 8 ml kg−1 of ideal body weight during TLV and 6 ml kg−1 of ideal body weight during OLV. The time of lung collapse on operated side (the time from the incision of pleura to the collapse of lung) and the degree of lung collapse were also recorded. The degree of lung collapse was scored as follows: The lung collapsed spontaneously was score 1; The lung collapsed after the suction was score 2; The lung collapsed after the squeezed by surgeon was score 3. Postoperative hoarseness scores were scored as follows: no hoarseness was scored 0; the patient's self-detection of hoarseness was scored 1; the observer clearly found that the patient had a hoarseness score of 2; patient unable to speak for hoarseness was scored 3. Postoperative sore throat was scored as follows: no sore throat was scored 0; the patient had a pain when swallowing was scored 1; the patient had persistent sore throat and worsens on swallowing was scored 2; the patient with sore throat required analgesic treatment was scored 317,18.
Statistical analysis
In this study, according to a pilot study and previous study, with the significance set at 0.05 and power set at 80%, the sample size required to detect the differences of the incidence of the airway complications such as hoarseness, sore throat was 48 patients. Taking into account the potential risk of failure to intubate, we planned to enroll 60 patients (30 per group) into the trial.
SPSS Statistics 25 was used for statistical analysis. Continuous variables were expressed as means and standard deviations. Categorical variables are expressed as the corresponding sample size or percentage. Continuous variables were analyzed using the Man-Whitney U test. Unordered categorical variables were analyzed using the Pearson's Chi-square test. Ordinal categorical variables were analyzed using the Pearson's Chi-square test, the Fisher’s Exact test or the weighted Man-Whitney U test. P < 0.05 was statistical difference.
Ethics approval and consent to participate
The Ethical Review Committee of the First Hospital of Qinhuangdao approved the present study (approval no. 201805A160). This research was performed in accordance with relevant guidelines/regulations. All the patients provided written informed consent.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Tikka, T. & Hilmi, O. J. Upper airway tract complications of endotracheal intubation. Br. J. Hosp. Med. 80, 441–447. https://doi.org/10.12968/hmed.2019.80.8.441 (2019).
Adolphs, N. et al. Dentoalveolar injury related to general anaesthesia: A 14 years review and a statement from the surgical point of view based on a retrospective analysis of the documentation of a university hospital. Dent. Traumatol. 27, 10–14. https://doi.org/10.1111/j.1600-9657.2010.00955.x (2011).
Roscoe, A., Kanellakos, G. W., McRae, K. & Slinger, P. Pressures exerted by endobronchial devices. Anesth. Analg. 104, 655–658. https://doi.org/10.1213/01.ane.0000255171.94527.c7 (2007).
Kim, E., Kim, I.-Y. & Byun, S.-H. Effect of lateral positioning on the bronchial cuff pressure of a left-sided double-lumen endotracheal tube during thoracic surgery: Study protocol for a prospective observational study. BMJ Open https://doi.org/10.1136/bmjopen-2018-026606 (2019).
Spaeth, J. et al. Characteristics of double-lumen tubes determine bronchial airway pressure. J. Cardiothorac. Vasc. Anesth. 30, 954–960. https://doi.org/10.1053/j.jvca.2016.03.126 (2016).
Chang, T.-R., Yuan, M.-K., Pan, S.-F., Chuang, C.-C. & So, E. C. Double-lumen endotracheal tube—predicting insertion depth and tube size based on patient’s chest X-ray Image data and 4 other body parameters. Diagnostics https://doi.org/10.3390/diagnostics12123162 (2022).
Eldawlatly, A. Double lumen tube: Size and insertion depth. Saudi J. Anaesth. https://doi.org/10.4103/sja.sja_192_21 (2021).
Kim, D., Son, J.-S., Ko, S., Jeong, W. & Lim, H. Measurements of the length and diameter of main bronchi on three-dimensional images in Asian adult patients in comparison with the height of patients. J. Cardiothorac. Vasc. Anesth. 28, 890–895. https://doi.org/10.1053/j.jvca.2013.05.029 (2014).
Hierlmeier, B., Nguyen, R., Kurnutala, L. & Tucci, M. Comparison of different size left-sided double-lumen tubes for thoracic surgery. Ann. Cardiac Anaesth. https://doi.org/10.4103/aca.ACA_93_19 (2021).
Gupta, E. et al. Comparison of lung ultrasound technique <em>versus</em> clinical method to evaluate the accuracy of size and placement of left endobronchial double lumen tube in patients undergoing elective thoracic surgery: A prospective observational study. Monaldi Arch. Chest Dis. https://doi.org/10.4081/monaldi.2023.2700 (2023).
Nakanishi, T. et al. Combined use of the ProSeal laryngeal mask airway and a bronchial blocker vs. a double-lumen endobronchial tube in thoracoscopic surgery: A randomized controlled trial. J. Clin. Anesth. 88, 111136. https://doi.org/10.1016/j.jclinane.2023.111136 (2023).
Szegedi, L., Huybrechts, I. & Tuna, T. Lung separation in adult thoracic anesthesia. Saudi J. Anaesth. 15, 272. https://doi.org/10.4103/sja.sja_78_21 (2021).
Slinger, P. A view of and through double-lumen tubes. J. Cardiothorac. Vasc. Anesth. 17, 287–288. https://doi.org/10.1016/s1053-0770(03)00058-2 (2003).
Shiqing, L., Wenxu, Q., Jin, Z. & Youjing, D. The combination of diameters of cricoid ring and left main bronchus for selecting the “best fit” double-lumen tube. J. Cardiothorac. Vasc. Anesth. 32, 869–876. https://doi.org/10.1053/j.jvca.2017.11.029 (2018).
Zhang, C. et al. Prediction of left double-lumen tube size by measurement of cricoid cartilage transverse diameter by ultrasound and CT multi-planar reconstruction. Front. Med. 8, 612. https://doi.org/10.3389/fmed.2021.657612 (2021).
Palaczynski, P. et al. A randomized comparison between the VivaSight double-lumen tube and standard double-lumen tube intubation in thoracic surgery patients. J. Thorac. Dis. 14, 3903–3914. https://doi.org/10.21037/jtd-22-451 (2022).
Seo, J. H., Cho, C. W., Hong, D. M., Jeon, Y. & Bahk, J. H. The effects of thermal softening of double-lumen endobronchial tubes on postoperative sore throat, hoarseness and vocal cord injuries: A prospective double-blind randomized trial. Br. J. Anaesth. 116, 282–288. https://doi.org/10.1093/bja/aev414 (2016).
Seo, J. H. et al. Comparison of techniques for double-lumen endobronchial intubation: 90° or 180° rotation during advancement through the glottis. Br. J. Anaesth. 111, 812–817. https://doi.org/10.1093/bja/aet203 (2013).
Author information
Authors and Affiliations
Contributions
Z.L. and G.C.: Investigation, Formal analysis, Writing-original draft; L.Z.: Investigation, Writing-original draft; C.C. Collected all the patient initial data, writing-original draft; S.L.: Collected all the patient initial data and drafted the manuscript; Z.L.: Manuscript editing, Modifying figures and tables.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cui, G., Zhao, L., Chi, C. et al. The feasibility and accuracy of the method for selecting the optimal size of double-lumen tube in thoracic surgery: a prospective, randomized controlled trial. Sci Rep 14, 17539 (2024). https://doi.org/10.1038/s41598-024-68349-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-68349-z
Keywords
This article is cited by
-
Quantitative CT measurements of segmental bronchial changes during inspiratory and expiratory phases in healthy subjects
BMC Pulmonary Medicine (2025)
-
Impact of cardiac factors on central airway anatomical parameters in patients undergoing lung mass surgery
Journal of Cardiothoracic Surgery (2025)