Abstract
There is insufficient research on bioaerosols in hospital waste decontamination stations. This study aimed to investigate the effect of three-layer and N95 masks in reducing the inhalation risk of bacterial bioaerosols in a waste decontamination station at a teaching hospital. Active sampling was conducted on five different days at three locations: the yard, resting room, and autoclave room in three different modes: without a mask, with a three-layer mask, and with an N95 mask. Bacterial bioaerosols passing through the masks were identified using biochemical tests and polymerase chain reaction (PCR). The median concentration and interquartile range (IQR) of bacterial bioaerosols was 217.093 (230.174) colony-forming units per cubic meter (CFU/m3), which is higher than the recommended amount by Pan American Health Organization (PAHO). The resting room had high contamination levels, with a median (IQR) of 321.9 (793.529) CFU/m3 of bacterial bioaerosols. The maximum concentration of bioaerosols was also recorded in the same room (2443.282 CFU/m3). The concentration of bacterial bioaerosols differed significantly between using a three-layer or N95 mask and not using a mask (p-value < 0.001). The non-carcinogenic risk level was acceptable in all cases, except in the resting room without a mask (Hazard Quotient (HQ) = 2.07). The predominant bacteria were Gram-positive cocci (33.98%). Micrococci (three-layer mask = 51.28%, N95 mask = 50%) and Coagulase-negative Staphylococci (three-layer mask = 30.77%, N95 mask = 31.82%) were the most abundant bioaerosols passing through the masks. The results obtained are useful for managerial decisions in hospital waste decontamination stations to reduce exposure to bioaerosols and develop useful guidelines.
Similar content being viewed by others
Introduction
Bioaerosols refer to biological air pollutants, including both living and non-living particles that have an aerodynamic diameter of less than 100 µm. Due to their small size, they can enter the respiratory system1,2,3. Exposure to bioaerosols is associated with various health effects, including skin and eye irritation, sick-building syndrome, hospital-acquired infections, asthma, lung infections, allergic reactions, and cancer4,5. Activities related to waste management, such as collection, storage, transportation, disposal, and treatment, contribute to the generation of bioaerosols6,7. Consequently, employees in waste management industries are exposed to high levels of bioaerosols8,9,10. Furthermore, hospitals are recognized as one of the settings where bioaerosols are prevalent. Moreover, they generate large amounts of medical waste, which contains substantial loads of bacteria and viruses11,12. Although approximately 85% of medical waste is non-hazardous, the remaining 15% is infectious and requires special management11,13,14. Proper disinfection and disposal of hospital waste are necessary to prevent the risk of environmental pollution and infectious diseases12,14,15. Therefore, each hospital has a waste decontamination station for the treatment of infectious waste and as a temporary storage facility for non-hazardous waste.
Previous studies have investigated bioaerosols in various locations. In composting facilities, there have been reports of occupational exposure to high concentrations of endotoxin, A. fumigatus, and actinobacteria/Streptomyces spp.16. High concentrations of airborne bacteria have been found at a sanitary landfill site, ranging from 3179 to 10,883 colony-forming units per cubic meter (CFU/m3) 1. Numerous studies have also investigated the concentration and types of bioaerosols in different hospital wards17. For instance, in a hospital, the highest and lowest concentrations of bioaerosols were obtained in the lung ward (336.67 CFU/m3) and operating room (15.25 CFU/m3)18. Studies have also been conducted to investigate the non-carcinogenic risks associated with exposure to bioaerosols. In a waste transfer station, 53 species of bacterial pathogens were identified, 39 of which were pathogenic to humans. The health risk assessment revealed that workers faced unacceptable levels of non-carcinogenic risk19. Inhalation of bioaerosols is a more significant route of exposure compared to dermal absorption20,21. The results of a study conducted in a wastewater treatment plant revealed that the non-carcinogenic risk associated with inhalation is 105 times higher than that of skin absorption21. In a sanitary landfill, the non-carcinogenic risk from exposure to bacterial bioaerosols was estimated to be less than one at all sampling locations, with a maximum rate of 0.16 recorded during the summer season10. In addition, to reduce exposure to bioaerosols, recommendations such as implementing disinfection methods, improving air ventilation systems, and utilizing personal protective equipment (PPE) have been provided5,9,22. One type of PPE that can effectively reduce exposure to bioaerosols is masks23,24. Three-layer masks and N95 masks are two common types of face masks used to minimize the inhalation of bioaerosols in healthcare and community settings. Three-layer masks provide a barrier against larger respiratory droplets; however, their filtration efficiency is 0.04 to 1.3 times lower compared to N95 masks25,26. N95 masks, on the other hand, are designed to achieve a close facial fit and, when subjected to careful testing, efficiently filter at least 95% of very small airborne particles (0.3 μm), including bioaerosols25. Understanding the performance and proper usage of these masks can help reduce the risks of inhaling bioaerosols and provide guidance to healthcare professionals, policymakers, and the general public to make informed decisions. A study found that the filtration efficiency of each mask varied from 82 to 99%, depending on the level of filtration27. In addition, various modifications have been shown to improve the filtration efficiency of commercially available medical procedure masks by 60.3 to 80.2 percent28.
Patients and hospital personnel are exposed to high concentrations of bioaerosols, which can cause respiratory diseases and harm the health of employees in occupational settings. The waste decontamination station in hospitals is a location with a high concentration of bioaerosols. However, there is a lack of research on bioaerosols in this location, and no standard has been proposed for occupational exposure to these biological pollutants in this particular setting. Therefore, the present study aimed to determine the effect of medical masks on the risk of inhaling bacterial bioaerosols at the waste decontamination station of a hospital. Since such a study has not yet been conducted, the data obtained can be valuable for making management decisions, implementing control measures to minimize workers' exposure to airborne bacteria, and serving as a basis for future research to establish specific standards for bioaerosol exposure in hospital waste decontamination stations.
Materials and methods
Study design
The study site was the waste decontamination station of one of the teaching hospitals in Mashhad, Iran, with 824 active beds. The hospital's daily waste production rate ranged from 1000 to 1200 kg. The waste was collected by a group of workers from various wards of the hospital and transported to the waste decontamination station. Three workers were engaged in waste management at this facility, working in 24-h shifts every other day with no days off. Three locations within the hospital waste decontamination station were selected for sampling: the yard where non-hazardous and decontaminated waste was stored; the autoclave room where infectious, sharp, chemical, and pharmaceutical wastes were managed, and the workers' resting room, which was equipped with a bathroom, toilet, and kitchen (Fig. 1).
Bioaerosols sampling
Sampling was conducted over five days, following the United States Environmental Protection Agency (US EPA) sampling schedule calendar, with a six-day interval between December 2022 and January 2023. Two replicated samples5,10 were collected under three different mask conditions: without a mask, with a three-layer mask, and with an N95 mask. These samples were collected at each of the three previously mentioned locations, resulting in a total of 90 collected samples. Bioaerosols were sampled using a QuickTake 30 Sample Pump at a flow rate of 14.15 L/min, equipped with a Biostage sampler (BioStage 200 single-stage viable cascade impactor) containing plates with a blood agar culture medium supplemented with Cyclohexamide antifungal. The sampling duration was 10 min to ensure that the microbial load on plates did not exceed 300 colonies17,32,33,34. For sampling, the biostage was positioned at a height of 150 cm above the ground, which is the average height at which humans breathe10,17,32. It was also placed one meter away from walls and obstacles18. For all tests, a single type of best-selling, publicly available three-layer and N95 mask was used. The three-layer mask consisted of a middle layer of melt-blown and two outer layers of spun-bond, while the N95 mask was composed of 5 layers, from the outside to the inside: spun-bond, melt-blown, spun-bond (ssmms), melt-blown, and spun-bond. The spun-bond and melt-blown are made of polypropylene. The melt-blown fabric plays a crucial role in filtering bacteria, particles, and droplets35. During sampling with masks, they were securely attached to the biostage using a metal ring to ensure no air could enter through any gaps. In each stage prior to sampling, the equipment was sterilized with 70% ethanol. The pump flow rate was calibrated using a rotameter. Moreover, meteorological parameters including air temperature (temp), relative humidity (RH), and wind velocity (W-velocity) were also recorded using humidity and temperature meter (Benetech, GM1362) and digital anemometer (Wintact WT87A) respectively36. Collected samples were immediately sealed and transported to the laboratory in a cooled box. Subsequently, they were incubated at 37 °C for 24–48 h17.
Bioaerosols quantification and identification
After incubation, colonies were counted, and the bioaerosol concentrations were quantified in terms of CFU/m3 3,4. Bacterial purification was performed based on the visual characteristics of the colonies5. Subsequently, Gram staining was conducted.
The bacterial bioaerosols that passed through the three-layer and N95 masks were isolated and mainly identified using biochemical tests, such as cultivation in TSI and SIM culture medium, mannitol, DNase, catalase, oxidase, coagulase, bile esculin, urease, citrate, and resistance to bacitracin and optochin10,33. If identification at the species level was not possible, the polymerase chain reaction (PCR) technique was employed. Deoxyribonucleic acid (DNA) extraction was performed using the boiling method. The concentration of the extracted DNA was determined by measuring the optical density (OD) using a spectrophotometric method with ultraviolet (UV) light37. For the PCR technique and amplification of 16S rDNA, the primers 27.F (27.F 5`AGAGTTTGATCCTGGCTCAG-3`) and 1492.R (1492.R 5`-TACGGYTACCTTGTTACGAACTT-3`) were used37,38. A mixture of 1 µl of each diluted forward and reverse primer, 2 µl of template DNA, 10 µl of master mix, and 11 µl of injected distilled water was prepared inside a microtube. Then, the microtube was placed in a Mastercycler gradient Eppendorf device.
The amplification program was set as follows: 1 cycle of initial denaturation at 95 °C for 5 min, followed by 30 cycles consisting of a secondary denaturation step at 94 °C for 45 s, an annealing step at 55 °C for 1 min, an extension step at 72 °C for 1.5 min, and one final extension at 72 °C for 5 min38. Then, the amplification product, along with the 100 bp ladder, was loaded onto a 1.5% agarose gel, and electrophoresis was performed. Then, the bands were observed using a UV transilluminator. If they appeared clear, the amplified DNA was sequenced, and the resulting sequence was searched in the National Center for Biotechnology Information (NCBI) database to determine the type of bacteria3,38.
Health risk assessment
People can be exposed to bioaerosols through skin absorption, inhalation, and ingestion routes33. Since the risk of the ingestion route is rare, previous research has predominantly focused on the risks associated with inhalation and skin contact21. In this study, the aim was to investigate the effect of masks on the inhalation risk of bioaerosols; therefore, only the inhalation route was considered. The non-carcinogenic risk associated with bacterial bioaerosol was evaluated based on previous studies. The concentration of bioaerosols allows for the calculation of the Average Daily Dose (ADD) using Eq. 1.
In this formula, ADDinh represents the average daily dose from the inhalation route (CFU/(kg.day)), C denotes the concentration of the pollutant (CFU/m3 for bioaerosols), IR stands for inhalation rate (m3/day), EF is the exposure frequency (days/year), ED indicates exposure duration (years), BW represents body weight (Kg) and AT is is the averaging time (days)3,10,20,21,33,39,40.
To assess the non-carcinogenic risk of bioaerosols, the Hazard Quotient (HQ) was calculated using Crystal Ball software. HQ is defined as the ratio of the ADD to the Reference Dose (RfD) for chronic exposure (Eqs. 2 and 3)1,20,33,40:
RfC (CFU/m3) represents the reference concentration for bioaerosols. The RfC upper limit values are not available for bioaerosols41,42. In such cases, a reference value of 500 CFU/m3 was considered based on previous studies1,3,10,39,40,43. HQ > 1 indicates a significant and concerning potential risk of non-carcinogenic effects that should not be ignored. However, HQ ≤ 1 suggests that the risk is at an acceptable level, meaning that non-carcinogenic hazards are unlikely to be a concern3,33,39,40. The values used to assess the inhalation risk of bioaerosols for adults in this study are presented in Table 1:
Statistical analysis
The concentration of bioaerosols, temprature, RH, and W-velocity were described using the mean (stanard deviation (SD)) and median (interquartile range (IQR)) for the levels of face masks. Quantitative variables were analyzed using relative frequency and represented as column charts. The consistency of distribution of quantitative variables with a normal distribution was explored using the Shapiro–Wilk test. The association of bacterial bioaerosols with temprature, RH, and W-velocity was assessed using Spearman's rank correlation coefficient and ilusterated in a heatplot. The association of bacterial bioaerosols with location was examined using Kruskal–Wallis test. The effect of medical face masks on bacterial bioaerosols was examined using quantile regression as an alternative to traditional linear regression, aiming to have regression coefficients as an effect measure and mitigate assumptions associated with linear regression models. P-value less than 0.05 was considered as statistically significant. Statistical analyses were performed using Stata SE version 18.
Declaration of Generative AI and AI-assisted technologies in the writing process
During the preparation of this work the authors used wordvice.ai in order to improve readability and language. After using this tool, the authors reviewed and edited the content as needed and takes full responsibility for the content of the publication.
Results and discussion
Bioaerosol concentrations
According to the Shapiro–Wilk test, the concentration of bioaerosols, temperature, RH, and W-velocity were found not to follow a normal distribution (Table 2). The median (IQR) of bacterial bioaerosols concentrations for different locations were as follows:193.388 (126.323) CFU/m3 for the yard, 321.9 (793.529) CFU/m3 for the resting room, and 230.269 (160.773) CFU/m3 for the autoclave room (Table 3). However, the Kruskal–Wallis test revealed that these differences were not statistically significant (p-value = 0.412). It was expected that the workers' resting room would have lower contamination levels. However, it was found that the resting room had high contamination levels, with a median (IQR) of 321.9 (793.529) CFU/m3 of bacterial bioaerosols. The maximum concentration of bacterial bioaerosols was also recorded in the same room (2443.282 CFU/m3). The contamination in the resting room can be attributed to various factors, including its small size, the presence of workers in contaminated clothing, unsanitary conditions, lack of periodic disinfection, absence of a proper ventilation system, and the building's old age5,17,47,48,49. The decreased number of bacterial bioaerosols in the autoclave room, compared to the resting room, can be attributed to factors such as the high temperature and pressure around the autoclaves, the use of six 1400 rpm fans for air ventilation, and the open doors that facilitate natural ventilation. In comparing the autoclave room and the yard, it can be observed that the presence of more infectious waste and its greater displacement in the autoclave room led to a higher concentration of bioaerosols6. On the other hand, the yard was an open space with a lower temperature, and there was less displacement of hospital waste in this area. As a result, this location registered the lower level of bacterial concentration. The findings of other studies also demonstrate that the concentration of bacterial bioaerosols in indoor air is higher than in outdoor air, which confirms the results of the present study5,33,50,51.
Currently, there is no established international standard for bioaerosols. However, the Pan American Health Organization (PAHO) recommends limits for bacterial bioaerosols in healthcare facilities. The recommended limits are less than 10 CFU/m3 for very clean areas, between 10 and 100 CFU/m3 for relatively clean areas, and between 100 and 200 CFU/m3 for other areas52. The concentration of bacterial bioaerosols in the studied hospital waste decontamination station, with a median and IQR of 217.093 (230.174), exceeded the recommended levels set by PAHO (100 to 200 CFU/m3).
During the sampling period, the temperature, RH, and W-velocity were in the ranges of 3.4 to 27.4 °C, 32.2 to 55%, and 0 to 0.45 m/s, respectively (Table 2). The highest temperature was recorded in the resting room, while the lowest temperature was obtained in the yard. Moreover, the highest levels of humidity and W-velocity were also recorded in the yard. The correlation between the concentration of bacterial bioaerosols and meteorological parameters was assessed using Spearman's rank correlation coefficient. The p-values for temperature, RH, and W-velocity were found to be 0.056, 0.316, and 0.429, respectively. Consequently, no statistically significant association was observed between the bacterial bioaerosol concentrations and meteorological variables. The related heatplot can be seen in Fig. 2. In Ghanbarian's study, a statistically significant difference was found between bioaerosol concentrations in cold and hot seasons32. Conversely, Valedeyni Asl's study showed no substantial correlation between bacterial concentration and environmental temperature and humidity53. Mehrasabi's research revealed a statistically significant relationship between bacterial bioaerosol concentration and air temperature but found no significant relationship with air pressure and humidity54. Fang's study confirmed a notable correlation among bacterial bioaerosols and temperature, pressure, and ozone levels7. Yousefzadeh's study recorded no correlation between relative humidity, temperature, and bacterial concentration and suggested that this might be due to the limited range of changes in the sampling interval18. Hosseini's study demonstrated that there was no substantial statistical correlation between bacterial bioaerosol concentration and both humidity and temperature55. The absence of a statistically significant relationship between bacterial bioaerosol concentrations and meteorological variables might be attributed to the limited sampling time and the restricted range of changes in these variables in the current study. However, considering the varying findings regarding the influence of temperature and humidity on bioaerosol concentrations, it is essential to conduct further research on this topic18. Sampling was conducted during the cold season. The use of heating equipment in the resting room resulted in higher temperatures compared to other sampling points. According to the findings of Bragoszewska's study, the increased air circulation and resuspension caused by the heating equipment led to the highest concentration of bacterial bioaerosols in this location51.
Mask Effects on bioaerosols
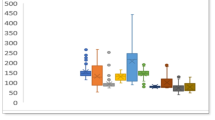
The concentration of bacterial bioaerosols under different sampling conditions with respect to mask usage is presented in Table 3. The concentration of bacteria in the sampling condition without a mask was noticeably higher than in the conditions where a three-layer mask or N95 mask was used23. As shown in Table 4, the quantitative regression coefficients for the three-layer mask and N95 mask were -210.257 (p-value < 0.001) and -210.604 (p-value < 0.001), respectively, indicating that the use of these masks effectively reduced the concentration of bioaerosols. However, due to the overlap of confidence intervals in quantile regression, no statistically significant difference was observed between the two types of masks.
A study has shown that N95 masks are more effective than three-layer masks in preventing the penetration of NaCl aerosols. Furthermore, within the various groups of N95 and three-layer masks, types with higher filtration capacity and better fitting characteristics also provide greater protection against biological aerosols56. The influenza virus had passed through eight types of surgical masks studied by Booth. However, all masks were found to be effective in reducing exposure to the influenza virus. The amount of reduction varied depending on the design of the mask, ranging from 1.1 to 55 times57. The filtration efficiency of commercially available medical procedure masks can be improved by 60.3 to 80.2 percent through various modifications. These include tightening the ear loops, using rubber bands to reduce gaps at the top and bottom of the mask, and placing a cut-out piece of nylon stocking over the mask to seal any remaining gaps28.
In this study, we employed a comparable approach to evaluate the effectiveness of a three-layer mask and an N95 mask when used with the Biostage sampler during sampling. We securely attached the masks to the biostage using a metal ring, ensuring that air only passed through the mask layers without any gaps. This setup allowed us to assess the impact of the masks. The absence of a statistically significant difference between these two mask types suggests that both a high-quality three-layer mask and an N95 mask are equally effective in reducing bacterial bioaerosol penetration into the respiratory system. This means that when it comes to preventing bacterial entry, focusing on proper mask fit and sealing to prevent air leakage is more effective than simply increasing the number of mask layers. It is important to note that factors such as mask design and proper placement on the face may influence the effectiveness of different types of masks.
In the future, it is recommended that studies be conducted on the design of masks, including investigating the impact of the number of layers and proper positioning on the face to prevent air leakage around the mask, in order to further assess the reduction of bacterial bioaerosol transmission.
Bioaerosols composition
The predominant bioaerosols in our study were Gram-positive cocci (33.98%), followed by Gram-positive bacilli (30.29%), Gram-negative bacilli (24.27%), and Gram-negative cocci (8.54%) (Fig. 3a). Previous studies have also reported a high frequency of Gram-positive cocci5,54,58,59, which are commonly found in the environment and are a prevalent part of the flora on human skin, hair, and mucous membranes51,55. Moreover, their high resistance to environmental stress contributes to their abundance in indoor environments, particularly hospitals5,27,33. In contrast, gram-negative bacteria show less resistance to environmental conditions due to their fragile cell wall and may break during sampling60. Therefore, a microorganism's ability to persist as a bioaerosol is linked to its surface biochemistry61. Among the passing bacteria from masks, 8 different types of bacteria were identified. In both types of masks, Micrococci and Coagulase-negative Staphylococci (SCN) had the highest frequency (Fig. 3b).
These findings are consistent with previous research that has also reported a significant prevalence of Coagulase-negative Staphylococci and Micrococci59. Staphylococci and Micrococci are part of the normal human flora, derived from the skin, hair, and clothing of individuals. As a result, the majority of airborne bacteria present in the hospital environments belong to these types5,55,58,62. According to Gizaw's study, the presence of Staphylococcus aureus and Streptococcus pyogenes, two highly pathogenic bacterial species, is prevalent across various departments within hospitals63. Staphylococci show good resistance to antibiotics. Moreover, they are found in abundance on human skin, making them easily spread in hospitals. They are also a significant cause of skin, blood, urinary, and respiratory infections5,18,54. Infections attributed to Staphylococci can be transmitted through contact with an infected person or the patient's belongings, such as clothes, towels, sheets, etc. Additionally, hospital personnel can also act as carriers of these bacteria18,55. Although Coagulase-negative Staphylococci possess low toxicity, they are one of the most important causes of infection in high-risk groups33.
Non-carcinogenic risk assessment
As the primary goal of this study was to examine the impact of masks on the potential risk of inhaling bacterial bioaerosols, the risk assessment focused solely on the inhalation exposure route. Generally, the amount of HQ resulting from the inhalation route is much higher than that from the skin absorption route20,21. In all sampling locations and different mask usage modes, except for the resting room, where sampling was done without a mask, the HQ derived from inhalation was below one. This indicates that the potential non-carcinogenic effects are unlikely to pose an important concern. According to Fig. 4, the use of three-layer or N95 masks reduced the HQ level by 3.14 to 69 times. The findings of Yan's study, conducted at a wastewater treatment plant, revealed that the use of PPE by workers and residents could minimize health risks by at least one order of magnitude, while utilizing higher-grade PPE could further enhance risk reduction23.
In contrast, the HQ value was recorded as 2.07 in the resting room during sampling without a mask, indicating a concerning level of potential risk and non-carcinogenic effects. Under these conditions, appropriate control measures should be taken to mitigate the risk. Although the use of three-layer masks and N95 masks reduced the HQ value to 0.05 and 0.04, respectively, in the resting room, certainly, masks are not being used in this area. Consequently, implementing control measures will be of greater importance in the resting room. For example, it is possible to improve conditions by establishing an efficient ventilation system, removing excess items from the resting room, separating the area for workers to change clothes from the resting room, carrying out regular disinfections, and prohibiting the entry of contaminated items into this space. The amount of HQ from the inhalation route in a municipal waste sanitary landfill was estimated to be less than one at all sampling locations, with a maximum recorded value of 0.16 during the summer season10. Two other studies also found that the HQ from the inhalation route was higher during summer than in winter7,39. The evaluation of non-carcinogenic risks associated with bioaerosols in the biochemical tank of an urban wastewater treatment plant and a hospital wastewater treatment station showed that the HQ was below one at all sampling locations. Nevertheless, the non-carcinogenic risk posed by the hospital wastewater treatment station was greater than that of the urban wastewater treatment plant due to the higher bacterial concentration3.
Our study demonstrated that both three-layer masks and N95 masks effectively reduce inhalation risk of bacterial bioaerosols in hospital waste decontamination stations. This finding holds important implications for healthcare workers who are daily exposed to potentially infectious bioaerosols. The use of masks as effective PPE by healthcare workers considerably reduces their risk of inhaling bioaerosols and potential infection from harmful bacteria, improving overall safety and health, and reducing infection spread within healthcare settings. It is worth noting that this study only evaluated two types of masks (three-layer and N95), so the findings may not apply to other types of masks or respiratory protective equipment. Further research in this area could be beneficial.
The findings of this study can be used as a valuable resource for educational purposes and provide a foundation for establishing and executing efficient preventive strategies to mitigate bioaerosol-related health hazards threats in hospitals’ waste decontamination stations ultimately promoting public health protection.
Conclusion
The concentration of bacterial bioaerosols in the hospital waste decontamination station exceeded the limit set by the PAHO guidelines. Gram-positive cocci were the most abundant phenotype and Micrococci and Coagulase-negative Staphylococci were the most prevalent species passing through the masks studied. The results showed that three-layer masks or N95 masks can significantly reduce the number of airborne bacteria and the risk of inhalation exposure. According to the findings, a three-layer mask can be as effective as an N95 mask in preventing the entry of bacterial bioaerosols if air entry is prevented from around the mask. Furthermore, it was discovered that the non-carcinogenic risk associated with inhaling bacterial bioaerosols in the resting room is at a concerning level and requires corrective action.
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
References
Li, L. et al. Microbial aerosol particles in four seasons of sanitary landfill site: Molecular approaches, traceability and risk assessment. J. Environ. Sci. 108, 120–133. https://doi.org/10.1016/j.jes.2021.01.013 (2021).
Morgado-Gamero, W. B., Parody, A., Medina, J., Rodriguez-Villamizar, L. A. & Agudelo-Castañeda, D. Multi-antibiotic resistant bacteria in landfill bioaerosols: Environmental conditions and biological risk assessment. Environ. Pollut. 290, 118037. https://doi.org/10.1016/j.envpol.2021.118037 (2021).
Wang, Y. et al. Characteristics, non-carcinogenic risk assessment and prediction by HYSPLIT of bioaerosol released from Hospital and Municipal Sewage, China. Ecotoxicol. Environ. Saf. 246, 114131. https://doi.org/10.1016/j.ecoenv.2022.114131 (2022).
Sajjad, B. et al. Size-resolved ambient bioaerosols concentration, antibiotic resistance, and community composition during autumn and winter seasons in Qatar. Environ. Pollut. 336, 122401. https://doi.org/10.1016/j.envpol.2023.122401 (2023).
Hassan, A. & Zeeshan, M. Microbiological indoor air quality of hospital buildings with different ventilation systems, cleaning frequencies and occupancy levels. Atmos. Pollut. Res. 13, 101382. https://doi.org/10.1016/j.apr.2022.101382 (2022).
Vilavert, L., Nadal, M., Figueras, M. J., Kumar, V. & Domingo, J. L. Levels of chemical and microbiological pollutants in the vicinity of a waste incineration plant and human health risks: Temporal trends. Chemosphere 84, 1476–1483. https://doi.org/10.1016/j.chemosphere.2011.04.041 (2011).
Fang, R. et al. From air to airway: Dynamics and risk of inhalable bacteria in municipal solid waste treatment systems. J. Hazard. Mater. 460, 132407. https://doi.org/10.1016/j.jhazmat.2023.132407 (2023).
Wikuats, C. F. H. et al. Health symptoms and inflammatory blood biomarkers from exposure of recyclable waste workers to particulate matter and bioaerosols. Atmos. Pollut. Res. 13, 101323. https://doi.org/10.1016/j.apr.2022.101323 (2022).
Nair, A. T. Bioaerosols in the landfill environment: An overview of microbial diversity and potential health hazards. Aerobiologia 37, 185–203. https://doi.org/10.1007/s10453-021-09693-9 (2021).
Samadi, M. T. et al. Characteristics and health effects of potentially pathogenic bacterial aerosols from a municipal solid waste landfill site in Hamadan, Iran. J. Environ. Health Sci. Eng. 19, 1057–1067. https://doi.org/10.1007/s40201-021-00672-3 (2021).
WHO.
Zhou, H. et al. A deep learning approach for medical waste classification. Sci. Rep. 12, 2159. https://doi.org/10.1038/s41598-022-06146-2 (2022).
Kwikiriza, S., Stewart, A. G., Mutahunga, B., Dobson, A. E. & Wilkinson, E. A whole systems approach to hospital waste management in rural Uganda. Front. Public Health 7, 136. https://doi.org/10.3389/fpubh.2019.00136 (2019).
Khalid, S. et al. Current practices of waste management in teaching hospitals and presence of incinerators in densely populated areas. BMC Public Health 21, 1340. https://doi.org/10.1186/s12889-021-11389-1 (2021).
Wang, J. et al. Disinfection technology of hospital wastes and wastewater: Suggestions for disinfection strategy during coronavirus Disease 2019 (COVID-19) pandemic in China. Environ. Pollut. 262, 114665. https://doi.org/10.1016/j.envpol.2020.114665 (2020).
Kontro, M. H., Kirsi, M. & Laitinen, S. K. Exposure to bacterial and fungal bioaerosols in facilities processing biodegradable waste. Front. Public Health 10, 789861. https://doi.org/10.3389/fpubh.2022.789861 (2022).
Dehghani, M., Sorooshian, A., Nazmara, S., Baghani, A. N. & Delikhoon, M. Concentration and type of bioaerosols before and after conventional disinfection and sterilization procedures inside hospital operating rooms. Ecotoxicol. Environ. Saf. 164, 277–282. https://doi.org/10.1016/j.ecoenv.2018.08.034 (2018).
Yousefzadeh, A. et al. Evaluation of bio-aerosols type, density, and modeling of dispersion in inside and outside of different wards of educational hospital. Environ. Sci. Pollut. Res. Int. 29, 14143–14157. https://doi.org/10.1007/s11356-021-16733-x (2022).
Jiawei, M., Han, Y., Li, L. & Liu, J. Distribution characteristics and potential risks of bacterial aerosol in waste transfer station. J. Environ. Manag. 326, 116599. https://doi.org/10.1016/j.jenvman.2022.116599 (2023).
Yan, X. et al. Distribution characteristics and noncarcinogenic risk assessment of culturable airborne bacteria and fungi during winter in Xinxiang, China. Environ. Sci. Pollut. Res. Int. 26, 36698–36709. https://doi.org/10.1007/s11356-019-06720-8 (2019).
Li, Y., Zhang, H., Qiu, X., Zhang, Y. & Wang, H. Dispersion and risk assessment of bacterial aerosols emitted from rotating-brush aerator during summer in a wastewater treatment plant of Xi’an, China. Aerosol Air Qual. Res. 13, 1807–1814. https://doi.org/10.4209/aaqr.2012.09.0245 (2013).
Mortazavi, H. et al. Detection of SARS-CoV-2 in the indoor air and surfaces of subway trains in Mashhad, Iran. Braz. J. Microbiol. 54, 1865–1873. https://doi.org/10.1007/s42770-023-01089-w (2023).
Yan, C., Wang, R.-N. & Zhao, X.-Y. Emission characteristics of bioaerosol and quantitative microbiological risk assessment for equipping individuals with various personal protective equipment in a WWTP. Chemosphere 265, 129117. https://doi.org/10.1016/j.chemosphere.2020.129117 (2021).
Sharma, A., Omidvarborna, H. & Kumar, P. Efficacy of facemasks in mitigating respiratory exposure to submicron aerosols. J. Hazard. Mater. 422, 126783. https://doi.org/10.1016/j.jhazmat.2021.126783 (2022).
Sureka, B. & Misra, S. N95 respirator or triple layer surgical mask: Radiologist perspective. Indian J. Radiol. Imag. 31, S198-s203. https://doi.org/10.4103/ijri.IJRI_350_20 (2021).
(CDC), C. f. D. C. a. P. (2021).
Jeong, S. B., Ko, H. S., Seo, S. C. & Jung, J. H. Evaluation of filtration characteristics and microbial recovery rates of commercial filtering facepiece respirators against airborne bacterial particles. Sci. Total Environ. 682, 729–736. https://doi.org/10.1016/j.scitotenv.2019.05.153 (2019).
Clapp, P. W. et al. Evaluation of cloth masks and modified procedure masks as personal protective equipment for the public during the COVID-19 Pandemic. JAMA Internal Med. 181, 463–469. https://doi.org/10.1001/jamainternmed.2020.8168 (2021).
https://commons.wikimedia.org/wiki/File:Iran_location_map.svg.
Ghanbarian, M., Ghanbarian, M., Ghanbarian, M., Mahvi, A. H. & Hosseini, M. Determination of bacterial and fungal bioaerosols in municipal solid-waste processing facilities of Tehran. J. Environ. Health Sci. Eng. 18, 865–872. https://doi.org/10.1007/s40201-020-00510-y (2020).
Sadigh, A., Fataei, E., Arzanloo, M. & Imani, A. A. Bacteria bioaerosol in the indoor air of educational microenvironments: Measuring exposures and assessing health effects. J. Environ. Health Sci. Eng. 19, 1635–1642. https://doi.org/10.1007/s40201-021-00719-5 (2021).
Madsen, A. M., Frederiksen, M. W., Jacobsen, M. H. & Tendal, K. Towards a risk evaluation of workers’ exposure to handborne and airborne microbial species as exemplified with waste collection workers. Environ. Res. 183, 109177. https://doi.org/10.1016/j.envres.2020.109177 (2020).
Li, L., Zhao, X., Li, Z. & Song, K. COVID-19: Performance study of microplastic inhalation risk posed by wearing masks. J. Hazard. Mater. 411, 124955. https://doi.org/10.1016/j.jhazmat.2020.124955 (2021).
Yan, C., Leng, Y.-L. & Wu, J.-T. Quantitative microbial risk assessment for occupational health of temporary entrants and staffs equipped with various grade PPE and exposed to microbial bioaerosols in two WWTPs. Int. Arch. Occup. Environ. Health 94, 1327–1343. https://doi.org/10.1007/s00420-021-01663-5 (2021).
Pahari, A. K., Dasgupta, D., Patil, R. S. & Mukherji, S. Emission of bacterial bioaerosols from a composting facility in Maharashtra, India. Waste Manag. 53, 22–31. https://doi.org/10.1016/j.wasman.2016.04.027 (2016).
Nabavi, B., Nikaeen, M., Amin, M. & Hatamzadeh, M. Isolation and identification of aerobic polychlorinated biphenyls degrading bacteria. Int. J. Environ. Health Eng. 2, 47–47. https://doi.org/10.4103/2277-9183.122443 (2013).
Wang, Y. et al. The pollution of bioaerosols in hospital sewage purification process: Composition characteristics, seasonal variation and risk assessment. J. Clean. Prod. 419, 138301 (2023).
Chalvatzaki, E., Katsivela, E., Raisi, L. & Lazaridis, M. Assessment of personal deposited dose of bioaerosols and particles in a wastewater treatment plant facility. Air Qual. Atmos. Health 16, 165–181. https://doi.org/10.1007/s11869-022-01264-2 (2023).
USEPA. USERS’ Guide and Background Technical Document for USEPA Region 9'S Preliminary Remediation Goals (PRG) Table. (2011).
Agency, U. S. E. P. Users’ Guide and Background Technical Document for USEPA Region 9—Preliminary Remediation Goals (PRG) Table. (2011).
Hygienists, A. C. o. G. I. ACGIH Committee Activities and Reports. Applied Industrial Hygiene 1, R-19-R-23, https://doi.org/10.1080/08828032.1986.10390461 (1986).
Committee on Risk Assessment of Hazardous Air Pollutants, N. R. C. (1994).
Regulation, D. o. P. (Department of Pesticide Regulation, 2000).
[ATSDR] Agency for Toxic Substances and Disease Registry. 2023. Exposure Dose Guidance for Body Weight. Atlanta, G. U. S. D. o. H. a. H. S. & Public Health Service, J. (2023).
Bahreini, A., Ghaffari, H. R., Behjati, A. M., Zare, S. & Dinarloo, K. The risk of exposure to infectious bacterial bioaerosols in different hospital wards: A case study. Hormozgan Med. J. 27, 73–78. https://doi.org/10.34172/hmj.2023.3087 (2023).
Hana, A.L.A.-R. et al. Assessment of indoor air quality of four primary health care centers in Qatar. Microorganisms 2, 10. https://doi.org/10.3390/microorganisms10102055 (2022).
Mirhoseini, S. H., Nikaeen, M., Shamsizadeh, Z. & Khanahmad, H. Hospital air: A potential route for transmission of infections caused by β-lactam-resistant bacteria. Am. J. Infect. Control 44, 898–904. https://doi.org/10.1016/j.ajic.2016.01.041 (2016).
Madureira, J. et al. Indoor exposure to bioaerosol particles: Levels and implications for inhalation dose rates in schoolchildren. Air Quality Atmos. Health 11, 955–964. https://doi.org/10.1007/s11869-018-0599-8 (2018).
Brągoszewska, E., Mainka, A. & Pastuszka, J. Bacterial aerosols in an urban nursery school in Gliwice, Poland: A case study. Aerobiologia https://doi.org/10.1007/s10453-015-9419-x (2016).
Pan American Health Organization. (2023).
Valedeyni, A. F., Hazrati, S., Arzanlo, M. & Fazlzadeh, M. Assessment of bacterial bio-aerosols types and its concentration in the ambient air of educational hospitals of Ardabil University of Medical Sciences. J. Health-Saf. Work 8, 15–28 (2018).
Mehrasbi, M. R., Mohammadi, G., Mohammadian, F. M., Hajikarim, B. & Jafari, G. Indoor airborne bio aerosols in valiasr hospital in Zanjan Iran. Zums-jhehp 1, 41–48 (2015).
Hosseini, S. S. K. H., Mousavi, S. & Gholampour, A. Seasonal and spatial variations of bioaerosols and antibiotic resistance bacteria in different wards of the hospital. J. Air Pollut. Health 5, 42 (2022).
Rengasamy, S., Eimer, B. C. & Szalajda, J. A quantitative assessment of the total inward leakage of NaCl aerosol representing submicron-size bioaerosol through n95 filtering facepiece respirators and surgical masks. J. Occup. Environ. Hygiene 11, 388–396. https://doi.org/10.1080/15459624.2013.866715 (2014).
Makison, B. C., Clayton, M., Crook, B. & Gawn, J. M. Effectiveness of surgical masks against influenza bioaerosols. J. Hospital Infect. 84, 22–26. https://doi.org/10.1016/j.jhin.2013.02.007 (2013).
Arezoo, T. A. T. Fatemeh karimi microbiological air quality and antibiotic resistance in isolated bioaerosols from various activities in Zanjan, Iran. J. Environ. Health Sustain. Dev. 2, 52. https://doi.org/10.18502/jehsd.v8i2.13042 (2023).
Sudharsanam, S. et al. Characterization of indoor bioaerosols from a hospital ward in a tropical setting. Afr. Health Sci. 12, 217–225. https://doi.org/10.4314/ahs.v12i2.22 (2012).
MJ, Z. S. [Guide to the Evaluation of Bioaerosols in the Workplace OEL-BA-9503]. 1 edn, (Markazsalamat Behdasht, 1395).
Pepper, I. L. & Gerba, C. P. Aeromicrobiology. Environ. Microbiol. 2015, 89–110 (2014).
Kooken, J. M., Fox, K. F. & Fox, A. Characterization of Micrococcus strains isolated from indoor air. Mol. Cell. Probes 26, 1–5. https://doi.org/10.1016/j.mcp.2011.09.003 (2012).
Gizaw, Z., Gebrehiwot, M. & Yenew, C. High bacterial load of indoor air in hospital wards: The case of University of Gondar teaching hospital, Northwest Ethiopia. Multidiscip. Respiratory Med. 11, 24. https://doi.org/10.1186/s40248-016-0061-4 (2016).
Acknowledgements
The authors would like to express their gratitude to Mashhad University of Medical Sciences for providing them with the opportunity to conduct this research. The research was conducted under the research code 4001922 for a student thesis.
Author information
Authors and Affiliations
Contributions
M.B.A. Initial search, sample collection, conducting experiments, manuscript drafting, risk assessments, preparation of figures and charts. M.D. guidance in determining the study design, conceptualization, critical revision, and editing of the manuscript. H.F. Guidance and confirmation of experiments results. M.S.: Guidance in determining the study design. S.G. Guidance in risk assessments.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Alipour, M.B., Davoudi, M., Farsiani, H. et al. The effect of medical face masks on inhalation risk of bacterial bioaerosols in hospital waste decontamination station. Sci Rep 14, 26259 (2024). https://doi.org/10.1038/s41598-024-69088-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-69088-x