Abstract
Head trauma is a common reason for emergency department (ED) visits. Delayed intracranial hemorrhage (ICH) in patients with minor head trauma is a major concern, but controversies exist regarding the incidence of delayed ICH and discharge planning at the ED. This study aimed to determine the incidence of delayed ICH in adults who developed ICH after a negative initial brain computed tomography (CT) at the ED and investigate the clinical outcomes for delayed ICH. This nationwide population cohort study used data from the National Health Insurance Service of Korea from 2013 to 2019. Adult patients who presented to an ED due to trauma and were discharged after a negative brain CT examination were selected. The main outcomes were the incidence of ICH within 14 days after a negative brain CT at initial ED visit and the clinical outcomes of patients with and without delayed ICH. The study patients were followed up to 1 year after the initial ED discharge. Cox proportional hazard regression analysis was used to estimate the hazard ratio for all-cause 1-year mortality of delayed ICH. During the 7-year study period, we identified 626,695 adult patients aged 20 years or older who underwent brain CT at the ED due to minor head trauma, and 2666 (0.4%) were diagnosed with delayed ICH within 14 days after the first visit. Approximately two-thirds of patients (64.3%) were diagnosed with delayed ICH within 3 days, and 84.5% were diagnosed within 7 days. Among the patients with delayed ICH, 71 (2.7%) underwent neurosurgical intervention. After adjustment for age, sex, Charlson Comorbidity Index, and insurance type, delayed ICH (adjusted hazard ratio, 2.15; 95% confidence interval, 1.86–2.48; p < 0.001) was significantly associated with 1-year mortality. The incidence of delayed ICH was 0.4% in the general population, with the majority diagnosed within 7 days. These findings suggest that patient discharge education for close observation for a week may be a feasible strategy for the general population.
Similar content being viewed by others
Introduction
Head trauma is among the most common reasons for emergency department (ED) visits, with most patients presenting with mild head injury1,2,3. Current clinical guidelines for head trauma patients provide clear criteria for performing a brain computed tomography (CT) in the ED; however, controversies exist for special populations in follow-up care after initial brain CT evaluation2,4. For instance, the National Institute for Health and Care Excellence clinical guidelines do not recommend additional observation or serial brain CT for patients on anticoagulants after an initially normal brain CT imaging, while the Eastern Association for the Surgery of Trauma practice management guidelines recommend admission for observation for those with supratherapeutic international normalized ratio2,4.
Delayed intracranial hemorrhage (ICH)—defined as the delayed presentation of ICH on follow-up brain CT after a normal finding at the initial brain CT examination—is among the major concerns for patients with head trauma5. According to previous studies, the incidence of delayed ICH ranges widely from 0.3% to 7.0% in those with any risk factors for delayed ICH6,7. Old age and taking oral anticoagulants or antiplatelet agents have been suggested as risk factors for delayed ICH2,6,7,8,9; however, recent observational studies have shown that oral anticoagulants do not increase the risk of delayed ICH6,10,11. Meanwhile, a recent propensity-matched cohort study conducted in Europe demonstrated anticoagulants and antiplatelet agents to be associated with an increased risk of delayed ICH but not with clinical course or outcomes12. Such a wide range of incidence data and conflicting results can cause confusion among emergency physicians when discharging head trauma patients with normal brain CT scans at the ED. Moreover, the outcomes of delayed ICH are uncertain due to the limited number of patients and hospital settings.
An enhanced understanding of the incidence and outcomes of delayed ICH in patients with minor trauma—where the clinician can conclude that the risk is low enough for discharge from the ED after negative brain CT—could help emergency and trauma physicians to share information with patients and their families after ED discharge and establish better after-care plans for effective hospital resource use. The nationwide population-based study aimed to assess the overall incidence of delayed ICH in adults with initially negative brain CT scans who visited EDs due to minor trauma between 2013 and 2019, as well as the outcomes of those diagnosed with delayed ICH.
Methods
Study design
This population-based cohort study used Korean national claims data from between 2013 and 2019. The Korean National Health Information Database has been releasing the claims data from the National Health Insurance Service (NHIS) annually since 201913. The Korean NHIS covers all Korean citizens and maintains the National Health Information Database, which captures health care utilization, prescription and procedure records, diagnosis codes based on the International Classification of Diseases (ICD) 10th edition, sociodemographic variables, and death records for all Korean citizens14. This study used demographic information, medical treatments, and drug prescriptions with diagnoses based on ICD 10th edition codes.
The primary outcome of this study was the incidence of delayed ICH on follow-up brain CT within 14 days after the initial ED visit among patients with brain trauma without evidence of ICH at the initial brain CT. The secondary outcomes were data related to the 1-year clinical course of those patients, including hospitalization, operation, and mortality after the initial ED visit.
Study patients and data definitions
We defined adult patients, aged 20 years or older, presenting with minor head trauma as individuals who underwent brain CT due to head trauma and were subsequently discharged directly from the ED without traumatic ICH diagnosis codes. Initially, we identified all adult patients whose discharge diagnoses covered by ICD 10th edition codes S00 to T14 at their initial ED presentation between 2013 and 2019. Among those patients, we excluded patients who expired in the ED, those who required emergency admissions, and those with traumatic ICH diagnoses with ICD codes from S061 to S069. We defined patients with delayed ICH as those who underwent brain CT within 14 days repeatedly after initial ED discharge and had traumatic ICH diagnosis codes from S061 to S069. The study patients were followed up from their respective initial ED visit dates to at least 1 year or the date of death, if it occurred within 1 year. We extracted information on provided medical services, including neurosurgery, ie, craniotomy for evacuation of hematoma (treatment codes S4621 and S4622), and hospitalization in an intensive care unit or a general ward. When patients had records of 2 or more hospital visits with the relevant ICD-10 diagnostic codes within a year before the initial ED visit, we assumed they had underlying comorbidities.
Statistical analysis
The characteristics of the patients with and without delayed ICH are presented using descriptive analyses. Continuous variables are presented as means with standard deviations. Categorical data are presented as absolute numbers with percentages. Comparisons of the characteristics and outcomes between the patients with and without delayed ICH were performed using the chi-square test or Fisher’s exact test for categorical variables and Student’s t-test for continuous variables, as appropriate. Cox proportional hazards regression analysis was used to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) for all-cause 1-year mortality associated with delayed ICH. The adjusted HR for delayed ICH associated with 1-year mortality was calculated after adjusting age, sex, Charlson Comorbidity Index, and insurance type (national health insurance vs. Medicaid). A two-tailed P value < 0.05 was considered statistically significant. These analyses were conducted using Enterprise Guide, version 7.1 (SAS Institute Inc., Cary, NC, USA).
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki. The institutional review board of Asan Medical Center approved the study protocol (No. 2020-1818). Need for patient informed consent was waived by the institutional review board of Asan Medical Center due to the de-identification of the national insurance claims data.
Results
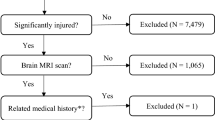
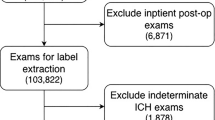
From 2013 through 2019, 995,476 adult patients aged 20 years or older underwent brain CT at the ED due to trauma. Finally, 626,695 patients were included in our analyses after the exclusion of 368,781 patients who were admitted to the hospital via the ED (n = 251,103), had a diagnosis of ICH (n = 115,831), died in the ED (n = 624), or were not followed up (n = 1223) (Fig. 1). Among the eligible patients, 2666 (0.4%) were diagnosed with ICH within 14 days after an initial ED visit. The median time from the initial ED visit to the diagnosis of delayed ICH was 2 days (interquartile range, 1–5 days). There were 1065 patients (39.9%) who were diagnosed within 24 h, 1714 patients (64.3%) diagnosed within 3 days, and 2252 patients (84.5%) within a week (Fig. 2).
Table 1 presents the characteristics of the study patients with and without delayed ICH. Patients with delayed ICH were older (mean, 60.1 vs. 52.9 years, p < 0.001) and more frequently male (63.2% vs. 57.1%, p < 0.001). The delayed ICH patients had approximately 1.5-to-2-fold higher rates of comorbid diseases, including ischemic stroke (12.2% vs. 6.8%, p < 0.001), ischemic heart disease (8.7% vs. 5.8%, p < 0.001), dementia (9.0% vs. 5.4%, p < 0.001), and atrial fibrillation (3.6% vs. 1.4%, p < 0.001). There was also a significant intergroup difference in insurance type, with Medicaid being more frequent in those with delayed ICH (10.6% vs. 7.5%, p < 0.001). Traumatic subdural hemorrhage (n = 1,113, 41.7%) was the most prevalent diagnostic code (S065) among patients with delayed ICH, followed by unspecified intracranial injuries (S068, S079; n = 408, 15.3%), diffuse brain injury (S062; n = 400, 15.0%), and traumatic subarachnoid hemorrhage (S066; n = 350, 12.9%) (Additional file 1).
Table 2 compares the outcomes among the patients with and without delayed ICH. All major adverse events occurred significantly more frequently in patients with delayed ICH relative to those without delayed ICH. A total of 73 patients (2.7%) underwent craniotomy for hematoma evacuation, and 554 patients (20.8%) were admitted to an intensive care unit within 6 months after the initial ED visit. The all-cause of mortality rate within 1 year was significantly higher in the delayed ICH group (8.0% vs. 2.5%, p < 0.001).
The cumulative incidence of all-cause death in patients with and without delayed ICH is depicted in Fig. 3 The univariate Cox proportional hazards analysis indicated the occurrence of delayed ICH (HR, 3.31; 95% CI 2.89–3.80; p < 0.001) to be significantly associated with all-cause 1-year mortality. After adjusting for age, sex, Charlson Comorbidity Index, and insurance type, delayed ICH (adjusted HR, 2.15; 95% CI 1.86–2.48; p < 0.001) remained significantly associated with all-cause 1-year mortality in the multivariate Cox proportional hazards analysis.
Discussion
This national population-based cohort study found that the incidence of delayed ICH was 0.4% (2666/626,695). The median time to the diagnosis of delayed ICH was 2 days (interquartile range, 1–5 days), with over 80% of patients being diagnosed within 1 week, which implies that intensive monitoring for 1 week would be necessary after discharge. Despite two-fifths of traumatic subdural hemorrhage among the patients with delayed ICH, neurosurgical intervention was rarely performed for these patients (2.7%), suggesting the majority of delayed ICH was treated conservatively. However, delayed ICH appeared to significantly increase the risk of 1-year mortality over twofold after adjusting for age, sex, Charlson Comorbidity Index, and insurance type (adjusted HR, 2.15; 95% CI 1.86–2.48; p < 0.001).
The overall incidence of delayed ICH in this study was 0.4%, consistent with recent well-designed studies. Chenoweth et al.6 found that the incidence of delayed ICH identified on follow-up brain CT within 14 days from the initial ED visit was 0.3% (3/859) among patients 55 years and older, regardless of their anticoagulant or antiplatelet medication use. Another prospective cohort study, including patients aged 65 years and older, demonstrated an overall incidence of delayed ICH of 0.4% (10/2423)15. Mourad et al.11 found that 0.5% (2/420) of patients on direct oral anticoagulants had delayed ICH on follow-up brain CT within 24 h following initially negative CT. Despite the similar 0.4% incidence found in our study, it is important to note that this incidence would be the maximum incidence of delayed ICH in the general population with clinical impact. Unlike previous research that focused on populations with known clinical risk factors for delayed ICH, such as advance age or the use of particular medications, our study encompassed a more general population. This population primarily included individuals with minor injuries who were likely to be discharged directly from the ED regardless of presence of specific risk factors. Furthermore, the observational nature of this study suggests that patients themselves revisited the hospital and underwent follow-up brain CT due to new-onset or worsening symptoms rather than as part of a predefined protocol. The 14-day window from the initial ED visit could include acute ICH cases associated with additional injury as the delayed ICH cases.
Some experts recommend hospital admission for observation for at least 12 to 24 h and routine follow-up of brain CT to detect the early development of extradural or subdural hematoma or diffuse cerebral edema16,17,18,19,20,21. However, there have been doubts about whether this observation period was sufficient to rule out the risk of delayed ICH2,22. Hemorrhagic progression usually occurs within the first 12 h but may occur as late as 3 to 4 days after head trauma23,24. Chenoweth et al.6 observed that 2 out of the 3 cases of delayed ICH occurred 3 days and 5 days after the initial brain CT scans, respectively. Swap et al.25 even documented a case wherein delayed ICH was identified 54 days after the initial CT scan. In our study, the median time for diagnosing delayed ICH was 2 days, with approximately two-fifths (39.9%) being diagnosed within 1 day and more than four-fifths (84.5%) within 1 week. Although the patients in our study were highly likely to undergo CT reevaluation due to their symptoms, our findings suggest that the strategy of 24-h observation and CT reevaluation may miss more than half of the patients with delayed ICH. Providing comprehensive discharge education to patients and their families regarding symptom monitoring for at least 1 week, with a focus on promptly returning to the ED if symptoms worsen, would be a more feasible and practical approach than admitting patients for 24 h and scheduling follow-up brain CT scans.
Many previous studies have investigated the clinical outcomes of patients with delayed ICH, but the low incidence of delayed ICH and limited number of patients with delayed ICH have contributed to unreliable results. Some studies have found that patients with delayed ICH did not undergo neurosurgical intervention or died as a consequence of the delayed ICH11,15,22,26. In contrast, Chenoweth et al.6 observed that 1 of 3 patients with delayed ICH among the 859 patients aged 55 and older with blunt head trauma underwent bilateral burr holes procedures with drainage of subdural hygromas. Another retrospective observational study including patients with head trauma and antithrombotic therapy found that 1 of 11 patients with delayed ICH needed urgent decompressive craniectomy with a 1.2% incidence of delayed ICH (11/793)27. Our nationwide population-level cohort study revealed that traumatic subdural hemorrhage was the most prevalent form of delayed ICH (41.7%). Although the pathogenesis of delayed ICH has not been entirely elucidated, our findings suggest that vascular dysfunction arising from enzymatic and free radical injury to vessel walls lead to perivascular leaks or microvascular ruptures, particularly affecting bridging veins28,29. In our study, craniotomy was performed for 73 of 2666 patients with delayed ICH (2.7%) and that 554 patients (20.8%) were admitted to an intensive care unit within 6 months after their respective initial ED visits. These results suggest that the majority of the patients were managed conservatively with a substantial sample size to obtain reliable results regarding clinical outcomes. However, it was also notable that the cumulative incidence of all-cause death among patients with delayed ICH was significantly higher, and delayed ICH was associated with increased all-cause 1-year mortality even after adjusting for other factors. Therefore, a protocol including routine repeat brain CT or hospitalization for observation may not be necessary, considering the low incidence of delayed ICH. Instead, it is crucial to provide systematic discharge education to both patients and caregivers, emphasizing thorough self-observation for potential delayed complications during the week after ED discharge.
To our knowledge, this study was the first to investigate the incidence of delayed ICH using the Korean National Health Information Database. This database covers almost all Koreans (97%) and has minimal loss to follow-up14. The highly accurate information about procedures, admissions, and deaths is another strength of our study, which contributes to a comprehensive understanding of the incidence and outcomes among patients with delayed ICH. However, this study had several limitations. Firstly, the National Health Information Database in Korea does not provide specific laboratory and clinical data13, such as trauma timing, injury type, and neurologic status at ED visits. The definition of minor head trauma was based on the Glasgow Coma Scale, but this study assumed the minor head trauma using the diagnosis codes and ED disposition, potentially leading to an overestimation of the incidence of delayed ICH. Distinguishing between acute ICH due to recurrent head trauma after the initial ED discharge and delayed ICH was impossible due to the lack of clinical data, which could lead to an overestimation of the incidence of delayed ICH. Also, as the cause of death in our study patients are unknown, making the causal relationship between delayed ICH and 1-year mortality uncertain. Secondly, delayed ICH may have been underestimated because some patients with mild symptoms might not seek additional hospital visits and examinations. Among the patients categorized as not having delayed ICH, 490 (0.1%) out of 624,029 underwent craniotomy within 6 months, and the possibility of delayed ICH cannot be ruled out for these cases. Lastly, it was possible that we included cases as delayed ICH in which acute ICH was initially missed during the first ED visit and later diagnosed.
Conclusions
The incidence of delayed ICH after minor head trauma was low in the general population (0.4%), and most patients were diagnosed within 1 week. Furthermore, even after the diagnosis of delayed ICH, neurosurgical interventions were rarely required. Systematic and aggressive discharge education, including thorough monitoring for neurological symptoms for at least 7 days after ED discharge, would be a more feasible strategy than routine follow-up brain CT scans or hospitalization for observation for the general population without any clinical risk factors.
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
- ED:
-
Emergency department
- CT:
-
Computed tomography
- ICH:
-
Intracranial hemorrhage
- NHIS:
-
National Health Insurance Service
- ICD:
-
International Classification of Diseases
- HRs:
-
Hazard ratios
- CIs:
-
Confidence intervals
References
Feigin, V. L. et al. Incidence of traumatic brain injury in New Zealand: A population-based study. Lancet Neurol. 12(1), 53–64 (2013).
Rajesh, S., Wonderling, D., Bernstein, I., Balson, C. & Lecky, F. Head injury: Assessment and early management—summary of updated NICE guidance. BMJ. 381, 1130 (2023).
Hang, A., Park, B. L. & Ro, Y. S. Trends in traumatic brain injury–related emergency department visits in Korea: A report from the National Emergency Department Information System (NEDIS) 2018–2022. Clin. Exp. Emerg. Med. 10(S), S63–S68 (2023).
Barbosa, R. R. et al. Evaluation and management of mild traumatic brain injury: An Eastern Association for the Surgery of Trauma practice management guideline. J. Trauma Acute Care Surg. 73(5), S307–S314 (2012).
Mitra, B., Ruggles, T., Seah, J., Miller, C. & Fitzgerald, M. C. Delayed intracranial hemorrhage after trauma. Brain Inj. 35(4), 484–489 (2021).
Chenoweth, J. A. et al. Incidence of delayed intracranial hemorrhage in older patients after blunt head trauma. JAMA Surg. 153(6), 570–575 (2018).
Colombo, G. et al. Incidence of delayed bleeding in patients on antiplatelet therapy after mild traumatic brain injury: A systematic review and meta-analysis. Scand. J. Trauma Resusc. Emerg. Med. 29(1), 123 (2021).
Miller, J. et al. Delayed intracranial hemorrhage in the anticoagulated patient: A systematic review. J. Trauma Acute Care Surg. 79(2), 310–313 (2015).
Cocca, A. T. et al. Delayed intracranial hemorrhage in anticoagulated geriatric patients after ground level falls. J. Emerg. Med. 57(6), 812–816 (2019).
Soleimani, T., Mosher, B., Ochoa-Frongia, L., Stevens, P. & Kepros, J. P. Delayed intracranial hemorrhage after blunt head injury with direct oral anticoagulants. J. Surg. Res. 257, 394–398 (2021).
Mourad, M., Senay, A. & Kharbutli, B. The utility of a second head CT scan after a negative initial CT scan in head trauma patients on new direct oral anticoagulants (DOACs). Injury. 52(9), 2571–2575 (2021).
Mathieu, F. et al. Impact of antithrombotic agents on radiological lesion progression in acute traumatic brain injury: A CENTER-TBI propensity-matched cohort analysis. J. Neurotrauma. 37(19), 2069–2080 (2020).
Kim, Y.-J., Kim, M.-J., Kim, Y.-J. & Kim, W. Y. Short and long-term mortality trends for cancer patients with septic shock stratified by cancer type from 2009 to 2017: A population-based cohort study. Cancers 13(4), 657 (2021).
Cheol Seong, S. et al. Data resource profile: The national health information database of the National Health Insurance Service in South Korea. Int. J. Epidemiol. 46(3), 799–800 (2017).
Alter, S., Solano, J., Engstrom, G. & Shih, R. 94 traumatic intracranial hemorrhage in geriatric patients on warfarin, direct oral anticoagulants, or no anticoagulation: A prospective study. Ann. Emerg. Med. 76(4), S37 (2020).
Vos, P. E. et al. EFNS guideline on mild traumatic brain injury: Report of an EFNS task force. Eur. J. Neurol. 9(3), 207–219 (2002).
Masters, S. J. Skull X-ray examinations after head trauma Recommendations by a multidisciplinary panel and validation study. N. Engl. J. Med. 316(2), 84–91 (1987).
Bartlett, J. et al. Recommendations from the Society of British Neurological Surgeons. Br. J. Neurosurg. 12(4), 349–352 (1998).
Committee on Quality Improvement AAoPCoCP, Research AAoFP. The management of minor closed head injury in children. Pediatrics. 104(6), 1407–1415 (1999).
Ingebrigtsen, T., Romner, B. & Kock-Jensen, C. Scandinavian guidelines for initial management of minimal, mild, and moderate head injuries. J. Trauma. 48(4), 760–766 (2000).
Twijnstra, A. et al. Richtlijnen voor de diagnostiek en behandeling van patienten met licht schedel-hersenletsel. Commissie Kwaliteitsbevordering van de Nederlandse Vereniging voor Neurologie. 1, 1–26 (2001).
Turcato, G. et al. Risk of delayed intracranial haemorrhage after an initial negative CT in patients on DOACs with mild traumatic brain injury. Am. J. Emerg. Med. 53, 185–189 (2022).
Kurland, D., Hong, C., Aarabi, B., Gerzanich, V. & Simard, J. M. Hemorrhagic progression of a contusion after traumatic brain injury: A review. J. Neurotrauma. 29(1), 19–31 (2012).
Fainardi, E., Chieregato, A., Antonelli, V., Fagioli, L. & Servadei, F. Time course of CT evolution in traumatic subarachnoid haemorrhage: A study of 141 patients. Acta Neurochir. 146(3), 257–263 (2004).
Swap, C., Sidell, M., Ogaz, R. & Sharp, A. Risk of delayed intracerebral hemorrhage in anticoagulated patients after minor head trauma: The role of repeat cranial computed tomography. Perm. J. 20(2), 14 (2016).
Hughes, P. G. et al. Acute and delayed intracranial hemorrhage in head-injured patients on warfarin versus direct oral anticoagulant therapy. J. Emerg. Trauma Shock. 14(3), 123–127 (2021).
Antoni, A. et al. Delayed intracranial hemorrhage in patients with head trauma and antithrombotic therapy. J. Clin. Med. 8(11), 1780 (2019).
Ziechmann, R., Pathak, S. M., Welch, J. & Villanueva, P. Delayed traumatic intracerebral hematoma: A pathophysiological classification and literature review. Cureus. 15(8), e42987 (2023).
Kuge, A. et al. Delayed acute subdural hematoma treated with endoscopic procedure: A case report. Surg. Neurol. Int. 11, 350 (2020).
Funding
This research was supported by a grant from the Ministry of Health & Welfare, Republic of Korea (grant number: HI23C0304). The study sponsors had no involvement in the study design; in the collection, analysis and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
HK contributed to investigation, writing—original draft preparation, writing—review and editing. YJK contributed to conceptualization, methodology, investigation, writing—original draft preparation, writing—review and editing, visualization, and project administration. JHL contributed to conceptualization, investigation, resources, writing—review and editing, supervision, and project administration. SK and YJK contributed to data curation, formal analysis, validation, writing—review and editing, and visualization. WYK contributed to resources and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kwon, H., Kim, YJ., Lee, JH. et al. Incidence and outcomes of delayed intracranial hemorrhage: a population-based cohort study. Sci Rep 14, 19502 (2024). https://doi.org/10.1038/s41598-024-70553-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-70553-w