Abstract
The risk of virus transmission via the touching of contaminated masks has long been assumed by infection control teams. Yet, robust evidence to support this belief has been lacking. This risk was investigated in a laboratory setting by measuring the amount of viable influenza virus successfully transferred from artificially contaminated medical (surgical) mask surfaces to a human finger used to swipe their outer surface under various experimental conditions. Despite being exposed to high levels of virus contamination on the masks, very little or no viable virus was successfully transferred from the mask to the finger in these experiments.
Similar content being viewed by others
Introduction
Respiratory viral infections such as influenza have been considered to spread through two major routes: by inhalation of aerosols or droplets and via direct or indirect contact with contaminated surfaces. The latter route has long been emphasized in the field of infection control. The touching of contaminated masks is also traditionally assumed to be a risk of viral transmission in hospital infection control practices for the prevention of nosocomial infection of influenza, as well as of other infectious diseases. However, there is a notable lack of evidence supporting this route of transmission, despite the amount of infection control guidance related to this, including various personal protective equipment (PPE) donning/doffing guidelines1.
This study, conducted in a laboratory setting, investigates this risk for influenza transmission by quantitatively assessing the transfer of viable viruses from artificially contaminated medical (surgical) masks to human fingers. The surgical masks were exposed to airborne virus under differing experimental conditions, which mimicked common clinical exposure scenarios.
Results
Overall, with this experimental simulation, the number of transferred viruses was under the detection level or almost undetectable from the contaminated mask surfaces to the swiping finger. No virus or only a small amount (maximum 10 pfu) of the virus was detected in the experiments that used the nebulizer and coughing machine, which used large amounts of the virus under conditions reasonably favorable for influenza virus survival (20 °C, 20% RH) (Fig. 1a, b). Similarly, in the spray experiments under a variety of temperatures and RHs, little or no virus was detected on the swiping fingertip (Fig. 1c).
External mask surface-to-finger virus transfer results, after mask exposure to the simulated environmental aerosols (a), simulated coughing (b) and large droplet spraying (c). For a (simulated environmental aerosols), the column plots show the amount of exhaled viable influenza virus particles (solid bar) and viral RNA (open bar) captured in the aerosols after sampling for 30 min from the air (I), the theoretical maximum amount of virus that should be captured on the mask during 30 min of simulated breathing (II), and the measured amount of virus collected by a finger swipe from the mask surface (III). Column (IV) shows the viral RNA copies detected from the outer layer of the mask. For (b) (simulated coughing), the amounts of viable virus (solid bar) and viral RNA (open bar) detected after finger-swiping of the mask, at exposure from distances of 100 and 200 cm are shown. For (c) (large droplet spraying), the plaque-forming (viable) virus and viral RNA detection, are shown at 20 and 30 °C, at 20, 50, and 70% relative humidities, for each size (100, 200, and 500 μm diameter) of the droplet, at 30 min sampling times. In all figures, the dotted and dashed lines show the minimum detection limits of the plaque-forming and RT-qPCR assays.
Discussion
Surgical masks are designed to capture and trap aerosol particles by multiple means, including inertial impaction, gravity sedimentation, electrostatic attraction, diffusion, and interception2. It has been a concern that viral transfer from the mask surface contaminated with the virus via fingers or hands causes infection since people touch the face frequently while even wearing it (e.g., 5–6.4 face touches/h)3,4. However, there is little or no evidence of transfer of the viable virus. Our calibration studies (Figs. S1c, S2b, S3) were performed in order to measure the viral load in the air when it was directly sampled for 30 min (225 L). This gave an estimate of the viral load entering the breathing zone of the unmasked manikin head and the total amount of virus passing through the mask area. This allowed an approximation of the theoretical maximum amount of virus that could potentially be trapped on or within the mask. They showed a clear contrast with the viral load recovered from the finger that swiped the mask surface. The viral titer of the sampled aerosol was 5.9 × 102 pfu/L air and 4.9 × 104 viral RNA copies/L air (see Fig. 1a). This is far higher than various studies of ambient aerosol viral loads for influenza in real-world studies5,6. Yet, despite exposing the mask to these massive aerosolized virus loads, little or no viable virus transferred to the fingertip from the mask surface. From these results, it would be unlikely that viable viruses would be recovered from fingertips that touched contaminated physical and environmental surfaces, even with different types/subtypes of other human influenza viruses.
So why was the amount of virus recovered from the mask surface via the fingertip so low? Firstly, not all of the airborne viruses inhaled through the mask would remain on the outer layer of the mask since a certain proportion of the inhaled viruses penetrate a surgical mask7. Those viruses that passed through the surface layer would not be touchable by the swiping fingertip. This ratio of surface (touchable) virus versus virus possibly penetrating the mask can be deduced as follows. In the pre-experimental calibration studies, the amount of virus that could have been inhaled without the mask, was theoretically calculated to be 1.0 × 107 viral RNA copies. The actual viral load detected from the surface sheet of the central area cut out was only 2.4 × 105 viral RNA copies (mean of 3.19 × 105 and 1.47 × 105 copies). Hence, the recovery efficiency of viral gene copy numbers is 2.4 × 10–2. Secondly, the airborne virus in this study had a viable virus/viral RNA copy ratio of about 1:103 (Fig. 1a column I).
So if this same recovery rate could be applied to the virus detected on the mask outer layer (2.4 × 105 viral RNA copies), about 2.4 × 102 pfu of viable virus might be detected. However, the amount of detectable virus recovered from the fingertip swipe was only < 3.3 pfu (less than the detection limit of the plaque assay) and < 3.0 × 103 viral RNA copies (less than the detection limit of the PCR assay) (the recovery efficiency of viable virus, < 1.4 × 10–2) (Fig. 1).
We noted relatively little change in the ratio of the airborne viruses released from the nebulizer for 30 min after atomization in the calibration experiments (Fig. S4). Therefore, this discrepancy is logically attributable to either some degree of viral inactivation on the mask surface, poor efficiency of the viral transfer from the mask surface to the finger, or a combination of the two. It might apply to the experiments using the coughing machine and sprays. Regarding the poor viral transfer efficiency from the mask surface, one may doubt the generalization of the result since our study was on only one brand of water-repellent surgical masks made of non-woven chemical fiber filters. However, there was a report that the transfer efficiency of a virus from the porous surface of the polyester fabric was also very poor at about 0.3%8.
It is notable that despite the viral loads used in these transmission experiments being very high compared to real-world settings, there was still little or no transmission via fingertip swiping. In addition, even if a very small amount of the virus were transferred to the fingertip or hand, their viability would decrease rapidly9,10. Furthermore, the transmission of influenza via fingers is thought to occur by contact of the contaminated fingertip with the nasal mucosal membrane, but the low infection efficiency by such a nasal route was also seen in data from an efficacy study for the influenza drug, oseltamivir11. Therefore, based on these study results, the risk of viral transmission via this fingertip-mask surface-touching route appears extremely low—in contrast to commonly cited infection control guidance.
While we agree that a ‘bundled’ approach to infection control may be effective in sending a single message of how to disinfect surfaces and maintain good hand hygiene, we believe that this can go too far, as was seen with the excesses of ‘hygiene theatre’ highlighted during the COVID-19 pandemic12. At least one other real-world study showed little or no external mask viral contamination13. Thus, that study, together with the results in this current study and the plausible mechanisms discussed to explain these findings, are likely applicable to other human respiratory viruses that are also substantially airborne14,15.
This is not to say that hand-washing and fomite transmission precautions are not important. This study, together with another12, simply suggests that the risk of viral transmission via touching the surface of used masks is low.
Methods
Surgical masks and experimental set-up
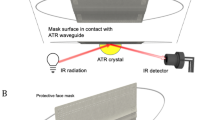
Water-repellent surgical masks (Medical Mask CP, Taketora, Tokyo, Japan) are made of three sheets of non-woven chemical fiber filters. They were exposed to a variety of ‘source’ influenza virus aerosols/ droplets generated in different ways: (1) via a commercial electric nebulizer (NE-C28, Omron Healthcare, Kyoto, Japan) to simulate general environmental airborne virus contamination, including that generated from coughing and sneezing (particle sizes: 0.3–5 µm, Fig. S5); (2) a coughing machine simulating strong coughs, with exit particle velocities of 9 –12 m/s16 (AC100, Saika, Tokyo, Japan) (particle sizes: 0.1–100 µm, Fig. S6); and (3) larger droplets generated by carefully calibrated spray bottles to simulate occasional exposures of the mask surface to large droplets contained in droplets released by speaking, coughing, or sneezing from a short distance of 40 cm (approximate particle sizes: 100, 200, and 500 µm, Fig. S7)17. All experiments were performed within an air-tight environmental chamber (3.6 m long × 3.3m wide × 2m tall) or 1 m3 cube, at 20 °C and 20% relative humidity (RH), except the spraying experiments that were performed at 20 and 30 °C, and 20, 50 and 70% RH conditions.
Simulations for human subject and exposure
A ‘recipient’ (exposed) manikin head was connected to a ‘breathing’ machine (SN-480-3, Shinano, Tokyo) (0.5 L/breath, 15 breaths/min) and set as a simulation model of a human wearing a mask8 (Figs. 2, S1, S8). The idea was that any virus-laden aerosols would be pulled towards the outer mask surface and become trapped there during the inhalation-exhalation (breathing) cycle, which would then act as a source of contamination to any fingers subsequently touching this outer mask surface. For general environmental exposure to the nebulizer-generated aerosols, the viral fluid was atomized for 30 s, followed by mixing the chamber air. The masked manikin head was set to breathe for 30 min from the start of the atomization to inhale the aerosol with the virus through the mask. After this, a human finger (coauthor YF) that had been cleaned (in 70% W/V ethanol) and allowed to dry, was used to swipe a 2 cm × 2 cm central area of the outer surface of the mask (Fig. S2 b). This now ‘contaminated’ finger was then rinsed immediately for up to 20 s with 3 mL MEM (viral minimum essential media). This MEM was then used in a viral plaque assay to detect and quantify any viable virus. It was also used in a reverse-transcription PCR (RT-PCR) assay to quantify any viral RNA present (Fig. S8).
Finger-swiping experiments
For the nebulizer experiments, where the manikin head was attached to the breathing machine, we also examined how much virus was present on the mask's outer surface that might be available to the finger swipe. For this, the 2cm x2cm central area of the mask that was not swiped by the finger as a control was also cut out, and its outer surface sheet was vortexed in RNA extraction buffer, which was then tested using the RT-PCR assay to directly quantify the amount of virus present (Fig. S8d). This same finger swiping and virus detection process, after the same 30-min delay, was repeated after the masked manikin head was exposed to the simulated coughing (five coughs, at 100 and 200 cm distance, expelling a total of 0.22 mL of viral fluid (Fig. S1b). For each new exposure distance, the manikin head was fitted with a new mask. The spraying experiments were performed at two temperatures (20 and 30 °C) and three different relative humidities (20, 50, and 70%) without connection to the breathing machine, with 2× spray puffs used for each particle size (100, 200, and 500 µm), from a distance of 40 cm distance, exposing the mask to a total of 0.08–0.25 mL of the viral fluid, containing up to a total of 107 pfu of virus (Fig. S9). For each new particle size, the manikin head was fitted with a new mask.
Aerosol sampling
Aerosolized influenza viruses were collected into MEM using a sampling system consisting of an air sampler containing a gelatin filter (MD8 AirScan Sartorius AG, Göttingen, Germany)5. Air containing airborne virus was pulled through the filter by the breathing machine for a sampling time of 30 min. The gelatin filter (80 mm diameter) membrane was dissolved in 10 mL MEM and then subjected to conventional plaque or real-time RT-qPCR assay detection.
Virus and cell culture
The virus used in these experiments was influenza A/Aichi/2/68 (H3N2), which was propagated in the allantoic cavity of 10-day-old fertilized hens’ eggs and then stored at − 80 °C as the working viral fluid. The viable titer of the viral fluid was about 108 pfu/mL, and its protein concentration was about 10 mg/mL. Madin-Darby canine kidney (MDCK) cells were cultured in minimum essential medium (MEM; Sigma-Aldrich, St. Louis, MO, USA) containing 10% fetal bovine serum (Thermo Fisher Scientific, Waltham, MS, USA), 1.7% glucose, 100 unit/mL penicillin G (Meiji Co., Tokyo, Japan), and 100 µg/mL streptomycin, sub-cultured in 24 well-plates and used for the conventional plaque assay of the virus.
Plaque assay of the virus
Briefly, MDCK cells cultured in 24-well plates were inoculated with the viral sample and placed in a 5% CO2 incubator at 34 °C for 1 h, followed by washing with serum-free MEM, overlayed with MEM supplemented with 5 µg/mL trypsin and 0.8% agar, and kept in the incubator at 37 °C. After two days, the overlay was removed, and the cell layer was stained with 0.1% crystal violet in 20% methanol for plaque number counting.
Viral RNA testing
Viral RNA was extracted from samples using the QIAamp viral RNA Mini Kits (QIAGEN, Hilden, Germany) according to the manufacturer’s protocol. A quantitative reverse transcription polymerase chain reaction assay was performed using PrimeScript One Step RT-PCR Kit Ver.2 (TaKaRa Bio, Shiga, Japan) with specific primers for RT-PCR designed for forward (5’-TAACCGAGGTCGAAACGTA-3’) and reverse (5’-GCACGGTGAGCGTGAA-3’) and probes targeting the matrix protein 1 (M1) gene18.
All the experiments using the virus were performed at least twice, and averages of viral titers were shown in the graphs (Fig. 1a, b), except the spray experiments that were performed three times, and the averages and standard deviations were shown in the graph (Fig. 1c).
Data availability
Data will be available upon reasonable request to the Corresponding Authors.
References
CDC. How to safely remove personal protective equipment (PPE) Example 2. ppe-sequence-p.pdf (cdc.gov) (2024).
Tcharkhtchi, A. et al. An overview of filtration efficiency through the masks: Mechanisms of the aerosols penetration. Bioactive Mater. 6, 106–122 (2021).
Lucas, T. L., Mustain, R. & Goldsby, R. E. Frequency of face touching with and without a mask in pediatric hematology/oncology health care professionals. Pediatr. Blood Cancer 67, e28593 (2022).
Church, L. E. & Nagi, G. Comment on: Frequency of face touching with and without a mask in pediatric hematology/oncology health care professionals: For application to the COVID-19 pandemic. Pediatr. Blood Cancer 67, e28634 (2020).
Hatagishi, E. et al. Establishment and clinical applications of a portable system for capturing influenza viruses released through coughing. PLoS One. 9, e103560 (2014).
Chamseddine, A. et al. Detection of influenza virus in air samples of patient rooms. J. Hosp. Infect. 108, 33–42 (2021).
Lopez, G. U. et al. Transfer efficiency of bacteria and viruses from porous and nonporous fomites to fingers under different relative humidity conditions. Appl. Environ. Microbiol. 79, 5728–5734 (2013).
Ueki, H. et al. Effectiveness of face masks in preventing airborne transmission of SARS-CoV-2. mSphere 5, 00637–20 (2020).
Bean, B. et al. Survival of influenza-viruses on environmental surfaces. J. Infect. Dis. 146, 47–51 (1982).
Thomas, Y. et al. Survival of influenza virus on human fingers. Clin. Microbiol. Infect. 20, O58–O64 (2014).
Hayden, F. G. et al. Safety and efficacy of the neuraminidase inhibitor GG167 in experimental human influenza. JAMA. 275, 295–299 (1996).
Goldman, E. Exaggerated risk of transmission of COVID-19 by fomites. Lancet Infect. https://doi.org/10.1016/S1473-3099(20)30561-238 (2020).
Fouda, A. et al. A study of staff mask contamination on a respiratory admissions ward managing COVID-19 patients reveals concern with infection prevention practice. Clin. Infect. Pract. 12, 100085 (2021).
Tang, J. W., Marr, L. C., Tellier, R. & Dancer, S. J. Airborne transmission of respiratory viruses including severe acute respiratory syndrome coronavirus 2. Curr. Opin. Pulm. Med. 29, 191–196 (2023).
Tang, J. W., Tellier, R. & Li, Y. Hypothesis: All respiratory viruses (including SARS-CoV-2) are aerosol-transmitted. Indoor Air 32, e12937 (2022).
Ogata, M. et al. Measurement of cough droplet deposition using the cough machine. Environ. Eng. AIJ 83, 57–64 (2018).
Jennison, M. W. Atomizing of mouth and nose secretions into the air as revealed by high-speed photography. In Aerobiology (ed. Moulton F. R) 106–128 (American Association for the Advancement of Science, 1942).
Daum, L. T. et al. Real-time RT-PCR assays for type and subtype detection of influenza A and B viruses. Influenza Other Respir. Viruses 1, 167–175 (2007).
Acknowledgements
We thank Ms. Atsuko Hayase and Dr. Mori Takuya of the Kao Corp. for their help in measuring particle sizes in the spray experiments. We also want to express our gratitude to a Master course student, Ms. Yang Jie for the useful discussion.
Funding
This work was funded by the Clinical Research Division of Sendai Medical Center, the Japan Agency for Medical Research and Development (Grant Numbers JPwm0125001 and 20fk0108119h0001) to HN.
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: HN, MK, SE, YF, JT.; Performed experiments: YF, HN, SS, YO. Analyzed the data: YF, HN, SS, YO, JT.; Contributed reagents/materials/analysis tools: YO, KM, SE, YF.; Wrote the manuscript: YF, HN, JT; All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fan, Y., Nishimura, H., Sakata, S. et al. Minimal influenza virus transmission from touching contaminated face masks: a laboratory study. Sci Rep 14, 20211 (2024). https://doi.org/10.1038/s41598-024-70615-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-70615-z