Abstract
Major earthquakes have occurred frequently in Japan throughout history, and the 2024 Noto earthquake is no exception. However, such natural disasters differ in some respects, and specific problems related to these events have also become clear. Kanazawa Medical University Hospital, which was the closest university hospital to the disaster area of the 2024 Noto earthquake, played a crucial role in serving the local community in the wake of the earthquake. The first method used to identify disaster-related patients is to tag them when they are examined by a physician. After confirming that a patient was eligible at the disaster-related patient-determination meeting, patients’ medical information was extracted from the tag name. A total of 421 disaster-related patients were transported and hospitalized by day 31. Fifty-two (14.4%) and 48 (13.3%) patients were admitted for orthopedic surgery and respiratory medicine, respectively. Forty (11.1%) and 38 (10.5%) patients were admitted to cardiology and nephrology departments, respectively. These four departments account for 49.3% of the total. The number of hospitalized patients in the nephrology and orthopedic surgery departments was high immediately after the 2024 Noto Earthquake. We also describe new hospital-specific initiatives and recommendations to improve Kanazawa Medical University Hospital’s system while sharing another hospital experience.
Similar content being viewed by others
Introduction
Japan is one of the most earthquake-prone countries in the world, as it is located at a point on the Earth’s surface where four of the ≥ 10 tectonic plates covering the globe collide, causing earthquakes1. According to a report from the Asian Disaster Reduction Center, more than 20% of the world’s earthquakes with magnitudes ≥ 6 on the Richter scale have occurred in or around Japan2. On January 1, 2024, at 16:10 Japan Standard Time, a magnitude 7.6 earthquake struck 7 km northwest of Suzu, located on the Noto Peninsula in Ishikawa Prefecture, Japan1. A seismic intensity of 7 was observed in Monzen town in Wajima city and Shiga town in Hakui-gun (Fig. 1). The shaking and accompanying tsunami, landslide, airport closure, railway service suspension, and road division caused extensive damage to the Noto Peninsula, particularly to Wajima, Suzu, and Anamizu. The ground was lifted up, the coastline extended approximately 250 m seaward, and more than 100 fishing boats sank or were capsized; therefore, some air routes were temporarily cut off. As of February 3, 2024, Ishikawa Prefecture had reported 240 fatalities and 15 missing people, while nearly 1200 were injured across multiple prefectures.
The location of Ishikawa prefecture (yellow color), Japan. Noto Peninsula is located on prefectural North side that juts out from near the center of the Hokuriku region to the Sea of Japan toward the north. It is also the peninsula with the largest protruding area on the coastline of the Sea of Japan. The straight-line distance from Wajima Morning Market, where the fire occurred, to Kanazawa Medical University is 86 km. Red circle: A seismic intensity of 7 was observed in Monzen town in Wajima city, and Shiga-town in Hakui-gun. Purple circle (The number in brackets is the number of hospital beds at the time): Affected by the disaster core general hospitals (From above. Suzu General Hospital (163), Wajima Municipal Hospital (175), Ushitsu general hospital (100), Anamizu General Hospital (100), Togi hospital (60), Keiju Medical Center (426), Noto General Hospital (434). Sky blue circle: Kanazawa Medical University.
The Noto Peninsula region is comprised of 12 cities and towns north of Kahoku-gun, Ishikawa Prefecture, and 13 cities and towns in Himi, Toyama Prefecture, Japan. The Ishikawa area includes the cities of Nanao, Wajima, Suzu, Hakui, Kahoku, Tsubata, Uchinada, Shiga, Hodatsushimizu, Nakanoto, Anamizu, and Noto, covering an area of 2404 km2 (of which 2173 km2 is in Ishikawa Prefecture), and according to the Ishikawa Prefecture Regional Development Division, the population in Ishikawa Prefecture was 275,225 (as of the 2023 census). The proportion of the population (persons) ≤ 14 years old, 15–64 years old, and ≥ 65 years old was high, at 11.2%, 54.2%, and 34.6%, respectively. In 1990, the proportion of people aged ≥ 65 years was 17.2%, indicating that the proportion of this age group has almost doubled in the past 25 years. According to actual figures from the 2020 census, the aging rate (≥ 65 years) in Oku-Noto (2 cities and 2 towns: Wajima, Suzu, Anamizu, and Noto) was 48.9%.
The unfortunate situation in which the arrows were as follows: (1) A fire broke out near the Wajima morning market and spread to about 200 houses in the neighborhoods, exacerbated by many houses using propane gas. (2) Many people returned home during the New Year holidays. (3) There were days when helicopters could not fly because of fog blanketing in the Hokuriku region. (4) The area is a long and narrow peninsula and land transportation is the primary transportation method. (5) The communication infrastructure, including mobile phone networks, was disrupted, earthquake and tsunami meters were not functioning, and tsunami information was not accurately captured (delays in grasping damage information). (6) People are accustomed to earthquakes, and there has been a lack of earthquake damage estimation owing to the Noto earthquake swarm since December 20203,4.
In addition to the points mentioned above, the area was originally a medically depopulated region as follows: (1) There are many elderly residents. (2) Many disaster victims require nursing care and it is difficult to evacuate after a disaster. (3). Reluctance to leave the primary evacuation center with mental characteristics such as attachment, inability to leave because the home remains, and the local community. In other words, the Noto Peninsula is a depopulated area, where the vitality of the local community has declined due to a significant decline in the population, and where production functions and development of living environments are at a lower level relative to other regions. It was also anticipated that it would be difficult to secure a regional medical system in the event of a disaster.
The post-disaster period can be divided into four phases: hyperacute (approximately 48 h), acute (approximately 1 week), subacute (approximately 4 weeks), and chronic, each of which requires a different response. This study describes the initial medical response in the first month after a disaster. The present study is the first to report the number of hospitalized patients, percentage of inpatients in each department, and trends in the number of inpatients in the main medical departments as an initial response to identify medical characteristics in post-disaster support university hospitals closest to the disaster area (Fig. 1). We also describe new hospital-specific initiatives and recommendations to improve Kanazawa Medical University Hospital’s system while sharing another hospital experience.
Methods
This retrospective observational study was conducted in accordance with the principles of the Declaration of Helsinki. The Institutional Review Board of Kanazawa Medical University approved the study protocol (approval number: C081), and a waiver of informed consent was granted by the Research Ethics Committee of Kanazawa Medical University. In this study, 2022 Noto earthquake-related patients were defined as those who were seen because of direct damage from the earthquake or those who were not directly affected by the earthquake but became ill or had a pre-existing illness that worsened because of fatigue from evacuation or deterioration of the environment. As this could affect future applications of disaster condolence payments, decisions must be made based on careful interviews.
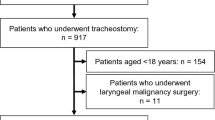
First, when recording medical records, tag names were standardized, for example, earthquake outpatient, earthquake hospitalization, difficulty returning home, and discharge coordination. Next, a disaster-related patient judgment meeting, consisting of members of the Medical Information Management Committee, Medical Information Department, and Hospital Management Committee, was held at the hospital to make decisions with impartiality, transparency, and factual equivalence. The items were classified into the following four categories: A (assign), earthquake-related; D (difficult), earthquake-related status difficult to judge; N (not authorized), not earthquake-related; P (possible), no tag note attached but may be earthquake-related based on a medical record check; and Q (questionable), tag note attached but may not be earthquake-related based on a medical record check (Supplemental Fig. 1).
The number of disaster-related patients was periodically adjusted according to the number of patients to be judged and those eligible for disaster-related treatment were approved. Finally, the number of hospitalized patients, percentage of inpatients in each department, and trends in the number of inpatients in the main medical departments were calculated from the management section. Furthermore, we examined the changes in the number of disaster-related inpatients in the main medical departments.
Results
Figure 2 shows the number of hospitalized disaster-related patients. Notably, up to 40 people were hospitalized each day. The disaster occurred in the evening, near night fall, making transportation difficult. On the third day after the disaster, it was cloudy and foggy, making air transport difficult and reducing the number of available transports. A total of 421 disaster-related patients were transported and hospitalized by day 31.
The percentage of disaster-related inpatients in each department was investigated. Fifty-two (14.4%) and 48 (13.3%) patients were admitted for orthopedic surgery and respiratory medicine, respectively. Forty (11.1%) and 38 (10.5%) patients were admitted to cardiology and nephrology departments, respectively. These four medical departments account for 49.3% of the total population. Thirty-four (9.4%), 28 (7.8%), 26 (7.2%), 21 (5.8%), 16 (4.4%), 15 (4.2%), 14 (3.9%), 13 (3.6%), 11 (3.0%), and 10 (2.8%) patients were admitted for gastroenterology, general and digestive surgery, geriatric medicine, emergency medicine, neurology, diabetic endocrinology, hematology and immunology, thoracic surgery, plastic and reconstructive surgery, obstetrics, and gynecology, respectively. These 14 medical departments account for 94.4% of the total population. The most frequently hospitalized departments were gastroenterology, general and digestive surgery, geriatric medicine, and emergency medicine (Fig. 3). Figure 4 shows the trends in the number of disaster-related inpatients in the four main medical departments. The number of patients in the nephrology and orthopedic surgery departments was high immediately after the disaster, whereas the number of patients in the respiratory medicine and cardiology departments was either constant or slightly higher immediately in the subacute phase after the disaster than in the acute phase.
Discussion
Establishment of a disaster response headquarters and team formation
A disaster response headquarters was established within the hospital on the first day of the 2022 Noto Earthquake. The staff members were summoned while checking their safety status. For example, from January 2 to 3, a total of 434 staff members (doctors, nurses, medical technology, and clerks) were mobilized to perform inpatient and outpatient services and triage of patients transported by ambulance. The Disaster Medical Assistance Team (DMAT) is a disaster relief force (January 2), and one team is dispatched to each team (January 4). Two nurses were dispatched for three nights and four days to provide disaster relief to the Ishikawa Prefecture Nursing Association. Furthermore, to strengthen support for emergency medical centers, two trainee doctors supported the weekday night shift for emergency treatment and day and night shifts on Saturdays, Sundays, and holidays. We also increased the number of nurses by 10 during the day and 15 at night to ensure that the emergency reception desk was staffed both day and night. We also increased the number of nighttime office staff members by one.
Meetings were held with the DMAT at Ishikawa Prefecture Response Headquarters. In addition, an emergency meeting of hospital department heads and liaison meetings were held. From the perspective of hospital functions, we were fortunate that although water was cut off in neighboring areas, Kanazawa Medical University Hospital had electricity, water, and other lifelines for the first four days, and elective surgeries and medical treatment were suspended to some extent during the New Year holiday period. Therefore, plenty of empty beds, spaces, and human resources were available. From an environmental perspective, we were fortunate that there was no heavy snowfall, and that the Shika Nuclear Power Plant was unharmed by the disaster. Consequently, 421 disaster-related patients were transported and hospitalized within the first month.
New approaches in the initial response to the 2024 Noto earthquake
We devised three points for the hospitals. First, we revised the guidelines regarding explanation and consent because there were cases in which family consent could not be obtained because of the 2022 Noto earthquake. Specifically, obtaining consent from patients and their families is necessary when providing medical treatment during a declared state of emergency. The patient or their family member stated that consent from these parties could be omitted only in cases where it was difficult or when there was no time available. However, in such cases, the head of the department, another doctor, and two or more doctors will each reconfirm that the situation is an emergency, and that there is no time available before emergency measures are taken (necessary medical actions). Priority was given to implementation. Second, tags were added to the medical records for later reference to public support, allowing for efficient discrimination between regular and disaster-related patients, recording, and follow-up. Finally, information was not available during the transportation of the patients from the disaster-affected core hospital. Therefore, we also established an information-sharing system between Kanazawa Medical University Hospital and other affected hospitals using Starlink in the event of a mobile network disconnection, named Kickstart to Manage Medical Accurate Sharing Information (KiMMAShi; meaning “please come” in the Kanazawa city dialect of Japanese) (Supplemental Fig. 2). To date, a number of information-sharing systems for disaster response teams, such as the Emergency Medical Information System (EMIS), have been established; however, when the disaster status transitions from the semi-acute stage to the middle and later stages, standardization is lacking5. Even in situations where the mobile network is cut off, hospitals are public institutions and a system is needed to ensure communication between hospitals and the government. After the 2022 Noto earthquake, mobile phones may become unusable because of the crowding of communication routes. Medical information is personal and requires a secure interhospital information-sharing system that can be used by all staff and shared with hospitals other than the initial hospital. This Starlink-based system has also been added to the disaster prevention and business continuity plan manuals. In other words, it will contribute to the digital transformation and strategic management of hospitals in the future through departments that manage, use, and research digital data, such as the Integrated Information Management Office, Integrated Information Management Department, Medical Information Department, Information Management Division, Medical Affairs Division, and in the bio-digital application research field.
Changes in the number of hospitalizations in each medical department and the relationship to earthquakes
The situation changed in our cohort, and the number of patients in the nephrology and orthopedic surgery departments was high immediately after the disaster. This indicates that trauma injuries were more frequent than other injuries immediately after the earthquake, and dialysis patients, who require huge amounts of water for treatment and have lost their way due to the water cut-off, are transported from damaged core general hospitals by disaster to Kanazawa Medical University Hospital (Fig. 1). MacKenzie et al. summarized the contents of several databases and searched for articles reporting primary injuries after significant earthquakes from 1970 to 2016. They concluded that most injuries requiring treatment after earthquakes (87%) were orthopedic in nature6. Gök et al. also reported 112 (42.2%) of 265 patients who were admitted to the emergency department and referred to the orthopedics and traumatology departments within the first week following the Kahramanmaraş earthquake7. In their study, 68 orthopedic patients underwent surgery, including 22 patients who underwent surgery on the first day after the earthquake, whereas 25 patients underwent surgery on the second day. In the present study, there were 82 surgeries in January compared with 59 in the same month last year at Kanazawa Medical University Hospital, with more orthopedic operations performed, especially for the first few days. Therefore, the surge in orthopedic hospitalized patients is consistent with previous reports8. If the earthquake occurred late at night, as in the Turkish earthquake, more cases of severe trauma such as chest trauma could have developed and caused even more extensive damage. In fact, over 50,000 people are known to have lost their lives, with over 100,000 injured in the Türkiye earthquake. The rate of thoracic trauma in this event has been reported to be 21.8%9. Therefore, the time of the disaster (daytime or nighttime) and severity of the awarded patients may be related to some extent.
Patients with chronic kidney disease are particularly vulnerable to earthquakes, as the term “renal disaster” suggests10. In fact, in the event of a major earthquake, hemodialysis patients face the risk of not being able to continue maintenance dialysis because of infrastructure disruption due to water outages. There were 344,640 dialysis patients with a mean age of 69.09 years old in Japan in 201911. As mentioned above, the rate of aging is high in the Noto Peninsula. The core general hospitals are affected by disasters (Fig. 1). Yoo insisted that long-term preparations should be made to handle renal disasters and patient safety logistics at the local and national government levels10.
The number of patients in the respiratory medicine and cardiology departments of Kanazawa Medical University Hospital was either constant or slightly higher in the subacute phase than in the acute phase, immediately after the disaster. This is assumed to be due to the exacerbations of chronic diseases and clusters of infectious diseases, such as influenza and coronaviruses, in temporary shelters. Systolic blood pressure was reported to be significantly elevated immediately after the Great East Japan Earthquake12. Stress from earthquakes, aftershocks, house damage, and obesity due to carbohydrate- and salt-rich foods in shelters are risk factors for hypertension and cardiovascular disease13. A previous study showed that the risk ratios in the interaction were significantly increased to 1.13, 1.17, and 1.28 for deaths due to stroke, pneumonia, and senility, respectively, in Miyagi Prefecture during the Great East Japan Earthquake that occurred in 201114. To make matters worse, the number of COVID-19 cases reported per fixed point in Ishikawa Prefecture was 5.42 from December 25 to 31, 8.44 from January 1 to 7, 10.48 from January 8 to 14, 14.33 from January 15 to 21, and 20.91, from January 22 to 28 according to a press release by the Ministry of Health, Labour and Welfare. Deterioration in toilet sanitation due to water cut-offs, nutritional status due to dietary deficiencies, depletion of oral medication, harsh winter months, inadequately ventilated shelter living conditions, and the background of group living with many older people also contributed to the high number of sick people4. For medical care to be effectively utilized in affected areas and countries, it is necessary to accurately predict climate change and to proactively build a medical care delivery system in the event of a disaster; that is, to set up details of mutual support between hospitals and an acceptance system and make this information public.
Limitation
Several limitations associated with the present study warrant mention, including its single-center, retrospective nature. In addition, there was a lack of data on the names of the diseases in each department. Despite these limitations, we received many patients with various conditions because the university hospital is closest to the disaster area. By clarifying the trends in the medical situation and what we have experienced as a hospital, we hope to apply this knowledge to future disaster medical care, as large-scale disasters such as earthquakes occur not only in Japan15,16,17 but around the world9,18,19.
Conclusion
We received many patients with various conditions because the university hospital was closest to the disaster area. By clarifying the trends in the medical situation and what we have experienced as a hospital, we would like to use this knowledge for future disaster medical care.
Data availability
All meteorological data necessary to support the results of this study, including daily changes in precipitation, are available on the website Wikipedia (https://en.wikipedia.org/wiki/Shika_Nuclear_Power_Plant), and information on the Noto Peninsula earthquake is available from Ishikawa Response Headquarters. (https://www.pref.ishikawa.lg.jp/saigai/documents/higaihou_78_0202_1400.pdf), and the Ishikawa Prefecture Regional Development Division (https://www.pref.ishikawa.lg.jp/shinkou/hantou/). and the Ministry of Health, Labour, and Welfare (https://www.mhlw.go.jp/content/001202247.pdf).
References
Conroy, G. Japan earthquakes: The science behind deadly tremors. Nature 625(228), 2024. https://doi.org/10.1038/d41586-024-00010-1 (2024).
Asian Disaster Reduction Center. Comparative study of disaster management of Japan and Kyrgyz Republic Kobe (Japan): Asian Disaster Reduction Center; 2012 from:http://www.adrc.asia/aboutus/vrdata/finalreport/2012A_KGZ_fr.pdf. (2012).
Kato, A. Implications of fault-valve behavior from immediate aftershocks following the 2023 Mj6.5 earthquake beneath the Noto Peninsula, central Japan. Geophys. Res. Lett. 51, e2023GL1064444. https://doi.org/10.1029/2023GL106444 (2024).
Moriwaki, Y., Morisaki, Y., Karashima, S. & Fujiu, M. Analysis of pharmaceutical demand in the region for chronic medicine users using national health insurance data: examination for disaster preparedness in Hakui city, Ishikawa Prefecture. Healthcare (Basel) 11, 3029. https://doi.org/10.3390/healthcare11233029 (2023).
Kondo, H. et al. Consideration of medical and public health coordination - experience from the 2016 Kumamoto Japan Earthquake. Prehosp. Disaster Med. 34, 149–154. https://doi.org/10.1017/S1049023X19000177 (2019).
MacKenzie, J. S., Banskota, B., Sirisreetreerux, N., Shafiq, B. & Hasenboehler, E. A. A review of the epidemiology and treatment of orthopaedic injuries after earthquakes in developing countries. World J. Emerg. Surg. 12, 9. https://doi.org/10.1186/s13017-017-0115-8 (2017).
Gök, M. & Melik, M. A. Clinical features and outcomes of orthopaedic injuries after the Kahramanmaraş earthquake: A retrospective study from a hospital located in the affected region. Scand. J. Trauma Resusc. Emerg. Med. 32, 10. https://doi.org/10.1186/s13049-024-01181-6 (2024).
Zhang, L. et al. Epidemiological analysis of trauma patients following the Lushan earthquake. PLoS ONE 9, e97416 (2014).
Ciflik, K. B. et al. Analysis of thoracic trauma patients transferred to Türkiye’s largest hospital after Kahramanmaraş earthquake. Ulus. Travma Acil. Cerrahi Derg. 30, 33–37. https://doi.org/10.14744/tjtes.2023.00748 (2024).
Yoo, K. D. et al. Disaster preparedness for earthquakes in hemodialysis units in Gyeongju and Pohang South Korea. Kidney Res. Clin. Pract. 38, 15–24. https://doi.org/10.23876/j.krcp.18.0058 (2019).
Hanafusa, N. et al. Annual dialysis data report 2019, JSDT Renal Data Registry. Ren. Replace Ther. 9, 47. https://doi.org/10.1186/s41100-023-00478-z (2023).
Satoh, M., Kikuya, M., Ohkubo, T. & Imai, Y. Acute and subacute effects of the Great East Japan Earthquake on home blood pressure values. Hypertension 58, e193–e194 (2011).
Kario, K. Disaster Hypertension—Its characteristics, mechanism, and management. Circ. J. 76, 553–562 (2012).
Fujimaki, T. et al. Major causes of death among older adults after the Great East Japan Earthquake: A retrospective study. Int. J. Environ. Res. Public Health 20, 5058. https://doi.org/10.3390/ijerph20065058 (2023).
Ozaki, A. et al. Breast cancer patient delay in Fukushima, Japan following the 2011 triple disaster: A long-term retrospective study. BMC Cancer 17, 423. https://doi.org/10.1186/s12885-017-3412-4 (2017).
Hashimoto, K. et al. Blood data trends of children in Fukushima after the Great East Japan Earthquake: Fukushima health management survey. Pediatr. Int. 65, e15656. https://doi.org/10.1111/ped.15656 (2023).
Nagae, M. & Nagano, E. Long-term effects of the Kumamoto earthquake on young children’s mental health. Healthcare (Basel) 11, 3036. https://doi.org/10.3390/healthcare11233036 (2023).
Akbari, K., Yari, A. & Ostadtaghizadeh, A. Nurses’ experiences of providing medical services during the Kermanshah earthquake in Iran: A qualitative study. BMC Emerg. Med. 24, 4. https://doi.org/10.1186/s12873-023-00920-9 (2024).
Okuyama, J. et al. Establishment of a post-disaster healthcare information booklet for the Turkey-Syrian earthquake, based on past disasters. Sci. Rep. 14, 1558. https://doi.org/10.1038/s41598-024-52121-4 (2024).
Acknowledgements
We would like to thank all participants, nurses, emergency department staff, and hospital administrative staff for their cooperation in this research. The following system companies provided free of charge assistance for the installation of Starlink, network construction, information-sharing services, and remote web conferencing systems: KDDI Corporation, KDDI Matomete Office Corporation, Fujitsu Japan Limited, Fujitsu F-Sus Limited, Japan Media Systems Corporation, Japan Total Systems Corporation, and JSS Corporation. We thank Dr. Satoru Mashiba of Kanazawa Medical University Himi Municipal Hospital. We were able to consult with KDDI Corporation via the Ishikawa Prefectural Government.
Author information
Authors and Affiliations
Contributions
H.U. contributed to the conception and design of the study. T.S. collected the data and performed data analyses. H.U. and T.S. wrote and critically revised the manuscript. H.S., Y. I., Y.K., and N.K. performed analyses and interpretations.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Uramoto, H., Shimasaki, T., Sasaki, H. et al. Initial response to the 2024 Noto earthquake by the university hospital closest to the disaster area. Sci Rep 14, 25013 (2024). https://doi.org/10.1038/s41598-024-75844-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-75844-w