Abstract
Treatment planning parameters in radiotherapy are key elements that dictate the success of treatment outcome. While some parameters are commonly evaluated irrespective of cancer type, others are site-dependent and strongly patient specific. Given the critical influence of planning parameters on personalized therapy, the aim of this study was to evaluate the correlations between the dosimetric indices (conformity, homogeneity and mismatch indices) related to tumor coverage and the patient-specific parameters which encompass parameters pertaining to organs at risk (widths and lengths of heart and ipsilateral lung included in treatment fields, mean/maximum doses to heart, ipsilateral lung, left anterior descending aorta and contralateral breast) and tumor volume. Forty breast cancer patients were divided into two groups according to tumor location: twenty with left-sided (group A) and twenty with right-sided breast cancer (group B). Conformal (3DCRT), intensity modulated (IMRT) and volumetric arc modulated (VMAT) radiotherapy techniques were used for plan creation. Moderate to strong correlations were found for ipsilateral lung parameters for both groups of patients regardless of the treatment technique. Moderate to strong correlations were found for heart parameters in group A patients, while no correlations were observed in group B. The mismatch index presented moderate to strong correlations with tumor volume for all treatment techniques (r = -0.861 3DCRT, r = -0.556 IMRT, r = -0.533 VMAT) particularly in group A. The evaluated correlations indicate the role of dosimetric indices in personalized treatment planning.
Similar content being viewed by others
Introduction
Based on global population incidence, breast cancer is among the first cancers leading to mortality and its occurrence is predicted to increase with over 7.00% in the future. Furthermore, female breast cancer has lately become the most commonly diagnosed malignancy (11.70%) thus slightly exceeding lung cancer incidence (11.40%)1. Radiotherapy plays a key role in the multidisciplinary approach of breast cancer. In order to increase survival, minimize tumor recurrence and reduce treatment-related toxicities, the focus of breast cancer radiotherapy must be balanced between tumor control and normal tissue protection. The most commonly used treatment techniques in breast cancer radiotherapy are still the linear accelerator-based ones: 3D conformal radiotherapy (3DCRT) and intensity modulated techniques (intensity modulated radiotherapy - IMRT and volumetric modulated arc radiotherapy - VMAT)2. Accurate treatment delivery is multifactorial dependent and involves a personalized approach, that besides the choice of treatment technique, of the immobilization board or the position on treatment couch, takes into account patient-related parameters (such as body mass index, comorbidities, tumor volume, the volume and position of the organs at risk (OARs) relative to the target) as well as the quality of dose distribution conformed to target volume geometry3.
Several factors have been reported in the literature to influence the final outcome of a treatment plan: the number of fields and field geometry4, tumor volume - depending on lymph nodes involvement5, irradiated healthy tissue areas4, overdosed and underdosed regions of tumor volume4, dosimetry of organs at risk4, the number of monitor units, and so on4. Given the association between the conformity and homogeneity indexes (CI and HI) and the quality of a treatment plan, their evaluation in regards to target and OARs dosimetry should be a key aspect of quality assurance. Also, the evaluation of mismatch index (MI) helps identify the differences between conformal and modulated intensity techniques regarding the percentage of prescribed dose outside the tumor volume.
In addition to target indices, for a more comprehensive assessment of the treatment plan, the evaluation of different OARs-related parameters should be taken into account in a quantitative manner. The importance of these parameters is given by the organs at risk located nearby the tumor volume, which in breast cancer irradiation are represented by the heart and ipsilateral lung. In view of the above, there are studies in the literature that evaluated heart and lung parameters depending on their inclusion in the irradiation field based on digitally reconstructed radiographs (DRR)6,7 or treatment field8,9,10. These parameters (maximum heart length - MHL, maximum heart distance - MHD, maximum ipsilateral lung length - MLL and maximum ipsilateral lung distance - MLD) showed an influence on dose and irradiated OAR volume, but also a correlation with a series of treatment-related sides effects, such as dermatitis11, incidence of poor cosmesis (modifications in breast volume, scars and skin changes)12 or fat necrosis13. A key factor in breast cancer irradiation is tumor location. Left- and right-sided breast cancer patients are exposed to different radiation-induced risks, owing to differences in the anatomical location of critical organs. Therefore, evaluation of dosimetric indicators for each patient category and their correlation with patient-related parameters can offer important information regarding optimization of breast cancer radiotherapy.
A variety of parameters were examined in the literature, which, in the current context, can be divided in patient-related parameters: (1) OAR (heart and ipsilateral lung volume inclusion in treatment field, heart and ipsilateral lung mean dose, mean and maximum dose of left anterior descending aorta - LAD and contralateral breast) and target volume-specific variables (planning target volume - PTV) and (2) dosimetric parameters (CI, HI and MI). A number of studies aimed to identify the influence of irradiation conditions (under free breathing or deep inspiration breath hold - DIBH) by looking for correlations between tumor volume and OARs dosimetry14 or by evaluating treatment planning-specific parameters (heart volume, lung volume, heart chest wall length, heart height, chest depth, central lung distance, heart chest wall distance, maximum heart depth, lung orthogonal distance) versus OARs dosimetric parameters (heart and LAD mean and maximum dose and contralateral and ipsilateral lung dose volumes)15 showing that the treatment outcome is better under DIBH technique due to reduced dose to OARs. Also, the influence of treated volume on OAR dosimetry was debated through correlations concluding that larger irradiated volumes increase heart and ipsilateral lung dosimetry (for OARs located in the proximity of the target)16.
However, the number of studies that evaluated the possible associations between patient-specific parameters (tumor volume, MHD, MHL, MLL, MLD and mean/maximum dose to OARs) and dosimetric indices (CI, HI, MI) that might influence the outcome of radiotherapy is scarce. Therefore, the purpose of this study was to assess through correlations analysis, the factors that lead to target coverage alterations for three radiotherapy techniques: (1) field-in-field tangential 3DCRT, (2) 6 fields IMRT and (3) 2 semiarcs VMAT. Anatomic distances included in the treatment field (MHD, MHL, MLL, MLD) were assessed given their known impact on setup errors3. Thus, another goal of this work was to determine the extent these parameters influence dosimetric indices (CI, HI and MI). This analysis was conducted, comparatively, in both left-sided and right-sided breast cancer patients.
Methods and materials
Patient selection and characteristics
Forty female patients with breast cancer (20 left-sided = Group A and 20 right-sided = Group B) were enrolled in this study. All patients were treated in our center between 2021 and 2023 using 6 and/or 15 MV photon beams from an Elekta Synergy Platform with Agility multi-leaf collimator (MLC). In addition to the original 3D conformal treatment, intensity modulated (IMRT) and volumetric modulated arc radiotherapy (VMAT) plans were also simulated on Monaco treatment planning system (TPS) version 6.1.2 for comparative purpose.
Patients were enrolled in this study regardless of age, tumor size or volume irradiated (presence/absence of positive lymph nodes). An exclusion criterion was the presence of tumor bed (boost) irradiation.
The study was carried out in accordance with relevant guidelines and regulations. The research was approved by the Bihor County Emergency Clinical Hospital ethics committee. Informed consent was waived because the research did not enroll patients for this retrospective study. This work analyzed the data of patients that have been treated as per the normal medical protocol without any change induced by this study.
Computed tomography simulation
Computed tomography (CT) simulation was performed on a Siemens Somatom Definition AS 20 in supine position on an inclined Quest breast board. Patients were positioned supine with hands raised above the head resting on hand and arm supports provided by the breast board. Also, the head was turned to the opposite side of the irradiated breast.
The scanning protocol for breast cancer was performed with 5 mm slices from the middle of the liver up to the mandible. Additionally, the isocenter was marked between the last two ribs.
Treatment planning
The prescribed dose for breast and supraclavicular lymph nodes (mean volume for group A of 115.82 cc and 84.96 cc for group B, respectively) irradiation was 50 Gy in 25 fractions. Target volume and organs at risk were contoured by each patient’s attending physician according to the RTOG consensus17. The OARs of interest were the heart, LAD, ipsilateral lung and contralateral breast.
3D conformal plans were calculated with Collapsed Cone Convolution (CCC) algorithm in Monaco 6.1.2 treatment planning system (TPS). Two opposite tangential fields (medial and lateral) were used for OARs sparing and field-in-field (FIF) technique for dose optimization in target volume. Lymph node irradiation was performed using 2 anterior and 1 posterior fields with FIF technique (Fig. 1).
The Monte Carlo algorithm was used for IMRT and VMAT plan calculations in Monaco 6.1.2 TPS. IMRT technique was performed using 6 fields for breast conformation and 2 anterior fields for lymph node irradiation (Fig. 1). VMAT technique was executed using 2 medial 45° (1 clockwise and 1 anti-clockwise) and 2 lateral 45° semiarcs with a region of avoidance (region without treatment field arrangements for lung sparing). Lymph node irradiation was performed using 1 anterior 45° semiarc. Cost functions were employed for plan optimization applied to organs at risk and target volume; for mean dose control: Dmean = 4 Gy for heart and Dmean = 20 Gy for ipsilateral lung, and for volume control: V25 < 10% for heart and V20 < 30% for ipsilateral lung18. Target volume was optimized obtaining a coverage > 95% of the prescribed dose and a maximum dose < 107% of the prescribed dose. Same dose constraints for organs at risk and dose optimization in target volume were used in conformal plan calculations.
Patient-related parameters: planning target volume
Target volume was defined by outlining the clinical target volume (CTV) for breast area and/or lymph node irradiation according to the RTOG consensus17. Planning target volume (PTV) delineation was achieved by adding 5 mm margins to the CTV in all directions (except the anterior - the volume was withdrawn 3 mm from the skin) to exclude the heart and ipsilateral lung from the contoured volume19.
The size of target volume differs from patient to patient, therefore, the contoured volume (tumor volume - TV) was considered a variable parameter influencing dosimetric indices.
Patient-related parameters: organs at risk
Patient’s characteristics and OAR geometrical indices are summarized in Table 1.
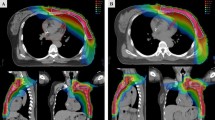
Organs at risk-related parameters were calculated using the medial tangent field for heart and ipsilateral lung. The evaluated parameters were the following: maximum heart distance (MHD), maximum heart length (MHL), maximum ipsilateral lung distance (MLD) and maximum ipsilateral lung length (MLL). Maximum heart and ipsilateral lung distances were calculated as the maximum width of heart and lung included in the tangent fields. Maximum heart and ipsilateral lung lengths were calculated as the maximum length of heart and lung, respectively, included in the radiation fields (Fig. 2)6,8.
In addition, mean dose (Dmean; heart, ipsilateral lung, LAD and contralateral breast), maximum dose (Dmax; heart, LAD and ipsilateral lung) and the dose to 1 cc of OAR volume (D1cc; heart) were also evaluated.
Dosimetric indices
Dosimetric indices were evaluated for both target dose distribution conformity and OARs statistics.
Dosimetric indices: planning target volume
Homogeneity index (HI) identifies the absorbed dose uniformity distribution regarding the target volume with an optimal value close to 120,21. The following formula was used for HI calculation:
where D5% represents the dose (Gy) received by 5% of the target and D95% is the dose (Gy) received by 95% of the target.
The conformity index (CI) characterizes the optimization of high-dose regions applied to the target volume with an optimal value close to 120,21. The following formula was used for CI calculation:
where Vtarget represents the volume (cc) of target and V95% is the volume (cc) of the 95% isodose of the prescribed dose (in our study, the isodose of 47.50 Gy).
The mismatch index (MI) was calculated to assess the percentage of prescribed dose outside the target volume22,23. The following formula was used for MI calculation:
where the V95%−target represents the volume outside the target, calculated by extracting the target volume from the volume of 95% isodose (V95%).
Dosimetric indices: organs at risk
For further consolidation of correlations between the parameters pertaining to organs at risk (MHD, MHL, MLD and MLL) and dosimetric indices (CI, HI and MI), heart dosimetry (V25, Dmean, Dmax, D1cc), ipsilateral lung (V20, Dmean), contralateral breast (Dmean, Dmax) and LAD (Dmean, Dmax) were evaluated. As all plans fulfil the corresponding constraints (heart V25 < 10%; ipsilateral lung V20 < 30%), the percentage of patients with dosimetry laying in the proximity of constraints was assessed, i.e. patients with 5% < V25 < 10% for heart and 25% < V20 < 30% for ipsilateral lung.
Statistical analysis
To identify factors that influence target conformity and homogeneity, correlations were calculated between dosimetric indices vs. patient-related parameters.
Furthermore, MI was used to identify the factors that influence the increase of reference isodose (95% of the prescribed dose) percentage laying outside target volume. The correlation between MI and both dosimetric indices (CI, HI) and OAR-specific parameters (MHD, MHL, MLD, MLL, Dmean/Dmax heart, ipsilateral lung, contralateral lung and LAD) was tested.
For right-sided breast cancer patients, the correlations between heart parameters (MHD and MHL) with CI, HI and MI were not possible due to the exclusion of the heart from the initial tangent fields.
Pearson correlation statistical test was used for evaluating the association between two variables. For moderate to strong correlation, results higher than r = ± 0.500 were taken into account (Pearson correlation coefficient: r > ± 0.500)24.
Student’s t-distribution test was employed to evaluate the statistical significance between differences among the 2 groups for CI, HI and MI. P-value threshold was set to 0.05 for statistical significance.
Results
Only for 3 patients in group B (right-sided breast cancer localization) the heart was present in treatment field projection. Therefore, heart parameters (MHD and MHL) were calculated only for 3 patients out of 20.
Dosimetric evaluation of heart for group A and B are presented in Fig. 3. Mean heart dose was higher than 4.00 Gy for all treatment techniques in group A (left-sided breast cancer patients): 4.99 ± 1.81 Gy for 3DCRT; 5.26 ± 1.15 Gy for IMRT and 5.09 ± 1.10 Gy for VMAT plans, and below 4.00 Gy for group B (right-sided breast cancer patients): 1.27 ± 0.66 Gy for 3DCRT; 2.66 ± 0.83 Gy for IMRT and 2.68 ± 0.59 Gy for VMAT plans. It is observed that Dmax and D1cc are below 30.00 Gy for group B and above 30.00 Gy for group A for all treatment techniques.
Dosimetric evaluations of the ipsilateral lung for groups A and B are presented in Fig. 4. Mean ipsilateral lung dose was smaller for 3DCRT plans in both groups (11.23 ± 3.10 Gy and 11.21 ± 3.12 Gy, p-value = 0.984) compared to IMRT (13.58 ± 2.26 Gy and 13.94 ± 1.41 Gy, p-value = 0.607) and VMAT plans (13.05 ± 2.61 Gy and 13.87 ± 1.46 Gy, p-value = 0.267).
LAD maximum and mean doses are represented in Fig. 5. Conformal plans presented higher mean (27.14 ± 10.91 Gy) and maximum doses (44.68 ± 12.18 Gy) than IMRT (Dmean 17.32 ± 5.55 Gy, Dmax 34.78 ± 8.10 Gy) and VMAT (Dmean 16.28 ± 6.29 Gy, Dmax 34.18 ± 8.70 Gy) in left-sided breast cancer patients (Group A). In group B, LAD was better spared with conformal plans (Dmean 1.00 ± 0.42 Gy, Dmax 1.25 ± 0.611 Gy) than with modulated techniques (IMRT: Dmean 2.19 ± 0.85 Gy, Dmax 3.48 ± 1.60 Gy; VMAT: Dmean 2.48 ± 0.99 Gy, Dmax 3.81 ± 2.20 Gy).
Figure 6 shows similar mean and maximum doses for the contralateral breast between the two groups for conformal plans (Dmean p-value = 0.468, Dmax p-value = 0.414), while modulated plans presented statistically significant differences regarding mean and maximum doses (IMRT: Dmean p-value < 0.001, Dmax p-value = 0.001; VMAT: Dmean p-value = 0.019, Dmax p-value = 0.014).
CI and HI are summarized in Table 2. Significant differences (p-value < 0.05) between the 2 groups were observed for CI in modulated treatment techniques and for HI only in IMRT plans.
The percentage of healthy tissue receiving 95% of the prescribed dose is represented in Fig. 7, through the mean MI for each group and for all treatment techniques. P-values are also indicated for statistical significance of differences between the 2 groups (p-value = 0.249 for 3DCRT, p-value = 0.904 for IMRT and p-value = 0.692 for VMAT).
Pearson correlation results (and p-values) are summarized in Table 3. Tumor volume positively correlated with CI in VMAT plans (r = 0.506, p-value = 0.022) for group A and in IMRT plans (r = 0.502, p-value = 0.023) for group B, while no correlation with HI was observed for conformal and modulated plans for either group. In addition, a moderate/strong negative correlation was found between tumor volume and MI for all treatment techniques (r = -0.861, p-value < 0.001 for 3DCRT, r = -0.556, p-value = 0.010 for IMRT and r = -0.533, p-value = 0.015 for VMAT) in group A and for 3DCRT plans (r = -0.532, p-value = 0.015) in group B. Positive correlations between TV and dosimetric indices indicates an increase in dosimetric parameters with an increase in TV.
Contralateral breast dosimetry correlated with HI in conformal plans (Dmeanr = 0.516, p-value = 0.019) and in modulated plans (Dmax: IMRT r = 0.506, p-value = 0.022; VMAT r = 0.505, p-value = 0.022) for group A patients (left-sided breast cancer).
MHL showed a moderate correlation only with the MI for conformal plans (r = -0.522, p-value = 0.003) for group A, while for group B the associations were not evaluated for heart parameters.
Mean heart dose correlated positively with CI (r = 0.616, p-value = 0.003) and with HI (r = 0.599, p-value = 0.003) for group A in conformal plans. However, mean ipsilateral lung dose moderately correlated with CI only for modulated plans (group A: r = 0.511, p-value = 0.020 IMRT and r = 0.531, p-value = 0.015 VMAT; group B: r = 0.576, p-value = 0.011 VMAT), while the association with HI was observed for VMAT plans in group A (r = 0.687, p-value < 0.001), and with 3DCRT (r = 0.573, p-value = 0.008) and IMRT (r = 0.515, p-value = 0.019) in group B.
In group A, all evaluated parameters correlated with MI for at least one treatment technique. In conformal plans, Pearson correlation coefficient was higher than 0.500 for tumor volume (r = -0.861, p-value < 0.001), heart parameters (r = -0.620, p-value = 0.003 MHD, r = -0.522, p-value = 0.017 MHL) and ipsilateral lung parameters (r = -0.660, p-value = 0.001 MLD, r = -0.582, p-value = 0.007 MLL). The r coefficient presented correlations in intensity modulated plans for tumor volume (r = -0.556, p-value = 0.010) and MLL (r = -0.594, p-value = 0.005), while in volumetric modulated plans the coefficient was higher than 0.500 for all evaluated parameters, except for heart (r = -0.195, p-value = 0.409 MHD and r = -0.347, p-value = 0.132 MHL).
Mismatch index correlations in group B were observed only in conformal plans for tumor volume (r = -0.532, p-value = 0.015) and MLL (r = -0.549, p-value = 0.011) parameters.
Moreover, mismatch index correlated negatively with conformity and homogeneity indices for both groups. A moderate correlation was observed in modulated plans in group A for CI (r = -0.543, p-value = 0.013 IMRT and r = -0.546, p-value = 0.012 VMAT) and for HI (r = -0.555, p-value = 0.010). Other moderate to strong correlations were found for conformal and intensity modulated plans for CI (r = -0.608, p-value = 0.004 3DCRT and r = -0.656, p-value = 0.001 IMRT) and in modulated plans for HI (r = -0.542, p-value = 0.013 IMRT and r = -0.571, p-value = 0.008 VMAT) for group B.
Figure 8 shows mean V20 for ipsilateral lung (for whole group A and B) and the percentage of patients exceeding dose constraints, i.e. V20 > 25%. A major difference between the 2 groups was observed for VMAT plans with mean V20 = 20.67% in left-sided patients (group A) and 24.82% in right-sided patients (group B).
Mean V25 for heart was evaluated only for left-sided breast cancer patients due to heart inclusion in tangent fields (the heart was included in tangent fields for only 3 right-sided patients so the evaluation of V25 was not conducted). Mean values represented for whole group A and B and the percentage of patients exceeding dose constraints, i.e. V25 > 5% are presented in Fig. 9. Modulated plans presented smaller values for V25 heart (3.74% IMRT and 3.47% VMAT) than conformal plans (5.65%), with more patients exceeding 5% of V25 for the latter technique.
Discussion
Plan personalization is a key concept in modern radiotherapy. Plan optimization according to the individual patient’s tumor characteristics improves treatment efficacy and limits radiation-induced side effects25. In view of this, plan personalization should take into account dosimetric indices pertaining to both target and OARs as an important indicators of treatment outcome. Conformity and homogeneity indices are two main indicators that reflect tumor coverage and dose uniformity within the tumor volume and were assessed in the current study in the context of breast cancer radiotherapy using three different treatment techniques.
Mean values of conformity and homogeneity indices were reported in the literature after analyzing the dosimetry of tumor volume and organs at risk of several treatment techniques26. Liu et al. evaluated right-sided breast cancer patients by using two methods of VMAT technique (continuous partial arc and non-continuous partial arc), IMRT and hybrid 3DCRT/IMRT obtaining CI values of 0.74 for VMAT, 0.64 for IMRT and 0.68 for 3DCRT techniques. The conclusion suggested by Liu et al. regarding the high conformity index obtained by VMAT was that the technique can increase dose modulation in treatment fields which in turn increases the quality of tumor coverage26. Another study evaluated treatment plans according to the CI for 100 plans comparing three treatment techniques: 3DCRT (CI = 0.46), FIF (CI = 0.59) and IMRT (CI = 0.72)27. The study, among others28,29, suggested that IMRT offers better tumor volume coverage than FIF plans and also that FIF has better coverage and fewer hot spots than 3DCRT. As shown by our study, the mean CI value obtained for right-sided patients was 0.78 for 3DCRT, while higher values were reached for IMRT (0.90) and VMAT (0.92), being consistent with the studies employing intensity-modulated techniques26. For left-sided breast cancer patients, the CI values reported by our study were 0.80 for 3DCRT, 0.88 for IMRT and 0.89 for VMAT, showing better conformality compared to the plan characteristics described by Takabi et al. (CI = 0.46 for 3DCRT and CI = 0.72 for IMRT). Their study asserted that changing the treatment technique also changes the dose distribution in target volume27.
The homogeneity index is a variable that analyzes the uniformity of dose distribution in tumor volume. Petrova et al. evaluated this index for 58 patients with breast cancer using two methods of conformational technique (3DCRT with segments and 3DCRT with standard tangent fields) and obtained HI = 1.08 with segments and 1.09 without segments, showing a significant statistical difference between the two groups (p-value < 0.001)30. Wang et al. evaluated the IMRT technique for 96 left-sided breast cancer patients reporting a mean homogeneity index of 1.095. The finding of the studies showed that although the index would be a good indicator of treatment plan evaluation8, the interpretation of the results should not be done from section to section, but based on the gradient and dose distribution in the tumor volume30. However, it was concluded that hot spot reduction by using segments30 or by modulating the intensity8, leads to an homogeneous dose distribution. In our study, the mean value of homogeneity index for 3DCRT was 1.10 for left-sided patients and 1.09 for right-sided patients, slightly higher than in modulated intensity plans (1.09 left-sided patients and 1.07 right-sided patients for IMRT; 1.08 left-sided patients and 1.07 right-sided patients for VMAT) although the FIF technique was used to control the hot spots.
Due to lack of information regarding 3D dose distribution outside target volume, the mismatch index was created to report the influence of a reference isodose (specifically the 95% of the prescribed dose) on healthy tissue23. Schoepen et al. evaluated the mismatch index for 51 patients divided into 4 groups depending on tumor stage and position (right or left-sided), using four treatment techniques (tangent fields with wedges - W-TF, tangent IMRT, multi-fields IMRT and VMAT) in three positions: supine, prone dive and prone crawl23. The results of MI in supine position were 46.43% W-TF, 18.94% tangent IMRT, 11.33% multi-fields IMRT and 8.00% VMAT. Also, Mulliez et al. analyzed three treatment techniques (W-TF, tangent IMRT and multi-fields IMRT) in supine and prone position suggesting higher values than Schoepen’s study for modulated techniques in supine position: 46.80% W-TF, 34.70% tangent IMRT and 28.50% multi-field IMRT. The conclusions drawn by the studies concerning mismatch index escalation in conformal techniques were related to the concave shape of the breast22 and the longer path lengths through healthy tissue in lateral tangent and axillary/shoulder regions for lymph node irradiation22,23. Mean values of mismatch index in our study were comparable to those in the literature, reporting higher values for 3DCRT (34.50% right-sided patients and 38.50% left-sided patients) and lower for modulated intensity plans for both groups of patients (11.59% right-sided patients and 11.35% left-sided patients for IMRT; 11.49% right-sided patients and 10.79% left-sided patients for VMAT plans).
Owing to the differences of CI, HI and MI among treatment techniques, our study evaluated the correlations between indices and tumor volume and OAR-related parameters for both groups of patients.
For right sided-breast cancer patients, dose normalization on heart and ipsilateral lung has been presented in the literature under different dosimetric values. Liu et al. evaluated patients with right-sided breast cancer using four radiotherapy techniques (continuous partial arc, non-continuous partial arc, hybrid 3DCRT/IMRT and IMRT) reporting mean heart doses of 1.73 Gy, 3.15 Gy, 1.47 Gy and 4.35 Gy for each of the above-mentioned technique, respectively26. A study conducted by Czeremszynska et al. evaluated 10 patients with right-sided breast cancer comparing three treatment techniques (3DCRT, IMRT and VMAT) showing mean heart doses of 0.85 Gy (3DCRT), 1.30 Gy (IMRT) and 1.70 Gy (VMAT)31. In our study, the mean heart dose for right-sided patients was under 3.00 Gy for all evaluated treatment techniques. In addition, the literature reported values between 7.60 and 10.14 Gy in conformal plans, between 8.50 and 12.76 Gy in IMRT and 8.32–9.00 Gy in VMAT plans26,31 for ipsilateral lung dosimetry. Our study presented comparative mean values of 11.21 Gy for 3DCRT, 13.94 Gy for IMRT and 13.87 Gy for VMAT plans. These different dosimetric values between studies reinforce the need for treatment personalization, for dose reduction to OARs on an individual basis.
Furthermore, LAD has become an organ at risk of interest in breast cancer treatment, therefore, it is often evaluated in right-sided breast treatments. Gocer et al. selected 40 patients with right and left-sided breast cancer treated with wedged tangent fields in order to evaluate radiotherapy-induced cardiotoxicity32. The study presented comparable values for mean LAD dose (9.76 Gy) and maximum dose (11.19 Gy) for right-sided patients. In our study, the mean LAD values were 1.00 Gy for 3DCRT, 2.19 Gy for IMRT and 2.48 Gy for VMAT. Maximum dose was 1.25 Gy in conformal plans and 3.48 Gy and 3.81 Gy for IMRT and VMAT, respectively.
Lower doses were also observed on contralateral breast in conformal plans (Dmean = 0.90 Gy, p-value 3DCRT vs. IMRT/VMAT < 0.01 and Dmax = 7.22 Gy, p-value 3DCRT vs. IMRT/VMAT < 0.01) compared to modulated plans (IMRT Dmean = 1.55 Gy and Dmax = 11.47 Gy; VMAT Dmean = 2.21 Gy and Dmax = 13.49 Gy), a trend that was observed by other studies31,33,34. This fact is mainly due to the scattered radiation from the linac head or within the treated breast, as the amount of radiation on contralateral breast increases with the decrease of its distance from the treated breast. Furthermore, this dose difference highlights one of the most important disadvantage of modulated techniques, namely the difficulty of controlling low-dose volumes, mainly because modulated plans were created with multiple fields (contributing to the cumulative dose), while conformal plans were created using two opposite tangent fields31,35,36. Moreover, MU delivered in modulated techniques are higher than conformal plans (IMRT: 471.20 ± 44.40 MU and VMAT: 672.40 ± 126.70 MU vs. 3DCRT: 395.50 ± 84.20 MU, p-value < 0.01) due to modulation complexity and small MLC segments, which increase the scattered radiation, leading to higher low-dose volumes31.
Owing to the limited number of reports in the literature regarding the factors influencing tumor volume coverage, this study included correlations between dosimetric indices and patient-specific variables depending on treatment field geometry (MHD, MHL, MLD, MLL, Dmean heart, Dmean lung) and tumor volume. Our study identified several factors that influence the conformity index, one of them being the tumor volume (r = 0.502, p-value = 0.023 IMRT). No correlation between tumor volume and homogeneity index was found for any of the evaluated treatment techniques.
However, correlations were observed between lung parameters and dosimetric indices (CI and HI). The MLL parameter showed correlation with CI for IMRT (r = 0.626, p-value = 0.003) and with HI for 3DCRT (r = 0.675, p-value < 0.001) and VMAT (r = 0.511, p-value = 0.020). Ipsilateral lung dosimetry was evaluated using mean dose (Dmean < 20 Gy) and volumetric parameters (V20 < 30%). Although the mean dose is below the limit imposed by the attending physician for all treatment techniques, the mean values of V20 were: 21.30% (6.19 − 29.30%) for 3DCRT, 25.36% (16.54 − 29.67%) for IMRT and 24.82% (16.43 − 28.25%) for VMAT. Values higher than 25% reaching 30% of irradiated volume (being an interval close to dose limit) were extracted for the V20 parameter. The results showed better lung sparing in 3DCRT plans, with 9 patients (45%) exceeding the interval in group B, while 14 patients (70%) for IMRT and 12 patients (60%) for VMAT plans were close to dose limits. The large number of patients presented with difficulties in lung sparing indicates the need for correlation with MLL parameter, as OARs dose reduction is detrimental to target volume coverage8,37.
In addition, the correlation between MLD and homogeneity index (r = 0.599, p-value = 0.005 IMRT) could be justified by the increased values of irradiated lung volume and the attempt of the calculation algorithm to reduce the dose, by penalizing the tumor volume uniformity dose distribution8,37.
The evaluation of mean and maximum LAD dose indicated the lack of correlations between these parameters and dosimetric indices (CI, HI and MI), suggesting no influence on target coverage and homogeneity due to its anatomical position and distance relative to the target. Likewise, no correlations were observed between the contralateral breast and dosimetric indices.
As stated by Wang et al., CI and HI mean values of intensity modulated plans were affected not only by gantry angle and MLC movement, but also by the OAR dose limitation and spatial distance. The increase in number of OARs and dose constraints would complicate planning optimization. To improve the efficiency of planning design by increasing the conformity index when increasing the subfields or using different gantry angles (factors not specific to patients), low-dose exposure volume of OARs increases as well37.
The mismatch index was evaluated to identify the influence of 95% isodose of the prescribed dose (47.50 Gy) outside the irradiated volume on organs at risk. A moderate correlation was observed between tumor volume and MI (r = -0.532, p-value = 0.015), suggesting an increase in the percentage of dose outside the target, especially in 3DCRT plans, which can be confirmed by the geometry used for planning (tangent fields) and dose accumulation in the patient’s posterior region (Fig. 7). The fact that there were no correlations with intensity modulated plans may suggest the algorithm’s ability to optimize the dose distribution taking into account the increase in target coverage. Also, the percentage escalation might influence OARs dosimetry, a fact that can be asserted by the correlation between MI and MLL parameter (r = -0.549, p-value = 0.011) in conformal plans.
In addition, the percentage of 47.50 Gy outside target volume might also influence tumor volume coverage, which is indicated by correlations between MI and CI (r = -0.608, p-value = 0.004 3DCRT, r = -0.656, p-value = 0.001 IMRT) and HI (r = -0.542, p-value = 0.013 IMRT, r = -0.571, p-value = 0.008 VMAT).
Mean heart and ipsilateral lung dose were assessed for left-sided breast cancer patients. A number of studies in the literature compared different treatment techniques regarding heart and ipsilateral lung dosimetry. Czeremszynska et al. evaluated 17 left-sided breast cancer patients and found mean heart doses of 3.60 Gy for 3DCRT, 3.70 Gy for IMRT and 3.80 Gy for VMAT techniques31. Cardiac dosimetry (mean dose) reported by Das Majumbar et al. for 35 left-sided breast cancer patients for three treatment techniques evaluated were 11.89 Gy for 3DCRT, 14.25 Gy for IMRT and 12.35 Gy for VMAT plans10. In our study, mean heart dose for left-sided breast cancer patients was approximately 5.00 Gy for all evaluated treatment techniques. Regarding the lung, studies reported values of 18.25 Gy for 3DCRT, 13.66 Gy for IMRT and 12.35 Gy for VMAT plans for mean ipsilateral lung dose10,37. Our study presented comparative mean values of 11.23 Gy for 3DCRT, 13.58 Gy for IMRT and 13.94 Gy for VMAT techniques.
Furthermore, both mean and maximum LAD doses were observed to be higher in conformal plans (Dmean = 27.14 Gy and Dmax = 44.68 Gy) compared to those from intensity modulated plans (IMRT Dmean = 17.32 Gy and Dmax = 34.78 Gy; VMAT Dmean = 16.28 Gy and Dmax = 34.18 Gy), outcome that was also observed by Czeremszynska et al. (3DCRT Dmax = 35.70 Gy, IMRT Dmax = 31.00 Gy and VMAT Dmax = 28.90 Gy)31 and by Garg et al. (3DCRT Dmax = 48.68 Gy, IMRT Dmax = 48.22 Gy, p-value = 0.66)38. This is owing to the inclusion of LAD in treatment fields, being located in the anterior part of the heart which receives a higher dose than the whole heart in breast cancer irradiation32.
The mean LAD dose reported in our study is comparable to other studies that used modulated plans (IMRT 11.04 Gy and VMAT 11.09 Gy)23, forward and inverse IMRT techniques (9.50 Gy forward IMRT and 17.17 Gy inverse IMRT)32 or tangent fields techniques (24.02 Gy)39.
Dosimetry of the contralateral breast showed a reduction in mean and maximum dose in conformal plans (Dmean = 0.99 Gy and Dmax = 6.07 Gy) compared to IMRT plans (Dmean = 3.58 Gy and Dmax = 18.35 Gy) and VMAT (Dmean = 3.56 Gy and Dmax = 19.44 Gy), which is explained by the chosen field geometry (tangent fields for 3DCRT and multi-field arrangement for IMRT/VMAT plans)35,36. Other studies reported mean doses of 1.43–2.39 Gy and maximum doses of 41.13–43.55 Gy for IMRT plans39.
The differences between treatment techniques regarding OARs dosimetry should raise careful consideration towards personalized plans while evaluating factors that suggest possible penalties on tumor volume or organs at risk.
Wang et al. evaluated 4 factors (tumor volume, apex of the heart distance to the field - MHD, lung maximum width - CLD and cardiothoracic ratio - CTR) for 96 left-sided patients using the IMRT technique8. The results expressed through linear regression analysis showed that the tumor volume, MHD and CTR appeared to be the factors influencing the conformity index, while the only evaluated parameter that influenced the homogeneity index was the tumor volume.
The correlation between CI and TV of our study was also observed in group A patients using volumetric modulation plans (r = 0.506, p-value = 0.022), but no correlation was observed with the homogeneity index for the evaluated treatment techniques.
Correlations with heart parameters were evaluated for this group of patients, being an organ at risk in the vicinity of the tumor volume. A correlation was observed between MHD and conformity index for the 3DCRT technique, a result implied by the 50% of the evaluated patients which had V25 values close to the maximum limit (10%) imposed by the attending physician. For the other techniques, V25 was 35% in IMRT and 25% in VMAT, without correlations with the conformity or homogeneity index. Other moderate correlations were observed with mean heart dose for both CI (r = 0.616, p-value = 0.003) and HI (r = 0.599, p-value = 0.003) in conformal technique due to large variations of mean doses: 1.31 – 8.56 Gy.
Ipsilateral lung parameters showed higher number of correlations with CI and HI than those for the heart. Plans with intensity modulation showed correlations between MLD and both indices (CI: r = 0.608, p-value = 0.004 IMRT and r = 0.641, p-value = 0.002 VMAT; HI: r = 0.517, p-value = 0.019 IMRT and r = 0.623, p-value = 0.003 VMAT) and between MLL and CI in VMAT plans (r = 0.576, p-value = 0.007). These correlations could be justified through the addition of V20 constraint on ipsilateral lung, which complicates tumor volume optimization8, although a strong correlation was observed in conformal plans with MLL and HI (r = 0.735, p-value < 0.001). The percentage of patients who presented values for V20 greater than 25% was 30% (6/20) for 3DCRT, 40% (8/20) for IMRT and 25% (5/20) for VMAT.
Correlations were also observed between mean ipsilateral lung dose and CI (for IMRT and VMAT) and HI (for VMAT) being in accordance with weight escalation in planning optimization and OARs dose accumulation8,37,40. Furthermore, LAD showed correlations with HI in conformal plans (r = 0.552, p-value = 0.039), suggesting that OAR dose reduction leads to coverage/homogeneity alteration of the target volume.
Significant positive correlations were observed between contralateral breast dosimetry and HI. Mean dose correlated in 3DCRT plans (r = 0.516, p-value = 0.019), and maximum dose in IMRT/VMAT plans (IMRT r = 0.506, p-value = 0.022; VMAT r = 0.505, p-value = 0.022), thus influencing the homogeneity of the tumor volume. In addition, a significant negative correlation (r = -0.657, p-value = 0.001) was observed in the 3DCRT plans between MI and the maximum dose of the contralateral breast, indicating that the 95% isodose outside the tumor volume influences the dose to the contralateral breast.
The mismatch index correlated strongly (r = -0.861, p-value < 0.001) with tumor volume in 3DCRT plans, due to the increased percentage of 47.50 Gy located outside the tumor volume (38.50%, range 16.21 − 54.44%). Correlations with tumor volume were also observed in intensity modulated techniques (r = -0.556, p-value = 0.010 IMRT; r = -0.533, p-value = 0.015 VMAT), although the 95% isodose percentages were lower than in conformal plans (11.35%, range 1.97 − 28.84% for IMRT; 10.79%, range 0.57 − 23.46% for VMAT).
Moderate to strong correlations between MI and MHD (r = -0.620, p-value = 0.003), MHL (r = -0.522, p-value = 0.017), MLD (r = -0.660, p-value = 0.001) and MLL (r = -0.582, p-value = 0.007) were observed for conformal plans, suggesting heart and lung sparing. Furthermore, moderate negative correlations were observed in VMAT plans for MLD (r = -0.507, p-value = 0.021), MLL (r = -0.554, p-value = 0.011), Dmean heart (r = -0.526, p-value = 0.016) and Dmean lung (r = -0.559, p-value = 0.010) possibly due to the impact of modulation on plan outcome. Also, owing to this reason, conformity and homogeneity indices correlated with mismatch index for modulated techniques, impacting on coverage and dose distribution uniformity.
When comparing the left-sided vs. right-sided breast cancer groups, the mean doses of OARs, especially to the heart, showed lower values in right-sided breast patients (Fig. 3) due to the heart’s anatomical position. This difference was also observed by Lamprecht et al. who evaluated 15 patients with left-sided and 15 with right-sided breast cancer using 3DCRT technique and two other VMAT techniques (reduced arc and reduced arc flattening filter free - reduced arc FFF). The values presented by the study for left-sided patients were 1.57 Gy 3DCRT, 1.19 Gy reduced arc VMAT and 1.20 Gy reduced arc FFF VMAT, and for right-sided patients the values were 0.51 Gy 3DCRT, 0.61 Gy reduced arc VMAT and 0.71 Gy reduced arc FFF VMAT41.
Mean doses to the ipsilateral lung appeared to be similar for both groups of patients between treatment techniques. However, it was ascertained that modulated techniques presented higher values on mean lung dose (left-sided patients: 13.58 Gy IMRT and 13.05 Gy VMAT; right-sided patients: 13.94 Gy IMRT and 13.87 Gy VMAT) compared to 3D plans (left-sided patients: 11.23 Gy; right-sided patients: 11.21 Gy), due to the increased number of fields used in treatment planning. In 3D technique 2 tangent fields were employed while 6 fields were used for IMRT and 2 semi-arcs with region of avoidance for VMAT plans. This conclusion was also drawn by Shanei et al. who evaluated 30 left-sided breast cancer patients comparing tangent 3DCRT with 6 and 9 IMRT fields (6 F IMRT and 9 F IMRT), showing an average dose of 6.80 Gy for 3DCRT, 9.28 Gy for 6 F IMRT and 10.30 Gy for 9 F IMRT42.
A major difference between the 2 groups was observed in the V20 values for ipsilateral lung dose in VMAT plans, with a mean value of 20.67% in left-sided (group A) and 24.82% in right-sided breast cancer patients (group B). The reduction in ipsilateral lung volume receiving 20 Gy in group A could be due to more dose constraints (extra cost-functions) used to protect the heart in vicinity of the tumor volume43.
Regarding the influencing factors of tumor volume coverage, correlations were found between tumor volume and CI for intensity modulated techniques (left-sided patients: r = 0.506, p-value = 0.022 VMAT; right-sided patients: r = 0.502, p-value = 0.023 IMRT), therefore the size of tumor volume might influence its coverage, and also OARs dosimetry43,44.
Moreover, most of the correlations with homogeneity index were observed for ipsilateral lung parameters, both for conformal and modulated intensity plans. These correlations reinforce the need for treatment plan personalization because the greater the coverage and uniformity of tumor volume (through HI and CI), the greater the dose delivered to OARs. A study conducted by Zhang et al. compared intensity modulated techniques in order to reduce dose to OARs and increase the homogeneity index by taking into account several factors: tumor complexity and shape, monitor unit reduction and organs at risk sparing. As reported in the study, mean heart dose was lower for VMAT (5.20 Gy) than for IMRT plans (6.00 Gy). Furthermore, virtual blocks were used for target homogeneity improvement without increasing the low-dose volumes (V5 = 20.90% VMAT and V5 = 27.90% IMRT). At the same time, the number of monitor units decreased in VMAT compared to IMRT plans (611 MU VMAT vs. 893 MU IMRT, p-value < 0.001)45.
Another difference between left-sided and right-sided breast cancer patients was observed in terms of contralateral breast dosimetry and HI. Left-sided patients (group A) showed moderate correlations for all treatment techniques evaluated, while right-sided breast cancer patients indicated no correlations. This result can be associated with the increased number of dose constraints (complexity of the treatment plan) applied to the treatment plan optimization (thus reducing the coverage and homogenization of tumor volume)43.
On the same note, the number of mismatch index correlations was higher for left-sided than for right-sided breast cancer patients. Correlations were observed between tumor volume and organs at risk parameters (MHD, MHL, MLD, MLL, Dmean heart and lung) for both conformal and intensity modulated techniques in left-sided breast patients, while patients with right-sided breast cancer did not show correlations in intensity modulated techniques for any evaluated parameter. The lack of correlations with the mismatch index could be due to reduced number of dose constraints (the heart was not included in treatment fields, therefore no need for constraints), thus not affecting the healthy tissue in order to decrease the percentage dose outside tumor volume.
Figure 10 is a summary of our findings together with literature-based results, to emphasize the need for breast cancer treatment personalization based on the presented correlations42,43,44.
Summary of findings regarding the impact of dosimetric indices on target coverage and OARs dosimetry (MI = mismatch index, CI = conformity index, HI = homogeneity index, TV = tumor volume, MHD = maximum heart distance, MHL = maximum heart length, MLD = maximum ipsilateral lung distance, MLL = maximum ipsilateral lung length, Dmean = mean dose, 3DCRT = 3D conformal radiotherapy, IMRT = intensity modulated radiotherapy, VMAT = volumetric modulated arc radiotherapy)42,43,44.
The findings of our study suggest a course of action to personalize treatment in patients with unfavorable geometry or in situations when dosimetric indices show suboptimal values. A simple step would be the adjustment of gantry angle to protect organs at risk while maintaining target coverage to 95% of the prescribed dose. Furthermore, an increased number of fields could lead to an improved target homogeneity and conformality; to limit doses to OARs, more complex techniques can be employed, such as the use of virtual blocks to increase tumor homogeneity and decrease low-dose volumes to OARs. Increasing cost functions to OARs and limiting monitor units to avoid complicated treatment plans should also be considered37,45.
Our study has certain limitations. One shortcoming is the limited number of patients evaluated for each group, which should be taken into account when transposing the results. However, similar other studies with small number of patients were reported in the literature which, nevertheless, presented valuable information regarding treatment techniques comparison from a dosimetric perspective10,31. Another limitation would be the lack of heart parameters in right-sided breast cancer patients to serve for comparative purpose. Nevertheless, correlations were evaluated for mean heart dose and the comparison of ipsilateral lung parameters between treatment techniques was achieved. Furthermore, while patients were treated with conformal 3DCRT, the plans derived from the intensity modulated techniques were calculated for simulation only.
Conclusions
Most of the moderate/strong correlations in our study were observed in ipsilateral lung parameters for all treatment techniques evaluated, regardless of tumor location, given that both groups of patients (left- and right-sided breast cancer) presented the associations.
The evaluated correlations between dosimetric indices and parameters pertaining to organs at risk suggest the involvement of dose constraints, treatment plan adaptation and field geometry modulation for a more personalized treatment plan. Different dosimetric indices and patient-specific parameters should be considered in left- and right-sided breast cancer patients and the analysis of these parameters should be conducted and interpreted on an individual basis.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Bray, F. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424 (2018).
Balaji, K., Subramanian, B., Yadav, P., Radha, C. A. & Ramasubramanian, V. Radiation therapy for breast cancer: Literature review. Med. Dosim. 41, 253–257 (2016).
Costin, I. C. & Marcu, L. G. Factors impacting on patient setup analysis and errors management during breast cancer radiotherapy. Crit. Rev. Oncol. /Hematol. 178, 103798 (2022).
Zhang, R., Heins, D., Sanders, M., Guo, B. & Hogstrom, K. Evaluation of a mixed beam therapy for postmastectomy breast cancer patients: Bolus electron conformal therapy combined with intensity modulated photon radiotherapy and volumetric modulated photon arc therapy. Med. Phys. 45(7), 2912–2924 (2018).
Nobnop, W., Phakoetsuk, P., Chitapanarux, I., Tippanya, D. & Khamchompoo, D. Dosimetric comparison of TomoDirect, helical tomotherapy, and volumetric modulated arc therapy for postmastectomy treatment. J. App l Clin. Med. Phys. 21(9), 155–162 (2020).
Ueda, Y., Gerber, N. K. & Das, I. J. Model-based cardiac dose estimation in radiation treatment of left breast cancer. Br. J. Radiol. 91, 20180287 (2018).
Eskandari, A. et al. Evaluation of the heart and lung dosimetric parameters in deep inspiration breath hold using 3D slicer. Radiat. Oncol. J. 38(1), 68–76 (2020).
Wang, Y. et al. Individualized estimates of intensity-modulated radiotherapy plans after breast conservation surgery for left-sided breast cancer. World J. Surg. Oncol. 21, 59 (2023).
Fadavi, P. et al. The relationship between lung and heart two-dimensional parameters and three-dimensional dose-volume data in adjuvant radiotherapy for breast cancer. Med. J. Islam Repub. Iran 36, 16 (2022).
Das Majumdar, S. K. et al. A dosimetric study comparing 3D-CRT vs. IMRT vs. VMAT in left-sided breast cancer patients after mastectomy at a tertiary care centre in eastern India. Cureus. 14(3), 23568 (2022).
Xie, Y. et al. Predicting acute radiation dermatitis in breast cancer: A prospective cohort study. BMC Cancer 23, 537 (2023).
Feizi, N. et al. Predictors of poor cosmesis in breast cancer patients treated with adjuvant whole breast radiation therapy plus high-dose-rate interstitial brachytherapy boost after breast conservation surgery. J. Contemp. Brachytherapy. 14(5), 429–437 (2022).
Rahimy, E. et al. Increased number of beam angles is associated with higher cardiac dose in adjuvant fixed gantry intensity-modulated radiation therapy of left-sided breast cancer. Int. J. Radiat. Oncol. Bio Phys.https://doi.org/10.1016/j.ijrobp.2017.06.2451 (2017).
Xin, X. et al. Retrospective study on left-sided breast radiotherapy: dosimetric results and correlation with physical factors for free breathing and breath hold irradiation techniques. Technol. Cancer Res. Treat. 20, 1–8 (2021).
Ferdinand, S. et al. Dosimetric analysis of deep inspiratory breath-hold technique (DIBH) in left-sided breast cancer radiotherapy and evaluation of pre-treatment predictors of cardiac doses for guiding patient selection for DIBH. Tech. Innov. Patient Support Radiat. Oncol. 17, 25–31 (2021).
Alaimo, R. et al. Breast volume is a predictor of higher heart dose in whole-breast supine free-breathing volumetric-modulated arc therapy planning. Curr. Oncol. 30, 10530–10538 (2023).
Radiation Therapy Oncology Group. Breast cancer atlas for radiation therapy planning: Consensus definitions. https://www.srobf.cz/downloads/cilove-objemy/breastcanceratlas.pdf
Bisello, S. et al. Dose–volume constraints fOr oRganS at risk in Radiotherapy (CORSAIR): An all-in-one. Multicenter–Multidiscip. Pract. Summ. Curr. Oncol. 29, 7021–7050 (2022).
Radiation Therapy Oncology Group 1005. A phase III trial of accelerated whole breast irradiation with hypofractionation plus concurrent boost versus standard whole breast irradiation plus sequential boost for early-stage breast cancer. (2011).
The International Commission on Radiation Units and Measurements (ICRU). Prescribing, recording and reporting photon beam therapy (supplement to ICRU report 50), report 62.
ICRU & The International Commission on Radiation Units and Measurements. Prescribing, recording and reporting photon beam IMRT. J. ICRU 10(1), Report83 (2010).
Mulliez, T. et al. Whole breast radiotherapy in prone and supine position: Is there a place for multi-beam IMRT? Radiat. Oncol. 8, 151 (2013).
Schoepen, M. et al. Four irradiation and three positioning techniques for whole-breast radiotherapy: Is sophisticated always better? J. Appl. Clin. Med. Phys. 23, e13720 (2022).
Stewart, A. Basic Statistics and Epidemiology a Practical Guide 4th edn (CRC Press Taylor & Francis Group, 2016).
Costin, I. C. & Marcu, L. G. Evaluation of Heart substructures as a function of dose and radiation-induced toxicities in left-sided breast cancer radiotherapy. Eur. J. Cancer Care 1294250, (2024).
Liu, Y. C., Chang, H. M., Lin, H. H., Lu, C. C. & Lai, L. H. Dosimetric comparison of intensity-modulated radiotherapy, volumetric modulated arc therapy and hybrid three-dimensional conformal radiotherapy/intensity-modulated radiotherapy techniques for right breast cancer. J. Clin. Med. 9, 3884 (2020).
Takabi, F. S., Broomand, M. A., Nickfarjam, A., Asadi, A. & Namiranian, N. Determination and comparison of dosimetric parameters of three-dimensional conformal radiotherapy, field in field, and intensitymodulated radiotherapy techniques in radiotherapy of breast conserving patients. J. Can. Res. Ther. 19, 624–632 (2023).
Dean, J. et al. Tangential intensity modulated radiation therapy (IMRT) to the intact breast. J. Med. Radiat. Sci. 63, 217–223 (2016).
Kim, S. & Choi, Y. Dosimetric advantages of the field-in-field plan compared with the tangential wedged beams plan for whole-breast irradiation. Prog Med. Phys. 25, 199 (2015).
Petrova, D., Smickovska, S. & Lazarevska, E. Conformity index and Homogeneity Index of the postoperative whole breast radiotherapy. Open. Access. Maced J. Med. Sci. 5(6), 736–739 (2017).
Czeremszynska, B. et al. Dosimetric comparison of three-dimensional conformal radiation therapy, intensity-modulated radiation therapy, and volumetric-modulated arc therapy for free-breathing whole-breast irradiation: a planning study. Indian J. Cancer 60, 258–265 (2023).
Gocer, G. P. S. & Ozer, E. E. Effect of radiotherapy on coronary arteries and heart in breast-conserving surgery: A dosimetric analysis. Radiat. Oncol. 54(1), 128–134 (2020).
Kundrat, P. et al. Minimum breast distance largely explains individual variability in doses to contralateral breast from breast-cancer radiotherapy. Radiother. Oncol. (2018).
Johansen, S., Cozzi, L. & Olsen, D. R. A planning comparison of dose patterns in organs at risk and predicted risk for radiation induced malignancy in the contralateral breast following radiation therapy of primary breast using conventional, IMRT and volumetric modulated arc treatment techniques. Acta Oncol. 48(4), 495–503 (2009).
Zhang, L. et al. Estimating cardiac substructures exposure from diverse radiotherapy techniques in treating left sided breast cancer. Medicine 94(18), e847 (2015).
Mehta, A. et al. Dosimetric parameters of heart and left ventricle – comparison of 3D CRT and IMRT in left cancer breast. Int. J. Med. Res. Rev. 7(6), 468–475 (2019).
Karpf, D., Sakka, M., Metzger, M. & Grabenbauer, G. G. Left breast irradiation with tangential intensity modulated radiotherapy (t-IMRT) versus tangential volumetric modulated arc therapy (t-VMAT): Trade-offs between secondary cancer induction risk and optimal target coverage. Radiat. Oncol. 14(1), 156 (2019).
Garg, A. & Kumar, P. Dosimetric comparison of the heart and left anterior descending artery in patients with left breast cancer treated with three-dimensional conformal and intensity-modulated radiotherapy. Cureus 14(1), e21108 (2022).
Azharuddin, S. et al. Comparison of dosimetric parameters and clinical outcomes in inversely planned intensity modulated radiotherapy (imrt) and field-in-field forward planned imrt for the treatment of breast cancer. Cureus 14(7), e26692 (2022).
Quan, E. M. et al. A Comprehensive comparison of IMRT and VMAT Plan quality for prostate cancer treatment. Int. J. Radiation Oncol. Biol. Phys. 83(4), 1169–1178 (2012).
Lamprecht, B. et al. Comparison of whole breast dosimetry techniques – from 3DCRT to VMAT and the impact on heart and surrounding tissues. J. Med. Rad Sci. 69, 98–107 (2022).
Shanei, A., Amouheidari, A., Abedi, I., Kazemzadeh, A. & Jaafari, A. Radiobiological comparison of 3D conformal and intensity modulated radiation therapy in the treatment of left-sided breast cancer. Int. J. Rad Res. 18(2), 315–322 (2020).
Xie, Y., Bourgeois, D., Guo, B. & Zhang, R. Comparison of conventional and advanced radiotherapy techniques for left-sided breast cancer after breast conserving surgery. Med. Dosim. 45(4), 9–16 (2020).
Xu, H. & Hatcher, G. Treatment planning study of volumetric modulated arc therapy and three dimensional field-in-field techniques for left chest-wall cancers with regional lymph nodes. Rep. Prac Oncol. Radiother. 21, 517–524 (2016).
Zhang, Y. et al. A dosimetric and radiobiological evaluation of VMAT following mastectomy for patients with left-sided breast cancer. Radiat. Oncol. 16, 171 (2021).
Acknowledgement
The APC was funded by the University of Oradea.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by ICC, original draft preparation was written by ICC and LGM, review and editing were performed by ICC and LGM. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Patient consent was waived due to the same reason as below by the Bihor County Emergency Clinical Hospital ethics committee.
Institutional review board statement
Ethical review and approval were waived by the Bihor County Emergency Clinical Hospital ethics committee for the research because it did not enroll patients for the said study. This work analysed the data of patients that have been treated as per the normal medical protocol without any change induced by this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Costin, IC., Marcu, L.G. Correlations between patient-specific parameters and dosimetric indices for personalized breast cancer radiotherapy. Sci Rep 14, 26141 (2024). https://doi.org/10.1038/s41598-024-75858-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-75858-4