Abstract
This study aims to observe the clinical efficacy and safety of rigid gas permeable corneal contact lenses (RGP-CLs) wearing after femtosecond laser-assisted minimally invasive lamellar keratoplasty (FL-MILK) in progressive and advanced keratoconus eyes. Twenty-five patients (27 eyes) fitted with RGP-CLs after FL-MILK were enrolled, and 22 grading-matched keratoconus patients (23 eyes) as a control group. Corneal morphological data, diopter, best corrected vision, corneal endothelium, non-invasive tear film rupture time (NIBUT), corneal perception and comfort questionnaire were analysed before and after wearing RGP-CLs. In the FL-MILK group, the flat K, steep K and Kmax of the corneal anterior surface were decreased by 3.05D, 3.48D and 7.17D respectively after surgery (P = 0.011, 0.004 and 0.007). The central corneal thickness increased by 175.29 μm (P < 0.001). The basic curve of RGP-CLs after surgery was about 0.23 mm flatter than that before surgery (P = 0.013). There was no statistical difference in the best corrected vision and the comfort of wearing RGP-CLs before and after FL-MILK (P = 0.923, 0.391). Compared with the control group, there was no significant difference in vision improvement by RGP-CLs (P = 0.669). During the follow-up, the comfort of wearing RGP-CLs in the two groups was good, and no obvious adverse events were observed. This study showed MILK significantly increases corneal thickness and flattens corneal curvature, achieving good RGP-CLs corrected vision.
Similar content being viewed by others
Introduction
Keratoconus (KC), typically occurring in adolescents1, is a bilateral progressive ectatic condition characterized by central corneal thinning and protrusion2,3,4,5,6. KC can lead to high irregular astigmatism, myopia or even blindness6,7,8. Rigid gas permeable corneal lenses (RGP-CLs) have been reported to be the best nonoperative way to significantly correct irregular astigmatism9,10, but it cannot control the development of KC11. How to control the development of KC and correct irregular astigmatism effectively remains very challenging.
Surgery is the main treatment to slow or halt the progression of KC. Corneal collagen cross-linking surgery can strengthen the cornea12,13, but cannot increase the thickness of the cornea. KC is the one of the leading indications for corneal transplantation in China and the United States14,15. For the patients with advanced KC, penetrating keratoplasty (PKP) or lamellar keratoplasty (LKP) was generally recommended6,16. Nevertheless, the large incisions and complications related to sutures and postoperative immune rejection are disadvantages of PKP and LKP17. In order to reduce the complications of conventional PKP and LKP, the author team developed a new type of surgery named femtosecond laser-assisted minimally invasive lamellar keratoplasty (FL-MILK) for progressive and advanced KC patients18,19. Without removing any corneal tissue, a 200–250 μm thick corneal stroma graft was implanted into the host corneal stroma through a 2.3 mm microincision, and the corneal thickness was increased to 550–650 μm after surgery with no sutures applied. The corneal nerve recovered well postoperatively, and the development of KC was well controlled20. At the same time, suture-related complications were avoided, and the recovery period after surgery was greatly shortened. For patients with poor results of cross-linking surgery, it can also play a better control effect.
After FL-MILK, the corneal anterior curvature can be reduced to a certain extent19. For patients with relatively flat preoperative curvature, the spectacles can effectively correct vision after the operation. However, for patients with significant preoperative and postoperative irregular astigmatism, RGP-CLs are required instead of spectacles for their poor correction effect, image magnification and aniseikonia9,21. However, the corneal morphology of these patients after FL-MILK has changed, whether RGP-CLs can be successfully fitted, and how about the efficacy and safety. This study prospectively observed the effect of RGP-CLs fitting, visual rehabilitation and the stability of epithelium after RGPCL wear, which is the focus and innovation of this paper.
Subjects and methods
Study design and subjects
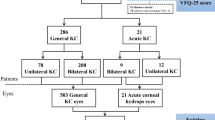
This is a prospective nonrandomized cohort study. According to 2-sample t-test, the effect size > 0.9, significance level (α) < 0.05, and statistical power (1 − β) > 0.8 were selected for sample size calculation, and obtain a minimum sample size of 21 cases. Eventually, 47 subjects, including 25 patients (27 eyes) with FL-MILK, and 22 patients (23 eyes) without operation as the control group, were included. The sample size was determined from G*Power22.
From June 2018 to December 2020, 25 patients (27 eyes) with progressive and advanced KC were included after receiving FL-MILK (FL-MILK group) in the Eye Hospital of Shandong First Medical University. 22 patients (23 eyes) with KC wearing RGP-CLs matched for age, sex and keratoconus grading were enrolled as the control group (KC group). Inclusion criteria: ① Diagnosed with progressive and advanced KC of Stage II-IV according to Belin ABCD grading preoperatively and postoperatively11,23,24,25; ② KC patients all received trial RGP-CLs fitting before FL-MILK, and the corrected vision with RGP-CLs ≤ 0.3logMAR; ③ At least 3 months postoperatively in the FL-MILK group; ④ Endothelial cell density ≥ 1000/mm2; ⑤ Expect to obtain better corrected vision; ⑥ At least 18 years old. There was no significant difference between the FL-MILK group and the control group in terms of age, sex and keratoconus grading.
Exclusion criteria: ① Accompanied with other eye diseases, such as severe dry eye, conjunctivitis, blepharitis, glaucoma, etc.; ② Accompanied with systemic diseases, such as diabetes, rheumatism, acute and chronic sinusitis, etc.; ③ History of contact lens solution allergy; ④ Women with breastfeeding infants, women who are pregnant or planning to get pregnant.
All participants signed an informed consent form. This study was carried out in strict accordance with the tenets of the Declaration of Helsinki and was approved by the Eye Hospital of Shandong First Medical University Research Ethics Committee (SDSYKYY20180511).
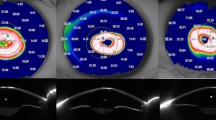
RGP-CLs materials and lens fitting
Corneal Rose-K lenses are used as treatment lenses. The lens diameter is 8.5 ~ 10.4 mm, and the material is Boston XO. The oxygen permeability coefficient (DK value) is 100 × 10− 11(cm2/s) (mlO2/mL mmHg). A diagnostic CL-fitting method was used to finalize the customized CL parameters. The fitting procedure was established in accordance with the guidelines in the Rose K fitting manual. The average K value is selected as the basic curve of the first trial lens. Following a 20-minute adaptation period, both the dynamic and static fit were evaluated. In dynamic fit, the lens was centered adequately on the cornea with good post-blink movement and stability on different gaze movements. In static fit, the central fitting was immediately evaluated with the lens on the center of the cornea after fluorescein staining, and the conical apex of cornea should be slightly in touch with the lens. After the basic curve parameters were adjusted to achieve the best central fitting, the peripheral curve was evaluated and the edge width was adjusted to 0.6–0.8 mm. The trial was conducted repeatedly until an acceptable dynamic and static fit was attained. Upon determining the optimal lens fit, the final power was calculated by performing a spherical over-refraction on the trial lens. The customized lens was observed under the slit lamp microscope to reach a satisfactory fitting: no obvious deviation, good center fitting, and 1.0 ~ 1.5 mm movement (Fig. 1). The fitting relationship between a lens and the corneal surface was examined by panoramic OCT (Tomy Inc., Japan) to show the distribution of the tear film under the lens in different parts. (Fig. 2)
Corneal healing status at 3 months after FL-MILK and RGP-CL lenses fitting. A shows that the cornea is transparent without sutures, the corneal interlaminar graft can be seen, and the healing is good. B shows that the RGP lens position is in the middle, the corneal conical apex is slightly contacted the lens, with good fitting and the peripheral edge about 0.6 mm. FL-MILK femtosecond laser-assisted minimally invasive lamellar keratoplasty, RGP-CLs rigid gas permeable corneal contact lenses.
Main outcome measures
Corneal topography data of the participants before and after FL-MILK and RGP-CLs wearing (Pentacam anterior segment analysis system, Wavelight Company, Germany) was collected, including flat K value, steep K value, Kmax value, central corneal thickness (CCT), thickness at the thinnest point, etc.
All patients were fit with RGP-CLs more than 3 months postoperatively in FL-MILK group, and the average wearing time was 8.4 ± 5.3 months after operation. The patients in the two groups were followed up regularly every 3 months after wearing RGP-CLs for 1 week, 1 month. The average follow-up period after wearing RGP-CLs was 2.0 ± 0.3 years. The complications such as corneal epithelial staining, infiltration, edema and acute red eye were observed under a slit lamp microscope. Uncorrected visual acuity (UCVA), best spectacle-corrected visual acuity (BSCVA) and RGP-CL-corrected visual acuity (RGPCLVA) were recorded with logMAR (logarithm of the minimum angle of resolution) acuity. Corneal topography and corneal endothelium were examined (SP-8000, Konan Company, Japan) by the same skilled medical technician every six months. Each data was measured 3 times per eye, and the best quality was selected as the measurement result.
Likert scale was used to evaluate the comfort of RGP-CLs wearing by filling in the subjective self-evaluation form (where 1 means very poor, 2 means poor, 3 means average, 4 means good, 5 means very good)26. Four aspects relating to comfort were included: wearing satisfaction, the clarity of visual acuity, dry foreign body sensation, and wearing comfort27.
Statistical analysis
SPSS 22.0 software (IBM Corp., Armonk, NY, USA) was used. All the continuous variables in this study, expressed in means ± standard deviations (SD), were in accordance with normal distribution by the Klomogorov Smirnow test. The comparison of visual acuity, diopter, corneal morphology and other data between the two groups was analyzed using an independent sample t-test. The data of visual acuity, diopter, corneal morphology and corneal safety before and after the operation were compared, using the paired t-test. One-way ANOVA was used for comparing these parameters differences in different times before and after RGP-CL within the group. Bonferroni’s adjustment for multiple comparisons was applied to all post hoc pairwise comparisons. Chi-square test was used for categorical variables. All p values were 2-sided and considered statistically significant when less than 0.05.
Results
Basic data
The FL-MILK group included 21 males (23 eyes) and 4 females (4 eyes), with an age of 23.0 ± 4.3 years. The values of Flat K, steep K and Kmax of the corneal anterior surface were decreased by 3.05D, 3.48D and 7.17D respectively after FL-MILK (P = 0.011, 0.004 and 0.007), with average postoperatively 8.4 ± 5.3 months (initial wearing of RGP-CLs). The thickness of the central cornea and the thinnest point increased about 175.29 μm and 114.51 μm (P both < 0.001). (See Table 1; Fig. 3)
Corneal topography before and after FL-MILK. Figure 3A and B, represent the left eye before and 10 months after FL-MILK, flat K, steep K and Kmax were flat by 1.5D, 0.6D and 8.6D respectively, central corneal thickness increased by 232 μm. FL-MILK femtosecond laser-assisted minimally invasive lamellar keratoplasty.
In the FL-MILK group, the average time of initially wearing RGP-CLs was 8.4 ± 5.3 months after operation. The average spherical diopter and cylindrical diopter of the participants were − 7.22 ± 6.37D and − 4.44 ± 2.84D respectively, and the average CCT was 616.39 ± 48.71 μm before RGP-CLs wear. There was no significant difference between the FL-MILK group and the control group in the curvature of the anterior corneal surface, including flat K, steep K and Kmax (P = 0.842, 0.350 and 0.397). No significant difference was found between spherical and cylindrical diopters (P = 0.937, 0.190). (See Table 2)
Comparison of uncorrected visual acuity (UCVA) and corrected vision before and after RGP-CLs wear between the two groups
When wearing RGP-CL continuously for 1 month, no significant difference was found in UCVA and BSCVA between the two groups (P = 0.143, 0.906). In the FL-MILK group, the average RGP-CL-corrected visual acuity was 0.15 ± 0.10logMAR, and 96.3% (26/27) of the patients achieved 0.3logMAR or above, compared with 29.6% (8/27) of BSCVA, it significantly improved the best corrected vision of patients. UCVA-BSCVA and UCVA-RGPCLVA had no significant difference between the two groups (P = 0.118, 0.669). (See Table 3)
Comparison of corneal morphological parameters and diopter before and after wearing RGP-CLs in the FL-MILK group
At the end of follow-up period (average time of wearing RGP-CLs was 2.0 ± 0.3 years), presented data from two follow-up periods, the flat K, steep K and Kmax had no significant changes compared with those before RGP-CLs wear (P all > 0.05). The sphere diopter, cylinder diopter and corneal thickness had no significant difference before and after wearing RGP-CLs (P all > 0.05). (See Table 4)
Comparison of base curve, UCVA and wear comfort of the trial RGP-CLs before FL-MILK and customized RGP-CLs after FL-MILK
In order to evaluate the patient’s best corrected vision, KC patients all received trial RGP-CLs fitting before FL-MILK. For the patients with RGP-CLs corrected vision ≤ 0.3logMAR, FL-MILK can be considered. The RGP-CLs data of 25 cases (27 eyes) before and after FL-MILK were compared. It was found that the customized base curve after FL-MILK was 0.23 mm flatter than the trial RGP-CLs before FL-MILK (6.37 ± 0.38 Vs. 6.60 ± 0.32, P = 0.013). There was no significant difference in the best corrected vision and wear comfort before and after keratoplasty (0.16 ± 0.07 Vs. 0.16 ± 0.11, P = 0.923; 3.82 ± 0.60 Vs. 4.09 ± 0.83, P = 0.391).
Corneal safety after wearing RGP-CLs in the two groups
During the follow-up period, one patient (one eye) in the FL-MILK group was found to have corneal epithelial staining after wearing RGP-CLs for 1 year, which was caused by obvious lens scratches and protein precipitation. After stopping wearing it for 1 day, it recovered and no recurrence was observed after replacing it with the new lens. One case (1 eye) with KC progression was noticed in the control group, for whom the original RGP-CLs was not well-fitted and surgical treatment was recommended. No other complications were found in all wearers, and no corneal graft rejection occurred in the FL-MILK group. The corneal endothelial cell density, non-invasive tear film rupture time (NIBUT) and corneal perception postoperatively at different wearing time points had no significant changes compared with those before wearing RGP-CLs in the FL-MILK group (P > 0.05). (See Table 5)
Comfort evaluation of wearing RGP-CLs in the two groups
In the FL-MILK group, 50% of patients wore RGP-CLs as a routine correction method preoperatively, so these patients can receive RGP-CLs again quickly postoperatively, and eight hours of daily routine wear can be achieved within 1 week. For the patients who wore RGP-CLs for the first time, the comfort was slightly poor within the first week, and the main manifestations were dry foreign-body sensation and vision fluctuation. As time went on, the discomfort gradually decreased. By the end of the first month, all patients felt comfortable wearing lens, and could accept routine worn for 8 h a day. The patients’ comfort Likert score of wearing satisfaction, vision clarity, dry foreign-body sensation and end-of-day comfort were all 4 points and above, and there was no significant difference between the two groups (P > 0.05). (See Fig. 4)
Comfort Likert score of wearing RGP-CLs in the two groups. The analysis shows that there is no statistical difference in wearing satisfaction, vision clarity, dry foreign-body sensation and the end-of-day comfort between the FL-MILK group and the KC group (P > 0.05). RGP-CLs rigid gas permeable corneal contact lenses, FL-MILK femtosecond laser-assisted minimally invasive lamellar keratoplasty, KC keratoconus.
Discussion
FL-MILK can control the progression of KC, moreover, good effects can still be achieved for the patients who experienced failed treatment of cross-linking surgery (CXL)18,20. FL-MILK is mainly performed to increase the corneal thickness and flatten the corneal curvature of the anterior surface28. However, corneal irregularity in some severe KC patients is still obvious postoperatively, and postoperative vision correction is a challenging problem to solve29,30. RGP-CLs can correct irregular astigmatism caused by corneal protrusion more effectively31. Its main advantage lies in forming a tear pool of uneven thickness between the lens and the cornea, which neutralizes the ocular aberration associated with KC distension, thus providing better corrected vision9,32. However, whether RGP-CLs can achieve a good and acceptable fitting after FL-MILK, whether the FL-MILK operation will affect the corrected vision and wearing comfort of RGP-CLs postoperatively, whether RGP-CLs increase the hypoxia of corneal endothelium and the abrasion of corneal epithelial cells, need to be explored. Therefore, this study conducted a prospective observation for the first time to answer these urgent clinical questions that need to be addressed.
This study found that good fitting of RGP-CLs and satisfactory best corrected vision can be achieved after FL-MILK. The average best corrected vision of RGP-CLs can reach 0.15 ± 0.10logMAR. 96.3% (26/27) of the patients achieved visual acuity of 0.3logMAR or above, which significantly improved the best corrected visual acuity compared with 29.6% (8/27) of the spectacles, so as to improve the quality of patient’s life33. In addition, the trial RGP-CL on the patients preoperatively with corrected vision of 0.3logMAR or above were given FL-MILK. It is gratifying that there is no significant difference between the customized RGP-CLs corrected vision after FL-MILK and the best corrected vision of trial RGP-CLs preoperatively (P = 0.923). There was no significant difference in UCVA-BSCVA and UCVA-RGPCLVA between the two groups (P > 0.05), which reflected that the use of spectacles or RGP-CLs correction in the FL-MILK group can reach the same extent that with the same correction method in the control group. Therefore, FL-MILK does not affect the patients’ best corrected vision.
The thickness of the cornea was increased uniformly after FL-MILK, and the CCT and the thickness of the thinnest point increased by 175.29 μm and 114.51 μm, respectively. The increase of CCT after FL-MILK is comparable to the increase of corneal thickness after deep anterior lamellar keratoplasty34. In this study, the flat K, steep K and K-max of the corneal anterior surface got flatter by 3.05D, 3.48D and 7.17D respectively compared with those before FL-MILK, which is consistent with the results before and after deep lamellar keratoplasty35. Therefore, this study supports that the treatment effect of FL-MILK on KC thinning and protrusion is very significant. In this study, the RGP-CL parameters that were fitted before and after FL-MILK were compared, and the base curve of customized lens after FL-MILK was about 0.23 mm flatter than that before FL-MILK, which facilitates a better match between the lens and the cornea. It is suggested that the base curve of RGP-CLs after FL-MILK should be 0.2–0.3 mm flatter than that preoperatively. The fitting of RGP-CLs after FL-MILK was basically the same as that of the KC group, for there is no suture and no big incision healing between the graft and the implantation bed36,37.Therefore, the selection of lenses was relatively free, both small-diameter and large-diameter Rose-k series lenses can be considered38. In addition, the success rate of RGP-CLs fitting was significantly higher than that of penetrating keratoplasty or lamellar keratoplasty39. In this study, the best RGP-CLs corrected vision and the wearing comfort of RGP-CLs were not significantly different before and after FL-MILK, which indicates that wound healing after FL-MILK is good and the operation has no effect on the wearing comfort of RGP-CLs and the corrected visual acuity. This finding is similar to the result of Bowman layer transplantation (BLT)40, which can enable patients to continuously wear RGP-CLs and obtain good corrected vision. Moreover, FL-MILK showed greater advantages in increasing corneal thickness and played a better role in delaying the progression of KC and improving corneal mechanical properties41.
During the 2.0 ± 0.3 years observation period of wearing RGP-CLs, in the FL-MILK group, only one patient with corneal epithelial staining was observed at the time of wearing RGP-CLs for 1 year, which was found to be caused by obvious lens scratches and protein precipitation. It was recovered after stopping wearing, and there was no recurrence after replacing with new lens. Compared with the control group, wearing RGP-CLs did not increase the risk of corneal epithelial abrasion. This team previous research found that the anterior corneal plexus was preserved, though there would be local corneal nerve transection in the peripheral corneal stroma layer, but the central corneal sensitivity returned to the preoperative level 12 months after FL-MILK18. If the RGP-CL is well-fitted, it has no obvious adverse effect on corneal epithelium. This study showed that in the process of wearing RGP-CLs for a long time, the corneal endothelial cell density had no significant change compared with that before wearing, which was consistent with the research results of Dogan C et al.42. NIBUT and Corneal perception had no significant changes compared with those before wearing. Therefore, this study supports that wearing RGP-CLs to correct vision is safe and has no obvious adverse reactions after FL-MILK.
This study has the limitations. On the one hand, the sample size of the study is small, and there may be a certain selection bias. On the other hand, the observation time after RGP-CL wear is 2.0 ± 0.3 years, which is relatively short. However, this study provides valuable insight into the stability and safety of RGP-CL correction 2-years following the surgical FL-MILK. It is encouraging that this study demonstrates FL-MILK is a highly promising surgical intervention for progressive and advanced keratoconus, with minimal damage. Furthermore, postoperative use of RGP-CLs can enhance visual acuity, with outcomes comparable to those observed in non-operative patients. Certainly, the long-term clinical efficacy and safety necessitate further validation through prospective comparative studies.
In conclusion, FL-MILK is a safe operation for KC patients, with short recovery time postoperatively and no sutures. The corneal thickness is significantly increased and the curvature of corneal anterior surface is flatter, which stabilizes and delays the KC progression. After FL-MILK, patients can achieve good RGP-CL fitting, and the best corrected vision of RGP-CL can be improved to a level close to that of KC patients without operation. Patients with keratoconus can receive good long-term wearing comfort and high wearing safety after FL-MILK.
Data availability
The data that support the findings of the current study are available from the corresponding author upon reasonable request.
Abbreviations
- RGP-CLs:
-
Rigid gas permeable corneal contact lenses
- FL-MILK:
-
Femtosecond laser-assisted minimally invasive lamellar keratoplasty
- NIBUT:
-
Non-invasive tear film rupture time
- KC:
-
Keratoconus
- PKP:
-
Penetrating keratoplasty
- LKP:
-
Lamellar keratoplasty
- CCT:
-
Central corneal thickness
- UCVA:
-
Uncorrected visual acuity
- BSCVA:
-
Best spectacle-corrected visual acuity
- RGPCLVA:
-
RGP-CL-corrected visual acuity
- CXL:
-
Cross-linking surgery
- BLT:
-
Bowman layer transplantation
References
Seitz, B. et al. Stage-appropriate treatment of keratoconus. Ophthalmologe. 118, 1069–1088 (2021).
Mou, Y., Qin, Q., Huang, X. & Jin, X. Risk factors and severity of keratoconus on the East Coast of China. Int. Ophthalmol. 42, 2133–2140 (2022).
Dou, S. et al. Single-cell atlas of keratoconus corneas revealed aberrant transcriptional signatures and implicated mechanical stretch as a trigger for keratoconus pathogenesis. Cell. Discov. 8, 66 (2022).
Santodomingo-Rubido, J. et al. Keratoconus: an updated review. Contact Lens Anterior Eye. 45, 101559 (2022).
Chan, E. et al. Incidence and prevalence of Keratoconus based on Scheimpflug Imaging. Ophthalmology. 130, 445–448 (2023).
Gomes, J. A. et al. Global consensus on keratoconus and ectatic diseases. Cornea. 34, 359–369 (2015).
Gomes, J. A., Rapuano, C. J., Belin, M. W. & Ambrósio, R. Jr. Global Consensus on Keratoconus diagnosis. Cornea. 34, e38–39 (2015).
Li, J. et al., Parental Corneal Tomographic and Biomechanical Characteristics of Patients with Keratoconus. Am. J. Ophthalmol. 256, 146–155 (2023).
Ortiz-Toquero, S., Rodriguez, G. & Martin, R. Clinical guidelines for the management of keratoconus patients with gas permeable contact lenses based on expert consensus and available evidence. Curr. Opin. Ophthalmol. 32, S1–s11 (2021).
Barba-Gallardo, L. F., Jaramillo-Trejos, L. M., Agudelo-Guevara, A. M., Galicia-Durán, A. P. & Casillas-Casillas, E. Binocular vision parameters and visual performance in bilateral keratoconus corrected with spectacles versus rigid gas-permeable contact lenses. J. Optom. 17, 100514 (2024).
Araki, S. et al. Effect of long-term rigid gas-permeable contact lens wear on keratoconus progression. Br. J. Ophthalmol. 105, 186–190 (2021).
Maier, P., Reinhard, T. & Kohlhaas, M. Corneal collagen cross-linking in the stabilization of keratoconus. Dtsch. Arztebl Int. 116, 184–190 (2019).
Sun, L. et al. Transepithelial accelerated corneal crosslinking for keratoconus eyes with maximum keratometry values larger than 58 diopters. J. Cataract. Refract. Surg. 48, 208–214 (2022).
Gao, H. et al. Survey report on keratoplasty in China: a 5-year review from 2014 to 2018. PLoS One. 15, e0239939 (2020).
Shi, W., Li, S., Gao, H., Wang, T. & Xie, L. Modified deep lamellar keratoplasty for the treatment of advanced-stage keratoconus with steep curvature. Ophthalmology. 117, 226–231 (2010).
Janiszewska-Bil, D. et al. Comparison of long-term outcomes of the lamellar and penetrating keratoplasty approaches in patients with keratoconus. J. Clin. Med. 10 (2021).
Feizi, S. et al. Penetrating keratoplasty versus deep anterior lamellar keratoplasty for advanced stage of keratoconus. Am. J. Ophthalmol. 248, 107–115 (2023).
Gao, H. et al. Femtosecond laser-assisted minimally invasive lamellar keratoplasty for the treatment of advanced keratoconus. Clin. Exp. Ophthalmol. 50, 294–302 (2022).
Li, N. et al. Effects of femtosecond laser-assisted minimally invasive lamellar keratoplasty (FL-MILK) on mild-to-moderate and advanced keratoconus. Graefes Arch. Clin. Exp. Ophthalmol. 261, 2873–2882 (2023).
Wang, S. et al. Trends in research on corneal cross linking from 2001 to 2020: a bibliometric analysis. Clin. Exp. Optom. 106, 395–401 (2023).
Saraç, Ö., Kars, M. E., Temel, B. & Çağıl, N. Clinical evaluation of different types of contact lenses in keratoconus management. Contact Lens Anterior Eye. 42, 482–486 (2019).
Kang, H. Sample size determination and power analysis using the G*Power software. J. Educ. Eval Health Prof. 18, 17 (2021).
Belin, M. W., Jang, H. S. & Borgstrom, M. Keratoconus: diagnosis and staging. Cornea. 41, 1–11 (2022).
Duncan, J. K., Belin, M. W. & Borgstrom, M. Assessing progression of keratoconus: novel tomographic determinants. Eye Vis. (Lond). 3, 6 (2016).
Vinciguerra, R. et al. Evaluating keratoconus progression prior to crosslinking: maximum keratometry vs the ABCD grading system. J. Cataract. Refract. Surg. 47, 33–39 (2021).
Hashemi, H., Shaygan, N., Asgari, S., Rezvan, F. & Asgari, S. ClearKone-synergeyes or rigid gas-permeable contact lens in keratoconic patients: a clinical decision. Eye Contact Lens. 40, 95–98 (2014).
Fortuin, M. F. et al. Randomised controlled study comparing comfort-related outcomes between two rigid gas permeable (RGP) lenses with different sessile drop contact angles. Ophthalmic Physiol. Opt. 31, 190–199 (2011).
Li, N. et al. Effects of femtosecond laser-assisted minimally invasive lamellar keratoplasty (FL-MILK) on mild-to-moderate and advanced keratoconus. Graefes Arch. Clin. Exp. Ophthalmol. 261, 2873–2882 (2023).
Shetty, R. et al. Biochemical markers and alterations in keratoconus. Asia Pac. J. Ophthalmol. (Phila). 9, 533–540 (2020).
Pérez-Rueda, A. & Castro-Luna, G. A model of visual limitation in patients with keratoconus. Sci. Rep. 10, 19335 (2020).
Asimellis, G. & Kaufman, E. J. Keratoconus. In StatPearls (StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC., Treasure Island (FL) Ineligible Companies (Evan Kaufman declares no relevant financial relationships with ineligible companies., 2024).
Ortiz-Toquero, S. & Martin, R. Current optometric practices and attitudes in keratoconus patient management. Contact Lens Anterior Eye. 40, 253–259 (2017).
Panthier, C., Moran, S. & Bourges, J. L. Evaluation of vision-related quality of life in keratoconus patients, and associated impact of keratoconus severity indicators. Graefes Arch. Clin. Exp. Ophthalmol. 258, 1459–1468 (2020).
Durusoy, G. K. & Ozveren, M. Stabilization period for central corneal thickness, anterior chamber depth, and Iridocorneal angle parameters after deep anterior lamellar keratoplasty in keratoconus patients. Beyoglu Eye J. 6, 14–18 (2021).
Arora, R., Jain, P., Jain, P., Manudhane, A. & Goyal, J. Results of deep anterior lamellar keratoplasty for advanced keratoconus in children less than 18 years. Am. J. Ophthalmol. 162, 191–198e192 (2016).
Rocha, G. A., Miziara, P. O., Castro, A. C. & Rocha, A. A. Visual rehabilitation using mini-scleral contact lenses after penetrating keratoplasty. Arq. Bras. Oftalmol. 80, 17–20 (2017).
Deshmukh, R. et al. Post-penetrating keratoplasty astigmatism. Surv. Ophthalmol. 67, 1200–1228 (2022).
Kapur, N. et al. Preferred practice patterns for keratoconus: an e-survey among Indian cornea specialists. Indian J. Ophthalmol. 72, 111–117 (2024).
Katsoulos, C., Nick, V., Lefteris, K. & Theodore, M. Fitting the post-keratoplasty cornea with hydrogel lenses. Contact Lens Anterior Eye. 32, 22–26 (2009).
van Dijk, K. et al. Bowman layer transplantation to reduce and stabilize progressive, advanced keratoconus. Ophthalmology. 122, 909–917 (2015).
Huo, Y. et al. Biomechanical properties analysis of forme fruste keratoconus and subclinical keratoconus. Graefes Arch. Clin. Exp. Ophthalmol. 261, 1311–1320 (2023).
Dogan, C., Hagverdiyeva, S., Mergen, B. & İskeleli, G. Effect of the rigid gas-permeable contact lens use on the endothelial cells in patients with keratoconus. Eye Contact Lens. 44 (Suppl 2), S314–s317 (2018).
Acknowledgements
The authors would like to thank Ms. Tong Liu from Eye Hospital of Shandong First Medical University for her editorial and linguistic assistance.
Funding
This study was supported by National Natural Science Foundation of China (nos: 82070923 and 81870639), Taishan Scholar Program (nos: 201812150 and 20150215), and Academic Promotion Programme of Shandong First Medical University (no: 2019RC009).
Author information
Authors and Affiliations
Contributions
Author Contributions: Z. J and L. X were responsible for its design, collection of data, analysis and interpretation of results and wrote the first draft of the manuscript. G. H, D. XL and S.WY participated in its design of manuscript. L. ZZ and Z. XW were involved in data collection and statistical analysis. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Informed consent was obtained from the participants or their guardians. The study was approved by the Eye Hospital of Shandong First Medical University Research Ethics Committee (SDSYKYY20180511) and complied with the tenets of the Declaration of Helsinki.
Consent for publication
Consent for publication of the image in Fig. 1 has been obtained from the participant.
Provenance and peer review
Not commissioned; externally peer reviewed.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, J., Lin, X., Li, Z. et al. Visual rehabilitation using rigid gas permeable contact lenses after femtosecond laser-assisted minimally invasive lamellar keratoplasty in patients with keratoconus. Sci Rep 14, 25106 (2024). https://doi.org/10.1038/s41598-024-76819-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-76819-7