Abstract
Complement activation is involved in idiopathic membranous nephropathy (IMN). We aimed to investigate the relationship of serum complement cleavage factor Bb with IMN progression, and to establish a model for early prediction of kidney outcomes. We measured serum factor Bb in a retrospective cohort of 449 IMN patients at the time of kidney biopsy. Cox regression analysis showed that higher levels of serum factor Bb were independently associated with IMN progression event defined as end-stage renal disease or ≥ 40% decline in estimated glomerular filtration rate. Patients in the middle and highest tertiles of serum factor Bb had respectively 2.1-, and 2.6-fold higher risk for disease progression compared with those in the lowest tertile. We developed an optimized prognostic nomogram model incorporating age, log serum anti-PLA2R antibody, log serum Bb, proteinuria and tubular atrophy/interstitial fibrosis. The model demonstrated good predictive ability with a concordance index of 0.77 (bootstrap-corrected of 0.76) for predicting 3-, and 5-year kidney survival. Calibration curves and decision curve analysis confirmed the model’s good calibration and clinical utility. Our findings suggest that serum factor Bb may serve as an essential prognostic indicator of IMN. The novel nomogram model may offer important guidance on the management of this patient population.
Similar content being viewed by others
Introduction
Idiopathic membranous nephropathy (IMN), an autoimmune-mediated glomerular disease, is a common cause of nephrotic syndrome in adults1,2,3. It is characterized by the formation of subepithelial immune complex deposits and subsequent thickening of glomerular basement membrane (GBM). M-type phospholipase A2 receptor (PLA2R) has been identified as the major target antigen on the podocyte4,5. Although most of the IMN patients with benign course may undergo spontaneous remission or show persistent proteinuria, approximately 30–50% of patients progress to end-stage renal disease (ESRD) within 5‑15 years6,7. Therefore, the identification of risk factors associated with disease progression, especially those based on disease mechanisms, is essential for patients with IMN.
Previous studies suggested that complement activation is involved in human IMN with predominance of the classical pathway in the early stage of the disease. Notably, it is proposed that alternative pathway is activated in later stages, which is backed up by the deposits of specific complement components including factor B and properdin in glomeruli8,9. This hints that alternative pathway may play a role in the pathogenesis and development of IMN. The activation of alternative pathway occurs through proteolytic cleavage of complement factor B by factor D generating Bb and Ba fragments, leading to the formation of C3 convertase (C3bBb)10,11. The binding of a second C3b molecule to the C3 convertase generates a C5 convertase complex (C3bBb3b), which in turn lead to the production of membrane attack complex (MAC). Hence, cleavage factor Bb is considered an indicator of overall activation of alternative complement pathway.
The clinical features of proteinuria, reduced estimated glomerular filtration rate (eGFR) and persistent increased anti-PLA2R antibody (PLA2R Ab) are well-established risk factors of progression toward ESRD among patients with IMN12. Recently, circulating complement activation products has gained considerable interest as potential predictors of renal outcome subsequent from time of biopsy. Previous studies identified aberrant levels of circulating complement components in IMN, with some appearing to be associated with disease activity and prognosis13,14. Yet, the clinical implication of factor Bb in serum has not been completely elucidated.
In the current study, we retrospectively enrolled 449 IMN patients and measured serum factor Bb levels at the time of biopsy. We aimed to further clarify the role of factor Bb in predicting prognosis of IMN. Moreover, we developed a nomogram model incorporating serum factor Bb and other traditional risk factors to assess the possibility of disease progression more intuitively for IMN.
Results
Characteristics of IMN patients
The characteristics of IMN patients and measurements of serum factor Bb at the time of biopsy were summarized in Table 1. This cohort included 252 (56.1%) men and 197 (43.9%) women with a median age of 49 (interquartile range [IQR] 39–59) years. At the time of biopsy, patients had a median eGFR of 105 (IQR 95–114) mL/min/1.73 m2, proteinuria of 4.55 (IQR 2.52–8.22) g/24 h, serum albumin of 25.0 (IQR 21.5–31.0) g/L, and a mean arterial pressure (MAP) of 100 (IQR 94–109) mmHg. The median serum PLA2R Ab level was 103.5 (IQR 25.3-236.4) RU/mL, and 346 (77%) patients tested positive for PLA2R Ab as determined by ELISA, with a cutoff value of 14 RU/mL. Based on pathological findings on kidney biopsy, a total of 226 (50.3%) patients presented with MN-I, 132 (29.4%) presented with MN-II, and 91 (20.3%) presented with MN-III. Tubular atrophy and interstitial fibrosis (TA/IF) were graded as scores 0–1 in 216 (48.1%) patients, score 2 in 127 (28.3%) patients and score 3 in 106 (23.6%) patients.
The median follow-up time was 46 (IQR 29–63) months. Patients had a median time of 7 (IQR 5–9) months from biopsy to initial treatment with immunosuppressive agents; when these patients were divided into subgroups by factor Bb levels, the median time was 8 (IQR 6–9) months, 6 (IQR 5–9) months and 6 (IQR 5–8) months in patients of the lowest, middle, and highest tertiles, respectively. Overall, 305 (67.9%) patients received immunosuppressive agents. Specifically, 120 (26.7%) patients received CNI, 78 (17.4%) received CTX, and 107 (23.8%) received others. There were 139 (31.0%) patients reaching the composite disease progression event, including 17 (3.8%) ESRD events.
Clinical and histological features of IMN patients stratified by factor Bb levels
The whole patients were divided into three groups based on the tertiles of factor Bb distribution (Table 1). Patients categorized by the lowest to the highest tertile of serum factor Bb presented with increasing serum PLA2R Ab level, urinary protein excretion, and proportion of TA/IF score 3 (P < 0.001). The serum albumin levels, eGFR and proportion of TA/IF scores 0–1 were significantly lower in patients of the highest tertile of serum factor Bb compared with those in the lower 2 tertiles (P < 0.05). The proportion of MN-I was higher in patients of the lowest tertile than in the middle tertile (P < 0.05). When compared with patients of the highest tertile, the proportion of MN-II was lower in patients of the lowest tertile (P < 0.05). No significant differences were observed among the three groups with respect to MAP, the proportion of TA/IF score 2, and the proportion of MN-III.
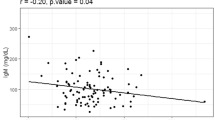
Serum factor Bb and kidney outcomes
We observed that the proportion of composite disease progression event was increased gradually in patients from the lowest tertile to the highest tertile of serum factor Bb (P < 0.001; Table 1). Kaplan-Meier survival analysis showed that the worse renal outcome was significantly associated with the higher tertile of serum factor Bb (P < 0.05; Fig. 1). Univariate Cox regression analysis found that age, serum PLA2R Ab level, albumin level, eGFR, proteinuria, intensity of TA/IF, immunosuppressive agents and serum factor Bb level were associated with kidney outcomes in IMN patients (Supplementary Table S1). After adjusting for potential confounders, patients in the highest and middle tertile of serum factor Bb had a higher risk for disease progression compared with those in the lowest tertile (the highest tertile: hazard ratio [HR] 2.592, 95% confidence interval [CI] 1.374–4.891, P = 0.003; the middle tertile: HR 2.054, 95%CI 1.076–3.920, P = 0.029; Table 2 and Supplementary Table S1). When expressed as a continuous variable, log serum factor Bb was identified as an independent predictor for IMN progression (HR 1.974, 95% CI 1.227–3.176, P = 0.005; Table 2).
Kaplan-Meier kidney survival curves of IMN patients by serum factor Bb tertiles. IMN patients were stratified into three groups based on the tertiles of serum factor Bb levels: lowest tertile < 1.21(103ng/mL), middle tertile 1.21–3.68 (103ng/mL), and highest tertile > 3.68(103ng/mL). IMN, idiopathic membranous nephropathy.
We also did a sensitivity analysis in IMN patients with serum albumin level ≤ 30 g/L or > 30 g/L, which found no significant interaction between levels of serum factor Bb and albumin on IMN progression (P for interaction > 0.05; Supplementary Table S2). Similarly, no significant interaction was observed between serum factor Bb and immunosuppressive therapy (P for interaction > 0.05; Supplementary Table S3).
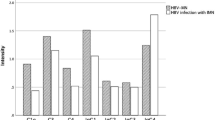
Nomogram and its validation
We developed a nomogram for predicting the 3-, and 5-year prognosis of IMN patients using multivariate Cox regression analysis by including age, log serum PLA2R Ab, log serum factor Bb, proteinuria, and TA/IF (Fig. 2). The point of each predictive factor was read out by drawing a line straight upward from the predictor to the point axis. A total point, calculated by summing each point, was then converted to kidney survival probability. The overall performance of the nomogram was assessed using bootstrap validation for internal validation. Survival analysis yielded an unadjusted concordance index (C-index) of 0.77 (95% CI 0.73–0.80) and a bootstrap-corrected C-index of 0.76, indicating adequate discriminative ability. The calibration curves showed that the nomogram-predicted progression probabilities were close to the actual progression probabilities (Fig. 3), confirming a reliable calibration ability. Decision curve analysis (DCA) indicated a positive net benefit for 5-year kidney survival over a wide range of threshold probabilities (between 0.1 and 0.9), supporting the clinical utility of the nomogram (Fig. 4).
Nomogram predicting probabilities of 3-, and 5-year kidney survival. Each independent predictive factor corresponded to a point by drawing a line straight upward to the point axis. The sum of the points located in the total points axis showing the probabilities of 3-, and 5-year kidney survival. PLA2R Ab, M-type phospholipase A2 receptor antibody; TA/IF, tubular atrophy/interstitial fibrosis.
Decision curve analysis of the nomogram: (a) for 3-year kidney survival; (b) for 5-year kidney survival. The gray solid line assumes all cases will reach disease progression event, while the black solid line assumes no cases will reach disease progression event. The dotted line represents the clinical net benefits based on the threshold probabilities.
Besides, we developed a nomogram to predict IMN progression within 5 years in patients who were followed up for more than 5 years (Supplementary Fig. S1-S2). The receiver operating characteristic (ROC) curve showed area under the curve (AUC) of 0.83 (95% CI 0.78–0.88), suggesting a good distinguishing ability. In addition, the calibration curves showed a high degree of agreement between actual observed results and predictions by the nomogram. The clinical utility of the nomogram assessed by DCA was largely in accord with our findings by survival analysis. We also calculated the risk reclassification statistics for IMN progression at 5-year. The addition of serum factor Bb to the reference model (including age, log serum PLA2R Ab, proteinuria and TA/IF) resulted in significantly improved risk reclassification as assessed by the integrated discrimination index (IDI, 0.03 [95% CI 0.01–0.05]). However, no significant improvement was observed in the net reclassification index (NRI, 0.11 [95% CI − 0.03 to 0.26]).
Discussion
In this cohort study with 449 IMN patients, we found that higher serum factor Bb values at diagnosis were associated with worse renal outcomes. Specifically, the serum factor Bb levels were positively and independently associated with IMN progression after adjusting for usual factors, including age, sex, MAP, serum PLA2R Ab, serum albumin, eGFR, proteinuria, pathological grading and immunosuppressant therapy. Importantly, we established a validated model and nomogram based on multivariate Cox regression analysis. This model, which included age, log serum PLA2R Ab, log serum factor Bb, proteinuria, and TA/IF, is of considerable significance for early prediction of renal outcomes.
Complement activation is strongly presumed to play a major role in kidney tissue injury and proteinuria in MN1,15. Previous studies in the Heymann nephritis animal models of MN demonstrated that C3 and MAC colocalized with the immune deposits, and that podocyte injury by insertion of MAC produced proteinuria16,17. Deposition of complement factor B and complement factor H were detected in glomeruli from patients with PLA2R-associated MN, suggesting that alternative pathway activation occurs in MN8,18. Factor Bb, a cleavage product of complement factor B, is critical for the formation of C3 convertase. A marked elevation of plasma Bb has been observed in MN patients compared with healthy controls, which was also linked to urinary protein excretion14.
In current study, increased serum PLA2R Ab levels and urinary protein excretion correlated with ascending tertiles of serum factor Bb in patients, while decreased serum albumin levels and eGFR correlated with the ascending tertiles. This indicates that accelerated alternative pathway activation is associated with increasing disease activity. Future experimental studies should shed light on the exact underlying mechanism of disease severity with increased levels of serum factor Bb in MN. Furthermore, the proportion of MN-I and MN-II across different groups vary. Similar findings were observed for the proportion of TA/IF scores 0–1 and score 3. These findings suggest that activation of alternative pathway may contribute to both glomerular damage and tubulointerstitial injury. Based on these observations, complement factor B may represent a potential therapeutic target for treating IMN, and further studies with respect to targeted intervention to modulate factor B function are needed. The inhibitor of complement factor B LNP023 has been shown to prevent proteinuria, attenuate glomerulopathy and prevent tubular degeneration in an experimental model of MN in rats10. Accordingly, measurement of serum factor Bb may serve as a useful biomarker for disease monitoring, and for assessing response to the potential therapy using factor B inhibitor in patients with IMN.
Although accumulating studies have examined a variety of complement components within IMN patients, few studies have focused on the prognostic impact of serum cleavage factor Bb on kidney outcome. In this study, we observed that the higher tertile of serum factor Bb was associated with a higher proportion of disease progression events in IMN. Consistently, Kaplan-Meier survival curves revealed that the renal outcome worsened with the ascending tertiles of serum factor Bb levels in IMN. Importantly, serum factor Bb level was identified as a strong and independent risk factor for IMN progression after adjusting for potential confounding factors. This association was further supported by the sensitive analysis in the subgroup stratified by baseline serum albumin level or the use of immunosuppressants after biopsy. Together, these findings demonstrate the prognostic significance of serum factor Bb in IMN. Clinicians could regard factor Bb as a routine clinical indicator to better predict disease progression and make more informed treatment decisions.
We also established a prognostic model based on multivariate Cox regression analysis, which included five variables: age, serum PLA2R Ab, serum factor Bb, proteinuria, and intensity of TA/IF. While decreased eGFR has been recommended to be a risk factor for disease progression19, the indicator of eGFR was not included in the prognostic model established in our cohort or any other studies3,20. This may be partly due to the relatively lower presence of reduced eGFR in this cohort of IMN patients at baseline (a median eGFR of 105 [IQR 95–114] mL/min/1.73 m2). Thus, our findings may facilitate early prediction of renal outcome for the patients with relatively normal eGFR, and offer important guidance for managing these patients before progressive loss of renal function. To our knowledge, the standardized prognostic models of MN has not yet been determined. This optimized model displayed a good level of discrimination and an increased IDI value when serum factor Bb was added into the reference model, which included age, PLA2R Ab, proteinuria and TA/IF. Additionally, it was shown to have good clinical utility assessed by DCA when applied to predict the probability of 5-year kidney survival. Thus, the nomogram is simple and widely applicable, which could be incorporated into the current clinical practice for management of IMN. It could contribute to identifying high-risk patients and tailoring their treatment plans more effectively. However, the benefit for clinical decision-making using this model needs to be validated in a future prospective controlled trail.
The present study showed that TA/IF significantly contributed to the prediction of renal outcome for IMN. We speculate that IMN progression is more closely related to the degree of chronic tubulointerstitial injury rather than glomerular damage. Our findings were in agreement with previous studies that have reported tubular injury as a risk factor for IMN progression3,21. The proportion of patients experiencing disease progression (139/449) was relatively high in our study, which may be partly due to severe chronic tubulointerstitial injury at baseline, unresponsive nephrotic syndrome or frequent relapse occurring in them (analyzed with additional data from our cohort)19,22. Moreover, some of the patients may be involved in another superimposed pathologic process associated with acceleration of the rate of eGFR decline.
There are several limitations in our study. First, the patients were recruited from a single center and external validation studies from other population are needed. Second, repeated measurements of serum factor Bb were unavailable during follow-up. Nevertheless, our study highlights for the first time the potential prognostic value of serum factor Bb for IMN. We then propose a novel nomogram model, consisting of serum factor Bb and other established risk factors, for the prediction of disease progression among IMN patients.
In conclusion, IMN patients with higher baseline serum factor Bb levels are at a higher risk for kidney progression. The developed nomogram model, which includes serum factor Bb as one of the risk factors, may help in providing clinical implications for the management of individual IMN patients. Therefore, the serum factor Bb levels warrant more attention, and future studies are needed to verify our findings.
Materials and methods
Patients and samples
This is a retrospective cohort study of 539 patients with MN confirmed by kidney biopsy at the First Affiliated Hospital of Zhengzhou University between March 2014 and April 2022. We excluded patients with missing baseline clinical data, follow-up data, or treatment regimens (Fig. 5). Patients with secondary MN were excluded, including malignancy, systemic lupus erythematosus and hepatitis B-related MN. All recruited patients had additional serum specimens for this research, and were followed up for at least 12 months. Ultimately, a total of 449 patients with IMN were finally included in this study.
Early morning fasting blood for assessment of factor Bb were collected from all included patients on the morning of kidney biopsy. The blood samples were centrifuged at 2000 g for 10 min and the sediment was discarded; the supernatant was stored at -80℃ until use.
This study was conducted in compliance of the Declaration of Helsinki and approved by the ethics committee of the First Affiliated Hospital of Zhengzhou University, China (Approval No: 2019-KY-361). Informed consent was obtained from all participants prior to their inclusion in this study.
Clinical and histological manifestations
The baseline clinical data were collected at the time of kidney biopsy, including age, sex, MAP, serum PLA2R Ab, serum albumin, serum creatinine and 24-h urinary protein. The use of steroids and immunosuppressive agents were in compliance with the existing KDIGO (Kidney Disease: Improving Global Outcomes) guidelines19,22. Accordingly, the patients were stratified into four groups: NO, were not treated with any immunosuppressive agents; CNI, treated with tacrolimus or cyclosporine with/without steroids; CTX, treated with cyclophosphamide with steroids; Others, treated with multiple immunosuppressive agents or immunosuppressants other than the above. The eGFR was calculated using the CKD-epidemiology Collaboration formula23.
The histopathological lesions in the renal biopsy were assessed by two independent pathologists who were blinded to patients’ clinical data. Glomerular MN lesions were classified into four stages based on the Ehrenreich and Churg’s criteria24. Accordingly, the patients were stratified into three groups: MN-I (n = 226), MN-II (n = 132), MN-III (n = 91), while no patients belonged to the group of stage IV. TA/IF were graded semi-quantitatively on a scale from 0 to 3: 0, normal; 1 (mild), < 25% of interstitial tissue affected; 2 (moderate), 25%-50% and 3 (severe), > 50%.
Outcomes
An ESRD event was defined as eGFR < 15 mL/min/1.73 m2 or need for renal replacement therapy25,26. The composite disease progression event was defined as a permanent reduction in eGFR ≥ 40% from baseline or ESRD, whichever occurred first. Those two indicated renal outcomes were confirmed by a second evaluation at least 4 weeks later.
Serum factor Bb
Serum factor Bb levels were measured by commercially available enzyme-linked immunosorbent assay kits (Quidel, San Diego, CA, USA) according to the manufacturer’ procedure. Each sample was performed in 2–3 replicates with low intra-assay and inter-assay coefficient of variations (%CV < 10–15).
Statistical analysis
The quantitative data were presented as median with IQR and compared using the Kruskal-Wallis test. Categorical data were presented as frequencies and percentages compared by chi-square test. The Kaplan-Meier analysis was conducted to derive cumulative kidney survival curves, with differences between curves analyzed with a log-rank test. Unadjusted and multivariable-adjusted Cox proportional hazards models were performed to analyze the impact of serum factor Bb on risk for disease progression in IMN. In these models, serum factor Bb levels were treated as either 3-level categorical variables (lowest, middle, and highest tertiles), or a continuous variable. Skewed distributed serum factor Bb and serum PLA2R Ab levels were log-transformed to approximate normality. The results were presented as HR and 95% CI. P values for trends in the Cox proportional hazards models were calculated by entering the median value of each tertile of serum factor Bb levels as a continuous variable. Interaction terms were performed to test the interaction of serum factor Bb with serum albumin level and with use of immunosuppression on IMN progression.
Furthermore, we developed a nomogram based on the independent prognostic factors identified from the multivariate Cox regression analysis to predict the probability of kidney survival at 3-, and 5- year in individual IMN patients. The model’s discriminative ability was assessed using the C-index with bootstrap resampling for internal validation. A receiver operating characteristic (ROC) curve was plotted, and AUC was analyzed to evaluate the model’s ability to predict IMN progression at 5 years. Calibration curve was constructed to evaluate the calibration of this model. DCA was applied to assess the clinical utility of this prediction model at different threshold probabilities by quantifying the net benefit. Moreover, NRI and IDI were calculated to assess the incremental prognostic value of serum factor Bb for 5-year kidney survival outcome after biopsy beyond traditional risk factors27,28. All statistical analysis was performed with the SPSS software (version 19.0; IBM Corp., Armonk, NY, USA) and R version 4.0.2 (http://www.Rproject.org/). A P-value < 0.05 was considered statistically significant.
Data availability
All data are available from the corresponding author upon reasonable request.
References
Couser, W. G. Primary membranous nephropathy. Clin. J. Am. Soc. Nephrol. 12, 983–997 (2017).
Gu, Y., Xu, H. & Tang, D. Mechanisms of primary membranous nephropathy. Biomolecules. 11, 513. https://doi.org/10.3390/biom11040513 (2021).
Zhang, J. et al. A nomogram for the prediction of renal outcomes among patients with idiopathic membranous nephropathy. Exp. Ther. Med. 20, 3130–3137 (2020).
Beck, L. H. Jr. et al. M-type phospholipase A2 receptor as target antigen in idiopathic membranous nephropathy. N Engl. J. Med. 361, 11–21 (2009).
Ronco, P. et al. Membranous nephropathy. Nat. Rev. Dis. Primers. 7, 69. https://doi.org/10.1038/s41572-021-00303-z (2021).
Troyanov, S., Wall, C. A., Miller, J. A., Scholey, J. W. & Cattran, D. C. Idiopathic membranous nephropathy: definition and relevance of a partial remission. Kidney Int. 66, 1199–1205 (2004).
Segal, P. E. & Choi, M. J. Recent advances and prognosis in idiopathic membranous nephropathy. Adv. Chronic Kidney Dis. 19, 114–119 (2012).
Reinhard, L., Stahl, R. A. K. & Hoxha, E. Is primary membranous nephropathy a complement mediated disease? Mol. Immunol. 128, 195–204 (2020).
Seifert, L. et al. The classical pathway triggers pathogenic complement activation in membranous nephropathy. Nat. Commun. 14, 473. https://doi.org/10.1038/s41467-023-36068-0 (2023).
Schubart, A. et al. Small-molecule factor B inhibitor for the treatment of complement-mediated diseases. Proc. Natl. Acad. Sci. U S A. 116, 7926–7931 (2019).
Oppermann, M. et al. Elevated plasma levels of the immunosuppressive complement fragment Ba in renal failure. Kidney Int. 40, 939–947 (1991).
Nafar, M., Dalili, N. & Samavat, S. Biomarkers in primary membranous nephropathy, a guide to precision medicine. Iran. J. Kidney Dis. 14, 335–347 (2020).
Liu, J., Zha, Y., Zhang, P., He, P. & He, L. The Association between Serum Complement 4 and kidney disease progression in idiopathic membranous nephropathy: a Multicenter Retrospective Cohort Study. Front. Immunol. 13, 896654. https://doi.org/10.3389/fimmu.2022.896654 (2022).
Zhang, M. F. et al. Complement activation products in the circulation and urine of primary membranous nephropathy. BMC Nephrol. 20, 313. https://doi.org/10.1186/s12882-019-1509-5 (2019).
Oto, O. A. et al. Clinical significance of glomerular C3 deposition in primary membranous nephropathy. J. Nephrol. 34, 581–587 (2021).
Lai, W. L. et al. Membranous nephropathy: a review on the pathogenesis, diagnosis, and treatment. J. Formos. Med. Assoc. 114, 102–111 (2015).
Pippin, J. W. et al. DNA damage is a novel response to sublytic complement C5b-9-induced injury in podocytes. J. Clin. Invest. 111, 877–885 (2003).
Ravindran, A. et al. Proteomic analysis of complement proteins in membranous nephropathy. Kidney Int. Rep. 5, 618–626 (2020).
Rovin, B. H. et al. KDIGO 2021 Clinical Practice Guideline for the management of glomerular diseases. Kidney Int. 100, S1–S276. https://doi.org/10.1016/j.kint.2021.05.021 (2021).
Liu, L. et al. Nomogram to predict the progression of patients with primary membranous nephropathy and nephrotic syndrome. Int. Urol. Nephrol. 54, 331–341 (2022).
Horvatic, I. et al. Prognostic significance of glomerular and tubulointerstitial morphometry in idiopathic membranous nephropathy. Pathol. Res. Pract. 208, 662–667 (2012).
Radhakrishnan, J. & Cattran, D. C. The KDIGO practice guideline on glomerulonephritis: reading between the (guide)lines–application to the individual patient. Kidney Int. 82, 840–856 (2012).
Levey, A. S. et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 150, 604–612 (2009).
Churg, J. & Ehrenreich, T. Membranous nephropathy. Perspect. Nephrol. Hypertens. 1 Pt. 1, 443–448 (1973).
Wen, L., Zhao, Z., Li, F., Ji, F. & Wen, J. ICAM-1 related long noncoding RNA is associated with progression of IgA nephropathy and fibrotic changes in proximal tubular cells. Sci. Rep. 12, 9645. https://doi.org/10.1038/s41598-022-13521-6 (2022).
Yang, X. et al. Urinary matrix metalloproteinase 7 and prediction of IgA nephropathy progression. Am. J. Kidney Dis. 75, 384–393 (2020).
Cook, N. R. Statistical evaluation of prognostic versus diagnostic models: beyond the ROC curve. Clin. Chem. 54, 17–23 (2008).
Pencina, M. J., D’Agostino, R. B. Sr., D., Agostino, R. B. Jr., Vasan, R. S. & ' & Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat. Med. 27, 157–172 (2008). (discussion 207–112).
Acknowledgements
This work was supported by The National Natural Science Foundation of China (grant number U1904208).Thank Professor Yongfu Yu for his assistance in manuscript revision.
Author information
Authors and Affiliations
Contributions
L.W., Q.L., G.C., Y.Z. and Z.Z. conceived and designed the study; L.W., Q.L., and G.C. performed experiments and collected data; L.W., G.C., Y.Z. and Z.Z. analyzed the data, draft the initial manuscript. All authors contributed to and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wen, L., Li, Q., Cheng, G. et al. Prognostic value of serum complement cleavage factor Bb in idiopathic membranous nephropathy and establishment of nomogram model. Sci Rep 14, 27266 (2024). https://doi.org/10.1038/s41598-024-78325-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-78325-2