Abstract
Cardioneuroablation (CNA) represents a promising therapy for recurrent vasovagal syncope (VVS), extrinsically driven atrioventricular block (AVB) and sinus node dysfunction (SND). However, effectiveness in patients aged 50 and above is not well-established. In this prospective study of patients referred for CNA, we compared syncope and pacemaker implantation free survival, heart rate (HR) variability (HRV) and quality of life between two age groups: group A (< 50 years) and B (≥ 50 years). A total of 50 patients were included (17 Group A and 33 Group B). The etiologies comprised VVS (56%), AVB (22%), and SND (22%). After a median follow-up of 17.0 (12.5–26.0) months, there were no differences of the combined endpoint of syncope or pacemaker implantation free-survival between groups (29.4.% vs. 21.2%; p-log-rank = 0.736). 84% of the entire cohort remained free from syncope, with a better but not significant syncope free survival in the older group (23.5% vs. 12.1%; p-log rank = 0.486). There were no differences in pacemaker implantation rate (A 5.9% vs. B 17.6%; p log-rank = 0.658). Notably, older patients had lower HR values post-procedure compared to younger patients (68.9 ± 13.3 vs. 80.4 ± 16.3 bpm; p = 0.012). Both groups exhibited a decrease in HRV parameters and an improvement in quality of life. In conclusion, CNA has comparable clinical benefits for patients aged 50 and above in terms of syncope or pacemaker implantation free survival and HRV reduction when compared to younger patients.
Similar content being viewed by others
Introduction
Endocardial ganglion plexus (GP) ablation, known as cardioneuroablation (CNA), is a technique1 with promising results in the treatment of vasovagal syncope (VVS), atrioventricular block (AVB) and sinus node disease (SND) due to parasympathetic hyperactivity2,3,4,5. The main objective is the total or partial destruction of postganglionic parasympathetic nerve fibers to attenuate the cardioinhibitory parasympathetic reflex response6,7. In recent years, there has been a spreading of the technique, with its main indication as an alternative strategy for young patients with recurrent VVS who are unresponsive to medical treatment8. However, evidence regarding its efficacy in patients over 50 years of age is limited to retrospective studies and isolated clinical cases9,10,11,12, recommending its use mainly for younger patients, while pacemaker implantation is mostly indicated for patients over 40 years of age13,14,15. Therefore, the aim of the present study was to evaluate the clinical impact of CNA in not so young patients, as well as the degree of acute and medium-term denervation.
Methods
Study population
This was a prospective, observational, single-center study that included consecutive patients with recurrent VVS, and functional bradyarrhythmias who were referred for CNA at our center. Patients were divided into two groups based on their age at the time of the procedure (group A < 50 years; group B ≥ 50). This cut off age criteria was based on previous studies assessing differences of the technique in clinical outcomes9. Minimum age for inclusion was 18 years. The inclusion criteria for patients with VVS were as follows: (1) at least one episode of syncope in the last 6 months accompanied by 3 or more presyncope episodes; (2) symptomatic cardioinhibitory component documented on a 24-hour Holter monitor or an implantable loop recorder (ILR) (asystolic pause greater than 3 s); (3) positive response to atropine test (≥ 25% increase in baseline heart rate (HR) after a dose of atropine 0.04 mg/kg if weight was less than 75 kg or 3 mg for the rest). In patients with extrinsic etiology SND, the inclusion criteria were: (1) symptoms related to bradycardia; (2) documented symptomatic sinus pauses > 3 s or daytime heart rate < 50 bpm; (3) positive response to atropine test. For patients with functional AVB, the inclusion criteria were (1) documented AVB on electrocardiogram, (2) history of presyncope or syncope; (3) absence of infra-His or intra-His AVB on electrophysiological study and (4) normalization of the AV conduction response with atropine or during treadmill exercise testing.
Exclusion criteria were any contraindication to perform an ablation procedure and the presence of relevant structural heart disease defined as moderate or severe valve disease or left ventricular ejection fraction < 50%. All patients underwent 24-hour continuous electrocardiographic monitoring to assess pre-procedure HR variability (HRV). The pre-procedure atropine test was performed at least 48 h prior CNA. Informed consent was obtained from all patients. The study was approved by the local Ethics Committee (Santiago-Lugo Research Ethics Committee) and adhered to the principles outlined in the Declaration of Helsinki.
Cardioneuroablation procedure
All procedures were performed under deep sedation with propofol and remifentanil. Baseline intervals, corrected sinus node recovery time (cSNRT), Wenckebach point, and effective refractory periods (ERP) of the RV and atrioventricular node (AVN) were measured. Subsequently, an endocardial voltage map was created using a high-density mapping catheter (Pentaray, Biosense Webster, and HD Grid, Abbot) and a non-fluoroscopic navigation system (CARTO 3, Biosense Webster, and NavX, Abbott). After the right atrial anatomical reconstruction and voltage map (low-voltage area < 0.5 mV), a catheter was placed near the jugular foramen (right or left) for extracardiac vagal stimulation (ECVS) and used as a denervation guideline after ablation of each plexus (20 V; 50 Hz; pulse width 2 ms; 6 s). Subsequently, after transeptal puncture and electroanatomical mapping of the left atrium, a purely anatomical approach was directed towards the main GP in the following order: left superior GP, superior paraseptal GP (left approach), inferior paraseptal GP (left approach), superior paraseptal GP (right approach), and inferior paraseptal GP (right approach)16. Ablation of the inferior left GP and the aortocaval GP was performed according to the operator’s discretion. The main objectives of the procedure were the absence of reproducible vagal responses with ECVS and if not feasible, an increase in baseline HR > 20% or a negative atropine test at the end of the study.
Objectives
The primary objective of the study was to evaluate differences in the combined endpoint of syncope or pacemaker-free survival between the two age groups. Secondary objectives of the study included differences in syncope-free survival, syncope incidence (episodes per year) in patients with history of syncope, pacemaker-free survival, along with the degree of denervation based on (1) HRV evaluated by 24-hour monitoring at 6 months, (2) acute HR increase after the procedure and (3) pre- and post-procedure atropine tests. To evaluate changes in HRV during 24-h monitoring time-domain and frequency-domain parameters were used. In patients with available data, HRV with the atropine test at 6 months was also evaluated. Finally, differences in quality of life at 6 moths using the SF-36 questionary were assessed.
Follow-up
The occurrence of syncope or presyncope and its incidence were assessed through telephone and face-to-face interviews. A standardized SF-36 questionary at 6 months was performed. In patients with ILR, device interrogation was performed at 3 and 6 months as well. All patients underwent 24 h-ECG monitoring at 6 months. Atropine test was performed at six months with the same dose employed in the initial test.
Statistical analysis
Continuous variables were summarized as mean ± standard deviation (SD) or median and range depending on their normality assessed with the Shapiro-Wilk test. Categorical variables were described as percentages and compared using the chi-square or Fisher’s exact tests. The comparison of continuous variables before and after the procedure was performed using Student’s t-test or Wilcoxon signed-rank test for paired data. The comparison of categorical variables before and after the procedure was done using the McNemar test. Syncope and pacemaker free survival between groups was performed using Kaplan–Meier survival analysis and the log-rank test. Statistical analyses were performed using version 15.1 of the STATA software (https://www.stata.com/). The significance level was set at p < 0.05.
Results
Study population
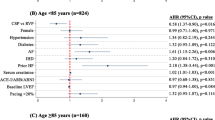
A total of 50 patients were included in the study, 17 in Group A and 33 in group B. The mean age in both groups was 42.8 ± 6.5 and 61.8 ± 9.7 years, respectively. Within the older age group, 19 (57.6%) patients were between 50 and 60 years old, 6 (18.2%) between 60 and 70 years old, and 8 (24.2%) between 70 and 80. The main indication for the procedure was recurrent VVS in both groups (A: 70.6% vs. B: 48.5%), however, in group B there was a significant proportion of patients with functional SND (33.3%). Moreover, a higher percentage of patients in group B presented carotid sinus hypersensitivity (42.4%). A total of 26 patients (52%) were continuously monitored with an ILR, all of whom had significant pauses > 3 s recorded prior CNA (Table 1).
Regarding HRV, there were differences between groups in frequency-domain parameters, with a significant lower HRV in group B. In the Valsalva test, greater HRV was observed in group A, which was not as pronounced in the deep inspiration test. There were no differences in the relative increase in HR after atropine infusion, although older patients reached a lower maximum HR (Table 2).
Cardioneuroablation procedure
ECVS was used in 33 patients (66.0%), but in only 48.5% of them, it was feasible or reproducible to guide the degree of denervation. There were no differences in the percentage of vagal responses observed with ECVS between groups (42.9% vs. 52.6%; p = 0.579). The localization of the GP was performed using a purely anatomical biatrial approach in all patients. The superior paraseptal GP was approached biatrially in 100% of patients, with a sustained increase in HR observed in 91.5% of cases. The mean increase in HR after ablation of this GP was 54.3 ± 9.4 to 71.1 ± 14.2 bpm (p < 0.001), with a greater maximum HR observed in group A (from 56.8 ± 11.8 bpm to 75.6 ± 17.3 bpm; p < 0.001) compared to the group B (from 53.2 ± 8.0 bpm to 69.1 ± 12.4 bpm; p < 0.001). Furthermore, the left superior GP was ablated in 98.0% of patients, with significant pauses (> 3 s) achieved in 44% of them. As for the inferior paraseptal GP, it was approached in 94.0% of cases, with a biatrial approach in 78.4%. There was no significant increase in HR after ablation of this two GP. Regarding the other GPs, the left inferior and the aorto-caval GP were approached in 36% and 18% of cases, respectively. Furthermore, there was a higher proportion of patients with some type of low-voltage area in the older age group, but not significant (Table 1).
After the procedure, no vagal responses were noted with ECVS in any of the patients in whom ECVS could be reliably performed and a significant increase in HR was observed (55.5 ± 11.0 to 72.8 ± 15.4; p < 0.001) in the cohort. A HR variation greater than 20% from baseline was observed in 72% of the patients, with no differences between groups (p = 0.873). Post-procedural HR was higher in younger patients (80.4 ± 16.3 bpm vs. 68.9 ± 13.3 bpm; p = 0.012). However, although the relative increase in HR after the procedure was smaller in patients ≥ 50 years, no significant differences were observed between the groups (A: 36.5 ± 27.1% vs. B: 31.5 ± 24.9%; p = 0.522).
At the end of the procedure, all patients underwent an atropine test to assess the degree of denervation. In 4 patients (8.5%), 2 from each group, an increase in HR greater than 25% was observed with the drug. Only one patient who could not be monitored with ECVS had a HR increase less than 20% and a positive atropine test at the end of the procedure, confirming an unsuccessful denervation. There was a significant reduction in the relative increase in HR post atropine after the procedure compared to previous in the cohort (post: 7.1% (2.6–13.9) vs. pre: 62.3% (45.6–78.6); p < 0.001). These differences were similar for both the group B and group A. There were no significant differences in the relative increase in HR after post-CNA atropine between the two age groups (Table 3).
Regarding baseline intervals, a significant decrease in the AH interval was observed in the group A (p = 0.019), but not in group B (p = 0.346). Concerning the AVN ERP, a decrease was observed in both groups, with a similar influence in the Wenckebach point (Supplemental Table 1, supplementary appendix).
Lastly, only one patient experienced procedure-related complications; a young woman experienced transient SND (nodal rhythm) after ablation of the superior right GP17. This dysfunction was transient, and normal sinus rhythm (with a higher HR than baseline) was restored within 24 h of the procedure.
Follow-up
Primary objective
After a median follow-up of 17.2 (12.5–26.0) months, a total of 12 (24.0%) patients had syncope recurrence or needed pacemaker implantation 8 (16%) patients suffered from syncope and 4 (8%) patients required pacemaker implantation). There were no differences of the combined endpoint of syncope or pacemaker implantation free-survival between groups (29.4.% vs. 21.2%; p-log-rank = 0.736) (Fig. 1).
Syncope recurrence
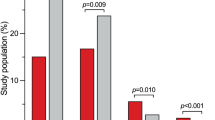
Overall, 84% of patients remained free from syncope. A total of 8 patients (50% group A and 50% group B) with a history of previous syncope experienced syncope recurrence in the long-term follow-up. In all cases, these were patients with recurrent VVS who were monitored with an ILR, and no asystole or cardioinhibitory component was documented during the episodes, suggesting a vasodepressor mechanism. Patients in the older group, had better syncope-free survival (23.5% vs. 12.1%; p-log rank = 0.486) albeit not significant. Moreover, there was a reduction in the number of syncope episodes per year (pre 2.6 (0.8–15.2) vs. post 0(0–0), p < 0.001), significant for both group B (pre: 2.1 (0.8–16.6) vs. post: 0 (0–0), p < 0.001) and group A (pre: 4.1 (1.2–13.9) vs. post: 0 (0–0), p < 0.001). In patients monitored with an ILR, only one patient experienced significant pauses (> 3 s) during follow-up, demonstrating a decrease in the annual incidence of cardioinhibitory events (pre: 3.6 (1.9–15.7) vs. post: 0 (0–0), p < 0.001). Furthermore, there was a decrease in the percentage of patients experiencing presyncope after CNA (98% vs. 26%, p < 0.001). This difference was significant for both group A (94.1% vs. 35.3%, p = 0.005) and B (100% vs. 21.2%, p < 0.001).
Pacemaker implantation
Regarding pacemaker-free survival, no significant differences were observed among groups (p-log-rank = 0.658). Four patients required pacemaker implantation after the procedure, one (5.9%) patient in the younger age group with recurrent symptomatic paroxysmal AV block despite two attempts of CNA and 3 (17.6%) in the older group; a 66-year-old patient with persistent nodal rhythm after the procedure, a 79-year-old male with persistent bradycardia and asthenia and 66-year-old-female with episodes of presyncope and persistent bradycardia.
HRV and atropine test
A significant increase in minimum HR was observed in both groups, while mean HR only increased significantly in patients in group B (Table 4). There were no differences in maximum HR pre- and post-procedure in any group. As for HRV, a significant decrease was observed in the main parameters evaluating variability in both groups in time-domain and frequency -domain parameters (Table 4; Fig. 2).
Evaluation of minimum, maximum, and mean HR, as well as HRV, pre-procedure, at 6 months and at 12 months. (A) Minimum HR, (B) Median HR, (C) Maximum HR, (D) SDNN (SD of NN intervals), (E) PNN50% (percentage of successive RR intervals that differ by > 50 ms), (F) RMSSD (root mean square of successive RR interval differences), (G) VLF (absolute power of the very-low-frequency band (0.0033–0.04 Hz)), (H) LF (absolute power of the low-frequency band (0.04–0.15 Hz)), (I) HF (absolute power of the high-frequency band (0.15–0.4 Hz)). CNA cardioneuroablation, HR heart rate.
Finally, a total of 35 patients underwent a repeat atropine test at six months. A decrease in the absolute increase in HR and relative HR variation was observed at six months compared to pre-procedure in both groups, with a slight tendency towards an increase in values compared to the acute post-procedure measurement (Table 5; Fig. 3).
Quality of life
There was an increase in most items in the SF-36 questionary which was significant in the physical function and health change items in the overall cohort at 6 months. This was due to a significant increase in the physical function item in the older group, and to a significant increase in the health change items in both groups (Fig. 4).
Discussion
This is the first study to date evaluating differences in syncope and pacemaker-free survival, response to atropine test, and HRV parameters in patients referred for CNA based on age. The main findings of our study were: (1) The clinical impact on syncope recurrence or pacemaker implantation was similar in both groups; (2) the relative increase in HR during the atropine test before and after the procedure did not differ between groups; (3) older patients had a lower post-procedure HR, but this did not result in a different response to atropine or worse prognosis and; (4) the degree of denervation at six months post-procedure, evaluated by HRV and atropine test, was also similar.
From our perspective, these results are clinically relevant due to the existing evidence regarding its effectiveness in patients over 50 years, mainly limited to isolated case reports and two retrospective studies. Qin et al. retrospectively compared HRV and clinical impact using a quality-of-life questionnaire in a cohort of symptomatic sinus bradycardia patients based on age (< 50 years vs. ≥50 years) after CNA9. In this study, the older age group consisted of 23 patients with a mean age of 58.3 ± 8.1 years (slightly lower than the mean age of 61.8 ± 9.7 years in our cohort), showed less improvement in the SF-36 quality-of-life questionnaire, suggesting that the procedure may be more effective in younger patients. Additionally, in this study, a smaller absolute increase in minimum and median HR was observed in the follow-up Holter monitoring in the group over 50 years old. It differs from our results, where minimum HR increased in both groups and remained similar at six months follow-up. This discrepancy may be explained by the heterogeneity of our cohort, with a lower proportion of patients with extrinsic SND in our older age group compared to Qin’s study. On the other hand, Francia et al. recently assessed the efficacy of CNA in a cohort of 60 patients, categorized into three groups: 14 young individuals (18–40 years old), 26 middle-aged individuals (41–60 years old), and 20 older individuals (over 60 years old)12. After 8-months, no significant differences in syncope-free survival were observed. However, when comparing patients younger than 40 years old to those older, there was a tendency toward lower syncope-free survival in the older group, but not significant. This contrasts with our results, where older patients exhibited better syncope-free survival, although this difference was not significant. The reason for this inconsistency remains elusive and requires further investigation. One plausible explanation could be that in younger patients, the autonomic nervous system (ANS) plays a more substantial role compared to older patients. This differential involvement might impact clinical outcomes, resulting in fewer cardioinhibitory events in older patients. In fact, older patients in our cohort had fewer number of syncope events per-year prior CNA. Additionally, achieving complete denervation in younger patients could be challenging due to their increased neural innervation compared to older patients. On a different note, in this study, both young and middle-aged patients exhibited a significant increase in mean HR at 1 and 3–6 months, which persisted over time. However, this increase was less pronounced and not sustained at 3–6 months in older patients. This finding differs from our results, where minimum HR at six months remained elevated in both groups. Nevertheless, we report frequency and time-domain HRV parameters that are consistent with our findings.
To understand the potential benefit of CNA in older patients, it is important to consider changes in the pathophysiology of the ANS with age and its effect on HR. The sinus node is a structure deeply innervated by sympathetic and parasympathetic axons18. Aging leads to degenerative changes not only in the ANS (extrinsic component) but also at the structural level (intrinsic component), resulting in a decrease in intrinsic HR19. The ANS undergoes a global decrease in both parasympathetic and sympathetic autonomic innervation of the sinus node but an increase in sympathetic tone with greater noradrenaline release and a global decrease in parasympathetic tone20,21. This decrease in parasympathetic tone with age has been suggested as a physiological compensation for the decrease in intrinsic HR22. On the other hand, with increasing age it seems to be a shift toward less cardioinhibition and more vasodepression in patients with tilt test induced VVS according to a recent study23. Due to these factors and the limited evidence for the procedure in older patients, some authors propose limiting the indication of the procedure to individuals under 60 years old16. However, in our study, the clinical benefit was similar in both groups (including the 14 patients over 60) despite a lower post-procedure HR in the older age group. Therefore, we suggest that the indication for CNA should be based more on the pre-procedure atropine test and autonomic functional testing rather than a specific age limit, as some symptomatic patients aged 50 or older with a predominant vagal tone may benefit from the procedure.
In our study, patients of older age had lower HR values post-procedure with a trend towards a smaller relative increase in HR. It is worth noting that acute HR increase could not be the best endpoint for appropriate denervation after the procedure, and there is no clear established cutoff point. The absence of vagal response to ECVS is likely the best endpoint of the procedure24. In a study involving 48 patients (mean age 39 ± 13 years), denervation of the sinus node with ECVS was evaluated and correlated with HR increase25. The authors found no correlation between HR increase and age or between HR increase and pre-procedure atropine test. Furthermore, no differences in HR increase were found between patients who achieved adequate denervation assessed by ECVS and those who did not. In our series, the relative HR increase did not differ between both groups in the pre- and post-procedure atropine test, despite a lower maximum HR in the older group. Based on the aforementioned considerations, we believe that older patients may have a smaller expected HR increase after the procedure. This should be taken into account when considering it as the final endpoint in CNA procedures, especially in extrinsic SND.
Regarding the long-term degree of denervation, our cohort showed a decrease in HRV at six months and an attenuated response to atropine in both groups. This is consistent with the findings of Pachon et al.26, where a decrease in parameters evaluating HRV by time-domain and frequency-domain methods was observed and persisted at two years. However, the mean age in their study was 47.3 ± 17 years, closer to our young age group, without differences based on age.
Limitations
The conclusions of our study need to be analyzed considering several limitations, mainly due to the small number of patients, which prevents generalizability to the general population. Firstly, the 50-year cut-off point is still an arbitrary threshold. However, in our modest opinion, we believe it is a reasonable cut-off, as it has been used in previous studies9 and falls within the currently recommended age limits for pacemaker implantation (> 40 years in vasovagal syncope in the most recent guidelines13 and > 60 years for cardioneuroablation in the most recent consensus document27), although we acknowledge that these thresholds are not based on robust scientific evidence. Additionally, the sample was heterogeneous in terms of indication, with a higher percentage of patients with recurrent VVS in the younger group and more patients with extrinsic SND and carotid sinus hypersensitivity in the older age group, which could have led to different clinical outcomes. However, the main endpoint of the study was a combined endpoint of syncope recurrence and pacemaker implantation trying to balance clinical outcomes in both groups (more expected syncope recurrence in VVS and more expected pacemaker implantation in SND). In addition, the aim of the study was to evaluate the clinical impact of CNA based on age and the degree of denervation, regardless the type of indication. On the other hand, there could have been a placebo effect after the procedure, however there was a clear objective effect in patients with ILR. Regarding HRV, the follow-up was limited to 12 months, and no conclusions can be drawn for longer periods. The limited response to ECVS in our study compared to other series, could be possibly due to the low voltage used (20 V).
Conclusions
In our experience, the degree of denervation evaluated by means of the atropine test and the decrease in HRV after CNA were similar in patients ≥ 50 compared to patients < 50 years old, indicating that the procedure is safe and effective in selected individuals. Furthermore, there were no differences in the clinical impact of the procedure between the two age groups in terms of syncope recurrence or pacemaker implantation. However, the current evidence regarding the technique’s effectiveness in this age group is limited, and it is necessary to conduct prospective randomized studies with longer follow-up periods to evaluate its efficacy.
Key points
What is known? Cardioneuroablation is a promising therapy in young patients with vasovagal syncope or functional bradyarrhythmias.
New contributions Cardioneuroablation could be a reasonable option in patients older than 50 years old with vasovagal syncope and functional bradyarrhythmias.
Data availability
The data that support the findings of this study are available on request from the corresponding author, [CMC].
References
Pachon, M. Cardioneuroablation’—new treatment for neurocardiogenic syncope, functional AV block and sinus dysfunction using catheter RF-ablation. Europace. 7, 1–13 (2005).
Aksu, T., Gopinathannair, R., Bozyel, S., Yalin, K. & Gupta, D. Cardioneuroablation for Treatment of Atrioventricular Block. Circ. Arrhythmia Electrophysiol. 14, 841–850 (2021).
Vandenberk, B. et al. Cardioneuroablation for Vasovagal Syncope – a systematic review and Meta-analysis. Hear. Rhythm (2022).
Debruyne, P. et al. Unifocal Right-Sided Ablation Treatment for Neurally Mediated Syncope and Functional Sinus Node Dysfunction under computed Tomographic Guidance. Circ. Arrhythm. Electrophysiol. 11, e006604 (2018).
Piotrowski, R., Baran, J., Sikorska, A., Krynski, T. & Kulakowski, P. Cardioneuroablation for Reflex Syncope. JACC Clin. Electrophysiol. 9, 85–95 (2023).
Wink, J. et al. Human adult cardiac autonomic innervation: controversies in anatomical knowledge and relevance for cardiac neuromodulation. Auton. Neurosci. Basic. Clin. 227, (2020).
Fedele, L. & Brand, T. The intrinsic Cardiac Nervous System and its role in Cardiac Pacemaking and Conduction. J. Cardiovasc. Dev. Dis. 2020. 7, 54 (2020).
Pachon, J. C. et al. Cardioneuroablation: where are we at? Hear. Rhythm O 20 (2023).
Qin, M. et al. Atrial Ganglionated Plexus modification: a Novel Approach to treat symptomatic sinus Bradycardia. JACC Clin. Electrophysiol. 3, 950–959 (2017).
Minguito-Carazo, C. et al. Changes in autonomic response during cardioneuroablation in an elderly patient with carotid sinus syndrome. Hear. Case Rep. https://doi.org/10.1016/J.HRCR.2022.08.010 (2022).
Štiavnický, P., Wichterle, D., Hrošová, M. & Kautzner, J. Cardioneuroablation for the treatment of recurrent swallow syncope. EP Eur. 22, 1741 (2020).
Francia, P. et al. Clinical impact of aging on outcomes of cardioneuroablation for reflex syncope or functional bradycardia: results from the cardionEuroabLation: patiEnt selection, imaGe integrAtioN and outComEs—The ELEGANCE multicenter study). Hear. Rhythm. 20, 1279–1286 (2023).
Glikson, M. et al. ESC Guidelines on cardiac pacing and cardiac resynchronization therapyDeveloped by the Task Force on cardiac pacing and cardiac resynchronization therapy of the European Society of Cardiology (ESC) With the special contribution of the European Heart Rhythm Association (EHRA). Eur. Heart J. 42, 3427–3520 (2021).
Brignole, M. et al. 2018 ESC guidelines for the diagnosis and management of syncope. Eur. Heart J. 39, 1883–1948 (2018).
Shen, W. K. et al. 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope: a report of the American college of cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society. Circulation. 136, e60–e122 (2017).
Brignole, M. et al. Clinical controversy: methodology and indications of cardioneuroablation for reflex syncope. EP Eur. https://doi.org/10.1093/EUROPACE/EUAD033 (2023).
Scanavacca, M. et al. Sinus node artery occlusion during Cardiac Denervation procedures. JACC Case Rep. 4, 1169–1175 (2022).
Aksu, T., Gopinathannair, R., Gupta, D. & Pauza, D. H. Intrinsic cardiac autonomic nervous system: what do clinical electrophysiologists need to know about the heart brain? J. Cardiovasc. Electrophysiol. 32, 1737–1747 (2021).
Peters, C. H., Sharpe, E. J. & Proenza, C. Cardiac pacemaker activity and aging. (2020). https://doi.org/10.1146/annurev-physiol-021119-034453 82, 21–43
Esler, M. et al. The influence of aging on the human sympathetic nervous system and brain norepinephrine turnover. Am. J. Physiol. - Regul. Integr. Comp. Physiol. 282, (2002).
Kuga, K., Yamaguchi, I. & Sugishita, Y. Age-relaterd changes of sinus node function and autonomic regulation in subjects without sinus node disease —Assessment by Pharmacologic Autonomic Blockade—. Jpn Circ. J. 57, 760–768 (1993).
Choi, S., Baudot, M., Vivas, O. & Moreno, C. M. Slowing down as we age: aging of the cardiac pacemaker’s neural control. GeroScience 2021 441. 44, 1–17 (2021).
van Dijk, J. G. et al. Influence of age on magnitude and timing of Vasodepression and Cardioinhibition in Tilt-Induced Vasovagal Syncope. Clin. Electrophysiol. 8, 997–1009 (2022).
Pachon, M. Simplified method for Vagal Effect evaluation in cardiac ablation and electrophysiological procedures. JACC Clin. Electrophysiol. 1, 451–460 (2015).
Wichterle, D. et al. P1097Heart rate acceleration is a poor surrogate of complete parasympathetic denervation of sinus node during cardioneuroablation. EP Eur. 22 (2020).
Pachon-M, J. C. et al. Long-term evaluation of the Vagal Denervation by Cardioneuroablation using Holter and Heart Rate Variability. Circ. Arrhythmia Electrophysiol. 13, E008703 (2020).
Aksu, T., Morillo, C. A. & Sutton, R. Pacing or ablation for vasovagal syncope: one size does not fit all. Eur. Heart J. 44, 2443–2446 (2023).
Funding
This work was supported by a grant of the Spanish Society of Cardiology and the Spanish Heart Rhythm Association (SECARIT-FOR-NAC 21/002).
Author information
Authors and Affiliations
Contributions
C.M.C collected the data, performed the statistical analysis and prepared the manuscript. J.D.M.A , J.L.M.S, J.G.S, O.S, I.L.E, T.G.F, J.E.T, M.A.P.V, X.A.F.L., J.R.G.J reviewed the manuscript. M.R.M reviewed and prepared the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Minguito-Carazo, C., Martínez-Alday, J.D., Martínez-Sande, J.L. et al. Effect of age on clinical impact and mid-term denervation in patients undergoing cardioneuroablation. Sci Rep 14, 27546 (2024). https://doi.org/10.1038/s41598-024-78665-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-78665-z
Keywords
This article is cited by
-
Older age is not an independent predictor of syncope recurrence following cardioneuroablation for reflex syncope
Journal of Interventional Cardiac Electrophysiology (2025)